Dallas, Texas, was founded in 1841 by John Neely Bryan on the east bank of the Trinity River (1). In 1842 he married Margaret Bryan (Figure 1). He was 33 years old and she was 18. Mr. Bryan had earlier been in Arkansas and wandered into Texas as early as 1839. It was not until 1844 that a surveyor laid out lots of one-half mile by one-half mile. He advertised the town but after 7 years had sold only 86 lots. Mr. Bryan left for the California gold fields in 1849. He returned to Dallas in 1851 and in 1852 sold his townsite real estate to Alexander Cockrell for $7000 (2). During his lifetime he sold most of his land at relatively cheap prices and thus did not profit from his real estate.
Figure 1.

John Neely Bryan, founder of the city of Dallas, with wife, Margaret. From the collections of the Texas/Dal las History and Archives Division, Dallas Public Library.
In 1842, Dr. Calder became the area's first physician. He settled at Cedar Springs and was killed by Indians the following year in Collin County. In May 1843, Dr. John Cole, originally from Virginia, moved to Dallas from Fayetteville, Arkansas. Cole Avenue, the street where he practiced, was named for him in 1882 following his death in 1850. Early physicians often had other jobs, mostly as farmers, as Dr. Cole had been. There was no surgical specialty since all physicians were known as physicians and surgeons. There were no hospitals, and physicians might ride a horse several miles to get to their patients.
The Republic of Texas had already passed a law creating a Board of Medical Censors on December 14, 1837. The board met annually to evaluate credentials and reputations of physicians (3). Four years after Dallas was founded, Texas became the 28th state under the governorship of Sam Houston. The following year, 1846, Dallas was named temporary seat of Dallas County, which was named for Vice President George Mifflin Dallas. The city was not officially incorporated until 1856.
MEDICINE IN DALLAS, 1850–1875
The population of Dallas in 1850 was approximately 1000, with 430 families (3). The primary industries were cotton production and railroad transportation. It was fairly easy to get into medical school by today's standards, since only a high school diploma or the equivalent was required—and that meant applicants could have as few as 8 or 10 high school credits. Medical school was only 2 years; thus, a student could have a diploma of medicine 2 years after high school graduation. However, to practice medicine it was not necessary to have a diploma but merely to appear before a district board appointed by some judges and successfully answer some questions. Students who passed the examination were eligible to legally practice medicine. Many physicians—including Dr. Charles M. Rosser, who was considered the founding father of Baylor University College of Medicine–practiced medicine between their first and second years of medical school. This was a common way to finance medical school education. Dr. Rosser returned to the University of Louisville to finish his second year of medical school in 1888 (4).
When a physician received a diploma, it was registered with the county clerk or with the health officer. The physician received some ethical instruction and could be called a “specialist,” although none were trained as such. These “specialists” were much more at ethical risk than so-called “primary care physicians.” There were some ethical restrictions: for example, Dr. Daniel W. Momand was severely reprimanded for attempting an operation on a horse (4).
Physicians performed the only operations known to pioneers, which were amputations and treatment of wounds in the home. Even appendectomies were not performed. Physicians were informed that the average office fee was $1 and a home visit was $2. If they traveled out of city limits by horseback, they could charge 50¢ per mile. They carried their drugs with them since the first drug store in Dallas was not established until 1855 by Frank A. Sayre. It was located at the corner of Houston and Main on the west side of the city square. The first railroad came to Dallas in 1872, which later accounted for explosive growth of the city (5).
In 1874 the first City Hospital was built (Figure 2). Prior to this, hospitals were in shacks. The City Hospital was a single room built on a piece of property owned by Mr. Long, which was sold for $1000. The building was approximately 50 × 50 feet, housed 18 people in one room, and cost $250 to build. It was located on the corner of South Lamar and Columbia Streets. Later a woman's facility and kitchen were added. There was no indoor plumbing, and sewerage was a problem. No one was available to pick up dead animals. The city health officer was the one primarily responsible for the hospital.
Figure 2.
Dallas' first City Hospital, built in 1874. Photo courtesy of Parkland Health and Hospital System.
SURGERY IN DALLAS, 1875–1900
By 1870 the population of Dallas was 3000, and by 1890 it was 38,000, making Dallas the largest city in Texas (1) (Figure 3).
Figure 3.
Downtown Dallas about 1873. Photo courtesy of the Center for American History at the University of Texas.
Dr. Henry Keirn Leake (1875)
The first private infirmary in Dallas was constructed in 1875 and was owned by Dr. Hughes and Dr. Henry K. Leake. Dr. Leake had moved to Dallas that year and began to specialize in surgery as a field separate from general medicine. He is credited with moving surgery from the home into the hospital. Dr. Leake was a pioneer surgeon and specialist in Dallas and the Southwest prior to 1900 (Figure 4). He was born in Yazoo City, Mississippi, in 1847. He was a member of the Confederate Army in Alabama and attended medical school at Louisville Medical School from 1867 to 1869, approximately 20 years before Dr. Charles M. Rosser. Dr. Leake founded the Leake Sanitarium for surgical cases in the early 1890s and was one of the first physicians in the Southwest to perform an appendectomy. The first appendectomy in the USA was not performed until around 1887. He had trained in London under Dr. Lawson Tate and received additional training in Berlin, New York, and the Mayo Clinic from 1885 to 1890. It was common for many physicians from Dallas to spend a few months at the Mayo Clinic and come back to Dallas as a so-called “specialist” in some particular area. Eventually, when St. Paul Hospital opened on June 15, 1898, Dr. Leake was the first chief of surgery (6). In addition to being president of the Texas State Medical Association, Dr. Leake was also editor of Texas Medical Record. He died in Dallas on October 30, 1916, and is buried in Greenwood Cemetery.
Figure 4.

Dr. Henry K. Leake.
The Dallas County Medical Surgical Association (1875)
The Dallas County Medical Surgical Association was founded in 1875 but lasted only 3 or 4 years. It was a forerunner of the Dallas County Medical Society (7). On April 1, 1876, the Dallas County Medical Society held its first meeting, and its first president was Dr. Albert Johnston. To be a member, the physician and surgeon had to have a diploma from a regularly constituted medical college recognized as such by the American Medical Association (AMA). The purpose of the organization was to establish a uniform fee for doctors to guarantee citizens against excessive charges. One of its original members was Dr. S. D. Thurston. The group met once a week in doctors' offices, which were usually over drugstores or dry goods stores (8). The name was changed to the Dallas County Medical and Surgical Society on August 8, 1876, but the organization disbanded in 1879.
Dallas County Medical Society (1884)
In 1884 the Dallas County Medical Society that we know today was established. Its first meeting was held on April 3,1884, in the offices of Dr. Robert Henry Chilton and Dr. Joseph H. Smith. After the first few meetings in Dr. Chilton's office, the 30 members of the 37 eligible candidates began to meet in the basement of City Hall at the present site of the Adolphus Hotel. The first president of the Dallas County Medical Society was Dr. John Morton, 1884–1887, who died in office on July 18, 1887. Dr. Morton was born in Rutherford County, Tennessee, in 1831 and graduated from the University of Pennsylvania Medical School. He served in the Russian Army and moved to Dallas in 1875, opening an office at 602 Main Street. Many of the physicians at that time practiced on Main Street and Lamar Street (9).
First trained surgical specialist in Dallas (1880)
Dr. Robert Henry Chilton came to Dallas in 1880 and was the only trained specialist in Dallas in the 1880s as an eye, ear, nose, and throat specialist. He was born in Cumberland County, Kentucky, in 1844 and started practicing medicine in 1864 at age 21 years, but he did not graduate from Miami Medical College in Cincinnati until 1870. Dr. Chilton had studied ophthalmology and otolaryngology at the University of Louisville and served on the staff of the City Hospital (10).
Pest houses (1876, 1882)
In 1876 and 1882, there were pest houses—which were usually shacks—primarily for the purpose of taking care of smallpox patients (11). However, in 1907, the Union Hospital was constructed about 4 miles from Main Street and took the place of the pest houses (Figure 5).
Figure 5.
Union Hospital, built in 1907. Photo courtesy of Parkland Health and Hospital System.
Stock market crash (1878)
There was a huge stock market crash in 1878. The Dow Index dropped from 55 to 20, far from the 9000 to 11,000 we know today. Some of the rail line stocks dropped 60%. By 1881 telephone exchanges opened in Dallas (1).
Germ theory (1885)
By 1885 there were 65 physicians in Dallas (12). They did not accept the “germ theory,” and there was no asepsis. It was not until 1890 that physicians even wore gloves during surgery. They commonly walked from one surgical procedure to another without even washing their hands.
St. Paul Hospital (1898)
The physicians in Dallas wanted a larger hospital with an open staff. Dr. C. M. Rosser and some other physicians petitioned the Sisters of Charity of Emmitsburg, Maryland, to open a general hospital in Dallas. They eventually agreed to do this, and in 1896 the hospital was chartered. The main St. Paul Hospital opened on June 15, 1898, with 110 beds (Figure 6). This was important because it was the first facility to have an open staff. Dr. Henry K. Leake was the first surgeon in chief.
Figure 6.
St. Paul Hospital. Photo courtesy of St. Paul Hospital.
By 1900, Dallas had a population of 42,638, and the population almost doubled every decade. There were 146 physicians, and during the first decade of the century, 8 medical schools were organized in Dallas. In Texas, the University of Texas Medical Branch at Galveston, organized in 1891, is the only school still in existence that was established before 1900.
Dr. V. P. Armstrong and the first Parkland Hospital (1894)
Dr. Charles M. Rosser was city health officer in 1891. In that year, Dr. Rosser was surgeon and chief at the Dallas City Hospital. Dr. V. P. Armstrong moved to Dallas in 1890 and went into practice with Dr. Rosser. Dr. Armstrong became health officer in 1892 following Dr. Rosser (Figure 7). He recognized the poor sanitary conditions that existed and finally convinced the city council to appropriate money to build a new hospital. Dr. Armstrong is credited with the development of the first Parkland Hospital, which opened on May 19, 1894, on 17 acres of park land at the corner of Maple and Oak Lawn (Figure 8). The newspaper ad stated that it was “the most elegant in the state and for terms of admission as to surgical cases, inquiries should be addressed to Dr. V. P. Armstrong who is 'Surgeon in Chief.'” Therefore, Dr. V. P. Armstrong was the first chief of surgery at the first of three Parkland Hospitals in Dallas.
Figure 7.

Dr. V. P. Armstrong.
Figure 8.
The first Parkland Hospital, about 1895. Photo courtesy of the Dallas Public Library.
All patients admitted after March 14, 1894, had to be bona fide residents of the city of Dallas, although eligibility has since been expanded to residents of Dallas County. Parkland Hospital was 2 stories and had 100 beds. There were 6 separate wards: one for white women, one for black women, one for white men, one for black men, one for children, and one for maternity cases. The single operating room had a cement floor. Dr. Armstrong, the county health officer, and his family lived in the hospital. The charge for a private room was $7 to $12 per week.
Dr. Armstrong was born in Davidson County, Tennessee, on February 18, 1855. He went to Notre Dame University and graduated from medical school at the University of Louisville in 1877. He studied at numerous universities abroad and practiced 13 years in Caldwell, Texas, before moving to Dallas in 1890. He died in Oak Cliff at home on November 30, 1923 (13).
The city bought its first ambulance, a buggy, in 1894 for $500 but did not have enough money for a horse to pull it. The horse was not purchased until 1896 for $100, and 3 years later, Health Officer John W. Hicks Florence insisted that rubber wheels be purchased for the wagon ambulance for humanitarian reasons since the ride was so rough (14) (Figure 9).
Figure 9.
Dallas' first buggy ambulance, 1894. Photo courtesy of Parkland Health and Hospital System.
Clinics, infirmaries, surgical institutes, and hospitals (1875–1900)
Several small clinics and hospitals were established in the later part of the 1800s. The first was the Dallas Medical Institute, established in 1875. Following that, the Dallas Sanitarium, with Dr. Carl Murray as proprietor, existed from 1881 to 1882. From 1884 to 1885, the sanitarium was renamed Dallas Medical and Surgical Institute; however, it was not listed after 1885.
The Weden and Temple Medical and Surgical Institute opened in 1893 at 333 Elm Street at the corner of North Akard, managed by Dr. Weden Smith and Dr. Temple Smith. Dr. Leake's private hospital, located at 176 South Pearl at the northeast corner of Pearl and Polk Streets, was the only hospital open to all physicians. It opened in 1894 and closed in 1914.
THE BEGINNINGS OF THE UNIVERSITY OF DALLAS MEDICAL DEPARTMENT AND THE TEXAS BAPTIST MEMORIAL SANITARIUM, 1900–1920
Establishment of the University of Dallas Medical Department (1900)
The driving force behind starting the University of Dallas Medical Department was Dr. Charles McDaniel Rosser (Figure 10), a native of Georgia who came to Texas in 1865 at the age of 4 years and settled near Pittsburg (15). Following medical school at Louisville, he returned to Waxahachie, Texas. Four years later in 1891, he was appointed health officer for the city of Dallas. He was also appointed surgeon and chief of the Dallas City Hospital. He resigned as public health officer after 1 year to become surgeon of Houston and Texas Central Railroad and chairman of the medical section of the Texas Medical Association. In 1895 Dr. Rosser was appointed superintendent of the North Texas Hospital for the Insane at Terrell but resigned in 1897 to join Dr. Samuel E. Milliken of Dallas as a partner in private practice. Dr. Rosser, by this time, was convinced that Dallas needed its own medical college.
Figure 10.

Dr. Charles Rosser, father of the University of Dallas Medical Department/Baylor University College of Medicine.
On August 14, 1900, at the office of Dr. J. B. Titterington and Dr. V. P. Armstrong (the first chief of surgery at Parkland Hospital), there was a meeting along with Drs. Rosser, Lawrence Ashton, J. P. Gilcreest from Gainesville, Joe Becton of Greenville, Texas, and A. F. Beddoe, B. E. Hadra, and Sam Milliken, all from Dallas. They decided it was time to organize a medical school in Dallas and went to Mayor Cabell, who immediately ran a newspaper advertisement announcing that all reputable physicians were to meet in the council chambers of City Hall on Thursday, August 16, at 8:30 PM for the purpose of taking preliminary steps to establish a medical college in Dallas. The advertisement was signed by Mayor Ben E. Cabell, Charles Steinman, president of the Commercial Club, and W. J. Maroney, a prominent attorney (16, 17).
Only 15 of the 55 physicians who attended the meeting favored a medical school. Those who favored the medical school included Drs. C. M. Rosser, Sam Milliken, Lawrence Ashton, V. P. Armstrong (a surgeon), and J. B. Titterington (an ophthalmologist and otologist). They had the backing of the mayor and city councilmen, as well as the influential businessmen. The opposition was led by Dr. Stephen Thurston, an original member of the Dallas County Medical Surgical Association, and he was supported by St. Paul Hospital. Dr. Rosser chastised many of the other physicians who thought there were too many medical colleges and there weren't enough faculty members capable of instructing medical students. He stated, “There may be some here that would not want to organize a medical college, but if there is going to be one they would like to be in it. I tell you now, not as a threat but as a matter of information, there is going to be one.” The Dallas Morning News published the next day that there was forced adjournment of the meeting but approximately 15 physicians remained (18).
The charter for the University of Dallas Medical Department was filed with the secretary of state 1 month later on September 15, 1900. The college leased a Jewish synagogue, the former Temple Emanu-el (Figure 11). The medical college officially opened its doors on November 19, 1900, in the Jewish synagogue in what is now the 1300 block of Commerce Street, across from the present site of the Adolphus Hotel. This would eventually be Baylor University College of Medicine. Not having a university affiliation would be a problem.
Figure 11.
Temple Emanu-el, the first building for the University of Dallas Medical Department. Photo from Dallas Historical Society Archives.
Dr. J. B. Titterington was appointed dean, acting secretary, and professor of anatomy and eyes, ears, nose, and throat. Dr. Titterington, a native Dallasite, was born in Dallas County in 1868 and was an 1897 graduate of New York's Bellevue Hospital Medical College. After postgraduate training in ophthalmology and otolaryngology in London, he returned to Dallas in 1898.
First chief of surgery and a faculty revolt (1900)
Dr. Sam Milliken was the first chief of surgery at the University of Dallas Medical Department (Figure 12). Other faculty included Dr. Gilcreest, an 1876 graduate of the University of Missouri Medical School. He was designated president of the medical school and teacher of gynecology. Dr. Charles Rosser taught clinical medicine and mental and nervous diseases.
Figure 12.

Dr. Sam E. Milliken.
The medical school had been opened only 2 months when a faculty revolt occurred during Christmas vacation, 1900. Dr. Titterington, dean and acting secretary, and his partner, Dr. Sam Milliken, chief of surgery, decided to take possession of the medical school without the knowledge of Dr. Rosser and Dr. Armstrong. One night they replaced the medical school's sign, changing it from the University of Dallas Medical Department to Dallas Polyclinic Medical College. This infuriated Dr. Rosser. He sought a court injunction and won, and Drs. Titterington, Ashton, and Milliken had to resign. Dr. Rosser became the dean in place of Dr. Titterington on January 4, 1901 (18).
Dr. Milliken was born on December 2, 1866, in Mansfield, Texas. He graduated from the University of Louisville in 1887 and was probably a classmate of Dr. Charles Rosser. He did postgraduate work from 1889 to 1897 at New York Polyclinic and was in the private practice of medicine and surgery at Elm and St. Paul Streets between two tombstone factories. Dr. Milliken moved to Dallas in 1897 and partnered with Dr. C. M. Rosser to codirect Hermitage Hospital, located at 449 Elm Street. He was also proprietor of the Polyclinic Infirmary at 228 S. Ervay until 1902. He served as president of the Dallas County Medical Society in 1916. Dr. Milliken was a fellow of the American College of Surgeons and practiced surgery in Dallas until he retired in 1941. He died in 1949 (19).
Second chief of surgery (1900)
In 1900, after Dr. Milliken's forced resignation, a delegation of Dallas physicians asked Dr. Berthold Ernest Hadra and his friend Dr. J. T. Harrington to come to Dallas and have Dr. Hadra head the surgical department at the University of Dallas Medical Department.
Dr. Hadra had become professor of surgery in 1888 at the medical college in Galveston but was replaced in 1891 by Dr. James Thompson from England. In 1900, as he came to Dallas, he was elected president of the Texas Medical Association. With the new faculty, the staff included Dr. J. M. Inge of Denton, Texas, who taught surgical anatomy. Dr. Joe Becton of Greenville was the head of operative surgery, and Dr. T. B. Fisher was instructor in surgery.
At the end of the first semester in 1902, the medical school was reorganized, and Dr. B. E. Hadra was appointed professor of clinical surgery and vice president of the faculty (Figure 13). He is likely the second chief of surgery at the University of Dallas Medical Department. Dr. Hadra was born in the village of Ofen, near Brieg, Silesia, then part of Germany, on November 8, 1842 (20). He was educated at the University of Breslau and Berlin and acquired the qualifications necessary to permit him to practice medicine and surgery. He became an assistant surgeon in the Prussian Army and in 1866 served during the Seven Week War between Austria and Germany. Dr. Hadra married Auguste Beyer, and in 1869 he and his wife came to the USA from Germany. A son named Frederick was born on the voyage and became a distinguished surgeon himself, with a rank of major in the US Army during the Spanish-American War. Upon arrival in the USA, the family settled in Houston, Texas, and remained there from 1870 until 1872. On February 9, 1872, Dr. Hadra opened an office in Austin and was considered an excellent surgeon (21). He was a very prominent physician and was appointed a regent of the University of Texas in May 1883. He was associated with Dr. Ashbel Smith on the board of regents. Dr. Smith was considered one of the most intellectual physicians of Texas. In 1878 and again in 1891, Dr. Hadra practiced in San Antonio. In 1885 he again practiced in Austin. Dr. Hadra had practiced in several towns, including Waco, where he lived for about a year in 1899.
Figure 13.

Dr. B. E. Hadra.
A close friend of Dr. Hadra was Dr. J. Marion Simms, a renowned gynecologist of New York. In fact, Dr. Hadra was associated with Dr. Simms and named his son James for him. Dr. Simms is credited with developing a surgical cure for vesicovaginal fistula, and a gavel was presented to the Southern Surgical Association from his operating room table in 1895. He became famous as a surgeon in Europe.
Dr. Hadra published articles in such journals as the American Journal of Obstetrics, Journal of the American Medical Association, New York Medical Journal, Boston Medical Journal, and Texas State Medical Journal. He was considered an excellent surgeon and diagnostician and soon became internationally known. Patients came from many countries, and he had a large clientele from Mexico. In 1888 two outstanding events occurred: one was the publication of his book Lesions of the Vagina and Pelvic Floor and the other was his acceptance of the appointment as professor of the science and art of surgery at Galveston Medical College, which had been in existence since 1866 and was the predecessor of the University of Texas Medical Branch. Dr. Hadra is credited with being the first surgeon in the world to recognize the relationship of the diaphragm to rectocele and cystocele and to devise an operation for correction of these conditions (22). Dr. Hadra has been given credit for the beginning of modern operations for prolapse.
In 1891, while at the University of Texas Medical Branch at Galveston, he was replaced by Dr. James Thompson from England. Dr. Hadra became president of the Texas Medical Association in 1900 while living in Waco. During that year he moved to Dallas to become professor of clinical surgery at the University of Dallas Medical Department. At the same time Dr. Hadra was appointed professor of surgery, Dr. J. B. Becton was appointed head of operative surgery (Figure 14). Dr. Becton was a charter member of the Texas Surgical Society, which was founded in 1915.
Figure 14.

Dr. J. B. Becton.
On January 12, 1903, at 10:00 PM, Dr. Hadra was found dead by his son James. He was seated in a chair in the office located on Elm and Akard Streets. He was 60 years of age and held the position of professor of clinical surgery at the University of Dallas Medical Department. Burial was in Austin, Texas.
Surgical anatomy (1900)
Around 1900 the principal method of teaching was by lectures. In such courses as human anatomy, the only cadavers available for dissection were unclaimed bodies snatched on the sly, either before or immediately after burial in pauper's graves. Two medical students worked their way through school by transporting bodies to the school's dissecting room (23). In 1903, the professor of anatomy at the medical college was Dr. Kent V. Kibbie (24).
The Good Samaritan Hospital (1901)
One of the main obstacles in producing fully qualified physicians was the lack of a hospital in which medical students could receive clinical training. The staff sought permission from the city council to have access to the wards and operating rooms of Parkland for teaching purposes. The senior students needed to have bedside and operating room training. Dallas municipal authorities agreed to allow the students to attend patients at city-operated Parkland Hospital (25). Thus, three times a week, students traveled by wagon across the town to the city hospital for clinical practice and observation, since it was too far to walk. Dr. Rosser approached St. Paul Hospital about rotating students there; however, the sister refused (26). He then contacted Col. C. C. Slaughter, the famed cattle baron who was worth millions, in hopes that he might fund a hospital for the new medical school.
Dr. Rosser, the dean, in the meantime decided to form a private hospital. He purchased the 14-room brick mansion on Junius Street known as “Hopkins Place.” The house was built in 1880 by Col. W B. Wright, an early day pioneer. It had previously been owned by Captain W. H. Gaston, for whom Gaston Avenue is named; however, it was owned by Judge M. L. Crawford when Dr. Rosser purchased it. The purchase price was $22,500 to be paid out over an extended period. The house was remodeled to provide space for a ward, an admitting area, and operating rooms, and by 1901 the mansion was ready to begin functioning in its new role as the city's second privately owned and operated general hospital. It was named the Good Samaritan Hospital, which was the forerunner of Baylor University Medical Center (BUMC) (25) (Figure 15).
Figure 15.
Good Samaritan Hospital.
First graduating class (1902)
The first class to graduate from the University of Dallas Medical Department in 1902 had 19 students (Figure 16). Graduation was held at the Carnegie Library (Figure 17). By the second session in 1902, only 30 of the 66 students returned. In 1901, the Texas State Board of Medical Examiners had been created. Prior to this, Texas required only $15 in the absence of a diploma to practice medicine.
Figure 16.
The faculty and first graduating class of the University of Dallas Medical Department, 1902. Front row, left to right: Dr. Charles M. Rosser, founder of the medical school and first dean; Dr. J. H. Florence of Houston, first professor of obstetrics; Dr. B. E. Hadra, first professor of surgery; Dr. J. E. Gilcreest of Gainesville, first professor of gynecology; Dr. W. M. Lively of Oak Cliff, professor; Dr. A. F. Beddoe, professor of pediatrics; Dr. A. Bell, first professor of physiology; Dr. J. M. Inge of Denton, first professor of anatomy; and Dr. James E. Wilson, assistant professor of obstetrics. The woman in the front row is listed as a student.
Figure 17.
Carnegie Library, a part of the Dallas Public Library system, in 1901. Photo from Dallas Historical Society Archives.
Burning of the Jewish synagogue (1902)
The faculty was constantly changing. All faculty members were volunteers, and teaching was a chore. They were discontent with the school's lack of progress. They had no university affiliation, and often faculty failed to meet their teaching assignments. To further complicate things, on February 4, 1902, the east half of the Jewish synagogue burned. Mayor Cabell made City Hall auditorium available for lectures. There were several times during the medical school's history that City Hall came to its aid. The school needed another building, so for $15,000, the College Building on Ervay was purchased. It was remodeled in time for the school to open in October 1902 (Figure 18). It would house the medical school for the next 4 years.
Figure 18.
The College Building.
The College Building also included a 12-bed emergency hospital, primarily a charity hospital with operating rooms and obstetrics, that was later moved to Dallas City Hall.
At the time of relocation of the school to the College Building, the president was Dr. J. M. Inge, the vice president was Dr. E. H. Cary, and the secretary and treasurer was Dr. Elbert Dunlap. Commencement exercises for the 1902–1903 session were held on April 3, 1903, in Lecture Hall A in the College Building. Only 3 students met the attendance and course completion requirements of the 4-year program to be eligible for graduation.
A new dean (1902)
Dr. E. H. Cary was recruited as professor of ophthalmology and otolaryngology. One year after Dr. Cary came, he was named chief of ophthalmology, and 3 months later, on April 15, 1902, he was made dean of the medical school to replace Dr. Rosser (Figure 19). Dr. Cary was dean from 1902 until 1920. The school was in a desperate financial situation. Tuition was $75 per year, with only 60 students enrolled, and the entire budget was only $5000. Nevertheless, Dr. Cary would guide this school for the next 50 years and would become chairman of the Department of Surgery of Baylor University College of Medicine in 1925.
Figure 19.

Dr. E. H. Cary, dean from 1902 to 1920.
Baylor University affiliation (1903)
The population of Dallas in 1903 was 45,000, and Teddy Roosevelt was president. There were only 40 cars in Dallas, and the average life expectancy in 1900 was 47 years.
In June 1903, negotiations were begun in the hope of establishing an affiliation with Baylor University in Waco, Texas. At this time there were several hospitals in town, including Parkland Hospital, St. Paul Hospital, Good Samaritan Hospital, Dr. Leake's private hospital, and the 12-bed emergency hospital in the college building (26). By the summer of 1903, at the annual meeting of the AMA in New Orleans, Dr. Cary heard Dr. Frank M. Billings, AMA president, say that the vast majority of privately owned medical schools throughout the nation were doomed and that within 5 years no medical school could survive without university affiliation. This impressed Dr. Cary (dean) and Dr. Rosser, and they agreed to secure university affiliation.
Within 3 weeks after Dr. Cary contacted Baylor University in Waco, they had an affiliation contract with the university. In return for that affiliation, the University of Dallas Medical Department had to donate all of its property to Baylor. The board of trustees was reorganized, and Dr. Cary quickly became vice chairman of the board of trustees of the medical college as well as dean. The property was given to Baylor University at Waco on June 29, 1903, just 3 years after the University of Dallas Medical Department had been founded. The name of the school was changed to Baylor University College of Medicine. Dr. Cary, who was vice chairman of the board of trustees and dean, was to serve as chairman of the board of trustees in the absence of President Brooks of Baylor University, who was ex officio chairman. This meant that Dr. Cary was not only dean but in reality chairman of the board of trustees, since President Brooks could rarely make a meeting due to the distance. Dr. C. M. Rosser was elected president of the faculty of Baylor University College of Medicine (27). Although university affiliation gave prestige to the medical college, Baylor University in Waco did not offer any financial aid to the medical school.
The first executive committee consisted of S. P. Brooks, chairman; E. H. Cary, vice chairman (ophthalmologist/otolaryngologist); Elbert Dunlap, secretary and treasurer (obstetrician/ gynecologist); C. M. Rosser (surgeon); Sam Milliken (surgeon); V. P. Armstrong (surgeon); and A. F. Beddoe (24).
Other medical schools (1903)
By 1903, there were 4 medical colleges in Dallas: Baylor University College of Medicine, Dallas Medical College, Physio Medical College of Texas, and Southwestern Medical School. In 1903 Dr. F. A. Bell, Dr. J. O. McReynolds (an ophthalmologist), Dr. Henry K. Leake, and Dr. J. M. Pace organized the Texas College of Physicians and Surgeons. This organization later became the Medical School of Southwestern University, Georgetown, Texas. Much later, the affiliation shifted to Southern Methodist University after that university was established (28).
Requirements for medical school entrance (1903)
Admission requirements for the 1903–1904 session stated that a student had to have a certificate from a legally constituted high school, a superintendent of state education, or a superintendent of some county board of education attesting to the fact that he or she possessed at least the educational attainments required of first-grade teachers of public schools. There were 11 graduates the first year after Baylor affiliation, and Dr. J. O. Hayes was the first graduate to be handed a diploma awarding a degree of doctor of medicine from Baylor University College of Medicine in 1904 (29).
The bloodless surgeon of Vienna and the vision of the Texas Baptist Memorial Sanitarium (1903)
The Philip Armour family, of the Armour and Co. meatpacking plant of Chicago, had a child with congenital hip dislocation. They brought Dr. Adolf Lorenz of Vienna, Austria, to Chicago to treat their child. Dr. Lorenz subsequently lectured before the AMA in New Orleans in May 1903 and attracted wide publicity. Dr. Charles Rosser met Dr. Lorenz in Chicago, went to the meeting in New Orleans, and invited Dr. Lorenz to visit Dallas and give a clinical demonstration of his bloodless surgery under the auspices of the faculty of the University of Dallas Medical Department and the Good Samaritan Hospital, both of which had been founded and directed by Dr. Rosser. Dr. Lorenz arrived in Dallas on May 20, 1903, and held two clinics daily for a week, alternating between Good Samaritan Hospital on Junius Street and the College Building on Ervay Street (Figure 20). At the end of the week, a banquet was held at the Oriental Hotel honoring Dr. Lorenz, and the final address of the evening was given by the Rev. Dr. George W. Truett. At the age of 36 years, he stated in his address, “Is it not now time to begin the erection of a great humanitarian hospital, one to which men of all creeds and those of none may come with equal confidence?” It is thought that Dr. Truett's address motivated individuals to found the Texas Baptist Memorial Sanitarium, which would eventually become BUMC.
Figure 20.
Drs. Blount, Lorenz, Cary, and Rosser in front of the Texas Baptist Memorial Sanitarium.
Col. C. C. Slaughter was contacted and originally was to give $25,000, but because he was so wealthy he was asked to give $50,000. Col. Slaughter not only gave $50,000 but also agreed to give $2 for every $1 contributed from other sources. J. P. Wilson, builder of the downtown Wilson Building, also gave $50,000 to match Col. Slaughter's original gift. In June 1903, the hospital project was undertaken by the Baptist General Convention of Texas (30).
Col. Slaughter was one of the wealthiest people in the USA. He was born in Sabine County, Texas, on February 9,1837, when Texas was still a republic. His father was George Webb Slaughter, who served as Sam Houston's chief of scouts during the Texas Revolution and was the last Texan to see the defenders of the Alamo alive. It is estimated that Col. Slaughter gave a half million dollars to the sanitarium and medical school between 1903 and 1919 (Figure 21). His heirs continued to be benefactors to Baylor Hospital. Notable among them was his daughter, Minnie (Mrs. George T. Veal), who subsequently became Baylor Hospital's greatest financial benefactor. Col. Slaughter's “Steamboat Victorian” home (Figure 22) was originally built by Col. W. E. Hughes, owner of the Grand-Windsor Hotel.
Figure 21.

Col. C. C. Slaughter with his wife.
Figure 22.
The home of Col. C. C. Slaughter, 1890. Photo courtesy of Old City Park, the Historical Village of Dallas, Dallas, Texas.
Purchase of Good Samaritan Hospital by the Texas Baptist Memorial Sanitarium (1903)
At a meeting on October 26, 1903, 3 days after the first meeting of the board of directors of the Texas Baptist Memorial Sanitarium, Dr. Rosser offered the Baptists the opportunity to purchase his Good Samaritan Hospital at the same price he had paid for it and presented them with all of his equipment. The board accepted on October 30. The Texas Baptist Memorial Sanitarium officially opened in the building formerly called the Good Samaritan Hospital on May 11, 1904 (31).
Within 6 months of the opening of the Texas Baptist Memorial Sanitarium, it was decided that a new hospital should be built. On February 25,1905, the board of directors decided to shut down the building they had bought from Dr. Rosser and not admit any more patients because they were concerned that it would be unsafe for patients to be so close to work and noise while the new hospital was being built. Thus, from March 11, 1905, until mid October 1909, no patients were treated at the Texas Baptist Memorial Sanitarium (the former Good Samaritan Hospital).
New requirements for medical schools (1905)
During the middle of 1905, the first session of the Council on Medical Education of the AMA was held. A medical school required 4 years of at least 30 weeks per year as determined by the Joint Conference of the Council on Medical Education. A total of 4000 hours of actual instruction was required by the Association of American Medical Colleges. Baylor University College of Medicine recognized these requirements and knew the critical need for more funds and more facilities. As a result of the higher standards set by the council, from 1905 to 1910 the number of medical colleges in the USA was reduced from 162 to 131, the number of students from 28,142 to 21,526, and the number of graduates per year from 5600 to 4440.
Sale of College Building; opening of Ramseur Science Hall (1906–1909)
Mrs. P. S. Ramseur of Paris, Texas, gave the sanitarium her estate, including 9000 acres and $15,000 in cash, which gave an overall value exceeding $100,000. With the money, a new science building, the Ramseur Science Building, was built. Based on the assumption that the new building would be completed by October 1, 1906, the College Building on Ervay Street was sold to R. V and Cecil Rogers in July 1906, but Ramseur Science Hall did not open until 1909. Thus, the medical school moved into the Texas Baptist Memorial Sanitarium on October 1, 1906, and remained there for 3 years (32).
Ramseur Hall housed all the departments of the medical college from 1909 to 1923 and was located near the current dental school (33) (Figure 23). A dispensary was established on the ground floor of Ramseur Hall, and this is the first definitive record of an outpatient department in the college. The dispensary was opened for the poorer of the city from 2:00 to 3:00 PM every day except Sundays and holidays.
Figure 23.
Ramseur Hall.
Legislative acts (1907)
Two legislative acts were passed by the 30th legislature for the state of Texas in 1907 that had significant influence on medical education in Texas. The first was the creation of the State Board of Medical Examiners, which became effective on July 13, 1907. The other was the creation of the State Anatomical Board, whose function was the procurement of anatomical material for medical schools, thus obviating private procurement of this material (34).
First interns from Baylor University College of Medicine (1907)
Six students graduated in 1907, and two became the first two interns appointed from the medical school. Miss Halle Earl, who had the highest class standing, was appointed intern at Dr. Gilcreest's Hospital in Gainesville, and M. F. Sloan was appointed intern at St. Paul Hospital (34).
First interns appointed to the Texas Baptist Memorial Sanitarium (1908)
The ninth session of Baylor University College of Medicine opened on October 1, 1908, with an enrollment of 53 students and closed on Thursday, April 29, 1909, with commencement exercises held at the Bush-Temple Music Hall. Sixteen students graduated from Baylor University College of Medicine in 1909, and two were appointed interns at the Texas Baptist Memorial Sanitarium: Dr. Audy V. Cash and Dr. W. W. Shortal, who would later become a member of the surgical staff at Baylor Hospital (35) (Figure 24).
Figure 24.
Intern record from the Texas Baptist Memorial Sanitarium, 1909.
New building for the Texas Baptist Memorial Sanitarium (1909)
The new Texas Baptist Memorial Sanitarium—the building that replaced the former Good Samaritan Hospital—opened on October 14, 1909, with 250 beds, including 114 private rooms, with every room having outside ventilation (32) (Figure 25). In 1910, nurses could expect to earn up to $4 for a 12-hour day without rest. The operating room fee was $15 for major operations and $10 for minor surgical procedures (Figure 26). A bed in a ward cost $10 per week, including board and nursing care (31).
Figure 25.
The new Texas Baptist Memorial Sanitarium building, built in 1909.
Figure 26.
Surgery at the Texas Baptist Memorial Sanitarium, c. 1920.
The first decade (1900–1910)
The tenth session closed on April 26,1910, with 9 graduates. Thus, for the first 10 years, the college had 134 graduates. In 1910, two medical schools remained in Dallas: Baylor University College of Medicine and Southwestern University College of Medicine, both of which were struggling for existence. During the first 10 years, 1900–1910, Baylor University College of Medicine had occupied 4 buildings: first, the leased Jewish synagogue, former Temple Emanu-el on Commerce Street damaged by fire in February 1902; second, the College Building on South Ervay Street; third, the original Texas Baptist Memorial Sanitarium on Junius Street; and fourth, Ramseur Science Hall in 1909. No record is available of any specific research projects engaged in during the time. The college had overcome the opposition of its foundation in 1900 and survived the faculty insurrection early in the first session. At the end of the l0-year period, the faculty consisted of only 2 full-time and 28 voluntary members.
Acceptance into the Association of American Medical Colleges (1910)
The Flexner Report of 1910 was critical of Baylor University College of Medicine, noting that the requirements for admission were low and basically there was a need for financial resources. During the 1910–1911 academic year, the library was organized and housed in the Texas Baptist Memorial Sanitarium. Rules and regulations recommended by the board of trustees at a meeting on June 1, 1911, stated that one negative vote by a faculty member would be sufficient reason to prevent a student from graduating. The second regulation was that the registrar keep class standings (35). In 1911, Dr. Walter H. Moursund, a 1906 graduate of the University of Texas Medical Branch at Galveston, joined the faculty as assistant in pathology and bacteriology. He would later become dean of the medical school and go with it when it moved to Houston. On February 13, 1913, at a meeting in Chicago, Baylor University College of Medicine was elected to membership in the Association of American Medical Colleges (36).
Departmental organization (1913)
It was not until the 1913–1914 session that all branches of the curriculum were set up in departments. The departments included anatomy, physiology, pharmacodynamics, chemistry, pharmacology, pathology, bacteriology and hygiene, medicine, surgery, and gynecology and obstetrics (37).
More admission requirements (1913–1917)
At the June 13, 1913, meeting, the Texas State Board of Medical Examiners announced that only graduates of class A and B medical schools would be accepted for examination for licensure. Baylor University College of Medicine was rated class Bat that time. By the time the 14th session (1913–1914) opened, only 3 of the 5 applicants for the freshman class were accepted due to new admission requirements, which included physics and German or French. By the 1915–1916 session, biology, physics, and chemistry were all required for admission (37).
The only other medical college operating in Dallas was Southwestern University Medical College, which had become the Medical Department of Southern Methodist University on April 14, 1911. It closed on June 14, 1915, and those students were accepted as transfers by Baylor University College of Medicine. When the 16th session closed on May 31, 1916, the honorary degree of doctors of laws was conferred by Baylor University on Dr. E. H. Cary, dean of the medical college (38). Finally, on June 12, 1916, the Council on Medical Education awarded the college a class A rating (39).
With the opening of the October 1, 1917, session, requirements for admission increased to a minimum of 2 years of college work. The Medical Department of Texas Christian University of Fort Worth announced that it would not open for another session after 1918. It merged with Baylor University College of Medicine since it lacked an endowment and could not accommodate the higher entrance requirements. Thus, Baylor was the sole surviving medical school not only in Dallas but also in North Texas in 1918 (40).
Second Parkland Hospital (1914)
Under the auspices of the Masonic Lodge, the cornerstone for a new city hospital was laid on March 18, 1913, with impressive ceremonies. On February 1, 1914, the new and second city-county Parkland Hospital opened at Oak Lawn and Maple Avenues in far North Dallas (Figure 27). The city continued to operate its emergency hospital separately in the City Hall (39).
Figure 27.

Parkland Hospital, built in 1914 and vacated in 1954; the building is now the Woodlawn Building. Photo courtesy of Parkland Hospital.
World War I and Hospital Unit V (1917)
President Wilson declared war on Germany on April 6,1917, and doctors were rapidly mobilized. A military hospital unit, designated as Hospital Unit V, was organized at Baylor, and members of the Baylor faculty, including Dr. W. W. Shortal, surgeon (captain) and Dr. Samuel D. Weaver, surgeon (first lieutenant), were among those in the unit. They did not return to the USA until February 1919 (41). Although Dr. Gary, then president of the Texas Medical Association, wanted to volunteer and head for France, President Brooks at Baylor in Waco convinced him that he was needed more at home than overseas. Thus, Dr. Cary was largely responsible for the reorganization and training of the Baylor Medical Surgical Unit formed in 1917, composed of sanitarium staff and medical school faculty. Dr. Cary secured authority from Washington to develop a Student's Army-Training Corps at Baylor, and the entire student body was organized. The government paid student tuition fees, but Dr. Cary had to borrow another $100,000 to build barracks and provide food for the students. The war ended on November 11, 1918, and almost 10 million had been killed, including 115,000 Americans. Two months later, on January 25, 1919, Col. Slaughter died (40).
Burning of City Hospital (1918)
In 1918, the original frame City Hospital Building, built in 1874 and used for infectious and contagious diseases, was destroyed by fire. The patients were transferred to the main building of Parkland Hospital on Oak Lawn Avenue (42).
Surgery specialty requirements (1920)
In 1920, the Council on Medical Education of the AMA appointed 9 committees to formulate requirements of necessary graduate training to prepare practitioners to become specialists. The two main groups were medicine and surgery. Under surgery were ophthalmology, otolaryngology, orthopaedic surgery, and urology (43).
Teaching hospital designation (1920)
After World War I, the clinical facilities were reorganized, and Baylor trustees designated the Texas Baptist Memorial Sanitarium as the official teaching hospital for the medical school and limited practice in the sanitarium to medical school faculty and members of the sanitarium staff (44).
Early surgical faculty (1903–1925)
In the 1903–1904 catalog, Baylor University Bulletin, Dr. Samuel E. Milliken is listed as professor of the principles and practice of surgery (24). Dr. Vernando P. (V. P.) Armstrong is listed as professor of gynecology and abdominal surgery. Dr. J. M. Inge is listed as emeritus professor of clinical surgery. Later catalogs list Dr. W. R. Blailock as professor of the principles and practice of surgery in 1904–1906 (45). Dr. V. P. Armstrong was professor of the principles and practice of surgery in 1906–1907 (46). In the 1904–1905 Bulletin, Dr. W. W. Samuel is professor of operative surgery and was so until 1908. These latter three surgeons followed Dr. Hadra in surgery, but it is unclear who was chief of surgery if there was one.
Dr. Garfield McCoy Hackler. In the 1905–1906 catalog with announcements for 1906–1907, Dr. Garfield McCoy Hackler is listed as professor of the theory and practice of medicine (47). Dr. Hackler's obituary in the Texas State Journal of Medicine in June 1937 states that he was born in 1865 in Independence, Virginia (48). He graduated from medical school at the University of Maryland in Baltimore in 1891 and did postgraduate work in New York, Chicago, and New Orleans. In 1907 he went to London and Leeds to study local and spinal anesthesia in surgery. In 1894 he located at Ennis, Texas, where he practiced for 10 years before moving to Dallas in 1904. After coming to Dallas he was associated with Baylor University College of Medicine as chairman of medicine from 1904 to 1907, at which time he became professor of the principles of surgery in 1911; 18 years later, he was appointed professor of surgery. He became one of the senior surgeons and participated in the groundbreaking ceremony for the new sanitarium building. Dr. Hackler was a member of the Texas Surgical Society, the Southern Clinical Society, and the Southern Medical Association. He became a fellow of the American College of Surgeons in 1915. He was a member of the First Baptist Church and died shortly after suffering a stroke in his office on May 6, 1937 (48).
Dr. Charles M. Rosser. In the 1906–1907 catalog for Baylor University, Dr. Charles M. Rosser is listed as professor of surgery. Dr. Rosser was born in Cuthbert, Georgia, on December 22, 1862. His father, Rev. M. F. Rosser, was a well-known Methodist minister who had served in the Confederate Army. The family moved to Texas in 1865, locating in Camp County. Dr. Rosser received his medical degree from the University of Louisville in 1888. He moved to Waxahachie, Texas, to practice medicine and teach school. Dr. Rosser moved to Dallas in 1890 for the practice of medicine and surgery and was one of the first Texans to confine his work entirely to surgery. He was married in 1897 to Alma Curtice of Eminence, Kentucky. They had two children, Dr. Curtice Rosser and Mrs. George McBlair of Dallas. In later years, the elder Dr. Rosser practiced with his son. He was considered the father of Baylor University College of Medicine at Dallas. In 1901 he founded the Good Samaritan Hospital in Dallas, which was the predecessor of the present BUMC.
Dr. Charles Rosser was an eloquent speaker, able to recall sentences and paragraphs from speeches and writings of months and even years past. He was president of the Southwest Surgical Association from 1904 to 1907 and of the Dallas County Medical Society in 1923. He was the 58th president of the Texas Medical Association in 1925–1926. He was a fellow of the American College of Surgeons and served as president of the first Texas State Board of Health. Dr. Rosser died on January 27, 1945, following an extended illness (49). It is likely that he was in charge of surgery at some time around 1910–1912, but this is unclear.
Dr. W. W. Shortal, first intern Dr. Shortal (Figure 28) was born in Ragsdale, Fannin County, on July 13,1886. He attended Honey Grove High School and graduated from Baylor University College of Medicine in 1909. He entered private practice in Dallas, specializing in general surgery. After serving as a major in World War I, he became clinical professor of surgery at Baylor University College of Medicine. According to the Dallas Medical Journal dated February 2, 1968, Dr. Shortal was chief surgeon at Scottish Rite Hospital from 1930 to 1936 and was chief surgeon at the City-County Hospital from 1920 to 1934. In 1933 he started the Shortal Clinic. He became a member of the American College of Surgeons in 1920. Dr. Shortal died on January 26, 1968, and was buried at Sparkman/Hillcrest at Northwest Highway (50, 51). In the 1909–1910 catalog, Dr. W. W. Shortal is listed as a faculty member and demonstrator of anatomy (52). He was the first intern from Baylor University College of Medicine. By 1916 he was listed as professor of applied anatomy.
Figure 28.

Dr. W. W. Shortal.
Dr. Harold M. Doolittle. In the Baylor University Bulletin announcements for 1916–1917, Dr. Harold M. Doolittle (Figure 29) is listed as professor of surgery along with Dr. Hackler and Dr. Rosser (53). Dr. Doolittle had become an associate professor of clinical surgery in 1911. He was born in Elyria, Ohio, on August 27,1877. He graduated from the University of Michigan Department of Medicine and Surgery in Ann Arbor in 1902. Dr. Doolittle served an internship at Northern Pacific Railroad Hospital in Brainerd, Minnesota. He was one of the first fellows of surgery at the Mayo Clinic in Rochester from 1904 to 1905. Dr. Doolittle came to Dallas in 1905 and was first associated with Dr. C. M. Rosser. Later he practiced independently and in 1915 joined Dr. R. W. Baird in a partnership that later developed into the Dallas Medical Surgical Clinic. He was chief of the surgical staff and chairman of the board of the Dallas Medical and Surgical Clinic from its founding to the time of his death (54). Dr. Doolittle married Leda Stimson in 1907. He was a fellow of the American College of Surgeons and a founding member and president of the Texas Surgical Society. He resigned from the staff in 1935 due to health conditions. He became an honorary fellow of the Texas Surgical Society in 1938. Dr. Doolittle, a member of the Episcopal Church, died in Dallas on February 22, 1950, after a brief illness (55).
Figure 29.

Dr. Harold M. Doolittle.
Dr. A. B. Small. In the catalog for 1916–1917 and announcements dated May 1917, Dr. A. B. Small (Figure 30) is listed as clinical professor of surgery. He was born on July 15, 1863, in Collinsville, Alabama, and educated at the Memphis Hospital Medical College in 1888. He moved to Dallas in 1895. He was clinical professor of surgery until 1935 and was the father of Andrew B. Small, Jr., who became assistant clinical professor of surgery in 1943. He served as chairman of the section on surgery of the Texas State Medical Association in 1926 and again in 1932. He was also vice president of the Texas State Medical Association. Dr. Small married Marie Watson of Waxahachie in 1900 (56). His grandson, Dr. Andrew B. Small III, did his residency at BUMC and is on the staff there. Dr. Andrew Small Ill's son, the fourth generation of the Small family, was a radiology resident at BUMC. Dr. Small was a founding member and also president of the Texas Surgical Society in 1926. He died suddenly on November 29, 1934, at age 71 years in Dallas.
Figure 30.

Dr. A. B. Small.
Early minutes of the hospital board of trustees (1904–1950)
Dr. Harold Cheek and Simira Meymand reviewed the minutes of the hospital board of trustees dating from October 1904 (57). These minutes were brief and mostly written in longhand. The staff of the Texas Baptist Memorial Sanitarium comprised 23 physicians, including Drs. E. H. Cary, J. M. Pace, and Charles M. Rosser; Pierre Wilson was president. In March 1910 rules and regulations were established for the development of an intern program that would consist of 6 months on the medical service and 6 months on the surgery service. Dr. W. W. Shortal was the first intern selected. In June 1910 there is evidence that medical services were organized to include a medical, surgical, and gynecological service. The following year, it was noted that 4 interns had been selected for the coming year.
In January 1912 the sanitarium hospital board created a medical staff chosen from the faculty of Baylor University College of Medicine. It would constitute the executive medical committee and shows Dr. Charles M. Rosser in surgery, who was likely the first chief of surgery at Baylor University College of Medicine. Dr. E. H. Cary was dean and head of ophthalmology and otolaryngology. Dr. Harold M. Doolittle was appointed head of operative and clinical surgery, and Dr. Elbert Dunlap head of gynecology. By November 1912, additional executive committee members included Drs. G. M. Hackler, C. M. Grigsby, H. L. Moore, C. R. Hanna, J. H. Dean, W. M. Peck, J. M. Martin, J. H. Martin, and S. L. Turner.
In February 1915 Dr. E. H. Cary, as spokesman for the staff, encouraged the board of trustees to organize the staff into 3 categories: 1) executive senior physicians and surgeons; 2) executive junior physicians and surgeons; and 3) honorary physicians and surgeons. This structure is similar to today's organization of associate attending and attending staff. On May 10, 1918, the staff recommended raising the hospital standards to conform to the minimal standards of the American College of Surgeons and to request that the board create a declaration opposing fee splitting (58). On June 18, 1927, the board of trustees formed divisions to include medicine, surgery, and obstetrics.
On October 5, 1927, Dr. Ozro T. Woods admitted patients through the dispensary to be used for the purpose of teaching. By January 23, 1928, the minutes note that 9 interns from the senior class were selected for the coming year. Dr. Rosser resigned on December 20, 1928. Dr. Doolittle resigned from the faculty on October 23, 1935. Dr. Charles W. Flynn became chairman of surgery in April 1936.
BAYLOR UNIVERSITY HOSPITAL AND BAYLOR UNIVERSITY COLLEGE OF MEDICINE, 1920–1960
Consolidation of the sanitarium and medical school under the Baylor name (1920)
On November 12, 1920, formal approval was granted to combine the Texas Baptist Memorial Sanitarium and the college of medicine by the Baptist General Convention of Texas in a meeting in El Paso. That consolidation placed the college of medicine, the dental school, and the nursing school under the board of trustees of Baylor University. The Texas Baptist Memorial Sanitarium was renamed Baylor Hospital on January 21,1921, and property, including Ramseur Hall and the sanitarium, passed to Baylor University in Waco (43).
Support of the medical school by Baylor University at Waco (1920)
In June 1920 at the 75th anniversary celebration of Baylor University, the executive committee of the board of directors of the Baptist General Convention of Texas passed a resolution stating that Baylor University would receive a sum equal to 5% of an endowment of $ 1 million payable annually to the trustees of Baylor University College of Medicine (59).
Departmentalization and reorganization (1920)
By 1920 the hospital had 400 beds and 7 operating rooms (60). A chairman was appointed to each medical school department, thus more clearly defining departments. There were only 8 full-time faculty members. It was specified that the position of dean should be filled by someone not in private practice. Because of this, Dr. Cary resigned as dean and became dean emeritus and chairman of the advisory committee as well as continuing his faculty responsibilities as professor of ophthalmology and otolaryngology. Dr. W. H. Moursund, professor of pathology, who had recently come back from the military service, was appointed acting dean (59) (Figure 31).
Figure 31.

Dr. Walter H. Moursund, dean of Baylor University College of Medicine.
In 1921, Dr. Mclver Woody, formally dean and chief of the surgical division at the University of Tennessee School of Medicine, was named dean of the medical school and professor of surgery (61). Dr. Woody had received his bachelor's degree from Harvard and his medical degree from Harvard in 1912. He had interned at Boston City Hospital in 1913–1914 and was a teaching fellow at Harvard from 1914 to 1919. However, after 1 year, Dr. Woody resigned the deanship and the professorship of surgery, and Dr. Moursund was again made acting dean and then permanent dean in 1923 (62).
Purchase of the Stephen F. Austin School (East Dallas City Hall) (1922)
In Dallas in 1920, the first paved highway was Beltline Road. In 1922 the Magnolia Building, with the flying red horse, opened. The same year, insulin was first used to treat diabetes. In that year Baylor Hospital bought from the board of education of the city of Dallas the Stephen F. Austin school building at the corner of Gaston Avenue and Hall Street for $40,000 (63). Built in 1886, the Stephen F. Austin building had formerly been City Hall of East Dallas and later had become one of the public grade schools (Figure 32). For several years Dr. Cary had advocated the purchase of this property, but there had been opposition by the neighbors. The black servants were leaving the area in droves, explaining that they did not want to work close to a place where “young boys cut up dead men.” In 1925 the medical college was housed in two buildings, Ramseur Hall and Cary Hall (Old City Hall). Cary Hall would be used by the medical college until 1943, when the school moved to Houston.
Figure 32.
Cary Hall, which had been the City Hall of East Dallas and an elementary school before being purchased by the medical college.
Beginning with the 1923 session, each student paid a hospital fee of $3 to cover expenses of hospitalization of the students for a period of up to 1 week. The operating room fee for the students was covered only when an operation was a distinct emergency (64). The 23rd session closed on June 12, 1923, with 17 graduates.
Medical Arts Building (1923)
In 1923, Dr. Cary, one of the wealthiest physicians in Dallas, opened his magnificent 19-story Medical Arts Building on Pacific Avenue in downtown Dallas (65). He opened a small hospital on 2 floors of the building with operating rooms for otolaryngology, dental, and abdominal surgery. The building received national publicity, but locally it signified a deep internal rift at Baylor, one destined to fester for more than 20 years and eventually lead to the removal of the medical college to Houston. The building was eventually torn down in 1977 because of difficulty with parking and downtown traffic; it had been outdone by newer and more modern buildings in more convenient locations.
Dr. Cary, chief of surgery (1925–1929)
Dr. E. H. Cary, former dean, became head of the Department of Surgery in 1925 and remained so until 1929 (66). In 1929 Dr. Cary was elected president of the Dallas County Medical Society, the Texas Medical Association, and the Southern Medical Association.
Faculty unrest—a second Flexner Report (1925)
Citizens of Dallas began talking in the late 1920s about making Dallas a great medical center. The men who were dreaming of making Dallas a great medical center, in time, thought their dream could not become a reality unless all denominational attachments of the scientific institutions were severed. Great foundations such as the Carnegie and Rockefeller Foundations were largely responsible for this thought. The board of trustees brought in Dr. J. F. Kimball as vice president of Baylor University in 1929, and he gave wise and constructed supervision to all the Baylor units in Dallas for 10 years. He had previously served as superintendent of Dallas Public Schools. Brice Twitty was also brought in; he was a man of great knowledge in the fields of public relations and finance. The doctors wanted departmentalization, and the trustees attempted to accommodate them.
The Flexner book on medical education was published in 1925 (67). Dallas physicians realized that medical education in Dallas was not what it should be. The board of trustees was sympathetic but did not want to put Baylor in debt. The physicians became impatient and felt that the leadership was inadequate. They felt the need to separate scientific institutions from denominations. Two reports were submitted to the board of trustees within 3 months of each other. The first was from Dean Moursund, Dr. Henry M. Winans, and Dr. W. W. Looney, dated December 20, 1928. The 8 page report from the faculty outlined the dissatisfaction and the lack of support for the medical college, the nursing service, and the nursing school. Dr. Moursund stated that it was “a wind that would blow into a storm.” The second report was dated March 6, 1929, and was submitted to the trustees and president of Baylor University. It proposed the new administrative structure for all units of Baylor in Dallas. It urged that the new clinic of the City Health Department be aligned with Baylor Hospital and that a baby hospital funded by Mr. Bradford, the Cancer and Pellagra Hospital, and the Psychopathic Hospital, which had been audiorized by the state legislature, all be located on the Baylor campus. The report was signed by Dr. E. H. Cary, chief of surgery; Dr. A. I. Folsom, who would follow as chief of surgery later in 1929; and Dr. C. C. Hannah (67). The board of trustees was reluctant to undertake too many large projects because of the financial risk. The Great Depression was coming. Although steps were taken, they were not enough to satisfy the physicians (68).
Stock market crash (1929)
Initially after World War I, there had been an economic boom, but this was quickly followed by a severe economic downturn in 1923, leaving the Texas Baptists saddled with huge debts. By November 1928 the hospital was in debt $261,330 (69, 70). On October 24, 1929, came Wall Street's infamous “Black Thursday,” and the stock market crashed. The Great Depression engulfed America. By 1933, 2294 banks had closed and 15 million Americans were unemployed.
Approval of the Baylor Plan by the American College of Surgeons (1929)
In December 1929 the Baylor Plan of prepaid hospital insurance was formed (the forerunner of Blue Cross/Blue Shield). As the Great Depression wore on, patients had more difficulty paying hospital bills, which had increased in cost. One afternoon in late 1929, Vice President Kimball, who was in charge of the Dallas unit, and Superintendent Twitty discussed the crisis in Mr. Kimball's office. Dr. Kimball suggested that people be allowed to pay a small amount each month toward future care. Dr. Kimball proposed that each teacher in the Dallas School District pay 50¢ per month or $ 1.50 per family into the treasury of his or her school. By December they had enrolled 1356 patients.
The first patient to receive hospital benefits under the Baylor Plan was Alma Dickson, who slipped on icy pavement in December 1929 and fractured her ankle. She spent Christmas Day in the hospital. Following hospitalization, she found her hospital bill paid in full by the plan. There had been considerable resistance to the new idea until one of the employees from the Dallas Morning News developed appendicitis. Her hospital bill was paid in full by the plan, and this so impressed the others that the rest of the Dallas Morning News employees enrolled. National recognition spread rapidly.
The American College of Surgeons became the first important national medical body to approve the Baylor Plan. It was ultimately endorsed by the American Hospital Association and eventually became known as Blue Cross. In 1946, the Blue Cross Plan was supplemented by the Blue Shield Plan, which provided insurance for the payment of doctor bills. By 1977, more than 90 million Americans were covered by Blue Cross. In the lobby of BUMC's Truett Hospital is a bronze plaque inscribed “to Baylor University Hospital, Dallas, Texas, the birthplace of the Blue Cross Program of prepaid hospital insurance” (70).
Events of the 1930s
In the 1931–1932 session at Baylor University College of Medicine, there were 256 medical students with 120 freshman, and 67 graduated on May 3,1932. The Baylor School of Pharmacy had to close in 1931 due to insufficient funds and lack of support by Baylor University in Waco (71).
During the 1930s, several events are noteworthy. In 1934, Bonnie Parker and Clyde Barrow, notorious bank robbers from Dallas, were killed in Arcadia, Louisiana. The Dionne quintuplets were born in Calendar, Ontario. The Empire State Building opened in 1935, and Al Capone was convicted of income tax evasion. The Hindenburg airship exploded in Lake Hurst, New Jersey (1937). Charles Lindbergh's son was kidnapped. Sulfa, “the wonder drug,” was marketed. The first Cotton Bowl game was played, and Bugs Bunny, the cartoon character, was originated. In 1935 Fort Knox was established. Congress passed Social Security, and Huey “Kingfish” Long was shot to death by a physician, Dr. Carl A. Weiss. The flying red horse was placed on the Magnolia Building in Dallas (1934).
Florence Nightingale Hospital and Baylor University Hospital (1937)
The Florence Nightingale Hospital, on the corner of Gaston Avenue and Adair Street, was completed in the summer of 1937 and was connected by underground corridors with Baylor Hospital. The hospital was made possible by a gift from Mr. and Mrs. Edwy Rolfe Brown of Dallas (72, 73). With the opening of the Florence Nightingale Hospital on May 12,1937, officials of Baylor Dallas used the term “Baylor University Hospitals” for what may have been the first time. As early as 1932, officials had added the word “university” in references to Baylor Hospital, but the name was not formally changed to Baylor University Hospital until July 16, 1937, when a new 50-year charter was issued to Baylor University and the hospital name change became official (73).
In 1938, Dr. Joseph M. Hill, a native of Buffalo, New York, began the development of a machine called “ADTEVAC” (adsorption temperature controlled vacuum) that could dry blood plasma. The blood plasma was changed to powder form that did not require refrigeration and could be mixed with a dissolving liquid immediately prior to its use in transfusion to form instant blood plasma. Due to widespread interest in the product, Baylor received a $13,000 grant in December 1939 from Dr. and Mrs. Stanley Seeger, a Milwaukee couple who had recently moved to Dallas. The donation was in memory of the late William Buchanan, Mrs. Seeger's father and a multimillionaire Texarkana lumber dealer and oilman. Dr. Seeger's daughter, Hannah Davis, and her husband, Wirt Davis, and family would subsequently make many significant endowments to the Department of Surgery (71).
Southwestern Medical Foundation (1939)
In 1938 Baylor University College of Medicine had many problems. The tuition paid could not resolve the basic problem that had always plagued the school: a lack of money. The school had no endowment, no support from a major financial foundation or granting agency, and no significant monetary assistance from its own parent, Baylor University. There was little research in the school, and instruction was basically limited to lectures. The physical plant was inadequate, and Baylor's position as a class A institution was again in jeopardy.
On January 21, 1939, with the support of several leading figures within the community, Dr. Cary obtained a charter for the Southwestern Medical Foundation. E. R. Brown, who had helped fund the Florence Nightingale Hospital; Karl Hoblitzelle, a business entrepreneur and interstate theater owner; and Dr. Hall Shannon were the incorporators for the nonprofit corporation with no capital stock. The foundation added Herbert Marcus, Jesse S. Jones of Houston, R. C. Fulbright of Houston, and T O. Walton, president of Texas A&M College at Bryan, Texas, to the board of trustees. The foundation's charter gave it the right to own and operate a medical school (74). A formal dinner sponsored by the foundation was held on January 23, 1939, at the Adolphus Hotel, and the formation and purpose of the foundation were announced. The members noted that a medical school located in Dallas would belong to the entire Southwest and would be strictly nonsectarian (75). It was estimated that from $5 million to $25 million would be needed from private sources. The foundation appointed a committee, including Dr. E. H. Cary, for the purpose of raising $5 million to support medical research at Baylor University College of Medicine. Dr. Allen Gregg, director of medical science for the Rockefeller Foundation, was the principal speaker. The endowment failed to materialize because within a few months the world was focusing on World War II prospects in Europe. With the opening of the 40th session of the medical school in October 1939, the admission requirements were increased to a minimum of 3 years of college credit.
Baylor surgeons in the 56th Evacuation Unit (1940)
In August 1940, Baylor University College of Medicine received a telegram from US Surgeon General James C. Magee asking that the college organize a medical unit for the army. The unit was to be designated the 56th Evaluation Hospital, and it would be composed almost entirely of hospital staff and medical school faculty and alumni just as its predecessor, Hospital Unit V, had been 22 years earlier in World War I. Included in the organization of the 56th Evacuation Hospital were several surgeons, including Majors Andrew D. Small, Charles D. Bussey, and James Hudson Dunlap, who were founding members of the Dallas Society of General Surgeons, and Captain Robert). Rowe, a colon and rectal surgeon (76).
Hitler had taken over France, and London was being bombed. President Franklin D. Roosevelt had Congress approve the first peace-time draft in American history. The USA and Britain were moving closer to a military alliance (77). Shortly before 8:00 AM on Sunday morning, December 7, 1941, hundreds of Japanese planes attacked the US naval base at Pearl Harbor and the Hawaiian islands without warning. The attack left 2330 Americans dead and another 1145 wounded. The next day President Roosevelt called for a declaration of war against Japan, and that request was approved in congress by a vote of 470 to 1. Three days later, Japan, Germany, and Italy declared war on the USA (78).
Several important surgeons came to Dallas in the 1930s and 1940s. Many were first in their specialty:
Dr. Walter Sistrunk, 1930
Dr. Oscar Marchman, 1931
Dr. Albert P. D'Errico, 1932, neurosurgery
Dr. James T Mills, 1935, plastic surgery
Dr. J. Warner Duckett, 1936, pediatric surgery
Dr. John Vivian Goode, 1938, general surgery
Dr. William Lee Hudson, 1938, general surgery
Dr. Hudson Dunlap, 1942, general surgery
Dr. Jack Carr, 1942, colon and rectal surgery
Dr. Frank Selecman, 1942, general surgery
Establishment of the Southwestern Medical College (1942)
In early 1942, the Southwestern Medical Foundation became active towards reaching an agreement with Baylor University for joint operation of Baylor University College of Medicine. Dr. Cary, former chief of surgery, ultimately put the college of medicine and the foundation on a collision course. It had been announced on March 8, 1942, by Southwestern Medical Foundation's president, Dr. E. H. Cary of Dallas, and reported in the Dallas Morning News on March 12, 1942, that plans for a great medical center on a 35-acre tract on Harry Hines Boulevard, including the Parkland Hospital grounds, had been made. The new medical school was to be named Southwestern Medical College.
Baylor University College of Medicine had been offered the opportunity of sponsoring the medical school that would be an integral part of the center. However, the plan would not involve Baylor Hospital. Committees from the clinical faculty and the foundation's board of trustees met with the trustees of both Baylor in Waco and Baylor in Dallas. The proposal for joint operation of the college was endorsed by the Dallas County Medical Society (President John J. Golforth, pathology) and the Dallas Southern Clinical Society (President Ozro Woods, general surgery). It was also endorsed by the staff of various hospitals and the Dallas Baylor Alumni Association. The Baylor dental college was also included in the proposal. Under the proposed group plan, Baylor would direct education and academic aspects while Southwestern Medical Foundation would control the physical affairs. Construetion was to be completed in 2 years, and titles to all buildings constructed by the foundation would remain at all times with the foundation. The college of medicine was to be governed by an administrative committee consisting of 3 members appointed by the foundation and 2 members appointed by the trustees of Baylor. This gave voting control to the foundation. Terms of the proposed agreement called for the foundation to provide 20 acres of land and a minimum of $ 1 million, of which $750,000 would be used for new quarters for the medical and dental colleges. It was noted that the Southwestern Medical Foundation was nonsectarian and the medical school at the projected center, as well as other activities, would be nonsectarian. However, it was also noted that there had never been any problems with appointment of faculty by religious creed at Baylor Hospital. In fact, one of the largest donor groups to Baylor Hospital was the Jewish community. The board at Baylor in Waco approved the agreement on June 23,1942, and on June 7 the agreement was also approved by the executive committee of the Baptist General Convention of Texas. Finally, in November 1942, the entire Baptist convention approved the agreement (78, 79).
Dean Moursund opposed Baylor's alliance with the foundation because he feared it would cause control of the medical school to shift from Baylor to Dr. Cary in the downtown “establishment.” There was also speculation that many others at Baylor opposed the agreement because it would change the medical school's affiliation from Baylor to Parkland Hospital since the new medical school facility would be located adjacent to Parkland. Baylor could not accept this. The agreement also stated that while the college was at its present location, it would be responsible to Baylor trustees; however, on occupation at its new location, if at any time the Baylor trustees failed to agree with its administrative committee, the Southwestern Medical Foundation would have the right to order Baylor to remove its college from the foundation property. When the buildings were to be completed, Baylor would have to agree to move its school from its present location to the new structures (79). It should be noted that throughout the years, the college of medicine had been operated and conducted without any sectarian or denominational interference; in fact, Dr. Cary had been a Presbyterian.
The Southwestern Medical Foundation had a contract with the city and county of Dallas for the use of Parkland Hospital as its clinical facility. The contract was approved by the Dallas City Council on May 10, 1943, subject to confirmation by the Dallas county commissioners. The foundation agreed to furnish a sufficient number of physicians and surgeons to direct and supervise professional services of all inpatients and outpatients of the city-county hospital system, and the activities would be confined to Parkland Hospital. At least 75% of the cost of such supervision would be furnished by the foundation, and the remaining 25% would be assumed by the city and county by their option. The city and county would bear the expense of interns and of hospitalization of patients. The foundation alone would have the right to submit to the medical advisory council of the city-county board all nominations of the medical staff, and the contract would remain in effect 25 years. This contract with the city and county simply meant that Baylor University College of Medicine was to be excluded from the use of Parkland Hospital for clinical teaching unless it was willing to recognize the fact that its control was completely vested in the administrative committee formed under the terms and under the agreement between Baylor and Southwestern Medical Foundation, and that the control of the college had been divested from the trustees of Baylor University. When the issues became so clearly defined, only 10 months after the original agreement, the Baylor trustees were compelled to advise the foundation that there was not a meeting of the minds with reference to construction of the agreement and that by mutual accord, it should be canceled. The agreement was canceled on April 27, 1943 (80).
Move of Baylor University College of Medicine to Houston (1943)
According to Powhatan James, three trustees of Baylor University Hospital, Carr P. Collins of Dallas and two individuals from San Antonio, D. K. Martin and H. L. Kokernot, contacted important people in organizations in Houston who were known to be interested in having the Baylor medical college located in Houston (81). As a result, Baylor University College of Medicine was invited to move from Dallas to Houston. A proposal was drawn up by the M. D. Anderson Foundation with major stipulations that the foundation would provide Baylor University College of Medicine with an adequate campus site in the medical center and would contribute $ 1 million for construction of a college building and another $ 1 million, payable $ 100,000 annually, primarily for research. The proposal was submitted to the board of trustees of Baylor University on May 5, 1943. It stated the M. D. Anderson Foundation would furnish and donate two new suitable sites of 20 acres in the proposed Texas Medical Center to be used solely as a location for the Baylor medical school and dental college. This proposal was made with the definite agreement and understanding that the M. D. Anderson Foundation would have no part in the management and control, directly or indirectly, of the operations or policies of the Baylor medical school or dental college.
The proposal was accepted by the board of trustees of Baylor University on May 7, 1943 (81). Later it was decided that Baylor College of Dentistry would not move to Houston, and the dental school has continued to operate in Dallas. In the agreement with the Southwestern Medical Foundation, the foundation entered into the control and conduct of the medical college directly, emphasizing that there could be no sectarianism. However, it recognized that the college has appointed faculty and selected students for admission without any sectarianism and wished that it be continued in that manner. Many things were done to embarrass Baylor University College of Medicine. Pressure was brought to bear upon the salaried faculty to join Southwestern Medical Foundation's school. Attempts to embarrass the Baylor medical college were directed toward creating unfriendliness and noncooperation among the members of the Houston medical profession (78). Dean Moursund felt that the college could not survive in the atmosphere that had been created in Dallas. He thought that at long last the college would have the opportunity to develop into an institution of the first rank.
The 1942–1943 medical college session opened on September 28, 1942, with a total enrollment of 318 students, with 84 freshmen. Early in the session, it was announced that beginning in June 1943 the medical college would enter upon an accelerated program of instruction because of wartime pressure to supply doctors for the military service. In spite of the turmoil during the last months of the 1942–1943 session, the commencement exercise for 77 graduates at Baylor University College of Medicine was held on May 31, 1943, at the First Baptist Church in Dallas. The commencement address was delivered by Dr. Ernst William Bertner of Houston, acting director of the M. D. Anderson Hospital for Cancer Research. The topic of his address was “A New Era of Medicine.” Dr. George W Truett, pastor of the First Baptist Church in Dallas and member of the board of trustees of Baylor University, delivered the baccalaureate sermon to the class on Sunday, May 30, 1943. These exercises marked the close of the final session in Dallas and the 43rd academic year of the college (79).
The University of Dallas Medical Department, during its 3 years of operation, had a total of 37 graduates, and Baylor University College of Medicine, during its 40 years of operation in Dallas, had a total of 1670 graduates (79). Its greatest weakness was insufficient and improperly arranged space for laboratory departments and insufficient operating funds. There was little endowment, and research was very limited. The clinical opportunities for the students, however, were more than adequate, and the clinical teaching was conducted very effectively by a voluntary faculty.
Financial support was increased in Houston when the directors of the chamber of commerce of Houston voted on May 11, 1943, to support the solicitation of $50,000 a year for 10 years for operating expenses of the college (79). It was subscribed in a relatively short time.
Concerns voiced by Houston physicians (1943)
Some members of the medical profession in Houston were disturbed by the prospect of having the medical college located in Houston; they felt that the medical society should have been consulted, or at least confided in, before the decision was reached to move the college. The Harris County Medical Society appointed a fact-finding committee, which met with the dean on Friday, May 14, in the Society Library in the Medical Arts Building. After this meeting, the Harris County Medical Society voted to cooperate with Baylor in the relocation of the college. The liaison committee issued a statement that said that the removal of the medical college to Houston, with its largely increased endowment and its fine facilities for research and clinical teaching, made it a real acquisition and asset to the city of Houston and that portion of the state. The board of managers of Jefferson Davis Hospital, at a meeting held on June 4, 1943, gave unanimous approval of a resolution to welcome and assure the medical college of its wholehearted support, the details of cooperation to be worked out between the staff of the hospital and the college. The board of trustees and the medical staff of Hermann Hospital took appropriate action to cooperate with the medical college in its educational program. The other hospitals of the city, Memorial, Methodist, St. Joseph's, and Tuberculosis Hospital, all made their facilities available to the college for clinical teaching.
Dr. Wilton M. Fisher, associate professor of bacteriology and preventive medicine, assumed the task of supervising the loading and shipment of the equipment from Dallas to Houston. The first 4 vanloads of equipment were received in Houston on June 9, 1943. The new impressive library building in Dallas, which had been occupied for the short period from December 1, 1941, had to be abandoned (Figure 33). The books, journals, and furniture and equipment of the library that belonged to the college were transferred to Houston. The temporary building used by the medical school in Houston was the former retail store of Sears, Roebuck and Company, which was a 2-story plus basement, brick-and-Stone building on Buffalo Drive and Lincoln Street. It was only a few blocks from Jefferson Davis Hospital. A lease of the building was obtained, and remodeling was begun promptly (82) (Figure 34).
Figure 33.
Baylor University College of Medicine library building in Dallas. Photo courtesy of Baylor College of Medicine.
Figure 34.
The Sears building, the first site of Baylor University College of Medicine when it moved to Houston. Photo courtesy of Baylor College of Medicine.
In November 1943, the M. D. Anderson Foundation purchased 134 acres of Hermann Park, which is located in the southern section of the city, from the city of Houston for $400,000. This was to become the site of the Texas Medical Center. Four years later, the first building in the center was completed.
Southwestern Medical College (1943)
In 1943 the Southwestern Medical Foundation established Southwestern Medical College in temporary buildings near Parkland Hospital in Dallas. Some members of the full-time faculty and many of the clinical faculty of Baylor University College of Medicine accepted appointment to the faculty of the new school. Most of the medical students elected to remain in Dallas despite President Neff's visit to Dallas, in which he met with the students and encouraged them to move to Houston.
For the first 3 months in 1943 as Southwestern Medical College emerged, the school was moved into the old Alex W. Spence Junior High School, which had previously been shut down. Dr. Cary, with Bradley Colley, chief of surgery for the Dallas-based 8th Service Command, agreed to build plywood buildings. On July 16, 1943, Southwestern Medical Foundation was authorized to buy and construct 2900 square feet of barracks next to Parkland Hospital on Oak Lawn (83). Dr. Cary had to gain accreditation for the new school, which was easier for him since he had been president of the AMA. He quickly gained approval with class A status in July 1943, and Southwestern Medical College became the 68th medical school in the USA. The chamber of commerce and citizens council agreed to fund the school at $100,000 per year for 10 years.
Truett Memorial Hospital (1944)
On July 7, 1944, at the age of 77 years, Rev. George W. Truett died. He had served as a trustee at Baylor University Hospital for 41 years from 1903 to 1944 and was the longest-standing member. He had received the title of “father of Baylor University Hospital.” Within a week after his death in 1944, the executive committee of the Baylor University board of trustees approved a plan for the “Truett Memorial Hospital.” There was considerable difficulty in raising money and it would have been simple to apply for federal funds, but Baylor refused to take this route, even though it was eligible. “Boone Powell, Sr., then Baylor Hospital's young business manager, said Texas Baptists not only believe in separation in church and state, but also in standing on their own financial feet, instead of seeking help from the government” (84). George W. Truett Memorial Hospital opened on November 30, 1950, as an 8-story, 436-bed hospital. Its final cost was $5.5 million. It contained 17 operating rooms as it does today, and Baylor Hospital, overnight, became the fifth-largest hospital in the entire country based on number of beds.
Dr. C. M. Rosser's death (1945)
Approximately 6 months after Dr. Truett's death, Dr. Charles M. Rosser, the father of Baylor University College of Medicine and founder of the Good Samaritan Hospital from which Baylor Hospital had evolved, died on January 27, 1945, at age 83 years. He had continued to be active on the clinical voluntary faculty until 1938 when he became emeritus professor of clinical surgery.
Staff reorganization after World War II (1946)
Eight months after Dr. Rosser died—on August 6, 1945—the atomic bomb was dropped on Hiroshima, and on August 14, 1945, Japan unconditionally surrendered, ending World War II. With physicians returning from World War II, the hospital staff was reorganized. To implement the reorganization, Baylor physicians circulated a petition throughout the medical staff, obtaining enough signatures to submit an official request that the trustees appoint a chief of service for each department (85). Dr. H. Walton Cochran was appointed chief of surgery in 1946.
Likewise, there were administrative changes. In October 1948, the board of trustees of Baylor University Hospital made major changes in the managerial structure. The administrator, Lawrence Payne, was named to a newly created position of director of the hospital, and Boone Powell, Sr., was designated as his successor in the position of administrator and chief executive officer. Mr. Powell was from Tennessee and had joined Baylor University Hospital as business manager 3 years earlier. Baylor would have to move from treating primarily charity patients (as the medical school had dictated) to treating private patients since the medical school had moved. This necessitated building several new facilities.
Dallas Society of General Surgeons (1946)
When surgeons returned to Dallas from World War II, a small group met to form a society of surgeons to be called the Dallas Society of General Surgeons whose members limited their practice to general surgery as opposed to subspecialty practice. The organization started January 7, 1946, with the following 17 charter members, many of whom were on the Baylor staff (86):
Sam Weaver (the first president; chief of surgery at Baylor)
William A. Altman (only surviving member)
Charles D. Bussey
C. B. Carter
H. Walton Cochran
J. W. Duckett
J. Hudson Dunlap
Sidney Galt
John V. Goode
Ben F. Harrison
Lee Hudson
G. D. Mayhon
J. H. McCracken, Jr.
Frank A. Selecman
Andrew B. Small
H. O. Taylor
Ozro T. Woods
Early on, membership was difficult to obtain since one negative vote could prevent membership. Subsequently, three negative votes were required, and by 1967 negative votes by 10% of the active membership were required to prevent membership. The organization grew to a current membership of over 100 active members. While Dr. Ronald C. Jones was president, the executive committee recommended and the membership approved the requirement for board certification for membership on November 22, 1977. Prior to that, the only requirement for membership was board eligibility for examination or membership in the American College of Surgeons.
Dr. Cary's death (1953)
Baylor University Hospital celebrated its 50th birthday in November 1953 and had grown to 850 beds. Dr. Cary, the man who had played such a prominent role in Baylor's fortunes during its first 50 years, lived to witness the hospital's golden anniversary, but he died 2 months later, on December 11, 1953, at the age of 81.
Mobile recovery service and recovery room (1954)
In 1954, the hospital established a unique approach to providing a new service to the patients, “the mobile recovery service.” When the hospital had been built, the value of having a recovery room for postoperative patients had not been fully realized, and when the decision was made to incorporate such a unit in the hospital, there was no conveniently located space for the service. Specially trained nurses had a mobile unit, similar to a grocery store cart, with a suction machine, drugs, oxygen, and intravenous solutions. They would accompany the patient from surgery to the hospital room and remain there until the patient had awakened from the anesthetic. A central recovery room department did not become available at Baylor for another 12 years, in 1962 (87).
Name change to Baylor University Medical Center (1959)
The named change from Baylor University Hospital to Baylor University Medical Center was announced during the opening ceremonies for the Women and Children's Hospital on October 28, 1959 (88).
CHIEFS OF SURGERY
First chief: Dr. Edward H. Cary (1925–1929)
In the 1925–1926 catalog, the chairman of the Department of Surgery was noted for the first time: Dr. Edward H. Cary, who was also professor of ophthalmology and otolaryngology (89) (Figure 35). Dr. Cary was born in Union Springs, Alabama, on February 28, 1872. He came to Dallas to work for his brother in the dental supply business. Dr. Cary obtained his medical education from Bellevue Hospital Medical College in 1898 and interned at Bellevue Hospital. He served at the New York Eye and Ear Infirmary and at the New York Polyclinic. Dr. Cary came to Dallas in 1901 and became professor of ophthalmology and otolaryngology at the Dallas medical college. He was president of the Dallas County Medical Society in 1910; dean of Baylor University College of Medicine from 1902 until 1920; and chairman of the Department of Surgery from 1925 to 1929. He married Georgie Fonda Schneider on April 19, 1911.
Figure 35.

Dr. Edward H. Cary, 1925–1929.
In addition to his medical duties when he returned to Dallas, Dr. Cary took over the management of A. P. Cary Surgical Supply Co., which had been founded by his brother, and he continued as president of that business. In 1923 he opened the Medical Arts Building prior to being chairman of the Department of Surgery. He served as president of Group Hospital Service, the Texas affiliate of Blue Cross, and as director of the Republic National Bank.
Dr. Cary was president of the Texas Medical Association in 1917–1918 and was the first president of the Texas Society of Ophthalmology and Otolaryngology. He was a trustee of the AMA from 1925 to 1929 and became president of the AMA in 1932, 3 years after stepping down as chairman of the Department of Surgery. He was the first president of the AMA from Texas.
In special ceremonies held in the library in Cary Hall on Friday evening, October 11, 1929, a life-sized bust of Dr. E. H. Cary, the chief of surgery and former dean of the college from 1902 to 1920 and then dean emeritus, was unveiled. Dr. Cary was referred to as the dean, the citizen, the physician, and the teacher and was given credit for development of the medical college, an institution recognized as class A. Dr. A. I. Folsom, the new chairman of the Department of Surgery at the college and chairman of the faculty committee, made the formal presentation on behalf of the faculty (90). He was president of the Dallas Historical Society and of the Texas Philosophical Society. Dr. Cary organized and became president of the Southwestern Medical Foundation and helped form the University of Texas Southwestern Medical School under the foundation (91). He also served as president of the Southern Medical Association. In 1945, Dr. Cary won the Linz Award as Dallas' outstanding citizen for his work in the Southwestern Medical Foundation. Dr. Cary died on December 11, 1953, just prior to the opening of the current and third Parkland Memorial Hospital. The name was changed from Parkland Hospital to Parkland Memorial Hospital following World War II to honor those killed in the war.
Second chief: Dr. Alfred I. Folsom (1929–1936)
Dr. Alfred Iverson Folsom is listed in the Baylor University Bulletin dated May 1920 as associate in genitourinary diseases, in 1923 as professor of urology, and in April 1929 as chairman of the Department of Surgery, having replaced Dr. Cary (Figure 36). He remained chairman until 1936. Dr. Folsom was born on May 9, 1883, at McGregor, Texas, and received his doctorate of medicine degree from Southwestern Medical College of Dallas in 1908. He did postgraduate work at Rochester, Minnesota. Dr. Folsom began practice in Alba, Texas, before moving to Dallas in 1910, where he practiced urology until his death. Dr. Folsom, a Methodist, married Anne Rebecca Hodge on September 29, 1909. He was one of 9 urologists who organized the American Board of Urology. He was president of the Texas Surgical Society in 1934 and president of the South Central Urological Society. He was chief of the Department of Urology at Parkland Hospital from 1923 to 1946. Dr. Folsom was president-elect of the American Urologic Association at the time of his death. He was killed in an automobile accident near Dallas on October 3, 1946, when he was returning from a meeting of the South Central Urologic Society in Hot Springs, Arkansas (92).
Figure 36.

Dr. Alfred. I. Folsom, 1929–1936.
In the Baylor University Bulletin dated April 1931, Dr. J. Warner Duckett is noted to be an instructor in clinical surgery and would eventually be a chief of surgery at Baylor (93). In the 1934–1935 bulletin, Dr. John V. Goode is listed as instructor of clinical surgery (94).
In the 1935–1936 bulletin, Dr. James Hudson Dunlap, Dr. Frank A. Selecman, and Dr. Andrew B. Small, Jr., are all listed as assistants in clinical surgery (95). Each would become a wellknown clinical surgeon in Dallas. No bulletins are available for the college of medicine from 1936 to 1950.
Third chief: Dr. C. W. Flynn, Jr. (1936–1941)
Dr. C. W. Flynn is noted to be professor of operative surgery in the catalog dated 1919–1920; Dr. Bacon Saunders is listed as professor of surgery and clinical surgery (96). Dr. Sanders was president of the Texas Medical Association in 1897. Dr. Charles W. Flynn, Jr., was born on March 28, 1884, on the Egypt Plantation, Lakeland, Louisiana. His medical education was received at the University of Pennsylvania, from which he graduated in 1911. He interned at St. Francis Hospital in Pittsburgh and moved to Dallas in 1912. Dr. Flynn was a fellow of the American College of Surgeons, a member of the Southern Surgical Association, and president of the Texas Surgical Society in 1936. Dr. Flynn became chief of surgery in April 1936 and was probably chief for a few years (Figure 37). A member of the Methodist church, he died at his home on August 13, 1943, of a cerebral hemorrhage (97).
Figure 37.

Dr. C. W. Flynn, Jr., 1936–1941.
Fourth chief: Dr. Christopher Bennett Carter (1941–1943)
Dr. Carter graduated from the University of Texas Medical Branch in Galveston in 1919. He practiced surgery at Baylor University College of Medicine in Dallas beginning in 1922. In World War II, he recruited the staff of the army's 58th Evacuation Hospital, in which he was chief of surgery, serving in North Africa and in Italy. He became chief of surgery in 1941 as well as president of the Baylor staff. He served as chief for 2 years until 1943 (Figure 38). Dr. Carter was professor of surgery and applied anatomy. In 1954, he was president of the Texas Surgical Society. He was an honorary member of the Texas Medical Association and the Dallas County Medical Society. He retired from practice in 1967. Dr. Carter was a member of the American College of Surgeons and the Southwestern Surgical Congress. He was a member of the First Baptist Church of Dallas and a former president of the Idlewild Club. Dr. Carter died at age 88 on August 12, 1981.
Figure 38.

Dr. C.B. Carter, 1941–1943.
Fifth chief: Dr. Sam D. Weaver (1943–1946)
Dr. Sam Dinwiddy Weaver was appointed to the Baylor staff on August 1, 1943, as professor of clinical and operative surgery and acting chairman of the Department of Surgery. He became the chairman from 1943 to 1946 (Figure 39). Dr. Weaver was born in Pontotoc, Mississippi, on November 1, 1887. He graduated Alpha Omega Alpha in 1916 from Tulane University of Louisiana School of Medicine, New Orleans, and completed a 1-year internship at Baylor Hospital in Dallas. For 7 months he was a fellow in surgery at the Mayo Clinic. He was a captain in the Medical Reserve Corps from February 1918 to June 1919, attached to Base Hospital 26 in France with the Baylor-Mayo unit. He was a fellow of the American College of Surgeons and former president of the Texas Surgical Society. Dr. Weaver became an associate professor of clinical surgery and operative surgery at Baylor University College of Medicine (98).
Figure 39.

Dr. Sam D. Weaver, 1943–1946.
Dr. Weaver died at Parkland Hospital on January 20, 1950. A few days after he was admitted to Parkland Hospital, he had his hair cut. When the barber finished, Dr. Weaver asked how much he owed him. Unbuttoning his shirt and pointing to the operative scar, the barber said, “You don't owe me anything. If it hadn't been for you, I wouldn't be here now.” The barber had been a charity patient of Dr. Weaver's at Parkland.
Sixth chief: Dr. H. Walton Cochran (1946–1950)
Following World War II with the reorganization and departmentalization of departments, Dr. H. Walton Cochran was appointed chief of surgery from 1946 to 1950 (Figure 40). He was one of the first members of the new medical board in 1946.
Figure 40.

Dr. H.Walton Cochran, 1946–1950.
Dr. Cochran was born in Belton, Texas, on February 18, 1904. He received his medical degree at Johns Hopkins University School of Medicine in 1928 and interned at Peter Brigham Hospital in Boston, Massachusetts. He completed his surgery residency at Presbyterian Hospital in New York City in 1934 and entered private practice in Dallas. Dr. Cochran was an honorary member of the Dallas County Medical Society. He died at his home on July 28, 1953.
Seventh chief: Dr. J. Warner Duckett (1951–1967)
Dr. J. Warner Duckett became the chairman of the Department of Surgery in 1951 (Figure 41). He had been appointed acting chairman on January 13, 1950, following Dr. Cochran's illness. He was chairman for 16 years until 1967. Dr. Duckett was born in Florence, Alabama, and grew up in Houston. He was an Alpha Omega Alpha graduate of Johns Hopkins University and did a 1 -year internal medicine internship prior to entering surgery. Dr. Duckett married Carolyn Knorr, a nurse in training at Johns Hopkins. He then spent 1 year at Boston Children's Hospital under the direction of Dr. William E. Ladd, the well-known pediatric surgeon. He came to Dallas for a final year of general surgery residency in 1930 at St. Paul Hospital. He later received a research appointment at the Rockefeller Institute. Dr. Duckett was with the Dallas Medical and Surgical Clinic for 23 years; after 1951 his primary hospital affiliation was at BUMC and Texas Children's Hospital. He was a pediatric surgeon and was the first surgeon to perform the Blalock-Taussig (blue baby) operation in the Southwest. He also served as chief of surgery at Texas Children's Hospital from 1945 until 1960. He was president of the Texas Surgical Society in 1963.
Figure 41.

Dr. J. Warner Duckett, 1951–1967.
Dr. Duckett started as instructor in clinical surgery in 1930. He is credited with the early growth of heart surgery at Baylor. He was chairman of the medical board from 1956 until 1967. In 1964–1965 he appointed Dr. James Garvey program director. However, Dr. Garvey left to enter private practice in Wheeling, West Virginia, after 1 year. Dr. Duckett died from a dissecting thoracic aortic aneurysm while en route to the hospital to perform elective surgery on November 7, 1967. Following his death, co chairmen were named for the Department of Surgery: Dr. Robert S. Sparkman and Dr. Jesse E. Thompson. They served for 1 year until Dr. Everard Cox was selected as the permanent chairman.
Eighth chief: Dr. Everard F. Cox (1969)
Dr. Everard Cox was the chairman of the Department of Surgery from January 1, 1969, until July 10, 1969. Dr. Cox was born on November 27, 1920, at St. George, Utah, and obtained his medical degree from the University of Maryland in 1955, where he was president of his class. He completed his residency at the University Hospital in Baltimore, Maryland, in 1960. He came to Baylor's Department of Surgery after being an assistant professor of surgery at the University of Maryland School of Medicine for 6 years. During World War II, he was a US navy carrier aviator and was on active duty for 5 years. His military decorations include Distinguished Flying Cross, Air Medal, Admiral's Commendation, Asiatic-Pacific Theatre Ribbon—9 Stars, and Pro-Pearl Harbor Ribbon. Dr. Cox now resides in Hempstead, Maryland.
Ninth chief: Dr. Robert S. Sparkman (1969–1981)
Dr. Robert S. Sparkman (Figure 42) was chief of surgery in 1969 and served 12 years in that position until December 1981. Dr. Sparkman was born in 1912 at Brownwood, Texas, the son of Viola and Ellis Sparkman. His father had been chairman of the Department of Spanish at Baylor University in Waco. Dr. Sparkman graduated from Baylor University College of Medicine in 1935 and completed a general surgery residency at Cincinnati General Hospital under Dr. Mont Reid in 1940. He immediately entered the US Army in 1940 and served for 6 years, eventually rising to colonel, and was honored with an Oak Leaf Cluster, Bronze Star, Invasion Arrowhead, and 3 battle stars. In 1942, while in the service, he married Willie Ford Bassett, a debutante in Dallas who was born in Kosse, Texas. Dr. Sparkman returned to Dallas after his military duty in 1946.
Figure 42.

Dr. Robert S. Sparkman, 1969–1981.
Throughout his professional career, Dr. Sparkman maintained an interest in clinical, historical, and biographical investigation. His particular interest was in the biliary tract. He edited The Texas Surgical Society, The First Fifty Years (1915–1965). He assisted with editing of the 2-volume edition of minutes of the American Surgical Association, 1880–1980. He edited The Southern Surgical Association, The First 100 Years (1887–1987) and was made an honorary member of the Southern Surgical Association. Dr. Sparkman served as a governor of the American College of Surgeons, president of the Texas Surgical Society (1965), president of the Southern Surgical Association (1978), and vice president of the American Surgical Association (1977). In 1976 Dr. Sparkman was honored as a distinguished alumnus of Baylor University, having received an honorary doctor of laws degree from Baylor University in Waco in 1974. Prior to his death, the North Texas Chapter of the American College of Surgeons established the Robert S. Sparkman lectureship. He was a strong advocate of continuing medical education; he was one of the founders of the Association of Program Directors in Surgery and was eventually made an honorary member of that organization. Dr. Sparkman was the first to establish significant endowments for the Department of Surgery with philanthropic support. The original gift in the amount of $ 115,702 was made on December 12, 1979. Dr. Sparkman utilized some of the endowment to found the Society of Baylor Surgeons, which now has a membership of 320.
Just prior to Dr. Sparkman's death, a dinner was held at the Dallas Petroleum Club on July 16, 1996, and architectural drawings were unveiled for the construction of the Robert S. Sparkman Library and Conference Center in the Department of Surgery at BUMC. The dinner was moderated by Dr. Ronald C. Jones. Appropriate comments were made by Boone Powell, Jr., and Joel Allison, administrative leaders; Gordon Caswell and Charles Cooper of Baylor Health Care System Foundation; and Drs. Harold Cheek and Allan Bookatz. The library and conference center was completed in January 1998 and dedicated on June 11, 1998.
During Dr. Sparkman's tenure, fundraising for a chair for the chief of surgery was started in 1976 and $l million was eventually raised by 1986. Dr. Ronald C. Jones was named the first Robert S. Sparkman Chairman in Surgery in 1987. Dr. Sparkman died on March 25, 1997.
Tenth chief: Dr. Jesse E. Thompson (1982–1986)
Dr. Thompson assumed the position of chief of surgery on January 1, 1982, a position he held for 4 years (Figure 43). Jesse Eldon Thompson was born in Laredo, Texas, on April 7, 1919. He obtained his medical degree from Harvard Medical School in 1943, graduating as an Alpha Omega Alpha. His surgical training was for 3 years at the Massachusetts General Hospital and the remainder at Massachusetts Memorial Hospital in Boston under Dr. R. H. Smithwick. The following year he was awarded both the Fulbright scholarship and the Rhodes scholarship to Oxford University in England. He was at the Nuffield Institute for Medicine and Research, studying cardiovascular physiology at Oxford University, England. His initial Rhodes scholarship appointment was in 1939; however, it was delayed by World War II. In 1944 he married Madeleine Curtis, a nurse at Massachusetts General Hospital. He entered the private practice of surgery in 1950 with Dr. Reginald H. Smithwick in Boston and practiced for 4 years prior to moving to Dallas. Dr. Thompson came to Baylor University Hospital in the private practice of vascular surgery with Dr. Dale J. Austin in 1954. He established a vascular surgery fellowship at BUMC 10 years later in 1964 and trained over 60 vascular surgeons. Dr. Thompson has numerous honorary memberships, including the Vascular-Surgical Society of Great Britain and Ireland and the European Society for Vascular Surgery. In 1978 the Jesse E. Thompson Vascular Surgical Society was established by the surgeons finishing the Baylor vascular program. Initially, there were two vascular fellowship programs, the other under the direction of Dr. Gene Wheeler.
Figure 43.

Dr. Jesse E.Thompson, 1982–1986.
Dr. Thompson has served as president of the Society for Vascular Surgery, the North American Chapter of the International Cardiovascular Society, and the International Society for Cardiovascular Surgery. He was president of the Southern Association of Vascular Surgery and president of the Texas Surgical Society in 1972. Dr. Thompson was a governor, treasurer, and vice president of the American College of Surgeons. He has served as second vice president of the American Surgical Association and was a director of the American Board of Surgery. Dr. Thompson has served on the editorial boards of Surgery, Journal of Cardiovascular Surgery, and Journal of Vascular Surgery.
In 1987 a fund was established to create the Jesse Eldon Thompson Surgical Education and Research Endowment. By this creation, the annual Jesse E. Thompson Visiting Vascular Professorship was established. Dr. Thompson resigned as chairman of the Department of Surgery on August 31, 1986.
Eleventh chief: Dr. Shields O. Livingston (1986–1987)
Dr. Shields Livingston was appointed acting chairman on September 1, 1986, a position he held for 11 months until July 20, 1987 (Figure 44). Dr. Shields Osco Livingston was born on December 14, 1919, in Morristown, Tennessee. He obtained his medical degree from Washington University School of Medicine in 1950. His residency was completed at the Veterans Administration Hospital in McKinney, Texas, in 1955, and he joined the attending staff at Baylor. Dr. Livingston married Harriette Lutz, who became an anesthesiologist at Presbyterian Hospital. Dr. Livingston is a member of the Texas Surgical Society, Western Surgical Association, and American College of Surgeons. He retired from active practice on June 30, 1990, and was placed in the honorary retirement category.
Figure 44.

Dr. Shields O. Livingston, 1986–1987.
Twelfth chief: Dr. Ronald C. Jones (1987-present)
Dr. Ronald Coy Jones was appointed chairman of the Department of Surgery on July 20, 1987, and was the first Robert S. Sparkman Chair in Surgery (Figure 45). He was born in Harrison, Arkansas, and obtained his medical degree from the University of Tennessee in 1957. Dr. Jones married Jane A. Allison, a dietitian from Fordyce, Arkansas, in 1956. He did a rotating internship at Los Angeles County General Hospital (1957) and completed a 2-year general practice residency at the University of Oklahoma (1958–1960) prior to completing his general surgery residency at Parkland Memorial Hospital in Dallas in 1964 under Dr. Tom Shires.
Figure 45.

Dr. Ronald C. Jones, 1987—present
As a chief resident in general surgery, Dr. Jones participated in the care of President John F. Kennedy when ne was assassinated in Dallas and brought to Parkland Memorial Hospital in 1963. He also was one of the surgeons who operated on Lee Harvey Oswald, the presumed presidential assassin.
Dr. Jones joined the staff at the University of Texas Southwestern Medical School in 1964 as instructor and rose to professor and acting chairman of the Department of Surgery 10 years later on January 1, 1974, a position he held for 2 years and 3 months. He is the only surgeon to be chairman at both the University of Texas Southwestern Medical School and BUMC. During his 23-year tenure on the faculty at the medical school, he held the positions of president of Parkland medical staff, president of the North Texas Chapter of the American College of Surgeons, president of the Dallas Society of General Surgeons, and second vice president of the Texas Surgical Society.
He was the chairman of the medical advisory committee that established the current emergency medical services system and ambulance service in Dallas in 1971. For this effort, he was recognized by the Dallas Hospital Council, the Dallas county commissioners, the North Central Texas Council of Governments, the Dallas City Council, and two mayors of Dallas, Adlene Harrison and Wes Wise.
Dr. Jones was very active in the American College of Surgeons, serving as the national chairman of the field liaison program, the committee that encourages hospitals to obtain approval by the American College of Surgeons as cancer hospitals. He was chairman of the executive committee of the Commission on Cancer from 1979 to 1982 and vice chairman of the Commission on Cancer in 1983. Following his appointment as chairman of the Department of Surgery at BUMC, he became a governor, a member of the executive committee of the board of governors, and secretary of the board of governors of the American College of Surgeons from 1989 to 1994.
He served as second vice president of the Western Surgical Association in 1995–1996 and is also a member of the Southern Surgical Association, American Surgical Association, Society of Surgical Oncology, Surgical Infection Society, Southwestern Surgical Congress, and Societe Internationale de Chirurgie.
Under Dr. Jones' chairmanship, the general surgery residency program at BUMC has expanded from 4 chief residents per year in 1990 to 8 chief residents in 2002, which made it the largest general surgery residency program in the USA in a community based hospital. Approximately 17 residents trained under Dr. Warner Duckett from 1951 to 1967. Approximately 37 residents completed their training under Dr. Robert Sparkman from 1969 to 1980. Twenty residents completed training under Dr. Jesse Thompson. As of 2004, 90 residents have completed training under Dr. Ronald Jones.
DEPARTMENT OF SURGERY, 1970–2004
In the early years, the Department of Surgery offices were located in the Veal Building. In the early 1980s the department was temporarily relocated to the Gaston Annex to await the opening in December 1986 of its present location on the first floor of the A. Webb Roberts Building. The offices now comprise approximately 6000 square feet and include individual study carrels for each resident, the Sparkman Surgical Library and Conference Center, an educational resource center, a laboratory, and several administrative offices. An audiovisual telecommunications system was installed in 2001 between BUMC and John Peter Smith Hospital to allow combined conferences using a Tl telephone line. Live surgical procedures from the operating rooms are viewed in the Sparkman Conference Center on the first floor of Roberts Hospital and the 17th floor of Roberts Hospital.
W. W. Caruth Surgical Research Laboratory and Dr. LeRoy J. Kleinsasser
On March 17, 1964, Baylor opened an entirely different type of laboratory facility—the Caruth Surgical Research Laboratory. This new animal research facility was made possible by a $55,000 gift from the W. W. Caruth, Jr., Fund of the Dallas Community Chest Trust. It was named in honor of W. W. Caruth, a nationally recognized land planner and developer. The new laboratory replaced BUMC's old animal research facility, which had been located in the “shacks” behind the Wadley Blood Institute at Gaston Avenue and Adair Street.
The original laboratory had been started in 1950 by Dr. LeRoy J. Kleinsasser, who had come to Baylor as director of surgical education (Figure 46). According to Dr. Kleinsasser, he had been specifically contacted by Dr. Henry Winans, chief of staff and chief of medicine, primarily to oversee the general surgery residents.
Figure 46.

Dr. LeRoy Kleinsasser.
Dr. Kleinsasser was born on February 24, 1913, in North Dakota. He graduated from the University of South Dakota School of Medicine, which was a 2-year school, and then the University of Nebraska School of Medicine in 1936. He did a rotating internship at Nebraska and completed his general surgery residency at Tulane University in Charity Hospital from 1938 to 1942 under Dr. Alton Ochsner and Dr. Michael DeBakey.
Dr. Kleinsasser had been discharged from the army in 1946 and had served 4 years as chief of surgery at the Dallas Veterans Administration Hospital. Although the old laboratory was started under less than desirable conditions, it provided facilities for testing the validity of open-heart surgery and heart-lung pumps before they were used at BUMC (99).
Dr. Kleinsasser was not only a general surgeon but also a cardiac surgeon and a vascular surgeon. He remained in charge of the general surgery residency program from September 1950 until 1956, when he resigned from his position. Dr. Kleinsasser believed that the chief of surgery and the director of general surgery training should be the same person in order to provide a complete teaching and training program. During Dr. Kleinsasser's tenure, he applied to the Accreditation Council for Graduate Medical Education to increase the general surgery program from 3 years, which it was approved for in 1949, to 4 years. This was approved when Dr. Oscar Creech, whom Dr. Kleinsasser knew personally, surveyed the program. Dr. Kleinsasser also started a weekly journal club.
Dr. Kleinsasser performed the first successful abdominal aortic graft on September 1, 1954, at Baylor University Hospital in Dallas. This consisted of resection of a large abdominal aortic aneurysm and replacement with a freeze-dried homologous bifurcation aortic graft.
Dr. Kleinsasser is a member of the Society of University Surgeons, Society of Vascular Surgery, International Cardiovascular Society, Southwestern Surgical Congress, and Western Surgical Association and is a fellow of the American College of Chest Physicians.
In 2001 the Caruth Laboratory was torn down to make way for a new thoroughfare and the Baylor Jack and Jane Hamilton Heart and Vascular Hospital, which opened in 2002.
Surgical advisory committee
In 1988 Dr. Jones organized the surgical advisory committee for the Department of Surgery, patterning it somewhat after the Department of Internal Medicine advisory committee. Eventually the makeup of the committee was 12 members, 6 of whom were appointed by the department primarily as division chiefs or vice chairman and 6 of whom were elected, 2 each year for a 3-year term, by the staff in the department.
GENERAL SURGERY RESIDENCY PROGRAM
The first intern at the University of Dallas Medical Department was Dr. William White Shortal, who graduated in 1909 and interned for 1 year in medicine and surgery. He subsequently joined the staff and rose to professor of surgery in 1929. Each year from 1909, there has been an intern or resident in training, although early on, the residency was only 1 year. By 1938, the interns were furnished room and board and laundry; however, they had to furnish their own uniforms and were given a stipend of $25 a month. By 1945, there were 14 interns and 10 residents at Baylor University Hospital, but only a total of 3 residents were surgery residents, or one resident per year (Table 1).
Table 1.
Surgical interns and residents at BUMC, 1909 to 1951
| Name | Period of internship | Period of residency |
| William W. Shortal | 1909 | |
| Joseph H. Dorman | 1912–1913 | |
| Samuel D. Weaver | 1916–1917 | |
| Hall Shannon | 1917 (6 months) | |
| Robert W. Cowart | 1917–1918 | |
| Penn Riddle | 1919–1920 | 1920–1921 |
| J. H. McGuire | 1920 | 1921–1922 |
| Robert F. Short | 1921 | |
| George Eugene Morris | 1920–1921 | 1921–1923 |
| H. Frank Carmon | 1922–1923 | 1923–1924 |
| Bernard Rubenstein | 1922–1923 | 1923–1925 |
| C. E. Carter | 1924–1925 | |
| Floyd R. Copeland | 1924–1925 | 1925–1926 |
| W. E. Schulkey | 1925–1926 | 1926–1927 |
| Elma May Fry | 1926–1927 | 1927–1928 |
| Rufus Alston Roberts | 1927–1928 | 1928–1929 |
| John L. Bradfield | 1928–1929 | 1929–1930 |
| A. L. Nelson | 1929–1930 | 1930–1931 |
| W. R. Weaver | 1930–1931 | 1931–1932 |
| J. S. Kerr | 1931–1932 | 1932–1933 |
| H. G. Williams | 1931–1932 | 1933–1934 |
| R. S. Willis | 1933–1934 | 1934–1935 |
| S. Galt | 1934–1935 | 1935–1937 |
| W. T. Henderson | 1935–1936 | 1936–1937 |
| Ben S. Harrison | 1936–1937 | 1937–1939 |
| J. B. Gordon | 1937–1938 | 1938–1940 |
| Dale S. Austin | 1938–1939 | 1939–1941 |
| Charles P. Donoho | 1939–1940 | 1941–1942 |
| Luis A. Kregel | 1940–1941 | 1941–1943, 1946–1947 |
| Charles B. Truett | 1940–1941 | 1941–1942 |
| Allen Crenshaw | 1942–1943 | 1946–1948 chief resident |
| Henry S. Montgomery | 1942–1944 chief resident | |
| Walter M. McNatt | 1944–1945 | |
| Carl A. Jordan | 1944–1945 | 1945–1946 |
| Keene F. Ludden | 1945 | 1945–1948 |
| Thomas P. Marinis | 1947–1950 chief resident | |
| J. Harold Cheek | 1945 (9 months) | 1948–1951 |
According to a letter from Dr. Robert S. Sparkman to Dr. Winfrey W Goldman, medical director of the John Peter Smith Hospital, Baylor obtained approval to finish 2 chief residents per year beginning July 1, 1970. By 1987, 4 residents were approved to annually complete the program. Dr. Ronald C. Jones obtained approval from the Residency Review Committee to finish 5 residents in 1991, 6 residents in 1992, 7 residents in 1996, and 8 residents in 2002. This is an outstanding achievement over a 10-year period and is a tribute to the surgery attending staff. The chief residents from 1952 to 2004 are listed in Table 2.
Table 2.
Chief surgical residents at BUMC, 1952 to 2003
| Year | Chief resident | Year | Chief resident | Year | Chief resident | Year | Chief resident |
| 1952 | C. Richard Bowers | 1977–1978 | John F. Anderson | 1988–1989 | Charles N. Headrick | 1997–1998 | Kathleen A. Crews |
| 1953 | Harold M. Mims | Julian Gomez | Bruce J. Hirschfeld | Patrick C. Dillawn | |||
| Ross Lee Curtis | Ronald S Kline | Joseph A. Kuhn | David L. Gish | ||||
| 1955 | George E. Reynolds | John W. Winter | Matthew V. Westmoreland | Mark G. Goss | |||
| George A. Balla | 1978–1979 | David B. McReynolds | 1989–1990 | Ronnie E. Calhoun | Guillermo P. Ponce De Leon | ||
| 1957 | Tom Hayes | George N. Peters | James E. Hagan | Randall A. Wright | |||
| 1958 | Paul R. Ellis, Jr. | Albert M. Rusher | Richard L. Tillquist | 1998–1999 | J. Clayton Collier | ||
| 1959 | Arturo Aguillan | Dan H. Shell | 1990–1991 | William M. Carpenter | Robert Farner | ||
| 1960 | Vernor F. Lovett | 1979–1980 | John E. Etlinger | Matthew A. Lovitt | Kristian Martin Ferry | ||
| Edward I. Hale | John T. Preskitt | Nancy G. Marquez | Robert A. Fuller | ||||
| 1962 | Arthur Grayson | Stephen A. Norris | Kevin M. O'Brien | Russell Gornichec | |||
| Stewart Wu | George A. Woodward | 1991–1992 | Robert C. Allen | Kinga Styperek | |||
| 1963 | Adel Nafrawi | 1980–1981 | Byron F. Cook | Clifford P. Clark | 1999–2000 | MarkBayouth | |
| Robert Hill | John A. Norris | Michael D. Grant | Daniel Diener | ||||
| 1965 | Felix Salerno | Daniel D. Tamez | John R. Moore | Erik Fetner | |||
| 1966 | Byron Brown | Brady C. Way | David M. Vanderpool | Brian Gogel | |||
| Raul Cruz | 1981–1982 | Richard C. Holmes | 1992–1993 | Kenneth Lynn Bryce | Stephen Maxwell | ||
| 1967 | Felix Peppard | J. Kelly Mahone | James Allan Day | John Schultz | |||
| Manuel Baeza | John Charles Nash | David Hampe | 2000–2001 | John C.Conrad | |||
| 1969 | James Cowan | Randall D. Rogers | Richard A. Katseres | Nathan T. Dew | |||
| Norman Hanks | 1982–1983 | Kenneth W. Eveland | Cecil D. Vaughn | Archana Ganaraj | |||
| Kenrick West | Fredrick C. Lester | 1993–1994 | Dana Carol Abraham | Salim H. Jabbour | |||
| 1970 | James Duff | Warren Lichliter | Glen Hanson | Jeffrey P. Lamont | |||
| 1971 | J. Peter Thiele | Bruce A. Smith | William J. Parker | David L. Stroman | |||
| 1972 | Ronald Atkins | 1983–1984 | M. Gareth Eck | John E. Roberts | Marc T. Warner | ||
| Evalea Glanges | David G. Fort | 1994–1995 | Larry Elliott | 2001–2002 | David T. Arnold | ||
| 1972–1973 | Philip Halloran | Jeffrey Jobe | Paul F. Fortes | Charles Bayouth | |||
| Mark Grisham | Gary Walker | Thomas T. Gallaher | Jeffrey D. Bell | ||||
| Robert Wilhelm | 1984–1985 | Bill Ardill | Johnny D. Howton | Wesley R. Heartfield | |||
| 1973–1974 | John George Henry | Robert Clark | Todd M. McCarty | Stacy L. Stratmann | |||
| Lawrence S. Barzune | Rob R. Cloud | Timothy M. McGee | Andrew Scott Walker | ||||
| John C. O'Brien | Charles T.Volk | 1995–1996 | Lisa K. Burton | 2002–2003 | James P. Carroll | ||
| 1974–1975 | John B. Barnett | 1985–1986 | Michael L. King | Harry Kourlis, Jr. | Alexandra Dresel | ||
| Thomas A. Cochran | Robert S. Pollard | Rita L. Lechleitner | Daniel C. Harris | ||||
| Charles E. Webber | Jay S. Roden | Jeffrey S. Lee | Todd O. Moore | ||||
| 1975–1976 | Michael S. Bumagin | Steve Schoettle | Carlos L. Macias | Blake A. Morrison | |||
| Robert M. Jacobson | 1986–1987 | Richard Anderson | Jeffrey S. Stephens | Amit N. Patel | |||
| Andrew B. Small III | Michael Foreman | 1996–1997 | Chris M.Cate | Michael Pendola | |||
| 1976–1977 | Howard C. Derrick | Bob McKinney | Julie A. Kwa | 2003–2004 | L. Scott Bloemendal | ||
| Philip L. Kelton | Paul Senter | Richard Gitter | Christopher Brennig | ||||
| Miles H. Mason | 1987–1988 | Mark E. Collins | Gordon H. Martin | Kevin M. Cottingham | |||
| L. Fabian Worthing | Jeffrey R. Stoltenberg | Todd A. Odom | Jason Harrison | ||||
| Martha A. Williams | David W. Ritter | Nelson Littrell | |||||
| Bridget Nelson |
Residency program directors and program coordinators
Since 1950, BUMC has had 4 residency program directors:
Dr. LeRoy Kleinsasser, 1950–1956
Dr. Jim Garvey, 1964–1965
Dr. J. Patrick O'Leary, 1985–1987
Dr. Ronald C. Jones, 1987–present
In the spring of 1989, Dr. Jones appointed Laurie Hardaway as the first full-time general surgery residency program coordinator to assist the program director of the general surgery residency program at BUMC. She had a master's degree in library science. After serving 6 years, she resigned from the position in 1995 and is now assistant director of the Dallas Public Library.
Bobbie Kenitzer was the second program coordinator appointed May 1995. Mrs. Kenitzer had previously been program coordinator in the Department of Surgery at the Medical College of Wisconsin for 4 years and prior to that was at Emory University in the Department of Pediatrics. She was a graduate of the University of Wisconsin. Mrs. Kenitzer was president-elect of the National Association of Program Coordinators but died unexpectedly on Memorial Day weekend in May 2002.
The third and current coordinator is Peggy Pazos, appointed July 1, 2002. She had been assistant to Mrs. Kenitzer and to Dr. Jones for 5 years and was previously employed by a Baylor ophthalmologist. She is from New Orleans.
Integration of John Peter Smith Hospital into the Baylor residency program
In 1964 residents from Parkland Memorial Hospital were rotating to John Peter Smith Hospital. The affiliation was confirmed in January 1967. However, in a letter from Dr. Robert S. Sparkman to Dr. Winfrey W. Goldman dated August 3,1970, Dr. Sparkman outlined a proposal to rotate residents from BUMC to John Peter Smith Hospital beginning on July 1, 1971. Later that month, Dr. Goldman notified Dr. Tom Shires, chairman of the Department of Surgery at the University of Texas Southwestern Medical School, of the arrangement made between Dr. Charles A. Crenshaw, director of the Department of Surgery at John Peter Smith Hospital, and Dr. Robert S. Sparkman. Dr. Crenshaw was a 1965 graduate of the residency program at Parkland Memorial Hospital. This resulted in withdrawal of residents from the training program from Parkland Memorial Hospital and the eventual dissolution of a separate general surgery residency program at the Veterans Administration Hospital. The University of Texas Southwestern Medical School Department of Surgery began rotating residents to the Veterans Administration Hospital instead of John Peter Smith Hospital in Fort Worth.
Baylor has rotated residents to John Peter Smith Hospital since 1971. In 1987, 5 residents rotated to John Peter Smith Hospital from BUMC. Since that time the number of residents rotating to that hospital has increased, and currently 11 residents rotate to that facility at all times under the supervision of 8 full-time staff. There are 4 general surgery services at John Peter Smith Hospital and 4 general surgery services at BUMC in order to meet the standards set by the Accreditation Council for Graduate Medical Education for an 80 hour work week implemented July 1,2003. Dr. David McReynolds has served as chairman of the Department of Surgery at John Peter Smith Hospital since 2000 (Figure 47). He completed his general surgery training at BUMC in 1979. Prior chiefs of surgery were Dr. Charles Crenshaw, 1965–1992; Dr. Evalea Glanges, 1992–1999; and Dr. Charles Webber, 1999–2000 (acting).
Figure 47.

Dr. David McReynolds, chairman of the Department of Surgery at John Peter Smith Hospital.
John Peter Smith. John Peter Smith helped direct Fort Worth during its growth from an abandoned fort to a progressive town (Figure 48), and John Peter Smith Hospital stands as a memorial to this great man. The City-County Hospital was erected on the present site in 1939 after older facilities at Fourth and Jones Streets were outgrown. The land on which the hospital stands was deeded on October 18, 1877 (100).
Figure 48.

John Peter Smith.
John Peter Smith was born on September 16, 1831, in Owen County, Kentucky, and was orphaned at age 13. Mr. Smith graduated from Bethany College in West Virginia with honors in 1853. He came to Fort Worth in December 1853. In January 1854 he acquired the old Pest Hospital, which was part of the original fort abandoned the year before when the troops moved to Fort Belknap. He taught school and opened Fort Worth's first school. However, after 3 months of teaching, his health became impaired and he closed the school and joined a surveying party west of Fort Worth. After a few years, he returned to Fort Worth and studied law under A.Y. Faler. He was admitted to the Texas Bar in 1860, began his practice in state and federal courts, and soon gained a reputation as one of the best title lawyers in the state. At the beginning of the Civil War, he joined the Confederate Army and served until the war ended. Mr. Smith was present at the recapture of Galveston in 1863 and was wounded twice the same year in conflicts at Donaldsonville and Mansfield, Louisiana. He was promoted to colonel of his regiment in 1864. Mr. Smith resumed law practice after his regiment was disbanded on May 18, 1865.
At the age of 36, on October 16, 1867, he married Mary E. Fox. Although they started with few possessions, by 1881 the Smiths were considered the largest property holders in Fort Worth and Tarrant County. Smith invested $7500 to open Tidball, Van Zandt, and Company Incorporated in 1877 as the Fort Worth National Bank, under which name it operates today. Mr. Smith donated to the city 5 acres of land to be used “when Fort Worth would become a large city and in need of a hospital where the indigent of Fort Worth and Tarrant County could have the best of medical care.” In 1879 and 1880, Smith donated land for Oakwood, Calvary, and Trinity Cemeteries, properties presently combined into the Oakwood Cemetery on Grand Avenue, where Smith himself and many other Fort Worth pioneers are buried. He was mayor of Fort Worth from 1882 to 1885 and under his administration initiated downtown street paving and laid water lines. Smith was a member of the original school board. He again served as mayor in 1890–1891.
In April 1901, while on a city government business trip to St. Louis, Mr. Smith was drugged, attacked, and robbed of $40, the assault leaving him confused and delirious. He had a broken tooth that caused an abrasion on his tongue. The tongue became infected and blood poisoning resulted; his tongue filled his mouth and protruded into his cheeks. A tracheostomy became necessary. The infection had gained too much headway, and respiration became so difficult that he died.
Integration of Presbyterian Hospital of Dallas into the Baylor residency program
On July 1, 2000, Presbyterian Hospital of Dallas became the second hospital to join the residency program, and 4 residents from BUMC rotate to Presbyterian Hospital. Presbyterian Hospital was opened on May 3, 1966, and had a close relationship with the University of Texas Southwestern Medical School. In the 1970s the chief of surgery at the University of Texas Southwestern Medical School was also chief of surgery at Presbyterian Hospital. However, there was a geographic chairman of the Department of Surgery at Presbyterian Hospital, who was Dr. Max Cole. Residents from Southwestern Medical School originally rotated to Presbyterian Hospital in Dallas; however, that rotation ceased in 1976. No surgery residents rotated to Presbyterian Hospital of Dallas from 1976 until July 1, 2000, when the residency at BUMC expanded to Presbyterian Hospital.
Dr. George Thomas Shires III is chief of the Department of Surgery at Presbyterian Hospital, a position he has held since 1997 (Figure 49). Dr. Shires graduated from Duke University School of Medicine and completed his general surgery restdency at Emory University. While at Emory, he served a 2-year fellowship as the Harvey Cushing Fellow in Surgical Research at Cornell University. Following residency at Emory, he served as the Daniel Collier Elkin Research Fellow for 2 years. He joined the faculty at Cornell University in New York, where he remained for 6 years, and then joined the faculty at Southwestern Medical School for 7 years. He was chief of surgery at Zale Lipshy Hospital from 1994 to 1997 before becoming chief at Presbyterian.
Figure 49.

Dr. George Thomas Shires III, chief of the Department of Surgery at Presbyterian Hospital.
Dr. Shires has served on the executive council of the Association for Academic Surgery and as a member of the Shock Society, the Southeastern Surgical Congress, and the Society of University Surgeons. He is also a member of the Society of Surgery of the Alimentary Tract and the Surgical Infection Society. As his first year as chief of surgery at Presbyterian Hospital, he was the James IV traveling scholar.
Continuing education
In 1972 the A. Webb Roberts Center for Continuing Education in the Health Sciences was started. The new educational center comprised the Beulah Porter Beasley Memorial Auditorium completed in 1971 with a $300,000 gift from the late Mrs. Beasley's husband, Dallas insurance man Theodore P. Beasley; a 25,000 Volume medical library; and adjoining lecture rooms for classes and seminars. The $ 1 million endowment necessary to make the center a full time operation was contributed by A. Webb Roberts, a wealthy Dallas banker and real estate developer for whom the center is named. The inaugural program for the center, entitled “Great Ideas in Surgery,” was presented on November 3–4, 1972. It was organized by Dr. Robert S. Sparkman, chief of the Department of Surgery. The program featured 9 speakers, all of whom had made monumental contributions in surgery or their related fields. These internationally known speakers included Drs. Warren Cole, Michael DeBakey, Lester Dragsteadt, John Gibbon, Charles A. Hufnagel (the first surgeon to implant an artificial heart valve), Charles Huggins of Chicago (a Nobel Prize winner), David Hume (noted for organ transplantation), Alton Ochsner of New Orleans' Ochsner Clinic, and Owen Wangensteen, chairman of surgery at the University of Minnesota (101).
Society of Baylor Surgeons
The first reunion of former surgery residents and fellows in the Department of Surgery at BUMC was held on March 19–21, 1981, at BUMC. Officers were elected: Dr. A. B. Small III as president and Dr. Howard C. Derrick III as secretary and treasurer. The second meeting was on April 8–15, 1985, at the South Hampton Princess Hotel in Bermuda. The bylaws and constitution for an organization to be called the Society of Baylor Surgeons (SOBS) were officially approved, and this society formally came into existence. Since then, regular meetings have been scheduled every other year, rotating between BUMC and locations outside Dallas. The presidents of the society following Dr. Small have been Dr. Howard Derrick, 1988–1992; Dr. John Preskitt, 1992–1996; Dr. George Peters, 1996–2000; and Dr. Bruce Smith, 2000–present (Figure 50).
Figure 50.

Dr. Bruce Smith.
The 2000 meeting was held at the Hilton Hotel in San Destin, Florida, with President George Peters presiding. Mary Pat Smith, the wife of current president Dr. Bruce Smith, is administrative director of the society. Several endowments support the society: the Mrs. Charles R. Moore Memorial Endowment, the Schwenkenberg Burrows Memorial Endowment, the Society of Baylor Surgeons Endowment, and a grant in aid from the Helen Buchanan and Stanley Joseph Seeger Endowment.
The Society of Baylor Surgeons has 4 honorary members. Dr. Ronald C. Jones became an honorary member at the May 1988 meeting, Dr. Allan Bookatz at the 1992 meeting, Dr. James Howell (dermatology) at the 1996 meeting (deceased), and Cecil Shelton (deceased).
ENDOWMENT FUNDS
The Department of Surgery Endowment Fund
The original gift for this endowment was made on December 11,1968, by Boone Powell, Sr., and Dr. Robert S. Sparkman. The purpose of the gift is to support all the Department of Surgery educational activities including research, travel, fellowships, and special equipment.
Boone Powell, Sr., Education and Research Endowment Fund
Several funds were established in Boone Powell, Sr.'s honor: an annual seminar on trustee–medical staff–administrative relationships, an annual visiting professorship on hospital management or related subjects, and the establishment of the Boone Powell Health Management Library located on the 17th floor of the A. Webb Roberts Hospital. A fourth fund was established through this endowment for the surgery department. The Dallas board of trustees of BUMC officially approved on August 20, 1970, the proposal that an endowed visiting professorship be established in the Department of Surgery to honor Boone Powell, Sr. This fund was officially established in 1976 with a goal of providing funds for a General Surgery Visiting Professorship. Donations and pledges amounting to $5000 were obtained from BUMC surgeons, another $5000 was obtained from BUMC physicians in other departments, and other donations were solicited. There was an anonymous gift of $50,000 to the general Education and Research Endowment Fund, as well as an unspecified amount given by A. Webb Roberts. On August 27,1982, Mrs. H. L. (Ruth) Hunt gave $50,000 to the endowment fund. In her letter she stated,
As I reflect on the years of service that Boone has rendered to Baylor Hospital, I find myself at a loss for superlatives powerful enough to adequately describe this great man. The fact that Baylor is one of the finest medical centers in the world is a testimony not only to the sanctions and blessings of our Lord, but it is also a tribute to the expertise, loyalty, and untiring efforts of Boone. Perhaps no one in our generation has affected the destiny of more lives than he.
The inaugural program of the endowed Boone Powell Visiting Professorship in the Department of Surgery was entitled “The Blalock Heritage in American Surgery.” Twelve nationally recognized speakers made presentations:
Dr. David C. Sabistin, chairman, Department of Surgery, Duke University
Dr. Mark M. Ravitch, surgeon in chief, Montefiore Hospital, Pittsburgh
Dr. C. Rollins Hanlon, director, American College of Surgeons
Dr. Frank C. Spencer, chairman, Department of Surgery, New York University
Dr. William H. Muller, Jr., chairman, Department of Surgery, University of Virginia
Dr. James V. Maloney, Jr., chief of thoracic surgery, University of California at Los Angeles
Dr. Denton A. Cooley, surgeon in chief, Texas Heart Institute, Houston, Texas
Dr. H. William Scott, Jr., chairman, Department of Surgery, Vanderbilt University
Dr. G. Raney Williams, chairman, Department of Surgery, University of Oklahoma College of Medicine
Dr. J. Alex Haller, Jr., children's surgeon in charge, Johns Hopkins Hospital
Dr. Henry T. Bahnson, chairman, Department of Surgery, University of Pittsburgh
Dr. William P. Longmire, Jr., chairman, Department of Surgery, University of California at Los Angeles
All of these physicians trained under Dr. Alfred Blalock, who in 1941 was appointed director of the Department of Surgery of the Johns Hopkins University School of Medicine.
Boone Powell, Sr., was born in Etowah, Tennessee, on July 15,1912. He attended North Georgia College and the University of Tennessee. In 1935 Boone Powell married Ruth Galloway of Lake City, Tennessee. Mr. Powell began his association with Baylor University Hospital as business manager in 1945 and was named administrator and chief executive officer in 1948 (Figure 51). Under his leadership, BUMC's growth was dramatic, and the medical center now ranks among the largest voluntary general hospitals in the nation both in size and admissions.
Figure 51.

Boone Powell, Sr.
In 1970 Mr. Powell was the recipient of the highest award of the American College of Hospital Administrators, the Gold Medal Award for excellence in hospital administration. The citation presented to Mr. Powell states:
Few institutions have responded so well to the leadership of one man as has the impressive medical center he manages. There, patient care has been administered with exemplary conscientiousness and sensitivity to innovative refinements designed to safeguard life and speed recovery. His profound interest in the value and the importance of teaching has, as one admirer said, “created within his institution an educational atmosphere which has been a hallmark of his professional leadership.”
Mr. Powell served as president of the American College Administrators, president of the Baptist Hospital Association, and president of the Texas Hospital Association.
Cecil Shelton Lectureship
The first lectureship in the Department of Surgery was funded by Cecil Shelton in 1971 under Dr. Sparkman's chairmanship. Mr. Shelton died at age 94 in 2003. Mr. Shelton's daughter, Jody, is married to Dr. Pick Scruggs, the chief of radiation oncology.
Charles and Elizabeth Prothro Visiting Professorship in the Department of Surgery
Mr. and Mrs. Charles Prothro of Wichita Falls, Texas, established the Charles and Elizabeth Prothro Visiting Professorship in the Department of Surgery. Mr. Prothro (Figure 52) had been a patient of a BUMC surgeon (Dr. William David Barnett) in 1972. The Prothros had been very generous with gifts to BUMC previously, including donation of a linear accelerator.
Figure 52.
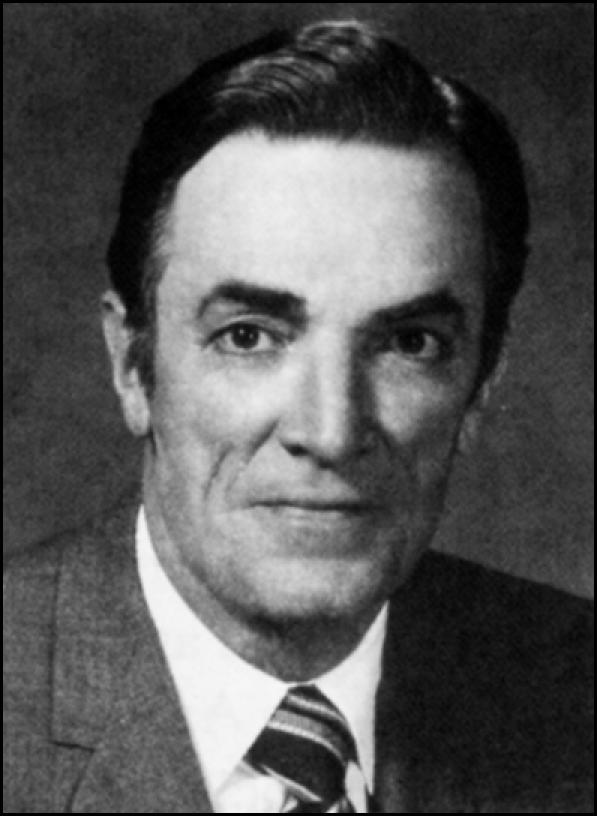
Mr. Charles Prothro.
Mr. Prothro married Elizabeth Perkins. At Southern Methodist University, the Perkins family made a significant gift toward building the Perkins School of Theology, the Perkins Chapel, and the Perkins Administration Building. The Perkins School of Theology was named for the parents of Elizabeth Perkins, Joe and Lois Perkins, in 1946.
The original gift for the Charles and Elizabeth Prothro Fund was in the amount of $10,000 in December 1972. Since the initial funding, the Prothro family has donated several times to the Department of Surgery, and the fund has grown to almost $300,000. The visiting professorship was instituted in 1974. The purpose of the Charles and Elizabeth Prothro Fund was to support the educational activities of the Department of Surgery, including periodic named lectures honoring Charles and Elizabeth Prothro.
The inaugural program for the Prothro Visiting Professorship was held on September 14, 1974, and was entitled “Osler, Halsted, and Welch.” Numerous national and international leaders in surgery have delivered this lectureship. Mr. Prothro served as chairman of the board of trustees of the Baylor Health Care System Foundation in 1981–1982. He died on March 5, 2001, in Wichita Falls, Texas, at age 83 years.
Visiting professorship in vascular surgery
In June 1978 an agreement was made between Dr. C. Gene Wheeler and BUMC to establish a visiting professorship in vascular surgery through the Department of Surgery and the A. Webb Roberts Center for Continuing Education. Dr. Wheeler trained at Massachusetts General Hospital in Boston and then practiced at BUMC. He left Dallas to become chief of vascular surgery at the Veterans Affairs Hospital in Phoenix, Arizona. The inaugural speaker on October 10, 1979, was Dr. Edwin J. Wylie, professor of surgery and chief of vascular surgery at the University of California at San Francisco.
The Mrs. Charles R. Moore Memorial Lectureship
This endowment was established by Mrs. Moore's daughter and son-in-law, Mr. and Mrs. Marion B. Solomon, their sons Charles and Bill Solomon, and Austin Industries of Dallas. Mrs. Moore (Sarah Cammack) (Figure 53) was born on June 17, 1878, and died on February 18, 1971. The first of the donations was received in January 1972 and the last in 1976. Charles R. Moore served on the hospital's board of trustees for 39 years, longer than anyone else in its history except Dr. G. W. Truett. Dr. Moore served as chairman of the board of trustees from 1943 to 1954. The sixth floor of the Truett Hospital, which opened in November 1950, was dedicated in memory of Austin Moore (son of Mr. and Mrs. Moore), who died in 1944.
Figure 53.

Mrs. Charles Moore.
The first visiting professor and guest lecturer was Dr. William J. Fry; he spoke shortly after his arrival at the University of Texas Southwestern Medical School as the new department chairman in 1976. Dr. Charles McLaughlin, a former president of the American College of Surgeons, delivered the lecture in 1977, and Professor Philip Sandblom, formerly head of the Department of Surgery of Lund in Sweden and an honorary fellow of the American College of Surgeons, the American Surgical Association, and the Southern Surgical Association, delivered the lecture in 1978. The lectures have subsequently been held in conjunction with meetings of the Society of Baylor Surgeons.
The Frank H. Kidd, Jr., Visiting Professorship and Endowment Fund
Dr. Frank H. Kidd, Jr., endowed two funds in the Department of Surgery, a lectureship and an endowment fund. The professorship was established in 1974 by a generous donation from Dr. Kidd. The endowment established a lectureship in the Department of Surgery, and at his death, money was contributed to establish a lectureship in general surgery at Presbyterian Hospital of Dallas. As such, the lectureship rotates every other year between these two hospitals. The inaugural program of the Kidd Visiting Professorship was given by Dr. Oliver H. Beahrs, head of the Section of General Surgery at the Mayo Clinic in Rochester, Minnesota.
The endowment fund supports various educational activities of the surgery department. When Dr. Kidd was interviewed 15 years after establishing the endowment, he commented, “I am at the point that I have something to leave behind as a surgical legacy. I cannot think of a better way to benefit the young men in surgery who follow me.” The general surgery endowment fund has been used to support resident education and resident travel in the department.
Dr. Kidd (Figure 54) was born on February 11, 1909, in Burnsville, West Virginia. He graduated from Southern Methodist University in 1931 and Baylor University College of Medicine in 1937. His residency was completed in St. Louis at Barnes Hospital, St. Louis City Hospital, and Barnard Free Skin and Cancer Hospital. Dr. Kidd was a governor of the American College of Surgeons in 1956–1958 and president of the BUMC medical staff in 1967. He was also active in hospital fundraising: he chaired the professional division fund drive for the construction of the Women's and Children's Hospital in 1957 and the Jonsson Hospital in 1967. Dr. Kidd died on February 8, 1988.
Figure 54.

Dr. Frank H. Kidd, Jr.
Surgical Oncology Endowment
The Surgical Oncology Endowment Fund was established by Dr. Z. H. Lieberman and Dr. John C. O'Brien (Figure 55) on May 19,1978. The purpose of the endowment is to provide for the development and enhancement of educational programs in surgical oncology. The endowment is now used to fund an annual citywide head and neck surgery visiting professorship.
Figure 55.

Dr. John C. O'Brien.
Breast Cancer Education and Research Endowment Fund
This fund was established in April 1974 primarily to support the cost of an annual visiting professor for breast cancer. Dr. J. Harold Cheek has been largely responsible for the development of this endowment fund. The principal donors who initiated the fund were Dr. Cheek and Kelly McCann.
Throughout this century, the care of the patient with breast disease has been an important part of the surgery department of BUMC. The importance and prominence of breast cancer has been elevated due to the significant increase in the incidence of the disease since 1950.
In the 1940s and before, due to the efforts of the American Cancer Society, surgeons, pathologists, and the public became more aware of the importance of early diagnosis and treatment of breast cancer. Noteworthy in this period were C. D. Haagensen and Arthur P. Stout, who had a worldwide influence. Through the 1940s and 1950s, the referral of care to Baylor rapidly increased and the opportunity to study all aspects of the treatment of breast cancer increased, benefiting the training of those in our residency program.
Dr. Walton Cochran was most influential, encouraging some of his residents, especially Dr. Cheek, to consider limiting their practices to treatment of those with cancer and some specifically to breast diseases, as the need was apparent.
An annual breast cancer lectureship was made possible with support of friends and patients of our physicians and was developed with the cooperation of the various department chiefs and administration. The Breast Cancer Education and Research Endowment Fund was one of the first lectureships started by a contribution of a friend, patient, and trustee of Baylor, Kelly McCann. The endowment was activated in early 1975, and the inaugural breast lectureship was presented by Dr. C. D. Haagensen on March 31, 1976.
Helen Buchanan and Stanley Joseph Seeger Endowment Funds
Four funds were established by Mr. and Mrs. Wirt Davis in honor of her parents, Helen Buchanan and Stanley Joseph Seeger (Figure 56). Dr. Seeger was a practicing surgeon in Milwaukee, Wisconsin, for approximately 25 years but found it necessary to retire from practice to manage the family businesses. Dr. Seeger resided in Texarkana and in Dallas at different stages of his career. Four gifts were made within a 12-month period, beginning in November 1979. The four gifts were designated for the following purposes:
Figure 56.

Dr. Stanley Joseph Seeger.
Endowment for a Fellowship in Breast Oncology, $500,000
Endowment for the Department of (General) Surgery, $500,000
Endowment for the Surgical Specialties, $500,000
Endowment for a Chair in General Surgery, $1,000,000 Thus, endowment gifts totaling $2.5 million dollars were made to BUMC, and they were established on August 15, 1980. The purpose of the gifts was to make it possible for members of the medical staff in the Department of Surgery to improve their skills in the care of patients, to encourage and support clinical research, and to enhance their own educational programs and their effectiveness in the instruction of residents, fellows, medical students, and allied health personnel.
In December 1983, Mr. and Mrs. Wirt Davis made a fifth donation in the amount of $600,000 to BUMC as an endowment for the Department of Surgery. Its title is the Helen Buchanan and Stanley Joseph Seeger Endowment for the Enhancement of Surgical Services. The check was dated December 2, 1983, and signed by Hannah Seeger Davis.
Later, $1.4 million was added to these existing endowments, and approximately $900,000 was given to establish the Hannah Seeger Davis Endowment for Surgical Educators to encourage young surgeons to become teaching physicians.
An advisory committee was created to oversee the use of the endowment income from each of these funds. Dr. Allan Bookatz chaired the committee for the Seeger Endowment for the Department of (General) Surgery. Dr. J. Harold Cheek chaired the committee for the Seeger Endowment for a Fellowship in Breast Oncology. Dr. Donald Paulson chaired the committee for the Seeger Endowment for Surgical Specialties; he was followed by Dr. Carl Henry and Dr. Fred Owens. The committee for the Seeger Endowment for the Enhancement of Surgical Services is always chaired by the chairman of the Department of Surgery; thus, Dr. Jesse Thompson and then Dr. Ronald Jones served as chair.
The fellowship in surgical oncology of the breast began in 1982, and to date 19 physicians have completed it (Table 3). These physicians now limit their practice to breast oncology and are located throughout the USA.
Table 3.
Fellows in breast surgery at BUMC, 1982–2003
| Year | Fellow |
| 1982–1983 | Robert Krupkin |
| 1983–1984 | Janet Hale |
| 1984–1985 | Phyllis Hochberg |
| 1985–1986 | Sally Moot Knox |
| 1986–1987 | Richard Clarfeld |
| 1987–1988 | Thomas Schmidt |
| 1989–1990 | Theodore Tsangaris |
| 1990–1991 | James Hagans III |
| 1992–1993 | Michael Cross |
| Michael Grant | |
| 1993–1994 | David Hampe |
| Richard Katseres | |
| 1994–1995 | Dana Abraham |
| Terre Quinn | |
| 1995–1996 | Jennifer Sabol |
| 1997–1998 | Rachel Dultz |
| 1999–2000 | Kinga Styperek |
| 2001–2002 | Jeri Fant |
| 2002–2003 | Shawn McKinney |
Seeger Chair
The Helen Buchanan and Stanley Joseph Seeger Endowed Chair in Surgery was established to attract a distinguished surgeon to the Department of Surgery to build upon its already considerable strengths and to extend its future potential for excellence in clinical research, medical education, and patient care. The Seeger Chair in Surgery is accountable to the chief of surgery. The functions of the chair are to direct and coordinate surgical research activities, to assume a strong role in surgical education, and to support, through clinical proficiencies, the maintenance of high-quality surgical care in the department. The Seeger Chair in Surgery coordinates clinical research, assists in residency education, maintains a high profile within the university environment and the specialty by contributions to the surgical literature, and when possible maintains a close working relationship with the University of Texas Southwestern Medical Center at Dallas, establishing joint programs of mutual benefit to the two institutions.
Dr. J. Patrick O'Leary (Figure 57) was the first surgeon designated the Seeger Chair in Surgery. Dr. O'Leary was born on June 20, 1941, in New York. He obtained his medical degree from the University of Florida in Gainesville in 1967 and completed his residency at the same institution, where he later became assistant professor of surgery. In 1978 Dr. O'Leary moved to Nashville, Tennessee, as professor of surgery at Vanderbilt University School of Medicine. He was chief of the surgical service at the Veterans Administration Hospital in Nashville from 1978 to 1984, when he was appointed Seeger Professor of Surgery at BUMC. In 1985 he was given the title of program director of the surgical residency program. On June 30, 1989, he became chairman of the Department of Surgery at Louisiana State University in New Orleans.
Figure 57.

Dr. Patrick O'Leary.
Allan and Selma Bookatz Lectureship in Surgery and Anesthesia
Dr. Allan Bookatz was born in Philadelphia, the son of Barnett and Anna Bookatz. He grew up in Cleveland, Ohio, and graduated magna cum laude from Miami University, Oxford, Ohio, where he was a Phi Beta Kappa. His medical degree was from Case Western Reserve University in 1936. Dr. Bookatz completed his internship and an additional 5 years of residency in surgery at Mount Sinai Medical Center in Cleveland.
In 1942 he joined the US Navy in Seattle, Washington, as a lieutenant. He then joined Kaiser Permanente Hospital in Vancouver, Washington, in 1943, where he remained until 1946, when he returned to Cleveland, Ohio, and entered private practice. Dr. Bookatz remained in private practice in Cleveland for 2½ years and was on the teaching staff at Mount Sinai Hospital.
Dr. Bookatz married Selma Kirschner in 1947 (Figure 58). In 1948 they moved to Dallas, where he started private practice at BUMC. Dr. Bookatz has served on the Baylor Health Care System Foundation board of trustees and now serves as director emeritus of the board. In 1996 Anna Kirschner endowed the annual Allan Bookatz, MD, Lectureship in Surgery and Anesthesia. Mrs. Kirschner was married to Herman N. Kirschner and lived in Dallas. The lectureship will have topics of discussion of mutual interest to surgeons and anesthesiologists.
Figure 58.

Dr. and Mrs. Allan Bookatz.
DIVISIONS OF THE DEPARTMENT OF SURGERY AND OTHER SURGICAL DEPARTMENTS
Division of Trauma
Dr. Michael Foreman, director of the Division of Trauma, graduated from the University of Texas at San Antonio and did his general surgery residency at BUMC (Figure 59). He completed his general surgery training in 1987 and took it upon himself to specialize in management of the severely injured patient. Eventually in February 1994, a Division of Trauma was established, and Dr. Foreman has since recruited 3 other trauma surgeons who now have rotations in the hospital 24 hours a day, 7 days a week to support the requirements of a level I trauma center, which Baylor has attained as of February 1999. There are only 9 level I trauma centers in Texas. Approximately 20% to 25 % of all major trauma in the city of Dallas is managed at BUMC, and many patients are referred to BUMC from outside Dallas County.
Figure 59.

Dr. Michael Foreman.
Division of Pediatric Surgery
Dr. Dale Coln moved to BUMC as a pediatric surgeon in 1987 (Figure 60). That same year, pediatric surgery was made a division within the Department of Surgery, and Dr. Coln is director of the division. Dr. Coln graduated from Baylor College of Medicine in 1961. He married Shirley Kindberg, MD, on May 12, 1962. Dr. Coln, who trained at Parkland Memorial Hospital and did a pediatric surgery fellowship at Cape Town, South Africa, returned to the USA to join the staff at the University of Texas Southwestern Medical School, where he remained for 17 years. He did additional training at Los Angeles Children's Hospital during this time. He served as president of the Texas Pediatric Surgery Society in 2001.
Figure 60.

Dr. Dale Coln.
Division of Vascular Surgery
The Division of Vascular Surgery was started by Dr. Dale Austin and Dr. Jesse Thompson in the 1950s. When Dr. Thompson retired, Dr. Clement “Mack” Talkington was appointed director of the division for 10 years until April 1996. Dr. Greg Pearl was appointed director of the Division of Vascular Surgery in April 1996 and continues in that position.
Dr. Pearl was born in Peoria, Illinois, and graduated from college at the University of Notre Dame (Figure 61). He graduated from Tulane University Medical School in 1980 and did his general surgery residency at Northwestern University Memorial Hospital in Chicago. His peripheral vascular fellowship was with Dr. Jesse E. Thompson. Dr. Pearl then joined the staff at BUMC in 1987. As director of vascular surgery, Dr. Pearl is responsible for training two vascular fellows annually. He married Allison Muller of New Orleans, Louisiana, in 1988.
Figure 61.

Dr. Greg Pearl.
Division of Transplant Surgery
Dr. Göran Klintmalm, the director of transplant surgery, came to BUMC in 1984, having worked with Dr. Thomas Starzl at Denver, Colorado, and at Pittsburgh, Pennsylvania (Figure 62). Dr. Starzl came to BUMC to assist with the first liver transplant performed by Dr. Klintmalm on December 21, 1984. A separate article is dedicated to transplant surgery (102).
Figure 62.

Dr. Göran Klintmalm.
Transplant review committee and cardiac transplantation
A transplant review committee was formed in 1984 to oversee the transplant programs at BUMC, which eventually included liver, kidney, bone marrow, heart, lung, small bowel, and pancreas. The chief of surgery was designated chairman of the committee; Dr. Jesse Thompson served from 1984 to 1986, and Dr. Ronald C. Jones from 1987 to the present.
On May 7, 1985, the transplant review committee established guidelines for the cardiac transplant program. A director and codirector of cardiac transplantation were appointed and have responsibility for the program. The chief of thoracic and cardiovascular surgery, in consultation with the chief of surgery, made recommendations to the transplant review committee for appointment of heart transplant physicians. The director and codirector of the cardiac transplant program were jointly accountable to the chief of cardiothoracic surgery and the chief of surgery and function within the guidelines established by the transplant review committee. It was also established that only one cardiac transplant team would perform transplants at BUMC. The transplant surgeons would be members of private practice groups, and it was not recommended that a hospital-based physician be recruited to direct the cardiac transplant team.
The first director, Dr. Peter Alivizatos, and codirector, Dr. Ivan Crosby, were appointed on May 22, 1985. Dr. Crosby left BUMC approximately 1 year later, and Dr. Alivizatos was the director of the cardiac and lung transplant program. By August 1991, 100 cardiac transplants had been performed. In May 1995 Dr. Alivizatos informed the committee that he was spending approximately half of his time developing a cardiac transplant program at the Onassis Hospital in Athens, Greece. Over the next several months, an agreement was made between Dr. Alivizatos and Dr. Steves Ring at the University of Texas Southwestern Medical School for Dr. Ring to assume the directorship of programs at St. Paul Hospital and BUMC. Under Dr. Alivizatos' directorship, the heart/lung transplant program had progressed very well. Dr. Alivizatos became chief of surgery at the Onassis Hospital in Athens in 1996. Dr. Alivizatos' father had also been professor of surgery at the Onassis Hospital. In July 1996, Dr. Steves Ring replaced Dr. Alivizatos.
Department of Colon and Rectal Surgery
Dr. Curtice Rosser, son of Dr. Charles M. Rosser, was the first physician in Dallas to specialize in proctology, or colon and rectal surgery. In 1947 he was chief of colon and rectal surgery at Baylor and established a residency program. Other chairman of colon and rectal surgery include Dr. Alvin Baldwin, 1961–1970; Dr. Wallace Bailey, 1970–1990; Dr. R. D. Dignan, 1991–2000; and Dr. Warren Lichliter, 2001–present.
Dr. Warren Lichliter completed his medical school training at the University of Texas Medical Branch in Galveston in 1978 and did his general surgery residency at BUMC under Dr. Robert Sparkman (Figure 63). Dr. Lichliter then did a colon and rectal fellowship at BUMC under Dr. Wallace Bailey. He married Carol Loftin on November 3,1979. Dr. Lichliter served as president of the medical staff in 1997 and chairman of the medical board in 1998. In 2003 he became president of the Dallas County Medical Society.
Figure 63.

Dr. Warren Lichliter.
Department of Neurological Surgery
Dr. Albert P. D'Errico came to Baylor in 1932 from University Hospital in New Haven, Connecticut, as Dallas' first neurosurgeon (Figure 64). Prior to that, all neurosurgical procedures had been performed by general surgeons at Baylor Hospital. Dr. D'Errico received his medical degree from Case Western Reserve University Medical School in his hometown of Cleveland. He noted that the aseptic technique at Baylor was lacking. In the early 1930s, examination of the spinal column was done by injecting “Lipiodol,” an opaque oil. Ventriculograms were used in the 1930s to detect brain tumors. This procedure involved withdrawing spinal fluid and injecting air so that the ventricles could be outlined. This was replaced by Pantopaque in the 1940s. In the 1940s electroencephalography became available as a diagnostic tool. In the 1950s brain scanning was introduced utilizing radionuclides. During his 43 years of practice at Baylor, Dr. D'Errico operated on more than 1000 brain tumors. Twenty-five percent of these were glioblastoma multiforme.
Figure 64.

Dr. Albert P. D'Errico.
Until the mid 1940s, Dr. D'Errico was the only neurosurgeon practicing at Baylor, but by the early 1950s there were 5 neurosurgeons on staff.
In 1965, Dr. D'Errico retired as chief of neurosurgery, and Dr. Charles M. Wilson assumed the position. Dr. Wilson was a graduate of Tulane Medical School and did his neurosurgery residency at the University of Michigan. He had joined Dr. D'Errico in practice 5 years earlier. From 1980 to 1990, Dr. R. Gordon Long was head of neurosurgery. Dr. John V. Coon was chief in 1991 to 1993 and was appointed again in 1996 (Figure 65).
Figure 65.

Dr. John V. Coon.
Department of Plastic and Reconstructive Surgery
The first plastic surgeon in Dallas was Dr. James Theodore “Ted” Mills, who came to Dallas in 1932 after receiving his medical degree from the University of Minnesota and completing his plastic surgery training in Grand Rapids, Michigan (Figure 66). He was a founding member of the American Board of Plastic Surgery in 1934 and served as its president in 1948. He also was president of the American Society of Plastic and Reconstructive Surgeons in 1952–1953. He became associate editor of Plastic and Reconstructive Surgery and was appointed the first chairman of the Division of Plastic Surgery at Southwestern Medical School in the 1960s. Dr. Fritz Barton and Dr. Steve Byrd have followed Dr. Mills as chairman. Dr. Byron Brown has twice served as chairman of the department and remains the chairman (Figure 67).
Figure 66.

Dr. James T. Mills.
Figure 67.

Dr. Byron Brown.
Other surgical departments
Other surgical departments inelude ophthalmology (103), otolaryngology (104), orthopaedic surgery (105), thoracic and cardiovascular surgery (106), urology (107), and oral and maxillofacial surgery (108). Those histories have been previously published.
In addition, the Baylor Charles A. Sammons Cancer Center has a division of surgical oncology, which was first headed by Dr. Billie Aronoff (109). Charles A. Sammons was the largest single contributor in the medical center's history.
SURGICAL PROCEDURES
Gallstone lithotripsy
On January 27, 1988, the first gallstone lithotripsy procedure in the USA was successfully performed at BUMC as part of a US Food and Drug Administration—approved study. Dr. David Vanderpool, a general surgeon, performed the 1½-hour procedure on a 37-year-old South Carolina woman. She was observed in the hospital for 48 hours and at the time of discharge was free of her gallstones. The new Medstone Lithotripsy device used focused shock waves to pulverize gallstones into small fragments that can then be dissolved in the gallbladder with Actigal or passed through the bile duct. An ultrasound machine was used to locate the stones, and a computer pinpointed them. The principal investigators were Dr. David Vanderpool, Dr. Ronald C. Jones (chief of surgery), Dr. Kent Hamilton (gastroenterologist), and Dr. Patrick O'Leary (Seeger Professor of Surgery). This new procedure resulted in calls from US and international patients who knew they had gallstones but were fearful of an open surgical procedure. Unfortunately after the investigation period was concluded, only about 50% of patients who had noncalcified gallstones 1 cm or less were freed of their stones. As a result, the procedure fell into disfavor partly because of the long-term results and partly because laparoscopic cholecystectomy became available. Nevertheless, BUMC received tremendous recognition throughout the country in the newspapers and television media. The machine cost approximately $1 million; however, it was estimated that BUMC received $475,000 in media coverage as a result of the first procedure. The machine was ultimately sold to be placed on a truck as a portable lithotripsy machine for the treatment of kidney stones, for which it was much more successful.
Laparoscopic surgery
The first laparoscopic cholecystectomy in the world was performed by Mouret in 1987 in France. Dr. Jones traveled to US Surgical headquarters in Norfolk, Connecticut, in April 1990 to take a laparoscopic cholecystectomy course. While there, he met Dr. Douglas Olsen of Nashville, Tennessee. He got Dr. Olsen to give a course for the general surgeons at Baylor. Dr. Howard Derrick assisted by Dr. John Preskitt performed the first laparoscopic cho-lecystectomy at BUMC on June 6, 1990, on a 45 year-old woman. The procedure took 2 hours and 45 minutes, and the patient was hospitalized for 3 days. The second laparoscopic cholecystectomy was performed the following day by Dr. Preskitt assisted by Dr. John Anderson and Dr. Bruce Smith. Within the first 10 months, 300 laparoscopic cholecystectomies were performed. As surgeon experience increased, the length of the operative procedure decreased to less than 1 hour, and now patients go home the same day.
Dr. Derrick (Figure 68) continued to lead the surgeons at Baylor in laparoscopic surgery, performing the first laparoscopic gastrostomy. In the spring of 2000, Drs. Derrick and Matthew Westmoreland performed the first laparoscopic donor nephrectomy at BUMC. The first laparoscopic hiatal hernia was repaired by Dr. Vanderpool on December 13,1994. Dr. Westmoreland also pioneered with Dr. David Vanderpool laparoscopic hiatal hernia repair. Dr. Derrick has served as president of the medical staff and currently is chairman of the medical board.
Figure 68.

Dr. Howard Derrick.
Robotic surgery
On June 7, 2000, the Baylor Health Care System Foundation purchased an intuitive computer-assisted robot, which was placed in the Caruth animal facility. The major donors were the Hillcrest Foundation, founded by Mrs. W. W Caruth, Sr., and Moss-Heart Trust. The Baylor thoracic surgeons trained at various places in Europe and the USA and entered into a Food and Drug Administration—approved project with 6 other institutions in the USA. The device has 3-dimensional visualization, whereas laparoscopic equipment is only 2-dimensional. On June 2, 2001, the first patient was treated using a computer-assisted robotic device by Dr. Baron Hamman and assisted by Dr. Richard Wood to harvest the internal mammary artery in preparation for coronary artery bypass.
Subsequently, Dr. Howard Derrick performed the first cholecystectomy using the robotic machine on April 18, 2001. Its use in general surgery and cardiothoracic surgery remains to be determined.
RETIRED HONORARY STAFF
Dr. Billie L. Aronoff
Dr. Billie Lewis Aronoff (Figure 69) was born on May 28, 1914, in Dallas, Texas. He did his undergraduate premedical training at the University of Chicago and Southern Methodist University and graduated Alpha Omega Alpha from Baylor University College of Medicine in 1938. Subsequently, he completed his general surgery residency at Parkland Memorial Hospital and did postgraduate training at Memorial Hospital in New York, Lahey Clinic, and Ochsner Clinic. He then entered the practice of surgical oncology at BUMC. Dr. Aronoff served in World War II and returned to Baylor in 1945. He married Valerie Rosenthal in 1942.
Figure 69.

Dr. Billie L. Aronoff.
Dr. Aronoff was active with the American Cancer Society: he was president of the Dallas County Unit, president of the Texas Division, on the national board of directors, and a recipient of its Volunteer of the Year Award. He also served on the Commission on Cancer of the American College of Surgeons and on the executive committee of the Society of Surgical Oncology. Dr. Aronoff was the first surgeon in Dallas to perform laser surgery in 1974. In 1981 he became president of the International Society for Laser Surgery. He published extensively regarding the use of the laser and managing the patient with malignancy. Dr. Aronoff was editor of Lasers in Surgery and Medicine and on the editorial board of Oncology Times and Seminars in Surgical Oncology. He lectured nationally and internationally. Dr. Aronoff is credited with keeping a major portion of head and neck surgery within the Department of Surgery. He retired in 1991 after 50 years of practice at BUMC and became an honorary member of the department in January 1992. He lives in Dallas with his wife, Valerie.
Dr. J. Harold Cheek
Dr. J. Harold Cheek (Figure 70) was born in El Dorado, Oklahoma, in 1917. He graduated from Texas Technological College in Lubbock, Texas, in 1941. Dr. Cheek entered Baylor University College of Medicine in Dallas in 1940; since the medical school moved to Houston in 1943, he finished medical school at Southwestern Medical College in December 1944. Dr. Cheek recalled during medical school that Hall Street, where Roberts Hospital is located today, was called College Avenue and both the medical school and dental school were on Hall Street. The Phi Chi house was near where Baylor Institute for Rehabilitation is today. During Dr. Cheek's junior and senior years of medical school, after Baylor moved to Houston, no classrooms were available for the Southwestern Medical College. Spence Junior High School, between Baylor Hospital and North Central Expressway near Fitzhugh, rented classrooms to the new medical school. In 1944 Dr. Cheek began an internship at Baylor University Hospital, and Dr. Sam Weaver was the acting chief of surgery, who was soon followed by Dr. Walton Cochran in 1946.
Figure 70.

Dr. J. Harold Cheek.
Dr. Cheek met Anna Lou Cave, a student nurse. She went to work for Dr. Albert D'Errico, a neurosurgeon, and eventually became Dr. D'Errico's full-time scrub nurse. Dr. Cheek married Miss Cave in August 1946. When Dr. Cheek was a senior resident, the Truett Hospital opened, and he performed the first operation in the Truett operating room. After serving 2 years in the army, Dr. Cheek returned to Baylor University Hospital and entered the private practice of surgery in 1951.
In 1974 Dr. Cheek was the first general surgeon in Dallas to limit his practice to diseases of the breast. He continued to operate for another 20+ years and retired from the practice of surgery in 1995. During that time he started a fellowship in breast oncology, and 19 breast oncologists have finished this 1 -year fellowship. He received many honors, including serving as president of the Texas Division of the American Cancer Society in 1977. He received the Sword of Hope Award from the American Cancer Society in 1970, the Certificate of Merit Award from the American Cancer Society in 1972, the Taittinger Award of Distinction from the Susan G. Komen Foundation in 1985, and the Wings of Eagles Award from Baylor Health Care System Foundation in 1999. Dr. Cheek served as vice chairman of the Department of Surgery from 1987 to 1991.
Dr. Cheek developed the lectureship now named in his honor, the J. Harold Cheek Annual Breast Lectureship. The first person to deliver the lectureship was Dr. Cushman Haagensen of New York City in 1976. The initial funding for the lectureship came from Kelly McCann.
Dr. Cheek currently lives near Tyler, Texas. He is greatly admired by his patients and by all the physicians at BUMC. He continues to be active on many committees, including the surgical advisory committee, the Baylor Health Care System Foundation board, and the executive committee of the Sammons Cancer Center (110).
Dr. David Barnett
Dr. David Barnett (Figure 71) practiced general and colorectal surgery at BUMC for 38 years. He was born in Thornton, Texas, on January 24, 1928, and completed his undergraduate studies at Texas A&M University. Dr. Barnett married Betty Pierce. He graduated from the University of Texas Medical Branch in Galveston, Texas, in 1952 and completed a general surgery residency at Parkland Memorial Hospital in 1959. This was followed by a colon and rectal fellowship with Dr. R. J. Rowe. Dr. Barnett was president of the North Texas Chapter of the American College of Surgeons in 1977, president of the Texas Surgical Society in 1981–1982, president of the Dallas Society of General Surgeons in 1986, and president of the Texas Society of Colon and Rectal Surgery in 1986. He served as treasurer of the Western Surgical Association from 1988 to 1992 and is a member of the Southern Surgical Association. Dr. Barnett retired from active practice in 1997 and resides in Dallas, Texas.
Figure 71.

Dr. David Barnett.
ACTIVE STAFF
The active staff has continued the tradition of excellence of early Baylor surgeons. Six of the founding members of Baylor University College of Medicine had been elected president of the Texas Medical Association, and they were followed by others on the Baylor medical staff (Table 4) In addition, many presidents of the Texas Surgical Society (founded in 1915) have been members of the BUMC medical staff (Table 5).
Table 4.
Baylor surgeons elected president of the Texas Medical Association
| Year | President from Baylor | Year | President from Baylor |
| 1900 | B. E. Hadra | 1922 | Joe Becton |
| 1905 | J. E. Gilcreest | 1925 | C. M. Rosser |
| 1916 | J. M. Inge | 1937 | Calvin R. Hannah |
| 1917 | E. H. Cary | 1987 | David Vanderpool |
Table 5.
Baylor surgeons elected president of the Texas Surgical Society*
| Year | President from Baylor | Year | President from Baylor |
| 1917 | Bacon Saunders | 1955 | C. B. Carter |
| 1925 | H. M. Doolittle | 1963 | J. Warner Ducket |
| 1926 | A. B. Small | 1965 | Robert S. Sparkman |
| 1931 | Joe Becton | 1972 | Jesse E. Thompson |
| 1934 | A. I. Folsom | 1982 | William David Barnett |
| 1936 | C. W. Flynn | 1994 | Harold C. Urschel, Jr. |
| 1938 | Elbert Dunlap | 2001 | David Vanderpool |
| 1945 | Sam D. Weaver |
*From Sparkman RS, Nixon PI, Crosthwait RW, King WB Jr, White RJ. The Texas Surgical Society: The First Fifty Years. Dallas: The Texas Surgical Society, 1965.
Dr. David Vanderpool
Dr. Brice David Vanderpool (Figure 72) was born in Dallas, Texas, and obtained his medical degree from the University of Texas Southwestern Medical School. He completed a general surgery residency at Parkland Memortal Hospital and after serving 2 years in the US Air Force joined the staff at BUMC. He has served as president of the Dallas County Medical Society, the Texas Medical Association, and the Texas Surgical Society and as governor of the American College of Surgeons. In addition, he has served as president of the American Society of General Surgery; he has been an advocate for the general surgeon. Dr. Vanderpool was a pioneer in developing the technique for laparoscopic hiatal hernia repair at BUMC. He continues an active private practice with Dr. Matthew Westmoreland and Dr. David Arnold.
Figure 72.

Dr. David Vanderpool.
Dr. John Preskitt
Dr. John Preskitt (Figure 73) was a 1975 graduate of the University of Texas Southwestern Medical School and did his general surgery training at BUMC. He subsequently performed a 1-year surgical oncology fellowship at M. D. Anderson Hospital in Houston and returned in solo practice to BUMC. Later he joined Dr. Zelig Lieberman's group. He married Rebecca Black. Dr. Preskitt became the third director of surgical oncology at Sammons Cancer Center in 2001.He has served as president of the North Texas chapter of the American College of Surgeons,as well as governor of the college and chairman of the committee on chapter activities.Dr.Preskitt was elected a regent of the American College of Surgeons in 2001,an honor given to very few surgeons in Dallas and no other surgeons who ever practiced full-time at BUMC.
Figure 73.

Dr. John Preskitt.
Dr. Zelig Lieberman
Dr. Zelig Lieberman (Figure 74) graduated from Tulane University in 1950. He did his general surgery residency at Barnes Hospital in St. Louis and did a surgical oncology fellowship at that institution in association with Ellis Fischel State Cancer Hospital. Dr. Lieberman came to Dallas to practice medicine in 1957. He followed Dr. Aronoff as the second director of surgical oncology and remained in that position until 2000. Dr. Lieberman soon formed his own group to include Drs. John O'Brien, Howard Derrick, John Preskitt, and Stacy Stratmann. When Dr. O'Brien left the group, Dr. Jeffrey Stephens, who had trained at BUMC and had done a surgical oncology fellowship at Roswell Park Hospital in Buffalo, New York, joined the group. Dr. Lieberman has served as vice chairman of the Department of Surgery since February 1991. He was one of three physicians to be elected to the board of trustees at BUMC in 1999. The Lieberman Research Building stands in Dr. Lieberman's honor, and his portrait hangs in the lobby. He is married to Marilyn Ely and remains active in the practice of surgical oncology.
Figure 74.

Dr. Zelig Lieberman.
Dr. John Anderson
Dr. John Anderson (Figure 75) is a general surgeon who trained at BUMC under Dr. Robert Sparkman. He is married to Rachel Presley, the daughter of Dewey Presley, who was chairman of the Baylor-in-Dallas board of trustees. Dr. Anderson completed a vascular surgery fellowship at the University of Tennessee Health Science Center in Memphis and returned to practice vascular surgery at BUMC. On July 1, 1995, he became senior vice president for clinical integration and has since become a leader in administration of BUMC. He is a strong supporter of physicians and surgeons and of graduate medical education.
Figure 75.

Dr.John Anderson.
Dr. Joseph Kuhn
Dr. Joseph Kuhn (Figure 76) is one of the associate program directors, having been an Alpha Omega Alpha graduate of the University of Texas Medical Branch in Galveston in 1984. He came to BUMC to complete his general surgery residency under Dr. Jesse Thompson and Dr. Ronald Jones. He went to City of Hope Hospital in Los Angeles, California, for a 3-year surgical oncology fellowship and returned to BUMC in solo practice in 1992. He is in charge of clinical research for the residents at Baylor. Dr. Kuhn was joined in practice by Dr. Todd McCarty in January 1998. Dr. Jeffrey Lamont, who completed his general surgery residency at Baylor and also completed a surgical oncology fellowship at City of Hope, joined Dr. Kuhn in private practice in 2003. Dr. Kuhn married Mollie Bloodworth in 1982.
Figure 76.

Dr. Joseph Kuhn.
Based on preliminary expertence with lymphatic mapping while he was a surgical oncology fellow, Dr. Kuhn introduced sentinel node biopsy to BUMC in 1993. Surgeons at BUMC were the first in Texas to apply the concept of the sentinel node to patients with breast cancer in 1994. Dr. Kuhn also performed the first liver cryosurgery in the state of Texas in January 1994, introducing a novel technique for freezing liver tumors.
Dr. Todd McCarty
Dr. Todd McCarty (Figure 77), born in Colorado, is a graduate of the University of Texas Southwestern Medical Center at Dallas, completing his general surgery residency at BUMC. He also went to City of Hope in California to perform a surgical oncology fellowship prior to returning to Baylor. In addition to surgical oncology, Dr. McCarty has an interest in bariatric surgery and has popularized gastric bypass and laparoscopic gastric bypass, having performed approximately 1000 procedures along with Dr. Kuhn and Dr. David Arnold. He is director of the Baylor Bariatric Surgery Center.
Figure 77.

Dr. Todd McCarty.
Dr. Steve Bell
Dr. Steve Bell (Figure 78) graduated from the Medical College of Georgia and completed a general surgery residency at Parkland Memorial Hospital in 1970. He then did a thoracic surgery residency at the same institution and began practice at the Dallas Medical Surgical Institute prior to joining the staff at BUMC. Early in his career, Dr. Bell developed an interest in endocrine surgery. He retired in 2003.
Figure 78.

Dr. Steve Bell.
CURRENT ISSUES
Resident work hours and competencies
Medical education remains a high priority for the Department of Surgery and BUMC. Within the past 2 years, the Accreditation Council for Graduate Medical Education has placed considerable emphasis on resident work hours. Effective July 1, 2003, residents cannot rotate any more often than every third night and cannot work longer than 80 hours per week when averaged over 4 weeks. They must have one full day off per week without any hospital duties. Residents must leave the hospital within 6 hours after their 24-hour duty. They must have at least 10 hours off before coming back to the hospital after being on for 24 hours. This is one of the biggest changes to occur in resident training in the last century.
Moonlighting is permissible but not in the parent institution. Any moonlighting at an outside institution must be approved by the department, and the resident must be monitored for fatigue.
These work hour restrictions have placed an additional load on the attending staff and paramedical personnel. However, the Department of Surgery has been able to work within these guidelines without hiring nurse practitioners or physician assistants. The guidelines do interfere with continuity of care but on the positive side give residents more time for rest, study, and family.
In addition, the Accreditation Council has established 6 competencies: professionalism, patient care, medical knowledge, practice-based learning and improvement that involves investigation and evaluation of their own patient care, interpersonal and communication skills, and systems-based practice. These must be put in place immediately, and outcomes need to be available for evaluation starting in 5 years.
Growth of the residency program
The general surgery residency program has doubled from finishing 4 chief residents in 1987 to 8 chief residents in 2002. Thus, the residency program is approved for 40 categorical 5-year residency positions and 5 one-year preliminary positions, for a total of 45 residents in general surgery.
Residents now rotate not only to BUMC but also to John Peter Smith Hospital (18 months), Presbyterian Hospital (6 months), Children's Medical Center (2 months), and Parkland Memorial Hospital burn unit (1 month). They also cover vascular surgery at the Baylor Jack and Jane Hamilton Heart and Vascular Hospital, which opened in April 2002.
Laparoscopy
Laparoscopic surgery has changed the procedures performed by general surgeons in the past decade. It continues to expand to include larger procedures such as gastric bypass, splenectomy, adrenalectomy, release of intestinal obstruction, colon and small bowel resection, diagnostic laparoscopy for abdominal pain, ablation of liver tumors, and even some liver resections. Distal pancreatectomy, hiatal hernia repairs, operations for achalasia, and closure of perforated peptic ulcers have all been performed laparoscopically. The general surgeon can no longer be expected to practice without significant laparoscopic skills.
Trauma
Cases of penetrating and blunt trauma have increased at BUMC. Approximately 20% to 25% of all trauma in Dallas is now managed at BUMC. This has created a staffing problem, particularly relating to surgical specialties such as neurosurgery, orthopaedics, and ophthalmology. Trauma in general has become a problem for Dallas County, and many of the hospitals are extended to maximum capacity in the management of the severely injured patient. Many of these patients are uninsured.
It is estimated that in the state of Texas, approximately 25% of patients do not have insurance, and charity care at BUMC has increased to approximately 10%. Without support from the city, county, state, or federal agencies, the uninsured caseload will be difficult for many hospitals to continue to support.
Operating rooms
The number of operating rooms has continued to increase. There are 27 operating rooms at Roberts Hospital and 17 at Truett. There are 4 operating rooms at Texas Surgery Center in the Sammons Cancer Center and 6 in the outpatient SurgiCare Center. Physicians Day Surgery has approximately 4 operating rooms, and the Baylor Hamilton Heart and Vascular Hospital has 4 operating rooms. This totals 62 operating rooms on the Baylor campus.
With this large number of operating rooms, approximately 30,000 operative procedures are performed annually at Roberts and Truett Hospitals and an additional 6000 procedures are performed in the outpatient surgery centers.
In 1998, Tim Parris, president of BUMC, appointed the chief of surgery and the chief of anesthesiology (Dr. Ronald Jones and Dr. Michael Ramsay) codirectors of the operating room. This is the first time that physicians have had direct management input into the operating room. In the past, the operating room has been strictly under administration and nursing services, with input from the operating room services committee. The codirectors must approve all major equipment expenditures in the operating room.
Technological changes and the future of surgery
Although the number of operative procedures continues to increase at BUMC, accuracy in preoperative diagnosis has changed tremendously in the past 2 decades. With the advent of sonography of the abdomen and rapid computed tomography of the abdomen in patients sustaining blunt trauma or penetrating injuries to extremities, the number of exploratory laparotomies and the need for exploration of vessels for proximity injuries has significantly decreased. Even with known intraabdominal injuries such as to the liver and spleen, surgery has decreased in favor of close observation. Computed tomography and magnetic resonance imaging of the body have significantly increased the accuracy of diagnosis of surgical diseases prior to surgery.
The use of colonoscopy and camera visualization of the entire gastrointestinal tract, as well as flexible upper and lower endoscopy and most recently virtual colonoscopy, has led to improved diagnosis and management.
Other technological improvements have included various stapling devices and have allowed for lower anterior colon resections and more extensive esophageal resections with anastomosis.
Chemotherapy has been used for the past decade to downstage breast tumors and rectal colon cancers. The use of preoperative irradiation has also downstaged rectal cancers.
Interventional radiology has allowed drainage of intraabdominal abscesses percutaneously, dilatation of stenotic blood vessels with angioplasty, and more recently the introduction of stents in the management of peripheral vascular disease and abdominal aortic aneurysms. The interventional radiologist has been able to dilate biliary strictures and even carotid artery stenosis. The duplex scan has replaced arteriography in many instances in preoperative evaluations. Computed tomography scans of the chest and abdomen, as well as positron emission tomography scans, have allowed patients to have preoperative diagnosis for metastatic disease that would have otherwise gone undetected. Sestamibi scans can now localize parathyroid adenomas in the neck, as can sonography. The Octreotide scan can identify neuroendocrine tumors in the abdomen and chest.
There will soon be a test to detect bleeding in the stool and differentiate upper from lower gastrointestinal bleeding. The genome project has allowed patients to have genetic testing for such tumors as breast and colon.
Thus, technological advances in the future appear to be unlimited. More noninvasive management of tumors will undoubtedly evolve, such as freezing or heating of tumors percutaneously. Shorter treatment utilizing radiation therapy has evolved.
The role of the surgeon in the management of surgical diseases will continue to be required. However, the technology used to accomplish these procedures is constantly changing, and the surgeon will require frequent updates as new procedures are developed and new instrumentations are developed. The growth and changes in the Department of Surgery have been beyond imagination during the past 100 years. The future always begins later today.
Acknowledgments
I would like to acknowledge Peggy Pazos, program coordinator, for assistance in preparation of the manuscript; Dr. J. Harold Cheek for review of early hospital staff board minutes; and Simira Meymand for assistance in research. Dr. Larry Wilsey, the staff of the Dallas County Medical Society, the staff of Baylor College of Medicine in Houston, the staff of the Texas Medical Association, and Elizabeth White of the McGovern Historical Collections & Research Center, Texas Medical Center Library, also provided important assistance.
Footnotes
Historical articles published in Proceedings will be reprinted in How We Care, volume 2. Readers who have any additional information, artifacts, photographs, or documents related to the historical articles are asked to forward such information to the Proceedings' editorial office for possible inclusion in the book version.
References
- 1.Timeline. Dallas and Fort Worth. Legacies. 1999;11(1):8–9. [Google Scholar]
- 2.McDonald WL. Dallas Rediscovered: A Photographic Chronicle of Urban Expansion, 1870–1925. Dallas: The Dallas Historical Society. 1978 [Google Scholar]
- 3.Giles ML, The Early History of Medicine in Dallas, 1841–1900. Unpublished thesis, The University of Texas, Austin, 1951;19:20.
- 4.Giles: 204.
- 5.Parkland Memorial Hospital: Celebrating the First 100 Years [special edition newspaper]. Dallas: Parkland Community Relations Department, 1994.
- 6.Giles: 341.
- 7.Giles: 155.
- 8.Giles: 161.
- 9.Giles: 164
- 10.Giles: 224.
- 11.Giles: 319.
- 12.Work Projects Administration. Dallas Guide and History, American Guide Series [manuscript in the Dallas Public Library], 1940.
- 13.Giles: 359–360.
- 14.Giles: 383.
- 15.Henderson L. Baylor University Medical Center: Yesterday, Today, and Tomorrow. Vol. 7. Waco, Tex: Baylor University Press; 1978. [Google Scholar]
- 16.Henderson: 9.
- 17.Moursund WH. A History of Baylor University College of Medicine 1900–1953. Vol. 7. Houston: Gulf Printing Company; 1956. [PubMed] [Google Scholar]
- 18.Henderson: 10.
- 19.Giles: 237.
- 20.Eggers GWN. Berthold Ernest Hadras (1842–1903): a biography. Clinical Orthopaedics. 1961;21:32–39. [Google Scholar]
- 21.Daily Journal of Austin, February 9, 1872.
- 22.Singleton AO., Jr . Berthold Ernest Hadra, MD: 1842–1903. In: Hood RM, editor. Early Texas Physicians, 1830–1915. Austin: State House Press; 1999. pp. 151–169. [Google Scholar]
- 23.Henderson: 13.
- 24.Baylor University Bulletin 1903–1904;VII.
- 25.Henderson: 18–20.
- 26.James PW. Fifty Years of Baylor University Hospital. Dallas: Baylor University Hospital; 1953. pp. 3–11. [Google Scholar]
- 27.Moursund: 25.
- 28.Moursund: 22.
- 29.Moursund: 29.
- 30.Henderson: 26.
- 31.Henderson: 28–29.
- 32.James: 20–21.
- 33.Moursund: 37–50.
- 34.Moursund: 42.
- 35.Moursund: 52.
- 36.Moursund: 56.
- 37.Moursund: 59.
- 38.Moursund: 62.
- 39.Henderson: 50–52.
- 40.Henderson: 45–57.
- 41.Moursund: 65.
- 42.Moursund: 66–67.
- 43.Moursund: 73.
- 44.Henderson: 60.
- 45.Baylor University Bulletin, 1904–1905, VIII.
- 46.Baylor University Bulletin, 1906–1907, X.
- 47.Baylor University Bulletin, 1905–1906, IX.
- 48.Texas Medical Journal, 1937 (June), 1154.
- 49.Texas State Journal of Medicine. 1945;27:671. [Google Scholar]
- 50.Dallas County Medical Journal, 1968 (February 2), 28.
- 51.Dallas Times Herald, January 28, 1968.
- 52.Baylor University Bulletin, 1909–1910, XIII.
- 53.Baylor University Bulletin, 1916–1917, XIX.
- 54.Dallas Moring News, February 23, 1950.
- 55.Texas Medical Journal. 1950 (May):341. [Google Scholar]
- 56.Texas Medical Journal. 1935 (January):615. [Google Scholar]
- 57.Baylor Hospital Board of Trustees Minutes, Book 1. Dalks: BUMC Archives.
- 58.Baylor Hospital Board of Trustees Minutes, Book II. Dallas: BUMC Archives: 47.
- 59.Moursund: 72.
- 60.James: 36.
- 61.Moursund: 74.
- 62.Henderson: 61.
- 63.James: 34.
- 64.Moursund: 80.
- 65.Henderson: 67.
- 66.Baylor University Bulletin, 1926 (April), XXIX.
- 67.James: 61–63.
- 68.Henderson: 69.
- 69.James: 54.
- 70.Henderson: 75–76.
- 71.Henderson: 71–92.
- 72.James: 76.
- 73.Henderson: 86.
- 74.Henderson: 90.
- 75.Moursund: 93.
- 76.Henderson: 95.
- 77.Henderson: 94.
- 78.Henderson: 93–113.
- 79.Moursund: 102–118.
- 80.Moursund: 112.
- 81.James: 83–84.
- 82.Moursund: 119–135.
- 83.Chapman JS. The University of Texas Southwestern Medical School: Medical Education in Dallas 1900–1975. Dallas: Southern Methodist University Press; 1976. pp. 34–52. [Google Scholar]
- 84.Henderson: 127.
- 85.Henderson: 118.
- 86.Pictured roster, Dallas Society of General Surgeons.
- 87.Henderson: 114–139.
- 88.Henderson: 140–152.
- 89.Baylor University Bulletin, 1925–1926, XXIX.
- 90.Moursund: 83–93.
- 91.Texas State Journal of Medicine. 1954;50:60. [PubMed] [Google Scholar]
- 92.Texas State Journal of Medicine. 1946:512. [PubMed] [Google Scholar]
- 93.Baylor University Bulletin, 1930–1931, XXXIV.
- 94.Baylor University Bulletin, 1934–1935, XXXVII.
- 95.Baylor University Bulletin, 1935–1936, XXXVIII.
- 96.Baylor University Bulletin, 1920, XXIII.
- 97.Texas State Journal of Medicine, 1943 (November), 411.
- 98.Texas State Journal of Medicine. 1950:221. [Google Scholar]
- 99.Henderson: 176.
- 100.John Peter Smith Hospital Proceedings. 1974;5:65. [Google Scholar]
- 101.Henderson: 210.
- 102.Klintmalm GB. The history of organ transplantation in the Baylor Health Care System. BUMC Proceedings. 2004;17:23–34. doi: 10.1080/08998280.2004.11927954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Uhr BW. History of ophthalmology at Baylor University Medical Center. BUMC Proceedings. 2003;16:435–438. doi: 10.1080/08998280.2003.11927941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Michael LA. Otolaryngology at Baylor University Medical Center. BUMC Proceedings. 2001;14:164–171. doi: 10.1080/08998280.2001.11927756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Jackson RW. Orthopaedic surgery at Baylor University Medical Center. BUMC Proceedings. 2001;14:254–263. doi: 10.1080/08998280.2001.11927773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Urschel HC., Jr History of the cardiothoracic surgical service at Baylor University Medical Center. BUMC Proceedings. 2003;16:422–429. doi: 10.1080/08998280.2003.11927939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ware EW., Jr A brief history of urology at Baylor University Medical Center. BUMC Proceedings. 2003;16:430–434. doi: 10.1080/08998280.2003.11927940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Wolford LW. The history of oral and maxillofacial surgery at Baylor University Medical Center. BUMC Proceedings. 2004;17:35–41. doi: 10.1080/08998280.2004.11927955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Stone MJ. History of the Baylor Charles A. Sammons Cancer Center. BUMC Proceedings. 2003;16:30–58. doi: 10.1080/08998280.2003.11927886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Cheek JH, Roberts WC. Jimmie Harold Cheek, MD: a conversation with the editor. BUMC Proceedings. 2002;15:154–170. doi: 10.1080/08998280.2002.11927834. [DOI] [PMC free article] [PubMed] [Google Scholar]






















