Webbing of the digits, or syndactyly, is not caused by the fingers sticking together in the womb; rather, it is caused by failure, during the sixth to eighth weeks of intrauterine life, of the usual longitudinal interdigital necrosis that normally separates the fingers. This “webbing” is the most common abnormality of the newborn hand. It happens either as an isolated anomaly or as part of a syndrome. When it occurs alone it is always inherited as an autosomal-dominant disorder. Five types of syndactyly are generally recognized:
Type 1: Zygodactyly. This is the most common form of syndactyly, occurring between the long and ring fingers.
Type 2: Synpolydactyly. This also involves the long and ring fingers but includes a duplication of the ring finger between the fingers.
Type 3: Ring-small syndactyly. This is usually bilateral, and occasionally the distal phalanges are fused. There may be only a rudimentary middle phalanx in the small finger.
Type 4: Haas-type syndactyly. In this rare type, described by Haas in the American Journal of Surgery in 1940, there is a complete syndactyly of all digits. Occasionally a sixth metacarpal and phalanges may be included in the cup-shaped hand.
Type 5. In this rare type, both the long and ring fingers and second and third toes are syndactylized. The fourth and fifth metacarpals and metatarsals may be fused.
Genetic counseling may be difficult, since the dominant genes show reduced penetrance and variable expressivities. Each future child carries a 50% chance of having the anomaly, but occurrence is rarely consistent from one generation to the next. A child's hand may well be different than a parent's hand, or neither parent may have a syndactyly. It does appear that paternal genes have a stronger influence than their maternal counterparts (Figure 1).
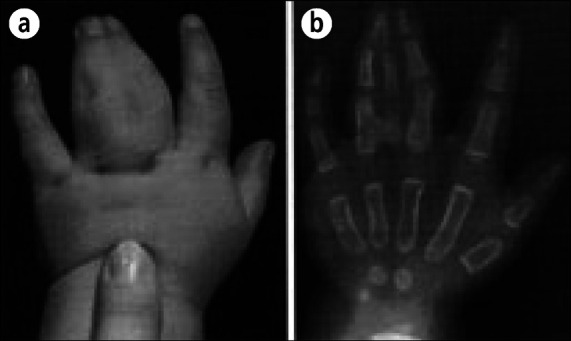
Figure 1.

Syndactyly—ring-small. A family with three generations of ring and small finger involvement, none of which was ever surgically corrected.
Syndactyly also occurs as part of many syndromes. In one group it predominates and is basic to identification of the syndrome; in a second, larger group it is a feature, but other medical problems are more characteristic of the syndrome. These problems are discussed in the second half of this paper.
INCIDENCE
In my personal series of over 3000 patients with congenital hand anomalies are more than 500 cases of true or isolated syndactyly. Nearly 40% of these patients were known to have a family history of the disorder. Syndactyly is thought to occur about once in every 2000 to 2500 births and is twice as common in males. Unilateral and bilateral cases occur about equally, and it is 10 times more common in whites than blacks.
The distribution of webbing between the digits varies, and the incidence is shown in Figure 2. There is no known reason why over 50% of all webbing should occur between the long and ring fingers. It seems reasonable that its lowest occurrence should be between the thumb and index fingers because of their gross difference in lengths. This webbing between long and ring fingers is probably less common than a similar condition between the second and third toes. This unimportant anomaly is inherited as a dominant trait, but sporadic cases are more frequent. I was surprised to find that I have incomplete webbing between my second and third toes and have been delighted to find it to be extremely common in friends, acquaintances, and succeeding generations of residents.
Figure 2.
Site of syndactyly. Percentage incidence in Iowa series when only true syndactyly of simple or complex types is considered. Reprinted with permission from Flatt AE, 1974.
CLASSIFICATION
Clinical classification of syndactyly is of value only insofar as it aids in treatment. Probably the most useful classification is based on a combination of two components: the degree of webbing and the presence or absence of bony fusion. In complete syndactyly, the skin web extends to the tips of the involved digits and sometimes produces a common fingernail. The web can stop at any point between the normal commissure and the ends of the fingers, in which case it is classified as incomplete (Figure 3).
Figure 3.

Simple syndactyly. Webbing between adjacent digits is either (a) complete, extending to the tips of the digits, or (b) incomplete, not reaching the tips.
Syndactyly is defined as simple when the webs contain only normal soft tissues and as complex when adjacent phalanges are fused or when there is interposition of accessory phalanges. In complex webbing, abnormalities of nerves, vessels, and tendons may also be present (Figure 4). The distribution and presence of digital nerves are quite unpredictable, but I have the clinical impression that the closer together the affected digits, the greater the likelihood of anomalies. The intrinsic muscles may be anomalous or absent, but there is no indication for tendon transfers in an attempt to replace their action.
Figure 4.

Complex/complicated syndactyly. (a) Drawing and x-ray film of the common side-to-side bony fusion in the usual complex syndactyly. (b) Drawing of a complicated complex syndactyly.
TREATMENT
Webbed fingers is an obvious physical defect, and individuals can and do, even in these times, go through life without having a separation of a syndactyly. For an otherwise normal individual I believe this is unnecessary cruelty. Parents are frequently subjected to social pressure urging early separation, but this is not necessarily in their child's best interest.
The timing of surgery is a problem—sometimes for the surgeon and always for the parents. I believe the question should be not how soon the operation can be done but rather how late the functional demands of the hand will allow postponement of surgery. Present-day surgical techniques have made obsolete old adages such as “Wait until the baby fat has gone” or “Do before 7 and revise at 14.” It should be explained to the parents that the timing and type of surgery must be related to the particular digits involved and the degree of completeness and complexity of the webbing.
I do not believe it kind or wise to simultaneously operate on both hands of either an adult or a child. It is devastating to be suddenly deprived of all prehensile ability. In the very young it might be justified by the possible risks of anesthesia, but in general I believe it better to operate on one hand at a time.
For the hand to develop and function as a prehensile organ, the thumb and small finger must be separated from their adjacent fingers early to allow the borders to oppose in grasp. Disturbances of the orderly growth of the long bones of the hand must also be corrected early if arch formation is to develop normally in the hand.
When two digits of unequal length are joined together, the longer digit inevitably develops a flexion contracture and may also show lateral deviation deformities. Figure 5 shows two patients with bilateral ring-small finger syndactyly, illustrating the deformities that occur if separation is delayed beyond 1 year of age. Similar uncorrectable deformities arise in triple syndactyly (Figure 6).
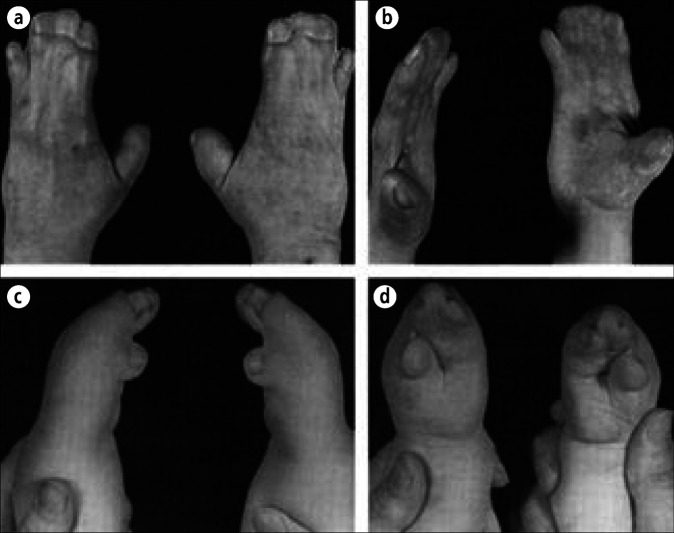
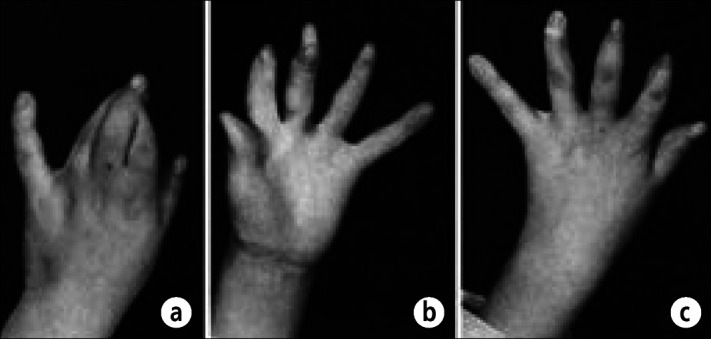
Figure 5.

Syndactyly—ring-small. Adult hands showing gross deformity of the ring fingers because correction was never done.
Figure 6.
Triple syndactyly. (a) Release done 30 years ago when the patient was 12 years old. The long and ring finger deformities have not corrected. (b) A mother's deformed right hand and her baby's unoperated right hand. (c) Index, long, and ring finger syndactyly before and after release in adult life, which could not correct the distal interphalangeal joint deformities in the right hand. Because these fingers are nearly equal in length, there is no flexion deformity of the proximal interphalangeal joints.
Because the thumb develops earlier than the fingers, thumb-index finger webbing is the least common pairing. When it occurs, the deformity of the index finger is profound and the web should certainly be separated by 6 months of age.
It is possible to separate both border digits from their adjacent fingers at the same operation since a single finger will not be denuded on both sides. The combination of ring-small finger and thumb-index finger webbing is rare in pure syndactyly but is the rule in acrocephalosyndactyly, and it is my practice to do both dewebbings in such patients at the same time.
There is no great urgency to separate a syndactyly between the long and ring fingers even if the condition is complex. Distal phalanx growth and fusion may continue undisturbed even into adult life. In index-long finger webbing, the interphalangeal joints are not on the same levels, and joint contractures will develop if separation is not carried out in the first few years of life. When the three central fingers are webbed, I usually separate the index-long finger web at about 1 to 2 years of age and the long-ring finger web at 2 to 4 year of age. When the long, ring, and small fingers are involved, early release is essential if deformity is to be avoided. Two operations are necessary (Figure 6).
In a review of syndactyly repair carried out at the University of Iowa Hospitals between 1946 and 1960, we showed that in those years more postoperative complications and less satisfactory results were obtained in children who were operated on when younger than 18 months. Others have reported similar results. The larger series tend to come from teaching programs, and I have a gut feeling that these results correlate better with the skill of the surgeon than the age of the patient. However, the operation can be postponed until after 18 months of age if the site and complexity of the condition allow it. During this waiting period the parents can be usefully occupied in stretching the skin between the digits; by doing so, the skin web can often be effectively widened. This “extra” skin makes the subsequent surgery considerably easier.
I believe that a child is entitled to have all webbing separated before being subjected to peer curiosity in school. I cannot agree with those who feel that surgery can be postponed until 6 to 10 years of age. The hand grows significantly in the early years, doubling in size by the age of 2. This rapid increase in skeletal length demands separation of the digits to allow unimpeded growth. It also dictates careful planning of incisions so that scarring after surgery will not lead to contractures.
When all the digits are webbed, the four necessary clefts can be established in only two operations. At the first operation the thumb-index and long-ring separations are carried out. This is followed within 3 to 6 months by separation of the small-ring and index-long fingers at the second operation. This plan avoids the risks inherent in dividing on both sides of one finger at the same time.
Syndactyly is common but its treatment is not easy; it requires good technical ability and judgment. I therefore recommend to the tyros in this field that they choose one operative technique and become expert at it before they try the many hundreds of modifications and methods that currently appear in the literature.
PRINCIPLES OF SEPARATION
Surgeons have been separating webbed fingers for nigh on 200 years, and from all this experience certain principles have evolved. Despite the many minor differences in techniques, the following principles are generally agreed upon:
The web space should be made from a local flap, usually dorsal.
The fingers are defatted before closure.
The sides of the fingers are closed with acute zigzag local flaps.
Bare areas are covered with full-thickness skin grafts.
Skeletal abnormalities are corrected.
Only one side of a digit is released at a time.
Meticulous technique is essential; use fine ophthalmic catgut sutures for skin closure.
Parents often do not understand the need for additional skin. A useful way to demonstrate the necessity for skin grafting is to measure the circumference of the two involved digits in a parent's hand individually and combined (Figure 7). The demonstrable difference between the sum of the two fingers and the combined circumference usually satisfies the parents' questions regarding use of a skin graft. In fact, a considerable amount of skin is needed because most operative plans do not mobilize skin beyond the midline of the dorsal and palmar surfaces.
Figure 7.
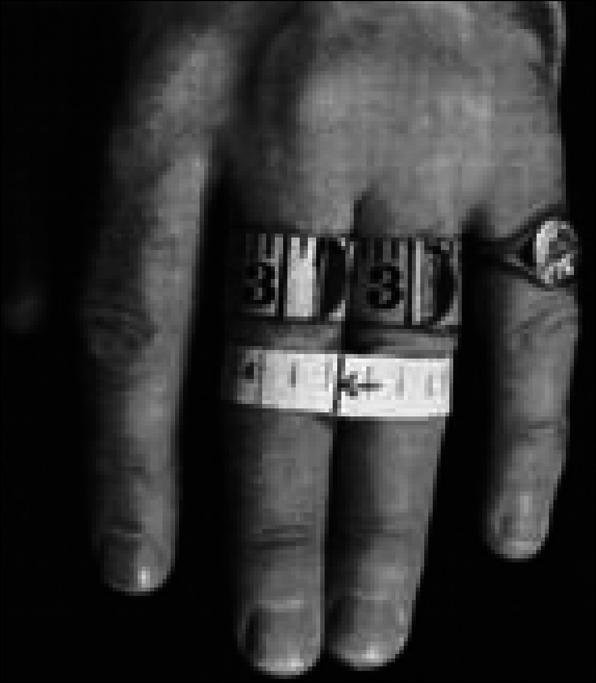
Skin grafting in syndactyly. The circumference of my long finger is 3¼ inches and of my ring finger, 3⅛ inches. The total of 6⅜ inches is considerably greater than the 4⅝-inch circumference of the two measured together. This difference in measurement can be used to explain to parents the need for skin grafts. Reprinted with permission from Flatt AE, 1974.
I have found that the most satisfactory basic operative plan is to establish the depth and width of the commissure by the use of a local dorsal flap. I use zigzag incisions along the sides of the digits to minimize any chance of secondary contracture, and wherever possible, I plan the flaps to completely cover one finger so that a skin graft is needed for the second digit only (Figure 8). An added advantage of the broad dorsal flap is that it tends to provide a replica of the normal commissure, which slopes downward toward the palm to give the palm a greater length than the dorsum of the hand. If the separation is carried back to the level of the metacarpophalangeal joint and the natatory ligament is excised, then the likelihood that a revision of the commissure will be necessary during the teenage growth spurt is greatly reduced; however, it cannot always be avoided. For this reason I stress to the parents the need for long-term follow-up, even though all primary surgery has been completed before the child enters school.
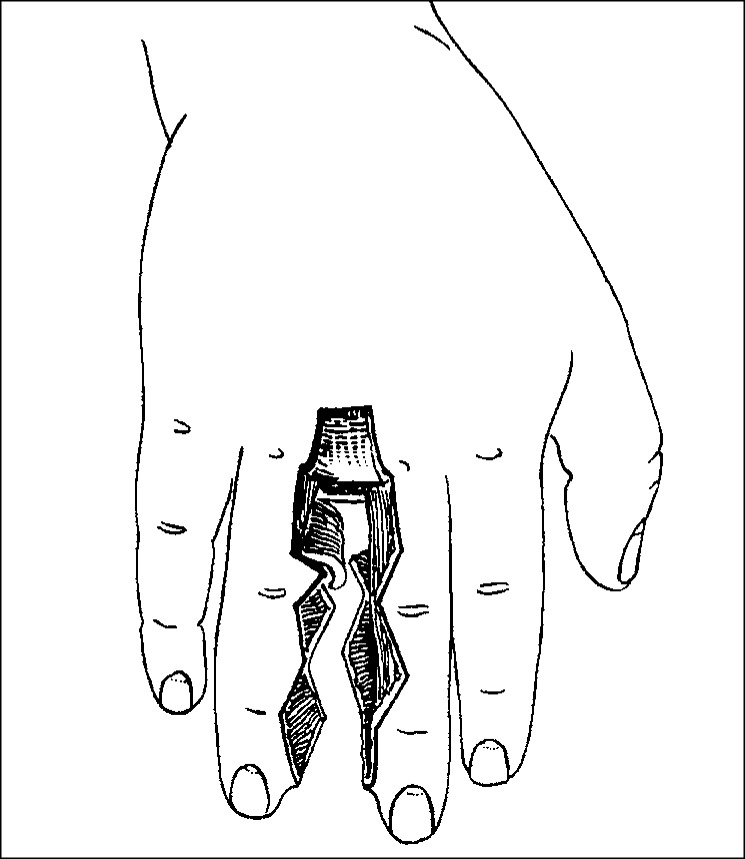
Figure 8.
Syndactyly separation. The basic flaps raised after the method described by Bauer, Tondra, and Trusler. Reprinted with permission from Flatt AE, 1974.
When establishing the web space, it is important to realize that the commissures between the index and long fingers and ring and small fingers are rectangular or square-U shaped and the central commissure between the long and ring fingers, while frequently V shaped, may be a square. This breadth of the border commissures should always be provided, since it is needed for the encircling span of wide grasp. The normal web space extends distally as far as the midpoint of the proximal phalanx, and the slope of the thin non–hair-bearing skin measures 45° to 50°. If the natatory ligament is not cut, then a ridge may mar this slope and create a potential for “web creep.” Web creep, or distal migration of the reconstructed commissure, is not uncommon and is basically caused by scar contracture. This scarring can be due to inept planning of the incisions, failure of primary healing, or failure of skin grafts. Split-thickness skin grafts are associated with web creep eight times more often than full-thickness skin grafts. If failure of a skin graft is treated by calculated neglect and secondary healing occurs, the scarring will inevitably tether the area, and subsequent bone growth will drag the commissure distally. Upton has pointed out that a 1.0-mm loss of tissue or graft in an infant translates into a 1.0-cm distraction in the adult. Accordingly, loss of a graft must be treated by regrafting as soon as possible. Often a split-thickness skin graft must be used because of the poor recipient bed.
I prefer using full-thickness skin grafts for all primary syndactyly repairs, and I take the grafts from the lateral inguinal area. It is important that the location of the donor site is well lateral, in the area of the anterior superior iliac spine. Grafts taken from more medial sites can become embarrassing hair-bearing areas after puberty. Parents sometimes request that the foreskin be used; although this seems a practical donor site, the skin is of unusual texture, frequently does not heal well, and eventually becomes deeply pigmented. The wounds should be closed with fine ophthalmic catgut.
I believe strongly that the key to this whole operation is the judicious defatting of the tissues on the adjacent sides of the fingers and on both palmar and dorsal aspects across to at least the midline of the two involved digits. In small children this fat will be absorbed later, and removing it early allows the flaps to sit in readily without tension. Failure to do this may lead to a considerable amount of edema following surgery and often even the loss or tearing apart of some of the interdigitated flaps.
Postoperative care is simple. I do not impale the fingers on wires or sew them to rigid splints. I use Dacron batting dressings. Dressings must be kept dry and usually left undisturbed for 2 weeks. Crusting over the graft and the incisions is common, and there is no urgency in its removal. The catgut sutures disintegrate at different times, and the parents should be taught to remove them when they loosen. If the crusts are attached by a few catgut sutures, these can be cut. Further dressings are applied for about another 7 to 10 days. Following this, there should be complete healing and the child can be allowed free use of the hand.
The full-thickness skin graft frequently takes several weeks to reepithelialize, depending on its thickness. If frank failure of the graft has occurred, I believe the child should be admitted to the hospital, the failure area should be cleaned up, and a new full-thickness or thick split-thickness graft applied. The area is functionally too important to have to tolerate the scarring of secondary healing.
Straight-line incisions are being used, on a trial basis, to release simple syndactylies in infants the first few days after birth. At this time the infant's very loose, pliable skin is said to contain considerable amounts of type III collagen rather than type I. This is thought to account for the rapid healing and virtually total absence of scarring of the wound. The operation can be done under local anesthesia, a tourniquet is not necessary, and the wound is closed with no. 6-0 catgut sutures. Only a simple dressing is needed and splints are not used. I first heard of this while listening to Elmer E. Raus, MD, read a paper in which he described a 4-year follow-up of two patients with syndactyly separation. I have not had the opportunity to try this operation, and colleagues who have done the occasional procedure report excellent early results; however, pediatricians may express resistance and skepticism, and parents may have reasonable concerns.
I have described only the principles I followed in the treatment of simple syndactyly and have deliberately left out a wealth of technical details. Complex problems are discussed below. Some would say that the plan I use is unnecessarily complicated and that simpler incisions can be used. This is probably true, but experience tells me that my method yields consistently good results because I've done a lot of these operations.
COMPLEX SYNDACTYLY
Syndactyly is a frequent feature in skeletal dysplasias and various malformation syndromes. The syndactyly is often a minor problem in relation to the restoration of function to the whole hand. The web distribution is different than in simple syndactyly, and the figures more nearly resemble those usually quoted as the incidence for “webbed fingers” (Figure 9). Many cases are complicated by bizarre skeletal deformities and by varying degrees of hypoplasia. The overriding principle is to establish as normal a skeleton as possible at a very early age. If this is done, then formation of digits and definitive work on the webs can be postponed until later.
Figure 9.
Site of syndactyly. Incidence when associated conditions (all webbed cases) are included. These figures more nearly resemble the usually quoted incidence for syndactyly. Reprinted with permission from Flatt AE, 1974.
Syndactyly is a predominant feature of conditions such as Poland syndrome and acrocephalosyndactyly, which comprises five separate syndromes, of which Apert and Chotzen are the most common. Two types of acrocephalopolysyndactyly are differentiated, Noack and Carpenter. In the former, the face and hands are mildly involved; in the latter, the face and hands are severely involved. Other syndromes with predominant syndactyly involvement include the two orofaciodigital syndromes and oculodentodigital dysplasia. I do not include the syndactyly associated with constriction rings (Streeter syndrome) because there is no evidence of a genetic basis for this condition.
The group of common syndromes in which syndactyly may be present but in which it does not have to occur to establish the diagnosis has been listed by Poznanski. It currently includes 28 syndromes grouped under four headings: chromosomal aberrations, craniofacial syndromes, syndromes with cutaneous manifestations, and a miscellaneous group. Some of the conditions in these groups are potentially lethal, and all newborns with syndactyly must have a complete physical examination to exclude potential problems before any reparative surgery.
FINGERTIPS
Complexity starts at the fingertips with a synonychia or solid union between nails, with or without side-to-side fusion of the terminal phalanges. When there is no bony union or a common nail, the fingertips can be separated at the same time as the fingers. Coverage for the fingertips is obtained in the same way as if there were a common nail (Figure 10). The central portion of the common nail and its root are removed and a small lateral wedge of pulp excised to allow the sides to be closed on the adjacent edge of the nails. When the gap on the side of the fingers is large, the use of composite skin grafts from the foot yields good results.
Figure 10.
Complex fingertip. A central slip of nail and its root wide enough to reduce each nail to a normal width should be removed. Closure is obtained by (a) wedge excision of pulp and bringing up the sides of skin to the nail or (b) creating two laterally based pointed flaps and rotating them into place. The first method is far easier to do but may make a narrower fingertip.
This method can be used at the same time as the separation of a complete syndactyly, or it can be used as a separate small procedure to free the skeleton in fusion of the distal phalanges before subsequent separation of the full webbing. The technical details are well described in the original article by Sommerkamp et al.
When the syndactyly conceals a polydactyly, the interdigital extra phalanges have to be removed. The only advantage of this particular problem is that the broad width between the digits supplies a considerable amount of extra skin that allows easy interdigitation of the skin flaps after the two digits have been separated (Figure 11).
Figure 11.
Concealed polydactyly. (a) In this patient, a type III polydactyly is hidden in the web between two apparently normal digits. (b) The polydactyly could be missed if an x-ray film is not made. Reprinted with permission from Wood VE, 1971.
It is always tempting to try to maintain four fingers in a hand, and superficially some complex cases of syndactyly may appear to present a relatively simple technical problem. At operation, however, additional complexities can be found that may lead to bad results later. When severely complicated syndactyly is present, I believe it foolhardy to attempt to obtain four normal looking and moving fingers; I go straight to a plan that will allow formation of three good moving digits. Figure 12 illustrates a complex polysyndactyly on the radial side of the hand involving the index and long fingers. I elected to trim the double proximal phalanx of the index finger and to totally remove the extremely disturbed skeleton of the long finger. The early end result of this showed that the epiphysis of the index proximal phalanx was growing satisfactorily, and long-term follow-up showed that growth continued and a satisfactory three-fingered hand was obtained.
Figure 12.

Complex syndactyly. The left hand has been provided with a functional three-fingered hand. Attempts to preserve four fingers in the right hand led to functional and cosmetic disaster. Reprinted with permission from Wood VE, 1971.
Figure 13 shows an extremely complicated jumble of bones representing a polysyndactyly of the index and long fingers. No attempt was made to create a four-fingered hand.
Figure 13.

Complex syndactyly. (a) The D-shaped duplicated proximal phalanx of the index finger was whittled down using a #15 blade because all impact tools such as a chisel might have destroyed the epiphysis. The operation was done when the child was 22 months of age. (b) Remodeling was proceeding satisfactorily 2 years after surgery. (c, d) The epiphysis continues to grow normally. The patient is right-handed and plays the violin. Parts a, b, and d were reprinted with permission from Flatt AE, 1971. Part c was reprinted from Wood VE, 1970, with permission from The Journal of Bone and Joint Surgery, Inc.
Syndactyly is a frequent feature in skeletal dysplasias and various malformation syndromes. These syndromes are not all equally common, and I have chosen to discuss the technical problems of only a few in which syndactyly predominates and is basic to the identification of the syndrome.
ACROSYNDACTYLY
In acrosyndactyly there is a fusion between the more distal portions of the digits with the space between the digits varying from broad to pinpoint in size, but there is always a communication between the dorsal and palmar aspects of the conjoined digits. This condition, which has been variously called terminal fenestrated, exogenous, or amniogenous syndactyly, is not hereditary and occurs spontaneously.
It presents in two basically different forms. One is associated with constriction rings; the deformity is bilateral in half the cases but the two hands are not symmetrically involved. Half of these cases have congenital “amputations” or shortening of the digits, and only half of these digits are stiff. The child's intelligence is normal. An intrauterine “insult” that occurs after the fingers have fully separated is the probable cause. It is usually associated with shortening of the affected fingers, and Patterson, who has studied this condition extensively, has established the following criteria for these cases: no real proximal webbing, no bony fusion between the fingers, a high degree of association with constriction rings, and various abnormalities of the affected fingers apart from the soft tissue fusion. When constriction rings are present, Patterson postulates that the intrauterine insult is an ulceration occurring at the rings, with subsequent fusion.
He established a useful clinical distinction of mild, moderate, or severe cases based on the skeletal abnormalities (Figure 14). Mild cases are those in which affected digits have three phalanges and two interphalangeal joints. Moderate cases are those in which affected digits have two phalanges and only one interphalangeal joint; in severe cases, fingers are stubby, containing one phalanx and no interphalangeal joints. Of the 92 patients I treated who met the criteria for acrosyndactyly, 6 cases were mild, 60 moderate, and 26 severe.
Figure 14.

Acrosyndactyly. (a) Mild. (b) Moderate. (c) Severe.
There is no standard pattern in the degree of adherence of the digits, nor is there a standard site for the epithelium-lined cleft or sinus that is always present between adjacent digits. The fingers are commonly joined side to side but can be stacked on top of each other. There is usually a soft tissue plane of separation between adjacent bones. Occasionally the fingers are joined by only a narrow skin bridge; this connection can be snipped or tied off in the newborn nursery.
Treatment
Separation of the less complicated forms of acrosyndactyly is simple, and the cosmetic and functional results are usually satisfactory. When, however, acrosyndactyly is associated with congenital constriction rings, the technical problem can be severe. The basic principle of establishing a proper longitudinal skeletal pattern may have to be combined with an early decision as to whether to salvage three or four fingers.
The other important factor in operative planning is the site and extent of the clefting or sinus between the digits. Whatever the size of the epithelium-lined space, it will invariably be more distal than the optimal site for commissure reconstruction. Sinuses will therefore have to be excised (Figure 15).
Figure 15.

Acrosyndactyly—sinus tracts. A single dorsal sinus connected to two palmar openings. These tracts must be excised completely.
Skin coverage of the separated fingers is obtained by local flaps, but planning these flaps around the sinuses can be a most frustrating experience. When constriction rings are present, local flaps can often be constructed out of the fatty skin protuberances. A surprising amount of coverage can often be obtained after these protuberances have been defatted and rotated into place. Despite the use of these local flaps, skin grafts frequently have to be used and to a greater extent than in a simple syndactyly. The rounded contour of the tips of the fingers should be established at the primary separation. Although length is always desirable, there is little functional value in a tapered fingertip that looks as if it had been sharpened like a pencil. Pointed tips of bone must be rounded off.
Mild deformities
The basic aim in surgical correction of mild cases is to free the digits early enough to allow the fingers to grow parallel and without articular deformities, particularly at the metacarpophalangeal joints. Frequently these patients have relatively long clefts rather than narrow cylindrical sinuses between the fingers, and skin grafts are needed on the more distal portions of the fingers.
Usually I prefer to separate these fingers when the child is around 6 months of age or as soon as possible if the patient is seen at a later age. Split-thickness skin grafts provide perfectly satisfactory skin cover at this primary operation. The technical problems involved in using multiple small full-thickness skin grafts are great, and the ultimate result is not significantly better than that obtained with split-thickness skin grafts (Figure 16).
Figure 16.
Mild acrosyndactyly. (a) Before surgery. (b, c) After surgical release. Separation should be done at an early age. Split-thickness skin grafts give satisfactory cover for the raw areas of the fingertips.
Moderate deformities
In most of these patients' hands, only two phalanges and one interphalangeal joint can be demonstrated on x-ray examination. Fusion of these shortened digits toward their tips adducts the border fingers at a considerable angle and causes early joint distortion unless the digits are released.
Frequently there appears to be a jumbled collection of fingertips distal to the site of fusion since it is rare for fusion to occur at the most distal portion of the fingers. These fingertips may not carry nails and often cannot be directly matched to an appropriate finger; however, every attempt should be made to do this rather than to excise these tips because they can contain phalangeal buds that may be associated with articular spaces not visible on the x-ray film.
The principles of surgical correction are the same as for mild cases—early liberation of the trapped fingers followed by deepening of the commissures (Figure 17).
Figure 17.

Moderate acrosyndactyly. (a, b) A patient in whom a three-fingered hand was created. (c, d) A similar type of deformity in which it was possible to develop four fingers.
Severe deformities
The variety of deformities possible in these cases makes it impossible to discuss their treatment except in generalities. Usually they are associated with varying degrees of constriction rings, and bulbous fatty protrusions occur distal to the rings. Often the fingers are affected to different degrees, and the varying lengths of the adherent digits make the planning of skin coverages for the separated digits a formidable task.
Since the fingers are always short and are frequently only stubs, it is important that they be separated as far proximal as is possible. Usually the separation can be combined with the deepening of the commissures, which should be carried well proximal, at least to the level of the metacarpal heads (Figure 18).
Figure 18.

Severe acrosyndactyly. Severe involvement of the hand in which four fingers were obtained by staged surgery. (a) Before surgery. (b) Border digit freed. (c) Index finger separated. (d) At completion of surgery.
Early release of these stubby fingers is mandatory because it will allow maximum use during the growth years. These little hands frequently present a much greater technical challenge than the actual separation of the fingers. When a ballooned and bulbous fingertip has to be amputated, the skin should be used as a graft after it has been defatted and flattened. Revision and further deepening of the commissures are often necessary during the teenage years.
Follow-up
A significant finding in my long-term follow-ups has been limitation of finger flexion. Motion is only poor or fair in most of the proximal interphalangeal joints of fingers with moderate involvement. Similar limitations of motion are found in the distal interphalangeal joints of patients with mild degrees of acrosyndactyly. In severe cases, motion at the metacarpophalangeal joints is usually within normal range.
SYMBRACHYDACTYLY
The infinite variety of these conditions makes it extremely difficult to describe therapy for this group of deformities, but I believe the principles are well established. The digits must be separated early to allow longitudinal growth. Frequently this dictates that a three-fingered instead of a four-fingered hand be obtained. It matters little if in the early months of life a false or elective syndactyly is established by skin grafting if in turn this allows longitudinal definition of the skeleton. Later separation can produce hands that function well but are frequently unattractive (Figure 19).
Figure 19.

Symbrachydactyly. (a) Coalesced fingers such as these must be freed in the first few months of life. (b) At primary surgery, fingers must be separated sufficiently to allow normal configuration of the hand skeleton and to be properly covered with skin. It is often advantageous to create a syndactyly at this time, as was done in the left hand. (c) The fingers were separated later, and a reasonable pair of three-fingered hands was salvaged from the original jumble. Reprinted courtesy of Dr. D. C. Riordan.
APERT SYNDROME
Acrocephalosyndactyly was first properly described as a syndrome by Apert in 1906. Since that time, a variety of closely related genetic disturbances characterized by premature fusion of the cranial sutures and varying degrees of syndactyly of one or more of the hands and feet have been described.
Individuals of all races show similar deformities. Mental retardation occurs but is certainly not inevitable. Patients with this condition used to be found in mental institutions, some because their mental status justified it and others because their parents abandoned them as a result of their repulsive appearance.
Two main clinical categories have been distinguished: the true or typical Apert syndrome and an atypical group. The hand in true Apert syndrome shows severe interdigital bony union, typically with a middigital bony mass and a single nail common to the index, long, and ring fingers. This severe mitten involvement of the hand is not seen in the atypical cases, although varying degrees of hand abnormality can be found. McKusick has subdivided these cases into various types such as Apert-Crouzon or Vogt, Saethre-Chotzen, Waardenburg, and Pfeiffer. As more patients with these conditions are recognized, the variety of abnormalities and their combinations increases and these distinctions become somewhat blurred.
A similar but distinct pair of syndromes can be recognized since they are characterized by acrocephalopolysyndactyly. In both Noack and Carpenter syndromes, the cranial and facial features are similar to those of Apert syndrome but the hands differ because of the presence of polydactyly.
The most consistent finding in the hands is syndactyly of all fingers, which occurs in two types. The other, more common and less severe form is a spadelike hand sometimes called the obstetrician's hand. The other, more severe deformity bunches the fingers together into what some liken to a rosebud but to my mind more resembles a spoon (Figure 20). The thumb is always short and radially deviated at the metacarpophalangeal joint. It may be included in the webbing with the fingers but is usually partially free to move. The index, long, and ring fingers usually share a common nail, but the small finger frequently has an independent nail and may not be fused to the ring finger at its terminal phalanx. Since independent motion of the fingers is not possible, the hand can be used only for gross movements in a paddle-like fashion. The fingers are stiff in adult life, but in early childhood, up to the age of 4, may retain some interphalangeal joint motion. The interphalangeal joints fuse, and a synostosis always develops between the bases of the fourth and fifth metacarpals. This fusion deprives the hand of the essential cupping movement of the ulnar border of the normal hand.
Figure 20.

Paronychia and Apert syndrome. Children with this disorder suck their whole hand, resulting in severe chronic infection. Nail trimming is usually insufficient, and the whole nail frequently has to be removed.
There is frequent shortening of the arm and forearm, with abnormalities and limited motion of both the shoulders and elbows. The feet are involved, and the foot is usually broad with complete syndactyly of all toes.
Treatment
Although some patients with Apert syndrome are mentally retarded to a varying degree, most of them are able, or can be taught, to care for themselves. A hand with individual fingers, even though they may be stiff, is more useful and more cosmetically acceptable than a fused, spoon-shaped, relatively immobile hand. Mental retardation is no reason to withhold surgical treatment of the hand in Apert syndrome.
The principle in planning reconstruction should be to provide the digits with skeletal elements as normal as possible covered by supple skin with normal sensitivity. In hands with complex syndactyly, particularly in those with bony fusion between phalanges, early operation is necessary. The operation should be planned to define the digits and allow unimpeded skeletal growth. If surgery is postponed, incongruities of length and growth between fingers usually produce additional deformities in an already malformed hand.
The two types of hands, paddle and spoon, pose different surgical problems; the paddle type is easier to release and reconstruct (Figure 21). The tight, tapered, spoonlike hand can be restored to a flattened paddle by early release of the synostosis of the terminal finger phalanges. This can be done in the first few months of life, and sometimes the terminal separation will heal per primum. If in doubt, use split-thickness skin grafts. This early release often allows the hand skeleton to rapidly regain its normal flattened parallel fingers.
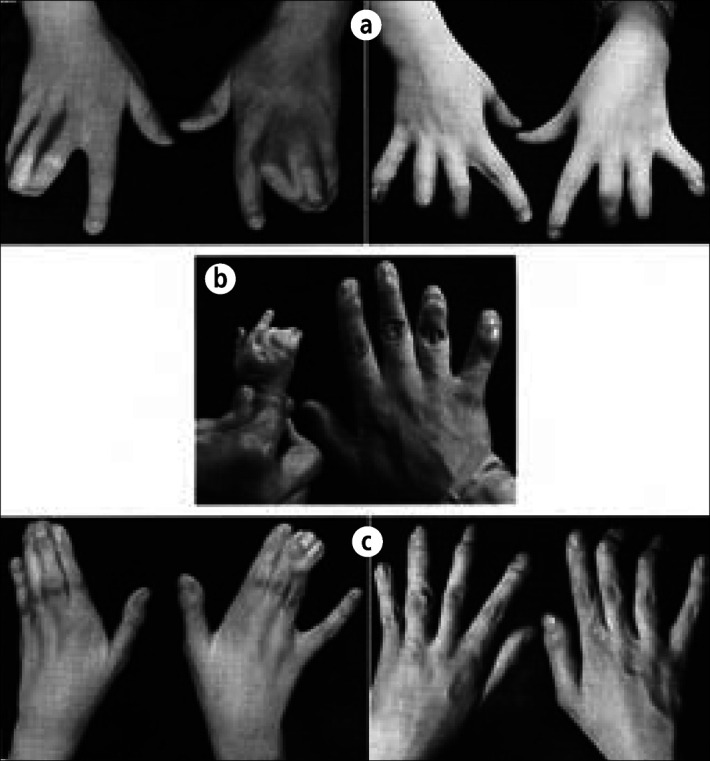
Figure 21.
The hand in Apert syndrome. (a, b) In the more common type, the fingers, though fused at the tips, lie parallel in the same flat plane as in the spade. (c, d) In the severe form, the tips of the fingers are bunched together and produce a rosebud or spoonlike hand. Reprinted from Hoover GH et al, 1970, with permission from The Journal of Bone and Joint Surgery, Inc.
In a child younger than 2 years, both hands are operated on at the same time. In the older patient, who must feed himself and care for his body functions, one hand at a time is operated on. In general, the surgical approach to these hands is as follows.
The border digits, the thumb and small finger, should be released before the patient is 1 year old. The thumb-index and ring-small finger webbing are fully released. If the thumb is not included in the syndactyly, a four-flay Z-plasty deepening of the thumb-index web space is sufficient.
It is vital that the first web space be fully developed at this operation. If the thumb is adducted to the second metacarpal, a wide flap will have to be rotated down from the dorsum of the hand and the consequent defect skin grafted. When separating the fourth web space, it is reasonable to use the standard zigzag incisions to provide side coverage. If the separation is being done when the interphalangeal joints have already fused, less elaborate incisions can be used since there is no joint motion.
Once the border digits have been freed and allowed to mobilize, the central mass of three fused fingers remains. The anatomy within this mass differs greatly from the normal and has been carefully studied by Upton. The digital vascular patterns vary considerably; both median and ulnar nerves are aberrant, and the extensor and flexor tendons show significant variations distal to the metacarpophalangeal joints.
The central mass therefore presents a formidable separation challenge, particularly if preservation of all three fingers is the goal. This is desirable but not always possible and depends largely on the findings at surgery. Since both sides of the long finger cannot be denuded at the same time, the index or the ring finger can be separated off and a careful exploration of the neurovascular status of the raw side of the long finger recorded in the operative notes.
Later, when the second separation is done, the neurovascular status of the other side of the long finger can be established, and the decision then becomes whether to make a four-fingered or three-fingered hand. Aesthetically it is pleasant to have four fingers, but functionally I believe the three-fingered hand has just as much utility, and when in doubt as to finger survival, I opt for three fingers without hesitation (Figure 22).
Figure 22.
Three-fingered hand in Apert syndrome. Functionally and cosmetically satisfactory hands can be provided for these individuals by amputating the long finger and producing a three-fingered hand. (a) Before surgery. (b, c) Completion of right-hand surgery and release of border digit on the left hand. (d) Final result. Reprinted from Hoover et al, 1970, with permission from The Journal of Bone and Joint Surgery, Inc.
The thumb radial deviation will continue with growth, and eventually a fusion and possibly even lengthening of the thumb will be needed. When making a three-fingered hand, there is plenty of skin to provide good coverage with proper sensibility. I believe it advisable to leave the third metacarpal in place and not to narrow the hand by removing it and shifting the index ray ulnarward. My long-term follow-up studies show that more deformity develops in hands so treated than in those in which the metacarpal has been left in place.
Hand function
As originally described by Apert, hand function before surgery typically consists of using one hand against the other in paddle-like fashion.
Our patients who have only their thumbs partially free have a prehensile pattern consisting of the ulnar aspect of the thumb (usually the interphalangeal or the metacarpophalangeal joint surface) opposing the proximal radial border of the index finger. All prehensile tasks are accomplished by using this lateral type of pinch and by using one hand against the other. Nearly all patients could find some ingenious way to perform the preoperative tasks expected of anyone of their intelligence and level of motor development. One patient could not; she had complete syndactyly of the thumb and all fingers, and her function consisted entirely of holding objects between her two hands and of batting at toys.
The operations I have used improved the versatility of prehensile patterns that these patients could use rather than added to the number of tasks they could perform. In some the three-fingered hand seems to have a greater versatility of prehensile patterns than the four-fingered hand. This is probably because of the ability to utilize more of the movement at the metacarpophalangeal joints.
All our patients with three-fingered hands could oppose the thumb to at least the base of each finger, and two patients could oppose the thumb to the tips of all fingers. Tasks that had been accomplished by using one hand against the other before surgery were accomplished after surgery by utilizing more of the prehensile patterns that a normal hand uses to perform the same task. Use of the body as a stabilizing surface for objects is eliminated to a great extent. Radio or television dials can be turned without being approached with the hand or body in the awkward position previously needed. Buttoning and bow-tying require fewer movements, and awkward hand positioning is eliminated. The grosser movements needed in self-care skills do not seem to change in pattern after surgical treatment.
POLAND SYNDROME
Professor Mark Ravitch has pointed out that Poland syndrome conforms to the pattern that has been established for any condition, disease, operation, or anatomical structure to which an eponym has been attached: the individual thus memorialized was not the first to describe the condition, structure, or operation named after him; he misunderstood or did not understand fully what he described; he has been misinterpreted or misquoted; or all of the above are true.
Characteristically the syndrome includes congenital dysplasia of the whole of the upper limb, absence of the sternocostal portion of the pectoralis major muscle, and varying degrees of syndactyly. The fingers are frequently shortened because of lack of growth, or even absence, of the middle phalanges.
The term “Poland's syndactyly” was first used to describe this group of congenital anomalies by Clarkson in 1962. He reported that in 1841 Alfred Poland first described the association of congenital thoracic anomalies with ipsilateral syndactyly. While a medical student at Guy's Hospital, London, he dissected a male cadaver which lacked the sternocostal head of the pectoralis major and the pectoralis minor, while the serratus anterior, the external oblique, and the muscles of the left arm were hypoplastic. The four essential features of this condition are 1) unilateral shortening of the index, long, and ring fingers, 2) syndactyly of the affected digits, 3) hypoplasia of the hand, and 4) absence of the sternocostal portion of the ipsilateral pectoralis major muscle.
The cause of Poland syndrome is unknown, but it is generally thought to occur sporadically. Although hereditary traits have been demonstrated for some anomalies of the hand such as polydactyly, only one report of Poland syndrome described familial incidence; we were unable to establish a positive family history of any of our 43 patients.
Physical signs
The involved hand is always hypoplastic, the forearm is usually hypoplastic, and the arm is only frequently affected. The extent of involvement of the upper limb tends to be proportional to the extent of the syndactyly and the hypoplasia of the hand. The extrinsic muscles in the forearm are variously involved, and the flexor tendons particularly may show abnormal insertions within the palm. The syndactyly and the involvement of the bones vary over a wide spectrum. Usually the index, long, and ring fingers are more affected than the thumb and small finger. Often all digits are involved, making a mitten hand; sometimes the involvement is so severe that the fingers may be represented only by nubbins. The thumb and its web space frequently appear disproportionately small, with the thumb lying adducted and supinated so that it lies in the same plane as the fingers. The webbing tends to be simple, involving soft tissues only, and may be incomplete or complete; aplasia of the nails is common. The characteristic bone anomaly is hypoplasia of the middle phalanges. It is often so severe that there is effectively only one interphalangeal joint. Shortening of the middle phalanges is more common on the ulnar side of the hand than on the radial and is not necessarily confined to the digits included in the syndactyly.
The thoracic deformity is variable, but in all patients with the syndrome the costal head of the pectoralis major is absent, and in many the pectoralis minor is absent. Pectoral aplasia is the most frequent skeletal muscle deficiency in the general population, but only 13.5% of the people with this defect have Poland syndrome. Absence of the pectoral muscles seems to cause little functional impairment despite Poland's original clinical description that implied an inability to internally rotate the arm:
George Elt, a convict, aged 27, respecting whom no history could be obtained; except that it was remarked that he could never draw his left arm across his chest; and that when asked to give his left hand, in order that his pulse might be felt by one standing on the right side, he invariably turned around to do so.
Brown and McDowell mention the case of a professional fencer whose pectoralis major was missing on the dominant side, and Christopher reported on a left-handed pitcher who had absence of the left pectoralis major muscle.
Operative plan
It is important that the parents realize early in the treatment plan that two features of this syndrome will be untreatable and will remain with their child throughout life. The affected limb will always be smaller than a normal limb, and the affected fingers will be stiffer and smaller than normal. When these limitations have been accepted, a realistic treatment plan can be made.
The surgical reconstruction should be completed by the time the child is of school age. The optimum age for starting treatment depends on the type of deformity. For example, border digits need early separation; separation of the index and long fingers may be delayed. Generally, separation should begin in the first year of life, before abnormal functional patterns have developed and before deformity has progressed.
The webbed fingers can be separated by the standard syndactyly method. Because the fingers are always short, the setting back of the webs with a dorsal flap should be more proximal than in a normal full-sized hand. Caution is necessary: if the flap is inset too proximally, it will fold into a V-shaped wedge between the metacarpal heads, producing a very odd-looking hand.
Even though the syndactyly is simple, the neurovascular bifurcations are often relatively distal in these hands. The digital nerves can be easily separated more proximally, but the vessels are more of a problem. To ligate one vessel and free up the web space may be risky, and use of a short vascular graft may be a better alternative.
The thumb-index web space can be satisfactorily separated by a four-flap Z-plasty when the web is only moderately shallow. For more complete first-web syndactyly, in which the thumb lies adducted and supinated in the same plane as the fingers, a single large, dorsal rotation-flap technique gives a deep, durable web space. A rotational osteotomy of the metacarpal occasionally may be needed to provide pulp-to-pulp opposition. The parents must be told that follow-up will be necessary until the child attains skeletal maturity, since deepening of the webs may be required after the pubertal growth spurt.
The sequence of surgery in these hands depends on the severity of the anomalies. If all the fingers are to be saved, I start by separating the thumb from the index finger and the long from the ring finger, followed 6 months later by separation of the index from the long finger and the ring from the small finger. All the webs can thus be deepened in two operations. If construction of a three-fingered hand is anticipated, initial separation of the border digits is best. The three central digits can then function as a post until the surgeon has to select the digit for amputation. The selection depends not only on the deformity but also on the need for an adequate first web space to allow unhampered opposition and abduction of the thumb. There should be a period of 6 months between consecutive operations to allow scar tissue to mature and to provide time for digits deficient congenitally or from prior surgery to become revascularized. Figure 23 illustrates the sequential treatment of a 6-year-old boy with a typical left-sided Poland syndrome.
Figure 23.

Poland syndrome—operative treatment. (a, b) Before surgery, showing the hypoplasia. (c) Multiple dorsal rotation flaps have been used to release the thumb. (d) Final result after development of a three-fingered hand. Reprinted from Ireland DC et al, 1976, with permission from The Journal of Bone and Joint Surgery, Inc.
I have reviewed many of my patients a number of years after completion of surgery and feel that, although the end result is a small, somewhat stiff hand, it is certainly of increased functional value. The parents are uniformly pleased with the cosmetic improvement in the hand, and the children appreciate the upgrading of their affected extremity from merely an assisting hand to one with useful, independent function.
Footnotes
This article is an updated and abbreviated form of chapter 11, “Webbed Fingers” in The Care of Congenital Hand Anomalies, 2nd ed. St. Louis: Quality Medical Publishing, Inc., 1994:228–275. All figures were originally published in the chapter.
Selected bibliography
- 1.Apert E. De l'acrocephalosyndactylie. Bull Mem Soc Med Hop (Paris) 1906;23:1310–1330. [Google Scholar]
- 2.Bauer TB, Tondra JM, Trusler HM. Technical modification in repair of syndactylism. Plast Reconstr Surg. 1956;17:385–392. doi: 10.1097/00006534-195605000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Beals RK, Crawford S. Congenital absence of the pectoral muscles. A review of twenty-five patients. Clin Orthop. 1976;119:166–171. [PubMed] [Google Scholar]
- 4.Carpenter G. Two sisters showing malformations of the skull and other congenital abnormalities. Rep Soc Study Dis Child. 1900–1901;1:110–118. [Google Scholar]
- 5.Carpenter G. A case of acrocephaly, with other congenital malformations. Proc R Soc Med. 1909;II(part I):45–53. doi: 10.1177/003591570900201418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clarkson P. Poland's syndactyly. Guys Hosp Rep. 1962;111:335–346. [PubMed] [Google Scholar]
- 7.Eaton CJ, Lister GD. Syndactyly. Hand Clin. 1990;6:555–575. [PubMed] [Google Scholar]
- 8.Flatt AE. Practical factors in the treatment of syndactyly. In: Littler JW, Cramer LM, Smith JW, editors. Symposium on Reconstructive Hand Surgery. St. Louis: CV Mosby; 1974. pp. 144–156. [Google Scholar]
- 9.Flatt AE. Problems in polydactyly. In: Cramer LM, Chase RA, editors. Symposium on the Hand. vol 3. St. Louis: CV Mosby; 1971. [Google Scholar]
- 10.Hoover GH, Flatt AE, Weiss MW. The hand and Apert's syndrome. J Bone Joint Surg Am. 1970;52:878–895. [PubMed] [Google Scholar]
- 11.Ireland DC, Takayama N, Flatt AE. Poland's syndrome: a review of forty-three cases. J Bone Joint Surg Am. 1976;58:52–58. [PubMed] [Google Scholar]
- 12.Losch GM, Duncker HR. Transactions of the International Society of Plastic Reconstructive Surgery, 5th Congress. North Ryde, Australia: Butterworth Pty Ltd; 1976. Acrosyndactylism; pp. 671–676. [Google Scholar]
- 13.Lundkvist L, Barfred T. A double pulp flap technique for creating nail-folds in syndactyly release. J Hand Surg [Br] 1991;16:32–34. doi: 10.1016/0266-7681(91)90123-6. [DOI] [PubMed] [Google Scholar]
- 14.McKusick VA. Mendelian Inheritance in Man: Catalogs of Autosomal Dominant, Autosomal Recessive and X-Linked Phenotypes. 10th ed. Baltimore: Johns Hopkins University Press; 1992. [Google Scholar]
- 15.Moss AL, Foucher G. Syndactyly: can web creep be avoided? J Hand Surg [Br] 1990;15:193–200. doi: 10.1016/0266-7681_90_90124-m. [DOI] [PubMed] [Google Scholar]
- 16.Patterson TJS. Congenital deformities of the hand. Hunterian lecture delivered at Royal College of Surgeons of England, London, April 1959.
- 17.Poland A. Deficiency of the pectoralis muscle. Guys Hosp Rep. 1841;6:191. [Google Scholar]
- 18.Raus EE. Repair of simple syndactylism in the healthy neo-newborn. Orthop Rev. 1984;13:498–502. [Google Scholar]
- 19.Ravitch MM. Poland's syndrome—a study of an eponym. Plast Reconstr Surg. 1977;59:508–512. [PubMed] [Google Scholar]
- 20.Saldino RM, Steinbach HL, Epstein CJ. Familial acrocephalosyndactyly (Pfeiffer syndrome) Am J Roentgenol Radium Ther Nucl Med. 1972;116:609–622. doi: 10.2214/ajr.116.3.609. [DOI] [PubMed] [Google Scholar]
- 21.Shewell PC, Nancarrow JD, Fatah F. Quantifying interdigital web morphology. J Hand Surg [Br] 1992;17:198–200. doi: 10.1016/0266-7681(92)90088-j. [DOI] [PubMed] [Google Scholar]
- 22.Sommerkamp TG, Ezaki M, Carter PR, Hentz VR. The pulp plasty: a composite graft for complete syndactyly fingertip separations. J Hand Surg [Am] 1992;17:15–20. doi: 10.1016/0363-5023(92)90105-x. [DOI] [PubMed] [Google Scholar]
- 23.Sugiura Y. Poland's syndrome: clinicoroentgenographic study on 45 cases. Cong Anom. 1976;16:17–28. [Google Scholar]
- 24.Temtamy SA. Carpenter's syndrome: acrocephalopolysyndactyly. An autosomal recessive syndrome. J Pediatr. 1966;69:111–120. doi: 10.1016/s0022-3476(66)80368-2. [DOI] [PubMed] [Google Scholar]
- 25.Toledo LC, Ger E. Evaluation of the operative treatment of syndactyly. J Hand Surg [Am] 1979;4:556–564. doi: 10.1016/s0363-5023(79)80009-x. [DOI] [PubMed] [Google Scholar]
- 26.Upton J. Syndactyly. In: May JW, Littler JW, editors. Plastic Surgery. vol 8. Philadelphia: WB Saunders; 1990. pp. 5279–5293. [Google Scholar]
- 27.Walsh RJ. Acrosyndactyly. A study of twenty-seven patients. Clin Orthop. 1970;71:99–111. [PubMed] [Google Scholar]
- 28.Wilson MR, Louis DS, Stevenson TR. Poland's syndrome: variable expression and associated anomalies. J Hand Surg [Am] 1988;13:880–882. doi: 10.1016/0363-5023(88)90264-x. [DOI] [PubMed] [Google Scholar]
- 29.Wood VE. Duplication of the index finger. J Bone Joint Surg Am. 1970;52:569–573. [PubMed] [Google Scholar]
- 30.Wood VE. The treatment of central polydactyly. Clin Orthop. 1971;74:196–205. [PubMed] [Google Scholar]
- 31.Woolf CM, Woolf RM. A genetic study of syndactyly in Utah. Soc Biol. 1973;20:335–346. doi: 10.1080/19485565.1973.9988062. [DOI] [PubMed] [Google Scholar]