Fatigue is a timely topic—for society as well as health care. In health care, most of the discussion of fatigue has focused on work hours. Surveys conducted over the past 20 years have shown that interns work more hours than residents, and surgical subspecialists tend to put in the most hours. The range is 35 to 120 hours a week, with an average of 60 to 90 work hours a week. Most survey respondents believe that long hours negatively impact patient care and safety.
Curtailing resident work hours has had both advocates and critics. On the one hand, most agree that long hours offer a valuable educational experience: residents can see the evolution of disease, retain continuity of patient care, and have adequate time to learn the profession. Rigorous schedules can also build confidence and prepare young physicians for the demands of practice. The arduous training schedule is also seen as a rite of passage and most importantly saves money for teaching hospitals.
On the other hand, scientific evidence has shown that fatigue affects performance (Table 1). Brief moments of sleep may intrude into wakefulness, so that the physician actually sleeps during patient care. In addition, fatigue may cause physicians to injure themselves—either at the hospital or on the drive home—and may expose the hospital or educational entity to litigation. Lack of sleep also affects mood: negative moods—such as anger, hostility, depression, confusion, tension, and sadness—increase, while positive moods such as vigor and happiness decrease. Such negative moods are bound to affect the quality of patient care.
Table 1.
The effects of fatigue on performance
| • Cognitive slowing |
| • More variable performance |
| • Neglect of nonessential activities |
| • Decrease in learning |
| • Decay in problem solving |
| • Impaired memory |
| • Decline in motivation |
The Accreditation Council for Graduate Medical Education now limits resident work hours to 80 per week—10% more if the program gets a dispensation. In comparison, residents in the United Kingdom work about 50 hours a week. As with any complex system, it is likely that changing the scheduling of residents will have unintended and unforeseen consequences, both good and bad. Someone has to pick up the slack since patients will continue to be ill, and those who do so may be less tolerant of sleep deprivation. In the future, regulations may be developed for all physicians and not just those in training.
Yet limitations on work hours may never be enough. In its large national surveys, the National Sleep Foundation found that we are a society of chronic undersleepers. Because of the many competing interests in our 24/7 world, a physician working 20 hours a week may still come to work fatigued. A culture change is required: it should be unacceptable to come to work impaired from any cause.
Fatigue has also become an issue in relation to patient safety. The Institute of Medicine report To Err Is Human revealed that medical errors cause 44,000 to 98,000 deaths a year. While caveats exist in the interpretation of the data, the number is irrefutably large: in fact, it is equivalent to a jumbo jet crashing daily. It is hard to know fatigue's role in these errors. However, since fatigue affects performance and decision-making processes, it is a likely contributor.
Fatigue has already been shown to be a contributing factor in non—health care accidents, including the explosion of the Space Shuttle Challenger and the nuclear meltdowns at Three Mile Island and Chernobyl (both of which occurred during the circadian low point between 3:00 and 5:00 AM). Fatigue was found to be the probable cause of the grounding of the Exxon Valdez. Each year, more automobile crashes are related to drowsy driving than to driving while under the influence of alcohol. In June 2003, New Jersey state lawmakers passed Maggie's Law, which allows a sleep-deprived driver to be convicted of vehicular homicide. Thus, compared with the safety culture in transporta-tion industries, health care is still in its infancy when evaluating safety and errors.
In this article, I review sleep physiology, discuss some relevant studies on sleep in a health care environment, and present recommendations to help counter the effects of fatigue.
SLEEP PHYSIOLOGY
Sleep is an active biological state. Sleepers are reversibly disengaged from the world; no information is coming in and no information is going out. Just as when people don't eat they become hungry and when they don't drink they become thirsty, when they don't sleep they become sleepy. It is an essential restorative drive state that is regulated by an internal clock, and it occupies one third of our existence.
Sleep consists of four stages of non—rapid-eye-movement (NREM) sleep and REM sleep. In NREM stage 1, people pass from relaxed wakeful-ness (alpha-type electroencephalogram [EEG] activity) to a slower rhythm, or theta type of activity. In NREM stage 2, special types of EEG phenomena called K complexes and sleep spindles are superimposed on theta activity. In NREM stages 3 and 4 sleep, the EEG continues to slow to what is called delta activity. This is where mental and physical processes slow and physical restoration occurs. In REM sleep, the brain is active; the sleeper is dreaming in a paralyzed body since skeletal muscle is quiescent. This stage of sleep is associated with mental restoration. The EEG of REM sleep is similar to the EEC of wakefulness, except for the right and left oculogram channels, which show rapid eye movements. Sleepers cycle in and out through these stages every 90 to 120 minutes; most slow-wave sleep occupies the early portion of the night, and most REM sleep comes at the end of the night (Figure 1). Those who are sleep deprived preferentially recover slow-wave sleep first, so teleologically slow-wave sleep is more important.
Figure 1.
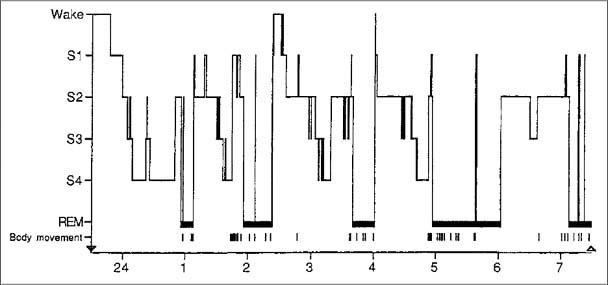
A histogram demonstrating a normal sleep pattern for a young adult. REM indicates rapid eye movement. Reprinted from Principles and Practice of Sleep Medicine (reference 1) with permission from Elsevier.
The average adult requires over 8 hours of sleep each night. While sleep need varies among individuals, it is genetically determined, does not change with age, and cannot be trained. Many physicians believe that they can change this basic element of functioning through motivation. Perhaps a quick adrenaline rush in emergencies briefly helps alertness, but that doesn't change the underlying physiology.
Daytime sleepiness has two physiologic determinants. The first is sleep homeostasis, or sleep balance. When the quality or quantity of sleep in prior nights has been inadequate, our body seeks to make up for that, and thus we become sleepy. Sleep quality is affected by interruptions from beepers, sick children, or other health factors such as obstructive sleep apnea. The second determinant is the circadian rhythm of alertness. Circadian low points occur from 2:00 to 6:00 AM and, to a lesser extent, from 2:00 to 6:00 PM. Typically we have a sleep debt, so sleepiness often becomes manifest in the afternoons. The circadian clock is very resistant to change. When flying across time zones, we get jet lag; similarly, shift work is made very difficult because of our circadian clock. Humans are animals that are programmed to be asleep at night and awake during the day. The invention of the light bulb allowed for extension of work periods but has been around only since the late 1800s, and our biology has not changed that fast.
While sleep need does not change with age, the amount and structure of sleep change significantly. By the age of 50, slow-wave sleep is essentially gone, and the ability to gain restorative sleep is dissipated. The process begins as early as age 25. Sleep becomes more disrupted for various reasons so that total nighttime sleep decreases. People will compensate, if allowed, by taking daytime naps, or they manifest sleepiness during the day.
In our society, few people—and certainly few physicians—get ≥8 hours of sleep daily, so the sleep loss accumulates and becomes a sleep debt. The only way to repay a sleep debt is by getting adequate sleep. Fortunately, the debt does not require an hour-per-hour payback. Most people can restore their functions by sleeping adequately on their days off.
STUDIES ON FATIGUE
Just how sleepy are our residents? In 2002, my research group evaluated physiologic and subjective sleepiness in a within-subject study of 11 anesthesiology residents (2). Sleep studies were conducted at baseline, when the residents had not been on call for the previous 48 hours; after call in the intensive care unit or obstetric anesthesia, typically the busiest services; and after 4 consecutive days of extended sleep, when they were allowed to report to work at 10:00 AM. The average amount of sleep in the three groups was 6.7 hours, 5.2 hours (range 0–9 hours), and 8.8 hours, respectively. The Multiple Sleep Latency Test (MSLT), a standard measure of daytime sleepiness, was used to measure physiologic sleepiness. Falling asleep in <5 minutes is considered pathologic daytime sleepiness; that result is seen with patients with obstructive sleep apnea and narcolepsy, as well as in normal people who are sleep deprived. MSLT scores were 6.7 minutes in the baseline group and 4.9 minutes in the postcall group, compared with 12 minutes in the extended-sleep group (P = 0.0001) (Figure 2). Daytime sleepiness in the postcall group was not surprising. However, it was surprising that the baseline group (averaging almost 7 hours of sleep per night) was also very sleepy, with scores that were not statistically distinguishable from those of the postcall group. Importantly, this group was able to “normalize” levels of daytime alertness by prioritizing (extending) sleep.
Figure 2.
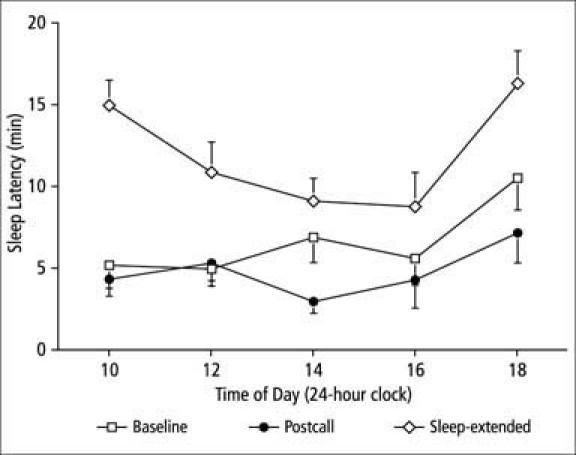
Physiologic sleepiness (sleep latency) as a function of condition and time of day. The 11 residents in the study had sleep latencies nearly at levels associated with clinical sleep disorders (<5 minutes) in the baseline condition and below these levels in the postcall condition. No specific circadian-rhythm effect was evident in these conditions. In the sleep-extended condition, the sleep latencies were normal and showed a typical circadian rhythm effect. Error bars are standard error of the mean. Reproduced with permission from Academic Medicine (reference 2).
When we asked subjects if they thought they had fallen asleep during the MSLT, only half gave the answer that corresponded with the EEG data. Among those who thought they had stayed awake, 68% were wrong. These findings have been reproduced elsewhere and raise important concerns in the complex environment of health care. Individuals have little ability to determine how sleepy they are or if they have fallen asleep. This may make them more likely to perform a critical task when they are not prepared or less likely to use a countermeasure strategy to improve alertness.
Health care workers need to begin to think of coming to work impaired by chronic sleep deprivation as similar to coming to work impaired by alcohol. Studies reveal that as ethanol and sleep loss increase, psychomotor performance decreases and memory is impaired. A 2-hour sleep loss is equivalent to a 0.045% breath-alcohol concentration, and a 4-hour sleep loss is equivalent to a 0.095% breath-alcohol concentration (3)—above Texas' legal limit of 0.08%.
So does the impairment affect performance? We used to be able to state that no conclusive evidence proved that physician work hours were unsafe. That may be changing. In October 2004, one of the nation's top sleep medicine laboratories and patient safety research groups published a prospective, randomized study examining whether intern work hours correlated with the number of medical errors. In the traditional-schedule group, interns were on call every third night, working 24 hours or more. In the intervention group, interns worked no extended shifts (>17 hours) and averaged 65 work hours each week. Besides having about 6 hours less sleep each week and twice the number of attentional failures (EEG evidence of severe drowsiness), the traditional-schedule group made 36% more serious medical errors than the intervention group (4).
A study published in the Lancet examined the effect of sleep deprivation on surgical manual dexterity in a Latin square design (5). Surgical skills were tested with a laparoscopic surgery simulator in six residents under three conditions: an undisturbed night of sleep, a night on call with three disturbances, and a night with no sleep. The study reported that surgeons who had not slept made 20% more errors and took 14% longer to complete the tasks than those who had a full night's sleep.
My research team studied the performance of anesthesiology residents in a sleep-deprived versus a sleep-extended condition using a patient simulator (6). The sleep-deprived group had been awake for 25 straight hours. In the sleep-extended condition, subjects were told to prioritize their nocturnal sleep and to report to work at 10:00 AM for 4 consecutive days. During a 4-hour simulated laparoscopic procedure, their response to probes and their behavioral alertness were evaluated. The simulator environment uses standard anesthesia equipment and a plastic computer-driven simulator as the patient. The simulator environment for the experiment was made intentionally soporific, with soft lighting (they were laparoscopic cases) and either classical music or no music.
Three types of probes were used: 1) a vigilance light next to a physiologic monitor; 2) a probe indicating dropout of an arterial line; and 3) a change in blood pressure or heart rate above or below the threshold value in an embedded probe. Subjects were given 3 minutes to verbally respond to each probe. Results showed that sleep-deprived subjects had longer latencies for all probe types (Figure 3). They missed some probes completely due to sleeping. Further, the responses were highly variable in the sleep-deprived group. One moment, the subject was performing adequately, and the next moment he or she was sleeping. Performance was much less variable when subjects were rested.
Figure 3.
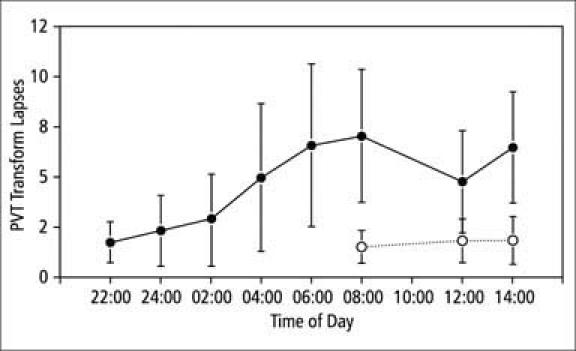
Psychomotor vigilance task “transform lapses,” √lapses + √(lapses + 1), as a function of condition (sleep-deprived condition =•; sleep-extended condition = O) and time of day. By convention, a lapse is a reaction time >500 ms. Residents had significantly more lapses (F = 25.4; P = 0.0004) and greater variability of performance in the sleep-deprived condition than in the sleep-extended condition. The worst performance occurred at the 08:00 trial in the sleep-deprived condition. Error bars show standard error of the mean (n = 12). Reproduced from Anesthesiology (reference 6) with permission of the American Society of Anesthesiologists.
While the subjects maintained their performance better than expected—which is a testimony to humans—they displayed many sleepy behaviors. We videotaped subjects and counted the number of behaviors that were unequivocally sleepy behaviors (i.e., we counted nodding and eye closing but did not count rolling eye movements). Results showed that some subjects spent large amounts of time very sleepy (one subject spent a third of the time of the operation displaying sleepy behaviors), while others never showed such behaviors (Table 2).
Table 2.
Time spent by sleep-deprived anesthesiology residents in sleepy behaviors during a 4-hour simulated laparoscopic operation*
| Subject | (Minutes (% time of entire operation) |
| 4 | 77.7 (32.4%) |
| 12 | 60.2 (25.1%) |
| 6 | 26.7 (11.1%) |
| 9 | 12.5 (5.2%) |
| 7 | 11.4 (4.8%) |
| 5 | 6.6 (2.8%) |
| 3 | 3.1 (1.3%) |
| 11 | 2.1 (0.9%) |
| 2 | 0 |
| 8 | 0 |
| 10 | 0 |
*“Sleepy behaviors” are defined as nodding and eyes closing (awakened head bob); nodding and eyes closing (not awakened); or eyes closed with no movement (sound asleep). Data from reference 6.
Sleep studies are difficult to do in a clinical environment. That is one reason for the small number of subjects in each study. It is clear, however, that the need for sleep affects us regardless of how professional we are. Gender, race, and specialty do not matter. Thus, it becomes important to address this problem.
FATIGUE COUNTERMEASURES
There is no magic bullet to cure the epidemic of fatigue among physicians or in our society. The solution has to do with more than just work hours; a comprehensive fatigue management plan is required.
Optimize scheduling
Much can be said about optimal scheduling and rostering. Health care can learn from industries such as aviation, trucking, and rail transportation. Optimal schedules can be developed using circadian principles and scientific evidence. The evidence shows, for example, that wake periods should not exceed 17 hours, especially for those working the night shift. Rest periods need to be at least 10 hours to protect the type of sleep that allows optimal recovery. Studies also show that those working the night shift end up with less sleep. Getting at least one full day off a week is a physiologically based need. Beyond these organizational changes, each individual can use a variety of strategies.
Improve sleep habits
The bottom line is that we all need more sleep and must get more sleep. It is helpful to keep a regular bedtime and wakeup time and to associate the bedroom with sleep. Mental relaxation techniques are helpful, particularly when we are on call and have an opportunity to sleep. Alcohol, caffeine, and nicotine must be managed because they impact our ability to gain adequate sleep. Regular exercise is important as well, but rigorous exercise should be done at least 3 hours before sleep because it inhibits the sleep initiation process. We should also take advantage of days off to catch up on sleep.
Make use of naps
“Presleep” focuses on minimizing the sleep debt before starting a work period. While napping has been shown to improve alertness and performance, it is not always viewed favorably in our culture. The military has referred to naps as “power naps” in an attempt to change this negative connotation. Although certain practice situations aren't amenable to naps, napping is workable in many cases. In a care team approach, team members can relieve each other to nap.
Based on sleep cycles, the optimal length is 45 minutes for a short nap and 2 hours for a long nap. In contrast, being awakened during slow-wave sleep may lead to sleep inertia—a feeling of grogginess, disorientation, and cognitive impairment that leaves us performing worse than before we took the nap. Slow-wave sleep can occur within 45 minutes of sleep onset and can last for up to 90 minutes. This concept is important for health care, because we never know when a trauma call will interrupt our sleep.
Use stimulants strategically
Caffeine is the most abused drug in the world. In the USA, 100 million coffee drinkers support a $20 billion per year industry. Coffee is used daily by 54% of the adult population; the average amount consumed is 3 cups per day. Caffeine is also found in tea, soda, and chocolate. Its onset time is 15 to 30 minutes, and it is effective for 3 to 4 hours. Yet, studies show that a constant dose of caffeine has minimal effects. The use of caffeine must be timed to boost alertness—for example, before the circadian low point. Caffeine should be avoided before sleep.
The alertness-promoting drug modafinil has been approved for narcolepsy. In January 2004, it was also approved for use in obstructive sleep apnea and shift work sleep disorder. It is a non-amphetamine and appears to have few side effects. Long-term effects are still unclear. The military is using it—and so are residents and shift workers in health care. The demand for this drug and its potential revenue are high because no one wants to be impaired by sleep deprivation and fatigue in our 24/7 society. The avail-ability of this drug raises important questions. Which is worse: to take drugs to alter our alertness or to be sleep impaired?
Interact socially
Since social interaction and activity breaks increase alertness and decrease sleepiness, we can force ourselves to interact socially when we're fatigued. Even standing up will help prevent falling asleep.
Make use of light therapy
Light has important alerting effects. When it is correctly timed, it can help alter the circadian clock. The use of light therapy in operational environments is being studied.
CONCLUSION
Only so much can be done to manage fatigue at an organizational or societal level. Regardless of what is known scientifically and operationally, the personal behavior of others cannot be controlled—even when schedule and work hours are regulated. Thus, each of us has to take personal responsibility to come to work prepared—not impaired. We need to keep in mind that being impaired by fatigue tends to be the norm; we don't always recognize when we are impaired. Thus, we need to be especially vigilant. The effects of fatigue can only be countered when we recognize their importance.
Acknowledgments
I thank my colleagues, particularly my mentors, David M. Gaba, MD, and Mark R. Rosekind, PhD, who have been involved in this research. I also acknowledge the support and collaboration of Rebecca Smith-Coggins, MD, and the NASA Ames Fatigue Countermeasure Program. Funding sources include the Office of Technology Licensing at Stanford, the Veterans Affairs Patient Safety Center of Inquiry Program, and the Anesthesia Patient Safety Foundation.
References
- 1.Carskadon MA, Dement WC. Kryger MH, Roth T, Dement WC. Principles and Practice of Sleep Medicine. 3rd ed. Philadelphia: WB Saunders; 2000. Norman human sleep: an overview; pp. 15–25. [Google Scholar]
- 2.Howard SK, Gaba DM, Rosekind MR, Zarcone VP. The risks and implications of excessive daytime sleepiness in resident physicians. Acad Med. 2002;77:1019–1025. doi: 10.1097/00001888-200210000-00015. [DOI] [PubMed] [Google Scholar]
- 3.Roehrs T, Burduvali E, Bonahoom A, Drake C, Roth T. Ethanol and sleep loss: a “dose” comparison of impairing effects. Sleep. 2003;26:981–985. doi: 10.1093/sleep/26.8.981. [DOI] [PubMed] [Google Scholar]
- 4.Landrigan CP, Rothschild JM, Cronin JW, Kaushal R, Burdick E, Katz JT, Lilly CM, Stone PH, Lockley SW, Bates DW, Czeisler CA. Effect of reducing interns' work hours on serious medical errors in intensive care units. N Engl J Med. 2004;351:1838–1848. doi: 10.1056/NEJMoa041406. [DOI] [PubMed] [Google Scholar]
- 5.Taffinder NJ, McManus IC, Gul Y, Russell RC, Darzi A. Effect of sleep depriva tion on surgeons' dexterity on laparoscopy simulator. Lancet. 1998;352:1191. doi: 10.1016/s0140-6736(98)00034-8. [DOI] [PubMed] [Google Scholar]
- 6.Howard SK, Gaba DM, Smith BE, Weinger MB, Herndon C, Keshavacharya S, Rosekind MR. Simulation study of rested versus sleep-deprived anesthesiologists. Anesthesiology. 2003;98:1345–1355. doi: 10.1097/00000542-200306000-00008. [DOI] [PubMed] [Google Scholar]


