Key summary points
Aim
To evaluate differences among older patients demonstrating low sit-to-stand (STS) performance in the 30-s STS test (30 s-STS) and/or the 5-repetition STS test (5r-STS).
Findings
Patients with low performance in both STS tests had lower gait speed, were more frail, and had more prior falls compared to patients with low performance in one test only.
Message
The 30 s-STS and the 5r-STS test cannot be used interchangeable and represent different aspects of physical function.
Keywords: Muscle strength, Muscle function, Lower limb, Mobility-limited patients, Old age
Abstract
Purpose
We aimed to assess differences among older patients demonstrating low STS performance in the 30 s-STS and/or the 5r-STS.
Methods
30 s-STS and 5r-STS were used to assess lower limb muscle strength and function in older adults. Analysis involved 376 patients (≥ 65 years) from a geriatric outpatient clinic for fall assessment.
Results
The mean age of patients was 79.8 (± 6.1) years (67% female). In total, 40.6% had low STS performance with 9.3% presenting only low 30 s-STS, 9.8% only low 5r-STS, and 21.5% low STS performance in both tests. Patients with low STS performance in both tests had lower gait speed, were more often frail, and had more prior falls compared to patients with low STS performance in one test only.
Conclusion
The two STS tests are not interchangeable, and the use of both STS tests capture a wider range of physical abilities in mobility-limited older adults.
Clinical trial registration
Background
Several factors have been demonstrated to increase the risk of falling, including muscle weakness, and in many cases, falling is a symptom of decline in functional status in older adults [1–3]. Moreover, muscle strength is crucial for older adults to perform daily activities, maintain proper posture and balance, and acts as primary indicator of sarcopenia [4]. Hence, lower body strength and functional mobility are key components in fall assessment in older adults.
The sit-to-stand (STS) test is commonly used to assess an individual’s ability to rise from a seated position, providing valuable insights into lower limb muscle strength, endurance, power, and functional mobility in older adults [5–8]. Different versions of the STS test exist, including the 30-s sit-to-stand test (30 s-STS) [6] and the 5-repetition sit-to-stand test (5r-STS) [5]. Whereas 30 s-STS evaluates the number of STS transitions performed in 30 s [6, 7], and the 5r-STS measures the time taken to complete five STS cycles [5]. Notably, the 5r-STS test is also a component of the Short Physical Performance Battery (SPPB), which is widely used to assess lower body function in older adults [5].
In Denmark, the 30 s-STS is commonly used as part of the initial assessment of older patients with frailty [9, 10]. According to the European Working Group on Sarcopenia in Older People 2 (EWGSOP2), both the 30 s-STS and the 5r-STS can be used to measure lower limb muscle strength [4]. Yet, it remains unclear whether the two tests identify low performance in the same patients and the same aspects of physical performance in older individuals.
The aim of this study was to assess potential differences related to demographic, clinical, and physiological characteristics among older patients demonstrating low STS performance in the 30 s-STS test and/or the 5r-STS test.
Methods
Design and settings
This study used data from the BIOFRAIL study, a cross-sectional cohort study including older patients (≥ 65 years) referred to the geriatric outpatient clinic for fall assessment at Copenhagen University Hospital, Herlev and Gentofte, Denmark, between September 2021 and June 2023 (Clinical Trial registration: NCT05795556). Exclusion criteria were: (i) known severe dementia, (ii) inability to provide informed consent or to adhere to the test protocol, and (iii) inability to walk independently without personal assistance (use of walking aids was permitted). The study was approved by the local Ethics Committee of Copenhagen (H-20057620) and was conducted in compliance with the Declaration of Helsinki. All patients provided written informed consent.
Measurements
Patient characteristics included age, sex, and body mass index (BMI). STS performance was measured by the 30 s-STS test and the 5r-STS test [5, 6]. Patients were seated in the middle of a standardized chair, back straight, feet approximately a shoulder width apart, and arms across the chest. Verbal encouragement was given during the test. The patients were allowed to try both tests one time before the maximum trial. Low 30 s-STS performance was evaluated using the cut-off ≤ 8 repetitions [11] and low 5r-STS performance was defined as using more than 15 s for the 5 reps [4].
The 9-point Clinical Frailty Scale (CFS) was used to evaluate the presence of frailty defined by a score ≥ 5 [12]. Handgrip strength (HGS) was assessed using a hand-held dynamometer (Jamar Smart, Sammons Preston Rolyan, Chicago, Illinois, USA). A minimum of three attempts were made using the dominant hand, and the highest value obtained was selected for statistical analysis. Cut-off values for low HGS were < 27 kg for male and < 16 kg for female [4].
Appendicular lean mass (ALM) was assessed using direct segmental multi-frequency bioelectrical impedance analyses (DSM-BIA) (Inbody770 and InbodyS10; Biospace Co., Seoul, Korea) and reported as skeletal muscle index (SMI) (ALM (kg) adjusted for height2). Cut-off values for low muscle mass were < 7.0 kg/m2 and < 5.5 kg/m2, for male and female, respectively [4].
Gait speed (GS) was evaluated at maximal speed during horizontal walking over a 6-m course, with patients permitted to use their usual walking aids. The cut-off for low GS was ≤ 0.8 m/s [4]. Fall incidents within the past year were reported by the patient as part of the SARC-F questionnaire and classified as either no falls, 1–3 falls, or 4 or more falls [13].
Statistical analysis
Descriptive statistics were applied and low 30 s-STS and low 5r-STS were reported as the relative frequency in percentage (%). Patients were grouped based on whether they presented low values in 30 s-STS test, 5r-STS test, or both tests. Potential differences between the groups with only low values on the 30 s-STS or the 5r-STS were investigated using independent t tests, non-parametric test, or Chi2, as appropriate. Corresponding statistics were applied to investigate potential differences between the group with low values on both STS tests and the group with low value on only one of the two tests. P-values ≤ 0.05 were considered statistically significant. Statistical analysis was performed in SAS Studio.
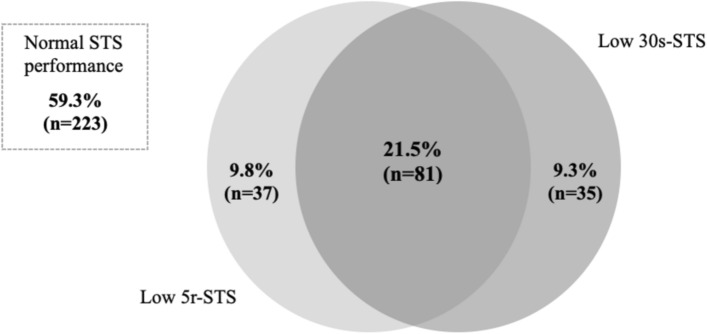
Results
This study included 376 patients (67% females (n = 252)), mean ± SD age 79.8 ± 6.1 years, and median [Q1;Q3] BMI 25.9 [23.0;28.4] kg/m2. Overall, 40.6% (n = 153) of the patients had low STS performance. Of these, 9.3% had only low 30 s-STS, 9.8% had only low 5r-STS, and 21.5% had low STS performance in both tests (Fig. 1).
Fig. 1.
A proportional Venn diagram showing the overlap of low performance on sit-to-stand test (STS) between the two tests, the 30 s-STS and the 5r-STS, in older geriatric outpatients. A total of 376 patients, of whom 223 (59.4%) did not have low STS performance
No significant differences were seen in age, BMI, frailty, low HGS, muscle mass, GS, or the number of falls in the past year, between patient characteristics according to the presence of low performance in either the 30 s-STS or the 5r-STS.
When comparing the group of patients who demonstrated low STS performance in both tests with the patients who exhibited low STS performance in one test only, the group with low performance in both tests had a significantly higher proportion of frailty, lower GS, and experienced more prior falls (Table 1).
Table 1.
Patient characteristics of the group who demonstrated low STS performance in both tests compared to the presence of either low 30 s-STS or 5r-STS performance
| All (n = 376) | Low STS both tests (n = 81, 21.5%) | Low 30 s-STS (n = 35, 9.3%) | p | Low 5r-STS (n = 37, 9.8%) | p | |
|---|---|---|---|---|---|---|
| Age (years), Mean (SD) | 79.8 (6.1) | 80.9 (6.6) | 80.9 (5.4) | 0.18 | 80.4 (4.8) | 0.64 |
| Sex—female, n (%) | 252 (67.0) | 60 (74.1) | 23 (65.7) | 0.20 | 23 (62.2) | 0.20 |
| BMI (kg/m2), Median (Q1;Q3) | 25.2 (23.0;28.4) | 26.3 (22.6;29.0) | 24.6 (22.7;28.1) | 0.26 | 24.3 (22.4;27.2) | 0.17 |
| Frailty (CFS ≥ 5), n (%) | 67 (19.4) | 33 (45.2) | 6 (18.2) | < 0.01 | 6 (17.7) | < 0.01 |
| Low HGSa, n (%) | 106 (28.6) | 32 (40.5) | 13 (37.1) | 0.84 | 9 (25.0) | 0.14 |
| Male, n (%) | 32 (26.2) | 10 (50.0) | 5 (41.7) | 3 (21.4) | ||
| Female, n (%) | 74 (29.7) | 22 (37.3) | 8 (34.8) | 6 (27.3) | ||
| Low SMIb, n (%) | 40 (11.3) | 10 (13.0) | 5 (16.7)α | 0.76 | 3 (8.1) | 0.54 |
| Male, n (%) | 10 (8.7) | 1 (5.3) | 1 (9.1) | 0 (0.0) | ||
| Female, n (%) | 30 (12.6) | 9 (15.5) | 4 (21.1) | 3 (13.0) | ||
| Low GS, n (%) | 43 (11.9) | 24 (31.2) | 5 (14.3) | 0.07 | 2 (2.7)β | < 0.01 |
| Self-reported falls during the past year, n (%) | 67 (19.4) | 68 (84.0) | 23 (65.7) | < 0.03 | 27 (73.0) | 0.13 |
Bold values indicate significant of p-values
30s-STS 30 s sit-to-stand, 5r-STS 5 repetitions sit-to-stand, BMI Body Mass Index, CFS Clinical Frailty Scale, GS gait speed, HGS Handgrip strength, SMI skeletal muscle index, STS sit-to-stand
an = 371 (male n = 122, female n = 249)
bn = 353 (male n = 115, female n = 238)
αn = 30, βn = 35
Discussion
The main finding of the study was the 30 s-STS and the 5r-STS test did not identifying low STS performance in the same patients, which may raise a discussion regarding the selection of which sit-to-stand tests to use in clinical practice among older adults. Our findings suggest that the 30 s-STS and the 5r-STS tests capture different aspects of lower body function and potentially identify different groups of patients at risk for falls, frailty, and functional decline.
In total, 40.6% (n = 153) of the patients had low STS performance. Of these, 21.5% (n = 81) had low performance in both STS tests, suggesting an ~ 50% overlap between the two tests in identifying individuals with lower limb muscle strength and functional impairments. Notably, patients with low performance in both tests had lower GS, higher prevalence of frailty, and experienced more falls compared to those with low performance in one test only, indicating these patients are at higher risk of adverse outcomes [14].
The finding that there is only ~ 50% overlap between the two STS tests highlights that the two STS tests capture different aspects of physical function. The 30 s-STS test measures a combination of muscle endurance and repetitive strength and is affected by motivation, balance, technique, and fatigue [6, 7]. In contrast, the 5r-STS test typically takes considerable shorter time, is more sensitive to lower limb muscle power, and less sensitive to changes in endurance [5, 8, 15]. Furthermore, the 5r-STS test tends to miss patients with very low muscle strength who cannot complete all five STS cycles [5, 8]. Therefore, the 30 s-STS is the most recommended and commonly used STS test in Denmark, whereas EWGSOP2 recommend that either of the 30 s-STS or the 5r-STS can be used to measure lower limb muscle strength [4].
We did not show significant differences between the group of patients with either low 30 s-STS or 5r-STS performance, which may be due to sample size. Future studies using larger samples should explore possible between group differences in other physiological parameters such as muscle power.
Our findings have important clinical implications for functional assessment in older adults. Using both the 30 s-STS and the 5r-STS tests in clinical and research settings will provide a more comprehensive assessment of older individual's physical capabilities. By doing so, practitioners can obtain a comprehensive evaluation of lower limb muscle strength, endurance, and power, thereby improving the accuracy of risk assessments and better fall prevention. However, we acknowledge that implementing both tests slightly extend the assessment time and therefore may not be possible in all settings. Moreover, some frail patients may have difficulty in performing both tests and the choice of test should, therefore, be setting dependent. Yet, it is noteworthy that these two tests that often are used interchangeable seems to represent different dimensions of physical function. Further research will help clarify the specific strengths and limitations of each test.
In conclusion, both the 30 s-STS and the 5r-STS are valuable for assessing lower limb muscle strength and functional performance in older adults. More importantly, the two STS assessments captures, to some extent, different aspects regarding physical ability and thereby risk of falls.
Acknowledgements
The authors would like to thank the physiotherapists, doctors, nurses, and secretaries from the outpatient clinic at Herlev and Gentofte Hospital for their cooperation and patience during patient recruitment and assessment. Furthermore, we would like to thank the physiotherapists for their help assessing the patients.
Author contributions
All authors met the criteria for authorship specified in the Uniform Requirements for Manuscripts Submitted to Biomedical Journals. Writing—original draft was done by PH and HN, and all authors were a part of the writing—review and editing process on previous versions. All authors read and approved the final manuscript.
Funding
No funds, grants, or other support was received to assist with the preparation of this manuscript.
Data availability
The data used in the analysis for the present study are available from the corresponding author [PH] upon reasonable request.
Declarations
Conflict of interest
PH, HN, JR, MTK and CS declare that they have no conflict of interest.
Ethical approval
The study protocol was approved by the local Ethics Committee of Copenhagen and Frederiksberg (H-20057620) and the Danish Data Protection Agency (P-2021–619). The project complies with the regulations set forth by the General Data Protection Regulation (GDPR) and the EU Data Protection Act. The study follows all ethical principles for research involving human subjects as stated by the Declaration of Helsinki, and all patients are given written informed consent prior to inclusion.
Informed consent
Informed consent was obtained from all individual participants included in the study. Prior to participation, all participants were provided with detailed oral and written information about the study, including its purpose, procedures, potential risks, and benefits. Participants were given the opportunity to ask questions and were informed that they could withdraw from the study at any time without penalty. Written informed consent was obtained from each participant prior to their inclusion in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ambrose AF, Paul G, Hausdorff JM (2013) Risk factors for falls among older adults: a review of the literature. Maturitas 75:51–61. 10.1016/j.maturitas.2013.02.009 [DOI] [PubMed] [Google Scholar]
- 2.Veronese N, Demurtas J, Soysal P, Smith L, Torbahn G, Schoene D et al (2019) Sarcopenia and health-related outcomes: an umbrella review of observational studies. Eur Geriatr Med 10:853–862. 10.1007/s41999-019-00233-w [DOI] [PubMed] [Google Scholar]
- 3.James SL, Lucchesi LR, Bisignano C, Castle CD, Dingels ZV, Fox JT et al (2020) The global burden of falls: Global, regional and national estimates of morbidity and mortality from the Global Burden of Disease Study 2017. Inj Prev 26:i3-11. 10.1136/injuryprev-2019-043286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T et al (2019) Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 48:16–31. 10.1093/ageing/afy169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG et al (1994) A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 49:85–94 [DOI] [PubMed] [Google Scholar]
- 6.Jones CJ, Rikli RE, Beam WC (1999) A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Res Q Exerc Sport 70:113–119. 10.1080/02701367.1999.10608028 [DOI] [PubMed] [Google Scholar]
- 7.McCarthy EK, Horvat MA, Holtsberg PA, Wisenbaker JM. Repeated chair stands as a measure of lower limb strength in sexagenarian women. J Gerontol A Biol Sci Med Sci 2004;59:1207–12. 10.1093/gerona/59.11.1207. [DOI] [PubMed]
- 8.Alcazar J, Losa-Reyna J, Rodriguez-Lopez C, Alfaro-Acha A, Rodriguez-Mañas L, Ara I et al (2018) The sit-to-stand muscle power test: An easy, inexpensive and portable procedure to assess muscle power in older people. Exp Gerontol 112:38–43. 10.1016/j.exger.2018.08.006 [DOI] [PubMed] [Google Scholar]
- 9.[in Danish] Den ældre skrøbelige patient. Dansk Selsk. Almen Med 2023. https://www.dsam.dk/vejledninger/aeldre/skrobelighed-i-almen-praksis#rejse-saette-sig-test. Accessed 29 July 2024
- 10.Kristensen MT, Dall CH, Aadahl M, Suetta C (2022) [in Danish] Systematisk måling af fysisk funktion hos voksne patienter på tværs af diagnoser. Ugeskr Laeger 184:1–7 [Google Scholar]
- 11.Rikli RE, Jones CJ (2013) Development and validation of criterion-referenced clinically relevant fitness standards for maintaining physical independence in later years. Gerontologist 53:255–267. 10.1093/geront/gns071 [DOI] [PubMed] [Google Scholar]
- 12.Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I et al (2005) A global clinical measure of fitness and frailty in elderly people. Can Med Assoc J 173:489–495. 10.1503/cmaj.050051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Malmstrom TK, Miller DK, Simonsick EM, Ferrucci L, Morley JE (2016) SARC-F: a symptom score to predict persons with sarcopenia at risk for poor functional outcomes. J Cachexia Sarcopenia Muscle 7:28–36. 10.1002/jcsm.12048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K (2013) Frailty in elderly people. Lancet 381:752–762. 10.1016/S0140-6736(12)62167-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bohannon RW, Bubela DJ, Magasi SR, Wang Y-C, Gershon R (2010) Sit-to-stand test: performance and determinants across the age-span. Isokinet Exerc Sci 18:235–240. 10.3233/IES-2010-0389.Sit-to-stand [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used in the analysis for the present study are available from the corresponding author [PH] upon reasonable request.