Abstract
Background:
Associations between fish consumption and stroke risk have been inconsistent, possibly because of the differences in types of fish meals consumed. Additionally, such relationships have not been specifically evaluated in the elderly, in whom disease burden may be high and diet less influential.
Methods:
Among 4775 adults 65 years or older (range, 65–98 years) and free of known cerebrovascular disease at baseline in 1989–1990, usual dietary intake was assessed using a food frequency questionnaire. In a subset, consumption of tuna or other broiled or baked fish, but not fried fish or fish sandwiches (fish burgers), correlated with plasma phospholipid long-chain n-3 fatty acid levels. Incident strokes were prospectively ascertained.
Results:
During 12 years of follow-up, participants experienced 626 incident strokes, including 529 ischemic strokes. In multivariate analyses, tuna/other fish consumption was inversely associated with total stroke (P=.04) and ischemic stroke (P=.02), with 27% lower risk of ischemic strokewith an intake of 1 to 4 times per week (hazard ratio [HR], 0.73; 95% confidence interval [CI], 0.55–0.98) and 30% lower risk with intake of 5 or more times per week (HR, 0.70; 95% CI, 0.50–0.99) compared with an intake of less than once per month. In contrast, fried fish/fish sandwich consumption was positively associated with total stroke (P=.006) and ischemic stroke (P=.003), with a 44% higher risk of ischemic stroke with consumption of more than once per week (HR, 1.44; 95% CI, 1.12–1.85) compared with consumption of less than once per month. Fish consumption was not associated with hemorrhagic stroke.
Conclusions:
Among elderly individuals, consumption of tuna or other broiled or baked fish is associated with lower risk of ischemic stroke, while intake of fried fish or fish sandwiches is associated with higher risk. These results suggest that fish consumption may influence stroke risk late in life; potential mechanisms and alternate explanations warrant further study.
CARDIOVASCULAR DISEASES are the leading cause of death and disability in the elderly, who are the fastest growing segment of the population; by 2030, it is projected that 70 million persons, or 1 in every 5, will be 65 years or older.1 Studies of fish consumption and stroke risk have yielded inconsistent results,2–7 and none have focused on elderly individuals, in whom disease burden may be high and dietary habits may have less influence. Furthermore, cardiovascular effects of fish intake may vary depending on the type of fish meal consumed; intake of tuna or other broiled or baked fish predicts lower risk of fatal coronary heart disease, while intake of fried fish or fish sandwiches (fish burgers) is associated with trends toward higher risk.8 Determining whether the cardio vascular effects of these fish meals differ is of considerable public health importance, because a large proportion of fish meals consumed in the United States are fried fish or fish sandwiches.9 Also, different types of stroke—ischemic vs hemorrhagic — may be affected differently by fish consumption; however, relationships of fish consumption with different stroke types are not well established.
We therefore evaluated associations of different types of fish meals with risk of incident total stroke and stroke subtypes in the Cardiovascular Health Study (CHS), a population-based, longitudinal cohort study of determinants of cardiovascular events among elderly individuals. Our primary hypothesis was that consumption of tuna and other fish, but not fried fish or fish sandwiches, would be associated with lower risk of total and ischemic stroke.
CME course available at www.archinternmed.com
METHODS
DESIGN AND POPULATION
The design and recruitment experience of the CHS have been described.10,11 Briefly, 5201 men and women 65 years or older were randomly selected and enrolled from Medicare eligibility lists in 4 US communities in 1989–1990; an additional 687 black participants enrolled in 1992 were not included in this analysis because a food frequency questionnaire was not administered to these participants at baseline. Each center’s institutional review committee approved the study, and all subjects gave informed consent. We excluded 333 participants with a history of stroke, transient ischemic attack, or carotid endarterectomy at baseline12 and 90 participants with incomplete data on fish consumption, resulting in 4778 subjects for this analysis. At baseline, participants completed questionnaires on health status, medical history, and cardiovascular risk factors and underwent standardized clinic examination, resting electrocardiography, 2-dimensional echocardiography, carotid ultrasonography, and laboratory evaluation.10–13
DIETARY ASSESSMENT
Usual dietary intake was assessed at baseline using a picture-sort version of the National Cancer Institute food frequency questionnaire.14 Participants were asked to indicate how often, on average, they had consumed various specific foods during the past year, including tuna fish, other broiled or baked fish, and fried fish or fish sandwiches (fish burgers). Nutrient intakes, such as saturated fat intake, were estimated from questionnaire responses and adjusted for total calories using regression analyses.15,16 We have previously reported correlations of fish intake with a biomarker of n-3 fatty acid intake, plasma phospholipid eicosapentaenoic acid (EPA, 20:5n-3) and docosahexaenoic acid (DHA, 22:6n-3), in a subsample of CHS participants.8 Combined EPA + DHA levels correlated with frequency of tuna intake (Spearman correlation [r]=0.35; P<.01) and other fish intake (r=0.59; P<.001), but not fried fish/fish sandwich intake (r=0.04; P=.78), which is consistent with the lean types of fish that are typically fried (eg, cod and pollock).
ASCERTAINMENT OF EVENTS
Potential strokes were identified during annual examinations and interim 6-month Telephone contacts, with centralized adjudication using interviews, medical records, physician questionnaires, death certificates, medical examiner forms, Centers for Medicare and Medicaid Services hospitalizations, and available computed tomographic scans or magnetic resonance images.17,18 Stroke was defined as a neurological deficit of rapid onset lasting longer than 24 hours unless death supervened or as a subarachnoid hemorrhage. Strokes were classified as (1) ischemic if there was evidence of focal brain deficit without evidence for primary hemorrhage; (2) hemorrhagic if there was bloody spinal fluid on lumbar puncture or evidence of blood in the subarachnoid space, ventricles, or parenchyma on cerebral imaging or at surgery or autopsy that did not appear consistent with hemorrhage into an infarction; or (3) unknown type if information was insufficient for classification.
STATISTICAL ANALYSIS
Cox proportional hazards models were used to estimate risk, with censoring at first event, death, or the latest date of adjudicated follow-up through June 30, 2001. Tuna and other fish consumption were correlated (r=0.37: P<.001), and associations of each with risk were similar to associations of tuna/ other fish intake combined. Tuna and other fish consumption were therefore evaluated together (combined correlation with EPA + DHA=0.55; P<.001).8 Fried fish/fish sandwich consumption was modestly correlated with tuna/other fish intake (r=0.14; P<.001) and was evaluated separately. Fish intakes were evaluated as categorical (indicator) variables; given that few persons consumed fried fish/fish sandwiches 5 or more times per week (n=63), these participants were combined with those consuming fried fish/fish sandwiches 1 to 4 times per week. To minimize potential confounding, covariates were selected based on clinical interest, previously published associations with stroke,18 or associations with exposures or outcomes in the current data set. Based on these considerations and the goal of parsimony in covariate selection, 3 final multivariate models are presented: (1) adjusted for cardiovascular risk factors (age, sex, education, diabetes, prevalent coronary heart disease, smoking status, pack-years of smoking, and aspirin use); (2) further adjusted for other risks and lifestyle factors (body mass index, leisure-time physical activity, alcohol use, and total caloric intake); and (3) further adjusted for potential confounders or mediators (systolic blood pressure and low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, triglyceride, and C-reactive protein levels). Other covariates that did not appreciably alter the relations between fish intake and stroke and were therefore excluded from the final models were race, income, enrollment site, hypertension, frequent falls, exercise intensity, diastolic blood pressure, carotid intimal medial thickness, and atrial fibrillation; use of β-blockers, lipid-lowering medication, fish oil, and estrogen; fasting glucose, insulin, fibrinogen, factor VII, and factor VIII; and estimated intake of total fat, saturated fat, linolenic acid, carbohydrates, protein, fiber, wine, thiamine, vitamin A, and vitamin C. Kaplan-Meier survival methods were also used to evaluate stroke-free survival according to tuna/other fish and fried fish/fish sandwich consumption (each adjusted for the other). Intake categories were entered as ordinal variables in tests for trend as well as for evaluation of differences in baseline characteristics using linear (continuous variables) or logistic (dichotomous variables) regression. Likelihood ratio testing using multiplicative interaction terms was used to assess effect modification by age, sex, education, diabetes, coronary heart disease, hypertension, systolic blood pressure, smoking, and aspirin use. All P values are 2-tailed (α=.05). Analyses were performed using Stata 8.0 (Stata Corp, College Station, Tex).
RESULTS
At baseline, mean participant age was 72.7 years (range, 65–98 years). Mean fried fish/fish sandwich and tuna/ other fish consumption were 0.7 and 2.2 servings per week, respectively. Tuna/other fish consumption was associated with younger age, female sex, and higher education, while fried fish/fish sandwich consumption was associated with male sex, nonwhite race, and lower education (Table 1). Tuna/other fish consumption was generally associated with a more favorable cardiovascular risk profile, although body mass index and low-density lipoprotein cholesterol level were higher with greater intake. Tuna/other fish consumption was inversely associated with saturated fat intake and positively associated with intake of total calories, alcohol, fruits, and vegetables; fried fish/fish sandwich consumption was positively associated with intake of total calories, saturated fat, beef/pork, and vegetables.
Table 1.
Baseline Characteristics According to Fish Consumption*
|
Tuna/Other Fish |
Fried Fish/Fish Sandwich |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristic | <1 Time/mo (n = 502) | 1–3 Times/mo (n = 1123) | 1–4 Times/wk (n = 2226) | ≥5 Times/wk (n = 927) | PValue† | <1 Time/mo (n = 2302) | 1–3 Times/mo (n = 1542) | ≥1 Times/wk (n = 934) | PValue† |
| Tuna/other fish intake, servings per week | 0.1 | 0.5 | 2.2 | 5.7 | <.001 | 2.1 | 1.9 | 3.1 | <.001 |
| Fried fish/fish sandwich intake, servings per week | 0.5 | 0.4 | 0.8 | 1.0 | <.01 | 0.1 | 0.5 | 2.7 | <.001 |
| Age, y | 74.2 | 73.2 | 72.5 | 71.8 | <.001 | 72.8 | 72.4 | 72.9 | NS |
| Male sex, % | 46 | 46 | 42 | 34 | <.001 | 37 | 45 | 50 | <.001 |
| White race, % | 93 | 95 | 95 | 95 | NS | 96 | 95 | 92 | <.001 |
| Education ≥ high school diploma, % | 51 | 68 | 76 | 82 | <.001 | 79 | 69 | 62 | <.001 |
| Diabetes, % | 24 | 23 | 22 | 21 | NS | 21 | 22 | 25 | <.05 |
| Coronary heart disease, % | 17 | 18 | 18 | 20 | NS | 18 | 18 | 21 | <.01 |
| Current smoker, % | 15 | 14 | 10 | 10 | <.001 | 12 | 11 | 11 | NS |
| Smoking, pack-years | 19 | 19 | 17 | 17 | <.01 | 17 | 18 | 19 | NS |
| Treated hypertension, % | 45 | 45 | 43 | 44 | NS | 43 | 44 | 45 | NS |
| Systolic blood pressure, mm Hg | 139 | 139 | 139 | 137 | NS | 138 | 139 | 140 | <.001 |
| BMI | 26.1 | 26.4 | 26.4 | 26.7 | NS | 26.1 | 26.6 | 26.8 | <.001 |
| Leisure time activity, kcal/wk | 1608 | 1816 | 1904 | 1858 | NS | 1791 | 1883 | 1909 | NS |
| Internal carotid IMT, mm | 1.6 | 1.5 | 1.5 | 1.5 | NS | 1.5 | 1.5 | 1.5 | <.01 |
| Atrial fibrillation, % | 6 | 6 | 5 | 5 | NS | 6 | 5 | 6 | NS |
| Daily aspirin use, % | 17 | 20 | 19 | 21 | NS | 19 | 18 | 23 | NS |
| LDL-C, mg/dL | 126 | 126 | 131 | 135 | <.001 | 130 | 130 | 131 | NS |
| HDL-C, mg/dL | 52 | 53 | 55 | 55 | <.001 | 56 | 53 | 52 | <.001 |
| Triglycerides, mg/dL | 143 | 142 | 139 | 144 | NS | 139 | 143 | 146 | <.05 |
| C-reactive protein, mg/L | 4.0 | 3.8 | 3.2 | 2.9 | <.001 | 3.1 | 3.6 | 3.7 | <.01 |
| Caloric intake, kcal/d | 1613 | 1614 | 1852 | 2118 | <.001 | 1616 | 1852 | 2282 | <.001 |
| Saturated fat, % calories | 13 | 13 | 12 | 11 | <.001 | 11 | 12 | 13 | <.001 |
| Alcohol, drinks/wk | 1.6 | 2.4 | 3.1 | 2.8 | <.05 | 3.0 | 2.6 | 2.3 | NS |
| Beef or pork, servings/d | 0.9 | 0.8 | 0.9 | 0.8 | NS | 0.7 | 0.9 | 1.2 | <.001 |
| Fruits, servings/d | 1.8 | 1.8 | 2.2 | 2.5 | <.001 | 2.2 | 2.1 | 2.2 | NS |
| Vegetables, servings/d | 1.9 | 1.9 | 2.5 | 3.3 | <.001 | 2.4 | 2.4 | 2.7 | <.001 |
| EPA + DHA, % phospholipids‡ | 2.6 | 3.4 | 3.9 | 4.7 | <.001 | 3.7 | 3.7 | 3.6 | NS |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by the square of height in meters); DHA, docosahexaenoic acid; EPA, eicosapentaenoic acid; HDL-C, high-density lipoprotein cholesterol; IMT, intimal medial thickness; LDL-C, low-density lipoprotein cholesterol; NS, nonsignificant (P≥.05).
SI conversion factors: To convert cholesterol to millimoles per liter, multiply by 0.0259; to convert triglycerides to millimoles per liter, multiply by 0.0113.
Values are mean (continuous variables) or frequency (categorical variables).
P value across categories of intake, after adjustment for age.
Among 64 participants with baseline plasma phospholipids EPA and DHA measurements.
Over 12 years of follow-up, participants experienced 626 incident strokes (529 ischemic, 65 hemorrhagic, and 32 unclassified). When stroke subtypes were separately examined, an additional 8 ischemic and 8 hemorrhagic strokes were included, because censoring occurred only for the stroke type being examined. The Figure presents survival free of stroke according to fish consumption. Incidence of stroke among persons consuming tuna/other fish 5 or more times per week was 12 per 1000 person-years compared with 19 per 1000 person-years among persons consuming tuna/other fish less than once per month (P=.002 for equality of survivor functions). Among persons consuming fried fish/fish sandwiches at least once per week, incidence of stroke was 17 per 1000 person-years compared with 13 per 1000 person-years among persons consuming fried fish/fish sandwiches less than once per month (P=.02 for equality of survivor functions).
Figure.
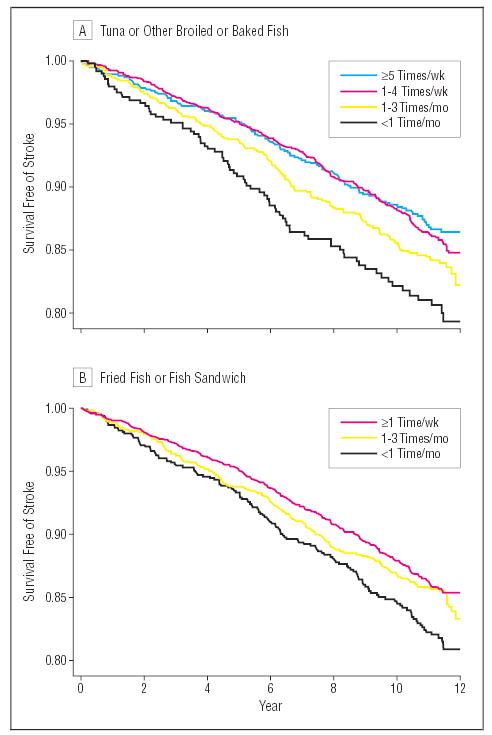
Survival free of stroke, according to tuna/other fish and fried fish/fish sandwich consumption. P=.002 and P=.02 for survival differences according to tuna/other fish (A) and fried fish/fish sandwich (B) intake, respectively (log-rank tests for equality of survivor functions).
After adjustment for age, sex, education, diabetes, prevalent coronary heart disease, smoking status, pack-years of smoking, and aspirin use, consumption of tuna/ other fish was inversely associated with total stroke, with a trend toward 14% lower risk with consumption 1 to 3 times per month (hazard ratio [HR], 0.86; 95% confidence interval [CI], 0.65–1.13), 26% lower risk with consumption 1 to 4 times per week (HR, 0.74; 95% CI, 0.57–0.97), and 28% lower risk with consumption 5 or more times per week (HR, 0.72; 95% CI, 0.53–0.98) compared with a consumption of less than once per month (P for trend, .02) (model 1, Table 2). When stroke subtypes were evaluated, tuna/other fish intake was inversely associated with ischemic stroke, with a trend toward 15% lower risk with consumption 1 to 3 times per month (HR, 0.85; 95% CI, 0.63–1.15), 28% lower risk with consumption 1 to 4 times per week (HR, 0.72; 95% CI, 0.54–0.96), and 32% lower risk with consumption 5 or more times per week (HR, 0.68; 95% CI, 0.48–0.95) compared with a consumption of less than once per month (P for trend, .009) (model 1). Results were not greatly altered by additional adjustment for other potential confounders (model 2) or mediators (model 3), though CIs included unity in some cases owing to fewer numbers of events among persons consuming tuna/other fish 5 or more times per week. There were no significant associations between tuna/other fish intake and hemorrhagic stroke.
Table 2.
Risk of Stroke According to Tuna/Other Fish Consumption*
|
Frequency of Fish Consumption |
|||||
|---|---|---|---|---|---|
| Stroke Risk | <1 Time/mo (n = 502) | 1–3 Times/mo (n = 1123) | 1–4 Times/wk (n = 2226) | ≥5 Times/wk (n = 927) | Pfor Trend |
| Total stroke | (n = 78) | (n = 154) | (n = 284) | (n = 110) | |
| Age adjusted | 1.0 (Referent) | 0.85 (0.64–1.11) | 0.74 (0.58–0.96) | 0.71 (0.53–0.95) | .01 |
| Model 1† | 1.0 (Referent) | 0.86 (0.65–1.13) | 0.74 (0.57–0.97) | 0.72 (0.53–0.98) | .02 |
| Model 2‡ | 1.0 (Referent) | 0.87 (0.65–1.15) | 0.75 (0.57–0.98) | 0.74 (0.54–1.02) | .04 |
| Model 3§ | 1.0 (Referent) | 0.88 (0.66–1.17) | 0.74 (0.56–0.98) | 0.77 (0.56–1.07) | .06 |
| Ischemic stroke | (n = 69) | (n = 135) | (n = 242) | (n = 91) | |
| Age adjusted | 1.0 (Referent) | 0.84 (0.62–1.12) | 0.71 (0.54–0.93) | 0.65 (0.47–0.89) | .003 |
| Model 1† | 1.0 (Referent) | 0.85 (0.63–1.15) | 0.72 (0.54–0.96) | 0.68 (0.48–0.95) | .009 |
| Model 2‡ | 1.0 (Referent) | 0.87 (0.64–1.17) | 0.73 (0.55–0.98) | 0.70 (0.50–0.99) | .02 |
| Model 3§ | 1.0 (Referent) | 0.89 (0.65–1.21) | 0.73 (0.54–0.98) | 0.72 (0.51–1.03) | .03 |
| Hemorrhagic stroke | (n = 8) | (n = 12) | (n = 37) | (n = 16) | |
| Age adjusted | 1.0 (Referent) | 0.63 (0.26–1.55) | 0.96 (0.44–2.09) | 1.00 (0.42–2.37) | .53 |
| Model 1† | 1.0 (Referent) | 0.58 (0.23–1.45) | 0.86 (0.39–1.92) | 0.89 (0.36–2.19) | .72 |
| Model 2‡ | 1.0 (Referent) | 0.57 (0.23–1.44) | 0.86 (0.39–1.93) | 0.93 (0.37–2.33) | .66 |
| Model 3§ | 1.0 (Referent) | 0.58 (0.23–1.46) | 0.84 (0.38–1.89) | 0.98 (0.39–2.46) | .63 |
Data are hazard ratios (95% confidence intervals) unless otherwise specified. All models include both tuna/other fish and fried fish/fish sandwich intake.
Adjusted for cardiovascular risk factors (age, sex, education, diabetes, prevalent coronary heart disease, smoking status, pack-years of smoking, and aspirin use).
Further adjusted for other risks and lifestyle factors (body mass index, leisure-time physical activity, alcohol use, and total caloric intake).
Further adjusted for potential confounders/mediators (systolic blood pressure and low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, triglyceride, and C-reactive protein levels).
In contrast, fried fish/fish sandwich consumption was associated with higher risk of stroke (Table 3). After multivariate adjustments (model 2), consumption of at least once per week was associated with 37% higher risk of total stroke (HR, 1.37; 95% CI, 1.09–1.73) and 44% higher risk of ischemic stroke (HR, 1.44; 95% CI, 1.12–1.85) compared with a consumption of less than once per month. Higher risk appeared graded with increasing intake (P for trend, .006 for total stroke and .003 for ischemic stroke; model 2). Evaluated continuously, each serving per week predicted a 10% higher risk of total stroke (HR, 1.10; 95% CI, 1.02–1.19) and 13% higher risk of ischemic stroke (HR, 1.13; 95% CI, 1.04–1.22) (adjustments as in model 2).
Table 3.
Risk of Stroke According to Fried Fish/Fish Sandwich Consumption*
|
Frequency of Fish Consumption |
||||
|---|---|---|---|---|
| Stroke Risk | <1 Time/mo (n = 2302) | 1–3 Times/mo (n = 1542) | ≥1 Times/wk (n = 934) | Pfor Trend |
| Total stroke | (n = 288) | (n = 201) | (n = 137) | |
| Age adjusted | 1.0 (Referent) | 1.13 (0.95–1.36) | 1.34 (1.09–1.66) | .005 |
| Model 1† | 1.0 (Referent) | 1.15 (0.95–1.39) | 1.30 (1.04–1.61) | .02 |
| Model 2‡ | 1.0 (Referent) | 1.17 (0.97–1.42) | 1.37 (1.09–1.73) | .006 |
| Model 3§ | 1.0 (Referent) | 1.14 (0.94–1.38) | 1.33 (1.05–1.68) | .02 |
| Ischemic stroke | (n = 243) | (n = 173) | (n = 121) | |
| Age adjusted | 1.0 (Referent) | 1.16 (0.95–1.41) | 1.43 (1.14–1.79) | .002 |
| Model 1† | 1.0 (Referent) | 1.17 (0.96–1.43) | 1.36 (1.08–1.72) | .008 |
| Model 2‡ | 1.0 (Referent) | 1.19 (0.97–1.46) | 1.44 (1.12–1.85) | .003 |
| Model 3§ | 1.0 (Referent) | 1.15 (0.94–1.42) | 1.39 (1.08–1.79) | .01 |
| Hemorrhagic stroke | (n = 37) | (n = 22) | (n = 14) | |
| Age adjusted | 1.0 (Referent) | 0.92 (0.54–1.57) | 0.94 (0.90–1.76) | .81 |
| Model 1† | 1.0 (Referent) | 0.92 (0.52–1.61) | 0.98 (0.51–1.88) | .90 |
| Model 2‡ | 1.0 (Referent) | 0.96 (0.54–1.70) | 1.06 (0.53–2.11) | .91 |
| Model 3§ | 1.0 (Referent) | 0.98 (0.55–1.74) | 1.10 (0.55–2.19) | .84 |
Data are hazard ratios (95% confidence intervals) unless otherwise specified.
Adjusted for cardiovascular risk factors (age, sex, education, diabetes, prevalent coronary heart disease, smoking status, pack-years of smoking, and aspirin use).
Further adjusted for other risks and lifestyle factors (body mass index, leisure-time physical activity, alcohol use, and total caloric intake).
Further adjusted for potential confounders/mediators (systolic blood pressure and low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, triglyceride, and C-reactive protein levels).
Exclusion of participants using fish oil supplements (n=178) or with atrial fibrillation (n=261) at baseline had little effect (not shown). There was little evidence for interaction between tuna/other fish and fried fish/ fish sandwich intake (P for interaction, .22, .39, and .27 for total, ischemic, and hemorrhagic stroke, respectively). There was also little evidence that findings varied by age, sex, education, diabetes, prevalent coronary heart disease, treated hypertension, systolic blood pressure, smoking, or aspirin use (P>.05 for each interaction).
Fish intake was assessed at baseline, and dietary habits may have changed over time, either owing to morbidity or regression to the mean. Such changes might result in bias toward the null over time. To evaluate this possibility, we divided the follow-up into 2 roughly equal halves and separately investigated associations in the first period (nearer to diet assessment) and the second period (further from diet assessment). As would be expected if there were changes in intake over time, associations between tuna/other fish consumption and stroke risk appeared stronger in the first period (Table 4), with consumption of 1 to 4 times per week associated with 39% lower risk of total stroke (HR, 0.61; 95% CI, 0.43–0.87) and 41% lower risk of ischemic stroke (HR, 0.59; 95% CI, 0.40–0.86) compared with a consumption of less than once per month (adjustments as in model 3). Risk estimates for fried fish/fish sandwich consumption were similar in both periods, suggesting potentially fewer changes in intake over time. Because socioeconomic status may relate to tendency or capability to change one’s diet, we also stratified these analyses by educational attainment. Movement of risk estimates toward the null over time was more notable among those with greater education (high school diploma or greater) compared with less education (less than a high school diploma) (not shown), though broad CIs in these subgroups limited confirmation of such differences. Associations of fish intake with hemorrhagic stroke were not statistically significant in either period (not shown).
Table 4.
Risk of Stroke According to Fish Consumption by Period of Follow-up*
|
Frequency of Fish Consumption |
|||||
|---|---|---|---|---|---|
| Stroke Risk | <1 Time/mo | 1–3 Times/mo | 1–4 Times/wk | ≥5 Times/wk | Pfor Trend |
| Tuna/Other Fish Intake | |||||
| Total stroke | |||||
| Baseline to 6 y | 1.0 (Referent) | 0.80 (0.56–1.15) | 0.61 (0.43–0.87) | 0.69 (0.45–1.06) | .03 |
| 6 to 12 y | 1.0 (Referent) | 1.04 (0.65–1.67) | 0.99 (0.63–1.55) | 0.93 (0.55–1.56) | .66 |
| Ischemic stroke | |||||
| Baseline to 6 y | 1.0 (Referent) | 0.78 (0.53–1.15) | 0.59 (0.40–0.86) | 0.65 (0.41–1.03) | .02 |
| 6 to 12 y | 1.0 (Referent) | 1.15 (0.68–1.95) | 1.04 (0.63–1.71) | 0.91 (0.51–1.61) | .49 |
| Fried Fish/Fish Sandwich Intake | |||||
| Total stroke | |||||
| Baseline to 6 y | 1.0 (Referent) | 1.21 (0.93–1.58) | 1.30 (0.94–1.79) | † | .08 |
| 6 to 12 y | 1.0 (Referent) | 1.08 (0.81–1.43) | 1.40 (1.00–1.98) | † | .07 |
| Ischemic stroke | |||||
| Baseline to 6 y | 1.0 (Referent) | 1.19 (0.89–1.58) | 1.31 (0.93–1.85) | † | .10 |
| 6 to 12 y | 1.0 (Referent) | 1.14 (0.84–1.55) | 1.53 (1.06–2.22) | † | .03 |
Values are hazard ratios (95% confidence intervals), with adjustments as in model 3 (Table 2). Follow-up is divided into 2 periods: baseline to 6 years (nearer to diet assessment) and 6 to 12 years (further from diet assessment). With fewer events, associations with hemorrhagic stroke were not significant in either period and are not shown.
The few individuals consuming fried fish/fish sandwiches 5 or more times per week (n = 63) were combined with those consuming fried fish/fish sandwiches 1 to 4 times per week.
COMMENT
In this population-based, prospective study among elderly adults, consumption of tuna or other broiled or baked fish was associated with lower incidence of stroke. This relationship was present after adjustment for a variety of demographic, clinical, lifestyle, and dietary characteristics. However, these findings do not prove causality. The observed relationship may be due to residual confounding from other factors associated with both fish intake and stroke risk, such as residual differences in socioeconomic status not accounted for by our adjustment for education, clinical risk factors, smoking, alcohol use, and physical activity.
On the other hand, there are plausible biological mechanisms for beneficial effects of tuna/other fish intake on incidence of stroke, particularly ischemic stroke. In experimental studies, n-3 fatty acids from fatty fish influence blood pressure, lipid levels, inflammatory responses, red blood cell deformability, endothelial cell function, and cerebral arteriolar reactivity.19–22 Each of these effects, separately or in combination, may plausibly reduce risk of ischemic stroke. While we were unable to evaluate each of these potential effects, the findings appeared independent of baseline differences in blood pressure, serum lipid levels, and C-reactive protein level.
Frequent intake of tuna/other fish (≥5 servings per week) was not associated with substantially lower stroke risk compared with modest intake (1–4 servings per week). Confidence intervals for persons with frequent consumption were broader owing to fewer events (110 vs 284 strokes), so a graded relationship with risk cannot be excluded by these data. However, a potential threshold effect of fish intake, as also suggested in a prior report,7 is compatible with in vivo pharmakinetics of n-3 fatty acids from fish, which produce changes in fatty acid composition in cell membranes that persist for days to weeks.23
Associations between tuna/other fish intake and total and ischemic stroke risk appeared stronger in the first half of follow-up (closer to dietary assessment) compared with the latter half (further from dietary assessment). These effects appeared possibly greater among those with higher education, which may reflect greater use of antiatherosclerotic treatments over time and could attenuate the benefits of fish intake or the greater tendency or capability to change one’s diet. If there is bias toward the null owing to dietary changes over time, the estimates of risk observed in the first half of follow-up may better represent associations between tuna/other fish intake and stroke risk, suggesting a 35% to 40% lower risk of ischemic stroke with consumption of 1 or more servings per week compared with little or no consumption (<1 time per month).
Tuna/other fish consumption was not associated with hemorrhagic stroke. Ecological studies in Greenland and Alaska have suggested a higher risk of hemorrhagic stroke with high dietary n-3 fatty acid intake, which was thought possibly due to antiplatelet effects.24,25 However, the n-3 fatty acid content of these diets was markedly higher than in most populations, and in experimental studies, n-3 fatty acids only affect bleeding times at pharmacologic doses (3–15 g/d).26,27 Our findings may be limited by the small number of hemorrhagic strokes. However, our results, together with those of prior cohort studies,6,7 suggest that modest consumption of tuna or other broiled or baked fish does not significantly increase risk of hemorrhagic stroke, particularly relative to potential benefits on risk of ischemic stroke.
We separately examined fried fish/fish sandwich consumption, hypothesizing that such fish meals—generally lean and not associated with n-3 fatty acid levels—would have different associations with stroke compared with tuna/other fish. The observed higher risks of total and ischemic stroke are consistent with associations of fried fish/fish sandwich consumption with incidence of coronary heart disease.8 While we could not separately evaluate the type of fish vs the preparation method, it seems less likely that consumption of lean fish per se would increase stroke risk. Fried fish/fish sandwich consumption may be a marker for some other factor that increases cardiovascular risk; however, observed relationships were independent of a wide variety of participant characteristics. Plausible potential mechanisms for increased risk include the preparation method, since frying can greatly alter a fish meal’s nutrient composition (eg, increasing the n-6:n-3 ratio).28 trans-Fatty acids and lipid oxidation products in fried fats and oils, especially oils used repeatedly for frying, may also increase cardiovascular risk.29,30 Further investigation is necessary to confirm these observations, to determine if they are specific for certain kinds of fish or frying oils, and to examine potential mechanisms and alternative explanations.
Results of prior epidemiologic studies of fish consumption and stroke have been inconsistent,2–7 possibly owing to differences in fish intake in the reference group or in types of fish meals consumed; for example, prior studies did not separately evaluate fried fish/fish sandwich intake. Stroke risk was not affected in a trial of low-dose n-3 fatty acid supplementation for secondary prevention of coronary heart disease; however, there was high fish intake in the placebo group (73%–87% consumed fish ≥1 time per week) and low overall stroke incidence (1.6%).31 Randomized trials of fish consumption for stroke prevention have not been reported.
Our analysis has several strengths. The prospective design and exclusion of persons with known cardiovascular disease at baseline reduce potential bias from recall differences or dietary changes due to known disease. The population-based recruitment strategy enhances generalizability. Standardized assessment of a wide variety of participant characteristics increases capacity to adjust for confounding. Close follow-up and centralized adjudication reduce potential for missed or misclassified outcomes.
There are potential limitations to our findings. Fish intake was assessed at baseline and may have changed over time; also, we could not assess differences within each response category of the food frequency questionnaire. Without apparent bias, such misclassification would diminish the ability to detect relationships, so our findings may underestimate associations between fish consumption and stroke risk. Such misclassification may also limit determinations of thresholds of effect. We could not separately evaluate the type of fish vs the preparation method. Additionally, while we adjusted for a variety of participant characteristics, we cannot exclude residual confounding by unmeasured or imprecisely measured factors.
Given the rising proportion of older adults in most populations, their cardiovascular disease burden, and the possibility that dietary habits may have less influence late in life, it is important to examine relationships between diet and cardiovascular risk in the elderly. Although the observed associations may reflect dietary habits earlier in life, our findings suggest that diet may influence stroke risk beyond the earlier development of cardiovascular disease in young adulthood and middle age. Our findings also suggest that n-3 fatty acid content or preparation methods may be important when considering relationships of fish intake with stroke risk. Continued elucidation of relationships and mechanisms of benefit and risk, with attention to different types of fish meals, is warranted.
Acknowledgments
We wish to acknowledge the contribution of each of the participants in the Cardiovascular Health Study (CHS), without whom this study would not be possible. For a full list of participating CHS investigators and institutions, see “About CHS: Principal Investigators and Study Sites,” at http://chs-nhlbi.org.
Footnotes
Funding/Support: The research reported in this article was supported by contracts N01-HC-85079 through N01-HC-85086, N01-HC-35129, and N01 HC-15103 from the National Heart, Lung, and Blood Institute, US Department of Health and Human Services, Bethesda, Md. Support for Dr Mozaffarian was provided in part by a National Research Service Award Training Grant in Academic Nutrition (DK07703) at the Harvard School of Public Health, Boston, Mass.
Previous Presentation: An abstract of this study was presented at the American Heart Association Scientific Sessions; November 17–22, 2002; Chicago, Ill.
Financial Disclosure: None.
References
- 1.US Census Bureau. Index of /population/projections/nation/summary. Available at: http://www.census.gov/population/projections/nation/summary Accessed September 23, 2002.
- 2.Keri SO, Feskens EJM, Kromhout D. Fish consumption and risk of stroke: the Zutphen Study. Stroke. 1994;25:328–332. doi: 10.1161/01.str.25.2.328. [DOI] [PubMed] [Google Scholar]
- 3.Morris MC, Manson JE, Rosner B, Buring JE, Willett WC, Hennekens CH. Fish consumption and cardiovascular disease in the Physicians’ Health Study. Am J Epidemiol. 1995;142:166–175. doi: 10.1093/oxfordjournals.aje.a117615. [DOI] [PubMed] [Google Scholar]
- 4.Orencia AJ, Daviglus ML, Dyer AR, Shekelle RB, Stamler J. Fish consumption and stroke in men: 30-year findings, Chicago Western Electric study. Stroke. 1996;27:204–209. doi: 10.1161/01.str.27.2.204. [DOI] [PubMed] [Google Scholar]
- 5.Gillum RF, Mussolino ME, Madans JH. Relationship between fish consumption and stroke incidence: NHANES I. Arch Intern Med. 1996;156:537–542. [PubMed] [Google Scholar]
- 6.Iso H, Rexrode KM, Stampfer MJ, et al. Intake of fish and omega-3 fatty acids and risk of stroke in women. JAMA. 2001;285:304–312. doi: 10.1001/jama.285.3.304. [DOI] [PubMed] [Google Scholar]
- 7.He K, Rimm EB, Merchant A, et al. Fish consumption and risk of stroke in men. JAMA. 2002;288:3130–3136. doi: 10.1001/jama.288.24.3130. [DOI] [PubMed] [Google Scholar]
- 8.Mozaffarian D, Lemaitre RN, Kuller LH, Burke GL, Tracy RP, Siscovick DS. Cardiac benefits of fish consumption may depend on the type of fish meal consumed: the Cardiovascular Health Study. Circulation. 2003;107:1372–1377. doi: 10.1161/01.cir.0000055315.79177.16. [DOI] [PubMed] [Google Scholar]
- 9.National Marine Fisheries Service. Fisheries of the US—2000. Silver Spring, Md: US Dept of Commerce; 2001.
- 10.Fried LP, Borhani NO, Enright P, et al. The Cardiovascular Health Study: design and rationale. Ann Epidemiol. 1991;1:263–276. doi: 10.1016/1047-2797(91)90005-w. [DOI] [PubMed] [Google Scholar]
- 11.Tell GS, Fried LP, Hermanson B, Manolio TA, Newman AB, Borhani NO. Recruitment of adults 65 years and older as participants in the Cardiovascular Health Study. Ann Epidemiol. 1993;3:358–366. doi: 10.1016/1047-2797(93)90062-9. [DOI] [PubMed] [Google Scholar]
- 12.Psaty BM, Kuller LH, Bild D, et al. Methods of assessing prevalent cardiovascular disease in the Cardiovascular Health Study. Ann Epidemiol. 1995;5:270–277. doi: 10.1016/1047-2797(94)00092-8. [DOI] [PubMed] [Google Scholar]
- 13.Cushman M, Cornell ES, Howard PR, Bovill EG, Tracy RP. Laboratory methods and quality assurance in the Cardiovascular Health Study. Clin Chem. 1995;41:264–270. [PubMed] [Google Scholar]
- 14.Kumanyika SK, Tell GS, Shemanski L, et al. Dietary assessment using a picture-sort approach. Am J Clin Nutr. 1997;65:1123S–1129S. doi: 10.1093/ajcn/65.4.1123S. [DOI] [PubMed] [Google Scholar]
- 15.Smucker R, Block G, Coyle L, et al. A dietary and risk factor questionnaire and analysis system for personal computers. Am J Epidemiol. 1989;129:445–449. doi: 10.1093/oxfordjournals.aje.a115149. [DOI] [PubMed] [Google Scholar]
- 16.Willett W, Stampfer MJ. Total energy intake: implications for epidemiologic analyses. Am J Epidemiol. 1986;124:17–27. doi: 10.1093/oxfordjournals.aje.a114366. [DOI] [PubMed] [Google Scholar]
- 17.Ives DG, Fitzpatrick AL, Bild DE, et al. Surveillance and ascertainment of cardiovascular events: the Cardiovascular Health Study. Ann Epidemiol. 1995;5:278–285. doi: 10.1016/1047-2797(94)00093-9. [DOI] [PubMed] [Google Scholar]
- 18.Longstreth WT, Jr, Bernick C, Fitzpatrick A, et al. Frequency and predictors of stroke death in 5,888 participants in the Cardiovascular Health Study. Neurology. 2001;56:368–375. doi: 10.1212/wnl.56.3.368. [DOI] [PubMed] [Google Scholar]
- 19.Agren JJ, Hanninen O, Hanninen A, Seppanen K. Dose responses in platelet fatty acid composition, aggregation and prostanoid metabolism during moderate freshwater fish diet. Thromb Res. 1990;57:565–575. doi: 10.1016/0049-3848(90)90073-l. [DOI] [PubMed] [Google Scholar]
- 20.Ellis EF, Police RJ, Dodson LY, McKinney JS, Holt SA. Effect of dietary n-3 fatty acids on cerebral microcirculation. Am J Physiol. 1992;262:H1379–H1386. doi: 10.1152/ajpheart.1992.262.5.H1379. [DOI] [PubMed] [Google Scholar]
- 21.Knapp HR. n-3 Fatty acids and human hypertension. Curr Opin Lipidol. 1996;7:30–33. doi: 10.1097/00041433-199602000-00007. [DOI] [PubMed] [Google Scholar]
- 22.Nestel PJ. Fish oil and cardiovascular disease: lipids and arterial function. Am J Clin Nutr. 2000;71:228S–231S. doi: 10.1093/ajcn/71.1.228S. [DOI] [PubMed] [Google Scholar]
- 23.Katan MB, Deslypere JP, van Birgelen AP, Penders M, Zegwaard M. Kinetics of incorporation of dietary fatty acids into serum cholesteryl esters, erythrocyte membranes, and adipose tissue. J Lipid Res. 1997;38:2012–2022. [PubMed] [Google Scholar]
- 24.Kromann N, Green A. Epidemiological studies in Upernavik, Greenland: incidence of some chronic diseases, 1950–1974. Acta Med Scand. 1980;208:401–406. [PubMed] [Google Scholar]
- 25.Middaugh JP. Cardiovascular deaths among Alaskan Natives, 1980–86. Am J Public Health. 1990;80:282–285. doi: 10.2105/ajph.80.3.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Parkinson AJ, Cruz AL, Heyward WL, et al. Elevated concentrations of plasma omega-3 fatty acids among Alaskan Eskimos. Am J Clin Nutr. 1994;59:384–388. doi: 10.1093/ajcn/59.2.384. [DOI] [PubMed] [Google Scholar]
- 27.Knapp HR, Reilly IA, Alessandrini P, FitzGerald GA. In vivo indexes of platelet and vascular function during fish-oil administration in patients with atherosclerosis. N Engl J Med. 1986;314:937–942. doi: 10.1056/NEJM198604103141501. [DOI] [PubMed] [Google Scholar]
- 28.Candela M, Astiasaran I, Bello J. Deep-fat frying modifies high-fat fish lipid fraction. J Agric Food Chem. 1998;46:2793–2796. [Google Scholar]
- 29.Ascherio A, Katan MB, Zock PL, Stampfer MJ, Willett WC. trans-Fatty acids and coronary heart disease. N Engl J Med. 1999;340:1994–1998. doi: 10.1056/NEJM199906243402511. [DOI] [PubMed] [Google Scholar]
- 30.Williams MJ, Sutherland WH, McCormick MP, de Jong SA, Walker RJ, Wilkins GT. Impaired endothelial function following a meal rich in used cooking fat. J Am Coll Cardiol. 1999;33:1050–1055. doi: 10.1016/s0735-1097(98)00681-0. [DOI] [PubMed] [Google Scholar]
- 31.GISSI-Investigators Dietary supplementation with n-3 polyunsaturated fatty acids and vitamin E after myocardial infarction: GISSI-Prevenzione trial. Lancet. 1999;354:447–455. [PubMed] [Google Scholar]


