Abstract
Background
To investigate the prevalence of poor eye-use behavior and myopia in Chinese students, and examine the associations of poor eye-use behavior with myopia, as well as its study phase differences.
Methods
From March to July 2023, a total of 67 910 students were selected from 56 schools in 14 cities of China by stratified cluster sampling. The Eye-use Behavior Evaluation Scale for Students (EBESS) was adopted to investigate the eye-use behavior of students. Students underwent an uncorrected visual acuity examination and a non-cycloplegic autorefraction examination. The chi-square test was used to compare the prevalence of myopia between different groups. The binary logistic regression model was conducted to analyze the association of poor eye-use behavior with myopia.
Results
The prevalence of poor eye-use behavior and myopia of students were 27.6% and 53.0%, respectively. The poorer the eye-use behavior of students, the higher the prevalence of myopia (P < 0.001). After adjusting for age, gender, sibling, parental myopia, parental education level, self-reported learning burden, mode of travel to school, physical education lesson, city, usage distance of mobile phone / iPad / game console, reading and writing distance, weekdays outdoor time, and weekends outdoor time, binary logistic regression model analysis results showed that the poor eye-use behavior was positively correlated with myopia (OR = 1.10, 95% CI: 1.03 ~ 1.19). According to the study phase and further stratified analysis, in primary school (OR = 1.35, 95% CI: 1.20 ~ 1.50) and senior high school students (OR = 1.28, 95% CI: 1.08 ~ 1.51), poor eye-use behavior was positively correlated with myopia. However, in kindergarten and junior high school students, there was no statistically significant difference (P > 0.05).
Conclusion
Poor eye-use behavior was a potential risk factor for myopia in students, and this effect was significantly different between study phases. This suggests that future research should establish interventions to protect students from the effects of poor eye-use behavior.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12886-025-04072-1.
Keywords: Eye-use behavior, Myopia, Study phase
Background
Myopia, a common refractive error disorder, refers to the condition in which rays of light parallel to the optic axis enter the refractive system and focus in front of the retina when ocular accommodation is relaxed [1]. It is predicted that by 2050, approximately 49.8% of the global population will have varying degrees of myopia, with roughly 9.8% of this group progressing to high myopia [2]. China is one of the countries with high prevalence of myopia among children and adolescents [3]. According to the latest statistics, the prevalence of myopia among children and adolescents in China is 51.9%, among which the myopia rates of primary school students, junior high school students, and senior high school students are 36.7%, 71.4%, and 81.2%, respectively [4]. Children and adolescents are not only more likely to develop high myopia, but also have an increased risk of eye diseases such as macular degeneration, glaucoma, cataracts, and chorio-retinal atrophy in adulthood, resulting in early vision impairment and even vision loss [5–8]. In addition, the global economic cost of myopia is estimated at $20.2 billion per year, with profound consequences for both individuals and society [9]. Therefore, it is crucial to reduce the prevalence of myopia in children and adolescents.
Both genetic and environmental factors play crucial roles in the development and progression of myopia, despite their precise mechanisms being unknown. Epidemiological studies have shown that factors such as increasing age, family history, and a larger amount of near work are related to the higher prevalence of myopia [10–12]. Poor eye use habits, prolonged sitting at a desk for homework, excessive eye use, frequent use of electronic devices, and other close-eye use behaviors can increase the risk of myopia, while, engaging in various outdoor activity can decrease the risk of myopia [13–15]. Similarly, studies have found that children and adolescents who spend more time outdoors are less likely to develop myopia [16–17]. This may be because outdoor light can effectively prevent myopia by stimulating the release of dopamine in the retina and inhibiting the elongation of the eye axis [18–19]. Sleep duration also plays a significant role in the development of myopia [20]. Children who slept for 7 h or less, or approximately 8 h per day, exhibited a higher risk of developing myopia compared to those who slept for 9 h or more each day [20]. Studies have demonstrated a strong correlation between the high incidence of axial myopia among children and adolescents and environmental factors, including the environment in which children develop and their lifestyle habits [21–22]. Thus, it is necessary to pay attention to eye-use behavior (such as reading and writing posture, electronic device use, outdoor activity time, and sleep…) and the living environment of children and adolescents.
Based on research evidence, it appears that maintaining good eye-use habits seems to be an important factor in preventing myopia, and these factors include sleeping, reading and writing habits, outdoor activity, time spent in outdoor light, electronic device use, near work, and other vision-related habits [12, 16–17, 23, 24, 25]. Therefore, we adopted the Eye-use Behavior Evaluation Scale for Students (EBESS) to evaluate the eye-use behavior of students from outdoor activity time, electronic device use, sleep, social jet lag, reading and writing posture, visual environment, eye relaxation behavior, and other aspects [26]. The EBESS developed by our team exhibits strong reliability and validity, and future studies will further report on its development and validation. Furthermore, the EBESS has been adopted by the National Disease Control and Prevention Administration in 2023 and incorporated into the “Technical Guide for Public Health Comprehensive Intervention in the Prevention and Control of Myopia in Children and Adolescents” [26]. The aim of the current study is twofold: (a) to describe the prevalence of poor eye-use behavior and myopia in Chinese students, (b) to examine the associations of poor eye-use behavior with myopia in Chinese students, as well as its study phase differences.
Methods
Participants
This research was conducted between March and July 2023. Participants were recruited from 14 cities in China including Anqing, Bengbu, Chizhou, Chuzhou, Fuyang, Ganzhou, Hefei, Huangshan, Jiujiang, Luan, Maanshan, Xuancheng, Yangzhou, and Zhongshan, using stratified cluster sampling. First, 14 cities were selected by convenience sampling. Then, 1 kindergarten, 1 primary school, 1 junior high school, and 1 senior high school were randomly selected for each city using stratified cluster sampling. Finally, all students from 56 schools were required to complete a questionnaire survey. Students completed the electronic questionnaire by using smartphones to scan the quick response code. The questionnaire for kindergarten and primary school grades 1 ~ 3 students was filled out by parents or other guardians, and the questionnaire for primary school grades 4 ~ 6, junior high school, and senior high school students was filled out by students. All students from 56 schools were required to complete an uncorrected visual acuity examination and a non-cycloplegic autorefraction examination. The exclusion criteria were as follows: having a history of ocular surgery and having an eye disease.
The Ethics Committee of Anhui Medical University approved this study (NO: 20210735). Both the adult participants and the parents / guardians of all under-18s provided written informed consent.
Sociodemographic data
The following sociodemographic characteristics were obtained: age, gender (boys, girls), ethnicity (Han-ethnicity, others), study phase (kindergarten, primary school, junior high school, senior high school), number of siblings (0, ≥ 1), parental myopia (none myopia, one myopia, both myopia), parental education level (middle school and below, senior high school, college and above), self-reported learning burden (a little, some, much), mode of travel to school (walk to and from school, take public transportation, take the electric bike, ride on a bicycle, take a car), physical education classes (1 time a day, 4 times a week, 3 times a week, 2 times a week, be unaware of), city (Anqing, Bengbu, Chizhou, Chuzhou, Fuyang, Ganzhou, Hefei, Huangshan, Jiujiang, Luan, Maanshan, Xuancheng, Yangzhou, and Zhongshan), usage distance of mobile phone / iPad / game console (< 20 cm, 20 ~ 30 cm, > 30 cm), reading and writing distance (< 20 cm, 20 ~ 30 cm, > 30 cm), weekdays outdoor time (< 1 h/d, 1 ~ 2 h/d, > 2 h/d), and weekends outdoor time (< 1 h/d, 1 ~ 2 h/d, > 2 h/d).
Eye-use behavior evaluation
The EBESS was used to assess eye-use behavior in students [26]. The EBESS was composed of 2 sub-scales, including 15 items for kindergarten and primary school grades 1 ~ 3 students scale (see Table S1) and 16 items for primary school grades 4 ~ 6, junior high school, and senior high school students scale (see Table S2). Each item was rated on a Likert-type scale: 0 = “I can’t do it,” 1 = “I sometimes do it,” 2 = “I can do it.” The higher the total score indicates the better the eye-use behavior. According to the score, eye-use behavior can be divided into 3 groups: poor (0 to 19 points), medium (20 to 27 points), and good (28 to 30 points) in kindergarten and primary school grades 1 ~ 3 students. Similarly, eye-use behavior can be divided into 3 groups: poor (0 to 18 points), medium (19 to 29 points), and good (30 to 32 points) in primary school grades 4 ~ 6, junior high school, and senior high school students.
Visual acuity examination
In the present study, the standard logarithmic visual acuity E chart (conforming to the National Standard of People’s Republic of China, GB 11533–2011) was used to evaluate the students’ visual acuity. This standard recommends a five-mark record for Chinese students, equivalent to five minus the logarithm of the minimum angle of resolution (LogMAR) [27]. Visual acuity is measured on a scale ranging from 4.0 to 5.3, where higher values indicate better visual acuity [28]. The standard logarithmic visual acuity E chart was positioned within an illuminated cabinet, maintaining a luminance range of 80–320 cd/m2, and has been extensively used for screening reduced visual acuity in ophthalmology clinics and schools in China for over two decades [29]. The visual acuity examination was performed at a distance of 5 m from the standard logarithmic visual acuity E chart. It started with the right eye and then moved to the left eye, with the visual acuity of both eyes being recorded using the five-mark recording method. The procedure conformed to the International standard for recording visual acuity [30]. Prior to the visual acuity examination, students were instructed to remove their glasses or contact lenses. Then, uncorrected visual acuity (UCVA) was tested by opticians adhering to standard logarithmic vision testing procedures to ensure accurate and reliable inspection results. Finally, the values were transformed into logMAR for subsequent analyses (see Table S3) [30]. In this study, since the visual acuity of students’ left and right eyes were highly correlated (rUCVA = 0.828, P < 0.001), we used data from the right eye for the analysis.
Non-cycloplegic autorefraction examinations
Following the visual acuity examination, the refractive error of both eyes was accurately measured using an auto-refractor keratometer (KR-8800, Topcon, Tokyo, Japan) in a non-cycloplegic state. The device automatically obtained three measurements, which were then averaged. The refractive error was subsequently calculated as the spherical equivalent (SE) of the sphere plus half of the cylinder based on the auto-refraction results. If the SE refraction values of any two examinations differed by 0.50 diopters (D) or more, an additional measurement was conducted. In this study, since the refractive powers of students’ left and right eyes were highly correlated (rSE = 0.853, P < 0.001), we used data from the right eye for the analysis.
Definitions of reduced UCVA and myopia
In this study, reduced UCVA and myopia were defined according to the “Appropriate Technical Guidelines for Prevention and Control of Myopia in Children and Adolescents (Updated Edition)” issued by the National Health Commission of the People’s Republic of China in 2021 [31]. Reduced UCVA was defined as UCVA ≥ 0.3 logMAR for children aged 3 years, UCVA ≥ 0.2 log MAR for children aged 4 years, UCVA ≥ 0.1 logMAR for children aged 5 years, and UCVA > 0.0 logMAR for children aged 6 years or older [31]. Myopia was defined as UCVA ≥ 0.3 logMAR and SE ≤ − 0.50 D for children aged 3 years, UCVA ≥ 0.2 logMAR and SE ≤ − 0.50 D for children aged 4 years, UCVA ≥ 0.1 logMAR and SE ≤ − 0.50 D for children aged 5 years, as well as UCVA > 0.0 logMAR and SE ≤ − 0.50 D for children aged 6 years or older [31].
Statistical analyses
Statistical analysis was performed using SPSS software (version 23.0). Categorical variables were presented as frequencies and percentages, and continuous variables as mean ± standard deviation (mean ± SD). A chi-square test was conducted to compare the prevalence of myopia between different groups. The binary logistic regression model was used to analyze the association of eye-use behavior with myopia, including myopia as outcomes, and eye-use behavior as predictors. Age, gender, sibling, parental myopia, parental education level, self-reported learning burden, mode of travel to school, physical education lesson, city, usage distance of mobile phone / iPad / game console, reading and writing distance, weekdays outdoor time, and weekends outdoor time as covariates. The odds ratio (OR) and 95% confidence interval (CI) were reported. P < 0.05 was considered to be statistically significant.
Results
Distribution of myopia among students with different characteristics
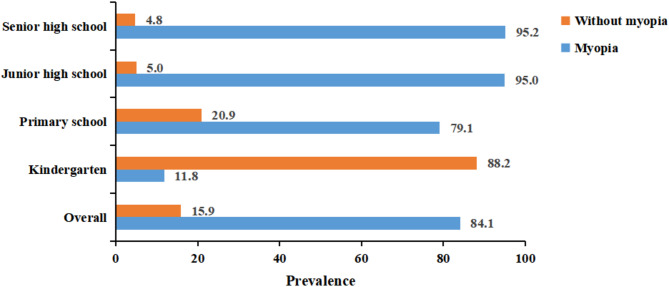
In this study, a total of 67 910 questionnaires were sent out, 50 299 were returned and 48 529 were valid. 25 595 were boys (52.7%), and 22 934 were girls (47.3%). The effective questionnaire rate was 96.5%. After the questionnaire and vision data were matched based on participants’ unique identification, the final data represented 36 400 valid cases. As shown in Table 1. The mean age of the 36 400 students was 12.23 years (SD = 3.75), and 52.5% (19 102 / 36 400) were boys. The prevalence of myopia in students was 53.0%. The prevalence of myopia was higher in girls than in boys (P < 0.001). The majority of the 36 400 students in this sample were of Han ethnicity (98.2%, n = 35 752). The prevalence of myopia in kindergarten, primary school students, junior high school students, and senior high school students was 7.3%, 35.1%, 68.9%, and 81.1%, respectively (P < 0.001). Students without siblings have a higher prevalence of myopia compared to those with siblings (P < 0.001). Students whose parents were myopia have a higher risk of developing myopia (P < 0.001). The prevalence of myopia exhibited a significant increasing trend with decreasing parental education levels and increasing study burdens among students (P < 0.001). The prevalence of myopia in students was highest among those who take public transportation, followed by those who ride bicycles, those who take cars, those who walk to and from school, and those who take the electric bike (P < 0.001). The closer the distance when students use mobile phone, iPad, or game console, as well as the reading and writing distance, the higher the prevalence of myopia (P < 0.001). Similarly, the shorter the time students spend on outdoor activities on weekdays and weekends, the higher the prevalence of myopia (P < 0.001). Additionally, the overall prevalence of myopia among students within the groups experiencing reduced UCVA was 84.1% (see Fig. 1). In kindergarten, primary school, junior high school, and senior high school, the prevalence of myopia among students within the groups with reduced UCVA was 11.8%, 79.1%, 95.0%, and 95.2%, respectively (see Fig. 1).
Table 1.
Distribution of myopia among students with different characteristics
| Variable | n (%) | Myopia | χ² value | P value |
|---|---|---|---|---|
| Age (mean ± SD) | 12.23 ± 3.75 | |||
| Sex | 171.25 | < 0.001 | ||
| Boys | 19,102(52.5) | 9506(49.8) | ||
| Girls | 17,298(47.5) | 9794(56.6) | ||
| Ethnicity | 2.94 | 0.087 | ||
| Han-ethnicity | 35,752(98.2) | 18,978(53.1) | ||
| Others | 648(1.8) | 322(49.7) | ||
| Study phase | 7860.72 | < 0.001 | ||
| Kindergarten | 2830(7.8) | 208(7.3) | ||
| Primary school | 14,757(40.5) | 5178(35.1) | ||
| Junior high school | 10,995(30.2) | 7573(68.9) | ||
| Senior high school | 7818(21.5) | 6341(81.1) | ||
| Number of siblings | 52.23 | < 0.001 | ||
| 0 | 11,728(32.2) | 6540(55.8) | ||
| ≥ 1 | 24,672(67.8) | 12,760(51.7) | ||
| Parental myopia | 18.60 | < 0.001 | ||
| None | 19,874(54.9) | 10,412(52.4) | ||
| One | 11,560(31.9) | 6345(54.9) | ||
| Both | 4781(13.2) | 2529(52.9) | ||
| Paternal education level | 745.13 | < 0.001 | ||
| Middle school and below | 15,594(42.8) | 9276(59.5) | ||
| Senior high school | 9697(26.6) | 5281(54.5) | ||
| College and above | 11,109(30.6) | 4743(42.7) | ||
| Maternal education level | 905.92 | < 0.001 | ||
| Middle school and below | 17,049(46.8) | 10,213(59.9) | ||
| Senior high school | 8833(24.3) | 4743(53.7) | ||
| College and above | 10,518(28.9) | 4344(41.3) | ||
| Self-reported learning burden | 1579.70 | < 0.001 | ||
| A little | 4845(13.3) | 1534(31.7) | ||
| Some | 24,006(66.0) | 12,624(52.6) | ||
| Much | 7549(20.7) | 5142(68.1) | ||
| Mode of travel to school | 662.71 | < 0.001 | ||
| Walk to and from school | 10,080(27.7) | 5420(53.8) | ||
| Take public transportation | 3496(9.6) | 2468(70.6) | ||
| Take the electric bike | 16,015(44.0) | 7621(47.6) | ||
| Ride on a bicycle | 1545(4.2) | 933(60.4) | ||
| Take a car | 5264(14.5) | 2858(54.3) | ||
| Physical education lesson | 1074.36 | < 0.001 | ||
| 1 time a day | 2107(5.8) | 1401(66.5) | ||
| 4 times a week | 5783(15.9) | 2942(50.9) | ||
| 3 times a week | 10,169(27.9) | 5497(54.1) | ||
| 2 times a week | 16,442(45.2) | 9095(55.3) | ||
| Be unaware of | 1899(5.2) | 365(19.2) | ||
| City | 1505.48 | < 0.001 | ||
| Anqing | 1805(5.0) | 912(50.5) | ||
| Bengbu | 2737(7.5) | 1857(67.8) | ||
| Chizhou | 1688(4.6) | 770(45.6) | ||
| Chuzhou | 4770(13.1) | 2970(62.3) | ||
| Fuyang | 2161(5.9) | 947(43.8) | ||
| Ganzhou | 3032(8.3) | 1219(40.2) | ||
| Hefei | 3250(8.9) | 2022(62.2) | ||
| Huangshan | 1612(4.4) | 1062(65.9) | ||
| Jiujiang | 3520(9.7) | 1378(39.1) | ||
| Luan | 1641(4.5) | 543(33.1) | ||
| Maanshan | 1554(4.3) | 915(58.9) | ||
| Xuancheng | 2471(6.8) | 1301(52.7) | ||
| Yangzhou | 2315(6.4) | 1288(55.6) | ||
| Zhongshan | 3844(10.6) | 2116(55.0) | ||
| Usage distance of mobile phone / iPad / game console | 266.82 | < 0.001 | ||
| < 20 cm | 18,755(51.5) | 10,567(56.3) | ||
| 20 ~ 30 cm | 10,187(28.0) | 5362(52.6) | ||
| > 30 cm | 7458(20.5) | 3371(45.2) | ||
| Reading and writing distance | 31.52 | < 0.001 | ||
| < 20 cm | 16,972(46.6) | 9144(53.9) | ||
| 20 ~ 30 cm | 12,623(34.7) | 6755(53.5) | ||
| > 30 cm | 6805(18.7) | 3401(50.0) | ||
| Weekdays outdoor time | 48.55 | < 0.001 | ||
| < 1 h/d | 15,170(41.7) | 8328(54.9) | ||
| 1 ~ 2 h/d | 11,021(30.3) | 5571(50.5) | ||
| > 2 h/d | 10,209(28.0) | 5401(52.9) | ||
| Weekends outdoor time | 259.04 | < 0.001 | ||
| < 1 h/d | 12,482(34.3) | 7332(58.7) | ||
| 1 ~ 2 h/d | 10,933(30.0) | 5590(51.1) | ||
| > 2 h/d | 12,985(35.7) | 6378(49.1) |
Fig. 1.
The prevalence of myopia among reduced UCVA
Comparison of myopia among different eye-use behavior
As shown in Table 2. The prevalence of good, medium, and poor eye-use behavior of students was 27.7%, 44.7%, and 27.6%, respectively. The poorer the eye-use behavior of students, the higher the prevalence of myopia (P < 0.001). According to the study phase and further stratified analysis, the results indicate that in both primary school and senior high school students, the poorer the eye-use behavior of students, the higher the prevalence of myopia (P < 0.001). However, there was no statistically significant difference among kindergarten and junior high school students (P > 0.05).
Table 2.
Comparison of myopia among different eye-use behavior groups
| Study phase | Eye-use behavior | n (%) | Myopia | χ² value | P value |
|---|---|---|---|---|---|
| Overall | Good | 10,099(27.7) | 4888(48.4) | 348.42 | < 0.001 |
| Medium | 16,279(44.7) | 8326(51.1) | |||
| Poor | 10,022(27.6) | 6086(60.7) | |||
| Kindergarten | Good | 1024(36.1) | 85(8.3) | 2.21 | 0.332 |
| Medium | 1196(42.3) | 80(6.7) | |||
| Poor | 610(21.6) | 43(7.0) | |||
| Primary school | Good | 4107(27.8) | 1261(30.7) | 61.78 | < 0.001 |
| Medium | 7313(49.6) | 2605(35.6) | |||
| Poor | 3337(22.6) | 1312(39.3) | |||
| Junior high school | Good | 3603(32.8) | 2504(69.5) | 1.98 | 0.372 |
| Medium | 4907(44.6) | 3346(68.2) | |||
| Poor | 2485(22.6) | 1723(69.3) | |||
| Senior high school | Good | 1365(17.5) | 1038(76.0) | 41.35 | < 0.001 |
| Medium | 2863(36.6) | 2295(80.2) | |||
| Poor | 3590(45.9) | 3008(83.8) |
Association of eye-use behavior with myopia
As shown in Table 3. Binary logistic regression model analysis results showed that medium and poor eye-use behavior was positively correlated with myopia, the OR values (95% CI) were 1.12 (1.06 ~ 1.17), and 1.65 (1.56 ~ 1.74), respectively. According to the study phase and further stratified analysis, in primary school students, the medium and poor eye-use behavior was positively correlated with myopia, the OR values (95% CI) were 1.25 (1.15 ~ 1.36), and 1.46 (1.33 ~ 1.61), respectively. In senior high school students, the medium and poor eye-use behavior was positively correlated with myopia, the OR values (95% CI) were 1.27 (1.09 ~ 1.49), and 1.63 (1.40 ~ 1.90), respectively. However, in kindergarten and junior high school students, there was no statistically significant difference (P > 0.05).
Table 3.
Eye-use behavior and myopia: results of binary logistic regression analysis
| Study phase | Eye-use behavior | Myopia | |
|---|---|---|---|
| OR value (95%CI) | P value | ||
| Overall | Good | 1.00 | |
| Medium | 1.12(1.06 ~ 1.17) | < 0.001 | |
| Poor | 1.65(1.56 ~ 1.74) | < 0.001 | |
| Kindergarten | Good | 1.00 | |
| Medium | 0.79(0.58 ~ 1.09) | 0.150 | |
| Poor | 0.84(0.57 ~ 1.23) | 0.363 | |
| Primary school | Good | 1.00 | |
| Medium | 1.25(1.15 ~ 1.36) | < 0.001 | |
| Poor | 1.46(1.33 ~ 1.61) | < 0.001 | |
| Junior high school | Good | 1.00 | |
| Medium | 0.94(0.86 ~ 1.03) | 0.198 | |
| Poor | 0.99(0.89 ~ 1.11) | 0.893 | |
| Senior high school | Good | 1.00 | |
| Medium | 1.27(1.09 ~ 1.49) | 0.002 | |
| Poor | 1.63(1.40 ~ 1.90) | < 0.001 | |
As shown in Table 4. After controlling for age, gender, sibling, parental myopia, parental education level, self-reported learning burden, mode of travel to school, physical education lesson, city, usage distance of mobile phone / iPad / game console, reading and writing distance, weekdays outdoor time, and weekends outdoor time. Binary logistic regression model analysis results showed that poor eye-use behavior was positively correlated with myopia (OR = 1.10, 95% CI: 1.03 ~ 1.19). According to the study phase and further stratified analysis, in primary school students, the medium and poor eye-use behavior was positively correlated with myopia, the OR values (95% CI) were 1.16 (1.06 ~ 1.27), and 1.35 (1.20 ~ 1.50), respectively. In senior high school students, the poor eye-use behavior was positively correlated with myopia (OR = 1.28, 95% CI: 1.08 ~ 1.51). However, in kindergarten and junior high school students, there was no statistically significant difference (P > 0.05).
Table 4.
The associations between eye-use behavior and myopia by adjusted binary logistic regression analysis
| Study phase | Eye-use behavior | Myopia | |
|---|---|---|---|
| OR value (95%CI) | P value | ||
| Overall | Good | 1.00 | |
| Medium | 1.04(0.98 ~ 1.11) | 0.165 | |
| Poor | 1.10(1.03 ~ 1.19) | 0.006 | |
| Kindergarten | Good | 1.00 | |
| Medium | 0.79(0.56 ~ 1.10) | 0.162 | |
| Poor | 0.81(0.53 ~ 1.23) | 0.323 | |
| Primary school | Good | 1.00 | |
| Medium | 1.16(1.06 ~ 1.27) | 0.001 | |
| Poor | 1.35(1.20 ~ 1.50) | < 0.001 | |
| Junior high school | Good | 1.00 | |
| Medium | 0.99(0.90 ~ 1.10) | 0.871 | |
| Poor | 1.00(0.88 ~ 1.13) | 0.991 | |
| Senior high school | Good | 1.00 | |
| Medium | 1.12(0.95 ~ 1.31) | 0.178 | |
| Poor | 1.28(1.08 ~ 1.51) | 0.004 | |
Note: Model adjusted for age, gender, sibling, parental myopia, parental education level, learning burden, mode of travel to school, physical education lesson, city, usage distance of mobile phone / iPad / game console, reading and writing distance, weekdays outdoor time, and weekends outdoor time
Discussion
The main findings of the present study were as follows: (a) the prevalence of poor eye-use behavior and myopia of students were 27.6% and 53.0%, respectively; (b) after adjusting for covariates, the poor eye-use behavior was positively correlated with myopia; and (c) according to the study phase and further stratified analysis, in primary school and senior high school students, the poor eye-use behavior was positively correlated with myopia, but not in kindergarten and junior high school students. This study can provide valuable information for the prevention and control of myopia in children and adolescents from the perspective of epidemiology.
In this study, the prevalence of myopia among students was 53.0%. The prevalence of myopia among kindergarten, primary school students, junior high school students, and senior high school students was 7.3%, 35.1%, 68.9%, and 81.1%, respectively. It was at a lower level compared with other studies. For instance, in a survey in Ningbo, China, the prevalence of myopia among primary school students, junior high school students, and senior high school students was 61.49%, 81.43%, and 89.72%, respectively [32]. Similarly, a study of 34 644 students in Shenyang, China, found that the prevalence of myopia was 60.0%, with a prevalence of 42.0% for primary school students, 76.0% for junior high school students, and 88.0% for senior high school students [33]. Additionally, this study revealed that the prevalence of myopia increased with grade level, with the highest prevalence of 81.1% among senior high school students, which was related to the accumulation of myopia, but also to the increasing study tasks and more frequent use of eyes as the grade level increased.
At the same time, we found that poor eye-use behavior was positively correlated with myopia. In further analyses, we also found that poor eye-use behavior was positively correlated with myopia in primary school and senior high school students, but not in kindergarten and junior high school students. Similarly, a study of 4 798 senior high school students in Beijing, China, revealed that a higher prevalence of myopia was linked to shorter near-work distance, longer time spent near work, and lower frequency of active rest during studying [34]. Another study of 8 319 students from 26 primary schools in Shanghai, China, found that adequate instruction in reading and writing postures, outdoor activities during class recess or physical education class, and providing suitable desks and chairs might protect against pathological eye growth [35]. Furthermore, a study of 14 296 Chinese students aged 7 to 18 years found that increased risk of myopia in students due to excessive screen time, unhealthy lifestyles, and poor eyesight habits [36]. This is consistent with the findings of our study that poor eye use habits were associated with the development of myopia.
Our research has several limitations. First, self-report questionnaires were used to evaluate the eye-use behavior and learning burden of students. Thus, recall and reporting biases could not be avoided. Second, although it was well-established that cycloplegic refraction was better than non-cycloplegic autorefraction, our study did not use this method. This decision was primarily due to the substantial number of students involved and the constraints of available resources, making it challenging to conduct cycloplegic refraction. Third, we were not able to adjust for all possible covariates in our analysis and potential residual confounding could lead to bias in reported estimates. Fourth, some other factors affecting students’ visual state may not be taken into account, such as daylight exposure time. Fifth, due to kindergarten students’ limited ability to recognize the letter E, using a standard logarithmic visual acuity E chart for vision acuity screening may not reflect their true vision status. Sixth, due to the cross-sectional study design, this study does not allow to make assumptions about causal relationships. Seventh, time spent on near work is closely associated with myopia [12]. In the present study, the learning burden and some items in the EBESS scale both reflect students’ close-range eye use behavior. However, neither of these two measurement methods can accurately reflect how long students spend in near work. Lastly, the poor correlation between eye use behavior and myopia observed in kindergarten and junior high school students may be attributed to the role of myopic shift from early stages, which has not yet progressed to a detectable level of myopia [37]. However, this phenomenon was not found in our study. Despite the above limitations, the strengths of our study include the large sample of participants, which may make our findings convincing. In addition, we use the EBESS to measure eye-use behavior in students. The EBESS was a comprehensive scale that included outdoor activity time, electronic device use, sleep, social jet lag, reading and writing posture, visual environment, eye relaxation behavior, and other aspects. It is an effective tool to evaluate the eye-use behaviors of students.
Conclusion
This research was the first to present evidence that poor eye use behavior was correlated with myopia among Chinese students. Our results suggest that poor eye-use behavior may be a potential risk factor for myopia in students. Therefore, future studies should establish interventions to protect students from the effects of poor eye-use behavior. Schools should strengthen eye use behavior education for students. Parents need to keep a close watch on their child’s eye use behavior. If they find that the child exhibits poor eye use behavior, such as squinting, eye rubbing, etc., they should promptly correct and provide proper guidance.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We were very grateful to the staff and students on site and to all the project teams.
Author contributions
Designed the experiments: Fangbiao Tao, Xiaoyan Wu. Conducted the experiments: Tingting Li, Peng Ding, Shaojun Xu, Shuman Tao. Analyzed the data: Tingting Li. Contributed materials: Feng Yang, Xiaoling Liu, Caiyun Cao. Wrote the essay: Tingting Li.
Funding
This work was supported by the Major Science and Technology Project of Anhui Provincial Science and Technology Innovation Platform (202305a12020015), the National Key Research and Development Program of China (2021YFC2702100, 2021YFC2702105), and the National Natural Science Foundation of China (82273653).
Data availability
The dataset for this study is kept in the School of Public Health, at Anhui Medical University, China and may be available upon request (Fangbiao Tao, taofangbiao@126.com).
Declarations
Ethics approval and consent to participate
The Ethics Committee of Anhui Medical University approved this study (NO: 20210735). All participants received written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Flitcroft DI, He M, Jonas JB, et al. IMI - Defining and classifying myopia: A proposed set of standards for clinical and epidemiologic studies. Invest Ophthalmol Vis Sci. 2019;60(3):M20–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and Temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036–42. [DOI] [PubMed] [Google Scholar]
- 3.Zhang J, Li Z, Ren J, et al. Prevalence of myopia: A large-scale population-based study among children and adolescents in Weifang, China. Front Public Health. 2022;10:924566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Disease Control and Prevention Administration. National Disease Control and Prevention Administration actively promotes the prevention and control of myopia in children and adolescents. (2024-3-13) [2024-3-29]. https://www.ndcpa.gov.cn/jbkzzx/c100008/common/content/content_1764617954927783936.html
- 5.Sankaridurg P, Bakaraju RC, Naduvilath T, et al. Myopia control with novel central and peripheral plus contact lenses and extended depth of focus contact lenses: 2 year results from a randomised clinical trial. Ophthalmic Physiol Opt. 2019;39(4):294–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tideman JW, Snabel MC, Tedja MS, et al. Association of axial length with risk of uncorrectable visual impairment for Europeans with myopia. JAMA Ophthalmol. 2016;134(12):1355–63. [DOI] [PubMed] [Google Scholar]
- 7.Jonas JB, Weber P, Nagaoka N, et al. Glaucoma in high myopia and parapapillary delta zone. PLoS ONE. 2017;12(4):e0175120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dang J, Cai S, Zhong P, et al. Associations of school physical activity environment with comorbid obesity and myopia in children and adolescents: findings from a Chinese National follow-up study. Scand J Med Sci Sports. 2024;34(1):e14562. [DOI] [PubMed] [Google Scholar]
- 9.Zhu Z, Chen Y, Tan Z et al. Interventions recommended for myopia prevention and control among children and adolescents in China: a systematic review. Br J Ophthalmol. 2021;bjophthalmol-2021-319306. [DOI] [PubMed]
- 10.Xiao J, Liu M, Huang Q, et al. Analysis and modeling of myopia-related factors based on questionnaire survey. Comput Biol Med. 2022;150:106162. [DOI] [PubMed] [Google Scholar]
- 11.Lim LT, Gong Y, Ah-Kee EY, et al. Impact of parental history of myopia on the development of myopia in Mainland China school-aged children. Ophthalmol Eye Dis. 2014;6:31–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dutheil F, Oueslati T, Delamarre L, et al. Myopia and near work: a systematic review and meta-analysis. Int J Environ Res Public Health. 2023;20(1):875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tang SM, Kam KW, French AN, et al. Independent influence of parental myopia on childhood myopia in a dose-related manner in 2 055 trios: the Hong Kong children eye study. Am J Ophthalmol. 2020;218:199–207. [DOI] [PubMed] [Google Scholar]
- 14.He M, Xiang F, Zeng Y, et al. Effect of time spent outdoors at school on the development of myopia among children in China: a randomized clinical trial. JAMA. 2015;314(11):1142–8. [DOI] [PubMed] [Google Scholar]
- 15.Sherwin JC, Reacher MH, Keogh RH, et al. The association between time spent outdoors and myopia in children and adolescents: a systematic review and meta-analysis. Ophthalmology. 2012;119(10):2141–51. [DOI] [PubMed] [Google Scholar]
- 16.Xiong S, Sankaridurg P, Naduvilath T, et al. Time spent in outdoor activities in relation to myopia prevention and control: a meta-analysis and systematic review. Acta Ophthalmol. 2017;95(6):551–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cao K, Wan Y, Yusufu M, et al. Significance of outdoor time for myopia prevention: A systematic review and Meta-Analysis based on randomized controlled trials. Ophthalmic Res. 2020;63(2):97–105. [DOI] [PubMed] [Google Scholar]
- 18.Liao S, Li X, Bai N, et al. An empirical study on the effect of outdoor illumination and exercise intervention on children’s vision. Front Public Health. 2023;11:1270826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Norton TT. What do animal studies tell Us about the mechanism of Myopia-Protection by light?? Optom Vis Sci. 2016;93(9):1049–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li M, Tan CS, Xu L, et al. Sleep patterns and myopia among school-aged children in Singapore. Front Public Health. 2022;10:828298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim H, Seo JS, Yoo WS, et al. Factors associated with myopia in Korean children: Korea National health and nutrition examination survey 2016–2017 (KNHANES VII). BMC Ophthalmol. 2020;20(1):31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xiang ZY, Zou HD. Recent epidemiology study data of myopia. J Ophthalmol. 2020;2020:4395278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dong XX, Xie JY, Li DL, et al. Association of sleep traits with myopia in children and adolescents: a meta-analysis and Mendelian randomization study. Prev Med. 2024;180:107893. [DOI] [PubMed] [Google Scholar]
- 24.Lau J, Koh WL, Ng JS et al. How can we better evaluate paediatric progression of myopia and associated risk factors? Lessons from the COVID-19 pandemic: a systematic review. Acta Ophthalmol. 2023. [DOI] [PubMed]
- 25.Yu M, Hu Y, Han M, et al. Global risk factor analysis of myopia onset in children: a systematic review and meta-analysis. PLoS ONE. 2023;18(9):e0291470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.National Disease Control and Prevention Administration. Technical guide for public health comprehensive intervention in the prevention and control of myopia in children and adolescents. (2023-8-30) [2024-3-29]. https://www.ndcpa.gov.cn/jbkzzx/c100012/common/content/content_1698993133687533568.html
- 27.Jin JX, Hua WJ, Jiang X, et al. Effect of outdoor activity on myopia onset and progression in school-aged children in Northeast China: the Sujiatun eye care study. BMC Ophthalmol. 2015;15:73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li JH, Zeng HX, Wei J, et al. Long-term exposure to PM2.5 and its constituents and visual impairment in schoolchildren: A population-based survey in Guangdong Province, China. Environ Int. 2025;195:109270. [DOI] [PubMed] [Google Scholar]
- 29.Standard no.GB/T 11533– 2011. National Standards Full Text Public System. 2011. https://openstd.samr.gov.cn/bzgk/gb/newGbInfo?hcno=A9F9E03A346211223DE34421A85CA1C8.
- 30.He X, Zhao R, Sankaridurg P, et al. Design and methodology of the Shanghai child and adolescent large-scale eye study (SCALE). Clin Exp Ophthalmol. 2018;46(4):329–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.National Health Commission of the PRC. Appropriate Technical Guidelines for Prevention and Control of Myopia in Children and Adolescents (Updated Edition) and interpretation. (2021-10-13) [2024-3-29]. http://www.nhc.gov.cn/jkj/s7934td/202110/0fc8a001d42345d9ac9b38842b295fe7.shtml
- 32.Jiang D, Shi B, Gao H, et al. Associations between reading and writing postures and myopia among school students in Ningbo, China. Front Public Health. 2022;10:713377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang D, Sun B, Wu M, et al. Prevalence and associated factors of myopia among school students in Shenyang, China: a cross-sectional study. Front Public Health. 2023;11:1239158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wu LJ, You QS, Duan JL, et al. Prevalence and associated factors of myopia in high-school students in Beijing. PLoS ONE. 2015;10(3):e0120764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shi JJ, Wang YJ, Lyu PP, et al. Effects of school myopia management measures on myopia onset and progression among Chinese primary school students. BMC Public Health. 2023;23(1):1819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dong Y, Jan C, Chen L, et al. The cumulative effect of multilevel factors on myopia prevalence, incidence, and progression among children and adolescents in China during the COVID-19 pandemic. Transl Vis Sci Technol. 2022;11(12):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chen Z, Gu D, Wang B, et al. Significant myopic shift over time: Sixteen-year trends in overall refraction and age of myopia onset among Chinese children, with a focus on ages 4–6 years. J Glob Health. 2023;13:04144. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The dataset for this study is kept in the School of Public Health, at Anhui Medical University, China and may be available upon request (Fangbiao Tao, taofangbiao@126.com).