Abstract
Background
The objectives of this study were to: (1) describe the longitudinal development of sleep-wake patterns of solitary-sleeping infants from 1 to 12 months of age, (2) identify effects on sleep patterns and on self-soothing behaviors of introducing a novel sleep aid, and (3) identify predictive factors of self-soothing at 12 months using a transactional model as a guide.
Methods
Eighty infants’ nighttime sleep-wake patterns and associated variables were studied at 5 times across the first year of life using videosomnography and questionnaires.
Results
Sleep-wake state developmental changes, as reported in investigations of infant sleep, were replicated, although a great deal of individual variability in the development of all sleep-related variables was noted. No major effects on sleep or on self-soothing behavior were evident from the introduction of the novel sleep aid. Three variables were identified as significant predictors of self-soothing at 12 months: decreasing amounts of time spent out of crib across the first year, high levels of quiet sleep at birth, and longer parental response times to infant awakenings at 3 months.
Conclusions
These data lend preliminary support for the transactional model and suggest that infant and parental factors interact to influence the development of self-soothing.
Keywords: Infancy, normal development, parent-child interaction, paediatrics, sleep, temperament
Abbreviations: AS: active sleep, AW: wakefulness, BDI: Beck Depression Inventory, GLM: general linear modeling, LSP: longest sleep period, OOC: out of crib, PSOCS: Parenting Sense of Competence Scale, QS: quiet sleep, RSA: representational sleep aid, SC: sham control, SS: self-soothed, TST: total sleep time
For infants who sleep independently, the ability to self-soothe when falling asleep at the beginning of the night and following nighttime awakenings appears to be a key ingredient for the development of healthy sleep-wake patterns. Although a number of studies have described the development of sleep-wake patterns during infancy, relatively few have examined factors related to the emergence of self-soothing behavior. Theoretically, self-soothing refers to an infant’s ability to regulate states of arousal; for example, calming from crying to quiet wakefulness without parental assistance. In this study, self-soothing refers to an infant’s ability to settle to sleep at the beginning of the night and to put herself back to sleep upon awakening during the night. The purpose of the current study was to objectively monitor infant sleep-wake patterns and other variables thought to relate to the development of self-soothing across the first year of life.
The development of sleep-wake patterns follows a somewhat prescribed path during infancy. First, the 24-hour distribution of sleep changes across the first year. Newborns tend to sleep for 16–17 hours in 3–4 hour increments dispersed throughout the 24-hour day (Parmelee, Shulz, & Disbrow, 1961). By 1 year of age, the bulk of sleep shifts to the nighttime hours and sleep periods lengthen (consolidate), but the total amount of sleep per 24 hours decreases relatively little (Anders & Keener, 1985; Kleitman & Engelmann, 1953). Second, the proportions of sleep states change with age, such that rapid eye movement (REM) or active sleep decreases and non-rapid eye movement (NREM) or quiet sleep increases over the first year (Anders & Keener, 1985; Fagioli & Salzarulo, 1982). Although these basic patterns have been confirmed by numerous studies over the past 40 years, few large-scale longitudinal investigations have examined factors associated with the development of nighttime self-soothing.
The few investigations that have examined falling asleep and self-soothing after nighttime awakenings during the first year of life have shown that this ability develops in some infants, but not others, by the end of the first year (Anders, Halpern, & Hua, 1992; Keener, Zeanah, & Anders, 1988; Goodlin-Jones, Burnham, Gaylor, & Anders, 2001; Goodlin-Jones, Eiben, & Anders, 1997). During the first months of life, infants most often fall asleep during or immediately after a feeding both at the beginning and during the middle of the night; self-soothing is observed only occasionally. By 4 to 6 months of age, however, self-soothing behaviors at sleep onset and following nighttime awakenings begin to appear in some infants and tend to increase in frequency to the first birthday (Goodlin-Jones et al., 2001).
Infants who self-soothe are generally considered by parents to be better sleepers than infants who consistently need assistance to make the wake-sleep transition. Infant sleep disturbances are often brought to the attention of pediatricians during well-child visits due to the sleep disruption imposed on families (Lozoff, Wolf, & Davis, 1985). Indeed, France and Blampied (1999) define a sleep-disturbed infant as ‘one who is unable to settle back to sleep without the parents being aware of the awakening’. More precisely, awakenings are most disturbing to parents when the child cannot return to sleep on her own and requires parental intervention. For the purposes of the current investigation, these infants are considered ‘non-self-soothers’. Clearly, infants who do not develop the ability to self-soothe can create turmoil in some families.
A simple linear model that describes the emergence of self-soothing is not sufficient. A transactional model embraces the complexities of interacting systems or domains across a developmental time span (Sameroff & Fiese, 2000). A transactional perspective to self-soothing might include infant characteristics, parental characteristics, and interactions between infants and parents. Figure 1 displays a tentative model of potential domains associated with self-soothing (Anders, 1994; Goodlin-Jones, Burnham, & Anders, 2000). Variables in the four domains are thought to relate to each other and, ultimately, to whether the child is or is not able to self-soothe to sleep from the waking state. The model reflects the notion that self-regulation of wake to sleep transitions results from a dynamic, interactive process between the infant and a number of proximal and distal influences, mediated mostly through interactions with caregivers. This model is a work in progress. Thus far, partial support for the transactional model comes from small-scale and/or cross-sectional investigations (e.g., Goodlin-Jones et al., 2001). There have been no longitudinal studies specifically designed to investigate the hypothesized links.
Figure 1.
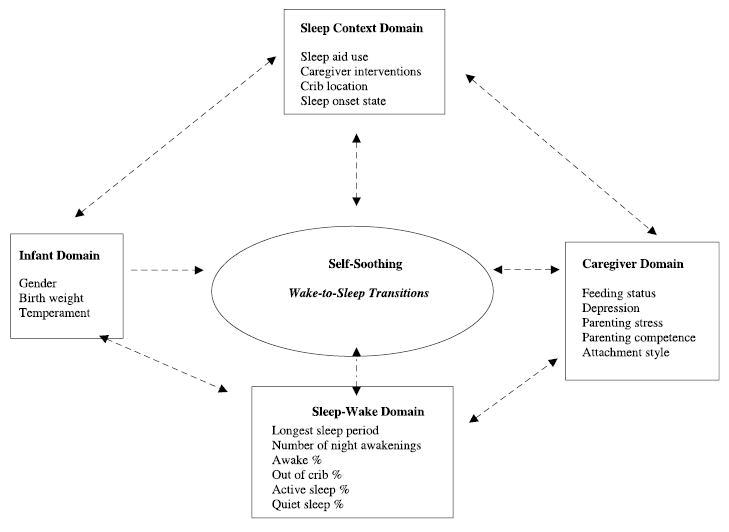
A transactional model for the development of self-soothing behaviors related to wake-to-sleep state transitions. The model, derived from empirical and clinical experience, provides a framework to guide investigation. More research is required to assess its predictive validity
Within the infant domain, the variable receiving most research attention in relation to infant sleep has been temperament. Infant temperament has been consistently, albeit moderately, related to the quality of nighttime sleep (Halpern, Anders, Garcia Coll, & Hua, 1994; Minde, Popiel, Leos, Falkner et al., 1993; Scher, Tirosh, & Lavie, 1998; Van Tassel, 1985). An association between temperament and middle-of-the-night self-soothing also has been reported (Keener et al., 1988). Fathers were found to rate non-self-soothing infants as more temperamentally difficult than self-soothing infants; however, a similar relationship did not hold for mothers’ ratings of temperament. Minde and colleagues (1993) reported an association between difficult temperament and problem sleep. In their study, problem sleepers were unable to return to sleep without a parental intervention (i.e., they were non-self-soothers).
Parental factors also have been associated with infant sleep disruption. Seifer and colleagues (Seifer, Sameroff, Dickstein, Hayden, & Schiller, 1996) reported an association between both higher levels of maternal mental illness and lower levels of overall family functioning and bedtime problems in toddlers. Benoit, Zeanah, Boucher, and Minde (1992) found that all of the sleep-disturbed toddlers in their sample had mothers with insecure attachment styles. Another study, however, failed to find a relation between maternal psychological well-being and infants’ tendency to self-soothe during the night. This null finding may have been due to the non-clinical range of maternal depression scores reported in this study (Goodlin-Jones et al., 2001).
Associations between the sleep context and sleep-wake domains and self-soothing have been illustrated most clearly to date. Infants who are placed into their cribs awake at the beginning of the night and who use a sleep aid are more likely to self-soothe than their counterparts (Anders et al., 1992; Goodlin-Jones et al., 1997). In addition, self-soothing infants have longer continuous sleep periods and longer total sleep times at night (Anders et al., 1992; Goodlin-Jones et al., 2001). There is clearly some evidence in support of the relationships between each of the model domains and nighttime self-soothing. A more detailed review of these associations has been published recently (France & Blampied, 1999).
The current study had three goals. As the first relatively large-scale longitudinal study to objectively investigate infant sleep, the first goal was to replicate previous work on the basic patterns of sleep-wake development across the first year of life. The second goal was to test a double blind, random assignment intervention trial to enhance self-soothing at night. The third goal was to identify potential factors leading to the development of self-soothing at 12 months of age.
Method
Participants
The study was approved by the Institutional Review Board of the University of California, Davis. Parents gave their informed consent to participate. Eighty-seven infants (43 males) and their families were initially recruited from community childbirth classes and announcements posted in local pediatric offices. Full term, singleton infants, without pregnancy or delivery complications and whose parents were not planning to co-sleep were included. In this sample of convenience, refusal and attrition rates were low. A total of 4 families dropped out of the study by the time their infants (3 females) were 1 month of age because of health problems in the infant or concerns about the video equipment. Three families with significant amounts of missing data were excluded from the final analyses, leaving 80 participants (42 males).
Demographic characteristics of the 80 participating families are presented in Table 1. The majority of infants were Caucasian (61; 76%), 1 infant (1%) was Asian, 3 (4%) were Hispanic, and 15 (19%) were considered by their parents as multiethnic. Seventy-seven percent of mothers in the sample delivered their infants vaginally; the remainder delivered via Caesarian section. All infants were healthy at birth and at all assessment periods. Families were not compensated for participation, but all families who completed the study were provided with a summary videotape of their infant’s sleep over the first year of life.
Table 1.
Sample characteristics
| Mean (SD) | Range | |
|---|---|---|
| Mother’s age | 29.60 (5.26) | 18–44 |
| Father’s agea | 32.24 (6.39) | 19–44 |
| SES (Hollingshead)a | 1.85 (.91) | 1–5 |
| Parity | 1.19 (.42) | 1–3 |
| Birth weight of child (g) | 3481.31 (432.14) | 2353.0–4479.2 |
Note. No significant differences between the RSA and SC groups were found for any of the demographic variables.
Missing data for one subject.
Protocols and procedures
The study was designed as a double-blind intervention trial that randomly assigned infants to either a ‘representational sleep aid’ (RSA) group or a ‘sham control’ (SC) group. Maternal scent has been shown to be a powerful and specific orienting and soothing stimulus for mammalian offspring. Rat pups locate and mark their personal feeding site immediately after birth by olfactory cues (Polan & Hofer, 1998). Similarly human infants, by 10 days of life, discriminate their own lactating mother from unfamiliar lactating mothers by areolar and axillary scents (Porter, Makin, Davis, & Christensen, 1992). Thus, the RSA group was provided a sleep aid infused with maternal odor while the SC group received an equivalent, but non-odorous sleep aid. The sleep aids were introduced into infants’ cribs at one month of age. Infants’ use of each sleep aid was repeatedly monitored to determine whether its introduction enhanced sleep and/or self-soothing across the first year of life. Although families were aware of their own group status, they were unaware of the other arm of the study. In addition, all sleep data coders were blind to the infants’ group membership.
In the RSA condition, mothers wore project T-shirts as nightshirts for two weeks. Each mother was given two T-shirts to wear on alternating nights when her infant was 2 weeks old. When the infant was 1 month, after 2 weeks of wearing, one of the T-shirts was knotted and placed into his/her crib. The second T-shirt was placed in a sealed plastic bag to be used as a ‘back-up’ during prescribed times when the first T-shirt needed to be washed. Each month from 2 to 12 months of age, using an odor-free detergent provided to them, mothers were asked to wash and then re-wear both T-shirts for 2–3 nights. This ‘refreshing’ procedure helped to assure that the T-shirt continued to smell like the mother. One worn T-shirt always remained in the crib, the other in a sealed plastic bag.
The same procedures and timing were followed in the SC condition, with the exception that mothers did not wear the T-shirts. Mothers in the SC condition were contacted at the same monthly intervals and the SC T-shirts were washed using the same odor-free detergent. Thus, infants in the RSA condition slept with an odoriferous soft object, refreshed monthly with their mothers’ scent, and infants in the SC condition slept with the identical soft object without maternal scent, refreshed monthly by washing with an odor-free detergent. During the initial 2-week period of wearing (or non-wearing), both groups of families were called on alternate days to ask about the child’s sleeping and eating habits and his/her health, and to verify fidelity to the assigned T-shirt protocol.
After the 2-week period of wearing (or non-wearing), when the infant was 1 month of age, a research assistant set up video equipment to record the infant’s nighttime sleep for two consecutive nights. Parents were asked to initiate recording at the child’s normal bedtime and turn the equipment off when the child woke for the day. At this time in both conditions, one of the T-shirts was knotted and placed into the child’s crib or bassinet and the other was placed in a plastic bag. Infants were videotaped again at 3, 6, 9, and 12 months of age for two consecutive nights. Caregivers filled out questionnaires at each age. Parents were asked to behave as they normally would in terms of bedtime routines and nighttime interventions. Although we cannot rule out the possibility that parents responded differently on the nights of recording, previous studies using the same method have shown little impact of the recording procedure on parents’ normal behavior (Anders et al., 1992).
Measures and apparatus
Measures are presented in terms of the model domains in which they fit.
Infant domain.
Demographics form.
Pertinent infant variables were gathered from a brief demographics form filled out by the primary caregiver when her infant was 2 weeks of age, detailing such background information as parental education and employment, pregnancy, birth and infant health history. Interim infant and family health status reports were repeated prior to each video recording.
Temperament.
Infant temperament was assessed at both 3 and 12 months of age using Rothbart’s Infant Behavior Questionnaire (IBQ; Rothbart, 1981). The IBQ is a 94-item instrument, from which 6 sub-scales are derived: activity level, smiling and laughter, distress and latency to approach novel stimuli, distress to limitations, soothability, and duration of orienting. Items are rated on a 7-point Likert scale, with 1 corresponding to ‘never’ and 7 to ‘always’. A ‘does not apply’ choice exists for each item as well. Higher scores on each sub-scale represent greater levels of that construct. Reported internal reliabilities for each sub-scale of this measure are moderate to high for both 3-and 12-month-old samples of infants (αs = .72−.85; Rothbart, 1981).
Sleep-wake & sleep context domains.
Time-lapse video recording.
Nighttime sleep was recorded for two consecutive nights at each of the 5 ages using time-lapse video equipment. The specifics of this method have been reported previously (Anders & Sostek, 1979; Anders & Keener, 1985). Briefly, nighttime sleep-wake behavior is recorded using a portable time-lapse video system consisting of a time-lapse videocassette recorder (Panasonic AG-6740P), a camera requiring low levels of illumination (e.g., Sanyo VDC-9212) that sits on a tripod next to the child’s crib, a 12" video monitor, and a microphone to record sound. Video and audio signals are recorded using the ‘18-hour mode’. Time-lapse video recording is not the same as time-lapse still photography in which single frames are exposed at pre-set time intervals and activity between exposures is missed. Time-lapse video records at an ultra-slow speed continuously, so that all behavior during the entire night can be recorded on one standard VHS videotape. The ‘18-hour mode’ insures that a whole night of sleep and waking behavior (8 hours, 10 hours or up to 18 hours) will be obtained. A time code generator records the ‘real’ clock time on the tape.
Graduate student research assistants, blind to the RSA/SC condition and trained to 85% reliability on sleep-wake state scoring, coded each tape using established criteria (Anders & Keener, 1985). The following sleep-wake variables were computed: the longest sleep period (LSP) and total sleep time (TST) in minutes, and the percentages of time in REM-active sleep (AS%), NREM-quiet sleep (QS%), wakefulness (AW%) and out of crib (OOC%) during the night’s recording period. Out of crib percent refers to the proportion of time, after sleep onset, that the child is removed from the crib by a caregiver for a nighttime intervention. The number of nighttime awakenings, the infant’s use of sleep aids, parental nighttime interventions in the crib or leading to an out of crib intervention, the sleep or waking state of the infant at entry into the crib, and crib location also were scored from the videotapes. In addition, the percent of awakenings for which infants self-soothed (SS%) was computed as the number of times an infant put herself back to sleep without a parental intervention following an awakening, divided by the total number of awakenings for a given night.
Caregiver domain.
Feeding status.
At each age (1, 3, 6, 9, and 12 months) mothers were queried about their method of feeding (breast, bottle or mixed), the introduction of solid foods, and the baby’s responses to feedings.
Depression.
Mothers were asked to fill out the Beck Depression Inventory (BDI; Beck, Ward, Mendelson, Mock, & Erbaugh, 1961) when their infant was 2 weeks of age, then at 1, 3, 6, 9, and 12 months. The BDI is a 21-item measure designed to assess levels of depression. Across studies, a mean internal reliability of .81 for non-psychiatric subjects has been reported (Beck, Steer, & Garbin, 1988). Scores range from 0 to 63, with higher scores indicating a higher degree of depression. In general, scores above 10 indicate at least mild levels of depression.
Parenting stress & parenting efficacy.
Mothers completed the Parenting Events Scale (PES) and the Parenting Sense of Competence Scale (PSOCS) when their infants were 1, 6, and 12 months of age. The PES, adapted for use with infants from original measure (Halpern & Garcia-Coll, personal communication, 1990), is a 20-item self-report instrument that measures the frequency and intensity of stresses associated with typical daily infant caregiving. Each item on the scale is rated on how often it occurs (rarely, sometimes, a lot, constantly) and how big of a hassle it is (1 = no hassle, 5 = big hassle). Higher scores on the frequency and intensity sub-scales indicate more parenting stress and a higher degree of hassle associated with this stress, respectively. High internal consistencies for both the frequency and intensity sub-scales have been reported (αs = .85 and .90, respectively; Crnic & Greenberg, 1990).
The PSOCS (Giband-Walston, 1977) assesses the caregiver’s sense of competence in the parenting role. Items are rated on a 6-point scale ranging from ‘strongly agree’ to ‘strongly disagree.’ Two sub-scale scores are derived from this instrument: ‘self-efficacy’ and ‘value of parenting.’ The first assesses the degree to which parents feel they have the knowledge and skills necessary to be a good parent and the second assesses the degree to which parents value and are comfortable in the parenting role.
Adult attachment style.
Caregivers’ attachment styles were assessed using the Relationship Questionnaire derived from Bartholomew’s prototype model of adult attachment (Bartholomew & Horowitz, 1991). Each of four statements are rated on a Likert-scale ranging from 1 (disagree strongly) to 7 (agree strongly). Participants are then asked which of the four statements describes them best. The four statements correspond to the secure, dismissing, preoccupied, and fearful attachment styles. Bartholomew and Horowitz (1991) report high concordance between this self-report measure and independent ratings from an adult attachment interview.
Data reduction and analysis
All statistics were computed using the Statistical Package for the Social Sciences (SPSS), Version 10. Because two nights of video were recorded at each age, two sets of sleep and sleep context variables were available at 1, 3, 6, 9, and 12 months. Pearson product-moment correlation coefficients were computed to compare the two nights. After verifying that all variables were significantly related from night to night at each age, all continuous variables were averaged across the two nights. For the nominal variables (state upon crib entry and sleep aid use), the Contingency Coefficient was used to compare nights. For state upon crib entry, a ‘mixed’ category was added to reflect the possibility that an infant was put to bed awake on one night and asleep on the other. For sleep aid use, infants using a different object on each of the nights were given the code ‘combination’ and those not using a sleep aid on one night but using one on the other were considered users of that object.
To examine the basic development of nighttime sleep-wake patterns, repeated measures general linear modeling (GLM) was used. To examine change over time in dichotomous sleep context variables (e.g., crib location, state upon crib entry, etc.) within subjects, Cochran’s Q was used. As an additional way of examining the longitudinal course of sleep-wake patterns, the sleep-wake variables were subjected to within-subjects ordinary least squares regression (Rogosa, 1995). This procedure involves computing a best fit, straight-line growth curve for each subject, with individual slope and intercept terms. The standardized slope can be interpreted as a measure of the degree of change over time and ranges from an absolute value of 0 to 1. The intercept represents the value at which the straight-line intersects the y-axis (i.e., the value at the presumed time of birth). In addition to allowing for the assessment of individual differences, this procedure served to reduce the number of variables for later analyses.
To examine the potential effects of sleeping with the odor-laden T-shirt on sleep-wake development and self-soothing, ‘protocol condition’ was added as a between-subjects contrast variable to the GLM procedure described above. In addition, a one-way Analysis of Variance (ANOVA) was used to examine whether the percent of self-soothed awakenings differed among those infants who were exposed to the odor-laden T-shirt versus those who were not at each age studied.
Stepwise multiple linear regression was used to test the relative impact of variables from each domain on self-soothing at 12 months. Only those variables that were independent within domains and correlated with self-soothing at 12 months were included in the regression analysis. Problems with multicollinearity between domains were avoided by excluding variables with shared variance.
Results
The development of sleep-wake patterns and self soothing
Sleep-wake state development.
Descriptive data on the nighttime sleep-wake variables are presented in Table 2. Results of the repeated measures GLM procedure revealed that the longest sleep period (LSP) increased significantly from 1 to 3 months, then leveled off for the remainder of the first year of life, F (4, 76) = 18.48, p < .01. Conversely, the number of nighttime awakenings per night dropped sharply from 1 to 3 months, then remained relatively stable from 3 to 12 months, F (4, 76) = 7.12, p < .01. The percent of time that infants spent out of the crib similarly decreased sharply from 1 to 3 months, then remained relatively constant from 3 to 12 months, F (4, 76) = 33.22, p < .01. The nightly proportion of time that infants were awake in their cribs, however, did not change significantly across the first year. The percent of time infants spent in active sleep decreased, F (4, 76) = 158.28, p < .01, while quiet sleep percent increased, F (4, 76) = 173.97, p < .01, from 1 to 12 months. Finally, total sleep time during the night increased linearly, F (4, 76) = 28.38, p < .01. It should be noted that all of these variables refer to nighttime sleep only. Although total 24-hour sleep decreases across the first year of life, sleep becomes consolidated such that nighttime sleep actually increases. As sleep periods consolidate, the percent of time out of the crib is reduced while the percent of time awake in the crib remains relatively constant. All of these results replicate previous findings on sleep-wake state development for healthy, solitary-sleeping infants (e.g., Anders & Keener, 1985).
Table 2.
Mean (SD) of sleep-wake variables and self-soothing percent from 1 to 12 months
| 1 month | 3 months | 6 months | 9 months | 12 months | |
|---|---|---|---|---|---|
| Total sleep time (min) | 341.38 (112.86) | 445.46 (116.92) | 477.88 (130.39) | 469.14 (138.84) | 480.49 (134.31)* |
| Longest sleep period (min) | 181.01 (58.18) | 281.38 (106.63) | 285.68 (131.88) | 284.34 (123.90) | 283.17 (120.50)* |
| # Night awakenings | 4.12 (2.57) | 2.78 (1.75) | 3.02 (2.09) | 2.81 (2.52) | 2.62 (2.03)* |
| Quiet sleep (%)a | 24.92 (8.98) | 38.46 (6.85) | 45.00 (8.45) | 49.96 (8.06) | 51.73 (6.82)* |
| Active sleep (%) | 66.01 (9.52) | 55.83 (6.12) | 48.25 (7.29) | 43.71 (7.15) | 40.88 (8.71)* |
| Out of crib (%) | 21.99 (16.12) | 8.18 (9.31) | 7.36 (11.22) | 6.36 (9.60) | 6.59 (10.00)* |
| Awake (%) | 5.49 (3.46) | 4.67 (3.29) | 5.70 (3.76) | 4.80 (4.60) | 5.19 (4.51) |
| Self-soothing (%) | 27.55 (26.18) | 33.25 (30.02) | 43.25 (38.02) | 47.55 (37.67) | 46.39 (36.31)* |
Percentages of QS, AS, OOC, and AW do not add up to 100% because the denominator for QS% is total recording period and the denominator for AS% is total sleep time.
p < .01.
Development of self-soothing.
The percentage of self-soothed awakenings increased in a linear fashion from 1 to 12 months of age, F (4, 57) = 4.86, p < .01. At 1 month, infants put themselves back to sleep following 27.6% of their awakenings. In contrast, by 12 months of age, infants self-soothed for 46.4% of their awakenings (see Table 2). A converse relationship exists for non-self-soothing awakenings which decreased proportionately with age. Remarkably, by one year of age, more than half of the infant awakenings still were non-self-soothing, requiring parental intervention.
Individual differences in the development of sleep-wake states and self-soothing
As indicated by the relatively large standard deviations in the sleep-wake and self-soothing variables (Table 2), individual differences clearly exist in their development. To further inspect these individual differences, the sleep-wake and self-soothing variables were examined using within-subjects regression. The resulting mean intercepts, standardized slopes, and percentage of infants with increasing and decreasing slopes are presented in Table 3. These results show, for example, that the longest sleep period increases over the first year for most children (as illustrated by a positive slope), but for some children it remains relatively constant or even decreases. The greatest amount of variability occurred for the percent of self-soothed awakenings (SS%), with 56.6% of the sample increasing and 43.4% decreasing across time. Thus, despite the significant linear increase found for SS% in the GLM analysis presented above, a substantial number of individual infants did not follow this pattern.
Table 3.
Descriptive data for the standardized slopes and intercepts of variables in the sleep-wake and self-soothing domains
| Standardized slope (β)
|
Intercept
|
|||
|---|---|---|---|---|
| Mean (SD) | % Increasing | % Decreasing | Mean (SD) | |
| LSP | .28 (.52) | 68.7 | 31.3 | 222.04 (85.07) |
| NAWK | −.25 (.57) | 33.7a | 65.0 | 3.73 (2.06) |
| QS% | .82 (.15) | 100.0 | 0.0 | 27.85 (7.37) |
| AS% | −.82 (.19) | 0.0 | 100.0 | 64.72 (7.66) |
| AW% | −.15 (.61) | 40.0 | 60.0 | 5.23 (3.14) |
| OOC% | −.47 (.46) | 18.7 | 81.3 | 16.65 (13.22) |
| TST | .38 (.52) | 71.2 | 28.8 | 382.78 (18.80) |
| SS% | .11 (.59) | 56.6 | 43.4 | 29.43 (24.74) |
One infant had a slope of .000.
Effects of the sleep aid intervention
There were no consistent effects on sleep patterns or on self-soothing behavior related to the sleep aid intervention, as determined by the analysis of representational sleep aid (RSA) versus sham control (SC) group differences. At 9 months of age, RSA infants did have slightly shorter longest sleep periods, F (4, 76) = 2.53, p = .04, and significantly more awakenings, F (4, 76) = 2.53, p = .04, than SC infants. However, because the RSA intervention demonstrated no consistent significant effects across time, the RSA and SC groups were collapsed for all analyses.
Domains of the transactional model
Infant domain.
Temperament.
Means and standard deviations for each dimension of temperament at 3 and 12 months of age are presented in Table 4. Correlations between the 6 dimensions of temperament at the two ages were moderate but significant, ranging from .27 for the activity level dimension to .53 for the smiling and laughter dimension (ps all < .05).
Table 4.
Descriptive data for sleep context variables from 1 to 12 months of age
| na | 1 month | 3 months | 6 months | 9 months | 12 months | |
|---|---|---|---|---|---|---|
| State at crib entry | ||||||
| Awake | 76 | 6 (8) | 15 (20) | 24 (32) | 19 (25) | 24 (32) |
| Asleep | 76 | 46 (61) | 36 (47) | 34 (45) | 38 (50) | 36 (47) |
| Mixed | 76 | 24 (32) | 25 (33) | 18 (24) | 19 (25) | 16 (21) |
| Crib location | ||||||
| Own room | 78 | 17 (22) | 34 (44) | 53 (68) | 58 (74) | 59 (76) |
| Parents’ room | 78 | 61 (78) | 44 (56) | 25 (32) | 20 (26) | 19 (24) |
| Sleep aid use | ||||||
| % awakenings | 57 | 29.1 (31.2) | 55.7 (37.0) | 60.4 (34.4) | 43.6 (33.8) | 54.8 (36.6) |
| Soft object | 76 | 0 (0) | 0 (0) | 1 (1) | 2 (3) | 4 (5) |
| Pacifier | 76 | 17 (22) | 7 (9) | 7 (9) | 11 (15) | 12 (16) |
| Thumb/fingers | 76 | 14 (18) | 18 (24) | 6 (8) | 3 (4) | 5 (7) |
| T-shirt (RSA/SC) | 76 | 3 (4) | 1 (1) | 2 (3) | 3 (4) | 1 (1) |
| Mixed w/o T-shirt | 76 | 8 (11) | 30 (39) | 24 (32) | 23 (30) | 21 (28) |
| Mixed w/T-shirt | 76 | 1 (1) | 6 (8) | 26 (34) | 14 (18) | 13 (17) |
| None | 76 | 33 (43) | 14 (18) | 10 (13) | 20 (26) | 20 (26) |
| Night interventions | ||||||
| # asleep | 74 | 1.4 (1.7) | 1.6 (1.8) | 1.6 (1.6) | 1.4 (1.2) | 1.2 (1.3) |
| Dur. to intv. (min) | 57 | 3.4 (2.5) | 3.3 (3.7) | 3.0 (3.0) | 2.8 (2.7) | 3.1 (4.3) |
Note. Results are reported as frequency or mean. Numbers in parentheses indicate percents or standard deviations.
Number of subjects (n) reflects subjects with complete data for the given variable. For ‘% awakenings where baby uses a sleep aid’ and ‘Duration to intervention,’ the number of subjects is reduced because some had no awakenings.
Caregiver domain.
Feeding status.
At 1 month of age, 65 (81%) infants were exclusively breastfed, an additional 12 (15%) were nursing at least part of the time, and only 3 (4%) were not breastfed at all. By 12 months, 44 infants (56%) had stopped breast-feeding altogether while the remaining 35 (44%) still nursed part of the time. The difference in the proportion of infants receiving some breast milk versus none with age was statistically significant, Cochran’s Q (4) = 112.43, p < .01.
Beck Depression Inventory.
Means and standard deviations for the total BDI scores are presented in Table 5. BDI scores decreased significantly from 2 weeks to 12 months, F (5, 73) = 7.63, p < .01. It should be underscored that all depression scores were well within the normal range as defined by Beck et al. (1988).
Table 5.
Mean (SD) of infant and caregiver domain variables across the first year
| 2 weeks | 1 month | 3 months | 6 months | 9 months | 12 months | |
|---|---|---|---|---|---|---|
| Infant temperament (n = 78) | ||||||
| Activity level | – | – | 3.31 (.65) | – | – | 4.10 (.72) |
| Distress to limitations | – | – | 3.40 (.81) | – | – | 3.59 (.78) |
| Distr. & lat. to approach stimuli | – | – | 2.17 (.76) | – | – | 2.89 (.58) |
| Smiling & laughter | – | – | 4.08 (.98) | – | – | 5.10 (.65) |
| Soothability | – | – | 4.39 (.78) | – | – | 5.12 (.85) |
| Duration of orienting | – | – | 3.74 (1.04) | – | – | 3.24 (.92) |
| Caregiver characteristics | ||||||
| Beck Depr. Inventory (n = 73) | 6.85 (4.24) | 5.55 (4.00) | 4.60 (4.28) | 4.73 (4.69) | 4.58 (6.03) | 3.97 (3.85)* |
| PES frequency (n = 74) | – | 34.36 (6.90) | – | 33.49 (5.86) | – | 35.19 (4.84)* |
| PES intensity (n = 74) | – | 33.42 (9.91) | – | 30.72 (7.98) | – | 33.73 (8.02)* |
| PSOC self-efficacy (n = 75) | – | 34.61 (5.47) | – | 36.36 (5.56) | – | 36.88 (5.05)* |
| PSOC value of parenting (n = 75) | – | 42.69 (5.93) | – | 44.61 (6.31) | – | 45.37 (4.84)* |
p < .00.
Parenting events scale.
The ‘frequency’ and ‘intensity’ sub-scores of the PES are presented in Table 5. These scores indicate the mothers’ reported amount of stress and the degree of associated hassle, respectively. The frequency and intensity sub-scores both started out relatively high at 1 month, decreased at 6 months, and increased again at 12 months, F (2, 74) = 3.85, p = .02 and F (2, 74) = 5.99, p < .01, respectively.
Parenting sense of competence scale.
As shown in Table 5, the ‘self-efficacy’ sub-score of the PSOCS showed a significant linear increase from 1 to 12 months of age, F (2, 75) = 11.44, p = .00. The same was true for the ‘value of parenting’ sub-score, F (2, 75) = 11.16, p = .00. Thus, both parental self-efficacy and comfort in the parenting role increased with time in this sample.
Attachment style.
Caregivers filled out the Relationship Questionnaire when their children were 2 weeks and 12 months of age. Significant between-age concordance was revealed for the attachment style ratings, C = .57, p = .00. Of the 76 caregivers with data at both ages, 49 (65%) agreed most with the ‘secure’ statement, 14 (18%) with the ‘dismissing’ statement, 4 (5%) with the ‘preoccupied’ statement, and 9 (12%) with the ‘fearful’ statement. These data are similar to those reported by Bartholomew and Horowitz (1991).
Sleep context domain.
State upon crib entry.
The infants’ state upon crib entry changed over the course of the first year (see Table 4). Among infants with full data at all 5 ages, 6 (8%) were placed into their cribs awake on both nights at 1 month. By 12 months, this number rose to 25 (32%). Conversely, at 1 month, 47 (60%) infants were placed into their cribs already asleep on both nights, while at 12 months the number had dropped to 37 (47%). This difference was not statistically significant, but revealed that a relatively higher proportion of parents began to place their infants into the crib consistently awake as their infants grew older. The percentage of infants placed into their cribs awake on one night and asleep on the other decreased slightly, but remained relatively constant across the first year (32% at 1 month versus 21% at 12 months).
Use of sleep aids.
Infants’ use of sleep aids changed significantly over the course of the first year (see Table 4). Sleep aid use was operationalized as both a dichotomous and continuous variable. As a dichotomous variable, infants were considered either ‘users’ or ‘non-users’ of sleep aids based on a global review of each night’s video data. Considered from this standpoint, more infants tended to use a sleep aid after 1 month of age, Cochran’s Q (4) = 27.56, p = .00. The proportion of non-users changed from 43.4% at 1 month to 26.3% at 12 months.
Sleep aid use was defined as a continuous variable as well, by viewing ‘use’ as the percent of awakenings for which an object was used. From this analysis, it was apparent that sleep aid use changed significantly over the course of the first year, F (4, 57) = 11.03, p = .00. At 1 month of age, infants used a sleep aid for just under 30% of their nighttime awakenings. This percent increased to 60% for 6-month-olds, decreased at 9 months to just over 40%, and increased again by 12 months to just over 50%. The types of sleep aids that infants used also changed with age. A higher percentage of 1-month-olds used a pacifier than infants at any other age. At 12 months of age, infants tended to use a mixture of different objects or nothing at all (see Table 4).
Crib location.
The location of the infant’s crib changed over the course of the year (see Table 4). Of the 78 infants with location data at all 5 ages, 78% were sleeping in their parents’ rooms at 1 month, compared to 24% of infants at 12 months, Cochran’s Q (4) = 114.72, p = .00. Interestingly, of the 61 infants who slept in their parents’ rooms at 1 month, 19 were still there at 12 months. That is, the only infants who were sleeping in their parents’ rooms at 12 months had been there from the beginning. Most infants were gradually moved into their own rooms in the first few months of life, with the majority (68%) sleeping in their own rooms by 6 months of age.
Caregiver interventions.
As shown in Table 4, the number of parental checks on a sleeping infant did not change substantially across the first year of life. The average number of parental checks when the baby was asleep ranged from 1.58 at 3 months (SD = 1.85, Range = 0–12) to 1.22 at 12 months (SD = 1.23, Range = 0–6). Similarly, the elapsed time between infant awakening and parent intervention did not change substantially over the first year. Among those infants who awoke and received an intervention, the average elapsed time was highest at 6 months (M = 3.72 min., SD = 4.56, Range = .5–26.75) and lowest at 12 months (M = 2.91 min., SD = 3.77, Range = .5–23.00).
Testing the model: Predicting self-soothing at 12 months of age
A regression analysis was conducted with the percent of self-soothed awakenings at 12 months as the dependent variable. The variables in each domain that were considered for entry into the regression equation because of their respective relationships with self-soothing at 12 months are discussed in detail below, followed by the results of the regression analysis.
Infant variables.
Birth weight, gender and parent-reported temperament were not related to self-soothing at 12 months.
Caregiver variables.
Twelve-month-old infants who were still breastfed part of the time had lower percentages of self-soothing at 12 months (M = 33.68, SD = 37.55) compared to those infants who had been weaned (M = 50.37, SD = 34.39; t (70) = 1.96, p = .05).
One-month caregiver scores for depression (r (71) = .30, p = .01), intensity of parenting stress (r (69) = .29, p = .01), caregiver self-efficacy (r (69) = −.28, p = .02), and value of the parenting role (r (69) = −.32, p = .00) were all significantly related to infants’ self-soothing at 12 months of age. Because the value of parenting score was significantly interrelated with each of the other variables, only this variable was entered into the regression equation.
Sleep context variables.
Significant correlations were found between infants’ state upon crib entry at 9 months (r (51) = −.44, p = .00) and 12 months of age (r (56) = −.32, p = .02) and self-soothing at 12 months. Infants who were placed into their cribs awake had higher percentages of self-soothing. The location of the infant’s crib (own room or parents’ room) at 3 months (r (72) = −.31, p = .00), 6 months (r (72) = −.36, p = .00), 9 months (r (72) = −.47, p = .00), and 12 months of age (r (72) = −.52, p = .00) also was related to self-soothing, with infants in their own rooms self-soothing more than infants in their parents’ rooms. The amount of time between an infant awakening and a parental intervention at 3 months (r (64) = .33, p = .01), 6 months (r (58) = .30, p = .02), and 9 months of age (r (52) = .41, p = .00) was related to self-soothing at 12 months as well, with longer durations associated with more self-soothing.
In terms of sleep aid use, the percent of awakenings during which any type of sleep aid was used at 12 months was positively related to self-soothing (r (72) = .33, p = .01). In addition, self-soothing at 12 months was positively associated with use of either the RSA or SC T-shirt as a soothing object at any time over the first year, compared to infants who had never used the T-shirt (r (72) = .45, p = .00). Because of the significant intercorrelations between crib location, use of T-shirt, percent of object use, state upon crib entry, and duration to intervention, only the two variables that were unrelated (crib location at 12 months and duration to intervention at 3 months) were entered into the regression equation.
Sleep-wake variables.
The standardized slopes for number of nighttime awakenings (r (72) = .26, p = .03), active sleep percent (r (72) = .37, p = .00), out of crib percent (r (72) = −.49, p = .00), and total sleep time (r (72) = .46, p = .00) and the intercepts for quiet sleep percent (r (72) = .312, p = .01) and active sleep percent (r (72) = −.35, p = .00) were related to self-soothing percent at 12 months. These variables were highly interrelated as well. Each of the slopes and intercepts were correlated with the intercept for quiet sleep percent and/or with the slope for out of crib percent; thus, only these two variables were included in the regression model. Infants who started out with higher percentages of quiet sleep and who spent increasingly less time out of their cribs across the first year self-soothed more at 12 months.
Multiple regression analysis.
For the regression analysis, the 6 significant, independent variables described above were entered into the equation in a stepwise fashion. These variables were: infant feeding status at 12 months, crib location at 12 months, duration to intervention at 3 months, value of parenting score at 1 month, the quiet sleep intercept, and the slope for out of crib percent. The most predictive variables of self-soothing percent at 12 months were the slope for out of crib percent, the intercept for quiet sleep, and the duration to intervention at 3 months (see Table 6). By far, the most influential predictor of self-soothing percent was the slope for out of crib percent, which explained approximately 22% of the variance in self-soothing by itself. The overall regression analysis with all 3 variables in the equation was significant, F (3, 79) = 18.16, p = .00. The final regression equation explained 40% of the variance in self-soothing percent at 12 months (adjusted R2 = .395). Each of the included variables contributed significantly, and independently, to the variance in self-soothing.
Table 6.
Summary of stepwise regression analysis for variables predicting self-soothing percent at 12-months (n = 78)
| Variable | B | SE B | β | ↖R2 | ↖F |
|---|---|---|---|---|---|
| Out of crib slope (std) | −38.37 | 6.76 | −.51* | .23 | 22.86* |
| Quiet sleep intercept | 1.74 | 0.42 | .37* | .15 | 18.16* |
| Duration to intervention, 3m | 2.21 | 0.93 | .21* | .04 | 5.64* |
Note. R2 = .417; Adj. R2 = .395 for full model; Reported ↖R2 and ↖F are for cumulative models (e.g., ↖F = 18.16 is for model including out of crib slope and quiet sleep intercept).
p < .03.
Discussion
Objective data regarding the factors associated with the emergence of nighttime infant self-soothing are increasingly important as families who need to adhere to their own sleep-wake schedules and meet their own sleep needs increase in number. The successful sales of popular books and videos designed to prevent or solve children’s sleep problems attest to a need for this type of information. Solitary-sleeping infants who put themselves back to sleep following nighttime awakenings, thereby allowing their parents to sleep through the night, are considered ‘good sleepers.’
The current study affords an opportunity to examine the development of sleep-wake states and the emergence of self-soothing in the same group of infants assessed at multiple ages across the first year of life. Contrary to our prediction, infants did not preferentially use the novel sleep aid saturated with maternal scent. Moreover, the odor-laden T-shirt’s presence in the crib affected neither the developmental course of sleep-wake state organization, nor the emergence of self-soothing per se. In an earlier pilot study, a similar non-effect had been noted (Goodlin-Jones et al., 1997). However, in that study, the maternal-scented (RSA) and scent free (SC) T-shirts had not been refreshed over the course of the year. In the current study, therefore, monthly washing and re-wearing of the RSA T-shirt and rewashing of the SC T-shirt were intended to refresh the RSA and SC conditions.
Introducing a purportedly attractive, familiar odor stimulus into an infant’s crib was an attempt to explore both the general role that sleep aids might play in enhancing self-soothing behaviors following nighttime awakenings over the first year of life, and the particular role of a ‘special’ sleep aid, a potential ‘transitional’ object. The absence of any effect supports Winnicott’s observations that infants choose their own transitional objects at some time between the ages of 4 and 12 months – the object of choice cannot be forced (Winnicott, 1953). Most infants in the current study did use some type of sleep aid during the night by 12 months, but their chosen object(s) did not necessarily include the odor-laden T-shirt.
Previous studies of infant sleep have not systematically examined contextual or parent–child interaction variables associated with sleep-wake organization. These experiential factors, such as crib location and infant state upon crib entry, are most likely transactional in that they are partly dependent on characteristics of both infant and caregiver. Age effects were noted for most of these variables. Although parents were more apt to put their infants into the crib awake at older ages, a significant proportion, close to 50%, continued to consistently place their child into the crib already asleep, even at 12 months. Parents were not less likely to check on their sleeping infants at older ages, nor were they more likely to wait longer before intervening at night. Interestingly, the elapsed intervention time was highest at 6 months and lowest at 12, suggesting that parents may attempt to wait longer in the middle months, but have learned the positive benefits of a quick response for infants who persist in waking at 12 months.
Infants’ use of sleep aids changed with age as well. Not surprisingly, a significantly larger proportion of infants used sleep aids at the older ages of study. Replicating the results of Passman and Halonen (1979), younger infants were more likely to use a pacifier and older infants a soft object. Similar to the results of a recent cross-sequential study of sleep aid use (Burnham, Goodlin-Jones, Gaylor, & Anders, in press), 6-month-olds used a sleep aid during a higher percentage of awakenings compared to all other age groups. Six-month-olds also used the intervention T-shirt more than infants at any other age in both studies. It is likely that 6-month-olds are at a stage in development during which exploration of the environment becomes prominent, thus making infants of this age more likely to explore objects in their cribs when compared to other age groups.
Sleeping location has rarely been objectively examined in previous studies of normal sleep practices in Western cultures. We observed that close to 80% of infants slept in their parents’ rooms at 1 month of age. Almost a third of these infants stayed in their parents’ rooms throughout the first year of life. It should be noted that the location of the infants’ crib in this sample was rarely, if ever, determined by a lack of space in the home. Further, most parents successfully moved their infants into a separate room between 3 and 6 months of age. It is likely that characteristics in both the infant and parent may contribute to the likelihood that an infant would remain in his parents’ room beyond the first few months of life. Although not examined a priori, a post-hoc analysis revealed that neither infant temperament nor maternal adult attachment style was related to crib location in this study. It would be of interest to determine prospectively what factors are related to crib location, and to follow infants who remained in their parents’ rooms at later developmental periods to see how their sleep patterns develop beyond the first year of life.
The longitudinal nature of this study provided an opportunity to examine which variables from the transactional model over the first year of life contributed significantly to the amount of self-soothing present at 12 months. Three independent variables explained approximately 40% of the variance in self-soothing. Infants who spent increasingly less time out of their cribs, who began life with higher levels of quiet sleep, and whose parents waited to respond to their awakenings were most likely to self-soothe at 12 months of age. It should be noted that each of these variables correlated highly with other variables within the same domain; these 3 predictor variables simply represented each domain best. Thus, the predictors really represent a cluster of variables that relate to self-soothing.
By far, the most influential predictor of self-soothing at 12 months was the slope for out of crib percent. It makes sense that infants who spend progressively more time in their cribs over the first year of life have more opportunities to self-soothe. This variable was related to a cluster of other sleep and contextual variables that were, in turn, also related to self-soothing percent. Infants who were placed into their cribs already asleep, who did not use a sleep aid, and who remained in their parents’ rooms spent increasing amounts of time out of their cribs across the first year of life and less time self-soothing.
The second significant predictor of self-soothing was the intercept term for the percent of quiet sleep. This term represents the mathematical or theoretical baseline level of quiet sleep, based on the slope of each individual’s quiet sleep trajectory. That is, it represents where the regression line intersects the y-axis at ‘time 0’ (i.e., birth). The percent of time an infant spends in quiet sleep is thought to be a marker for neurological maturity (Anders, Keener, & Kraemer, 1985). Thus, infants who exhibit higher levels of quiet sleep earlier may be intrinsically more mature and thus, more likely to exhibit the desired outcome of self-soothing at 12 months of age.
The final significant predictor variable was the average length of time it took for parents to respond to an infant’s awakenings at 3 months of age. The children of parents who waited longer to respond to their awakenings at 3 months were more likely to be self-soothers by 12 months of age. The 3-month duration-to-intervention variable was significantly correlated with the later duration-to-intervention variables as well, suggesting that parents who consistently wait longer to intervene are more likely to have self-soothing infants. A number of behavioral recommendations for the treatment of nighttime waking have included this ‘wait and see’ approach (e.g., Ferber, 1985; Mindell, 1999). To our knowledge, these are the first objective observations to show that longer response times early in the first year can lead to higher levels of self-soothing at 12 months.
Although not retained in the final regression equation via the stepwise procedure, a number of 1-month variables from the caregiver domain were related to self-soothing at 12 months. For example, the degree to which parents valued the parenting role when the infant was 1 month of age was negatively related to self-soothing at 12 months. Scores on this value of parenting scale were correlated with depression, parental self-efficacy, and the intensity of parenting stress. The nature of the relationships suggests that parents who were not able to dedicate themselves 100% to parenting (that is, placed lower value on the parenting role, had higher levels of depression and stress, and lower levels of parental self-efficacy) were more likely to have self-soothing infants at 12 months. These results do not suggest that parental absence or stress is a necessary ingredient for self-soothing. On the contrary, all of the scores within the caregiver domain were well within the normal range of functioning. It seems more likely that parents who are slightly less focused on immediate responsiveness, either through somewhat elevated depression scores, higher levels of stress, or other such symptoms, are less likely to respond to all awakenings, thus giving their children more opportunities to self-soothe. These relationships must be interpreted with caution; the caregiver variable was dropped from the regression equation, indicating that it did not explain significantly more variance in self-soothing than did the included variables.
It appears that infants who sleep in their own rooms are at an advantage for developing self-soothing behaviors compared to infants who remain in close proximity to their parents. Awakenings are more likely to go unnoticed if infants are sleeping separately. It is plausible that the children still in their parents’ rooms at 12 months may be there because they sleep poorly. Parents may choose to keep poor sleepers nearby so that sleep can be reinitiated more quickly after middle-of-the-night awakenings. Interestingly, a post-hoc analysis of these infants showed no differences in self-soothing percent, longest sleep period, or out of crib percent at the earliest ages of study, suggesting that the infants who remained in their parents’ rooms did not start out differently on any of these variables. In summary, these data clearly show that a cluster of sleep-wake and sleep context variables significantly impact the tendency for infants to self-soothe at 12 months of age.
It was surprising to find that several variables in the transactional model that were expected to relate to self-soothing at 12 months did not. In particular, none of the temperament dimensions related. Previous investigations have provided minimal or mixed results relating sleep to temperament (e.g., Halpern et al., 1994; Scher et al., 1998; Van Tassel, 1985). Most of these studies evaluated toddlers so it is possible that temperament affects sleep at later ages. But even in these studies, the findings are not robust. Only some aspects of temperament are related to sleep, and the relationship varies depending on the temperament measure used. Nevertheless, it was expected that ‘easier’ infants would more likely be self-soothers. The null result does not necessarily mean that temperament and self-soothing are not related.
It also was surprising to find that adult attachment orientation did not relate to self-soothing at 12 months. It was predicted that caregivers endorsing the secure statement would be more likely to have self-soothing infants, given theoretical speculation and the result of a previous investigation (Anders, 1994; Benoit et al., 1992). It is likely that positive results may require a more sensitive measure of adult attachment.
Several limitations should be kept in mind when evaluating the results of this investigation. The sample was largely Caucasian, middle-class, and non-clinical. It is possible that a more diverse sample would yield different and/or stronger results. For example, more variables from the caregiver domain may have related to self-soothing had this sample had more divergent scores on depression and parenting stress. Furthermore, although the domain constructs demonstrated moderate independence, there was some overlap. The slope for out of crib percent can be thought of as belonging to both the sleep-wake domain and the sleep context domain, in that being taken out of the crib is partly due to infant and caregiver characteristics. Further, the intercept for quiet sleep percent can be thought of as belonging to both the sleep-wake domain and the infant domain, due to the purported function of early quiet sleep as a marker for infants’ neurological maturity.
Finally, generalizations about the predictive capacity of the 3 most influential variables found in this study cannot be made due to the limited sample size. The inter-correlated nature of the variables within each domain suggests, at least, that the infant, sleep context, and sleep-wake domains impact self-soothing outcome.
The results of this study replicate previously reported developmental studies of sleep-wake state maturation (e.g., Anders & Keener, 1985). The proportions of active sleep decreased, quiet sleep increased, and the length of the longest sleep period increased sharply in the first 3 months and then leveled off for the remainder of the first year. What has not been previously reported is that deviations from these mean trajectories clearly exist. Our within-subjects analyses demonstrate that a number of infants do not follow the standard pathway. The current investigation was not designed to assess whether such differing trajectories might relate to future developmental, behavioral and/or sleep problems, but such associations deserve future study. For example, it is possible that two or more sub-groups of infants might be combined in our study. One group might comprise infants who are more immature and require more maternal intervention; a second group might comprise infants who are maturing appropriately but whose caregivers are responding more than necessary. Both groups would portray fewer non self-soothing awakenings. Only by analyzing unique trajectories can we begin to understand the potential consequences of individual differences.
The results of the current investigation suggest a number of avenues for future research. For instance, what happens to these self-soothers and non-self-soothers later in the toddler and preschool years? A follow-up study of the children at 2, 3, and 4 years of age is under way. In addition, further studies should continue to test the transactional model, using more advanced analytical techniques to examine the interrelationships between domains. Another area of research that has not been adequately addressed is whether or not daytime behavior is adversely affected by prominent and persistent nighttime non-self-soothing. If daytime behavior is not affected by fragmented nighttime sleep, then the suggestion that non-self-soothing infants are manifesting symptoms of a sleep disorder may need to be reconsidered. Only further research can address these issues.
Acknowledgments
This research was supported by a grant from the National Institute of Mental Health (R01-MH50741) to Thomas F. Anders. The authors wish to thank all of the families who participated in this study and the students, especially Amy Mao, who helped with data coding and collection.
References
- Anders TF. Infant sleep, nighttime relationships, and attachment. Psychiatry. 1994;57:11–21. doi: 10.1080/00332747.1994.11024664. [DOI] [PubMed] [Google Scholar]
- Anders TF, Halpern LF, Hua J. Sleeping through the night: A developmental perspective. Pediatrics. 1992;90:554–560. [PubMed] [Google Scholar]
- Anders TF, Keener M. Developmental course of nighttime sleep-wake patterns in full-term and premature infants during the first year of life I. Sleep. 1985;8:173–192. doi: 10.1093/sleep/8.3.173. [DOI] [PubMed] [Google Scholar]
- Anders TF, Keener MA, Kraemer H. Sleep-wake state organization, neonatal assessment and development in premature infants during the first year of life II. Sleep. 1985;8:193–206. doi: 10.1093/sleep/8.3.193. [DOI] [PubMed] [Google Scholar]
- Anders TF, Sostek AM. The use of time-lapse video recording of sleep-wake behavior in human infants. Psychophysiology. 1976;13:155–158. doi: 10.1111/j.1469-8986.1976.tb00092.x. [DOI] [PubMed] [Google Scholar]
- Bartholomew K, Horowitz LM. Attachment styles among young adults: A test of a four-category model. Journal of Personality and Social Psychology. 1991;61:226–244. doi: 10.1037//0022-3514.61.2.226. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Benoit D, Zeanah CH, Boucher C, Minde K. Sleep disorders in early childhood: Association with insecure maternal attachment. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:86–93. doi: 10.1097/00004583-199201000-00013. [DOI] [PubMed] [Google Scholar]
- Burnham, M.M., Goodlin-Jones, B.L., Gaylor, E.E., & Anders, T.F. (2001). The use of sleep aids during the first year of life In press, Pediatrics [DOI] [PMC free article] [PubMed]
- Crnic KA, Greenberg MT. Minor parenting stresses with young children. Child Development. 1990;61:1628–1637. doi: 10.1111/j.1467-8624.1990.tb02889.x. [DOI] [PubMed] [Google Scholar]
- Fagioli I, Salzarulo P. Sleep states development in the first year of life assessed through 24-h recordings. Early Human Development. 1982;6:215–228. doi: 10.1016/0378-3782(82)90109-8. [DOI] [PubMed] [Google Scholar]
- Ferber, R. (1985). Solve your child’s sleep problems New York: Simon & Schuster.
- France KG, Blampied NM. Infant sleep disturbance: Description of a problem behavior process. Sleep Medicine Reviews. 1999;3:265–280. [Google Scholar]
- Giband-Walston J. Self-esteem and situational stress: Factors related to competence in new parents (Doctoral dissertation, George Peabody College for Teachers, 1977) Dissertation Abstracts International. 1977;39:379B. [Google Scholar]
- Goodlin-Jones, B.L., Burnham, M.M., & Anders, T.F. (2000). Sleep and sleep disturbances: Regulatory processes in infancy. In A.J. Sameroff, M. Lewis, & S.M. Miller (Eds.), Handbook of developmental psychopathology (2nd edn, pp. 309–325). New York: Kluwer Academic/Plenum.
- Goodlin-Jones BL, Burnham MM, Gaylor EE, Anders TF. Night waking, sleep-wake organization, and self-soothing in the first year of life. Developmental and Behavioral Pediatrics. 2001;22:226–233. doi: 10.1097/00004703-200108000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodlin-Jones BL, Eiben LA, Anders TF. Maternal well-being and sleep-wake behaviors in infants: An intervention using maternal odor. Infant Mental Health Journal. 1997;18:378–393. [Google Scholar]
- Halpern LF, Anders TF, Garcia-Coll C, Hua J. Infant temperament: Is there a relation between sleep-wake states and maternal nighttime behavior? Infant Behavior and Development. 1994;17:255–263. [Google Scholar]
- Keener MA, Zeanah CH, Anders TF. Infant temperament, sleep organization, and nighttime parental interventions. Pediatrics. 1988;81:762–771. [PubMed] [Google Scholar]
- Kleitman N, Engelmann TG. Sleep characteristics of infants. Journal of Applied Physiology. 1953;6:269–282. doi: 10.1152/jappl.1953.6.5.269. [DOI] [PubMed] [Google Scholar]
- Lozoff B, Wolf AW, Davis NS. Sleep problems seen in pediatric practice. Pediatrics. 1985;75:477–483. [PubMed] [Google Scholar]
- Minde K, Popiel K, Leos N, Falkner S, et al. The evaluation and treatment of sleep disturbances in young children. Journal of Child Psychology and Psychiatry. 1993;34:521–533. doi: 10.1111/j.1469-7610.1993.tb01033.x. [DOI] [PubMed] [Google Scholar]
- Mindell JA. Empirically supported treatments in pediatric psychology: Bedtime refusal and night wakings in young children. Journal of Pediatric Psychology. 1999;24:465–481. doi: 10.1093/jpepsy/24.6.465. [DOI] [PubMed] [Google Scholar]
- Parmelee AH, Shulz HR, Disbrow MA. Sleep patterns of the newborn. Pediatrics. 1961;58:241–250. doi: 10.1016/s0022-3476(61)80164-9. [DOI] [PubMed] [Google Scholar]
- Passman RH, Halonen JS. A developmental survey of young children’s attachments to inanimate objects. Journal of Genetic Psychology. 1979;134:165–178. [Google Scholar]
- Polan HJ, Hofer MA. Olfactory preference for mother over home nest shavings by newborn rats. Developmental Psychobiology. 1998;33:5–20. [PubMed] [Google Scholar]
- Porter RH, Makin JW, Davis LB, Christensen KM. Breast-fed infants respond to olfactory cues from their own mother and unfamiliar lactating females. Infant Behavior and Development. 1992;15:85–93. [Google Scholar]
- Rogosa, D. (1995). Myths and methods: Myths about longitudinal research, plus supplemental questions. In J.M. Gottman (Ed.), Analysis of change (pp. 3–65). Mahweh, NJ: Lawrence Erlbaum.
- Rothbart MK. Measurement of temperament in infancy. Child Development. 1981;52:569–578. [Google Scholar]
- Sameroff, A.J., & Fiese, B.H. (2000). Models of development and developmental risk. In C.H. Zeanah, Jr. (Ed.), Handbook of infant mental health (2nd edn, pp. 3–19). New York: Guilford.
- Scher A, Tirosh E, Lavie P. The relationship between sleep and temperament revisited: Evidence for 12-month-olds: A research note. Journal of Psychology and Psychiatry. 1998;39:785–788. [PubMed] [Google Scholar]
- Seifer R, Sameroff AJ, Dickstein S, Hayden L, Schiller M. Parental psychopathology and sleep variation in children. Child and Psychiatric Clinics of North America. 1996;5:715–727. [Google Scholar]
- Van Tassel EB. The relative influence of child and environmental characteristics on sleep disturbances in the first and second years of life. Developmental and Behavioral Pediatrics. 1985;6:81–86. [PubMed] [Google Scholar]
- Winnicott DW. Transitional objects and transitional phenomena: A study of the first not-me possession. International Journal of Psycho-analysis. 1953;34:89–97. [PubMed] [Google Scholar]


