Abstract
Background—Consumption of polyunsaturated fatty acids (PUFAs) may reduce coronary heart disease (CHD) risk, but n-6 PUFAs may compete with n-3 PUFA metabolism and attenuate benefits. Additionally, seafood-based, long-chain n-3 PUFAs may modify the effects of plant-based, intermediate-chain n-3 PUFAs. However, the interactions of these PUFAs in relation to CHD risk are not well established.
Methods and Results—Among 45 722 men free of known cardiovascular disease in 1986, usual dietary intake was assessed at baseline and every 4 years by using validated food-frequency questionnaires. CHD incidence was prospectively ascertained. Over 14 years of follow-up, participants experienced 218 sudden deaths, 1521 nonfatal myocardial infarctions (MIs), and 2306 total CHD events (combined sudden death, other CHD deaths, and nonfatal MI). In multivariate-adjusted analyses, both long-chain and intermediate-chain n-3 PUFA intakes were associated with lower CHD risk, without modification by n-6 PUFA intake. For example, men with ≥ median long-chain n-3 PUFA intake (≥ 250 mg/d) had a reduced risk of sudden death whether n-6 PUFA intake was below (<11.2 g/d; hazard ratio [HR] = 0.52; 95% confidence interval [CI] = 0.34 to 0.79) or above (≥ 11.2 g/d; HR = 0.60; 95% CI = 0.39 to 0.93) the median compared with men with a < median intake of both. In similar analyses, ≥ median intake of intermediate-chain n-3 PUFAs (≥ 1080 mg/d) was associated with a reduced total CHD risk whether n-6 PUFA intake was lower (HR = 0.88; 95% CI = 0.78 to 0.99) or higher (HR = 0.89; 95% CI = 0.79 to 0.99) compared with a < median intake of both. Intermediate-chain n-3 PUFAs were particularly associated with CHD risk when long-chain n-3 PUFA intake was very low (<100 mg/d); among these men, each 1 g/d of intermediate-chain n-3 PUFA intake was associated with an ≈ 50% lower risk of nonfatal MI (HR = 0.42; 95% CI = 0.23 to 0.75) and total CHD (HR = 0.53; 95% CI = 0.34 to 0.83).
Conclusions—n-3 PUFAs from both seafood and plant sources may reduce CHD risk, with little apparent influence from background n-6 PUFA intake. Plant-based n-3 PUFAs may particularly reduce CHD risk when seafood-based n-3 PUFA intake is low, which has implications for populations with low consumption or availability of fatty fish.
Keywords: coronary disease, diet, fatty acids, nutrition
Intake of polyunsaturated fatty acids (PUFAs) may influence coronary heart disease (CHD) risk. n-6 PUFAs, such as linoleic acid found in vegetable oils, may reduce CHD risk as a result of favorable effects on serum lipids, insulin sensitivity, or hemostatic factors.1,2 n-3 PUFAs, derived from seafood and plant sources, may also reduce CHD risk,3–16 particularly the risk of arrhythmic death.11–16 Compared with traditional diets, patterns of PUFA intake in industrialized nations have shifted markedly during the past 150 years toward higher amounts of n-6 PUFAs and lower amounts of n-3 PUFAs, with parallel increases in CHD incidence in ecological studies.17,18 Experimental evidence suggests that n-6 PUFAs may compete with n-3 PUFAs for common metabolic enzymes and thereby increase the production of prothrombotic rather than antithrombotic, aggregatory, and inflammatory leukotrienes, thromboxanes, and prostaglandins (Figure 1).17,19–23 n-6 and n-3 PUFAs may also compete during their incorporation (esterification) into plasma lipid fractions (eg, phospholipids and triglycerides).24 These ecological and experimental data have raised concerns that n-6 PUFAs may counteract the potential cardiovascular benefits of n-3 PUFAs, resulting in national and international recommendations regarding relative intakes of n-6 and n-3 fatty acids.17,18 However, few prospective studies have evaluated the interplay between n-6 and n-3 PUFAs and CHD risk. The potential competition between n-6 and n-3 PUFAs may be most relevant for intermediate-chain n-3 α-linolenic acid (18:3, ALA), which requires desaturation and elongation to form longer-chain metabolites, compared with long-chain n-3 eicosapentaenoic acid (20:5, EPA) and docosahexaenoic acid (22:6, DHA), which do not require these enzymes for metabolism (Figure 1). Effects of intermediate-chain n-3 PUFAs may also be influenced by long-chain n-3 PUFAs; eg, EPA may regulate ALA elongation via feedback inhibition (Figure 1), and thus, plant-based, intermediate-chain n-3 PUFAs (ALA) may only influence CHD risk when intake of seafood-based, long-chain n-3 PUFAs (EPA + DHA) is low.25
Figure 1.
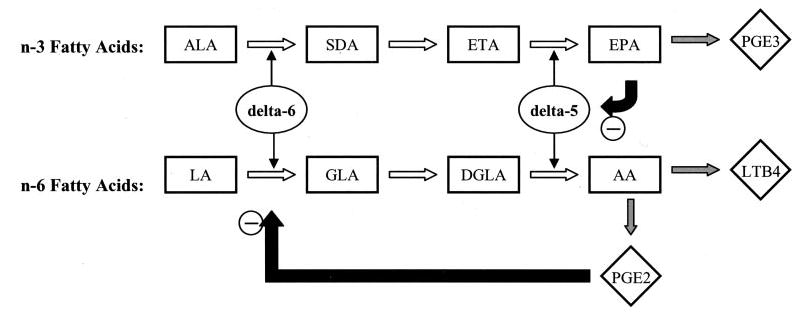
Metabolism of n-6 and n-3 PUFAs. δ-5 and δ-6 desaturase enzymes (ovals) are active in both n-3 and n-6 fatty acid metabolism, converting intermediate-chain n-3 ALA to long-chain n-3 EPA and n-6 linoleic acid (LA) to n-6 arachidonic acid (AA). EPA is converted to prostaglandin E3 (PGE3), an eicosanoid with potential antiinflammatory and antithrombotic effects, whereas AA is converted to PGE2 and leukotriene B4 (LTB4), both proinflammatory eicosanoids. Thus, n-3 and n-6 fatty acids compete for common metabolic enzymes, and relative intake of these fatty acids has been hypothesized to determine potential proinflammatory vs antiinflammatory, thrombotic, and aggregatory effects. Metabolites in these pathways also exert feedback inhibition (black arrows); eg, long-chain n-3 EPA inhibits an important step in the elongation of intermediate-chain n-3 ALA. SDA indicates stearidonic acid (octadecatetranoic acid); ETA, eicosatetraenoic acid; GLA, γ-linolenic acid; and DGLA, dihomo-γ-linolenic acid. Other abbreviations are as defined in text.
Thus, each of these PUFAs may modify the others’ relations with CHD risk. However, such potential interactions are not well established. These relations are of considerable public health importance, given the ubiquity of n-6 PUFAs in the diet, the strong evidence for beneficial effects of n-3 PUFAs on CHD risk, and the low availability of seafood sources compared with plant sources of n-3 PUFAs in many populations. We therefore investigated the associations between different patterns of intake of these PUFAs and incident CHD among 45 722 men in the Health Professionals Follow-up Study.
Methods
Design and Population
The Health Professionals Follow-up Study is a cohort study among 51 529 male, US health professionals aged 40 to 75 years at baseline in 1986. Health information and disease status have been assessed biennially by self-administered questionnaires that included questions about medical examinations, medications, smoking, alcohol use, weight, height, physical activity, blood pressure, and cholesterol levels.26–28 Family history of CHD has been updated periodically. Questionnaire response rates averaged between 92% and 96%, with an overall follow-up rate of 96.4% for all person-times from 1986 through 2000. Nonrespondents were assumed to be alive if not listed in the National Death Index. The Harvard institutional review committee approved the study, and all subjects gave implied informed consent through return of mailed questionnaires. For the present analysis, we excluded 4175 men with prevalent cardiovascular disease at baseline and 1632 men with implausible total energy intake at baseline (<800 or >4200 kcal/d), resulting in 45 722 participants included in this analysis.
Dietary Assessment
A 131-item, semiquantitative, food-frequency questionnaire (FFQ) was administered at baseline and every 4 years thereafter to assess usual dietary intake.29,30 On each questionnaire, participants were asked to indicate how often, on average, they had consumed given amounts of various specified foods during the past year. The FFQ includes open-ended sections for foods and supplements not specifically listed, including breakfast cereal, multivitamin supplements, margarine, and vegetable oil used for frying or baking. Small adjustments were made to the FFQ in 1994 and 1998 to incorporate new products. Nutrient intakes were calculated as the frequency of intake multiplied by the nutrient composition of the specified portion size, computed with and without vitamin and mineral supplements, and modified by responses to the open-ended questions. Nutrient estimates were based on US Department of Agriculture31 and Harvard University food composition database sources. We adjusted all nutrient values for total energy intake by regression analyses.32,33
The reproducibility and validity of the FFQ have been described in detail.29,30 Adjusted for energy and within-person variation, correlation coefficients for total and types of fat when compared with two 1-week dietary records ranged from 0.37 to 0.75.29 Correlations for EPA and n-6 fatty acids as assessed by the FFQ versus the proportion in adipose tissue were 0.47 and 0.50, respectively.30 Our use of multiple FFQs over time to compute cumulative averages of dietary intake reduces measurement error and provides more stable estimates of average dietary intake.33 Because more recent n-3 PUFA intake may be more relevant to clinical CHD events than distant intake,25,34 greater weight was given to the most recent FFQ compared with prior FFQs. Thus, CHD incidence from 1990 to 1994 was related to the average dietary intakes reported in 1986 and 1990; CHD incidence from 1994 to 1998 to the average of (averaged intakes reported in 1986 and 1990) and intake reported in 1994, etc. Because intermediate events may lead to systematic changes in dietary intake, we stopped updating dietary information after new diagnoses of angina, coronary bypass surgery, hypercholesterolemia, hypertension, diabetes, or stroke. Results were similar with continued updating after intermediate events or using other updating methods, such as simple updating or cumulative updating with long-term averaging; therefore, only results from the primary method of updating are presented.
Events
Methods for ascertainment and classification of outcomes have been described.35 In brief, when an outcome of interest was reported, we sought permission from participants (or next of kin for fatal events) to review medical records, which were used to confirm and classify self-reported diagnoses against standardized criteria by physicians blinded to the information reported on the questionnaires. Deaths were ascertained from relatives, postal authorities, or the National Death Index, and cause of death was classified according to medical records, death certificates, and autopsy findings. Permission for medical record review was granted for 95% of all requests. Myocardial infarction (MI) was diagnosed according to World Health Organization criteria,36 supplemented after 1998 by guidelines accounting for troponin measurements. CHD death was diagnosed by autopsy findings, medical records according to criteria for definite fatal MI, or when CHD was listed as a cause of death in persons with confirmed CHD and no other plausible cause of death. Sudden death was diagnosed when CHD death occurred within 1 hour of symptom onset without another plausible cause of death. The main outcomes of interest were incident sudden death, nonfatal MI, and total CHD (combined sudden death, other CHD deaths, and nonfatal MI).
Statistical Analysis
Cox proportional-hazards models with time-varying covariates were used to evaluate risk, with censoring at the first event, death, or last date of adjudicated follow-up through January 31, 2000. We first assessed the main effects of n-6, long-chain n-3 (EPA + DHA), and intermediate-chain n-3 (ALA) PUFA intake. We then evaluated different patterns of n-3 and n-6 PUFA intake by using joint categories of higher (≥ median) versus lower (<median) intakes and ratios of intake. To assess potential confounding, multivariate models were evaluated after adjustment for cardiovascular risk factors, lifestyle habits, and other dietary habits, including age (5-year categories); body mass index (quintiles); smoking (5 categories); physical activity (quintiles); history of diabetes, hypertension, or hypercholesterolemia; aspirin use; alcohol intake (quintiles); and intake of protein, saturated fat, dietary fiber, monounsaturated fat, trans fatty acids, total calories, and (as appropriate) n-6 fatty acids, EPA + DHA, or ALA (each in quintiles). All covariates were updated over time except for incident diabetes, hypertension, or hypercholesterolemia, because dietary intake was not updated after a new diagnosis of these conditions (avoiding potential confounding due to changes in diet after a new diagnosis) and because the incidence of these conditions may be in the causal pathway relating diet to CHD. Inclusion or exclusion of fatty acids consumed as supplements (eg, by 0.9% of the cohort in 1990) had little effect on results; results are presented for dietary fatty acids (excluding supplements). Analyses were performed with SAS 8.2 software. All probability values are 2 tailed (α = 0.05).
Results
At the 10th, 50th, and 90th percentiles of energy-adjusted intake, EPA + DHA intake was 70, 250, and 560 mg/d; ALA intake was 790, 1080, and 1470 mg/d; and n-6 PUFA intake was 7.6, 11.2, and 15.9 g/d. Intakes of n-6 PUFAs and ALA were modestly correlated (Spearman correlation = 0.38); there was little correlation between intakes of n-6 PUFAs and EPA + DHA (r = −0.08) or between intakes of ALA and EPA + DHA (r = 0.02). Baseline characteristics of participants according to both EPA + DHA and n-6 PUFA intake are shown in Table 1. Men with a higher EPA + DHA intake were more likely to have hypercholesterolemia, greater physical activity, and higher protein intake. These differences, however, were fairly modest, as were differences in other characteristics by EPA + DHA and n-6 PUFA intake (Table 1). Differences in baseline characteristics according to both ALA and n-6 PUFA intake or both EPA + DHA and ALA intake were similarly modest (data not shown).
TABLE 1.
Age-Adjusted Baseline Characteristics According to EPA + DHA and n-6 Polyunsaturated Fatty Acid Intake*
| Low EPA + DHA
|
High EPA + DHA
|
|||
|---|---|---|---|---|
| Low n-6 (n = 10 982) | High n-6 (n = 12 129) | Low n-6 (n = 11 880) | High n-6 (n = 10 731) | |
| Hypertension, % | 20 | 19 | 22 | 21 |
| Hypercholesterolemia, % | 8 | 9 | 13 | 13 |
| Diabetes, % | 2 | 3 | 2 | 3 |
| Body-mass-index, kg/m2 | 25.5 | 25.5 | 25.4 | 25.5 |
| Smoking, % | ||||
| Never | 45 | 47 | 46 | 45 |
| Former | 40 | 39 | 42 | 42 |
| Current, 1–14 cigarettes/d | 3 | 3 | 2 | 3 |
| Current, ≥ 15 cigarettes/d | 8 | 6 | 5 | 5 |
| Missing | 3 | 4 | 4 | 4 |
| Physical activity, MET/wk | 20 | 18 | 25 | 22 |
| Aspirin ≥ 2 times/wk, % | 26 | 27 | 26 | 27 |
| β-Blocker, % | 7 | 7 | 8 | 7 |
| Lipid-lowering medication, % | 0.4 | 0.4 | 0.5 | 0.5 |
| Energy intake, kcal/d | 2031 | 2010 | 1958 | 1977 |
| Alcohol, g/d | 14 | 9 | 13 | 10 |
| Carbohydrates, g/d | 242 | 227 | 244 | 223 |
| Protein, g/d | 86 | 86 | 99 | 98 |
| Saturated fat, g/d | 26 | 27 | 22 | 24 |
| Monounsaturated fat, g/d | 26 | 31 | 24 | 29 |
| Trans PUFAs, g/d | 2.9 | 3.4 | 2.3 | 2.8 |
| ALA, g/d | 1.0 | 1.2 | 1.0 | 1.2 |
| Fiber, g/d | 20 | 20 | 23 | 21 |
Values are mean (continuous variables) or frequency (categorical variables), adjusted for age.
Grouped according to < or ≥ median intake of both EPA + DHA (250 mg/d) and n-6 fatty acids (11.2 g/d).
During 14 years of follow-up, participants experienced 218 sudden deaths, 1521 incident nonfatal MIs, and 2306 total incident CHD events (combined sudden deaths, other CHD deaths, and nonfatal MI). We first evaluated the associations of EPA + DHA, ALA, and n-6 PUFA intakes with CHD risk separately (multivariate model; see Methods for covariates). As reported previously,12 the relation between EPA + DHA intake and CHD risk was nonlinear and largely a result of a lower risk of sudden death; divided at median intake (250 mg/d), higher EPA + DHA intake was associated with a 35% lower risk of sudden death (hazard ratio [HR] = 0.65; 95% confidence interval [CI] = 0.47 to 0.88) compared with a lower intake. Higher ALA intake (each 1 g/d) was not significantly associated with sudden death (HR = 1.15; 95% CI = 0.69 to 1.93) but was associated with trends toward a lower risk of nonfatal MI (HR = 0.82; 95% CI = 0.67 to 1.02) and total CHD (HR = 0.84; 95% CI = 0.71 to 1.00), whereas higher n-6 PUFA intake (each 5 g/d) was not significantly associated with the risk of sudden death (HR = 0.82; 95% CI = 0.63 to 1.06), nonfatal MI (HR = 1.00; 95% CI = 0.91 to 1.11), or total CHD (HR = 0.96; 95% CI = 0.89 to 1.04). Findings were not appreciably different when PUFA intakes were evaluated as indicator variables in quintiles (data not shown).
When we assessed the risk of CHD according to joint intakes of EPA + DHA and n-6 fatty acids, higher EPA + DHA intake was associated with a lower risk of sudden death regardless of n-6 PUFA intake (Table 2). After adjustment for cardiovascular risk factors, lifestyle habits, and other dietary habits (multivariate model), higher EPA + DHA intake (≥ 250 mg/d) was associated with a 40% to 50% lower risk of sudden death among men with a lower n-6 PUFA intake (HR = 0.52; 95% CI = 0.34 to 0.79) and among men with a higher n-6 PUFA intake (HR = 0.60; 95% CI = 0.39 to 0.93) compared with men with lower intakes of both. The combination of a higher n-6 PUFA intake and a lower EPA + DHA intake was associated with a modest and nonsignificant reduction in risk of sudden death (HR = 0.76; 95% CI = 0.52 to 1.11) compared with lower intakes of both. Different patterns of EPA + DHA and n-6 PUFA intake were not significantly associated with nonfatal MI or total CHD (Table 2). For example, higher intakes of both EPA + DHA and n-6 fatty acids were not associated with nonfatal MI (HR = 1.09; 95% CI = 0.91 to 1.29) or total CHD (HR = 1.02; 95% CI = 0.89 to 1.16) compared with lower intakes of both (multivariate model). There was little formal evidence for interaction between EPA + DHA and n-6 PUFA intake for relations with sudden death (P interaction = 0.13), nonfatal MI (P interaction = 0.15), or total CHD (P interaction = 0.99).
TABLE 2.
Relative Risk of CHD According to Both EPA + DHA and n-6 Polyunsaturated Fatty Acid Intake*
| Low EPA + DHA
|
High EPA + DHA
|
|||
|---|---|---|---|---|
| Low n-6 (n = 10 982) | High n-6 (n = 12 129) | Low n-6 (n = 11 880) | High n-6 (n = 10 731) | |
| Sudden death, n | 62 | 65 | 46 | 45 |
| Age adjusted | 1.0 (reference) | 0.85 (0.60–1.20) | 0.48 (0.32–0.71) | 0.69 (0.48–1.01) |
| Multivariate | 1.0 (reference) | 0.76 (0.52–1.11) | 0.52 (0.34–0.79) | 0.60 (0.39–0.93) |
| Nonfatal MI, n | 349 | 395 | 408 | 369 |
| Age adjusted | 1.0 (reference) | 1.14 (0.99–1.32) | 1.08 (0.94–1.25) | 1.09 (0.94–1.27) |
| Multivariate | 1.0 (reference) | 1.09 (0.93–1.28) | 1.16 (0.99–1.36) | 1.09 (0.91–1.29) |
| Total CHD, n | 549 | 576 | 617 | 564 |
| Age adjusted | 1.0 (reference) | 1.01 (0.90–1.14) | 0.96 (0.86–1.08) | 1.02 (0.91–1.16) |
| Multivariate | 1.0 (reference) | 0.97 (0.85–1.10) | 1.05 (0.92–1.19) | 1.02 (0.89–1.16) |
Grouped according to < or ≥ median intake of both n-6 fatty acids (11.2 g/d) and EPA + DHA (250 mg/d), with the reference group being men consuming < median intake of both. Values are hazard ratios (95% CI). Multivariate model is adjusted for age (5-year categories); body mass index (quintiles); smoking (5 categories); physical activity (quintiles); history of diabetes, hypertension, or hypercholesterolemia; aspirin use; alcohol use (quintiles); and intake of protein, saturated fat, dietary fiber, monounsaturated fat, trans fatty acids, total calories, and ALA (each in quintiles). Total CHD represents combined sudden death, other coronary heart disease deaths, and nonfatal MI.
When joint intakes of ALA and n-6 fatty acids were assessed, higher ALA intake was associated with lower risk or trends toward a lower risk of nonfatal MI, whether n-6 PUFA intake was lower (HR = 0.85; 95% CI = 0.72 to 0.99) or higher (HR = 0.89; 95% CI = 0.77 to 1.02) and with a lower risk of total CHD, whether n-6 PUFA intake was lower (HR = 0.88; 95% CI = 0.78 to 0.99) or higher (HR = 0.89; 95% CI = 0.79 to 0.99) (multivariate model, Table 3). Different patterns of ALA and n-6 PUFA intake were not significantly associated with sudden death (Table 3). As with EPA + DHA, there was little formal evidence for interaction between ALA and n-6 PUFA intake for relations with sudden death (P interaction = 0.71), nonfatal MI (P interaction = 0.52), or total CHD (P interaction = 0.38).
TABLE 3.
Relative Risk of CHD According to Both ALA and n-6 Polyunsaturated Fatty Acid Intake*
| Low ALA
|
High ALA
|
|||
|---|---|---|---|---|
| Low n-6 (n = 14 462) | High n-6 (n = 8385) | Low n-6 (n = 8400) | High n-6 (n = 14 475) | |
| Sudden death, n | 66 | 36 | 42 | 74 |
| Age adjusted | 1.0 (reference) | 1.02 (0.68–1.53) | 1.07 (0.73–1.58) | 1.17 (0.84–1.64) |
| Multivariate | 1.0 (reference) | 0.88 (0.56–1.36) | 0.95 (0.64–1.43) | 0.93 (0.64–1.35) |
| Nonfatal MI, n | 491 | 284 | 266 | 480 |
| Age adjusted | 1.0 (reference) | 1.04 (0.89–1.20) | 0.90 (0.77–1.05) | 1.03 (0.90–1.16) |
| Multivariate | 1.0 (reference) | 0.98 (0.84–1.15) | 0.85 (0.72–0.99) | 0.89 (0.77–1.02) |
| Total CHD, n | 737 | 407 | 429 | 733 |
| Age adjusted | 1.0 (reference) | 0.99 (0.88–1.12) | 0.94 (0.83–1.06) | 1.03 (0.93–1.14) |
| Multivariate | 1.0 (reference) | 0.93 (0.82–1.07) | 0.88 (0.78–0.99) | 0.89 (0.79–0.99) |
Grouped according to < or ≥ median intake of both n-6 fatty acids (11.2 g/d) and ALA (1080 mg/d), with the reference group being men consuming < median intake of both. Values are hazard ratios (95% CI). Multivariate model is adjusted for age (5-year categories); body mass index (quintiles); smoking (5 categories); physical activity (quintiles); history of diabetes, hypertension, or hypercholesterolemia; aspirin use; alcohol use (quintiles); and intake of protein, saturated fat, dietary fiber, monounsaturated fat, trans fatty acids, total calories, and EPA + DHA (each in quintiles). Total CHD represents combined sudden death, other coronary heart disease deaths, and nonfatal MI.
We had hypothesized that intake of long-chain n-3 fatty acids from seafood (EPA + DHA) may modify effects of intermediate-chain n-3 fatty acids from plant sources (ALA). As described earlier, ALA intake was associated with a modestly lower risk of both nonfatal MI and total CHD. However, these lower risks occurred almost entirely as a result of an association among men with very low EPA + DHA intake (Figure 2). Among men with little or no EPA + DHA intake (<100 mg/d), each 1 g/d of ALA intake was associated with a 58% lower risk of nonfatal MI (HR = 0.42; 95% CI = 0.23 to 0.75, P = 0.004) and a 47% lower risk of total CHD (HR = 0.53; 95% CI = 0.34 to 0.83, P = 0.008). The risk estimate was similar for sudden death (HR = 0.52; 95% CI = 0.14 to 1.90), although CIs were broad due to fewer numbers of events. In contrast, among men with a higher EPA + DHA intake (≥ 100 mg/d), ALA intake was not associated with CHD risk (Figure 2). This interaction by EPA + DHA intake was highly significant for both nonfatal MI (P interaction = 0.003) and total CHD (P interaction = 0.006). There was little evidence that these relations between ALA and CHD risk were modified by n-6 PUFA intake (P > 0.10 for the ratio of ALA to n-6 PUFA intake and for their multiplicative interaction term).
Figure 2.
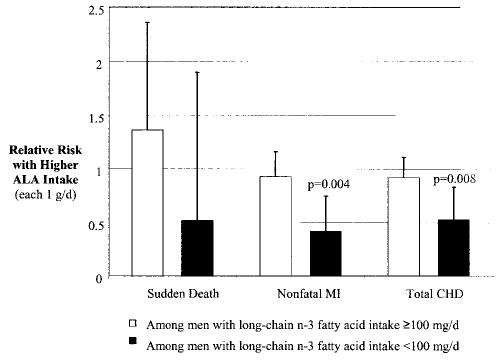
Relative risks (hazards) of CHD associated with each 1 g/d of ALA intake, among participants with long-chain n-3 PUFA intake ≥ 100 mg/d (n = 38 367, open columns) and among participants with little or no long-chain n-3 PUFA intake (<100 mg/d, n = 7355, filled columns). Long-chain n-3 PUFA intake modified effects of ALA intake for both nonfatal MI (P interaction = 0.003) and total CHD (P interaction = 0.006). Error bars indicate upper limit of 95% CI; probability values for significant relative risks are shown. Adjustments as in multivariate model, Table 2. Abbreviations are as defined in text.
As described earlier, n-6 PUFA intake was not associated with CHD risk overall, nor did this relation appear to be modified by EPA + DHA or ALA intake. n-6 PUFA intake was also not associated with CHD risk when evaluated as indicator categories in deciles (data not shown). We also evaluated whether the associations between n-6 PUFA intake and CHD risk were modified by age, body mass index, or intake of trans fatty acids (based on information from personal communication from K. Oh and F. Hu, 2004). There was little evidence for effect modification by these factors (P > 0.10 for each interaction). Ratios of intake of different PUFAs (eg, EPA + DHA to n-6 PUFA, ALA to n-6 PUFA, and ALA to EPA + DHA) in which, for example, men with very low intakes of both EPA + DHA and n-6 fatty acids would have the same value as those with very high intakes of both, were also not significantly associated with CHD risk (P > 0.10 for each).
Discussion
In this large prospective cohort study, modest dietary intake of long-chain n-3 PUFAs (≥ 250 mg/d) was associated with a 40% to 50% lower risk of sudden death, regardless of background intake of n-6 PUFAs. This lower risk was observed after adjustment for a variety of cardiac risk factors, lifestyle characteristics, and other dietary habits. These results suggest that n-6 PUFAs neither greatly counteract nor greatly augment the cardiovascular benefits of a modest intake of long-chain n-3 PUFAs from seafood. EPA + DHA intake was associated with a lower risk of sudden death but not of nonfatal MI or total CHD. This is consistent with results from other observational and experimental studies, which suggest an effect of long-chain n-3 PUFAs on fatal ventricular arrhythmias.11–16,25,34,37 In vitro, long-chain n-3 PUFAs decrease myocyte excitability and reduce cytosolic calcium fluctuations via inhibition of Na+ and L-type Ca2+ channels,37 supporting a potential antiarrhythmic effect of these fatty acids.
Relations between intermediate-chain n-3 PUFAs and CHD risk also appeared independent of n-6 PUFA intake. Although theoretical considerations and short-term studies of secondary outcomes have suggested that n-6 fatty acids may counteract the effects of ALA on CHD incidence,17–23 few prior studies have evaluated this hypothesis. In the Nurses Health Study, intake of linoleic acid (18:2n-6) did not appreciably modify the inverse association between ALA and CHD risk, nor was the ratio of ALA to linoleic acid associated with risk8; however, these analyses were not the main focus, and detailed results were not reported. Results were similar in the cross-sectional Family Heart Study,38 although findings may be limited by the evaluation of prevalent, rather than incident, CHD. Our findings provide the strongest evidence to date that n-6 PUFA intake does not appreciably counteract the effects of either intermediate- or long-chain n-3 PUFAs on the risk of CHD events.
Three randomized trials,39–42 but not 2 others,43,44 demonstrated reductions in some CHD end points with higher n-6 PUFA intake (one trial also increased ALA intake41,42). In some prior cohorts, an inverse association was observed between n-6 PUFA intake or the ratio of polyunsaturated to saturated fat and CHD risk.2 We did not observe an association between n-6 PUFA intake and CHD risk, even by comparing extreme deciles of intake (comparing <7.6 g/d to ≥15.9 g/d). The discrepancy of the findings between prior studies and our study could be due to differences in age or body mass index distribution or to the low trans fatty acid intake in these men, although our secondary analyses do not support these hypotheses. Although our findings do not exclude the possibility of a modest effect, our results suggest that higher n-6 PUFA intake is unlikely to substantially reduce CHD risk in men over the range that was studied. Our results also indicate that higher n-6 PUFA intake is unlikely to appreciably attenuate the beneficial effects of n-3 PUFA intake on CHD risk.
The strongest relation between ALA intake and CHD risk was seen when EPA + DHA intake was very low (<100 mg/d). Long-chain n-3 PUFAs inhibit metabolism of ALA via feedback inhibition (Figure 1), suggesting a potential biological mechanism for this observation. In experimental studies, both intermediate-chain and long-chain n-3 PUFAs influence platelet aggregation, thrombosis, blood pressure, lipids, inflammatory responses, and arrhythmia.1,17 Many of the effects of long-chain n-3 PUFAs are seen only at pharmacological doses, and our findings as well as those of prior studies13,15,16 suggest that antiarrhythmic effects of EPA + DHA may predominate at usual dietary doses. Conversely, ALA intake was associated with a lower risk of nonfatal MI and total CHD, suggesting that in the absence of significant long-chain n-3 PUFA intake, ALA may influence CHD risk via multiple pathways, including non–arrhythmia-related mechanisms. Further research is needed to determine whether ALA is also related to the risk of sudden death in the setting of low long-chain n-3 PUFA intake.
To our knowledge, this is the first prospective study to evaluate whether EPA + DHA intake influences relations between ALA and CHD incidence. Results of prior studies of ALA intake and CHD risk have been mixed, with some5–9 but not others45–47 observing an inverse association between ALA and CHD risk. If effects of ALA are influenced by background EPA + DHA intake, as suggested by our results, this may in part explain the prior null associations45–47 between ALA intake and CHD risk. Our findings suggest that plant sources of n-3 PUFAs may particularly reduce CHD risk in men when intake of long-chain n-3 PUFAs is low, which may have important implications for CHD prevention in populations with low consumption or availability of fatty fish. Further observational, clinical, and animal-experimental studies are needed to investigate this relation and potential underlying mechanisms.
Our study has several strengths. Nutrient intakes were estimated with a validated dietary instrument in a large, well-described cohort. Cumulative averaging of multiple diet assessments over time reduced misclassification. Prospective assessment and cessation of dietary updating after intermediate events reduced potential bias from changes in diet due to known disease. Standardized assessment of participant characteristics increased the ability to adjust for potential confounding factors. Little loss to follow-up and centralized adjudication of outcomes reduced the likelihood of missed or misclassified outcomes.
There are also potential limitations to our findings. We may have had inadequate power to detect more subtle interactions between n-6 PUFAs, EPA + DHA, and ALA intakes. Nutrient intakes were likely estimated with some error owing to imperfect estimates of specific food intakes and nutrient contents of foods. Such misclassification would bias results toward the null, which might, for example, in part account for the lack of significant overall associations between n-6 PUFA intake and CHD risk. There may also have been misclassification of outcomes, particularly sudden death. Although such misclassification would limit our ability to detect relations, the robust association between EPA + DHA intake and sudden death, rather than nonfatal MI or total CHD, is consistent with other observational and clinical studies of EPA + DHA11–16 and suggests that many events are likely correctly classified. Participants were male health professionals with generally healthier behaviors, and our findings may not be generalizable to all populations. Although we adjusted for a variety of clinical and dietary factors, residual confounding by unmeasured or imprecisely measured factors cannot be excluded.
Our findings suggest that dietary intake of long-chain n-3 PUFAs from seafood may lower the risk of sudden death regardless of the background intake of n-6 fatty acids. This lower risk was seen with modest dietary intake (≥ 250 mg/d), the equivalent of ≈1 to 2 fatty fish meals per week. Our results also suggest that when long-chain n-3 PUFA intake is low, dietary intake of intermediate-chain n-3 PUFAs from plant sources may lower CHD risk, regardless of background n-6 PUFA intake. Together these results suggest that attention to relative intakes of n-3 and n-6 fatty acids may be less important than simply increasing the intake of n-3 PUFAs. Our findings also suggest that dietary consumption of plant sources of n-3 fatty acids may be important for CHD prevention among persons who do not regularly consume fatty fish or in populations in which fatty fish is not readily available.
Acknowledgments
This study was sponsored by grants from the National Heart, Lung, and Blood Institute (HL-35464), the National Cancer Institute CA55075), and Dr Rimm’s Established Investigator Award from the American Heart Association. Dr Mozaffarian was supported in part by a National Research Service Award training grant in academic nutrition (DK07703). Special thanks are extended to Dr Anwar Merchant for assistance.
References
- 1.Hu FB, Manson JE, Willett WC. Types of dietary fat and risk of coronary heart disease: a critical review. J Am Coll Nutr. 2001;20:5–19. doi: 10.1080/07315724.2001.10719008. [DOI] [PubMed] [Google Scholar]
- 2.Sanders TA, Oakley FR, Miller GJ, Mitropoulos KA, Crook D, Oliver MF. Influence of n-6 versus n-3 polyunsaturated PUFAs in diets low in saturated PUFAs on plasma lipoproteins and hemostatic factors. Arterioscler Thromb Vasc Biol. 1997;17:3449–3460. doi: 10.1161/01.atv.17.12.3449. [DOI] [PubMed] [Google Scholar]
- 3.Bang HO, Dyerberg J. Lipid metabolism and ischemic heart disease in Greenland Eskimos. In: Draper H, ed. Advances in Nutrition Research. New York, NY: Plenum Press; 1980:1–22.
- 4.Burr ML, Fehily AM, Gilbert JF, Rogers S, Holliday RM, Sweetnam PM, Elwood PC, Deadman NM. Effects of changes in fat, fish, and fibre intakes on death and myocardial reinfarction: diet and reinfarction trial (DART) Lancet. 1989;2:757–761. doi: 10.1016/s0140-6736(89)90828-3. [DOI] [PubMed] [Google Scholar]
- 5.Dolecek TA. Epidemiological evidence of relationships between dietary polyunsaturated PUFAs and mortality in the multiple risk factor intervention trial. Proc Soc Exp Biol Med. 1992;200:177–182. doi: 10.3181/00379727-200-43413. [DOI] [PubMed] [Google Scholar]
- 6.Ascherio A, Rimm EB, Giovannucci EL, Spiegelman D, Stampfer M, Willett WC. Dietary fat and risk of coronary heart disease in men: cohort follow up study in the United States. BMJ. 1996;313:84–90. doi: 10.1136/bmj.313.7049.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singh RB, Niaz MA, Sharma JP, Kumar R, Rastogi V, Moshiri M. Randomized, double-blind, placebo-controlled trial of fish oil and mustard oil in patients with suspected acute myocardial infarction: the Indian Experiment of Infarct Survival-4. Cardiovasc Drugs Ther. 1997;11:485–491. doi: 10.1023/a:1007757724505. [DOI] [PubMed] [Google Scholar]
- 8.Hu FB, Stampfer MJ, Manson JE, Rimm EB, Wolk A, Colditz GA, Hennekens CH, Willett WC. Dietary intake of α-linolenic acid and risk of fatal ischemic heart disease among women. Am J Clin Nutr. 1999;69:890–897. doi: 10.1093/ajcn/69.5.890. [DOI] [PubMed] [Google Scholar]
- 9.Baylin A, Kabagambe EK, Ascherio A, Spiegelman D, Campos H. Adipose tissue α-linolenic acid and nonfatal acute myocardial infarction in Costa Rica. Circulation. 2003;107:1586–1591. doi: 10.1161/01.CIR.0000058165.81208.C6. [DOI] [PubMed] [Google Scholar]
- 10.Hu FB, Bronner L, Willett WC, Stampfer MJ, Rexrode KM, Albert CM, Hunter D, Manson JE. Fish and ω-3 PUFA intake and risk of coronary heart disease in women. JAMA. 2002;287:1815–1821. doi: 10.1001/jama.287.14.1815. [DOI] [PubMed] [Google Scholar]
- 11.Siscovick DS, Raghunathan TE, King I, Weinmann S, Wicklund KG, Albright J, Bovbjerg V, Arbogast P, Smith H, Kushi LH. Dietary intake and cell membrane levels of long-chain n-3 polyunsaturated PUFAs and the risk of primary cardiac arrest. JAMA. 1995;274:1363–1367. doi: 10.1001/jama.1995.03530170043030. [DOI] [PubMed] [Google Scholar]
- 12.Albert CM, Hennekens CH, O’Donnell CJ, Ajani UA, Carey VJ, Willett WC, Ruskin JN, Manson JE. Fish consumption and risk of sudden cardiac death. JAMA. 1998;279:23–28. doi: 10.1001/jama.279.1.23. [DOI] [PubMed] [Google Scholar]
- 13.Mozaffarian D, Lemaitre RN, Kuller LH, Burke GL, Tracy RP, Siscovick DS. Cardiac effects of fish consumption may vary depending on the type of fish meal consumed: the Cardiovascular Health Study. Circulation. 2003;107:1372–1377. doi: 10.1161/01.cir.0000055315.79177.16. [DOI] [PubMed] [Google Scholar]
- 14.Albert CM, Campos H, Stampfer MJ, Ridker PM, Manson JE, Willett WC, Ma J. Blood levels of long-chain n-3 PUFAs and the risk of sudden death. N Engl J Med. 2002;346:1113–1118. doi: 10.1056/NEJMoa012918. [DOI] [PubMed] [Google Scholar]
- 15.Lemaitre RN, King I, Mozaffarian D, Kuller LH, Tracy RP, Siscovick DS. Plasma phospholipid n-3 polyunsaturated PUFAs, fatal ischemic heart disease, and nonfatal myocardial infarction in older adults: the Cardiovascular Health Study. Am J Clin Nutr. 2003;77:319–325. doi: 10.1093/ajcn/77.2.319. [DOI] [PubMed] [Google Scholar]
- 16.Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto miocardico. . Dietary supplementation with n-3 polyunsaturated PUFAs and vitamin E after myocardial infarction: results of the GISSI-Prevenzione trial. Lancet. 1999;354:447–455. [PubMed] [Google Scholar]
- 17.Simopoulos AP. Essential PUFAs in health and chronic disease. Am J Clin Nutr. 1999;70:560S–569S. doi: 10.1093/ajcn/70.3.560s. [DOI] [PubMed] [Google Scholar]
- 18.Kris-Etherton PM, Taylor DS, Yu-Poth S, Huth P, Moriarty K, Fishell V, Hargrove RL, Zhao G, Etherton TD. Polyunsaturated PUFAs in the food chain in the United States. Am J Clin Nutr. 2000;71:179S–188S. doi: 10.1093/ajcn/71.1.179S. [DOI] [PubMed] [Google Scholar]
- 19.Emken EA, Adlot RO, Gulley RM. Dietary linoleic acid influences desaturation and acylation of deuterium-labeled linoleic and linolenic acid in young adult males. Biochim Biophys Acta. 1994;1213:277–288. doi: 10.1016/0005-2760(94)00054-9. [DOI] [PubMed] [Google Scholar]
- 20.Chan JK, McDonald BE, Gerrard JM, Bruce VM, Weaver BJ, Holub BJ. Effects of dietary α-linolenic acid and its ratio to linoleic acid on platelet and plasma PUFAs and thrombogenesis. Lipids. 1993;28:811–817. doi: 10.1007/BF02536235. [DOI] [PubMed] [Google Scholar]
- 21.Freese R, Mutanen M, Valsta LM, Salminen I. Comparison of the effects of two diets rich in monounsaturated PUFAs differing in their linoleic/α-linoleic acid ratio on platelet aggregation. Thromb Haemost. 1994;71:73–77. [PubMed] [Google Scholar]
- 22.McLennan PL, Dallimore JA. Dietary canola oil modifies myocardial PUFAs and inhibits cardiac arrhythmias in rats. J Nutr. 1995;125:1003–1009. doi: 10.1093/jn/125.4.1003. [DOI] [PubMed] [Google Scholar]
- 23.James MJ, Gibson RA, Cleland LG. Dietary polyunsaturated PUFAs and inflammatory mediator production. Am J Clin Nutr. 2000;71:343S–348S. doi: 10.1093/ajcn/71.1.343s. [DOI] [PubMed] [Google Scholar]
- 24.Fickova M, Hubert P, Cremel G, Leray C. Dietary n-3 and n-6 polyunsaturated fatty acids rapidly modify fatty acid composition and insulin effects in rat adipocytes. J Nutr. 1998;128:512–519. doi: 10.1093/jn/128.3.512. [DOI] [PubMed] [Google Scholar]
- 25.Siscovick DS, Lemaitre RN, Mozaffarian D. The fish story: a diet-heart hypothesis with clinical implications: n-3 polyunsaturated fatty acids, myocardial vulnerability, and sudden death. Circulation. 2003;107:2632–2634. doi: 10.1161/01.CIR.0000074779.11379.62. [DOI] [PubMed] [Google Scholar]
- 26.Rimm EB, Stampfer MJ, Colditz GA, Chute CG, Litin LB, Willett WC. Validity of self-reported waist and hip circumferences in men and women. Epidemiology. 1990;1:466–473. doi: 10.1097/00001648-199011000-00009. [DOI] [PubMed] [Google Scholar]
- 27.Giovannucci E, Colditz G, Stampfer MJ, Rimm EB, Litin L, Sampson L, Willett WC. The assessment of alcohol consumption by a simple self-administered questionnaire. Am J Epidemiol. 1991;133:810–817. doi: 10.1093/oxfordjournals.aje.a115960. [DOI] [PubMed] [Google Scholar]
- 28.Chasan-Taber S, Rimm EB, Stampfer MJ, Spiegelman D, Colditz GA, Giovannucci E, Ascherio A, Willett WC. Reproducibility and validity of a self-administered physical activity questionnaire for male health professionals. Epidemiology. 1996;7:81–86. doi: 10.1097/00001648-199601000-00014. [DOI] [PubMed] [Google Scholar]
- 29.Rimm EB, Giovannucci EL, Stampfer MJ, Colditz GA, Litin LB, Willett WC. Reproducibility and validity of an expanded self-administered semi-quantitative food frequency questionnaire among male health professionals. Am J Epidemiol. 1992;135:1114–1126. doi: 10.1093/oxfordjournals.aje.a116211. [DOI] [PubMed] [Google Scholar]
- 30.Hunter DJ, Rimm EB, Sacks FM, Stampfer MJ, Colditz GA, Litin LB, Willett WC. Comparison of measures of PUFA intake by subcutaneous fat aspirate, food frequency questionnaire, and diet records in a free-living population of US men. Am J Epidemiol. 1992;135:418–427. doi: 10.1093/oxfordjournals.aje.a116302. [DOI] [PubMed] [Google Scholar]
- 31.US Department of Agriculture, Agricultural Research Service. 2004. USDA National Nutrient Database for Standard Reference, release 15. Nutrient Data Laboratory Home Page, http://www.nal.usda.gov/fnic/foodcomp
- 32.Willett WC, Stampfer MJ. Total energy intake: implications for epidemiologic analyses. Am J Epidemiol. 1986;124:17–27. doi: 10.1093/oxfordjournals.aje.a114366. [DOI] [PubMed] [Google Scholar]
- 33.Hu FB, Stampfer MJ, Rimm E, Ascherio A, Rosner BA, Spiegelman D, Willett WC. Dietary fat and coronary heart disease: a comparison of approaches for adjusting for total energy intake and modeling repeated dietary measurements. Am J Epidemiol. 1999;149:531–540. doi: 10.1093/oxfordjournals.aje.a009849. [DOI] [PubMed] [Google Scholar]
- 34.McLennan PL. Myocardial membrane PUFAs and the antiarrhythmic actions of dietary fish oil in animal models. Lipids. 2001;36:111S–114S. doi: 10.1007/s11745-001-0692-x. [DOI] [PubMed] [Google Scholar]
- 35.Rimm EB, Stampfer MJ, Ascherio A, Giovannucci E, Colditz GA, Willett WC. Vitamin E consumption and the risk of coronary heart disease in men. N Engl J Med. 1993;328:1450–1456. doi: 10.1056/NEJM199305203282004. [DOI] [PubMed] [Google Scholar]
- 36.Rose GA, Blackburn H. Cardiovascular Survey Methods, 2nd ed. Geneva, Switzerland: World Health Organization; World Health Organization monograph series No. 58. 1982. [PubMed]
- 37.Leaf A, Kang JX, Xiao YF, Billman GE. Clinical prevention of sudden cardiac death by n-3 polyunsaturated PUFAs and mechanism of prevention of arrhythmias by n-3 fish oils. Circulation. 2003;107:2646–2652. doi: 10.1161/01.CIR.0000069566.78305.33. [DOI] [PubMed] [Google Scholar]
- 38.Djousse L, Pankow JS, Eckfeldt JH, Folsom AR, Hopkins PN, Province MA, Hong Y, Ellison RC. Relation between dietary linolenic acid and coronary artery disease in the National Heart, Lung, and Blood Institute Family Heart Study. Am J Clin Nutr. 2001;74:612–619. doi: 10.1093/ajcn/74.5.612. [DOI] [PubMed] [Google Scholar]
- 39.Dayton S, Pearce ML, Goldman H, Harnish A, Plotkin D, Shickman M, Winfield M, Zager A, Dixon W. Controlled trial of a diet high in unsaturated fat for prevention of atherosclerotic complications. Lancet. 1968;2:1060–1062. doi: 10.1016/s0140-6736(68)91531-6. [DOI] [PubMed] [Google Scholar]
- 40.Leren P. The Oslo diet-heart study: eleven-year report. Circulation. 1970;42:935–942. doi: 10.1161/01.cir.42.5.935. [DOI] [PubMed] [Google Scholar]
- 41.Turpeinen O, Karvonen MJ, Pekkarinen M, Miettinen M, Elosuo R, Paavilainen E. Dietary prevention of coronary heart disease: the Finnish Mental Hospital Study. Int J Epidemiol. 1979;8:99–118. doi: 10.1093/ije/8.2.99. [DOI] [PubMed] [Google Scholar]
- 42.Miettinen M, Turpeinen O, Karvonen MJ, Pekkarinen M, Paavilainen E, Elosuo R. Dietary prevention of coronary heart disease in women: the Finnish Mental Hospital Study. Int J Epidemiol. 1983;12:17–25. doi: 10.1093/ije/12.1.17. [DOI] [PubMed] [Google Scholar]
- 43.Woodhill JM, Palmer AJ, Leelarthaepin B, McGilchrist C, Blacket RB. Low fat, low cholesterol diet in secondary prevention of coronary heart disease. Adv Exp Med Biol. 1978;109:317–330. doi: 10.1007/978-1-4684-0967-3_18. [DOI] [PubMed] [Google Scholar]
- 44.Frantz ID, Jr, Dawson EA, Ashman PL, Gatewood LC, Bartsch GE, Kuba K, Brewer ER. Test of effect of lipid lowering by diet on cardiovascular risk: the Minnesota Coronary Survey. Arteriosclerosis. 1989;9:129–135. doi: 10.1161/01.atv.9.1.129. [DOI] [PubMed] [Google Scholar]
- 45.Pietinen P, Ascherio A, Korhonen P, Hartman AM, Willett WC, Albanes D, Virtamo J. Intake of PUFAs and risk of coronary heart disease in a cohort of Finnish men: the Alpha-Tocopherol, Beta-Carotene Prevention Study. Am J Epidemiol. 1997;145:876–887. doi: 10.1093/oxfordjournals.aje.a009047. [DOI] [PubMed] [Google Scholar]
- 46.Pedersen JI, Ringstad J, Almendingen K, Haugen TS, Stensvold I, Thelle DS. Adipose tissue PUFAs and risk of myocardial infarction—a case-control study. Eur J Clin Nutr. 2000;54:618–625. doi: 10.1038/sj.ejcn.1601064. [DOI] [PubMed] [Google Scholar]
- 47.Oomen CM, Ocke MC, Feskens EJ, Kok FJ, Kromhout D. α-Linolenic acid intake is not beneficially associated with 10-y risk of coronary artery disease incidence: the Zutphen Elderly Study. Am J Clin Nutr. 2001;74:457–463. doi: 10.1093/ajcn/74.4.457. [DOI] [PubMed] [Google Scholar]


