Abstract
Objectives: This is an annual report indicating the number and early clinical results of annual vascular treatment performed by vascular surgeons in Japan in 2019, as analyzed by database management committee (DBC) members of the JSVS.
Materials and Methods: To survey the current status of vascular treatments performed by vascular surgeons in Japan, the DBC members of the JSVS analyzed the vascular treatment data provided by the National Clinical Database (NCD), including the number of treatments and early results such as operative and hospital mortality.
Results: In total 154,460 vascular treatments were registered by 1,082 institutions in 2019. This database is composed of 7 fields including treatment of aneurysms, chronic arterial occlusive disease, acute arterial occlusive disease, vascular injury, complication of previous vascular reconstruction, venous diseases, and other vascular treatments. The number of vascular treatments in each field was 23,826, 17,100, 4,947, 2,369, 674, 54,023, and 51,521, respectively. In the field of aneurysm treatment, 20,369 cases of abdominal aortic aneurysm (AAA) including common iliac aneurysm were registered, and 63.3% were treated by endovascular aneurysm repair (EVAR). Among AAA cases, 1,739 (8.5%) cases were registered as ruptured AAA. The operative mortality rates of ruptured and un-ruptured AAA were 15.0%, and 0.6%, respectively. 43.8% of ruptured AAA were treated by EVAR, and the EVAR ratio was gradually increasing, but the operative mortality rates of open repair and EVAR for ruptured AAA were 12.6%, and 15.4%, respectively. Regarding chronic arterial occlusive disease, open repair was performed in 8,026 cases, including 1,250 distal bypasses to the crural or pedal artery, whereas endovascular treatment (EVT) was performed in 8,879 cases. The EVT ratio was gradually increased at 51.9%. Varicose vein treatment was decreased in 42,313 cases (1.9% less than in 2018), and 79.8% of the cases were treated by endovenous thermal ablation (ETA) including endovenous laser ablation (EVLA) and radio-frequency ablation (RFA). Regarding other vascular operations, 47,605 cases of vascular access operations and 1,703 lower limb amputation surgeries were included.
Conclusions: The number of vascular treatments increased since 2011, and the proportion of endovascular procedures increased in almost all fields of vascular diseases, especially EVAR for AAA, EVT for chronic arterial occlusive disease, and ETA for varicose veins. (This is a translation of Jpn J Vasc Surg 2024; 33: 307–335.)
Keywords: peripheral arterial disease, stent graft, endovascular treatment, aneurysm, venous surgery
Introduction
Following the launch of the National Clinical Database (NCD) and initiation of surgical case registration in 2011, the Japanese Society for Vascular Surgery has been compiling vascular surgery cases from NCD-registered cases and publishing an annual report on vascular surgery as an academic meeting.1–14) This paper presents the results of the vascular surgery cases registered in NCD from January 2019 to December 2019, which were tabulated and analyzed by the members of the Database Management and Steering Committee of the Japanese Society for Vascular Surgery.
Methods
The vascular surgery data extracted from the surgical procedures registered with NCD in 2019, at the request of the Japanese Society for Vascular Surgery (member society of NCD), were classified into the following 7 categories: (1) revascularization for aneurysms, (2) revascularization for chronic arterial occlusive disease, (3) revascularization for acute arterial occlusive disease, (4) treatment of vascular trauma, (5) surgery for complications of revascularization, (6) venous surgery, and (7) other vascular diseases and related surgeries. Tabulated data were reviewed by members of the Japanese Society for Vascular Surgery Database Management Steering Committee, and tabulated results were analyzed.
The compiled results included the number of surgical procedures performed, etiology of conditions treated, number of operative and in-hospital deaths, and materials used. Operative death, synonymous with surgical death, refers to any death that occurs within 30 days following surgery, irrespective of the cause or patient’s hospitalization status. In-hospital deaths are defined as those occurring during the period of continuous hospitalization after surgery, regardless of the duration of the stay.
For data on etiology and materials used, there were some discrepancies in the values presented in tables, such as the data sum was inconsistent with the total number of cases. After careful investigation by the Committee and NCD, it was concluded that the discrepancies were due to one of the following 5 reasons: (1) selection of multiple choices was permitted, (2) blank choices were permitted, (3) omissions or incorrect entries made by the data entry person, (4) use of multiple materials in a single procedure or treatment involving multiple sites, and (5) inadequate item expansion conditions. Since 2013, we have implemented measures to viably minimize input errors. These measures include reorganizing existing options, introducing new ones, and programming the system to prevent the registration of incomplete items for fields where leaving them blank would make registration impossible.
Table 1 shows the items for which the registration and tabulation methods have changed since 2017.
Table 1 Major changes in the 2019 annual report.
| Item | Change details |
|---|---|
| Thoracic aortic aneurysm (ascending, arch, descending) | Unified registration with JCVSD |
| Thoracoabdominal aortic aneurysm | If "Thoracoabdominal" is selected under "Site of aortic aneurysm," the thoracoabdominal registry will be shown |
| Arterial occlusive diseases | The input was to be made for both sides or for each of the left and right sides |
| Venous surgery | The input was to be made for both sides or for each of the left and right sides |
Tabulation and Analysis Results
The total number of vascular surgeries registered with NCD in 2019 was 154,460 (a 7.5% increase from the previous year), accounting for 9.9% of the total number of surgical procedures (1,558,465) registered with NCD in the same year (9.4% in the previous year). Moreover, 1,082 institutions registered vascular surgery, which represented 28.1% of the 3,854 institutions registering surgeries. Of these 1,082 institutions, 517 (46.8%) were certified cardiovascular surgery training facilities (as of 2019). However, the total number of certified cardiovascular surgery training facilities was 544, and 95% (517/544) of these institutions registered data for vascular surgery. The tabulated and analytical results for 2019 are explained below by category.
1. Treatment for Aneurysms (Tables 2-1 and 2-2)
Table 2 Treatment for aneurysm: Table 2-1 Aortic aneurysm.
| Region of aortic aneurysm | Cases | Gender | Mortality | Ruptured aneurysm | Dissectionc | Etiology | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | 30-day death | In-hospital death | Cases | 30-day death | In-hospital death | Degeneratived | Inflammatory | Vasculitis | Infected | Connective tissue diseasee | Others | |||||
| Cases | 30-day death | In-hospital death | |||||||||||||||
| Thoracoabdominal aortaa | 177 | 137 | 40 | 9 | 11 | 21 | 5 | 7 | 51 | 160 | 9 | 10 | 1 | 0 | 5 | 2 | 9 |
| Abdominal aortic aneurysmb | 20,369 | 16,813 | 3,556 | 370 | 487 | 1,739 | 261 | 327 | 928 | 19,621 | 345 | 436 | 213 | 12 | 255 | 31 | 237 |
| With renal artery reconstruction | 372 | 306 | 66 | 9 | 16 | 31 | 4 | 9 | 33 | 358 | 9 | 15 | 3 | 0 | 5 | 1 | 5 |
| With renal artery clamping | 1,439 | 1,221 | 218 | 51 | 72 | 192 | 33 | 44 | 82 | 1,356 | 45 | 61 | 36 | 0 | 29 | 4 | 14 |
| With internal iliac artery aneurysm | 879 | 771 | 108 | 20 | 23 | 85 | 13 | 13 | 48 | 847 | 19 | 22 | 8 | 1 | 15 | 1 | 7 |
| With internal iliac artery reconstruction | 1,360 | 1,214 | 146 | 13 | 17 | 78 | 9 | 9 | 91 | 1,312 | 12 | 16 | 13 | 0 | 11 | 9 | 15 |
| Simultaneous thoracic aortic surgery | 178 | 136 | 42 | 15 | 18 | 18 | 8 | 9 | 50 | 162 | 15 | 18 | 2 | 1 | 1 | 2 | 10 |
Table 2-1 Aortic aneurysm (continued).
| Region of aortic aneurysm | Treatment procedure | Graft materialsg | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Replacement | Exclusion with bypass | Stent graft | Hybridf | Polyester | ePTFE | Others | |||
| Cases | Bifurcated-graft | Straight-graft | |||||||
| Thoracoabdominal aortaa | 4 | 3 | 0 | 1 | 115 | 6 | 47 | 8 | 0 |
| Abdominal aortic aneurysmb | 6,936 | 5,577 | 992 | 38 | 12,846 | 47 | 6,566 | 433 | 60 |
| With renal artery reconstruction | 342 | 265 | 54 | 5 | 12 | 4 | 326 | 30 | 6 |
| With renal artery clamping | 1,416 | 1,124 | 243 | 2 | 7 | 4 | 1,329 | 91 | 10 |
| With internal iliac artery aneurysm | 786 | 623 | 36 | 2 | 17 | 13 | 730 | 57 | 8 |
| With internal iliac artery reconstruction | 1,303 | 999 | 54 | 3 | 23 | 20 | 1,231 | 79 | 20 |
| Simultaneous thoracic aortic surgery | 11 | 9 | 0 | 5 | 112 | 2 | 34 | 13 | 3 |
a: These data are not including cases recorded in JCVSD Database in which most cardiac surgeons were entering their cases.
b: Including common iliac artery aneurysm.
c: Including both acute and chronic aortic dissection.
d: Most likely atherosclerosis.
e: Connective tissue abnormalities such as Marfan syndrome.
f: Debranch bypass surgery combined with two staged TEVAR is counted as one case of hybrid treatment.
g: Only for open surgery.
Table 2-2 Abdominal aortic aneurysm mortality classified by treatment procedures.
| Procedure for aneurysm repair | Ruptured aneurysm | Non-ruptured aneurysm | ||||
|---|---|---|---|---|---|---|
| Cases | 30-day death | In-hospital death | Cases | 30-day death | In-hospital death | |
| Replacement | 911 | 115 | 144 | 6,025 | 53 | 82 |
| Exclusion with bypass | 11 | 0 | 5 | 27 | 1 | 1 |
| EVAR | 742 | 113 | 141 | 11,732 | 43 | 62 |
| EVAR with branch chimney | 17 | 3 | 4 | 187 | 4 | 5 |
| Fenestrated/branched EVAR | 0 | 0 | 0 | 168 | 1 | 1 |
| Hybrid | 3 | 1 | 1 | 44 | 0 | 0 |
EVAR: endovascular aneurysm repair
1) Thoracic aortic aneurysm
In consultation with the Japanese Cardiovascular Surgery Database (JCVSD), it was decided that from 2019, surgeries for thoracic aortic aneurysm, including thoracic endovascular aortic repair (TEVAR), performed by vascular surgeons will be registered in JCVSD. Only surgeries for thoracoabdominal aortic aneurysms performed by vascular surgeons will be registered in NCD.
2) Abdominal aortic aneurysm (Tables 2-1 and 2-2)
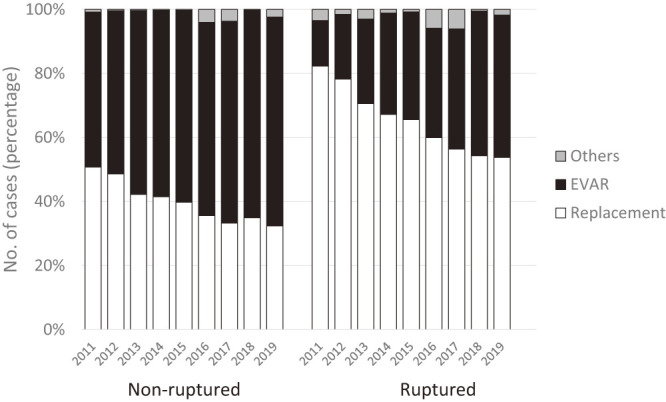
The total number of surgeries for abdominal aortic aneurysms (including common iliac artery aneurysms) registered in NCD in 2019 was 20,369, showing a slight increase each year from 19,144 cases in 2016, 19,982 cases in 2017, and 20,160 cases in 2018. Of these, 6,936 (34.1%) were replacement surgeries, and 12,893 (63.3%) were stent graft endovascular repair (EVAR), including hybrids. The proportion of EVAR cases has continued to increase gradually since it exceeded 50% in 2013 (60.3% in 2016, 61.4% in 2017, and 61.6% in 2018). This trend can be attributed to the fact that EVAR has become the standard treatment for abdominal aortic aneurysms. Furthermore, the number of replacement procedures, which had been between 7,000 and 8,000 cases, declined slightly, falling below 7,000 cases (Fig. 1).
Fig. 1 Treatment procedure for non-ruptured and ruptured AAA. Comparing the year 2011–2018, the proportion of EVAR selection gradually increased in 2019. AAA: abdominal aortic aneurysm; EVAR: endovascular aneurysm repair.
Among the replacement procedures, 1,439 cases (20.7%) required renal artery clamping, and 372 cases (5.4%) required renal artery reconstruction. With the popularization of EVAR, the number of pararenal artery lesions requiring renal artery clamping has increased gradually from 17.6% in 2016 to 20.2% in 2017, and 19.1% in 2018, approximately 20% in 2019.
Regarding the treatment outcomes for non-ruptured AAAs, the operative and in-hospital mortality rates were 0.9% and 1.4%, respectively, for the replacement procedure, and 0.4% and 0.6%, respectively, for EVAR, including specialized and hybrid procedures (Fig. 2). In cases, requiring renal artery clamping, the mortality rates increased to 1.4% and 2.2%, respectively, and further increased to 1.5% and 2.1%, respectively, when reconstruction was performed.
Fig. 2 Early clinical results of non-ruptured AAA in the year 2011–2019. AAA: abdominal aortic aneurysm.

The number of surgeries for ruptured AAAs was 1,739 and was approximately 1,800 each year. The operative mortality rate was 15.0%, and the in-hospital mortality rate was 18.8%. For ruptured cases, the operative mortality rate was approximately 15%, and the in-hospital mortality rate was just under 20%, which was similar to the results in recent years. EVAR was performed in 762 cases (43.8%), and although there was an increasing trend, the proportion of EVAR for ruptured cases was similar to that in 2018 (35.9% in 2016, 37.9% in 2017, and 43.3% in 2018) (Fig. 1). The operative and in-hospital mortality rates for ruptured cases were 15.4% and 19.2%, respectively, which are similar to the results from recent years: 2016 (15.3% and 18.8%, respectively), 2017 (12.3% and 15.8%, respectively), and 2018 (14.6% and 16.4%, respectively). Despite the increasing number of ruptured EVARs, the outcome has remained stable. This may be due to the increasing experience with EVAR at each institution and the accumulation of experience with EVAR for ruptured cases. Although patient selection bias must be considered (as EVAR is generally performed in anatomically more favorable patients), the results were comparable to those of replacement surgery, which had operative and in-hospital mortality rates of 12.6% and 15.8%, respectively (Fig. 3).
Fig. 3 Early clinical results of ruptured AAA in the year 2011–2019. AAA: abdominal aortic aneurysm.

3) Peripheral aneurysm (Tables 2-3 and 2-4)
Table 2-3 Peripheral artery aneurysm.
| Aneurysm | Cases | Gender | Mortality | Ruptured aneurysm | Etiology | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | 30-day death | In-hospital death | Cases | 30-day death | In-hospial death | Degenerative | Vasculitisa | Takayasu arteritis | Connective tissue diseaseb | Infected | Traumas | Others | ||
| Aortic arch branches | |||||||||||||||
| Carotid | 13 | 12 | 1 | 0 | 0 | 2 | 0 | 0 | 3 | 0 | 0 | 1 | 2 | 1 | 6 |
| Vertebral | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Subclavian | 60 | 41 | 19 | 1 | 4 | 7 | 1 | 2 | 41 | 1 | 0 | 3 | 5 | 3 | 7 |
| Multiple in arch branches | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Others | 20 | 14 | 6 | 0 | 0 | 2 | 0 | 0 | 9 | 0 | 1 | 1 | 0 | 2 | 7 |
| Upper limb artery | |||||||||||||||
| Axillary | 26 | 19 | 7 | 1 | 1 | 3 | 1 | 1 | 22 | 0 | 0 | 1 | 2 | 1 | 0 |
| Brachial | 181 | 111 | 70 | 5 | 5 | 30 | 3 | 2 | 55 | 1 | 0 | 0 | 19 | 42 | 64 |
| Forearm-hand | 122 | 67 | 55 | 2 | 4 | 18 | 0 | 0 | 46 | 1 | 0 | 0 | 16 | 27 | 32 |
| Others | 20 | 14 | 6 | 0 | 0 | 2 | 0 | 0 | 10 | 0 | 0 | 0 | 1 | 2 | 7 |
| Visceral artery | |||||||||||||||
| Celiac | 27 | 22 | 5 | 1 | 1 | 5 | 1 | 1 | 18 | 1 | 0 | 0 | 1 | 0 | 7 |
| Hepatic | 15 | 11 | 4 | 1 | 1 | 4 | 1 | 1 | 10 | 0 | 0 | 0 | 1 | 0 | 4 |
| Splenic | 93 | 45 | 48 | 0 | 1 | 5 | 0 | 1 | 87 | 0 | 0 | 1 | 1 | 0 | 4 |
| Superior mesenteric | 41 | 32 | 9 | 3 | 3 | 6 | 1 | 1 | 25 | 0 | 1 | 1 | 8 | 3 | 3 |
| Renal | 90 | 63 | 27 | 1 | 1 | 12 | 1 | 1 | 75 | 1 | 0 | 0 | 1 | 2 | 11 |
| Others | 122 | 100 | 22 | 2 | 2 | 16 | 1 | 1 | 102 | 1 | 0 | 2 | 4 | 2 | 11 |
| Lower limb artery | |||||||||||||||
| External iliac | 204 | 171 | 33 | 5 | 9 | 28 | 4 | 7 | 159 | 1 | 1 | 1 | 13 | 5 | 24 |
| Internal iliac | 1,493 | 1,274 | 219 | 24 | 31 | 111 | 15 | 19 | 1,448 | 4 | 1 | 3 | 15 | 0 | 22 |
| Femoral | 470 | 367 | 103 | 15 | 18 | 97 | 9 | 9 | 214 | 3 | 0 | 0 | 58 | 69 | 126 |
| Popliteal | 269 | 209 | 60 | 1 | 0 | 14 | 0 | 0 | 240 | 3 | 0 | 0 | 7 | 3 | 16 |
| Others | 55 | 34 | 21 | 0 | 1 | 7 | 0 | 1 | 25 | 0 | 0 | 0 | 2 | 12 | 16 |
| Total | 3,166 | 2,468 | 698 | 60 | 79 | 354 | 36 | 45 | 2,453 | 16 | 3 | 12 | 153 | 173 | 356 |
Table 2-3 Peripheral artery aneurysm (Continued).
| Aneurysm | Treatment procedure | Graft material for open surgery | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Replacement | Exclusion with bypass | Ligation/ resection | Stent graft | Coil embolization | Others | Polyester | ePTFE | Autogenous vessel | Others | |
| Aortic arch branches | ||||||||||
| Carotid | 2 | 0 | 0 | 7 | 0 | 4 | 1 | 0 | 1 | 0 |
| Vertebral | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| Subclavian | 13 | 7 | 4 | 29 | 13 | 7 | 6 | 11 | 3 | 0 |
| Multiple in arch branches | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 |
| Others | 1 | 0 | 5 | 9 | 7 | 1 | 1 | 2 | 0 | 0 |
| Upper limb artery | ||||||||||
| Axillary | 11 | 7 | 4 | 2 | 1 | 3 | 1 | 7 | 10 | 0 |
| Brachial | 39 | 7 | 90 | 4 | 1 | 52 | 5 | 24 | 16 | 0 |
| Forearm-hand | 9 | 5 | 91 | 0 | 0 | 20 | 0 | 7 | 6 | 0 |
| Others | 1 | 0 | 13 | 0 | 1 | 5 | 0 | 1 | 0 | 0 |
| Visceral artery | ||||||||||
| Celiac | 3 | 1 | 2 | 13 | 11 | 1 | 2 | 1 | 1 | 0 |
| Hepatic | 2 | 0 | 4 | 4 | 6 | 1 | 1 | 0 | 2 | 0 |
| Splenic | 3 | 1 | 11 | 8 | 69 | 6 | 2 | 0 | 0 | 0 |
| Superior mesenteric | 3 | 5 | 13 | 10 | 14 | 5 | 0 | 0 | 7 | 0 |
| Renal | 11 | 1 | 14 | 27 | 36 | 12 | 3 | 1 | 5 | 1 |
| Others | 27 | 6 | 17 | 43 | 41 | 7 | 28 | 3 | 3 | 0 |
| Lower limb artery | ||||||||||
| External iliac | 57 | 8 | 11 | 118 | 35 | 10 | 52 | 14 | 0 | 0 |
| Internal iliac | 187 | 9 | 136 | 716 | 795 | 44 | 183 | 21 | 1 | 2 |
| Femoral | 157 | 32 | 152 | 39 | 19 | 101 | 57 | 114 | 27 | 0 |
| Popliteal | 123 | 89 | 47 | 15 | 7 | 16 | 19 | 78 | 113 | 6 |
| Others | 8 | 6 | 24 | 6 | 8 | 6 | 3 | 7 | 4 | 0 |
| Total | 586 | 172 | 620 | 1,000 | 1,027 | 292 | 309 | 271 | 186 | 8 |
a: Including TAO, Takayasu aortitis, collagen disease related vasculitis, Behçet disease, fibromuscular dysplasia.
b: Connective tissue abnormalities such as Marfan syndrome.
Y-graft: Y-shape artificial graft; T-graft: straight artificial graft; Polyester: polyester artificial graft such as Dacron graft; ePTFE: expanded polytetrafluoroethylene graft
Table 2-4 Internal iliac artery aneurysm.
| Internal iliac artery aneurysm | Cases |
|---|---|
| Unilateral solitary | 639 |
| Bilateral solitary | 202 |
| Associated with AAA | 558 |
| Associated with other aneusym | 94 |
AAA: abdominal aortic aneurysm
A total of 3,166 patients were registered, with a male-to-female ratio of 2,468:698, indicating that male cases were more common. Affected regions included the lower limb arteries in 2,491 cases, abdominal visceral arteries in 388 cases, upper limb arteries in 349 cases, and aortic arch branches in 95 cases. It is estimated that 157 cases involved multiple lesions in different regions. Case distribution by artery was as follows: 44.9% in the internal iliac artery, 14.1% in the femoral artery, 8.1% in the popliteal artery, 6.1% in the external iliac artery, and 5.4% in the brachial artery. Of the internal iliac artery aneurysms, 42.8% were unilateral solitary, 13.5% were bilateral solitary, and 37.4% coexisted with abdominal aortic aneurysms. Symptoms were noted in 29.4% of overall cases, with higher rates observed in the brachial (65.2%), femoral (52.8%), and popliteal arteries (55.4%). Rupture occurred in 11.1%. The most common cause was degenerative disease (77.9%). Surgical procedures included coil embolization in 24.5%, stent graft placement in 24.1%, replacement in 16.9%, ligation/resection in 16.4%, and exclusion with bypass in 4.7%, with endovascular treatment accounting for 54.3% of cases. It is inferred that 23.1% of cases involved multiple procedures. The number of registrations increased by 6.3% from 2018, but the incidence by region, etiology, symptomatic cases, and percentage of endovascular procedures were similar to those in 2018.
2. Revascularization for Chronic Arterial Occlusive Disease (Table 3)
1) Aortic arch branch, upper limb, and abdominal visceral arteries (Tables 3-1 and 3-6)
Table 3 Reconstruction for chronic arterial occlusive diseasesa: Table 3-1 Arterial reconstruction for aortic arches.
| Aortic branches | Cases | Gender | Mortality | Background | Etiology | Revascularization procedures | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | 30-day death | Dialysis | ASO | TAO | Vasculitisb | Takayasu arteritis | Others | CAS | CEA | PTA/ stentd | Replacement | Visceral artery bypass | Internal iliac artery bypass | |||||
| Cases | Brain complicationc | Cases | Brain complicationc | Cases | Brain complicationc | ||||||||||||||
| Carotid artery | 267 | 202 | 65 | 9 | 10 | 96 | 0 | 0 | 1 | 170 | 14 | 0 | 70 | 4 | 21 | 0 | 3 | 0 | 0 |
| Vertebral artery | 4 | 4 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 3 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | ||
| Subclavian artery | 589 | 450 | 139 | 15 | 41 | 134 | 1 | 1 | 1 | 452 | 0 | 0 | 99 | 0 | 2 | 0 | 0 | ||
| Multiple lesions of arch branches | 29 | 20 | 9 | 0 | 1 | 4 | 0 | 0 | 0 | 25 | 0 | 0 | 2 | 0 | 1 | 0 | 0 | ||
| Upper limb including axillar artery | 119 | 75 | 44 | 1 | 62 | 85 | 0 | 2 | 0 | 31 | 0 | 0 | 66 | 0 | 0 | 0 | 1 | ||
| Celiac/ Superior mesenteric artery | 101 | 71 | 30 | 5 | 8 | 48 | 0 | 0 | 3 | 49 | 0 | 0 | 32 | 0 | 5 | 57 | 6 | ||
| Renal artery | 119 | 86 | 33 | 2 | 2 | 71 | 0 | 1 | 0 | 45 | 0 | 0 | 88 | 0 | 1 | 25 | 1 | ||
| Others | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| Total | 1,043 | 767 | 276 | 23 | 119 | 424 | 1 | 4 | 5 | 605 | 14 | 0 | 70 | 4 | 285 | 0 | 11 | 63 | 8 |
Table 3-1 Arterial reconstruction for aortic arches (Continued).
| Aortic branches | Revascularization procedures | Graft materialse | Previous recontruction | Revision reason | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Anatomical bypass | Carotid-subclavian bypass | Axillo-axillar bypass | Others | Upper limb artery recanalization | Polyester | ePTFE | Autogenous veins | Others | None | Once | Twice | Three times and more | Unclear | Host artery stenosis/ occlusion | Graft stenosis | Graft occlusion | EVT stenosis | EVT occlusion | Stent graft-caused stenosis/ occlusion | Poor symptom recovery | Others | |
| Carotid artery | 13 | 143 | 87 | 34 | 1 | 50 | 154 | 11 | 11 | 257 | 8 | 1 | 1 | 0 | 1 | 2 | 0 | 2 | 0 | 3 | 0 | 5 |
| Vertebral artery | 0 | 3 | 1 | 1 | 0 | 1 | 2 | 0 | 0 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Subclavian artery | 16 | 277 | 280 | 61 | 4 | 132 | 411 | 2 | 6 | 550 | 27 | 4 | 8 | 0 | 5 | 8 | 8 | 6 | 3 | 4 | 2 | 8 |
| Multiple lesions of arch branches | 4 | 5 | 6 | 15 | 1 | 19 | 8 | 0 | 0 | 28 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Upper limb including axillar artery | 5 | 4 | 7 | 27 | 20 | 8 | 16 | 13 | 6 | 73 | 28 | 9 | 7 | 2 | 13 | 5 | 4 | 16 | 3 | 1 | 1 | 3 |
| Celiac/ Superior mesenteric artery | 0 | 0 | 1 | 7 | 0 | 36 | 29 | 16 | 2 | 84 | 12 | 1 | 3 | 1 | 2 | 0 | 0 | 5 | 3 | 1 | 1 | 4 |
| Renal artery | 0 | 1 | 1 | 6 | 1 | 20 | 14 | 3 | 1 | 100 | 14 | 2 | 1 | 2 | 0 | 2 | 0 | 11 | 0 | 1 | 1 | 3 |
| Others | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 26 | 301 | 295 | 118 | 26 | 202 | 496 | 44 | 21 | 920 | 83 | 16 | 19 | 5 | 20 | 16 | 12 | 38 | 9 | 8 | 4 | 21 |
a: Bypass surgery combined with endovascular treatment is counted in both the bypass category (Table 3-2) and the endovascular category (Table 3-5).
b: Including TAO, Coarctation of aorta, collagen disease related vasculitis, Behçet disease, fibromuscular dysplasia.
c: Postoperative irreversible brain complication.
d: Including percutaneous transluminal angioplasty (PTA), stent, and other endovascular means such as catheter atherectomy.
e: Only for open surgery.
Table 3-2 Arterial reconstruction for chronic lower limb ischemia.
| From aorta to lower limb arterial systems | Cases | Gender | Mortality | Dialysis cases | Etiology | Graft materials | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | 30-day death | ASO | TAO | Vasculitis | Takayasu arteritis | Others | Polyester | ePTFE | Autogenous veins | Others | |||
| Aorto-aortic bypass | 50 | 33 | 17 | 2 | 3 | 43 | 0 | 2 | 1 | 3 | 22 | 9 | 0 | 0 |
| Infrarenal aortic reconstruction (suprarenal clamp) | 40 | 31 | 9 | 0 | 1 | 37 | 0 | 0 | 0 | 2 | 15 | 0 | 0 | 0 |
| Aorto-femoral bypassa | 497 | 376 | 121 | 2 | 33 | 465 | 2 | 2 | 2 | 23 | 174 | 102 | 16 | 6 |
| Femoro-popliteal (above the knee) bypass | 1,203 | 880 | 323 | 14 | 164 | 1,189 | 1 | 2 | 0 | 11 | 106 | 719 | 219 | 20 |
| Infrapopliteal arterial bypass | 1,865 | 1,314 | 551 | 35 | 707 | 1,810 | 12 | 10 | 0 | 31 | 49 | 256 | 1,480 | 62 |
| Femoro-popliteal (below the knee) bypass | 633 | 442 | 191 | 7 | 188 | 621 | 1 | 2 | 0 | 8 | 33 | 187 | 360 | 27 |
| Femoro-crural/pedal bypassb | 1,250 | 882 | 368 | 28 | 526 | 1,207 | 11 | 8 | 0 | 23 | 17 | 74 | 1,137 | 35 |
| Extended deep femoral plasty | 65 | 50 | 15 | 0 | 9 | 63 | 0 | 0 | 0 | 2 | 8 | 17 | 19 | 5 |
| Others | 84 | 64 | 20 | 1 | 10 | 75 | 0 | 1 | 0 | 6 | 19 | 32 | 23 | 0 |
| Total | 3,698 | 2,669 | 1,029 | 54 | 915 | 3,576 | 15 | 17 | 3 | 78 | 369 | 1,094 | 1,722 | 90 |
Table 3-2 Arterial reconstruction for chronic lower limb ischemia (Continued).
| From aorta to lower limb arterial systems | Previous reconstruction | Revision reason | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| None | Once | Twice | Three times and more | Unclear | Host artery stenosis/occlusion | Graft stenosis | Graft occlusion | EVT stenosis | EVT occlusion | Stent graft-caused stenosis/ occlusion | Poor symptom recovery | Others | |
| Aorto-aortic bypass | 45 | 4 | 1 | 0 | 0 | 2 | 0 | 1 | 0 | 0 | 0 | 1 | 1 |
| Infrarenal aortic reconstruction (suprarenal clamp) | 34 | 3 | 3 | 0 | 0 | 0 | 0 | 3 | 1 | 2 | 0 | 0 | 0 |
| Aorto-femoral bypassa | 419 | 54 | 15 | 7 | 2 | 11 | 11 | 20 | 8 | 14 | 2 | 5 | 8 |
| Femoro-popliteal (above the knee) bypass | 863 | 220 | 54 | 58 | 8 | 80 | 21 | 61 | 20 | 83 | 16 | 39 | 26 |
| Infrapopliteal arterial bypass | 1,022 | 445 | 183 | 192 | 23 | 164 | 42 | 154 | 60 | 185 | 19 | 149 | 61 |
| Femoro-popliteal (below the knee) bypass | 378 | 133 | 54 | 62 | 6 | 44 | 17 | 59 | 18 | 63 | 11 | 20 | 27 |
| Femoro-crural/pedal bypassb | 658 | 315 | 129 | 131 | 17 | 121 | 25 | 95 | 42 | 124 | 8 | 130 | 34 |
| Extended deep femoral plasty | 37 | 19 | 1 | 8 | 0 | 7 | 2 | 5 | 3 | 5 | 0 | 3 | 4 |
| Others | 50 | 20 | 6 | 8 | 0 | 9 | 2 | 13 | 2 | 4 | 0 | 1 | 3 |
| Total | 2,392 | 750 | 258 | 265 | 33 | 270 | 75 | 250 | 91 | 284 | 37 | 197 | 101 |
a: Including aorto-iliac bypass or ilio-femoral bypass.
b: Including popliteal-crural (or pedal) bypass.
Table 3-3 Extra-anatomical bypassa.
| Extra-anatomical bypass | Cases | Gender | Mortality | Dialysis cases | Etiology | Graft materials | Previous reconstruction | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | 30-day death | ASO | TAO | Others | Polyester | ePTFE | Autogenous veins | Others | None | Once | |||
| Carotid-subclavian bypass | 301 | 222 | 79 | 11 | 9 | 20 | 0 | 281 | 70 | 256 | 0 | 2 | 291 | 8 |
| Axillo-axillar bypass | 295 | 227 | 68 | 10 | 14 | 45 | 0 | 250 | 62 | 253 | 1 | 4 | 283 | 9 |
| Axillo-femoral bypassb | 204 | 125 | 79 | 5 | 32 | 188 | 0 | 16 | 33 | 164 | 8 | 1 | 163 | 22 |
| Femoro-femoral crossover bypass | 614 | 491 | 123 | 9 | 62 | 568 | 0 | 45 | 125 | 453 | 32 | 19 | 465 | 102 |
| Others | 56 | 43 | 13 | 0 | 9 | 45 | 2 | 9 | 7 | 45 | 4 | 2 | 28 | 10 |
| Total | 1,616 | 1,192 | 424 | 27 | 157 | 1,103 | 2 | 511 | 331 | 1,282 | 63 | 29 | 1,336 | 185 |
Table 3-3 Extra-anatomical bypassa (Continued).
| Extra-anatomical bypass | Previous reconstruction | Revision reason | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Twice | Three times and more | Unclear | Host artery stenosis/ occlusion | Graft stenosis | Graft occlusion | EVT stenosis | EVT occlusion | Stent graft-caused stenosis/ occlusion | Poor symptom recovery | Others | |
| Carotid-subclavian bypass | 0 | 2 | 0 | 0 | 2 | 3 | 0 | 0 | 2 | 0 | 4 |
| Axillo-axillar bypass | 1 | 2 | 0 | 2 | 1 | 3 | 1 | 0 | 2 | 0 | 4 |
| Axillo-femoral bypassb | 8 | 8 | 3 | 3 | 2 | 15 | 3 | 6 | 1 | 4 | 7 |
| Femoro-femoral crossover bypass | 23 | 19 | 4 | 33 | 5 | 40 | 10 | 21 | 11 | 13 | 14 |
| Others | 5 | 10 | 3 | 1 | 1 | 9 | 1 | 2 | 0 | 3 | 8 |
| Total | 45 | 39 | 11 | 42 | 13 | 82 | 22 | 36 | 15 | 26 | 41 |
a: Cases underwent extraanatomical bypass because of graft infection should not be include this category. Those cases are listed in vascular complication (Table 6-1).
b: A case that underwent axillo-femoro-femoral crossover bypass is counted as one case. A case combined with an additional contralateral side of the axillo-femoral bypass as second staged surgery is counted as 2 cases.
Table 3-4 Thromboendarterectomya for chronic lower limb ischemia.
| Thromboendarterectomy | Cases | Gender | Mortality | Dialysis cases | Etiology | Previous reconstruction | Revision reason | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | 30-day death | ASO | TAO | Others | None | Once | Twice | Three times and more | Unclear | Host artery stenosis/ occlusion | Graft stenosis | Graft occlusion | EVT stenosis | EVT occlusion | Stent graft-caused stenosis/ occlusion | Poor symptom recovery | Others | |||
| Aorto-iliac lesion | 74 | 52 | 22 | 2 | 17 | 71 | 2 | 1 | 52 | 15 | 3 | 4 | 0 | 6 | 3 | 0 | 3 | 3 | 2 | 2 | 5 |
| Femoro-popliteal lesion | 1,239 | 922 | 317 | 12 | 329 | 1,233 | 2 | 4 | 940 | 187 | 49 | 57 | 6 | 115 | 10 | 24 | 47 | 50 | 2 | 26 | 30 |
| Othersb | 577 | 421 | 156 | 27 | 149 | 527 | 4 | 46 | 301 | 145 | 48 | 70 | 13 | 31 | 41 | 28 | 25 | 20 | 8 | 36 | 77 |
| Total | 1,864 | 1,375 | 489 | 41 | 492 | 1,805 | 8 | 51 | 1,275 | 340 | 99 | 131 | 19 | 151 | 51 | 52 | 73 | 73 | 12 | 64 | 109 |
a: Including patch plasty.
b: Including reconstruction, thrombolysis and others.
Table 3-5 Endovascular treatment for chronic lower limb ischemiaa.
| Endovascular treatment | Cases | Gender | Mortality | Dialysis cases | Etiology | Previous reconstruction | Revision reason | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | 30-day death | In-hospital death | ASO | TAO | Others | None | Once | Twice | Three times and more | Unclear | Host artery stenosis/ occlusion | Graft stenosis | Graft occlusion | EVT stenosis | EVT occlusion | Stent graft-caused stenosis/ occlusion | Poor symptom recovery | Others | |||
| Aorto-iliac lesionb | 4,281 | 3,363 | 918 | 35 | 49 | 640 | 4,214 | 3 | 64 | 3,377 | 553 | 172 | 154 | 25 | 301 | 59 | 53 | 267 | 89 | 46 | 35 | 52 |
| Femoro-popliteal lesionb | 5,091 | 3,521 | 1,570 | 50 | 89 | 1,476 | 5,063 | 4 | 24 | 3,035 | 1,088 | 418 | 521 | 29 | 548 | 204 | 120 | 615 | 303 | 62 | 126 | 78 |
| Infrapopliteal-ankle lesionb | 2,743 | 1,743 | 1,000 | 50 | 92 | 1,358 | 2,716 | 11 | 16 | 1,333 | 599 | 266 | 531 | 14 | 286 | 197 | 114 | 351 | 286 | 14 | 127 | 36 |
| Others | 230 | 147 | 83 | 3 | 7 | 121 | 221 | 2 | 7 | 28 | 42 | 42 | 116 | 2 | 10 | 114 | 46 | 12 | 9 | 1 | 4 | 5 |
| Total (number of lesions underwent EVT)b | 10,581 | 7,587 | 2,994 | 117 | 207 | 2,950 | 10,463 | 17 | 101 | 6,719 | 1,923 | 751 | 1,126 | 62 | 977 | 507 | 274 | 1041 | 557 | 106 | 246 | 152 |
| Total (number of limbs underwent EVT)c | 8,879 | 6,440 | 2,439 | 98 | 179 | 2,330 | 8,774 | 14 | 91 | 5,703 | 1,574 | 611 | 937 | 54 | 815 | 441 | 216 | 845 | 431 | 91 | 201 | 134 |
a: Including PTA, stent, and other endovascular means such as catheter atherectomy.
b: When endovascular treatment performed for multiple lesions, the case should be counted in each lesions (If a case underwent endovascular treatment in both aorto-iliac and femoro-popliteal lesion, this case can be counted one in aorto-iliac, and one in femoro-popliteal lesion).
c: Counting the patients number not treated lesions. When a case underwent endovascular treatment in multiple lesion, the case is counted as one case.
ASO: arteriosclerosis obliterans; TAO: thromboangitis obliterans (Buerger's disease); CAS: carotid artery stenting; CEA: carotid endarterectomy; PTA: percutaneous transluminal angioplasty; EVT: endovascular treatment; IIA: internal iliac artery
Table 3-6 Debranch for TEVAR or EVAR.
| Debranch for TEVAR or EVAR | Cases |
|---|---|
| Ascending aorta-brachiocephalic-left common carotid(-left subclavian) arterial bypass | 15 |
| Right axillar-left common carotid(-left axillary) arterial bypass | 271 |
| Right common carotid-let common carotid(-left subclavian) arterial bypass | |
| Left common carotid-left subclavian arterial bypass or transposition | |
| Right axillar (subclavian)-left axillar (subclavian) arteril bypass | 237 |
| Abdominal aorta (iliac) (-celiac)-superior mesenteric-renal arterial bypass | 45 |
EVAR: endovascular aneurysm repair; TEVAR: thoracic endovascular aortic repair
In 2019, there was an overall decreasing trend, with 267 cases of carotid artery, 4 cases of vertebral artery, 589 cases of subclavian artery, 29 cases of multiple lesions of aortic arch branches, and 119 cases of axillary and upper extremity artery conditions. The celiac and superior mesenteric arteries showed an increase from 83 cases in 2018 to 101 cases. The number of carotid artery stenting (CAS) and carotid endarterectomy (CEA) carotid arteries increased from 77 cases in 2018 to 84 cases in 2019 but remained below 112 cases recorded in 2017. Surgical revascularization was performed in 83% of subclavian artery lesions, which was similar to the previous year in terms of technique. Among lesions of the axillary and upper extremity arteries, 45% were treated surgically, with a high proportion of dialysis patients at 52%, up from 41% in the previous year.
Regarding debranching with TEVAR/EVAR, the number of registered cases was 15 for ascending aorta–brachiocephalic–left common carotid (–left subclavian) arterial bypass, 271 for right axillar (subclavian)–left common carotid arterial bypass, 237 for right axillary (subclavian)–left axillary (subclavian) arterial bypass, and 45 for abdominal aorta–superior mesenteric artery–renal artery bypass. Compared to 2018, this represents a decrease of 29%, 8%, and 26%, and an increase of 136%, respectively, indicating a decline in cases except for abdominal debranching.
2) Anatomical bypass (Table 3-2), non-anatomical bypass (Table 3-3), thromboendarterectomy (Table 3-4), and endovascular treatment (Table 3-5) in the aorta–lower extremity artery region
Aortoiliac artery territory: For anatomic bypass in lesions of the aortoiliac artery region, the number of cases increased slightly from 553 in 2018 to 587 in 2019, reflecting a 6% increase, with no changes noted in the breakdown, including etiology and graft vessel used. However, for non-anatomic revascularization procedures, such as axillary–femoral and femoral–femoral artery bypass, the number of cases decreased from 311/719 in 2018 to 204/614 in 2019, indicating a 34%/15% decrease (Fig. 4A).
Fig. 4 The annual trends of the number of arterial reconstructions in aorto-iliac (A), femoro-popliteal (B), and crural/pedal region (C), comparing open repair and endovascular treatment. Ao-F: aorto-femoral; Ax-F: axillo-femoral; F-F: femoro-femoral crossover; EVT: endovascular treatment; FPAK: femoropopliteal (above the knee); FPBK: femoro-popliteal (below the knee); SFA: superficial femoral artery; TEA: thromboendarterectomy.

Femoropopliteal artery region: Femoral–above-knee popliteal artery bypass surgeries decreased for the second consecutive year by 4.3%, from 1,257 cases in 2018 to 1,203 cases in 2019, and by 13.9% from 2017 (1,348 cases) to 2019 (Fig. 4B). Artificial vessels accounted for 69% of the grafts (ePTFE/polyester = 60%/9%), whereas the use of autologous veins remained at 18%, similar to that in 2018 (22%). In addition, revascularization to the popliteal artery below the knee decreased by 8%, from 690 cases in 2018 to 633 cases in 2019 (Fig. 4B). Autologous veins comprised 57% of grafts, similar to 59% in 2018. Regarding previous revascularization, 28% of patients underwent above-knee bypass, 39% underwent below-knee bypass, and among dialysis patients, 14% underwent above-knee bypass and 30% underwent below-knee bypass, with no significant difference from the previous year.
Below-knee and foot region: Bypass procedures of the lower leg and foot were similar to the previous year, with 1,292 cases in 2018 and 1,250 cases in 2019 (Fig. 4C). Autologous veins were used as the graft in 91% of cases, similar to the previous year (91%), and dialysis cases accounted for 42%, which was similar to the previous year (40%). Previous revascularization was noted in 46% of cases, suggesting that the frequency of previous revascularization tends to increase with more distal bypass.
Thromboendarterectomy (Table 3-4): Regarding thromboendarterectomy cases of lower extremity arteries, cases in the iliac artery region decreased by 14%, from 86 cases in 2018 to 74 cases in 2019. By contrast, cases in the femoral–popliteal artery region increased by 7%, from 1,159 cases in 2018 to 1,239 cases in 2019. Cases classified as other, including vascular replacement, decreased by 3%, from 597 cases in 2018 to 577 cases in 2019. As a result, the total number of cases in 2019 increased by 5% compared to 2018. For extended deep femoral arterioplasty, the number of cases in 2019 was 65, which was similar to 64 cases in 2018.
Endovascular treatment (Table 3-5): The total number of endovascular treatments was 8,879 cases, representing an increase of 878 cases, or approximately 10%, compared to 2018. Of these, 26% were performed on dialysis patients. Surgical revascularization procedures (bypass, thromboendarterectomy) in the lower limb region showed varying trends by region, but overall, there was a gradual decrease in the total number, whereas endovascular procedures continued to increase over time. By region, the iliac artery region showed the highest increase, with a 13% increase from 3,774 cases in 2018 to 4,281 cases in 2019. The femoral–popliteal artery region showed a 7% increase, whereas endovascular treatment in the lower leg artery region remained unchanged, with the same number of cases as the previous year (Figs. 4A–4C).
3. Revascularization for Acute Arterial Occlusion (Table 4)
Table 4 Revascularization for acute arterial occlusive diseasea.
| Obstructive arteryb | Cases | Gender | Mortality | Etiology | Procedure | Graft materials for open surgery | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | 30-day death | In-hospital death | Embolism | Thrombosisc | Others | Thrombectomy ± patchd | Bypass | Replacement | PTA ± stent | Thrombolysis | Others | Autogenous vessel | Polyester | ePTFE | Others | ||
| Carotid artery | 16 | 10 | 6 | 2 | 2 | 3 | 5 | 8 | 4 | 4 | 3 | 5 | 0 | 1 | 0 | 2 | 5 | 1 |
| Subclavian artery | 70 | 34 | 36 | 8 | 10 | 29 | 24 | 17 | 37 | 17 | 2 | 12 | 0 | 6 | 0 | 4 | 14 | 0 |
| Axillary artery | 79 | 42 | 37 | 6 | 7 | 50 | 20 | 9 | 61 | 10 | 0 | 1 | 0 | 7 | 1 | 2 | 8 | 0 |
| Brachial artery | 690 | 336 | 354 | 30 | 32 | 337 | 336 | 17 | 573 | 18 | 5 | 48 | 2 | 68 | 11 | 6 | 12 | 0 |
| Celiac/superior mesenteric artery | 117 | 75 | 42 | 26 | 36 | 50 | 38 | 29 | 48 | 23 | 2 | 38 | 3 | 11 | 14 | 4 | 7 | 0 |
| Renal artery | 39 | 31 | 8 | 4 | 7 | 11 | 10 | 18 | 8 | 7 | 2 | 21 | 0 | 4 | 1 | 5 | 6 | 1 |
| Abdominal aorta-iliac artery | 846 | 616 | 230 | 90 | 105 | 316 | 406 | 124 | 535 | 207 | 18 | 251 | 6 | 43 | 13 | 76 | 167 | 10 |
| Femoro-popliteal artery | 2,837 | 1,769 | 1,068 | 191 | 268 | 1,262 | 1,465 | 110 | 2,292 | 315 | 26 | 486 | 28 | 174 | 149 | 109 | 223 | 12 |
| Crural artery | 891 | 578 | 313 | 73 | 96 | 397 | 474 | 20 | 679 | 86 | 5 | 196 | 13 | 85 | 55 | 34 | 36 | 6 |
| Pedal arterye | 86 | 64 | 22 | 6 | 7 | 35 | 46 | 5 | 54 | 13 | 0 | 19 | 3 | 14 | 9 | 4 | 3 | 2 |
| Others | 252 | 141 | 111 | 12 | 16 | 52 | 182 | 18 | 191 | 17 | 1 | 48 | 7 | 28 | 7 | 7 | 19 | 0 |
| Total | 4,947 | 3,051 | 1,896 | 351 | 476 | 2,080 | 2,525 | 342 | 3,690 | 596 | 54 | 887 | 47 | 380 | 216 | 218 | 424 | 26 |
a: Cases with non-traumatic acute arterial occlusion are listed in this table. Please see Table 5-1 for acute arterial occlusion by trauma.
b: If the primary occlusion site cannot be identified, the most proximal lesion is described.
c: Cases with acute exacerbation of chronic lesion are excluded. Treatment for those cases are listed in Table 3.
d: If either thrombectomy or patch plasty is performed, cases are listed in this section.
e: Including acute occlusion of dorsalis pedis or plantar artery.
PTA: percutaneous transluminal angiography; ePTFE: expanded polytetrafluoroethylene
Excluding vascular trauma, there were 4,947 cases of acute arterial occlusion, and the total number of occlusions by region was 5,923 cases, suggesting that 976 cases (16%) involved simultaneous occlusions at multiple sites. The affected sites included the abdominal aorta and infra-aortic peripheral arteries in 4,660 cases (79%), upper limb arteries (subclavian, axillary, and brachial) in 839 cases (14%), and abdominal viscera (celiac, superior mesenteric, and renal arteries) in 156 cases (2.6%). The etiology was thrombosis in 50% of cases, embolism in 40%, and other causes in 10%, which was consistent with previous years. Of the 4,947 cases, 934 (19%) underwent endovascular treatment, including percutaneous transluminal angioplasty (PTA) with or without stent, and thrombolysis, which was almost the same as the previous year. By region, endovascular treatment was performed in 30% of abdominal aorta–iliac artery, 18% of femoral–popliteal arteries, 23% of crural arteries, and 26% of pedal artery cases. For femoral–popliteal artery cases, thrombectomy was performed in 81% of cases, and 12% required revascularization (bypass or replacement). For crural artery cases, thrombectomy was performed in 76%, and revascularization was performed in 10%. The operative and in-hospital mortality rates were 11%/12% for the abdominal aorta–iliac artery (10%/12% in the previous year), 7%/9% for the femoral–popliteal artery (7%/9% in the previous year), 8%/11% for the crural artery (8%/11% in the previous year), and 7%/8% for the pedal artery (15%/17% in the previous year). As in previous years, the prognosis was clearly poorer compared to elective revascularization surgery. The operative and in-hospital mortality rates for the celiac and superior mesenteric arteries were 22%/31% (16%/24% in the previous year), indicating a very poor prognosis, consistent with previous years.
4. Treatment of Vascular Trauma (Table 5)
Table 5 Treatment for vascular traumaa: Table 5-1 Arterial trauma.
| Injured artery | Cases | Gender | Mortality | Cause of trauma | Procedure | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | 30-day death | In-hospital death | Traffic accident | Labor accident | Iatrogenic | Others | Direct closure | Patch plasty | Replacement | ||
| Carotid artery | 39 | 17 | 22 | 5 | 10 | 0 | 0 | 29 | 10 | 17 | 1 | 0 |
| Subclavian artery | 78 | 51 | 27 | 9 | 14 | 8 | 3 | 54 | 13 | 21 | 1 | 2 |
| Axillar artery | 23 | 14 | 9 | 0 | 0 | 4 | 4 | 12 | 3 | 7 | 0 | 1 |
| Brachial artery | 362 | 216 | 146 | 8 | 13 | 5 | 12 | 304 | 41 | 240 | 2 | 17 |
| Descending aorta (thoracic/thoracoabdominal) | 26 | 20 | 6 | 8 | 9 | 9 | 1 | 5 | 11 | 6 | 2 | 1 |
| Celiac/ superior mesenteric artery | 69 | 44 | 25 | 7 | 7 | 18 | 1 | 27 | 23 | 12 | 1 | 1 |
| Renal artery | 27 | 19 | 8 | 2 | 3 | 3 | 2 | 14 | 8 | 5 | 0 | 2 |
| Abdominal aorta-iliac artery | 266 | 149 | 117 | 36 | 38 | 32 | 14 | 165 | 55 | 66 | 5 | 14 |
| Femoro-popliteal artery | 991 | 589 | 402 | 72 | 94 | 23 | 31 | 848 | 89 | 682 | 40 | 37 |
| Crural artery | 44 | 25 | 19 | 0 | 0 | 7 | 6 | 15 | 16 | 11 | 2 | 1 |
| Others | 318 | 180 | 138 | 15 | 23 | 16 | 27 | 184 | 91 | 135 | 0 | 6 |
| Total | 2,186 | 1,298 | 888 | 154 | 202 | 109 | 97 | 1,635 | 345 | 1,193 | 51 | 77 |
Table 5-1 Arterial trauma (Continued).
| Injured artery | Procedure | Status of injured artery | Prosthesis | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bypass | Endo-vascular | Ligation | Others | Obstruction/stenosisb | Bleeding without specificationc | GI fistula | Non-GI fistula | Pseudo-aneurysm | Others | Autogenous vessel | Polyester | ePTFE | Others | |
| Carotid artery | 2 | 10 | 5 | 5 | 6 | 21 | 1 | 5 | 2 | 4 | 0 | 0 | 2 | 1 |
| Subclavian artery | 8 | 32 | 8 | 10 | 15 | 34 | 1 | 2 | 10 | 17 | 5 | 1 | 6 | 0 |
| Axillar artery | 8 | 4 | 2 | 2 | 10 | 7 | 0 | 1 | 6 | 3 | 5 | 0 | 4 | 0 |
| Brachial artery | 15 | 13 | 55 | 38 | 23 | 46 | 0 | 8 | 237 | 64 | 23 | 2 | 8 | 0 |
| Descending aorta (thoracic/ thoracoabdominal) | 4 | 6 | 1 | 7 | 1 | 16 | 0 | 0 | 5 | 5 | 1 | 3 | 4 | 0 |
| Celiac/ superior mesenteric artery | 9 | 41 | 1 | 6 | 15 | 36 | 4 | 2 | 8 | 5 | 7 | 2 | 2 | 0 |
| Renal artery | 1 | 18 | 2 | 0 | 4 | 16 | 0 | 2 | 3 | 4 | 0 | 3 | 0 | 0 |
| Abdominal aorta-iliac artery | 28 | 134 | 16 | 29 | 48 | 130 | 9 | 14 | 47 | 37 | 1 | 24 | 23 | 1 |
| Femoro-popliteal artery | 77 | 68 | 70 | 81 | 103 | 226 | 0 | 7 | 553 | 152 | 62 | 29 | 55 | 9 |
| Crural artery | 15 | 9 | 7 | 4 | 9 | 15 | 0 | 0 | 15 | 6 | 15 | 1 | 2 | 0 |
| Others | 6 | 64 | 83 | 41 | 27 | 155 | 2 | 8 | 71 | 61 | 3 | 2 | 10 | 0 |
| Total | 161 | 371 | 247 | 213 | 236 | 675 | 17 | 46 | 950 | 355 | 117 | 59 | 108 | 10 |
a: Iatrogenic pseudoaneurysm in endovascular treatment is listed in this table.
b: Including arterial dissection.
c: Without GI fistula or non-GI fistula. Cases with vessel injury involving both vein and accompanying artery are listed in this table.
GI: gastro-intestinal; ePTFE: expanded polytetrafluoroethylene
Table 5-2 Venous trauma.
| Injured veins | Cases | Cause of trauma | Procedure | Prosthesis | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Traffic accident | Labor accident | Iatrogenic | Others | Direct closure | Patch plasty | Replacement | Bypass | Endo-vascular | Ligation | Others | Autogenous vessel | Polyester | ePTFE | Others | ||
| Superior vena cava | 5 | 0 | 1 | 3 | 1 | 4 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| Inferior vena cava | 20 | 1 | 3 | 10 | 6 | 14 | 1 | 1 | 0 | 1 | 1 | 3 | 1 | 0 | 0 | 1 |
| Brachiocephalic- subclavian vein | 9 | 1 | 2 | 5 | 1 | 7 | 0 | 0 | 1 | 0 | 1 | 2 | 1 | 0 | 0 | 0 |
| Iliac-femoral- popliteal vein | 48 | 1 | 1 | 40 | 6 | 32 | 0 | 1 | 3 | 8 | 7 | 6 | 1 | 1 | 2 | 0 |
| Others | 103 | 3 | 7 | 46 | 47 | 65 | 1 | 2 | 4 | 1 | 26 | 10 | 7 | 0 | 0 | 0 |
| Total | 183 | 6 | 13 | 103 | 61 | 120 | 2 | 4 | 8 | 10 | 35 | 22 | 10 | 1 | 2 | 1 |
ePTFE: expanded polytetrafluoroethylene
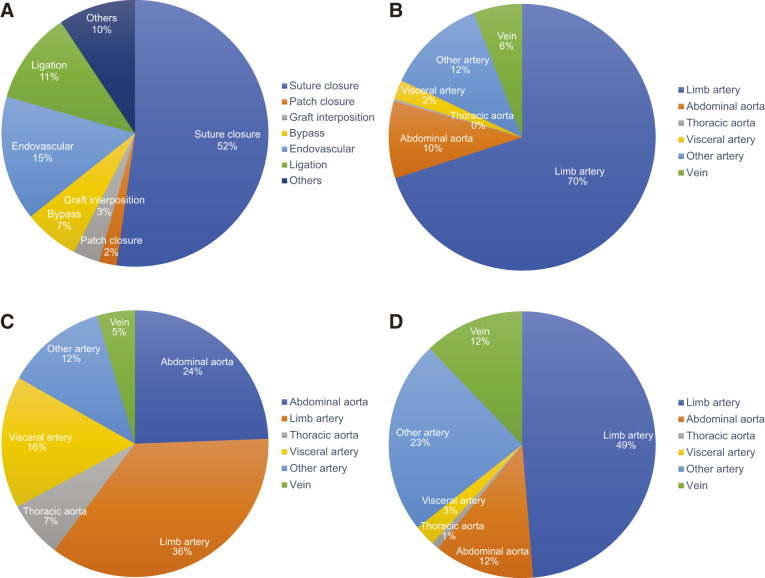
The site of vascular trauma, cause of injury, procedure, and type of graft used in the 2019 NCD registry data are shown in Table 5. The total number of arterial and venous trauma cases was 2,369. The most common cause of vascular trauma was iatrogenic, accounting for 1,738 cases (73%), followed by traffic accidents in 115 cases (5%), and labor accidents with 110 cases (5%). A total of 2,428 sites of vascular injury were recorded, with the most common site being the arteries of the lower extremities, accounting for 1,035 cases (43%), followed by the arteries of the upper extremities with 463 cases (19%), and the abdominal aorta–iliac artery with 266 cases (11%). Regarding the procedure, direct suturing was used in 1,313 cases (52%), endovascular treatment in 381 cases (15%), and ligation in 282 cases (11%) (Fig. 5A). Vascular grafts were used in 308 cases, with 38% of these grafts being autologous.
Fig. 5 Treatment procedure and location of vascular trauma in the year 2019. Operation mode (A), location vascular trauma by iatrogenic (B), traffic accident (C), and work-related accident (D).
1) Iatrogenic vascular trauma
Examination by site revealed that, among the 1,738 cases of iatrogenic vascular trauma at 1,761 sites, the lower extremity arteries were most commonly affected (863 sites, 49%), followed by the upper extremity arteries (370 sites, 21%), together accounting for 70% of the total. Most of these injuries were believed to be complications from puncture sites associated with endovascular catheterization and treatment (Fig. 5B).
2) Traffic accidents
Of 131 sites in 115 cases of traffic accidents, the most commonly injured were the upper and lower limb arteries (47 sites, 36%), followed by the abdominal aorta and iliac arteries (32 sites, 24%), visceral arteries (21 sites, 16%), and the descending aorta and thoracoabdominal aorta (9 sites, 7%) (Fig. 5C). Vessels in the extremities, being closer to the body surface, are assumed to be more susceptible to direct external force. However, unlike vascular trauma from other causes, injuries to the thoracic and abdominal aorta, which are protected by the thoracic cage and abdominal wall, make up a significant proportion of traffic accident injuries. This is likely due to high-energy trauma involving rapid deceleration, such as in collisions.
3) Occupational injuries
This category is based on the assumption of labor accidents, such as falling from a high place or being caught in a machine tool, with 110 cases and 115 sites registered, respectively. By site, the arteries of the extremities, which are close to the body surface and more susceptible to external forces, accounted for 49% of the 56 sites (Fig. 5D).
5. Surgery for Complications after Revascularization (Table 6)
1) Prosthetic graft infection (Table 6-1)
Table 6 Revascularization for vascular complication after revascularization: Table 6-1 Graft infection.
| Position of infected garft | Cases | mortality | Status of infected graft | Proceduere for graft infection | Material for revision or redo surgery | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 30-day death | In-hospital death | Sepsis | Graft-GI fistulab | Garaft-skin fistulab | Others | In-situ replacement | Extra-anatomical bypass | Prosthetic graft extirpation | Others | Polyester | ePTFE | Autogenous vessel | Cryo-preserved homograft | Others | ||
| Descending thoracic aorta | 2 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 2 | 1 | 0 | 0 | 0 | 0 |
| Thoracoabdominal aorta | 13 | 1 | 1 | 2 | 7 | 0 | 4 | 5 | 0 | 1 | 7 | 3 | 1 | 2 | 0 | 0 |
| Abdominal aorta-iliac artery | 78 | 10 | 20 | 36 | 20 | 4 | 21 | 39 | 18 | 4 | 17 | 33 | 19 | 5 | 0 | 8 |
| Abdominal aorta-femoral artery | 35 | 2 | 2 | 12 | 2 | 16 | 8 | 4 | 10 | 14 | 7 | 8 | 6 | 4 | 0 | 0 |
| Femoro-distal artery | 104 | 4 | 10 | 20 | 0 | 55 | 34 | 10 | 23 | 44 | 27 | 5 | 40 | 18 | 0 | 3 |
| Othersa | 174 | 7 | 16 | 33 | 9 | 61 | 79 | 19 | 34 | 79 | 42 | 23 | 50 | 17 | 0 | 4 |
| Total | 406 | 24 | 49 | 103 | 38 | 137 | 147 | 77 | 85 | 142 | 102 | 73 | 116 | 46 | 0 | 15 |
a: Cases with graft infection involving aortic arch branch or upeer limb artery are listed on this column.
b: Including anastomotic disruption.
GI: gastrointestinal; ePTFE: expanded polytetrafluoroethylene
The number of cases registered remained unchanged compared to 2018, with 406 cases. By site, “other,” which includes upper extremity arteries, accounted for 42.9% of all cases, reflecting a trend similar to previous years. Approximately half of the cases in the “other” category involved only graft excision, suggesting that many of these cases were likely due to graft infections in the arteriovenous fistula. In the aorta–iliac and aorta–femoral artery regions, sepsis occurred in approximately 40% of patients, and graft–gastrointestinal fistulas occurred in approximately 20% of patients, with a 30-day postoperative mortality rate of 10.6%. In the femoral–peripheral artery region, sepsis occurred in approximately 20% of patients, and graft–skin fistula occurred in approximately half of the patients, with a 30-day postoperative mortality rate of 3.8%.
2) Anastomotic aneurysm (non-infected) (Table 6-2)
Table 6-2 Anastomotic aneurysma.
| Location of anastomotic aneurysm | Cases | Mortality | Rupture | Cause of aneurysm treated at the primary operation | Repair procedure | Material for repair surgery | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 30-day death | Cases | 30-day death | Degenerativeb | Takayasu arteritis | Other vasculitisc | Infection | Others | Replacement | Excludion and bypass | Stent graft | Others | Polyester | ePTFE | Autogenous vessel | Others | ||
| Aortic arch branch | 9 | 0 | 1 | 0 | 1 | 0 | 2 | 0 | 6 | 2 | 0 | 6 | 1 | 5 | 1 | 0 | 2 |
| Upper limb artery including axillar artery | 14 | 0 | 2 | 0 | 6 | 0 | 0 | 1 | 7 | 0 | 0 | 2 | 12 | 1 | 0 | 1 | 0 |
| Thoracic aorta | 4 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 3 | 0 | 0 | 1 | 3 | 0 | 0 | 0 | 1 |
| Splanchnic artery | 7 | 0 | 2 | 0 | 3 | 0 | 1 | 0 | 3 | 1 | 0 | 3 | 3 | 1 | 1 | 0 | 1 |
| Renal artery | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Abdominal aorta | 39 | 3 | 13 | 1 | 28 | 0 | 0 | 0 | 11 | 11 | 1 | 26 | 2 | 16 | 7 | 2 | 4 |
| Iliac artery | 25 | 1 | 8 | 1 | 10 | 0 | 1 | 3 | 11 | 3 | 0 | 19 | 4 | 6 | 3 | 1 | 4 |
| Femoral artery | 51 | 2 | 13 | 1 | 24 | 1 | 5 | 4 | 17 | 17 | 5 | 4 | 26 | 12 | 17 | 5 | 0 |
| Popliteal or more distal lower limb artery | 13 | 0 | 3 | 0 | 8 | 0 | 0 | 2 | 3 | 2 | 3 | 2 | 6 | 1 | 3 | 4 | 1 |
| Total | 159 | 6 | 42 | 3 | 80 | 1 | 8 | 10 | 60 | 35 | 9 | 61 | 57 | 42 | 32 | 12 | 13 |
a: Cases with infected pseudoaneurysm located at the anastomotic site to the artificial graft are listed in Table 6-1.
b: Including the atherosclerotic aneurysm.
c: Including TAO, collagen disease, Behçet disease, and fibromuscular dysplasia.
ePTFE: expanded polytetrafluoroethylene; TAO: thromboangitis obliterans (Buerger’s disease)
The number of cases has remained almost unchanged over the past several years. The abdominal aorta–iliac artery and lower extremity arteries below the femoral artery each accounted for approximately 40% of the cases. Approximately one-quarter of the cases were ruptured. The treatment involved stent graft insertion in approximately 40% of cases, with the proportion increasing steadily each year.
3) Autologous vascular graft aneurysm (Table 6-3)
Table 6-3 Autogenous graft aneurysm.
| Revascularization area | Cases | Mortality | Repair procedure | ||
|---|---|---|---|---|---|
| 30-day death | Replacement | Bypass | Others | ||
| Visceral artery | 3 | 1 | 1 | 0 | 2 |
| Upper limb artery | 10 | 0 | 0 | 1 | 9 |
| Lower limb artery | 30 | 0 | 6 | 9 | 15 |
| Others | 2 | 0 | 1 | 0 | 1 |
| Total | 45 | 1 | 8 | 10 | 27 |
The number of cases remained almost unchanged, with lower extremity arteries accounting for two-thirds of the cases.
4) Prosthetic graft deterioration (Table 6-4)
Table 6-4 Graft degeneration.
| Revascularization | Cases | Mortality | Initial revascularization procedure | Degenerative material | Repair procedure | Graft material | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 30-day death | Replacement | Bypass | Stent graft | Others | Polyester | ePTFE | Others | Replacement | Bypass | Stent graft | Patch plasty | Others | Polyester | ePTFE | Others | ||
| Desceding thoracic aorta | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| Thoracoabdominal aorta | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 |
| Abdominal aorta-femoral artery | 18 | 0 | 6 | 6 | 3 | 3 | 15 | 2 | 1 | 2 | 4 | 5 | 0 | 7 | 7 | 4 | 4 |
| Femoro-popliteal artery | 17 | 0 | 2 | 12 | 1 | 3 | 3 | 12 | 2 | 5 | 5 | 1 | 0 | 7 | 2 | 7 | 1 |
| Others | 29 | 0 | 11 | 13 | 2 | 4 | 16 | 10 | 3 | 11 | 4 | 4 | 2 | 9 | 8 | 12 | 5 |
| Total | 64 | 0 | 20 | 30 | 6 | 10 | 34 | 24 | 6 | 17 | 14 | 10 | 2 | 23 | 16 | 24 | 10 |
ePTFE: expanded polytetrafluoroethylene
The number of registered patients decreased by approximately 10% from the previous year to 64 cases, continuing the downward trend. Of these, approximately 10% of graft deterioration cases occurred after stent grafting. Among the materials of the degenerated grafts, polyester and ePTFE accounted for 53.1% and 37.5%, respectively.
6. Venous Surgery (Table 7)
1) Lower extremity varicose veins (Table 7-1)
Table 7 Venous surgery: Table 7-1 Varicose veins.
| Varicose veins treatment | Casesa | Male | Female | 30-day death |
|---|---|---|---|---|
| Saphenous vein treatmentsa | ||||
| High ligation | 2,258 | 780 | 1,478 | 0 |
| Stripping | 5,239 | 2,125 | 3,114 | 0 |
| Endovenous thermal ablation | 41,676 | 15,172 | 26,504 | 2 |
| EVLA | 23,749 | 8,486 | 15,263 | 2 |
| RFA | 17,877 | 6,666 | 11,211 | 0 |
| Valvuloplasty | 2 | 1 | 1 | 0 |
| Perforating vein treatmentsa | ||||
| Ligation (Direct surgery) | 439 | 171 | 268 | 0 |
| SEPS | 58 | 27 | 31 | 0 |
| Varicose veins treatmentsa | ||||
| Avulsion | 824 | 282 | 542 | 0 |
| Sclerotherapy | 1,473 | 304 | 1,169 | 0 |
| Others | 249 | 90 | 159 | 0 |
| Totalb | 52,218 | 18,952 | 33,266 | 2 |
a: Only one procedure can be registered in one leg.
b: Total number of surgeries.
EVLA: endovenous laser ablation; RFA: radiofrequency ablation; SEPS: subfascial endoscopic perforator surgery
The number of target tabulating facilities decreased from 909 in 2018 to 905 in 2019. The number of varicose vein surgeries had been increasing steadily through the NCD-based surveys up until 2016 but began to decline in 2017, further dropping to a total of 43,133 in 2018 and 42,131 in 2019. A 2.4% decrease from the previous year was noted, with an average of 47 procedures per center per year. Endovascular thermal ablation (ETA) includes endovenous laser ablation (EVLA) and radiofrequency ablation (RFA). In 2019, EVLA and RFA were performed in 23,749 cases and 17,877 cases, respectively, with the proportion of EVLA cases increasing from the previous year. Stripping and high ligation remained unchanged, with ETA continuing to be the mainstay of treatment, accounting for 79.8% of the total number of procedures (Fig. 6). With the approval of cyanoacrylate embolization15) and the statement on inappropriate treatments, further changes in treatment methods are expected in the future.
Fig. 6 Changes in varicose veins treatment in the year 2011–2019. EVLA: endovenous laser ablation; RFA: radiofrequency ablation.

2) Deep vein thrombosis of the lower limbs (including deep vein stenosis/occlusion) (Table 7-2)
Table 7-2 Deep vein thrombosis (including venous stenosis or obstruction).
| Deep vein thrombosis treatment | Cases | Male | Female | 30-day death |
|---|---|---|---|---|
| Thrombectomy | 35 | 18 | 17 | 1 |
| Catheter-directed thrombolysisa | 41 | 26 | 15 | 0 |
| Bypass (peripheral venous reconstruction) | 6 | 5 | 1 | 0 |
| IVC filter insertionb | 207 | 87 | 120 | 2 |
| IVC filter retrievalb | 108 | 44 | 64 | 1 |
| Direct surgery of stenosisc | 1 | 1 | 0 | 0 |
| Endoluminal treatment of stenosis | 12 | 6 | 6 | 0 |
| Others | 9 | 5 | 4 | 0 |
| Total | 384 | 170 | 214 | 4 |
a: Including the catheter-directed thrombolysis using hydrodynamic thrombectomy catheter.
b: Including temporary IVC filter.
c: Including obstruction.
IVC: inferior vena cava
Surgery for lower extremity deep vein thrombosis was registered in 384 cases, decreasing from 449 cases in 2018. Although the number of surgeries related to inferior vena cava filters decreased with increased awareness of the guidelines, 207 cases (53.9%) involved filter insertion, and 108 cases (28.1%) involved filter retrieval, representing the majority. The removal rate was 52.2% (down from 61.4% in the previous year), reflecting a significant decrease in removals (−27.1%) compared to insertions (−14.1%) from 2018. The number of catheter-directed thrombolysis cases was 41 (10.6%), compared to 45 (10.0%) from the previous year, showing no significant change.
3) Upper limb and jugular vein stenosis/obstruction (Table 7-3)
Table 7-3 Upper limb vein stenosis or obstruction.
| Cases | Male | Female | 30-day death | |
|---|---|---|---|---|
| Thrombectomy | 95 | 59 | 36 | 0 |
| Catheter-directed thrombolysisa | 5 | 5 | 0 | 0 |
| Bypass | 41 | 32 | 9 | 0 |
| SVC filter insertionb | 1 | 1 | 0 | 0 |
| Direct surgery of stenosis | 8 | 5 | 3 | 0 |
| Endovascular treatment of stenosis | 92 | 54 | 38 | 1 |
| Others | 8 | 4 | 4 | 0 |
| Total | 204 | 131 | 73 | 1 |
a: Including the catheter-directed thrombolysis using hydrodynamic thrombectomy catheter.
b: Including temporary IVC filter.
SVC: superior vena cava; IVC: inferior vena cava
The number of upper extremity and jugular vein procedures increased from 148 cases in 2016 to 157 cases in 2017 and 213 cases in 2018 but decreased by 4.3% from the previous year to 204 cases in 2019. Thrombectomy decreased from 106 cases (49.8%) in 2018 to 95 cases (46.6%) in 2019, showing a decline from the previous year. Bypass procedures also showed a decreasing trend, from 54 cases (25.4%) in 2018 to 41 cases (19.7%) in 2019, while endovascular treatment increased from 63 cases (29.6%) in 2018 to 92 cases (45.1%) in 2019.
4) Vena cava reconstruction (Table 7-4)
Table 7-4 Vena cava reconstruction.
| Vena cava reconstruction cases |
Cases | Mortality | Etiology | Treatment procedures | Material for open surgery | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 30-day death | In-hospital death |
Tumor | Thrombus | Others | Patch plasty |
Bypass | Replacement | PTA ± stent | Others | Polyester | ePTFE | Autogenous vein | Autogenous artery | Cryopreserved vessel | Others | Unused | ||
| SVC reconstruction | 13 | 0 | 0 | 9 | 2 | 2 | 3 | 5 | 2 | 3 | 1 | 0 | 6 | 1 | 0 | 0 | 4 | 2 |
| IVC reconstruction | 37 | 0 | 1 | 35 | 0 | 2 | 10 | 1 | 13 | 1 | 12 | 3 | 8 | 7 | 0 | 0 | 3 | 16 |
| Total | 50 | 0 | 1 | 44 | 2 | 4 | 13 | 6 | 15 | 4 | 13 | 3 | 14 | 8 | 0 | 0 | 7 | 18 |
IVC: inferior vena cava; SVC: superior vena cava; PTA: percutaneous transluminal angiography; ePTFE: expanded polytetrafluoroethylene
The ratio of inferior vena cava reconstruction to superior vena cava reconstruction was similar to that of the previous year, although the number of vena cava surgeries was 50, which was slightly lower than that of the previous year. The most common cause was tumor (44 cases, 88.0%), and there was one death without surgery and one death in hospital, accounting for 2.0%.
5) Budd–Chiari syndrome (Table 7-5)
Table 7-5 Budd-Chiari syndrome.
| Treatment | Cases | Gender | Mortality | Material for open surgery | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | 30-day death | In-hospital death |
Polyester | ePTFE | Autogenous veins | Autogenous artery | Cryopreserved vessels | Others | Unused | ||
| Shunting | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Percutaneous shunting (TIPS) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Direct surgery of stenosis | 2 | 2 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 |
| Endoluminal treatment of stenosis | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Liver transplantation | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 2 | 2 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 |
TIPS: transjugular intrahepatic portosystemic shunt; ePTFE: expanded polytetrafluoroethylene
There were no registered cases of transjugular intrahepatic portosystemic shunt (TIPS) in this study, with only 2 cases of direct surgery registered.
6) Others (Table 7-6)
Table 7-6 Other surgery.
| Treatment | Cases | Gender | Mortality | ||
|---|---|---|---|---|---|
| Male | Female | 30-day death | In-hospital death |
||
| Plication of deep venous aneurysma | 10 | 2 | 8 | 0 | 0 |
| Plication of abdominal venous aneurysm | 4 | 2 | 2 | 0 | 0 |
| Others | 1,151 | 632 | 519 | 27 | 77 |
| Total | 1,165 | 636 | 529 | 27 | 77 |
a: Including patch plasty.
There were 10 cases of aneurysmorrhaphy for deep venous aneurysm and 4 cases of surgery for visceral venous aneurysm, both representing a small number of surgeries, similar to the numbers in 2018.
7. Other Vascular Diseases and Associated Procedures (Table 8)
Vascular access surgeries continued to increase significantly in 2019 compared to 2018, while the number of other surgeries remained stable, showing no significant changes from previous years.
1) Popliteal artery entrapment syndrome and adventitial cystic disease (Tables 8-1 and 8-2)
Table 8 Other vascular diseases: Table 8-1 Popliteal artery entrapment syndrome.
| Treatment | Cases | 30-day death |
|---|---|---|
| Myotomy | 20 | 0 |
| Revascularization | 16 | 0 |
| Total | 26 | 0 |
Table 8-2 Adventitial cystic disease.
| Treatment | Cases | 30-day death |
|---|---|---|
| Cyst excision ± patch plasty | 25 | 0 |
| Replacement | 8 | 0 |
| Bypass | 6 | 0 |
| Total | 35 | 0 |
The number of cases has remained almost unchanged over the past few years, and the disease continues to be rare.
2) Thoracic outlet syndrome (Table 8-3)
Table 8-3 Throracic outlet syndrome (TOS).
| Treatment | Cases | Male | Female | 30-day death | Type of TOSa | ||
|---|---|---|---|---|---|---|---|
| Neurogenic | Venous | Arterial | |||||
| Rib resectionb | 7 | 4 | 3 | 0 | 6 | 0 | 2 |
| Rib resection + scalenectomy | 7 | 4 | 3 | 0 | 7 | 0 | 1 |
| Bypass | 1 | 0 | 1 | 0 | 1 | 0 | 1 |
| Total | 14 | 8 | 6 | 0 | 13 | 0 | 3 |
a: In the case with mixture type, the type having the most significant impact on the clinical symptom is listed. But, if the impacts are similar, multiple response is allowed.
b: Including cervical rib.
The number of cases has remained almost unchanged over the past few years, and the disease continues to be rare.
3) Vascular access procedures (Table 8-4)
Table 8-4 Vascular access operation.
| Treatment | Cases | 30-day death |
|---|---|---|
| Arteriovenous access creation by autogenous material | 16,061 | 133 |
| Arteriovenous access creation by artificial materiala | 4,050 | 59 |
| Open surgery for access repair | 3,822 | 33 |
| Endovascular access repair | 21,272 | 93 |
| Arterial transposition | 611 | 10 |
| Arteriovenous access aneurysm repair | 565 | 5 |
| Venous transposition with arteriovenous access creation | 187 | 3 |
| Arteriovenous access closure | 584 | 13 |
| Artificial graft extirpation | 453 | 10 |
| Total | 47,605 | 359 |
a: Including cases with access repair using artificial graft.
While the number of cases has generally increased every year, this year also saw an increase of 3,600 cases compared to last year, with a particular increase in PTA cases, as was the case in the previous year.
4) Lymphedema surgery (Table 8-5)
Table 8-5 Surgery for lymphedema.
| Treatment | Cases | Male | Female | 30-day death |
|---|---|---|---|---|
| Lymphovenous anastomosis | 13 | 3 | 10 | 0 |
| Lymph drainage operation | 1 | 0 | 1 | 0 |
| Resection | 25 | 16 | 9 | 0 |
| Total | 39 | 19 | 20 | 0 |
Although the number of cases has decreased slightly compared to last year, it remains a rare procedure.
5) Sympathectomy (Table 8-6)
Table 8-6 Symphatectomy.
| Symphatectomy | Cases | 30-day death |
|---|---|---|
| Thoracic sympathectomy | 29 | 0 |
| Lumbar sympathectomy | 3 | 0 |
| Total | 32 | 0 |
As in the previous year, >30 cases were reported this year, but it remains a rare procedure.
6) Upper and lower extremity amputations (Tables 8-7, 8-8)
Table 8-7 Amputation of upper limb.
| Amputation level | Cases | 30-day death |
|---|---|---|
| Digit | 10 | 0 |
| Forearm/ upper arm | 6 | 2 |
| Total | 16 | 2 |
Table 8-8 Amputation of lower limba.
| Amputation level | Cases | 30-day death | Etiology | |||
|---|---|---|---|---|---|---|
| ASO | DM-ASO | TAO | Others | |||
| Toe | 689 | 12 | 241 | 387 | 1 | 60 |
| Transmetatarsal | 361 | 17 | 79 | 245 | 1 | 36 |
| Lisfranc/chopart | 55 | 4 | 20 | 33 | 0 | 2 |
| Syme | 7 | 0 | 0 | 6 | 0 | 1 |
| Below-knee | 242 | 15 | 104 | 109 | 1 | 28 |
| Through-knee/above-knee | 341 | 31 | 168 | 115 | 2 | 56 |
| Hip | 8 | 1 | 6 | 0 | 0 | 2 |
| Total | 1,703 | 80 | 618 | 895 | 5 | 185 |
a: Amputations not due to ischemia are not included.
ASO: arteriosclerosis obliterans; DM-ASO: diabetic ASO; TAO: thromboangitis obliterans (Buerger's disease).
Upper limb amputations remained stable this year; however, lower limb amputations continued to increase.
7) Arterial/venous graft harvesting, and surgical cannulation and removal for IABP, PCPS, and ECMO (Table 8-9)
Table 8-9 Arterial graft harvest, venous graft harvest, surgical cannulation and removal of IABP, PCPS, ECMO.
| Cases | 30-day death | |
|---|---|---|
| Arterial graft harvest | 153 | 5 |
| Venous graft harvest | 238 | 6 |
| Surgical cannulation and removal of IABP, PCPS, ECMO | 1,660 | 483 |
| Total | 2,051 | 494 |
IABP: intraaortic balloon pumping; PCPS: percutaneous cardiopulmonary support; ECMO: extracorporeal membrane oxygenation.
Although the overall number of grafts increased compared to last year, the number of arterial and venous grafts decreased, and the future trend should be closely monitored.
Conclusion
One of the main purposes of participating in NCD is to utilize the data to improve the quality and safety of medical care. The Japanese Society for Vascular Surgery initiated a nationwide multicenter study in 2018 on treatment options for ruptured abdominal aortic aneurysms, comparing open surgery and EVAR. Enrollment was closed at the end of DEC 2021, and the paper is currently being prepared. One of the first attempts by the Japanese Society for Vascular Surgery to use NCD data involved a model research project. “A retrospective study on the treatment and prognosis of infected abdominal aortic and common iliac artery aneurysms” was published in the British Journal of Surgery in 2021,16) and the Journal of Vascular Surgery in 2024,17) while “a retrospective study on the surgical technique and prognosis of popliteal artery entrapment syndrome” was published in the European Journal of Vascular and Endovascular Surgery in 2023.18) Furthermore, the Database Management and Administration Committee of the Japanese Society for Vascular Surgery plans to modify the databases on abdominal aortic aneurysms and acute occlusive arterial disease starting JAN 2024 and to substantially revise the database on chronic occlusive arterial disease from 2025 to make better use of NCD as a database. We are engaging in continuous discussions with the Japanese Committee for Stentgraft Management (JACSM) and the Japan Critical Limb Ischemia Database (JCLIMB) to create a more efficient, useful, and user-friendly database. We welcome your candid opinions and suggestions.
We sincerely hope that the vascular surgery NCD database will contribute to providing high-quality medical care to patients suffering from vascular diseases.
Acknowledgments
A great deal of effort went into the preparation of this annual report.
We would like to thank Ms. Chigusa Yamamoto of the Secretariat of the Japanese Society for Vascular Surgery, Ms. Kyoko Namatame and Ms. Momoka Shimada of the Secretariat of the NCD, and other persons for their great efforts devoted to preparation of this annual report.
Ethical Review
Data disclosure and analysis of vascular surgery data registered with the NCD are conducted on an opt-out basis. The Vascular Surgery Annual Report was approved by the NCD Ethics Committee on 10-OCT-2023 and by the Keio University School of Medicine Ethics Committee on 27-SEP-2024.
Annual Report 2019 Analysis Team
Members of the Database Management Committee of the Japanese Society for Vascular Surgery:
Hideaki Obara (chairperson), Yukio Obitsu (vice-chairperson), Akihiro Hosaka (vice-chairperson), Kunihiro Shigematsu, Shinsuke Mii, Hiroshi Banno, Noriyasu Morikage, Keisuke Miyake, Terutoshi Yamaoka, Kentaro Matsubara, Jin Okazaki, Kinya Matsui, Shinya Takase, Naoki Fujimura, Nobuyoshi Azuma (president of the Japanese Society for Vascular Surgery)
NCD Vascular Surgery Data Analysis Team:
Hiraku Kumamaru
Conflicts of Interest
All co-authors have no conflicts of interest.
References
- 1).Japanese Society for Vascular Surgery database management committee member, NCD Vascular Surgery data analysis team. Vascular surgery in Japan: 2011 annual report by the Japanese Society for Vascular Surgery. Jpn J Vasc Surg 2017; 26: 45–64. (in Japanese) [Google Scholar]
- 2).Japanese Society for Vascular Surgery database management committee member, NCD Vascular Surgery data analysis team. Vascular surgery in Japan: 2012 annual report by the Japanese Society for Vascular Surgery. Jpn J Vasc Surg 2018; 27: 437–56. (in Japanese) [Google Scholar]
- 3).Japanese Society for Vascular Surgery database management committee member, NCD Vascular Surgery data analysis team. Vascular surgery in Japan: 2013 annual report by the Japanese Society for Vascular Surgery. Jpn J Vasc Surg 2019; 28: 273–92. (in Japanese) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4).Japanese Society for Vascular Surgery database management committee member, NCD Vascular Surgery data analysis team. Vascular surgery in Japan: 2014 annual report by the Japanese Society for Vascular Surgery. Jpn J Vasc Surg 2020; 29: 15–31. (in Japanese) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5).Japanese Society for Vascular Surgery database management committee member, NCD Vascular Surgery data analysis team. Vascular surgery in Japan: 2015 annual report by the Japanese Society for Vascular Surgery. Jpn J Vasc Surg 2020; 29: 161–79. (in Japanese) [Google Scholar]
- 6).Japanese Society for Vascular Surgery database management committee member, NCD Vascular Surgery data analysis team. Vascular surgery in Japan: 2016 annual report by the Japanese Society for Vascular Surgery. Jpn J Vasc Surg 2021; 30: 23–41. (in Japanese) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7).Japanese Society for Vascular Surgery database management committee member, NCD Vascular Surgery data analysis team. Vascular surgery in Japan: 2017 annual report by the Japanese Society for Vascular Surgery. Jpn J Vasc Surg 2021; 30: 359–79. (in Japanese) [Google Scholar]
- 8).Japanese Society for Vascular Surgery database management committee member, NCD Vascular Surgery data analysis team. Vascular surgery in Japan: 2018 annual report by the Japanese Society for Vascular Surgery. Jpn J Vasc Surg 2022; 31: 217–37. (in Japanese) [Google Scholar]
- 9).Japanese Society for Vascular Surgery database management committee member, NCD Vascular Surgery data analysis team. Vascular surgery in Japan: 2011 annual report by the Japanese Society for Vascular Surgery. Ann Vasc Dis 2018; 11: 377–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10).Japanese Society for Vascular Surgery database management committee member, NCD Vascular Surgery data analysis team. Vascular surgery in Japan: 2012 annual report by the Japanese Society for Vascular Surgery. Ann Vasc Dis 2019; 12: 260–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11).Japanese Society for Vascular Surgery database management committee member, NCD Vascular Surgery data analysis team. Vascular surgery in Japan: 2013 annual report by the Japanese Society for Vascular Surgery. Ann Vasc Dis 2019; 12: 566–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12).Japanese Society for Vascular Surgery database management committee member, NCD Vascular Surgery data analysis team. Vascular surgery in Japan: 2014 annual report by the Japanese Society for Vascular Surgery. Ann Vasc Dis 2020; 13: 474–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13).Japanese Society for Vascular Surgery database management committee member, NCD Vascular Surgery data analysis team. Vascular surgery in Japan: 2015 annual report by the Japanese Society for Vascular Surgery. Ann Vasc Dis 2021; 14: 289–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14).Japanese Society for Vascular Surgery database management committee member, NCD Vascular Surgery data analysis team. Vascular surgery in Japan: 2016 annual report by the Japanese Society for Vascular Surgery. Ann Vasc Dis 2021; 14: 419–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15).Hirokawa M, Satokawa H, Yasugi T, et al. Cyanoacrylate glue closure for varicose veins: consensus guidelines of the Japanese Society of Phlebology. Jpn J Phlebol 2020; 31: 141–52. (in Japanese) [Google Scholar]
- 16).Hosaka A, Kumamaru H, Takahashi A, et al. Nationwide study of surgery for primary infected abdominal aortic and common iliac artery aneurysms. Br J Surg 2021; 108: 286–95. [DOI] [PubMed] [Google Scholar]
- 17).Hosaka A, Takahashi A, Kumamaru H, et al. Prognostic factors after open and endovascular repair for infected native aneurysms of the abdominal aorta and common iliac artery. J Vasc Surg 2024; 79: 1379–89. [DOI] [PubMed] [Google Scholar]
- 18).Fujimura N, Obara H, Takahashi A, et al. Surgical treatment for popliteal artery entrapment syndrome in Japan: a retrospective, multicentre study using a National Clinical Registry. Eur J Vasc Endovasc Surg 2023; 66: 381–8. [DOI] [PubMed] [Google Scholar]