Abstract
A truncated recombinant 56-kDa outer membrane protein of the Karp strain of Orientia tsutsugamushi (Kp r56) was evaluated in cynomolgus monkeys (Macaca fascicularis) for immunogenicity and safety as a vaccine candidate for the prevention of scrub typhus. This recombinant antigen induced strong humoral and cellular immune responses in two monkeys and was found to be well tolerated. Antigen-specific immunoglobulin M (IgM) and IgG were produced to almost maximal levels within 1 week of a single immunization. Peripheral blood mononuclear cells from vaccinated animals showed an induction of antigen-specific proliferation and gamma interferon production. The Kp r56 was not as efficient as infection with live organisms in preventing reinfection but was able to reduce the inflammation produced at the site of challenge. This report describes the results of the first systematic study of the immunogenicity of a recombinant scrub typhus vaccine candidate in a nonhuman primate model.
Scrub typhus is a potentially fatal, acute, febrile disease caused by infection with the bacterium Orientia tsutsugamushi following the bite of an infected trombiculid mite. Mortality rates for scrub typhus range from <1% to 50%, depending upon proper antibiotic treatment, status of the individual infected, and the strain of O. tsutsugamushi encountered (26). Scrub typhus is typically treatable with doxycycline, tetracycline, or chloramphenicol. However, recent reports of decreased effectiveness of appropriate antibiotic treatment and prophylaxis (12, 32, 47, 50) emphasize the need for the development of a vaccine that will protect individuals from disease caused by infection with one of the many disparate strains of O. tsutsugamushi (26, 42).
Initial vaccine efforts with killed O. tsutsugamushi were successful in animals but not in human studies conducted in Burma and Japan (3, 6). The failure of these vaccines in humans was most likely due to the inability of the killed organisms to stimulate long-lasting heterologous protection. To compensate for the inadequacy of the killed vaccines, a live O. tsutsugamushi vaccine was evaluated in human subjects. Because no known attenuated strain of O. tsutsugamushi existed, the volunteers were treated with antibiotics upon initial expression of the symptoms of scrub typhus. This immunization protocol did not provide significantly longer-lasting heterologous protection than the previous killed vaccines (46). The failure of this vaccine may have been due to the short duration of the infection associated with the early treatment with antibiotics. Subsequently, irradiated O. tsutsugamushi were evaluated as vaccine candidates. They were believed to have the advantages of a live vaccine but did not produce disease and so did not require antibiotic treatment. However, long-lasting heterologous protection was not achieved with this vaccine methodology either (14). Succeeding studies have, in large part, focused on the characterization of the host immune response to O. tsutsugamushi and more recently to potential subunit vaccine candidates.
The immunodominant outer membrane 56-kDa protein of O. tsutsugamushi comprises 10 to 15% of the total bacterial cellular protein content (15, 36). It is recognized by sera collected from 95 to 99% of patients with scrub typhus (35). The 56-kDa protein consists of regions that are conserved among the different strains of O. tsutsugamushi, as well as regions that vary from one strain to another. The vaccine candidate used in this study was a truncated major outer membrane protein (Kp r56) derived from the recombinant form of the 56-kDa protein of the Karp strain of O. tsutsugamushi. It includes both the conserved and variable domains and has been expressed and refolded to its native form (9). Kp r56 has been shown to provide 100% homologous protection to C3Heb/FeJ mice and 60 to 80% homologous protection to Swiss CD-1 outbred mice (W.-M. Ching et al., unpublished data). Similarly, Seong et al. have shown the induction of homologous protection and immune responses in C3H/HeDub mice to O. tsutsugamushi Boryong with a partial 56-kDa recombinant antigen fused with the maltose-binding protein (43).
Clinical and immunological responses to experimental scrub typhus infections have been previously studied in two different species of monkey indigenous to areas where this disease is endemic: the cynomolgus monkey (Macaca fascicularis) (45) and the silver-leaf monkey (Presbytis cristatus) (41, 44, 45, 49). The cynomolgus monkey has been found to be a better model than the silver-leaf monkey due to the fact that the latter is very difficult to maintain in captivity without a high mortality rate (40 to 50%) (45). In addition, it was shown that the two species developed similar clinical syndromes, but the antibody responses were greater in the cynomolgus monkeys (45). Ridgway et al. suggested the use of laboratory-bred cynomolgus monkeys that had not been exposed to scrub typhus and therefore would not have the preexisting immune response to O. tsutsugamushi that had been found in many of the wild-caught monkeys (39). Therefore, the cynomolgus monkey model was chosen for this study to evaluate the immunogenicity, efficacy, and safety of Kp r56.
Specifically, the present study was designed to do the following: (i) confirm the use of cynomolgus monkeys as a nonhuman primate (NHP) model for scrub typhus by evaluating the clinical outcome together with the humoral and cellular immune responses after experimental infection and reinfection with the Karp strain of Orientia tsutsugamushi; (ii) evaluate the immunogenicity and safety of the scrub typhus vaccine candidate Kp r56 in cynomolgus monkeys; and (iii) examine the efficacy of Kp r56 in protecting two cynomolgus monkeys from homologous challenge with O. tsutsugamushi Karp.
MATERIALS AND METHODS
Animals.
Six female juvenile cynomolgus monkeys (Macaca fascicularis) that were 2 to 4 years old, weighed 2 to 3.5 kg, and were obtained from TherImmune stock colony were used for this study. They were housed at the Veterinary Facilities of TherImmune Research Corporation, Gaithersburg, MD. TherImmune's Institutional Animal Care and Use Committee reviewed and approved the use of these animals in this study in accordance with provisions of the USDA Animal Welfare Act, the PHS Policy on Humane Care and Use of Laboratory Animals, and the U.S. Interagency Research Animal Committee Principles for the Utilization and Care of Research Animals. The animals tested negative for preexisting antibody to Karp, Kato, and Gilliam (KpKtGm) r56 and KpKtGm whole-cell antigen by enzyme-linked immunosorbent assay (ELISA) (data not shown) using methods previously described (9, 24, 51).
Orientia tsutsugamushi Karp.
The challenge inoculum was Karp plaque-purified seed (L cells, 11 passages). The cells were semipurified on 8 February 1995 by a Renografin density gradient centrifugation procedure described previously (51). The murine 50% lethal dose (LD50) was determined as previously described (7), except that semipurified orientiae from L cells were used instead of orientia-infected liver-spleen tissue homogenates.
Recombinant protein.
Truncated recombinant 56-kDa protein from O. tsutsugamushi Karp strain (Kp r56) was made as described previously and produced under good manufacturing practices conditions (9).
Adjuvant.
Montanide ISA 51 (Seppic, Inc., Fairfield, NJ) and CpG 10103 (provided by Coley Pharmaceutical Group, Ottawa, Canada) were used together as an adjuvant for the Kp r56 vaccine studies. Montanide ISA 51 alone is an adjuvant that forms a stable water-in-oil emulsion and has been found to induce strong humoral and cellular immune responses when administered with antigens (1). Oligonucleotides, such as CpG 10103, containing bacterial CpG motifs (CpG oligodeoxynucleotides) have been used successfully as adjuvants and have been found to induce strong type 1 immune responses in mice (2, 10) and NHP (48). Together, CpG motifs with Montanide ISA 51 or ISA 720 have combined to enhance immune responses to and protection efficacy of vaccine candidates (1, 29).
Vaccine formulation.
The vaccine preparation utilized in this study included CpG 10103 dissolved in 0.2× phosphate-buffered saline (PBS) (VWR, West Chester, PA) together with the antigen Kp r56. This solution was subsequently mixed with an equal volume of Montanide ISA 51 in a test tube. The complete emulsion was prepared fresh just before immunization and was used within 1 hour of its manufacture. The final concentrations of Kp r56 and CpG 10103 in the vaccine preparation were 425 μg/ml and 125 μg/ml, respectively.
Experimental design.
The study was designed so that four cynomolgus monkeys could be utilized to characterize the response to a series of O. tsutsugamushi Karp inocula and that two additional cynomolgus monkeys could be used to evaluate the safety, immunogenicity, and efficacy of the vaccine candidate Kp r56. Table 1 shows the protocol as performed.
TABLE 1.
Experimental design for the study of cynomolgus monkeys as an NHP model for scrub typhus
| Animal ID | Phase I (week 0, infection)
|
Phase II (week 4, vaccination)
|
Phase III (week 8, challenge)
|
|||
|---|---|---|---|---|---|---|
| Dose (MuLD50) | Type | Dose (μg Kp r56) | Type | Dose (MuLD50) | Type | |
| 1 | 106 | Infection | 0 | Control | 106 | Challenge |
| 2 | 104 | Infection | ||||
| 3 | 102 | Infection | 0 | Control | 106 | Challenge |
| 4 | 101 | Infection | ||||
| 5 | 0 | Control | 850 | Vaccination | 106 | Challenge |
| 6 | 0 | Control | 850 | Vaccination | 106 | Challenge |
Observation of monkeys.
The animals were viewed at least twice daily for mortality, morbidity, general health, and signs of toxicity. Physical examinations were conducted and body weights were determined prior to each treatment and weekly thereafter. The examinations included skin and fur characteristics, eye and mucous membranes, respiratory, circulatory, autonomic, and central nervous systems, and somatomotor and behavior patterns. Body temperatures and food consumption were monitored prior to each treatment and daily thereafter. Dermal Draize observations (13) were recorded daily following each treatment for areas of abnormality in regards to edema and erythema.
Blood collection.
The animals were bled every week. The first bleed was done just prior to the initial infection at week 0. Blood samples were evaluated by chemical, hematological, and immunological methods. Chemical analyses were performed on serum separated from clotted blood. Hematological analyses were performed on whole blood mixed with EDTA. Cellular immunological studies utilized peripheral blood mononuclear cells (PBMC) separated from 4-ml blood samples (with EDTA) on Ficoll-Hypaque gradients (Pharmacia, Peapack, New Jersey). Plasma was collected and stored at −80°C for use in antibody studies. The cell layer was transferred to a test tube, washed twice with PBS, and resuspended in complete medium (containing 10% fetal bovine serum [FBS; Equitech-Bio, Kerrville, TX], RPMI 1640, 2 mM l-glutamine, 50 U/ml gentamicin [Quality Biological Inc., Gaithersburg, MD], and 0.1 mM nonessential amino acids [Sigma-Aldrich, St. Louis, MO]). Cells were subsequently used for antigen-specific lymphocyte proliferation and enzyme-linked immunospot (ELISpot) assays.
Blood was also collected three times per week to determine the onset and duration of orientemia by quantitative real-time PCR (qPCR) detection of a segment of the O. tsutsugamushi 47-kDa protein gene (23). Whole blood collected for the qPCR assays was stored at −80°C until DNA was extracted as described below.
Infection.
Four animals (animals 1 to 4) were initially infected with 106,104, 102, and 101 murine LD50 (MuLD50) of O. tsutsugamushi Karp. Infection was by intradermal injections of 50 μl/site at two sites in the scapular region of the back of the neck. Two animals (animals 5 and 6) served as uninfected controls.
Immunizations.
Four weeks following experimental infection of animals 1 to 4, control animals (5 and 6) were both vaccinated by subcutaneous injections of 850 μg of Kp r56 together with 250 μg of CpG 10103 emulsified in Montanide ISA 51 at four sites (0.5 ml each) at the scapular region of the back of the neck. Animals 1 to 4 were not immunized.
Challenge.
Four weeks after vaccination, two of the infected animals (1 and 3) and the two vaccinated ones (5 and 6) were challenged with an intradermal inoculation of 106 MuLD50 of O. tsutsugamushi Karp at two sites at the scapular region of the back of the neck. Animals 2 and 4 were removed from the study.
Evaluation of blood samples. (i) Detection of Orientia in peripheral blood by qPCR.
DNA was extracted from 100 μl of whole-blood samples (with EDTA) by using the DNeasy tissue kit (QIAGEN, Valencia, CA) according to the manufacturer's instructions. qPCRs were conducted as previously described (23). Briefly, a total reaction volume of 25 μl consisting of 5 μl of DNA template, 2.5 μl of 10× PCR buffer with 50 mM MgCl2, 2.5 μl of 2 mM deoxynucleoside triphosphates (IDAHO Technology, Salt lake City, UT), 0.25 μl of each 10 μM primer, 0.5 μl of 10 μM probe, 0.15 μl of 5-U/μl platinum Taq DNA polymerase (Invitrogen, Carlsbad, CA), and 13.75 μl of water was used for each reaction. Thermocycling parameters included a hot start at 94°C for 5 min followed by 50 cycles of a two-step amplification protocol of 94°C for 5 s and 60°C for 30 s. All reactions were performed on a SmartCycler system (Cepheid, Sunnyvale, CA). Three “no template” negative controls were run with each reaction. Plasmid DNA containing 105 copies/μl of the 47-kDa protein gene from O. tsutsugamushi Kato (Ching et al., unpublished observations) target sequence was used as a positive control.
(ii) Chemistry.
The animals fasted overnight prior to sample collection. Blood was collected via puncture of the saphenous vein. Serum collected from clotted blood was assessed for concentrations of sodium, potassium, chloride, total protein, albumin, calcium, phosphorus, creatinine, aspartate aminotransferase, alanine aminotransferase, globulin, alkaline phosphatase, cholesterol, triglycerides, total bilirubin, urea nitrogen, carbon dioxide, albumin/globulin ratio, glucose, and creatinine kinase. These analyses were conducted at the clinical pathology department of TherImmune Research Corporation.
(iii) Hematology.
A complete blood count was conducted, and the following indices were determined: erythrocyte count, hemoglobin, hematocrit, platelet count, leukocyte count, leukocyte differential, mean red blood cell volume, mean red blood cell hemoglobin, mean red blood cell hemoglobin concentration, and mean platelet volume. All hematological analyses were performed by the clinical pathology department of TherImmune Research Corporation.
(iv) Immunology.
Blood samples for immunological analyses were collected and the resultant whole-blood samples shipped immediately on cold packs to the Naval Medical Research Center for the following analyses.
(a) Determination of antibody titer by ELISA.
r56 (0.3 μg/100 μl; 0.1 μg from each strain of O. tsutsugamushi [Karp, Kato, and Gilliam]) in PBS (VWR) was passively adsorbed onto each well of one half of a 96-well plate (Dynatech Laboratories Inc., Chantilly, VA). No antigen (PBS only) was added to the other half of the plate. Plates were covered with plastic wrap and stored at 4°C in a refrigerator for at least 48 h. After coating, plates were washed three times with 300 μl/well of wash buffer that included PBS (VWR) with 0.1% Tween 20 (Sigma Chemical Co., St. Louis, MO). Plates were blocked with 5% skim milk and 0.1% Tween 20 in PBS for 1 hour at room temperature and then washed three times. Plasma samples were serially diluted (fourfold dilutions from 1:100 to 1:409,600) in PBS (pH 7.4) with 5% skim milk and 0.1% Tween 20 in the coated plates to a final volume of 100 μl/well and incubated at room temperature for 1 hour, after which the plates were washed three times with wash buffer. The presence of specific antibodies was demonstrated by the subsequent binding of 100 μl/well of horseradish peroxidase-conjugated goat antibodies directed to monkey immunoglobulin G (IgG) or IgM (Kirkegaard & Perry Laboratories, Gaithersburg, MD). The plates were incubated at room temperature for 1 hour and washed, and 100 μl/well substrate [equal volumes of 2,2′-azino-di-(3-ethylbenzthiazoline-6-sulfonate) (ABTS) and hydrogen peroxide (Kirkegaard & Perry Laboratories)] was added to each well. The plates were incubated at room temperature for 15 min. Optical densities at 405 nm were measured by Vmax/Kinetic Microplate Reader (Molecular Devices, Sunnyvale, CA). Titers were expressed as the inverse of the highest dilution in which a net optical density (absorbance with antigen − absorbance without antigen) of 0.200 or greater was obtained. The mean net absorbance plus 3 standard deviations of three negative control sera was consistently less than an optical density of 0.200.
(b) Antigen-specific lymphocyte proliferation.
Cells were cultured in 96-well plates at 105 cells/well with or without antigen (Kp r56). Plates were incubated at 37°C in the presence of 5% CO2. After 72 h, [3H]thymidine (Perkin-Elmer Life Sciences Wallac, Inc., Gaithersburg, MD) was added at 1 μCi/well. Radioactivity was measured after overnight incubation in a Wallac 1450 Microbeta liquid scintillation and luminescence counter. Results were expressed as the stimulation index (SI), which is the ratio of counts per minute of the antigen-stimulated cultures to that of the control cultures stimulated with medium only.
(c) Determination of antigen-specific IFN-γ production by ELISpot assay.
An ELISpot kit for gamma interferon (IFN-γ) was used per the manufacturer's instructions (Mabtech, Sweden). Briefly, multiscreen 96-well plates (Millipore, Bedford, MA) were coated with monoclonal antibody (GZ-4) against human/monkey IFN-γ at 15 μg/ml in PBS, pH 7.2, in a total volume of 100 μl overnight at 4°C. The following day, plates were washed six times with PBS-0.05% Tween 20 (Sigma). Plates were then blocked with RPMI medium containing 10% FBS. PBMC were plated at 4 × 105, 2 × 105, or 1 × 105 cells per well in a 200-μl final volume of complete RPMI medium (containing 10% FBS, 2 mM l-glutamine, 0.1 mM nonessential amino acids, 5 × 10−5 M β-mercaptoethanol, 50 U/ml gentamicin). Antigen (Kp r56) was added to the cultures at a final amount of 5 μg/well. Concanavalin A (Sigma) was added as positive control at 2 μg/well. Plates were incubated at 37°C, 5% CO2 for 36 h. After incubation, plates were washed six times with PBS-Tween 20. Biotinylated anti-IFN-γ antibody, 7B6-1, at a concentration of 2.5 μg/ml in PBS with 0.5% FCS (PBS-0.5% FCS) was added at 100 μl/well. Plates were incubated at room temperature for 2 hours. After six washings with PBS-Tween 20, streptavidin-alkaline phosphatase conjugate was added at a 1:1,000 dilution in PBS-0.5% FCS at room temperature for 1 hour. Spots were developed with BCIP (5-bromo-4-chloro-3-indoyl-phosphate p-toluidine)/p-nitroblue tetrazolium chloride substrate (Bio-Rad, Hercules, CA) after 15 to 20 min of incubation at room temperature. Plates were washed with water and air dried. Spots were counted on a CTL ELISpot counter (Cellular Technology Ltd., Cleveland, OH).
RESULTS
Phase I: inoculation of cynomolgus monkeys with O. tsutsugamushi.
Evaluation of signs and symptoms of animals after infection with one of four different doses of O. tsutsugamushi Karp showed a lack of systemic disease among the four animals with each dose evaluated (106, 104, 102, and 101 MuLD50). The general health of the animals appeared normal compared to the appearance of the same animals before infection and to the two control animals. There were no significant changes in body weight, food consumption, body temperature, blood chemistries, or hematological evaluations. The only detectable signs of infection were orientemia and the presence of inflammation at the site of inoculation.
The inflammatory presentations varied in the extent of edema, erythema, and duration in an inoculum dose-dependent manner (Table 2). Animal 1, infected with a dose of 106 MuLD50, was observed to have erythema, starting with minimal coloration (light pink, with a score of 1) on day 6 after infection and increasing to severe coloration (dark red, with a score of 4) on day 9. This erythema persisted up to day 13 and decreased slowly to day 23, disappearing thereafter. This animal also had minimal edema starting on day 6 (with a score of 1) that increased to moderate (with a score of 3) from day 8 to day 10 and then slowly declined and recovered to normal by day 16. Animals 2 and 3, infected with 104 and 102 MuLD50, respectively, were observed with minimal (score of 1) erythema and edema. Of these two animals, animal 2 showed erythema from days 8 to 10 and edema from days 8 to 15, whereas animal 3 showed erythema from days 14 to 24 and edema on days 14 and 15. There was a lack of inflammation noted at the inoculation sites for animal 4, and this was considered to be the result of the low dose of infection. A single observation of minimal erythema and edema was made on day 13 for one control animal (animal 5), and the rest of the observations for the control animals were considered normal.
TABLE 2.
Dermal observations at the site of infection with O. tsutsugamushi in infected and vaccinated cynomolgus monkeysa
| Animal ID | Phase I (infection)
|
Phase III (challenge)
|
||||
|---|---|---|---|---|---|---|
| Dose (MuLD50) | Duration, maximum scoreb
|
Dose (MuLD50) | Duration, maximum scoreb
|
|||
| Edema | Erythema | Edema | Erythema | |||
| 1 | 106 | Days 6-15, 3 | Days 6-23, 4 | 106 | 0 | 0 |
| 2 | 104 | Days 8-15, 1 | Days 8-10, 1 | |||
| 3 | 102 | Days 14-15, 1 | Days 14-24, 1 | 106 | 0 | 0 |
| 4 | 101 | 0 | 0 | |||
| 5c | 0 | Day 13, 1 | Day 13, 1 | 106 | Days 5-32, 3 | Days 5-20, 1 |
| 6c | 0 | 0 | 0 | 106 | Days 5-27, 3 | Days 5-20, 1 |
No dermal abnormalities were observed during the phase II vaccination period.
Scores for edema observations: 0, none (no swelling); 1, minimal (slight swelling); 2, mild (defined swelling [distinct]); 3, moderate (defined swelling [raised]). Scores for erythema observations: 0, none (normal color); 1, minimal (light pink); 2, mild (bright pink/pale red); 3, moderate (bright red); 4, severe (dark red).
For phase III, animals 5 and 6 were vaccinated 4 weeks prior to challenge with 850 μg Kp r56.
O. tsutsugamushi nucleic acid was detected in the blood by qPCR analysis of nucleic acid extracted from the monkeys' whole blood (Tables 3 and 4). Blood from monkey 1 (inoculation dose, 106 MuLD50) had detectable O. tsutsugamushi DNA (4.2 copies/10 μl) on day 4. This nucleic acid was detected again on day 8 and day 10. The next assay, performed on day 14, showed an absence of detectable target nucleic acid. The highest copy number of 55/10 μl was detected on day 8. The initial detections of O. tsutsugamushi nucleic acid for the inoculation doses 104, 102, and 101 were on days 4, 8, and 14, respectively. The highest copy numbers detected were 119, 31, and 96/10 μl on days 14, 14, and 21, respectively, for the doses of 104, 102, and 101. No O. tsutsugamushi nucleic acid was detected in any of the blood samples from control animals collected at the same time as the blood from the four infected monkeys or in the assay's nontemplate controls.
TABLE 3.
Real-time PCR for detection of O. tsutsugamushi in infected monkeys (phase I)
| Animal IDa | Dose of infection (MuLD50) | Detection of O. tsutsugamushi on given day of blood collection (after infection)b
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2 | 4 | 8 | 10 | 14 | 16 | 18 | 21 | 23 | 25 | 28 | ||
| 1 | 106 | − | + | + | + | − | − | − | − | − | − | − |
| 2 | 104 | − | + | + | + | + | + | − | − | − | − | − |
| 3 | 102 | − | − | + | + | + | + | + | − | − | − | − |
| 4 | 101 | − | − | − | − | + | + | + | + | + | − | − |
| 5 | 0 | − | − | − | − | − | − | − | − | − | − | − |
| 6 | 0 | − | − | − | − | − | − | − | − | − | − | − |
Animals 1 to 4 were infected, while animals 5 and 6 were controls.
+, positive; −, negative.
TABLE 4.
Determination of O. tsutsugamushi DNA copy number in infected monkeys (phase I)
| Animal IDa | Dose of infection (MuLD50) | DNA copy no./10 μl of blood on dayb:
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2 | 4 | 8 | 10 | 14 | 16 | 18 | 21 | 23 | 25 | 28 | ||
| 1 | 106 | 4.2 | 55 | 47 | ||||||||
| 2 | 104 | 11 | 11 | 47 | 119 | 38 | ||||||
| 3 | 102 | 5.8 | 21 | 31.1 | 24 | 13 | ||||||
| 4 | 101 | 8.9 | 17 | 94 | 95.6 | 44.3 | ||||||
| 5 | 0 | |||||||||||
| 6 | 0 | |||||||||||
Animals 1 to 4 were infected, while animals 5 and 6 were controls.
Blood was collected the given number of days after infection.
Determination of antibody titer by ELISA.
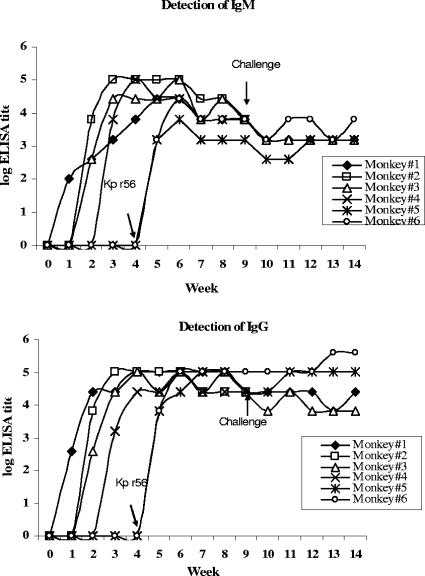
There was a Kp r56-specific antibody response, both IgM and IgG, induced by O. tsutsugamushi Karp infection in cynomolgus monkeys 1 to 4 (Fig. 1). The antibody titers increased with time and then became steady by week 4. The initial appearance of antibody response and the period between infection and peak of the response was related to the dose of inoculum, with the animal receiving the highest inoculum dose exhibiting the earliest appearance and highest peak of antigen-specific antibodies.
FIG. 1.
Antibody (IgM and IgG) titers in serum of cynomolgus monkeys after infection and challenge with O. tsutsugamushi and vaccination with Kp r56.
Antigen-specific lymphocyte proliferation.
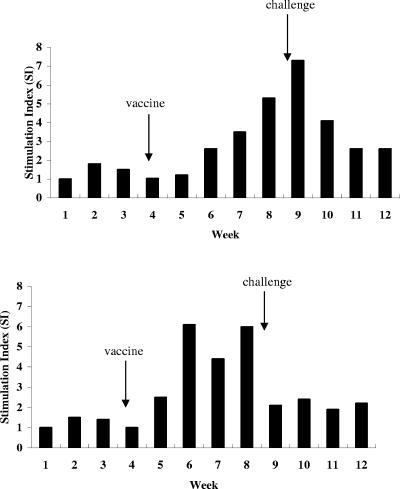
PBMC of infected animals showed in vitro proliferative response to the presence of Kp r56. The extent of proliferation, as expressed by SI, increased with time postinfection, and the onset of increase was related to the dose of the infectious inoculum (Fig. 2). The animal infected with 106 MuLD50 (animal 1) showed an increase in SI at week 2 (Fig. 2A), while the animal infected with 102 MuLD50 (animal 3) showed a positive SI at week 4 (Fig. 2B).
FIG. 2.
In vitro proliferation of PBMC from cynomolgus monkeys in response to infection with O. tsutsugamushi Karp. Animals 1 and 3, respectively, were infected with 106 (A) and 102 (B) MuLD50 and challenged after 8 weeks with 106 MuLD50.
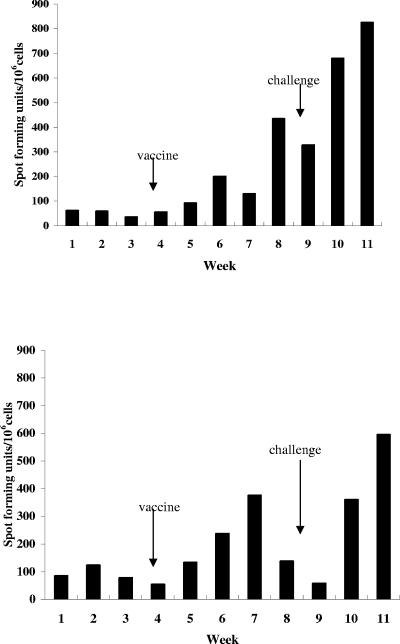
ELISpot assay for detecting IFN-γ production.
PBMC from infected and vaccinated animals were tested for Kp r56-specific IFN-γ production by ELISpot assay, according to procedure of Kumar et al. (28). The results showed that the production of IFN-γ increased after infection. The time of onset of the increase was related to the dose of infection. At an infectious dose of 106 (Fig. 3A), the increase in production started at week 2 postinfection, whereas at a dose of 102 (Fig. 3B), the increase in IFN-γ production was detectable at week 4 after infection.
FIG. 3.
In vitro production of IFN-γ by PBMC of cynomolgus monkeys infected and challenged with O. tsutsugamushi Karp. Monkeys (1 and 3) were infected at week 0 with 106 (A) and 102 (B) MuLD50, respectively, and challenged after week 8 with 106 MuLD50 of O. tsutsugamushi Karp.
Phase II: vaccination of cynomolgus monkeys with Kp r56.
In phase II, animals 5 and 6 were vaccinated in the scapular region of the back with Kp r56 and CpG 10103 emulsified in Montanide ISA 51. No untoward signs or symptoms, either systemically or locally, were associated with the vaccination. Chemistry and hematology results were within normal limits. No abnormal dermal observations were noted. In the animals receiving the vaccine, r56-specific IgM and IgG developed quickly and to almost maximal levels within the first week following vaccination, demonstrating the very strong immunogenicity of this vaccine candidate (Fig. 1). The vaccinated animals also showed an increase in the antigen-specific proliferative response after vaccination (Fig. 4). The response was initiated just after vaccination and continued to increase through the next 4 weeks. The vaccinated animals also showed an increase in Kp r56-specific IFN-γ production in ELISpot assays (Fig. 5). This gradually increased over time. The animals were challenged with O. tsutsugamushi 4 weeks after vaccination.
FIG. 4.
In vitro proliferation of PBMC from two cynomolgus monkeys in response to vaccination and challenge with O. tsutsugamushi Karp. Animals 5 and 6 were vaccinated with Kp r56 and challenged after 4 weeks with 106 MuLD50 of O. tsutsugamushi Karp.
FIG. 5.
In vitro production of IFN-γ by PBMC of two cynomolgus monkeys vaccinated with Kp r56 and challenged with O. tsutsugamushi Karp. Monkeys 5 and 6 were vaccinated with Kp r56 and challenged 4 weeks later with 106 MuLD50 of O. tsutsugamushi Karp.
Phase III: challenge of vaccinated monkeys.
In phase III, the previously infected (animals 1 and 3) and vaccinated (animals 5 and 6) monkeys were challenged with an infectious dose of 106 MuLD50 of O. tsutsugamushi Karp, and the animals were monitored for the appearance of disease. Animals 5 and 6, which received vaccine 4 weeks prior during phase II, demonstrated a minimal (score of 1) to moderate (score of 3) edema and minimal (score of 1) erythema from day 5 to day 32 after challenge (Table 2). Animals 1 and 3 (vaccine controls; live infected in phase I and challenged in phase III), however, had no notable inflammation at the inoculation sites after challenge. The results show that the inflammation at the site of infection was quite limited in vaccinated animals (animals 5 and 6) compared to that observed in the naïve monkey (animal 1), which received a similar infectious dose of 106 MuLD50 in phase I.
Orientemia was detectable by qPCR of blood from the vaccinated monkeys (5 and 6) but not in the previously infected monkeys (1 and 3). The results (Tables 5 and 6) showed that the prior infection of animals 1 and 3 provided sterile immunity to homologous challenge, whereas the animals that were vaccinated (5 and 6) showed orientemia after challenge similar in magnitude to that of animal 1 upon initial infection in phase I.
TABLE 5.
Real-time PCR for detection of O. tsutsugamushi after challenge in infected and vaccinated monkeys (phase III)
| Animal IDa | Dose of challenge (MuLD50) | Detection of O. tsutsugamushi in blood collected on given day after challengeb
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 4 | 6 | 8 | 11 | 13 | 15 | 18 | 20 | 22 | 25 | ||
| 1 | 106 | − | − | − | − | − | − | |||||
| 3 | 106 | − | − | − | − | − | − | |||||
| 5 | 106 | − | + | + | + | + | + | − | − | − | − | − |
| 6 | 106 | − | + | + | + | + | + | + | − | − | − | − |
Animals 1 and 3 were infected, while animals 5 and 6 were vaccinated.
+, positive; −, negative.
TABLE 6.
Determination of O. tsutsugamushi DNA copy number after challenge in infected and vaccinated monkeys (phase III)
| Animal IDa | Dose of challenge (MuLD50) | DNA copy no./10 μl of blood on dayb:
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 4 | 6 | 8 | 11 | 13 | 15 | 18 | 20 | 22 | 25 | ||
| 1 | 106 | |||||||||||
| 3 | 106 | |||||||||||
| 5 | 106 | 2.7 | 35 | 67 | 89.1 | 1.9 | ||||||
| 6 | 106 | 11 | 29 | 83 | 50.1 | 16 | 10 | |||||
Animals 1 and 3 were infected, while animals 5 and 6 had been vaccinated in phase II.
Blood was collected the given number of days after infection.
Following challenge with 106 MuLD50 of O. tsutsugamushi Karp, previously infected animals (1 and 3) did not show an increase in the antibody response. The vaccinated animals (5 and 6) did show, in time, a fourfold rise in IgG titer (Fig. 1). In all four animals (1 and 3 [live infected] and 5 and 6 [vaccinated]), antigen-specific in vitro proliferation and IFN-γ production decreased initially upon challenge (Fig. 2 to 5).
DISCUSSION
The results obtained in this study showed that the pattern of a strong immune response produced in cynomolgus monkeys by vaccination with Kp r56 is similar to that produced by infection with O. tsutsugamushi. The parameters used to measure the immune response were antigen-specific antibody production, in vitro lymphocyte proliferation, and IFN-γ production. Similar immune responses were initiated after infection and after vaccination, as evidenced by an increase in all parameters. Both infection and vaccination demonstrated a positive humoral response with increases in both IgM and IgG titers. Moreover, there was a strong cellular response indicated by an antigen-specific increase in in vitro lymphocyte proliferation and IFN-γ production. The two animals that were treated as negative controls (5 and 6) did not exhibit any antigen-specific immune response until vaccinated in phase II of the study. The time to onset of the immune responses to O. tsutsugamushi and the presence of Orientia in blood were directly related to the dose of infectious inoculum, with the animals infected with higher doses showing an earlier onset of detectable Orientia and immune response. The pattern of immune response to vaccination with Kp r56 (in phase II) was similar to that of infection with O. tsutsugamushi Karp (in phase I), confirming data derived in the Swiss CD-1 outbred mouse model (Ching et al., unpublished observation).
A previous study of the immune response in cynomolgus monkeys to infection with O. tsutsugamushi reported that the antibody response after infection was initially IgM followed by IgG (31). This was in contrast to what was observed in the present study, where IgM and IgG responses were induced almost simultaneously after infection, both of them increasing and reaching a plateau almost at the same time (Fig. 1). Similarly, C3H/HeDub mice immunized with a partial 56-kDa recombinant antigen fused with maltose-binding protein (MBP-Bor56) produced IgM and IgG almost simultaneously (43). The difference in the natures of antibody responses between these studies could be due to the magnitude and characteristic of the antigens used. These same studies also showed a cell-mediated immune response in the animals after infection/immunization. Cellular immune responses to rickettsial infections have been shown to coincide with the development of protection from infection. Studies completed with the murine model of scrub typhus suggested that lymphocyte proliferation responsiveness correlated with resistance to rickettsial infection (19) and that the production of IFN-γ was associated with the development of protective immunity against scrub typhus (37, 38). There are a number of reports that show that IFN-γ inhibits rickettsial growth in macrophages and fibroblasts in vitro (16-18, 27, 33). The presence of a strong cell-mediated immune response to Kp r56 suggests that this vaccine candidate might be successful in providing protective immunity from scrub typhus.
The animals were challenged with equivalent infectious doses in phase III of the study, 8 weeks after initial infection (1 and 3) and 4 weeks after vaccination (5 and 6). The immune responses were monitored through the subsequent 4 weeks. It might be expected that animals previously infected or vaccinated would show an immediate immune response against the infection. The results, however, showed that the responses immediately decreased after challenge in all of the infected as well as the vaccinated animals relative to the observed response following infection or vaccination. This indicates an initial suppression in the immune response in all of the animals, whether reinfected after initial infection or challenged after vaccination.
The observation of immunosuppression at both humoral and cellular levels was seen in experimental infections among animals and has been previously reported (19, 20). Moreover, a report has described the induction of apoptosis in lymphocytes of mice infected with O. tsutsugamushi (25). This report demonstrated prominent apoptotic changes in lymphocytes in the regional lymph nodes and spleens, denoted by the enlargement of the white pulps, in rickettsia-infected animals. These changes were observed in mice infected with both the Karp (murine lethal) and Gilliam (murine nonlethal) strains of O. tsutsugamushi. However, prominent apoptosis occurred only in the Karp-infected mice. The authors suggested that an apoptotic process in lymphocytes may explain the immunosuppression seen in rickettsial infections. Immunosuppression was also suggested to be associated with the development of chronic infections with O. tsutsugamushi in inbred mice (20). The development of chronic infections by a number of microorganisms has been shown to be associated with at least a transient immunosuppression (4, 5, 8, 11, 34, 40). A role of suppressor cells has also been suggested in depression of in vitro lymphoproliferative responses in other systems (21).
The infection process was monitored by qPCR, which detected the presence of the gene for the 47-kDa protein (htrA) of O. tsutsugamushi. The presence of Orientia was measurable starting from a few days after the infection until day 10 for animal 1 (receiving the highest infectious dose) and to day 23 for animal 4 (receiving the lowest infectious dose). The time to initial detection of Orientia and its disappearance were related to the dose of infection. This is similar to results previously described by Ley et al. (30). In the infected animals (1 and 3), orientemia was not detectable after challenge with 106 MuLD50. The vaccinated animals (5 and 6), on the other hand, demonstrated orientemia after challenge. The lack of sterile immunity provided by a vaccine candidate, irradiated O. tsutsugamushi, was reported previously for mice. In the same report, control mice immunized with viable O. tsutsugamushi did show sterile immunity from challenge (14, 22), as we show in our NHP model in this report.
Inflammation at the site of inoculation for monkey 1 was extreme; that is, it had a Draize score for erythema observation of 4 (out of 4), which is defined as “severe erythema (beet redness) to slight eschar formation (injuries in depth)” (13). This response was ameliorated in the two monkeys (5 and 6) vaccinated with Kp r56, in which the same dose given to monkey 1 gave Draize scores of only 1, which is defined as a “very slight erythema (barely perceptible)” (13). Monkeys 1 and 3, upon second infection, produced no perceptible lesion at the site of inoculation. These results, shown in Table 2, suggest that the vaccine candidate provided some immunity to the monkeys, as the occurrence of the primary lesion in patients with scrub typhus has been reported to depend upon both the degree of immunity of the individual and the size of the infecting dose (46).
The challenge of establishing a vaccine for scrub typhus caused by O. tsutsugamushi was embarked upon decades ago (3, 6). The present work provides additional data that will help in this effort by describing for the first time the safety, immunogenicity, and efficacy of a recombinant scrub typhus vaccine candidate in a nonhuman primate model. In addition, the results of this study showed the utility of the cynomolgus monkey as a model for O. tsutsugamushi infections in nonhuman primates and serve as a model for evaluation of different scrub typhus vaccine candidates for this disease prior to use in human clinical trials. Characterization of the immune response of primates to infection, vaccination, and rechallenge is important in the preclinical phase of development of any vaccine for scrub typhus.
Acknowledgments
The opinions expressed in this paper are those of the authors and do not reflect the official policy of the Department of Navy, Department of Defense, or the U.S. Government.
The experiments reported herein were conducted according to the principles set forth in the Guide for the Care and Use of Laboratory Animals (34a).
This investigation was supported by the U.S. Military Infectious Diseases Research Program, Work Unit Number 61102A.870.J.AJ0002.02.
We are grateful to Arthur Krieg for his valuable assistance throughout this investigation and for his review of the manuscript. We are also grateful to Patrick J. Rozmajzl for his discussions and review of the manuscript.
Editor: J. D. Clements
REFERENCES
- 1.Aucouturier, J., L. Dupuis, S. Deville, S. Ascarateil, and V. Ganne. 2002. Montanide ISA 720 and 51: a new generation of water in oil emulsions as adjuvants for human vaccines. Expert Rev. Vaccines 1:111-118. [DOI] [PubMed] [Google Scholar]
- 2.Beloeil, L., M. Tomkowiak, G. Angelov, T. Walzer, P. Dubois, and J. Marvel. 2003. In vivo impact of CpG 1826 oligodeoxynucleotide on CD8 T cell responses and survival. J. Immunol. 171:2995-3002. [DOI] [PubMed] [Google Scholar]
- 3.Berge, T. O., R. L. Gauld, and M. Kitaoka. 1949. A field trial of a vaccine prepared from the Volner strain of Rickettsia tsutsugamushi. Am. J. Hyg. 50:337-342. [DOI] [PubMed] [Google Scholar]
- 4.Boraschi, D., and J. E. Niederhuber. 1982. Regulation of macrophage suppression and cytotoxicity by interferon role of Ia-bearing macrophages. J. Immunol. 129:1854-1858. [PubMed] [Google Scholar]
- 5.Bullock, W. E., E. M. Carlson, and R. K. Gershon. 1978. The evolution of immunosuppressive cell populations in experimental mycobacterial infection. J. Immunol. 120:1709-1716. [PubMed] [Google Scholar]
- 6.Card, W. I., and J. M. Walker. 1945. Scrub-typhus vaccine; field trial in South-East Asia. Lancet 1:481-483. [DOI] [PubMed] [Google Scholar]
- 7.Chan, T. C., J. Jiang, J. J. Temenak, and A. L. Richards. 2003. Development of a rapid method for determining the infectious dose (ID)50 of Orientia tsutsugamushi in a scrub typhus mouse model for the evaluation of vaccine candidates. Vaccine 21:4550-4554. [DOI] [PubMed] [Google Scholar]
- 8.Cheers, C., H. Pavlov, C. Riglar, and E. Madraso. 1980. Macrophage activation during experimental murine brucellosis. III. Do macrophages exert feedback control during brucellosis? Cell. Immunol. 49:168-177. [DOI] [PubMed] [Google Scholar]
- 9.Ching, W. M., H. Wang, C. Eamsila, D. J. Kelly, and G. A. Dasch. 1998. Expression and refolding of truncated recombinant major outer membrane protein (r56) of Orientia tsutsugamushi and its use in enzyme-linked immunosorbent assays. Clin. Diagn. Lab. Immunol. 5:519-526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chu, R. S., O. S. Targoni, A. M. Krieg, P. V. Lehmann, and C. V. Harding. 1997. CpG oligodeoxynucleotides act as adjuvants that switch on T helper (Th1) immunity. J. Exp. Med. 186:1623-1631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Collins, F. M., and S. R. Watson. 1979. Suppressor T-cells in BCG-infected mice. Infect. Immun. 25:491-496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Corwin, A., R. Soderquist, N. Suwanabun, J. Sattabongkot, L. Martin, D. Kelly, and J. Beecham. 1999. Scrub typhus and military operations in Indochina. Clin. Infect. Dis. 29:940-941. [DOI] [PubMed] [Google Scholar]
- 13.Draize, J., G. Woodward, and H. Calvery. 1944. Methods for the study of irritation and toxicity of dermal substances applied topically to the skin and mucous membrane. J. Pharmacol. Exp. Ther. 82:377-390. [Google Scholar]
- 14.Eisenberg, G. H., Jr., and J. V. Osterman. 1979. Gamma-irradiated scrub typhus immunogens: broad-spectrum immunity with combinations of rickettsial strains. Infect. Immun. 26:131-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hanson, B. 1985. Identification and partial characterization of Rickettsia tsutsugamushi major protein immunogens. Infect. Immun. 50:603-609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hanson, B. 1991. Susceptibility of Rickettsia tsutsugamushi Gilliam to gamma interferon in cultured mouse cells. Infect. Immun. 57:4125-4133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hanson, B. 1991. Comparative susceptibility to mouse interferons of Rickettsia tsutsugamushi strains with different virulence in mice and of Rickettsia rickettsii. Infect. Immun. 59:4134-4141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jerrells, T. R., and J. V. Osterman. 1982. Role of macrophages in innate and acquired host resistance to experimental scrub typhus infection of inbred mice. Infect. Immun. 37:1066-1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jerrells, T. R., and J. V. Osterman. 1983. Development of specific and cross-reactive lymphocyte proliferative responses during chronic immunizing infections with Rickettsia tsutsugamushi. Infect. Immun. 40:147-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jerrells, T. R. 1985. Immunosuppression associated with the development of chronic infections with Rickettsia tsutsugamushi: adherent suppressor cell activity and macrophage activation. Infect. Immun. 50:175-182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jerrells, T. R., J. H. Dean, G. L. Richardson, J. L. McCoy, and R. B. Herberman. 1978. Role of suppressor cells in depression of in vitro lymphoproliferative responses of lung cancer and breast cancer patients. J. Natl. Cancer Inst. 61:1001-1009. [PubMed] [Google Scholar]
- 22.Jerrells, T. R., B. A. Palmer, and J. V. Osterman. 1983. Gamma-irradiated scrub typhus immunogens: development of cell-mediated immunity after vaccination of inbred mice. Infect. Immun. 39:262-269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jiang, J., T. C. Chan, J. J. Temenak, G. A. Dasch, W. M. Ching, and A. L. Richards. 2004. Development of a quantitative real-time PCR assay specific for Orientia tsutsugamushi. Am. J. Trop. Med. Hyg. 70:351-356. [PubMed] [Google Scholar]
- 24.Jiang, J., K. J. Marienau, L. A. May, H. J. Beecham, R. Wilkinson, W. M. Ching, and A. L. Richards. 2003. Laboratory diagnosis of two scrub typhus outbreaks at Camp Fuji, Japan in 2000 and 2001 by enzyme-linked immunosorbent assay, rapid flow assay, and Western blot assay using outer membrane 56-KD recombinant proteins. Am. J. Trop. Med. Hyg. 69:60-66. [PubMed] [Google Scholar]
- 25.Kasuya, S., I. Nagano, T. Ikeda, C. Goto, K. Shimokawa, and Y. Takahashi. 1996. Apoptosis of lymphocytes in mice induced by infection with Rickettsia tsutsugamushi. Infect. Immun. 64:3937-3941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kelly, D. J., A. L. Richards, J. J. Temenak, D. Strickman, and G. A. Dasch. 2002. The past and present threat of rickettsial diseases to military medicine and international public health. Clin. Infect. Dis. 34:145-169. [DOI] [PubMed] [Google Scholar]
- 27.Kodama, K., M. Yasukawa, and Y. Kobayashi. 1988. Effect of rickettsial antigen-specific T-cell line on the interaction of Rickettsia tsutsugamushi with macrophages. Microbiol. Immunol. 32:435-439. [DOI] [PubMed] [Google Scholar]
- 28.Kumar, A., W. Weiss, J. A. Tine, S. L. Hoffman, and W. O. Rogers. 2001. ELISPOT assay for detection of peptide specific interferon-gamma secreting cells in rhesus macaques. J. Immunol. Methods 247:49-60. [DOI] [PubMed] [Google Scholar]
- 29.Kumar, S., T. R. Jones, M. S. Oakley, H. Zheng, S. P. Kuppusamy, A. Taye, A. M. Krieg, A. W. Stowers, D. C. Kaslow, and S. L. Hoffman. 2004. CpG oligodeoxynucleotide and Montanide ISA 51 adjuvant combination enhanced the protective efficacy of a subunit malaria vaccine. Infect. Immun. 72:949-957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ley, H. L., Jr., J. E. Smadel, F. H. Diercks, and P. Y. Paterson. 1952. Immunization against scrub typhus. V. The infective dose of Rickettsia tsutsugamushi for men and mice. Am. J. Hyg. 56:313-319. [PubMed] [Google Scholar]
- 31.MacMillan, J. G., R. M. Rice, and T. R. Jerrells. 1985. Development of antigen-specific cell-mediated immune responses after infection of cynomolgus monkeys. J. Infect. Dis. 152:739-749. [DOI] [PubMed] [Google Scholar]
- 32.Mathai, E., J. M. Rolain, G. M. Verghese, O. C. Abraham, D. Mathai, M. Mathai, and D. Raoult. 2003. Outbreak of scrub typhus in Southern India during the cooler months. Ann. N. Y. Acad. Sci. 990:359-364. [DOI] [PubMed] [Google Scholar]
- 33.Nacy, C. A., and M. S. Meltzer. 1979. Macrophages in resistance to rickettsial infection: macrophage activation in vitro for killing of Rickettsia tsutsugamushi. J. Immunol. 123:2544-2549. [PubMed] [Google Scholar]
- 34.Nakamura, R. M., and T. Tokunaga. 1980. Induction of suppressor T cells in delayed-type hypersensitivity to Mycobacterium bovis BCG in low-responder mice. Infect. Immun. 28:331-335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34a.National Research Council. 1996. Guide for the care and use of laboratory animals. Institute of Laboratory Animal Resources, Commission on Life Sciences, National Research Council, National Academy Press, Washington, D.C.
- 35.Ohashi, N., A. Tamura, H. Sakurai, and T. Suto. 1988. Immunoblotting analysis of anti-rickettsial antibodies produced in patients of tsutsugamushi disease. Micrbiol. Immunol. 32:1085-1092. [DOI] [PubMed] [Google Scholar]
- 36.Ohashi, N., A. Tamura, M. Ohta, and K. Hayashi. 1989. Purification and partial characterization of a type-specific antigen of Rickettsia tsutsugamushi. Infect. Immun. 57:1427-1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Palmer, B. A., F. M. Hetrick, and T. R. Jerrells. 1984. Production of gamma interferon in mice immune to Rickettsia tsutsugamushi. Infect. Immun. 43:59-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Palmer, B. A., F. M. Hetrick, and T. R. Jerrells. 1984. Gamma interferon production in response to homologous and heterologous strain antigens in mice chronically infected with Rickettsia tsutsugamushi. Infect. Immun. 46:237-244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ridgway, R. L., S. C. Oaks, Jr., and D. D. LaBarre. 1986. Laboratory animal models for human scrub typhus. Lab. Anim. Sci. 36:481-485. [PubMed] [Google Scholar]
- 40.Riglar, C., and C. Cheers. 1980. Macrophage activation during experimental murine brucellosis. II. Inhibition of in vitro lymphocyte proliferation by brucella-activated macrophages. Cell. Immunol. 49:154-167. [DOI] [PubMed] [Google Scholar]
- 41.Robinson, D. M., E. Gan, T. C. Chan, and D. L. Huxsoll. 1981. Clinical and immunologic responses of silvered leaf monkeys (Presbytis cristatus) to experimental reinfection with Rickettsia tsutsugamushi. J. Infect. Dis. 143:558-561. [DOI] [PubMed] [Google Scholar]
- 42.Rosenberg, R. 1997. Drug-resistant scrub typhus: paradigm and paradox. Parasitol. Today 13:131-132. [DOI] [PubMed] [Google Scholar]
- 43.Seong, S. Y., M. S. Huh, W. J. Jang, S. G. Park, J. G. Kim, S. G. Woo, M. S. Choi, S. Kim, and W. H. Chang. 1997. Induction of homologous immune response to Rickettsia tsutsugamushi Boryong with a partial 56-kilodalton recombinant antigen fused with the maltose-binding protein MBP-Bor56. Infect. Immun. 65:1541-1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shirai, A., R. D. Montrey, R. M. Werner, S. Arimbalam, and D. L. Huxsoll. 1979. Clinical responses of silvered leaf monkeys to infection with selected strains of Rickettsia tsutsugamushi. J. Infect. Dis. 140:811-814. [DOI] [PubMed] [Google Scholar]
- 45.Shirai, A., R. D. Montrey, R. M. Werner, S. Arimbalam, and D. L. Huxsoll. 1979. Comparison of experimental Rickettsia tsutsugamushi infections in silvered leaf (Presbytis cristatus) and cynomolgus (Macaca fascicularis) monkeys. Jpn. J. Med. Sci. Biol. 32:345-351. [DOI] [PubMed] [Google Scholar]
- 46.Smadel, J. E., H. L. Ley, Jr., F. H. Diercks, P. Y. Paterson, C. L. Wisseman, Jr., and R. Traub. 1952. Immunization against scrub typhus: duration of immunity in volunteers following combined living vaccine and chemoprophylaxis. Am. J. Trop. Med. Hyg. 1:87-99. [DOI] [PubMed] [Google Scholar]
- 47.Strickman, D., T. Sheer, K. Salata, J. Hershey, G. Dasch, D. Kelly, and R. Kuschner. 1995. In vitro effectiveness of azithromycin against doxycycline-resistant and -susceptible strains of Rickettsia tsutsugamushi, etiologic agent of scrub typhus. Antimicrob. Agents Chemother. 39:2406-2410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Verthelyi, D., R. T. Kenney, R. A. Seder, A. A. Gam, B. Friedag, and D. M. Klinman. 2002. CpG oligodeoxynucleotides as vaccine adjuvants in primates. J. Immunol. 168:1659-1663. [DOI] [PubMed] [Google Scholar]
- 49.Walker, J. S., F. C. Cadigan, R. A. Vosdingh, and T. C. Chye. 1973. The silvered leaf monkey of Malaysia, Presbytis cristatus: disease model for human scrub typhus. J. Infect. Dis. 128:223-226. [DOI] [PubMed] [Google Scholar]
- 50.Watt, G., C. Chouriyagune, R. Ruangweerayud, P. Watcharapichat, D. Phulsuksombati, K. Jongsakul, P. Teja-Ishavadharm, D. Bhodhidatta, K. D. Corcoran, G. A. Dasch, and D. Strickman. 1996. Scrub typhus infections poorly responsive to antibiotics in northern Thailand. Lancet 348:86-89. [DOI] [PubMed] [Google Scholar]
- 51.Weiss, E., J. C. Coolbaugh, and J. C. Williams. 1975. Separation of viable Rickettsia typhi from yolk sac and L cell host components by renografin density gradient centrifugation. Appl. Microbiol. 30:456-463. [DOI] [PMC free article] [PubMed] [Google Scholar]