Abstract
Objective:
To examine the differential efficacy of trauma-focused, cognitive behavioral therapy (TF-CBT) and Child Centered Therapy (CCT) for treating posttraumatic stress disorder (PTSD) and related emotional and behavioral problems in children who have suffered sexual abuse.
Method:
Two hundred and twenty-nine 8–14 year old children and their primary caretakers were randomly assigned to the above alternative treatments. These children had significant symptoms of Posttraumatic Stress Disorder (PTSD) with 89% meeting full DSM-IV PTSD diagnostic criteria.
Results:
A series analyses of covariance indicated that children assigned to TF-CBT, as compared to those assigned to CCT, demonstrated significantly more improvement with regard to PTSD, depression, behavior problems, shame and abuse-related attributions. Similarly, parents assigned to TF-CBT showed greater improvement with respect to their own self-reported levels of depression, abuse-specific distress, support of the child, and effective parenting practices.
Conclusions:
This study adds to the growing evidence supporting the efficacy of TF-CBT with children suffering PTSD symptoms as a result of sexual abuse.
Keywords: PTSD, child sexual abuse, trauma-focused CT, treatment, trauma
INTRODUCTION
Child sexual abuse (CSA) is associated with numerous negative sequelae during childhood including depression, anxiety, behavioral problems, sexualized behaviors, and Posttraumatic Stress Disorder (PTSD) (Saywitz et al., 2000). CSA is also correlated with an increased risk for serious problems in adulthood, such as substance use disorders, social anxiety, depression and suicide attempts, and becoming a victim of adult rape (Brent et al., 2002; Nelson et al., 2002). Studies have also provided vital information about disordered psychobiological functioning related to CSA, including the finding that abused children with PTSD symptoms had smaller total brain and corpus collosum volumes and lower IQs than carefully matched controls, and that these differences were correlated with younger age of abuse onset and longer duration of PTSD symptoms (DeBellis et al., 1999). Thus, there is strong evidence that CSA, and in particular, CSA-related PTSD, places children at increased risk for suffering potentially life-long difficulties. Identifying treatment interventions which can effectively treat PTSD and other sequelae of such abuse in a timely manner is therefore of critical importance.
There has been a recent increase in empirical studies evaluating treatment outcome for sexually abused children; these have been reviewed in detail elsewhere (Saywitz et al., 2000). The most rigorous studies have included random assignment to well-defined, manualized treatments, and have compared these treatments to distinct comparison treatments or wait list control conditions. Deblinger, Lippmann and Steer (1996, 1999) followed 100 sexually abused children who were randomly assigned to receive one of four conditions: standard community care, trauma-focused cognitive behavioral therapy (TF-CBT) provided to the child only, TF-CBT provided to the non-offending parent only, or TF-CBT provided to both the child and parent. This study found that the children who received TF-CBT (either with or without the inclusion of their parent in treatment) experienced significantly greater improvement in PTSD symptoms, whereas children whose parents received TF-CBT (with or without inclusion of the child in treatment) experienced significantly greater improvement in child-reported depression and parent-reported behavioral problems; and that these differences were maintained at a two-year follow-up. Deblinger and her colleagues also evaluated the efficacy of this treatment approach with very young sexually abused children (ages 2 to 8) in a group format (Deblinger et al., 2001) and demonstrated the enhanced benefits of CBT groups, as compared to supportive group counseling with respect to maternal abuse- specific distress and children’s body safety skills.
Cohen and Mannarino (1996a; 1997) randomly assigned 69 sexually abused preschool children to TF-CBT or to non-directive supportive therapy (NST); children receiving TF-CBT experienced significantly greater improvements in PTSD symptoms including sexualized behaviors, and internalizing and total behavior problems than children receiving NST. These differences were maintained over the course of a one-year follow-up. Cohen and Mannarino (1998) also conducted a parallel study for sexually abused children ages 8–15 years and found that among 49 treatment completers, children who received TF-CBT experienced significantly greater improvement over time in depression and social competence than children who received NST. At one year follow-up, treatment completers in TF-CBT had significantly greater improvement in PTSD and dissociative symptoms. An intent-to-treat analysis indicated superior response in the TF-CBT group from pretreatment to 12-month follow-up, in depression, state and trait anxiety, and in sexual concerns (Cohen et al., 2003). Both of these studies included an individual parent treatment component.
King et al. (2000) randomly assigned 36 sexually abused children and adolescents to individual CBT, family CBT, or a wait list control condition, and found that children in both active treatment conditions improved significantly more than the wait list condition. Inclusion of family members in treatment showed a differential benefit in decreasing anxiety symptoms at a 3-month follow-up, but not immediately post-treatment. Two other studies evaluating trauma-focused treatments among sexually abused children did not demonstrate differential treatment responses with regard to PTSD or other anxiety symptoms (Berliner & Saunders, 1996; Celano et al., 1996).
Randomized controlled trials of treatment models other than TF-CBT have been rare. One study randomly assigned sexually abused children to 30 sessions of individual psychoanalytic psychotherapy or 18 sessions of group psychoeducation (Trowell et al., 2002). Children receiving the individual psychoanalytic therapy experienced significantly greater improvement in PTSD symptoms; however it is not clear whether this was because of differences in type of treatment (psychoanalytic versus psychoeducation), format of treatment (individual versus group) or length of treatment (30 versus 18 sessions). Another study (Downing et al., 1988) randomly assigned 22 sexually abused children to either psychodynamic therapy or behavioral reinforcement therapy, and found that the reinforcement therapy resulted in significantly greater improvements in sleep, enuresis, sexualized behaviors and general behavior problems than the psychodynamic treatment. Thus, there is some preliminary evidence that behavioral and psychodynamic therapies may also have some efficacy for improving certain symptoms in sexually abused children. More rigorous randomized trials of these treatments, using standardized assessments of DSM-IV disorders, will be helpful in determining the efficacy of these models.
Although treatment research for TF-CBT has grown impressively in the past decade, relatively small sample sizes have called into question the generalizability of the findings and have made it difficult to effectively examine the potential moderating effects of background characteristics. In addition, no study sample to date has documented a sufficiently high rate of other types of traumatic experiences to be considered representative of sexually abused children seen in community settings (Saunders, 2003). None has been simultaneously conducted at two or more sites, in order to include children from inner-city, suburban and rural settings and to compare findings across sites. The present study was designed to address these shortcomings. To our knowledge it is the first two-site, randomized controlled treatment trial for sexually abused children which includes a sample which is large and diverse enough to be considered representative of symptomatic sexually abused children who present for treatment. The current paper presents the design of the study and initial treatment outcome findings.
METHOD
Subjects
Subjects were 229 consecutively referred children ages 8–14 years, who had experienced contact sexual abuse which was confirmed by Child Protective Services (CPS), law enforcement or professional independent forensic evaluator, who met all study criteria and agreed (along with a custodial adult) to participate in the study. Children were recruited from two sites, one in a large metropolitan area and one in a suburban setting. Both sites are academically-affiliated outpatient clinical treatment programs for abused/traumatized children. Referral sources included CPS, police, victim advocacy centers and Child Advocacy Centers, pediatric care providers, mental health care providers, and self-referrals. No recruitment ads were placed. The recruitment, assessment and treatment protocols were identical at both sites and were reviewed and approved by the programs’ respective Institutional Review Boards.
For inclusion in the study, children had to meet at least 5 criteria for sexual abuse-related DSM-IV-defined PTSD, including at least one symptom in each of the three PTSD clusters (reexperiencing, avoidance or numbing, and hyperarousal). In addition, children were required to have a parent or other caretaker (including long-term foster parents) who was willing and able to participate in the parental treatment component of the study. Informed child assent and parental consent were required for admission to the study.
Children were excluded if they had an active psychotic disorder or an active substance use disorder which resulted in significant impairment in adaptive functioning, or if the parent or primary caretaker who would be participating in the treatment had such a disorder. Additionally, children were excluded if they were not fluent in English, and/or had a documented developmental disorder (e.g., autism). Children who were currently on psychotropic medication had to have been on a stable medication regimen for at least two months prior to admission to the study. Children in the study could not be receiving psychotherapy for sexual abuse outside of the study.
Of the original 229 children in the sample 5(2%) never returned for treatment, 8 (3%) left after attending one session, and 13 (6%) left after attending only two sessions. These 26 (11%) children and their parents were defined as dropouts. Therefore, 203 (88%) of the children attended at least three psychotherapy sessions, and this is the final sample upon which the analyses of covariance (ANCOVA) below are based. All 229 original subjects were included in the intent-to-treat analyses. The following flow sheet accounts for subjects at all stages of the study.
Nineteen (9%) of the final sample were currently taking psychotropic medications, and 39 (20%) had previously received counseling for the present sexual abuse episode. According to the Kiddie-Schedule for Affective Disorders and Schizophrenia Present and Lifetime Version PTSD section (K-SADS-PL-PTSD), 180 (89%) met full criteria for current PTSD. These children were described by their parents as having a variety of other psychological and behavioral problems. For example, although the mean pretest CBCL T score of the 203 children was 63.61 (SD=10.87), indicating that the average child had above normal levels of psychopathology, 71 (35%) children had T scores greater than 70, representing severe psychopathology.
The K-SADS-PL-PTSD was used to identify children’s exposure to traumatic events other than sexual abuse. For example, 144 (70%) these children had been confronted with news of the sudden unexpected death or life-threatening illness of a loved one, 118 (58%) had witnessed domestic violence; 53 (26%) were victims of physical abuse, 75 (37%) had witnessed or been involved in a serious accident; 35 (17%) were victims or witnesses of community violence; 28 (14%) had experienced a fire or natural disaster, and 51 (25%) had experienced other PTSD-level traumatic events, such as medical traumas, traumatic custody situations (e.g., being kidnapped by non-custodial parent), school violence not included in the K-SADS definition of community violence, and terrorist attacks. These children experienced a mean of 2.66 (SD=1.61) of traumatic events in addition to sexual abuse.
Among the 203 children, there were 14 sibling pairs, therefore there were 189 caretakers from whom we collected pretreatment data. Sibling pairs were assigned to the same treatment as it was essential for parents to receive only one parent treatment model. Sibling pairs were evenly distributed between the two treatment models. It should be noted that parents completed only one BDI at each evaluation point, even if they had more than one child in the study. Demographic information about participating children and parents are summarized in Table 1.
Table 1.
Demographics of Child Sample (N=203) and Participating Parents (N=189)
| Demographic Variables | Results |
|---|---|
| Gender: | |
| Female | 160(79%) |
| Male | 43(21%) |
| Age: | |
| Range | 8 yrs, 0 mos.-14 yrs, 11 mos |
| Mean | 10.76 yrs |
| Ethnicity (self-described): | |
| Caucasian | 122(60%) |
| African American | 56(28%) |
| Hispanic American | 9(4%) |
| Biracial | 14(7%) |
| Other | 2(1%) |
| Identity of Perpetrator: | |
| Stepparent | 46(23%) |
| Biological/adoptive parent | 15(7%) |
| Other adult relative | 33(16.3%) |
| Other adult non-relative | 42(20.7%) |
| Stranger | 5(2.5%) |
| Sibling | 13(6.4%) |
| Older peer (relative) | 13(6.4%) |
| Older peer (non-relative) | 25(12.3%) |
| Multiple perpetrators | 10(5%) |
| Most Intrusive Type of Sexual Abuse: | |
| Sexual touching over clothes | 6(2.9%) |
| Non-genital touching under clothes | 9(4.4%) |
| Digital penetration | 45(22%) |
| Simulated intercourse | 21(10.3%) |
| Oral-genital abuse | 41(20.1%) |
| Penile penetration | 76(37.4%) |
| Other | 8(3.9%) |
| How Perpetrator Engaged Child: | |
| Playful/coaxing | 22(10.8%) |
| Bribes | 8(3.9%) |
| Command | 40(19.7%) |
| Verbal threats | 38(18.7%) |
| Physical threats | 10(4.9%) |
| Physical force | 74(36.5%) |
| Mean Age at First Sexual Abuse Episode | 8.90 yo (SD = 2.59 years) |
| Mean Age of Most Recent Abuse | 9.81 yrs (SD = 2.33 years) |
| Median Number of Abuse Episodes | 4 (range 1-1000) |
| Mean Months Since Last Abuse | 12.25 (SD = 19.4) |
| Identity of Participating Parent: | |
| Biological mother | 148(78%) |
| Adoptive mother | 5(3%) |
| Stepmother | 3(2%) |
| Foster mother | 7(4%) |
| Grandmother | 9(5%) |
| Other female relative | 7(4%) |
| Biological father | 8(4%) |
| Stepfather | 1(1%) |
| Grandfather | 1(1%) |
| Mean Age of Participating Parent | 37.07 years (SD = 7.79) |
| Marital Status of Participating Parent | |
| Currently married | 77(41%) |
| Divorced or never married | 112(59%) |
| Employment Status | |
| Full time | 98(52%) |
| Part-time or unemployed | 91(48%) |
| Family Income: | |
| < $25,000 per year | 99(52%) |
| > $25,000 per year | 90(48%) |
| Participating Parent Currently Taking Psychotropic Medication | 30(16%) |
| Participating Parent with Drug/ETOH Abuse | 46(24%) |
| Participating Parent Received Treatment for Personal Sexual Abuse | 15/121 respondents (8%) |
Procedures
Upon referral to either participating center, an extensive initial phone screen was conducted, and the possibility of participating in the study was discussed with parents of children who appeared to meet study criteria. Those who agreed were scheduled for an initial assessment, which was conducted by independent evaluators at each site. Independent evaluators from the two sites were trained together in the administration and scoring of the semi-structured assessment instruments. Training was provided by the first and third authors, who had been trained to criteria in the administration of the K-SADS at Western Psychiatric Institute and Clinic. Acceptable inter-rater agreement was established between interviewers at the two sites. At the initial assessment, children and parents completed the assessment instruments described below, and those who qualified for admission to the study read and signed informed assent/consent forms. They were then assigned to a study therapist who was informed by one of the investigators as to the type of treatment they would be offering. The independent evaluator was blind to the treatment condition and informants were told that they would be paid $25 for the initial evaluation and $50 for each follow-up assessment.
Outcome Measures
The following instruments were administered by the independent evaluators at pre- and post-treatment to the children to measure psychiatric symptomatology: Kiddie-Schedule for Affective Disorders and Schizophrenia- Present and Lifetime Version (K-SADS-PL) (Kaufman et al., 1996), a semi-structured interview administered independently to child and parent to assess the presence of DSM-IV psychiatric disorders (for this study, the PTSD, Psychosis and Substance Use Disorders sections were used); Children’s Depression Inventory (CDI) (Kovacs, 1985), a well established self-report instrument for depressive symptoms in children; State-Trait Anxiety Inventory for Children (STAIC) (Spielberger, 1973), a widely used self-report measure of both present (state) and trait anxiety symptoms; and Children’s Attributions and Perceptions Scale (CAPS) (Mannarino et al., 1994), a self-report measure of children’s stigmatization, interpersonal trust, self-blame for negative events, and perceived credibility.
The following instruments were administered pre- and post-treatment to the parents: K-SADS-PL (described above); Child Behavior Checklist (CBCL) (Achenbach, 1991) which includes 4 broad band scales and 9 narrow band scales to assess child behavior problems (for the purposes of this study, only the broad band scales of social competence, internalizing, externalizing and total behavior problems were analyzed); Child Sexual Behavior Inventory (CSBI) (Friedrich et al., 1992), a parent report instrument for normative as well as inappropriate sexual behaviors; Beck Depression Inventory II (BDI) (Beck et al., 1996), a parent self-report measure of depression; the Parent’s Emotional Reaction Questionnaire (PERQ) (Mannarino & Cohen, 1996), a parent self-report measure for emotional distress related to their children’s sexual abuse experience; the Parental Support Questionnaire (PSQ) (Mannarino & Cohen, 1996), a self-report measure of parental support of their sexually abused child and attributions about responsibility for the abuse; and the Parenting Practices Questionnaire (PPQ) (Strayhorn & Weidman, 1998), a parent self-report instrument of parenting practices modified for use with this population (Stauffer & Deblinger, 1996). Three items from the original PPQ were modified from questions about general parenting practices to questions specific to interactions with children specific to sexual abuse. This revised version of the PPQ had an alpha coefficient of .72. All of these instruments have established acceptable psychometric properties and have been used in previous treatment studies of sexually abused children.
Treatment
Subjects were randomly assigned to either trauma-focused cognitive-behavioral therapy (TF-CBT) or Child Centered Therapy (CCT). Both treatments were manualized (Cohen & Mannarino, 1996b; Deblinger & Heflin, 1996). Study therapists at both sites were trained together over a three day period. Therapists were diverse in terms of their professional training (i.e. psychologists and social workers) and theoretical backgrounds (i.e. cognitive-behavioral, psychodynamic and play therapy). Three therapists had extensive experience in both TF-CBT and CCT; one had extensive experience in primarily providing CCT and one in primarily providing TF-CBT, and two therapists had relatively little experience in either modality. All therapists learned both treatment modalities and provided both treatments throughout the study. This design was used both to maintain the blindness of independent evaluators (who typically knew which therapist was treating each family), and also to eliminate the potential bias of a particularly effective therapist skewing treatment response in favor of one treatment over the other. Therapists had intensive weekly supervision in each treatment model. Additionally, twice monthly cross-site phone supervision for each treatment modality was provided. Fidelity to assigned treatment modality was monitored through supervisors listening to all treatment audiotapes, and through independent random rating of 25% of all audiotapes. Therapist fidelity for both treatments was >95%.
The treatment models used in this study were selected because they each had strong theoretical bases for treating sexually abused children, were widely used in community settings, and were sufficiently distinct from one another. Each treatment was provided in 12 weekly individual sessions to parent and child. One therapist treated each child-parent dyad. Treatment sessions lasted 90 minutes, with 45 minutes for each individual session. In three of the TF-CBT sessions, a joint parent-child session lasting approximately 30 minutes was provided; for these sessions, the individual child and parent sessions were reduced to 30 minutes.
Child Centered Therapy (CCT)
Child Centered Therapy (CCT) is a child/parent centered treatment model focused on establishing a trusting therapeutic relationship which is self-affirming, empowering and validating for the parent and child. This model is consistent with those widely used in rape crisis centers and other community settings to treat sexually abused children. It is based on the empirically supported premise that these children and their parents develop difficulties because they have experienced a violation of trust and disempowerment (Barker-Collo & Read, 2003; Finkelhor, 1987). CCT aims to reverse these difficulties through the establishment of an empowering trusting relationship and by encouraging children and parents to direct the content and structure of their own treatment, thereby allowing them to choose when, how and whether to address aspects of the child’s sexual abuse rather than the therapist deciding this. Therapists provided active listening, reflection, accurate empathy, encouragement to talk about feelings, and belief in the child’s and parent’s ability to develop positive coping strategies for abuse-related difficulties. Therapists offered limited interpretations when clinically appropriate, and addressed behavioral difficulties by encouraging the parent and child to formulate their own personal strategies for behavioral change, rather than providing prescriptive advice in this regard. Although sessions were generally client directed, written psychoeducational information about child sexual abuse was provided and children specifically prompted to share feelings about the sexual abuse during two therapy sessions if they did not do so spontaneously.
Trauma-focused CBT (TF-CBT)
The TF-CBT treatment model is informed by effective interventions for adult PTSD and for non-PTSD child anxiety disorders, and by cognitive and learning theories about the development of PTSD in children. It includes several components which are presented in a logical sequence with each module of treatment building on skills and progress gained from previous sessions.
Specific elements of the TF-CBT model include feeling expression skills, coping skills training, recognizing the relationships between thoughts, feelings and behaviors, gradual exposure (also referred to as creating the child’s trauma narrative), cognitive processing of the abuse experience(s), joint child-parent sessions, psychoeducation about child sexual abuse and body safety, and parent management skills.
As sessions proceeded, children were encouraged to confront increasingly detailed and distressing abuse-related reminders and memories. Children created narratives of their sexual abuse experiences, typically by writing and illustrating a book, which was shared with parents in their parallel sessions. The three joint parent-child sessions were used to optimize comfortable communication, to provide education about personal safety and healthy sexuality and to allow the child and parent to share and discuss the child’s trauma narrative together.
RESULTS
There were no significant differences between treatment completers and treatment dropouts on any demographic or psychosocial background characteristics of the children or parents. These demographic/psychosocial variables were also not significantly related to the likelihood of completing the posttreatment assessments. The two sites did not significantly differ on any of these background variables as well. Accordingly, the data from the two sites were pooled for analytic purposes, focusing on those participants who completed three or more sessions and participated in the posttest evaluations.
The mean number of CBT sessions provided was 10.47 (SD = 2.89) while the mean number of CCT sessions provided was 10.75 (SD = 2.44), t(201) =.75, ns, d = .10. These differences were not statistically significant. It should be noted that 149 (73%) of the children completed all 12 therapy sessions. Comparisons of the two treatment conditions are summarized in Table 2.
Table 2.
Treatment Outcome Measures
| Posttest | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pretest Scale | N | M | SD | M | SD | Madj | Mdiff | MS | F (1 | df) | d |
| Child | |||||||||||
| K-SADS Scales: | |||||||||||
| Reexperiencing | |||||||||||
| CBT | 89 | 3.98 | 1.31 | 1.53 | 1.39 | 1.55 | .75 | 2.38 | 10.68** | 177 | .49 |
| CCT | 91 | 4.08 | 1.30 | 2.32 | 1.81 | 2.30 | |||||
| Avoidance | |||||||||||
| CBT | 89 | 4.13 | 1.33 | 1.81 | 1.36 | 1.83 | 1.04 | 2.18 | 21.90*** | 177 | .70 |
| CCT | 91 | 4.35 | 1.13 | 2.89 | 1.62 | 2.87 | |||||
| Hypervigilance | |||||||||||
| CBT | 89 | 3.67 | 1.21 | 1.69 | 1.28 | 1.69 | .54 | 1.83 | 7.22** | 177 | .40 |
| CCT | 91 | 3.68 | 1.26 | 2.23 | 1.59 | 2.23 | |||||
| CBCL Scales: | |||||||||||
| Competence | |||||||||||
| CBT | 87 | 15.84 | 3.59 | 16.60 | 3.53 | 16.47 | −.02 | 7.02 | 0 | 173 | −.01 |
| CCT | 89 | 15.45 | 3.60 | 16.33 | 3.43 | 16.45 | |||||
| Internalization | |||||||||||
| CBT | 88 | 13.97 | 9.24 | 8.02 | 7.21 | 8.85 | 1.76 | 40.37 | 3.36 | 176 | .28 |
| CCT | 91 | 17.04 | 9.88 | 11.41 | 8.87 | 10.61 | |||||
| Externalization | |||||||||||
| CBT | 88 | 15.59 | 10.47 | 11.10 | 8.52 | 11.65 | 1.64 | 40.58 | 2.94 | 176 | .26 |
| CCT | 91 | 17.18 | 9.88 | 13.82 | 10.22 | 13.29 | |||||
| Total | |||||||||||
| CBT | 88 | 48.48 | 27.90 | 31.45 | 21.75 | 33.30 | 5.71 | 301.55 | 4.78* | 176 | .33 |
| CCT | 91 | 54.29 | 28.03 | 40.79 | 27.09 | 39.01 | |||||
| CDI | |||||||||||
| CBT | 92 | 9.92 | 7.50 | 5.70 | 5.47 | 6.34 | 1.80 | 36.36 | 4.04* | 180 | .30 |
| CCT | 91 | 12.11 | 8.59 | 8.79 | 9.37 | 8.14 | |||||
| STAIC Trait | |||||||||||
| CBT | 92 | 37.27 | 6.83 | 30.78 | 7.20 | 31.30 | 1.86 | 44.80 | 3.39 | 180 | .28 |
| CCT | 91 | 39.10 | 7.96 | 33.69 | 8.57 | 33.16 | |||||
| STAIC State | |||||||||||
| CBT | 92 | 30.51 | 6.84 | 26.22 | 5.10 | 26.42 | 1.13 | 26.92 | 2.17 | 180 | .22 |
| CCT | 91 | 31.48 | 8.32 | 27.76 | 6.94 | 27.55 | |||||
| CAPS Scales: | |||||||||||
| Feeling Different | |||||||||||
| CBT | 92 | 9.28 | 3.01 | 8.55 | 2.96 | 8.97 | −.03 | 7.60 | .01 | 180 | −.01 |
| CCT | 91 | 10.81 | 3.42 | 9.36 | 3.57 | 8.94 | |||||
| Negative Events | |||||||||||
| CBT | 92 | 7.82 | 3.05 | 6.46 | 2.46 | 6.63 | .43 | 5.35 | 1.57 | 180 | .19 |
| CCT | 91 | 8.58 | 2.91 | 7.24 | 2.89 | 7.06 | |||||
| Credibility | |||||||||||
| CBT | 92 | 12.46 | 3.14 | 10.37 | 3.38 | 10.65 | 1.22 | 12.58 | 5.16* | 180 | .34 |
| CCT | 91 | 13.82 | 3.98 | 12.15 | 4.26 | 11.87 | |||||
| Trust | |||||||||||
| CBT | 92 | 12.45 | 3.97 | 9.86 | 3.81 | 10.01 | 1.22 | 12.59 | 5.34* | 180 | .34 |
| CCT | 91 | 13.13 | 3.97 | 11.38 | 4.11 | 11.23 | |||||
| CSBI | |||||||||||
| CBT | 88 | 10.38 | 9.02 | 6.26 | 6.02 | 6.58 | 1.31 | 36.49 | 2.08 | 176 | .22 |
| CCT | 91 | 11.42 | 10.99 | 8.20 | 10.45 | 7.89 | |||||
| Shame | |||||||||||
| CBT | 91 | 2.84 | 2.28 | 0.87 | 1.35 | .90 | .67 | 2.09 | 9.52** | 178 | .46 |
| CCT | 90 | 3.03 | 2.18 | 1.60 | 1.87 | 1.57 | |||||
| Parent | |||||||||||
| BDI-II | |||||||||||
| CBT | 83 | 17.34 | 11.30 | 6.83 | 8.73 | 6.59 | 2.90 | 58.67 | 5.93* | 163 | .38 |
| CCT | 83 | 16.10 | 11.10 | 9.25 | 8.82 | 9.49 | |||||
| PERQ | |||||||||||
| CBT | 88 | 51.36 | 12.50 | 30.76 | 11.29 | 30.24 | 8.24 | 103.43 | 29.24*** | 176 | .81 |
| CCT | 91 | 49.49 | 11.44 | 37.98 | 12.84 | 38.48 | |||||
| PPQ | |||||||||||
| CBT | 82 | 135.60 | 15.20 | 144.38 | 15.55 | 144.67 | −5.77 | 101.03 | 13.82*** | 165 | −.57 |
| CCT | 86 | 136.44 | 15.80 | 139.19 | 13.61 | 138.90 | |||||
| PSQ | |||||||||||
| CBT | 88 | 88.38 | 6.52 | 90.28 | 6.50 | 90.52 | −2.81 | 37.02 | 9.53** | 176 | −.46 |
| CCT | 91 | 89.12 | 6.56 | 87.95 | 8.09 | 87.71 |
Note. Madj = Adjusted means, Mdiff = Adjusted mean differences, MS = Within mean squares, d = effect sizes for adjusted mean differences, K-SADS = Schedule for Affective Disorders and Schizophrenia for School Age Children, CBCL = Child Behavior Checklist, CDI = Children’s Depression Inventory, STAIC = Spielberger Trait-State Anxiety inventory for Children, CAPS = Children’s Attributions and Perceptions Scale, CSBI = Child Sexual Behavior Inventory, Shame = Shame Questionnaire, BDI-II = Beck Depression Inventory-II, PERQ = Parent Emotional Reaction Questionnaire, PPQ = Parent Practices Questionnaire, and PSQ = Parent Support Questionnaire.
p < .05,
p < .01,
p < .001
There was a main effect for time as children and parents in both treatments improved significantly from pre- to post-treatment on all measures but the PSQ. Consequently, analyses of covariance (ANCOVAs) were next performed to determine whether the adjusted mean scores of the scales for both treatments were comparable. The standardized effect size for the adjusted mean difference between the TF-CBT and the CCT groups for each scale was calculated by dividing the mean difference by the square root of the ANCOVAs Within Mean Square Error for the adjusted posttest score (Smithson, 2002). After controlling for the pretest score, the adjusted posttest scores of all three K-SADS-PTSD subscales (re-experiencing, avoidance and hyperarousal), the CBCL total scale, the CDI, the CAPS Credibility subscale, the CAPS Interpersonal Trust subscale, the Shame Questionnaire, the BDI-II, and the PERQ of the children and parents who were treated with TF-CBT were significantly lower than the adjusted posttest scores of those who were treated with CCT. Furthermore, the adjusted posttest mean scores of the PPQ and the PSQ were significantly higher than the adjusted mean score of those who were treated with CCT. These differences all reflect outcomes demonstrating the superiority of TF-CBT to CCT treatment. Table 2 indicates that all of these latter, significant adjusted-mean differences reflected medium to large effect sizes (Cohen, 1992).
A series of additional ANCOVAs were then conducted entering site, gender, ethnicity, age, and number of treatment sessions as main effects, and their interactions (product variables) with type of treatment to ascertain whether any of these characteristics might moderate differential responses to treatment. Intent-to-treat (end-point) analyses were also performed in which pretest scores were used to replace missing posttest scores. In addition, the SAS Multiple Imputation and Multiple Imputation Analysis (SAS Institute, 2001) procedures were employed to estimate the sample’s missing posttest scale scores. All of the ANCOVAS for the scales based on the end-point and multiple-imputation analyses to estimate missing posttest data displayed similar patterns of results to those previously described for the ANCOVAS summarized in Table 2. Furthermore, none of the ANCOVAs testing for the moderating effects of site, gender, race, ethnicity, age, and number of sessions yielded any significant main effects for these potential moderating variables and these variables’ possible interactions with type of treatment for any of the measures.
To estimate the clinical significance of treatment in reducing the prevalence of PTSD symptoms, a chi-square test for independence was used to compare the numbers of children who were diagnosed with PTSD at posttest in the TF-CBT and the CCT groups. Of the 89 children treated with TF-CBT for whom complete K-SADS data were available, 19 (21%) were diagnosed with PTSD at posttest. Forty-two (46%) of the 91 children who were treated with CCT were diagnosed with PTSD at posttest. These differences were statistically significant, χ2Yates (1, N = 180) = 11.28, p < .001, ϕ = .26. At pretest, the percentages of these 180 children who had been diagnosed with PTSD had been comparable for both the CBT (N = 75, 84%) and the CCT (N = 83, 91%) groups, χ2Yates (1, N = 180) = 1.42, ns., ϕ = .11.
DISCUSSION
This study is the first two-site controlled trial comparing alternative treatments designed for children suffering PTSD symptoms as a result of child sexual abuse. The findings demonstrated a consistent pattern of results, across completer, end-point and multiple imputation analyses. Children who received TF-CBT exhibited significantly greater improvements than those who received CCT on measures of PTSD, depression, and total behavior problems. Findings documented clinically as well as statistically significant benefits of receiving TF-CBT as more than twice as many CCT as TF-CBT children continued to meet full PTSD DSM-IV criteria at post-treatment.
This study was designed to not only replicate, but to extend earlier investigations. Previous studies have documented poorer outcomes in children who experience dysfunctional abuse attributions, higher levels of shame and distressed and/or unsupportive parental responses. These variables will be examined in future analyses as potential mediators of treatment outcome. However, in this investigation, they were conceptualized as important direct targets of treatment as well. In this regard, findings demonstrated that the TF-CBT group led to significantly greater improvements in children with respect to interpersonal trust, perceived credibility, and shame. Similarly, parents assigned to TF-CBT as opposed to CCT, reported significantly greater improvements with respect to their own levels of depression, abuse-related distress, parental support, and parenting practices. Thus, this study not only replicated previous findings concerning PTSD, depression and behavioral symptom outcomes, but revealed the enhanced benefits of TF-CBT with respect to these other crucial aspects of children’s cognitive and affective responses as well as parental functioning.
As compared to previous studies, the subject sample here was considerably larger; participants were recruited from geographically distinct regions; a larger number of therapists with diverse discipline and theoretical backgrounds were involved; a multiply traumatized population was included; and there was greater gender diversity represented in the treatment cohort. This larger, more diverse sample allowed analyses of these factors as potential moderators of treatment. The positive treatment response to TF-CBT among these multiply traumatized children suggests that there may be more commonality than differences among children who develop PTSD (Saunders, 2003) and that similar treatment interventions may be effective for children traumatized by different types of traumatic events.
Limitations
One limitation of this study is the lack of a no treatment control group. We chose not to include such a group, because of ethical concerns as well as previous studies that have demonstrated little to no symptom improvement in sexually abused children during wait list periods (King, et al. 2000; Stauffer & Deblinger, 1996). This study also did not elucidate which specific TF-CBT components underlie its superior effectiveness. Dismantling studies may help to determine if the exposure based interventions included in this TF-CBT approach are critical to the resolution of PTSD and/or shame in this population of children. Another limitation is that, although the population was diverse in many ways, relatively few Hispanic and no Asian families were included in this study. Although this largely is reflective of the ethnic population of the geographic areas involved in the study, it will be important to evaluate the generalizability of findings to families of other ethnicities.
Clinical Implications
This study empirically supports the effectiveness of a short term TF-CBT approach for multiply traumatized sexually abused children with PTSD and related difficulties. Given the mounting research documenting the severe and long-lasting risks associated with child sexual abuse, it is critical that we provide sexually abused children with the most effective treatment as early as possible. This imperative is further underscored by recent research reporting a relationship between early sexual abuse and the potential negative psychobiological impact of chronic PTSD on the developing brain (DeBellis et al., 1999b). In addition to the potential devastating effect of chronic PTSD, researchers have noted that shame and dysfunctional abuse attributions are also associated with poorer psychosocial outcomes in children who have suffered sexual abuse (Feiring et al., 1999; Mannarino & Cohen, 1996) and are predictors of negative outcomes in adulthood (Barker-Collo & Read, 2003). The TF-CBT approach evaluated here appears to not only effectively treat PTSD, but also is superior to CCT in reducing abuse-related attributions and shame. It is also effective in reducing parallel depression and parental distress about their children’s sexual abuse, and in enhancing parental support of the child and positive parenting practices. This study thus adds further support for the use of TF-CBT in treating multiply traumatized sexually abused children and adolescents.
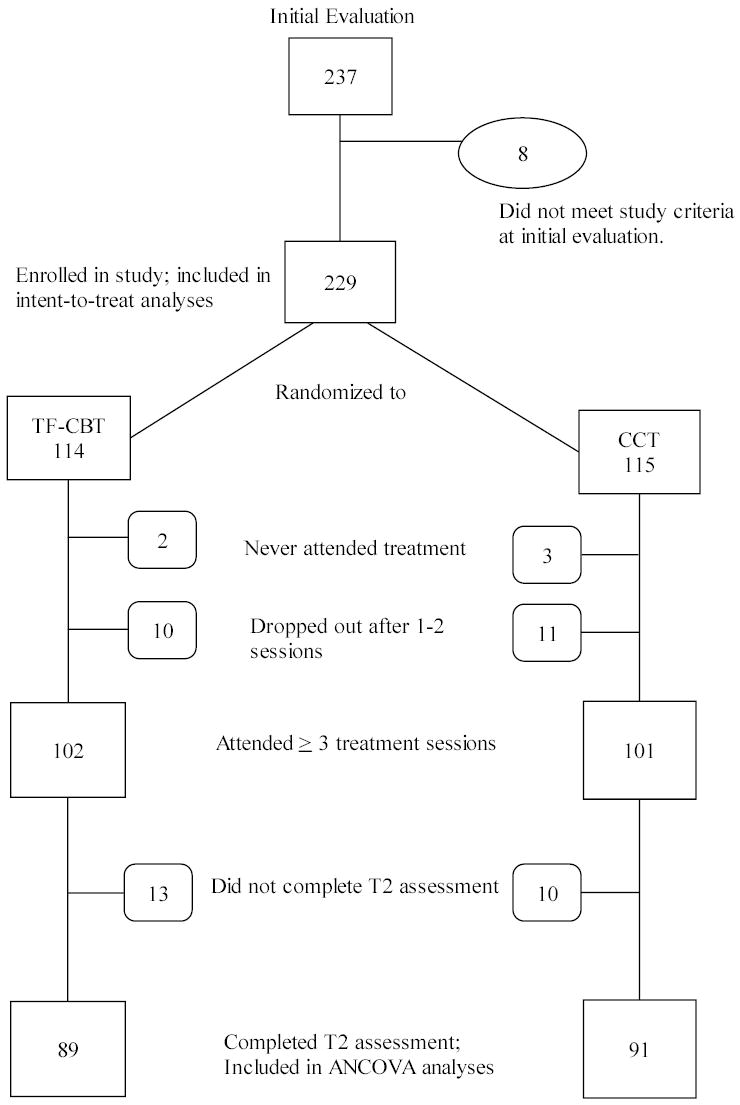
FLOW CHART
Footnotes
This research was funded by the National Institute of Mental Health, grants R10 MH55963 and R10 MH56224. The authors thank the study therapists, project coordinators, treatment supervisor, technical assistant, and the children and families who participated in this study.
References
- Achenbach TM (1991), Integrative guide for the 1991 CBCL/4-18 YSR and TRF profiles. Burlington, VT: University of Vermont, Department of Psychiatry
- Barker-Collo S, Read J. Models of response to childhood sexual abuse: Their implications for treatment. Trauma, Violence and Abuse. 2003;4:95–111. doi: 10.1177/1524838002250760. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK (1996), Manual for the Beck Depression Inventory II. San Antonio, TX: Psychological Corporation
- Berliner L, Saunders B. Treating fear and anxiety in sexually abused children: Results of a controlled two-year follow-up study. Child Maltreatment. 1996;1:294–309. [Google Scholar]
- Briere J (1995), Trauma Symptom Checklist for Children (TSC-C) Manual Odessa, FL: Psychological Assessment Resources, Inc
- Brent DA, Oquenda M, Birmaher B, Greenhill L, Kolko D, Stanley B, Zelazny J, Brodsky B, Bridge J, Ellis S, Salazar O, Mann J. Familial pathways to early-onset suicide attempt. Arch Gen Psychiatry. 2002;59:801–807. doi: 10.1001/archpsyc.59.9.801. [DOI] [PubMed] [Google Scholar]
- Celano M, Hazzard A, Webb C, McCall C. Treatment of traumagenic beliefs among sexually abused girls and their mothers: An evaluation study. J Abnorm Child Psychology. 1996;24:1–16. doi: 10.1007/BF01448370. [DOI] [PubMed] [Google Scholar]
- Cohen J. A power primer. Psychol Bull. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP. A treatment study for sexually abused preschool children: Initial findings. J Am Acad Child Adolesc Psychiatry. 1996;35:42–50. doi: 10.1097/00004583-199601000-00011. [DOI] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP. A treatment study of sexually abused preschool children: Outcome during one year follow-up. J Am Acad Child Adolesc Psychiatry. 1997;36(9):1228–1235. doi: 10.1097/00004583-199709000-00015. [DOI] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP (1996b), Child Centered Therapy Treatment Manual Unpublished treatment manual, MCP Hahnemann University School of Medicine, Pittsburgh, PA
- Cohen JA, Mannarino AP. Interventions for sexually abused children: Initial treatment findings. Child Maltreatment. 1998;3:17–26. [Google Scholar]
- Cohen JA, Mannarino AP, Knudsen K (2003), Treating sexually abused children: One year follow-up of a randomized controlled trial. Presented at American Psychiatric Association 156th Annual Meeting, San Francisco, CA
- Deblinger E, Heflin AH (1996), Treating Sexually Abused Children and Their Nonoffending Parents: A Cognitive-behavioral Approach Thousand Oaks, CA: Sage
- Deblinger E, Lippmann J, Steer R. Sexually abused children suffering posttraumatic stress symptoms: Initial treatment outcome findings. Child Maltreatment. 1996;1:310–321. [Google Scholar]
- Deblinger E, Steer R, Lippmann J. Two-year follow-up study of cognitive behavioral therapy for sexually abused children suffering posttraumatic stress symptoms. Child Abuse and Neglect. 1999;23(12):1371–1378. doi: 10.1016/s0145-2134(99)00091-5. [DOI] [PubMed] [Google Scholar]
- Deblinger E, Stauffer LB, Steer RA. Comparative efficacies of supportive and cognitive behavioral group therapies for young children who have been sexually abused and their nonoffending mothers. Child Maltreatment. 2001;6:332–343. doi: 10.1177/1077559501006004006. [DOI] [PubMed] [Google Scholar]
- Downing J, Jenkins SJ, Fisher GL. A comparison of psychodynamic and reinforcement treatment with sexually abused children. Elem School Guidance Counseling. 1988;22:291–298. [Google Scholar]
- Feiring C, Taska L, Lewis M. Adjustment following sexual abuse discovery: The role of shame and attributional style. Dev Psychol. 2002;38:79–82. doi: 10.1037//0012-1649.38.1.79. [DOI] [PubMed] [Google Scholar]
- Friedrich WN, Grambsch P, Damon L, Hewitt SK, Koverola C, Lang R, Wolfe V, Broughton D. Child Sexual Behavior Inventory: Normative and clinical comparisons. Psychol Assessment. 1992;4:303–311. [Google Scholar]
- Finkelhor DA. The trauma of child sexual abuse: Two models. Interpers Violence. 1989;2:348–366. [Google Scholar]
- Kaufman J, Birmaher B, Brent DA, et al. Schedule for Affective Disorders and Schizophrenia for School-Aged Children: Present and lifetime version (K-SADS-PL): Initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1996;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- King NJ, Tange BJ, Mullen P, Myerson N, Heyne D, Rollings S, Martin R, Ollendick TH. Treating sexually abused children with posttraumatic stress symptoms: A randomized clinical trial. J Am Acad Child Adolesc Psychiatry. 2000;39:1347–1355. doi: 10.1097/00004583-200011000-00008. [DOI] [PubMed] [Google Scholar]
- Mannarino AP, Cohen JA. Family related variables and psychological system formation in sexually abused girls. J Child Sexual Abuse. 1996;5:105–119. [Google Scholar]
- Mannarino AP, Cohen JA, Berman SR. Children’s Attribution and Perception Scale: A new measure of sexual abuse-related factors. J Clin Psychol. 1994;23:204–211. [Google Scholar]
- Nelson EC, Heath AC, Madden PAF, Cooper ML, Dinwiddie SH, Bucholz, KK, Glowinski A, McLaughlin T, Dunne MP, Statham DJ, Martin NG. Association between self-reported childhood sexual abuse and adverse psychosocial outcomes. Arch Gen Psychiatry. 2002;59:39–145. doi: 10.1001/archpsyc.59.2.139. [DOI] [PubMed] [Google Scholar]
- SAS Institute, Inc. (2001), SAS/STAT software: Changes and enhancements, release 8.2. Cary, NC: SAS Institute, Inc
- Saunders BE. Understanding children exposed to violence: Toward an integration of overlapping field. J Interpers Violence. 2003;18:356–376. [Google Scholar]
- Saywitz KJ, Mannarino AP, Berliner L, Cohen JA. Treatment for sexually abused children and adolescents. American Psychologist. 2000;55:1040–104. [PubMed] [Google Scholar]
- Smithson M (2002), Confidence Intervals: Quantitative Applications in the Social Sciences, No. 140. Thousand Oaks, CA: Sage
- Spielberger CD (1973), Manual for the State-Trait Anxiety Inventory for Children. Palo Alto, CA: Consulting Psychologists Press
- Stauffer L, Deblinger E. Cognitive behavioral groups for nonoffending mothers and their young sexually abused children: A preliminary treatment outcome study. Child Maltreatment. 1996;1(1):65–76. [Google Scholar]
- Strayhorn JM, Weidman CS. A parent practices scale and its relation to parent and child mental health. J Am Acad Child Adolesc Psychiatry. 1988;27:613–618. doi: 10.1097/00004583-198809000-00016. [DOI] [PubMed] [Google Scholar]
- Trowell J, Kolvin I, Weeramanthri T, Sadowski H, Berelowitz M, Glasser D, Leitch I. Psychotherapy for sexually abused girls: Psychopathological outcome findings and patterns of change. Br J Psychiatry. 2002;160:234–247. doi: 10.1192/bjp.180.3.234. [DOI] [PubMed] [Google Scholar]


