Abstract
Background
Most of the landmark cohorts and reviews that assessed the psychosocial outcomes among adolescent and young adult (AYA) cancer survivors have focused on Western populations. This scoping review summarizes the existing evidence on psychosocial challenges experienced by AYAs with cancer in Asia, specifically work- and school-related outcomes, financial distress, social relationships, and concerns with infertility.
Methods
A literature search was conducted on Embase and Medline for studies that (1) were published in English between 2000 and 2023, (2) recruited AYAs diagnosed with cancer between the age of 15 and 39 years, (3) were conducted in Asia, and (4) assessed outcomes related to (i) work or/and school performance, (ii) financial distress, (iii) romantic relationship or/and relationship with family and peers, and (iii) concerns with childbirth and infertility. Titles, abstracts, and full texts were screened independently by two reviewers to identify eligible studies. Information of included studies was summarized and aggregated using structured forms based on Joanna Briggs Institute’s (JBI) data extraction form. Both quantitative and qualitative studies were assessed for methodological validity using JBI Critical Appraisal Checklist.
Results
Thirteen studies, enrolling a total of 1,108 survivors, reported outcomes related to work or school performance (n = 8), relationships with families and peers (n = 5), and desires or concerns regarding childbirth or infertility (n = 5). Although no differences in resignation rates between AYA survivors of cancer and non-cancer controls or other age groups were reported in three studies, 21%-40% of AYAs expressed concerns regarding employment or impaired work outcomes after cancer diagnosis. Studies identified health concerns and socioenvironmental factors that affected family functioning and romantic relationships. The uncertainty and the lack of information on fertility preservation were consistently reported by participants.
Conclusions
Our review demonstrated differences in concerns and disparities in social support and interventions available to AYA cancer survivors among various Asian countries/regions. We found Asian studies have focused more on family relationships than peers, likely due to sociocultural nuances when compared with Western societies. Given the variability in economic development and healthcare infrastructure across Asia, region-specific healthcare policies and services are required for AYA survivors.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12885-025-14169-x.
Keywords: Adolescents and young adults, Cancer, Survivorship, Work, Relationships, Infertility
Introduction
Adolescent and young adult (AYA) patients with cancer typically comprise individuals diagnosed with cancer between the ages of 15 and 39 years [1]. Over the past decades, advancements in cancer treatment have led to a decrease in overall cancer mortality rates among AYAs [1, 2]. Given that the transition period during adolescence and young adulthood is characterized by significant developmental changes toward independence [3–6], changes in the functional outcomes of AYA survivors during their cancer trajectory are complex, including physical, mental, and psychosocial aspects [6–9]. Older adolescents face challenges during puberty and social identity development in school, whereas young adults focus on pursuing higher education, career goals, and independent social relationships [6].
In this review, we adopted the National Cancer Institute definition of “survivorship”, which focuses on the health and well-being of a person with cancer from the time of diagnosis until the end of life [10]. To enhance awareness and support for AYA survivors of cancer, the National Comprehensive Cancer Network (NCCN) has highlighted the unique psychosocial needs of this population, particularly employment and occupational opportunities, insurance/financial problems, fertility, childcare, and psychosocial support [11]. Psychosocial functioning for AYA cancer survivors involves their ability to establish relationships and fulfil their roles in various contexts, such as family, peer groups, educational or occupational settings, and the broader community. AYA cancer survivors encounter greater challenges in social functioning than the general AYA population [12], and are more likely to report psychosocial issues than older patients with cancer [13–15]. Treatment-related side effects, physical limitations, and disruptions in daily routines can also impede AYA cancer survivors’ ability to participate in social activities and maintain social connections [7]. In addition, problems related to infertility and family planning may lead to altered family dynamics in young adult survivors [9, 16–18].
Many reviews and landmark cohort studies have examined psychosocial outcomes among AYA cancer survivors [19–22]. However, most of these studies have focused on Western populations, such as US [23, 24], Italy [25], UK [26], and Canada [27]. Data on the psychosocial outcomes of AYA cancer cohorts in Asian are limited, mostly focusing on Asian women with breast cancer or older adults with cancer. The literature has suggested that psychosocial functioning outcomes may differ between Western and Asian cancer populations [28]. In addition, Asian patients diagnosed with cancer reported more unmet needs for psychosocial care and had a significantly lower quality of life than Australian [29]. These studies have indicated that racial and cultural differences may impact psychosocial outcomes of AYA cancer survivors.
This scoping review aimed to explore the existing literature on psychosocial challenges among AYA cancer survivors in Asia, specifically focusing on school or occupational performance, financial distress, romantic and family relationships, and issues related to childbirth and infertility. The findings of this review may help identify cultural nuances and unmet social needs in Asian AYA survivors of cancer, and guide the development of future psychosocial research and rehabilitation programs among the Asian population.
Methods
Overall approach
The protocol for this review was registered on PROSPERO in September 2023 (CRD42023459051) originally as a systematic review. However, the preliminary search showed high heterogeneity in the assessment and scope of psychosocial outcomes. The investigators decided to conduct a scoping review instead, based on the understanding that scoping reviews are better applicable to stressing the research gaps and summarizing studies with various methodologies. We followed the methodological framework recommended by Arksey and O’Malley [30] to conduct this scoping review, including: (1) identifying the research question; (2) identifying relevant studies; (3) study selection; (4) charting the data; (5) collating, summarizing and reporting the results. The Preferred Reporting Items for Systematic Review and Meta-Analysis extensions for Scoping Review (PRISMA-ScR) checklist was used to guide the review process [31].
Literature search
A literature search was performed through two major English databases (Ovid Medline and Ovid Embase) in September 2023 to identify studies published between 2000 and 2023. The search strategy was developed based on the combination of Medical Subject Headings (MeSH) terms and keywords. A hand search was conducted by screening the reference lists of the included studies and key journals to identify publications that were potentially relevant to the research question. The specific search terms and full search strategy are presented in Supplemental Table 1.
Eligibility criteria
While there is no consensus on the age range for AYAs across different countries, AYAs with cancer are generally defined as individuals diagnosed with cancer between the ages of 15 and 39 years [32, 33]. To include AYA cancer survivors who were diagnosed at the upper age limit (i.e., 39 years) and were recruited or evaluated for psychosocial outcomes after the completion of cancer treatment or during the cancer survivorship stage, the maximum age at recruitment/assessment for survivors included in this review was extended to 42 years. This extension of upper age limit allows us to capture the characteristics of the AYA population who were diagnosed within the specified age range and are still within the AYA category at the time of the study. Thus, this review selected studies that (1) included AYA survivors diagnosed with cancer between the age of 15 to 39 years old, who were no more than 42 years old at the time of recruitment/assessment; (2) assessed either: (i) school or work performance, (ii) financial distress, (iii) concerns related to childbirth or infertility, or (iv) intimate/romantic relationships, or relationships with children, siblings, families, and friends at any time during cancer survivorship; (3) were written in English; (4) were quantitative studies of any design (e.g., cross-sectional, longitudinal, cohort, case–control, and randomized controlled trials) or qualitative interviews or assessments; and (5) were conducted in the United Nations geoscheme for Asia.
Studies were excluded if they (1) focused on treatment effectiveness, pathophysiological analysis, or genetic polymorphisms as main outcomes; (2) reported only the proportion of related outcomes (e.g., educational attainment, marital status, or employment) as demographic characteristics and not as the main outcomes of interest; (3) were case reports, reviews or meta-analyses, comments, conference abstracts, study designs, or protocols; or (4) lacked full-text availability.
Study selection, data extraction and data synthesis
Retrieved articles were imported into EndNote for management. Duplicates were removed both automatically and manually. Two reviewers (YW and WD) independently screened the titles and abstracts using Covidence (www.covidence.org). Furthermore, the two reviewers reviewed full texts in parallel to identify eligible articles based on the aforementioned inclusion and exclusion criteria. Disagreements were resolved through discussion with a third reviewer (YTC) until a consensus was reached.
Data extraction was independently conducted and reviewed by two investigators (YW and PX) using standardized, pilot-tested data extraction forms designed for this study based on the Joanna Briggs Institute’s (JBI) data extraction form [34]. Extracted data included (1) information on the article (title, author, year of publication, country or region, and study design); (2) characteristics of the study population (sample size, age at diagnosis, age at study, sex, cancer diagnosis, and treatment); and (3) results (specific outcome, instruments used, follow-up duration, risk factors, and control groups).
The outcomes of this review were determined a priori based on the NCCN guidelines for Adolescent and Young Adult Oncology (version 2) [11], which emphasized individual functioning (education, career, and employment), relationships (social, peer and family relationships), socioeconomic issues and infertility concerns as key psychosocial domains assessed in the AYA cancer population. Outcomes concluded from extracted data were summarized and aggregated by the corresponding domains, including (1) work or school performance, or socioeconomic outcomes, (2) romantic relationship or relationship with family and peers, and (3) concerns with childbirth and infertility.
Quality assessment
Although quality assessment of the included studies is generally not required for a scoping review, assessment of the methodological limitations was evaluated to establish the quality of existing evidence and address variation in the study approaches. Quantitative and qualitative studies were assessed for methodological validity using JBI Critical Appraisal Checklist for Analytical Cross-Sectional Studies and JBI Critical Appraisal Checklist for Qualitative Research, respectively [35, 36]. Each article was independently appraised by two investigators (YW and PX) and any discrepancies in the ratings were resolved by discussion. In accordance with the literature [37, 38], a high methodological quality (i.e. low risk of bias) was determined if the “yes” score (suggesting that the study had addressed the possibility of bias in its design, conduct, and analysis) was 70% or higher. Studies with a “yes” score between 50 and 69% were regarded as moderate methodological quality, while those with a score of 49% or lower were rated as low methodological quality.
Results
Study selection and characteristics
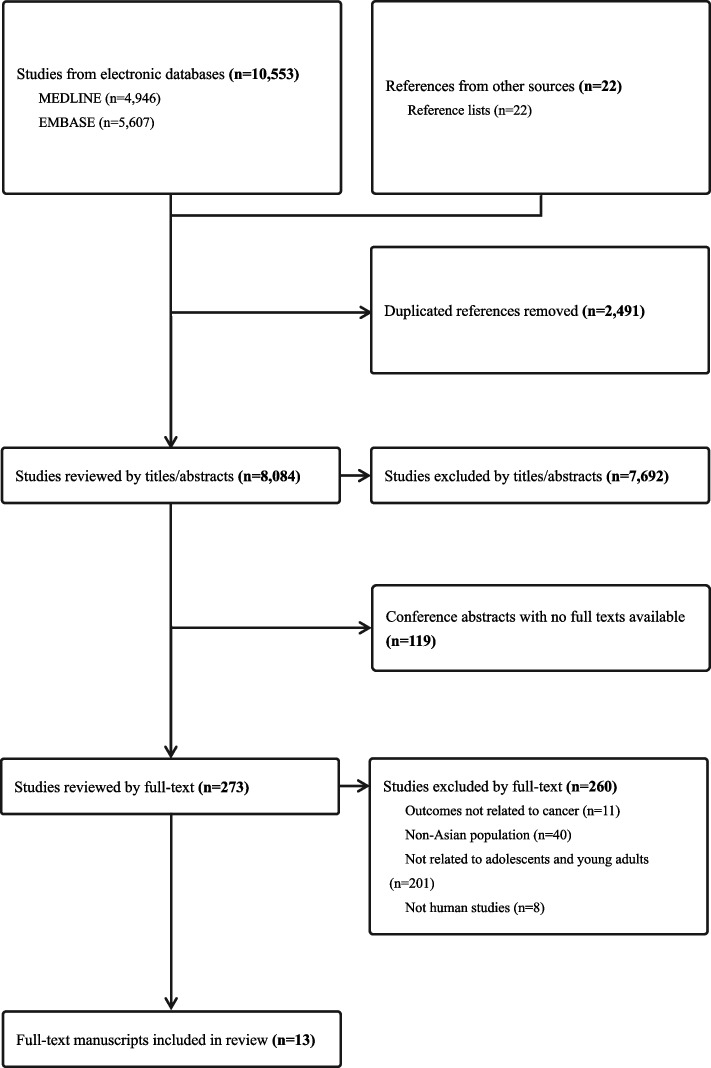
The flowchart of study selection and results is presented in Fig. 1. A total of 10,575 articles were extracted from the databases. Among them, there were 10,553 articles from MEDLINE (n = 4,946) and EMBASE (n = 5,607), and 22 were from other sources. After removing duplicates (n = 2,491), ineligible titles or abstracts (n = 7,692), and conference abstracts (n = 119), 273 full-text articles were assessed for eligibility. Finally, 13 studies that met the criteria were included for the scoping review.
Fig. 1.
PRISMA flow chart of literature search
Among the 13 studies (Table 1), nine were quantitative studies [39–47] and four were qualitative studies [48–51]. All the qualitative studies were considered to be of high methodological quality (Supplemental Table 2). The methodology of the quantitative studies ranged widely from low (n = 2) [40, 41], moderate (n = 2) [42, 44], to high (n = 5) [39, 43, 45–47] quality. Most studies (76.9%) were conducted in developed countries, including Japan (n = 6) [40–43, 45, 50] and Singapore (n = 4) [39, 46, 48, 49], whereas two studies were performed in China [47, 51] and one study was from Malaysia [44]. The total number of survivors enrolled in the 13 studies was 1,108. The majority of the studies enrolled less than 60 participants. The three studies with the largest study population were from Malaysia (n = 400) [44], Japan (n = 206) [45] and China (n = 150) [47]. In most studies, the proportion of the female survivors was higher than that of the male survivors, with three studies involving only female participants [42, 47, 51].
Table 1.
Characteristics of included studies
| Author | Year | Country | Sample size | Gender (% female) | Study design | Cancer diagnosis | Outcomes | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Work or school performance | Financial distress | Family relationships | Romantic relationships | Childbirth desires/concerns | |||||||
| Chan, et al. [39] | 2018 | Singapore | 65 | 44.6 | Prospective longitudinal cohort | Mixed | √ | √ | √ | √ | √ |
| Fujii, et al. [40] | 2019 | Japan | 28 | NR | Cross-sectional | Sarcoma | √ | ||||
| Furui, et al. [41] | 2019 | Japan | 36 | 88.9 | Cross-sectional | Mixed | √ | ||||
| Furui, et al. [42] | 2019 | Japan | 52 | 100.0 | Cross-sectional | Mixed | √ | ||||
| Endo, et al. [43] | 2020 | Japan | 60 | 85.0 | Cross-sectional | Mixed | √ | ||||
| Hamzah, et al. [44] | 2020 | Malaysia | 400 | 56.8 | Cross-sectional | Mixed | √ | ||||
| Ke, et al. [48] | 2020 | Singapore | 23 | 60.9 | Qualitative interview | Mixed | √ | √ | |||
| Tan, et al. [49] | 2020 | Singapore | 23 | 60.9 | Qualitative interview | Mixed | √ | √ | |||
| Okamura, et al. [45] | 2021 | Japan | 206 | 87.4 | Cross-sectional | Mixed | √ | √ | |||
| Yoshida, et al. [50] | 2022 | Japan | 24 | 66.7 | Qualitative interview | Mixed | √ | ||||
| Qiu, et al. [51] | 2023 | China | 12 | 100.0 | Qualitative interview | Breast cancer | √ | √ | |||
| Tan, et al. [46] | 2023 | Singapore | 29 | 48.3 | Cross-sectional | Mixed | √ | ||||
| Wu, et al. [47] | 2023 | China | 150 | 100.0 | Cross-sectional | Colorectal cancer | √ | ||||
NR Not reported
Studies are arranged in chronological order
Work or school performance
Eight studies [39, 40, 43–46, 48, 49] examined work or school performance and financial burdens (Table 2), including one prospective longitudinal study [39] and two qualitative studies [48, 49]. Two studies reported resignations from work [43, 46], but no significant differences in the resignation rate were found between AYA survivors of cancer and other age groups or healthy populations. A population-based cross-sectional survey conducted in Japan [43] indicated that 20% of participants (n = 750) resigned after the diagnosis of cancer; however, this proportion was not significantly higher than those in other age groups (11.4%, 12.1%, and 11.6% for the age groups of 41–49, 51–59, and > 60 years, P = 0.317). Another study conducted by Tan et al. in Singapore [46] revealed no significant difference in the proportion of successful employment between AYA survivors (n = 29) who were actively seeking jobs and their sibling controls (n = 23). After adjusting for age, sex, education level, and siblings’ correlation, the diagnosis of cancer was not significantly associated with decreased employment opportunities among AYA survivors compared with their healthy siblings (OR = 0.60, 95% CI: 0.07–5.07, P = 0.64) [46].
Table 2.
Studies on work or school performance and financial distress
| Author, year | Country | Study design | N | Control group (n) | Age at dx range in years | Age at study mean ± SD (range) in years | Follow up time | Treatment (%) | Outcomes | Assessments | Main results |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Quantitative studies | |||||||||||
| Chan, et al. [39], 2018 | Singapore | Prospective, longitudinal cohort | 65 | NA | 15–39 | 27.8 ± 6.7 |
‧ At diagnosis (T1) ‧ 1 month (T2) ‧ 6 months (T3) |
NR |
‧ Financial and insurance issues ‧ Work and school stress |
The NCCN Distress Thermometer |
‧ Distress about financial and insurance problems (46.2% at T1, 23.1% at T2, 23.1% at T3) ‧ Work and school issues (38.5% at T1, 18.5% at T2, 21.6% at T3) |
| Fujii, et al. [40], 2019 | Japan | Cross-sectional | 28 | Childhood cancer survivors (22) | 15–29 | NR | Overall mean follow-up: 6 years |
‧ Surgery (NR) ‧ Chemotherapy (NR) ‧ Radiation (NR) |
Socio-occupational outcomes | Simplified socio-occupational disability scoring system using the PCQL- 32 and MMQL-YF |
‧ Drop-out or delays in high school or college (50%, overall cohort) ‧ Unemployed or difficulties in searching for a job (56%, overall cohort) ‧ No significant difference in socio-occupational problems between AYA and childhood cancer survivors |
| Endo, et al. [43], 2020 | Japan | Cross-sectional | 60 |
‧ Age 40–49 years (167) ‧ Age 50–59 years (298) ‧ Age > = 60 years (225) |
20–39 | NR | NA | NR | Resignation after cancer diagnosis | Online structured questionnaire | ‧ Resignation rate (20%) in AYA survivors; not significantly different from other age groups |
| Hamzah, et al. [44], 2020 | Malaysia | Cross-sectional | 400 | NA | NR | 29.1 ± 7.2 (18–40) | NA | NR |
‧ Quality of working life ‧ Career engagement |
‧ QWLQ-CS ‧ Career engagement scale |
‧ Career engagement associated with quality of work life ‧ Effect of cancer and treatment mediated the association between quality of work life and career engagement |
| Okamura, et al. [45], 2021 | Japan | Cross-sectional | 206 | NA | NR (< 39) | 33.7 ± 4.3 (16–39) | NA | Chemotherapy (43.7) | ‧ Change in work and school |
‧ SCNS-SF34 ‧ MSPSS |
‧ Decreased work/study hours (9.7%), absence from work/school (24.3%), left work/school (28.1%), changed jobs/schools (10.7%), dismissed from work (1.0%) ‧ Decreased income status (41.7%), increased income status (8.3%) ‧ Change in work/school after diagnosis associated with total supportive needs, physical/daily living needs, and psychological needs |
| Tan, et al. [46], 2023 | Singapore | Cross-sectional | 29 | Healthy siblings (23) | 15–39 | 26.6 ± 5.1 | NA |
‧ Chemotherapy (86.2) ‧ Surgery (48.3) ‧ Radiation (27.6) Immunotherapy (3.4) |
‧ Employment status ‧ Work changes ‧ Absenteeism and presenteeism at work |
‧ Structured questionnaire |
‧ Fully employed (78.9%) ‧ Work reallocation (6.7%) ‧ Absenteeism within past 3 months (73.3%) ‧ Decreased work ability (40.1%) ‧ Median productivity loss due to absenteeism in the past 3 months: USD 110 |
| Qualitative studies | |||||||||||
| Ke, et al. [48], 2020 | Singapore | Qualitative interview | 23 | NA | 16–39 | 25 (18–39) | NA | NR | Employment support | Focus group discussions |
‧ Deemed cancer history as “disadvantageous” in job search process ‧ Highlighted the need for to ensure fair hiring practices for cancer survivors, and to assist survivors in their job search |
| Tan, et al. [49], 2020 | Singapore | Qualitative interview | 23 | NA | 16–39 | NA |
‧ Chemotherapy (91.3) ‧ Radiation (30.4) ‧ Surgery (56.5) |
‧ Problems with returning to work ‧ Financial issues |
Focus group discussions |
‧ Majority of AYA survivors expressed eagerness to return to work ‧ Highlighted challenges due to cancer complications, work restrictions, and inadequate insurance coverage |
|
Dx Diagnosis, IQR Interquartile range, MMQL-YF Minneapolis-Manchester Quality of Life-Youth Form, MSPSS Multidimensional Scale of Perceived Social Support, NA Not applicable, NCCN National Comprehensive Cancer Network, NR Not reported, PCQL- 32 Pediatric Cancer Quality of Life Inventory- 32, QWLQ-CS Quality of Working Life Questionnaire for Cancer Survivors, SCNS-SF34 The short-form Supportive Care Needs Survey questionnaire, SD Standard deviation
Impaired outcomes at work due to the cancer experience were noted among Asian AYA survivors [40, 44–46]. Hamzah et al. [44] reported the mediating role of cancer and related treatment on the association between career engagement and quality of work among AYA cancer survivors in Malaysia (n = 400). Tan et al. [46] found that in Singapore, more than half of the employed survivors (n = 29) experienced work impairments, including reallocation of work (6.7%), absenteeism (26.7%) and decreased ability due to the lingering effects of cancer (40.0%); half of the unemployed survivors attributed their unemployment to cancer and its treatment [46]. Japanese AYA survivors with sarcoma (n = 28) reported poor socio-occupational quality of life scores that were comparable with those of childhood cancer survivors [40]. Furthermore, Japanese survivors who experienced changes in work or school performance after the cancer diagnosis were more likely to report unmet physical and psychological needs than those who did not experience such changes [45].
Financial distress
A prospective longitudinal study conducted in Singapore [39] reported insurance or financial burdens experienced by AYA survivors (n = 65) at the time of diagnosis (46.2%) and at the 6-month follow-up (23.1%). The decrease in concerns related to insurance or finances over time was not significant (P = 1.000). While some of the survivors were concerned about disclosing their medical history and not being able to meet work expectations, the majority of AYA survivors (n = 23) from a qualitative interview in Singapore [49] expressed eagerness to return to work after cancer treatment due to financial needs. Despite the challenges, several survivors used their cancer experience to enhance job opportunities, demonstrating resilience and adaptability in the face of adversities [49]. Moreover, through qualitative studies, Ke et al. and Tan et al. emphasized the need for employment services and insurance coverage among Singaporean AYA cancer survivors [48, 49].
Romantic relationship or relationship with families and peers
Five studies [39, 45, 48, 50, 51] reported outcomes related to relationships with peers and families, particularly focusing on partners and children (Table 3). A prospective study performed in Singapore [39] did not identify any significant changes in family-related outcomes at diagnosis and 1- and 6-month follow-ups (n = 65). These outcomes included issues related to childcare (9.2% vs 7.7% vs 4.6%, P = 0.067), family health (26.2% vs 10.8% vs 14.0%, P = 0.078), partner relationships (9.2% vs 7.7% vs 1.5%, P = 0.174), and interaction with children (9.2% vs 3.1% vs 1.5%, P = 0.097). However, a descriptive trend towards a decrease in self-reported problems over time was noted. Okamura et al. [45] conducted a population-based cross-sectional study in Japan (n = 206) and found that 35.4% of the participants were concerned regarding changes in sexual feelings.
Table 3.
Studies on relationships with families, partners and peers
| Author, year | Country | Study design | N | Control group (n) | Age at dx range in years | Age at study mean ± SD (range) in years | Follow up time | Treatment (%) | Outcomes | Assessments | Main results |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Quantitative studies | |||||||||||
| Chan, et al. [39], 2018 | Singapore | Prospective, longitudinal cohort | 65 | NA | 15–39 | 27.8 ± 6.7 |
‧ At diagnosis (T1) ‧ 1 month (T2) ‧ 6 months (T3) |
NR |
‧ Problems with childcare ‧ Dealing with partner ‧ Dealing with children |
The NCCN Distress Thermometer |
‧ Problems with childcare (9.2% at T1, 7.7% at T2, 4.6% at T3) ‧ Dealing with partner (9.2% at T1, 7.7% at T2, 1.5% at T3) ‧ Dealing with children (9.2% at T1, 3.1% at T2, 1.5% at T3) ‧ Concerns about family health (26.2% at T1, 10.8% at T2, 14.0% at T3) |
| Okamura, et al. [45], 2021 | Japan | Cross-sectional | 206 | NA | NR (< 39) | 33.7 ± 4.3 (16–39) | ‧ NA | Chemotherapy (43.7) | ‧ Sexuality needs |
‧ SCNS-SF34 MSPSS |
‧ Expressed changes in sexual feelings (35.4%) |
| Qualitative studies | |||||||||||
| Ke, et al. [48], 2020 | Singapore | Qualitative interview | 23 | NA | 16–39 | 25 (18–39) | NA | NR | Family support | Focus group discussions |
‧ Multiple roles of AYAs in relation to their family members ‧ Most AYA patients had children as dependents or parents as caregivers |
| Yoshida, et al. [50], 2022 | Japan | Qualitative interview | 24 | NA | 15–38 | 35.5 (24–43) | NA | NR | Romantic relationship and marriage | Semi-structured interview |
Top three concerns about romantic relationship: ‧ Fertility and parenthood concerns (45.8%) ‧ Disclosure of cancer history to partners (37.5%) ‧ Recurrence, metastasis, and poor health (25.0%) |
| Qiu, et al. [51], 2023 | China | Qualitative interview | 12 | NA | 24–40 | 32.8 ± 4.1 | NA |
‧ Surgery (100) ‧ Chemotherapy (66.7) ‧ Radiation (58.3) ‧ Endocrine therapy (75.0) ‧ Targeted therapy (25.0) ‧ Neoadjuvant chemotherapy (25.0) |
Familial and peer support | Semi-structured interview |
‧ Highlighted the need for emotional support from family members and peers ‧ Expressed gratitude for the husband and maintenance of marriage bond |
Dx Diagnosis, IQR Interquartile range, MAPSS Multidimensional Scale of Perceived Social Support, NA Not applicable, NCCN National Comprehensive Cancer Network, NR Not reported, SCNS-SF34 The short-form Supportive Care Needs Survey questionnaire, SD Standard deviation
In a qualitative study [50], over one third of Japanese AYA survivors (n = 24) expressed difficulties in deciding when, how, and to what extent to disclose their cancer history to potential partners. They feared rejection due to their cancer history when establishing new romantic relationships [50]. Qiu et al. and Ke et al. highlighted the multiple roles related to family members and the lack of adequate emotional support from families [48, 51].
Desire for or concerns regarding childbirth
Five studies [39, 41, 42, 47, 51] reported desires or concerns regarding childbirth or infertility among AYA cancer survivors (Table 4). In a longitudinal study conducted in Singapore (n = 65) [39], patients reported concerns regarding having children at diagnosis (18.5%) and 1-month (4.6%) and 6-month follow-ups (4.6%), but the change in these concerns over time was not significant (P = 0.157). Furui et al. [41] found that 25% of male survivors and 75% of female survivors had reproduction and fertility concerns, which were significantly higher than the rates among AYAs without cancer (3.0%, P < 0.01) (n = 36). Another Japanese study (n = 52) [42] reported that a higher proportion of AYA survivors who underwent chemotherapy expressed reproductive concerns as one of their top five “current problems” compared with AYAs without cancer (51.9% vs 3.0%, P < 0.01). It also reported that 21.2% of AYA survivors who initially desired having children had to abandon this desire after the cancer diagnosis [42]. Studies conducted in the metropolitan areas of China also addressed AYA survivors’ fertility concerns. Qiu et al. [51] identified a strong desire for childbearing after cancer diagnosis among Chinese AYA breast cancer survivors in Guangzhou (n = 150), and emphasized the crucial role of support from families, partners, society, and healthcare professionals as well as self-perception in reproductive decision-making [51]. Wu et al. [47] found that among Chinese AYA survivors with colorectal cancer in Shanghai (n = 12), the children’s health and their personal health were the top concerns associated with childbirth, followed by those related to pregnancy, fertility potential, and the partner’s disclosure and acceptance. They also noted that more significant reproductive concerns were observed in AYA cancer survivors with fewer children or only female children, as well as lower education level, early-stage cancer diagnosis, and poorer family functioning [47].
Table 4.
Studies on childbirth concerns and desires
| Author, year | Country | Study design | N | Control group (n) | Age at dx range in years | Age at study mean ± SD (range) in years | Follow up time | Treatment (%) | Outcomes | Assessments | Main results |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Quantitative studies | |||||||||||
| Chan, et al. [39], 2018 | Singapore | Prospective, longitudinal cohort | 65 | NA | 15–39 | ± 6.7 |
‧ At diagnosis (T1) ‧ 1 month (T2) ‧ 6 months (T3) |
NR | Concerns about ability to have children | The NCCN Distress Thermometer | ‧ Concerns about having children (18.5% at T1, 4.6% at T2, 4.6% at T3) |
| Furui, et al. [41], 2019 | Japan | Cross-sectional | 36 |
‧ Healthy AYAs (200) ‧ Childhood cancer survivors (76) |
16–39 | 33.2 ± 4.8 | NA | Chemotherapy (69.4) | Concerns about reproductive function and infertility | Structured questionnaire | ‧ More concerns about reproductive function and infertility in AYA survivors (69.5%) than healthy controls (2.5%) |
| Furui, et al. [42], 2019 | Japan | Cross-sectional | 52 | Healthy AYAs (100) | 15–39 | 32.3 ± 6.6 | NA | Chemotherapy (100) |
‧ Concerns about infertility ‧ Desire for childbearing |
Structured questionnaire |
‧ More concerns about reproductive function in AYA survivors (51.9%) than healthy controls (3%) ‧ Diagnosed as “infertile” (19.2%) ‧ Menstrual cycle abnormalities as a late effect of therapy (36.5%) ‧ More AYA survivors reported “giving up trying for a child” (21.2%) than healthy controls (0%) |
| Wu, et al. [47], 2023 | China | Cross-sectional | 150 | NA | 18–40 | 34.7 ± 3.97 | NA |
‧ Surgery (100) Chemoradiotherapy (NR) |
‧ Reproductive concerns |
‧ RCAC Family Adaptation and Cohesion Evaluation Scale II |
‧ Mean score for overall reproductive concerns: 54.78 ± 8.97 (out of 90 points) ‧ High prevalence of concerns in child's health, personal health, becoming pregnant, fertility potential, partner disclosure and acceptance |
| Qualitative studies | |||||||||||
| Qiu, et al. [51], 2023 | China | Qualitative interview | 12 | NA | 24–40 | ± 4.1 | NA |
‧ Surgery (NR) ‧ Chemotherapy (NR) ‧ Radiation (NR) ‧ Endocrine therapy (NR) ‧ Targeted therapy (NR) ‧ Neoadjuvant chemotherapy (NR) |
‧ Desire for childbearing ‧ Emotional experience during pregnancy ‧ Reproductive decision-making |
Semi-structured interview |
Major themes: ‧ Awareness that the cancer may impair fertility status ‧ Worries about health of unborn child affected by treatment ‧ Expressed regret if the goal of childbearing is not achieved ‧ Expressed pressure from family elders to have children ‧ Trust in doctors and science influencing reproductive decisions |
Dx Diagnosis, IQR Interquartile range, NA Not applicable, NCCN National Comprehensive Cancer Network, NR Not reported, RCAC Reproductive Concerns After Cancer, SD Standard deviation
Discussion
Although numerous studies have examined psychological outcomes and unmet supportive care needs in AYA cancer survivors, few have specifically focused on the downstream occupational and family outcomes in this population in Asia. To the best of our knowledge, this study is the first to summarize concerns about work/school, financial distress, relationships and concerns with infertility among AYA cancer survivors in Asian countries. Almost all the studies we reviewed were conducted in high-income or upper-middle regions/countries with excellent cancer survival rates and survivorship care. We did not identify any similar studies conducted in other developing or low- or middle- income countries (LMICs) in Asia. Our review demonstrated differences in concerns and disparities in social support and interventions available to AYA cancer survivors among various Asian countries and regions. Given that occupational achievement and family values are highly regarded in many Asian societies [52], more studies examining psychosocial functioning outcomes in AYA cancer survivors should be conducted in the future.
Similar to the Western population [53, 54], we found that 20% to 56% of the Asian AYA cancer survivors in this review expressed concerns regarding employment after their diagnosis. However, three included studies did not identify significant differences in the resignation rate between AYA cancer survivors and their counterparts (i.e. cancer survivors of other age groups, healthy populations, or sibling controls). Collectively, our review showed that Asian AYA survivors experienced pressure and distress related to employment; however, many were eager to return to work and resume a daily life similar to that of their healthy peers [19, 40, 45]. This finding highlights the importance of employment services, which include various initiatives to ensure fair hiring practices for cancer survivors.
In Western countries, there are several comprehensive programs offering extensive and integrated support to help young cancer survivors return to work. For example, the European Network of Youth Cancer Survivors (EU-CAYAS-NET) advocates for policies to reduce financial discrimination and improve access to employment for young cancer survivors, and also provides rehabilitation programs that include vocational training and psychological support [55]. Such services in Asian countries are less widespread but are emerging, especially in high-income countries. According to a survey conducted by the Economist Intelligence Unit, Japan was the representative Asian country to offer rehabilitation programs and supports for cancer survivors to return to work [56]. The Japanese government urged employers to implement supportive measures for cancer survivors, including employer policy statements, sick leave programs, and flexible working arrangements to help them balance work and treatment [57]. In addition, the Singapore Cancer Society has introduced the Return-To-Work-Programme to help cancer survivors rejoin the workforce or retaining their employment [58]. It is well documented that many European countries have established an extensive network of support programs for young cancer survivors [59, 60]. Encouragingly, Asia is also making significant strides due to the higher prioritization of cancer survivorship in public health agendas, particularly in high-income countries [61, 62]. However, such policies may differ across regions or countries in terms of the level of support provided and region-specific implementation barriers [63], and are expected to be tailored against discrimination. For example, one study in Japan reported that female cancer patients are more likely to be marginalized in the workplace than male cancer patients [64]. Key recommendations for a work reintegration program should include (1) adapting to local resource availability with dedicated budgets and infrastructure for work integration for AYA cancer survivors, (2) fostering a multidisciplinary team (including clinicians, nurses, social workers, rehabilitation specialists, and occupational therapists) to support a successful transition back to work, and (3) creating a supportive environment and policies addressing potential discrimination (such as gender or chronic disability discrimination) at the workplace.
Financial distress has been less commonly investigated and reported in Asian AYA cancer survivors than in Western populations [19–21, 23]. This may be because in contrast to the United States, most Asian countries/regions such as China, Hong Kong, Japan, Singapore, and South Korea, have a well-established universal health coverage system to cover basic cancer treatment. However, the out-of-pocket expenditure for cancer treatment may vary across countries, and as reflected by the included studies of our review, many cancer patients in Asia may still face financial burdens related to cancer treatment. A study focusing on cancer survivorship in the Indo-Pacific region highlighted that the top unmet needs of cancer survivors in this region, especially in LMICs, included access to local health services and best medical care [65]. For instance, the Korean government has established a financial support program for children and adult patients from low-income households [66, 67]. However, specialized policies and programs targeting AYA cancer survivors are limited because this demographic often receives less priority than children and older adults with cancer [68]. This lack of dedicated attention and resources for AYAs highlights a gap in the healthcare system, emphasizing the need for dedicated healthcare policies to reduce the financial burden on this age group.
Previous reviews of studies from Western countries have reported challenges in various aspects of relationships with family, partners, and peers [3, 69, 70]. Our review suggested that Asian studies have focused more on family relationships than peers. These differences might be attributed to sociocultural and socioenvironmental factors prevalent in Asian societies [71–73]. For example, Asian cultures often emphasize strong family bonds and interdependence, whereas Western AYAs might rely on a broader network of friends, peers, and support groups outside their immediate family for social connections and support [74]. Furthermore, it is considered a cultural norm for young adults in some Asian societies to live with their parents and siblings before they get married [75]. For this reason, family-oriented relationships might play a more significant role in Asian than in Western cultures [74]. Understanding and addressing these culturally specific factors can guide the development of family-targeted interventions and supportive programs for AYA cancer survivors. For example, adopting a “full-cycle, whole family, whole-person rehabilitation” approach could be crucial in survivorship care for this population [76], enabling family members to provide supportive care to patients and assist them in self-care and home responsibilities. Overall, our findings highlight the importance of contextual awareness and the need to develop and implement culturally and socially sensitive interventions in collaboration with the family members of Asian AYA cancer survivors.
Fertility rates in general have declined steadily across most developed countries, with only about 1/5 of the global livebirths recorded in southeast Asia, east Asia and Oceania [77]. However, our review still highlighted childbearing and infertility as major concerns among Asian AYA cancer survivors. The uncertainty regarding fertility status and the lack of information on fertility preservation were consistently reported by participants in the included studies. The maturity and accessibility of onco-fertility programs also varied across regions/countries in Asia. For example, Japan has established regional networks for bridging oncology and reproductive medication, and introduced a national public subsidy for fertility preservation to reduce the financial burden on cancer patients [78]. The Fertility Preservation Support Service Programme led by the Hong Kong Cancer Fund, a nongovernmental organization, provides financial assistance for fertility preservation to AYAs with cancer [79]. Cultural and societal factors also affect family planning and parenting in both Asian and Western countries. In addition, changes in traditional values and economic pressure have led to lower fertility rates in many developed countries/regions of Asia. This has caused governments to review their policies and measures to encourage childbirth. For instance, China and Japan offer up to 14 weeks of maternity leave [80], which is still shorter than that in Western countries, such as Sweden, which provides extensive parental leave, with up to 480 days per child [81]. These differences may impact reproductive decisions and highlight the need for supportive policies tailored to the context of each region. Given that more knowledge on fertility preservation options can improve psychosocial functioning [82], it is hoped that increasing numbers of Asian countries will provide AYA cancer survivors with equal access to fertility services, including financial resources, insurance coverage, and availability of fertility specialists. National and regional facilities, along with community-level support, should provide information on advancements in fertility preservation techniques and options and offer guidance on family planning, reproductive health, and assisted reproductive technologies when necessary. The ongoing support and follow-up care addressing the unique concerns of AYA patients should be integral to these efforts.
This review has several limitations that should be addressed. First, this review was limited by the small sample sizes and the narrow geographical scope of the included studies. The majority of the included studies were conducted in high-income Asian countries and single centers, which may have led to misrepresentation of the diversity of psychosocial outcomes. The paucity of literature from Central, Southern and Western Asian countries may limit the generalizability of our findings to the broader Asian context. This finding suggests that AYA oncology is still an evolving specialty in many countries of Asia. Second, it was not feasible to conduct a pooled or meta-analysis as there was much variation in outcome assessments, such as family functioning and childbearing concerns. Third, this review only included studies published in English as it is methodologically difficult to conduct search and translation processes for literature written in the multiple languages represented in Asia. Despite the limitations, this scoping review captured a wide range of studies and perspectives, offering a more holistic understanding of psychosocial outcomes where the evidence is diverse and not yet well-defined. By providing a comprehensive overview of existing research, we can identify and highlight gaps that need further investigation. Future studies should consider multi-centered approaches, collaborating with international organizations and major AYA cohorts to evaluate best practices and research priorities from Asian countries. Through knowledge sharing and collaborative research, policies and capacities can be developed to improve the overall well-being of AYA cancer survivors in Asia.
Conclusions
This review provided an overview of the current research on psychosocial challenges among Asian AYA cancer survivors. We highlighted the unmet needs of the Asian AYA cancer population in areas such as family relationships, returning to work, and childbirth and discussed potential support mechanisms and interventions for Asian survivors. Given the variability in economic development and healthcare infrastructure across Asia, tailored policies, health insurance schemes, and healthcare services and support are required for AYA patients. Future studies should be conducted in Asian countries to comprehensively evaluate the psychosocial outcomes of Asian AYA cancer survivors. These studies could inform targeted care and interventions for long-term survivorship and boost the overall well-being of Asian AYA cancer survivors.
Supplementary Information
Acknowledgements
Not applicable.
Authors’ contributions
YTC and YW contributed to the study conception and design. Data collection and analysis were performed by YW, WD, PX and YTC. All authors contributed to the interpretation of the results. The first draft of manuscript was written by YW. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
The study is funded by the Hong Kong Research Grant Council, General Research Fund (Ref: 14604022).
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Miller KD, et al. Cancer statistics for adolescents and young adults, 2020. CA Cancer J Clin. 2020;70(6):443–59. [DOI] [PubMed] [Google Scholar]
- 2.Bleyer, A., et al. Global assessment of cancer incidence and survival in adolescents and young adults. Pediatr Blood Cancer. 2017; 64(9):e26497. [DOI] [PubMed]
- 3.Barnett M, et al. Psychosocial outcomes and interventions among cancer survivors diagnosed during adolescence and young adulthood (AYA): a systematic review. J Cancer Surviv. 2016;10(5):814–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Geue K, et al. Sexuality and romantic relationships in young adult cancer survivors: satisfaction and supportive care needs. Psychooncology. 2015;24(11):1368–76. [DOI] [PubMed] [Google Scholar]
- 5.Patterson P, et al. Emerging issues among adolescent and young adult cancer survivors. Semin Oncol Nurs. 2015;31(1):53–9. [DOI] [PubMed] [Google Scholar]
- 6.Turgeman I, West HJ. Adolescents and young adults with cancer. JAMA Oncol. 2023;9(3):440. [DOI] [PubMed] [Google Scholar]
- 7.Berkman AM, Mittal N, Roth ME. Adolescent and young adult cancers: unmet needs and closing the gaps. Curr Opin Pediatr. 2023;35(1):84–90. [DOI] [PubMed] [Google Scholar]
- 8.Roth, M.E., et al. Children's Oncology Group 2023 blueprint for research: Adolescent and young adult oncology. Pediatr Blood Cancer. 2023; 70 Suppl 6(Suppl 6):e30564. [DOI] [PMC free article] [PubMed]
- 9.Coccia PF, et al. Adolescent and young adult oncology, version 2.2018, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2018;16(1):66–97. [DOI] [PubMed] [Google Scholar]
- 10.National Cancer Institute. Office of Cancer Survivorship, Definitions, Cancer Survivor. [Cited 2024; Available from: https://cancercontrol.cancer.gov/ocs/definitions#terms.
- 11.National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology, Adolescent and Young Adult (AYA) Oncology. Version 1. 2023 [cited 2023 Sep]; Available from: https://www.nccn.org/professionals/physician_gls/pdf/aya.pdf. [DOI] [PubMed]
- 12.Smith AW, et al. Unmet support service needs and health-related quality of life among adolescents and young adults with cancer: The AYA HOPE Study. Front Oncol. 2013;3:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pulewka K, et al. Clinical, social, and psycho-oncological needs of adolescents and young adults (AYA) versus older patients following hematopoietic stem cell transplantation. J Cancer Res Clin Oncol. 2021;147(4):1239–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lang MJ, et al. Does age matter? Comparing post-treatment psychosocial outcomes in young adult and older adult cancer survivors with their cancer-free peers. Psychooncology. 2018;27(5):1404–11. [DOI] [PubMed] [Google Scholar]
- 15.Bleyer A. Increasing cancer in adolescents and young adults: cancer types and causation implications. J Adolesc Young Adult Oncol. 2023;12(3):285–96. [DOI] [PubMed] [Google Scholar]
- 16.Keegan TH, et al. Unmet adolescent and young adult cancer survivors information and service needs: a population-based cancer registry study. J Cancer Surviv. 2012;6(3):239–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jackson Levin N, et al. Banking on fertility preservation: financial concern for adolescent and young adult cancer patients considering oncofertility services. J Adolesc Young Adult Oncol. 2023;12(5):710–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Acquati C, et al. Sexual functioning among young adult cancer patients: A 2-year longitudinal study. Cancer. 2018;124(2):398–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Di Giuseppe G, et al. Financial toxicity among adolescent and young adult cancer survivors: a systematic review of educational attainment, employment, and income. Crit Rev Oncol Hematol. 2023;183: 103914. [DOI] [PubMed] [Google Scholar]
- 20.Ellis SJ, et al. Fertility concerns among child and adolescent cancer survivors and their parents: a qualitative analysis. J Psychosoc Oncol. 2016;34(5):347–62. [DOI] [PubMed] [Google Scholar]
- 21.Gorman JR, et al. How do you feel about fertility and parenthood? The voices of young female cancer survivors. J Cancer Surviv. 2012;6(2):200–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bradford NK, et al. Psychological, functional and social outcomes in adolescent and young adult cancer survivors over time: a systematic review of longitudinal studies. Psychooncology. 2022;31(9):1448–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Parsons HM, et al. Impact of cancer on work and education among adolescent and young adult cancer survivors. J Clin Oncol. 2012;30(19):2393–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smith AW, et al. Understanding care and outcomes in adolescents and young adult with cancer: a review of the AYA HOPE study. Pediatr Blood Cancer. 2019;66(1): e27486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Trama A, et al. Late mortality, subsequent malignant neoplasms and hospitalisations in long-term survivors of adolescent and young adult hematological cancers. Front Oncol. 2022;12: 823115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bright CJ, et al. Risk of cerebrovascular events in 178 962 five-year survivors of cancer diagnosed at 15 to 39 years of age: The TYACSS (Teenage and Young Adult Cancer Survivor Study). Circulation. 2017;135(13):1194–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Punnett A, et al. Treatment patterns and outcomes in adolescents and young adults with nodular lymphocyte-predominant Hodgkin lymphoma: an IMPACT cohort study. Br J Haematol. 2023;201(6):1081–7. [DOI] [PubMed] [Google Scholar]
- 28.Lu Q, et al. Differences in quality of life between American and Chinese breast cancer survivors. Support Care Cancer. 2016;24(9):3775–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Molassiotis A, et al. Mapping unmet supportive care needs, quality-of-life perceptions and current symptoms in cancer survivors across the Asia-Pacific region: results from the International STEP Study. Ann Oncol. 2017;28(10):2552–8. [DOI] [PubMed] [Google Scholar]
- 30.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Intern J Soc Res Methodol. 2005;8(1):19–32. [Google Scholar]
- 31.Tricco AC, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467–73. [DOI] [PubMed] [Google Scholar]
- 32.American Cancer Society. Special Section: Cancer in Adolescents and Young Adults. Cancer Facts & Figures 2020. Surveillance Research 2020 2020 [cited 2020; Available from: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2020/special-section-cancer-in-adolescents-and-young-adults-2020.pdf.
- 33.National Cancer Institute. Closing the gap: research and care imperatives for adolescents and young adults with cancer: a report of the Adolescent and Young Adult Oncology Progress Review Group. 2006; Available from: https://www.livestrong.org/sites/default/files/what-we-do/reports/ayao_prg_report_2006_final.pdf. Cited 2023 Sep
- 34.JBI. Appendix 8.1 JBI Mixed Methods Data Extraction Form following a Convergent Integrated Approach. 2024 [Cited 2024; Available from: https://jbi-global-wiki.refined.site/space/MANUAL/355829472/Appendix+8.1+JBI+Mixed+Methods+Data+Extraction+Form+following+a+Convergent+Integrated+Approach.
- 35.JBI. Critical-Appraisal-Tools—Critical Appraisal Tools. 2020; Available from: https://jbi.global/critical-appraisal-tools. Cited 2023 December
- 36.Lockwood C, Munn Z, Porritt K. Qualitative research synthesis: methodological guidance for systematic reviewers utilizing meta-aggregation. Int J Evid Based Healthc. 2015;13(3):179–87. [DOI] [PubMed] [Google Scholar]
- 37.Mohapatra, S., S. Wisidagama, and F. Schifano Exploring vaping patterns and weight management-related concerns among adolescents and young adults: a systematic review. J Clin Med 2024 13. 10.3390/jcm13102896. [DOI] [PMC free article] [PubMed]
- 38.Yapa HE, et al. The relationship between chronic kidney disease, symptoms and health-related quality of life: a systematic review. J Renal Care. 2020;46(2):74–84. [DOI] [PubMed] [Google Scholar]
- 39.Chan A, et al. Assessment of psychological distress among Asian adolescents and young adults (AYA) cancer patients using the distress thermometer: a prospective, longitudinal study. Support Care Cancer. 2018;26(9):3257–66. [DOI] [PubMed] [Google Scholar]
- 40.Fujii H, et al. Miscorrelation of functional outcome and sociooccupational status of childhood, adolescent, and young adult generation with bone and soft tissue sarcoma patients. J Pediatr Hematol Oncol. 2019;41(2):112–7. [DOI] [PubMed] [Google Scholar]
- 41.Furui T, et al. Problems of reproductive function in survivors of childhood- and adolescent and young adult-onset cancer revealed in a part of a national survey of Japan. Reprod Med Biol. 2019;18(1):105–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Furui T, et al. Fertility preservation in adolescent and young adult cancer patients: from a part of a national survey on oncofertility in Japan. Reprod Med Biol. 2019;18(1):97–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Endo M, et al. Predictors of post-cancer diagnosis resignation among Japanese cancer survivors. J Cancer Surviv. 2020;14(2):106–13. [DOI] [PubMed] [Google Scholar]
- 44.Hamzah, S.R.a., et al. Quality of working life and career engagement of cancer survivors: the mediating role of effect of disease and treatment. Eur J Train Dev. 2021; 45(2–3):181–99.
- 45.Okamura M, et al. Unmet supportive care needs and associated factors among young adult cancer patients in Japan. BMC Cancer. 2021;21(1):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tan CJ, et al. Work outcomes and medical costs among Singaporean adolescent and young adult cancer survivors. J Adolesc Young Adult Oncol. 2023;12(3):416–24. [DOI] [PubMed] [Google Scholar]
- 47.Wu X, et al. Factors associated with reproductive concerns among young female patients with colorectal cancer: a cross-sectional study. J Clin Nurs. 2023;32(15–16):5274–85. [DOI] [PubMed] [Google Scholar]
- 48.Ke Y, et al. Optimizing survivorship care services for Asian adolescent and young adult cancer survivors: a qualitative study. J Adolesc Young Adult Oncol. 2020;9(3):384–93. [DOI] [PubMed] [Google Scholar]
- 49.Tan CJ, et al. Work- and insurance-related issues among Asian adolescent and young-adult cancer survivors: a qualitative study. Support Care Cancer. 2020;28(12):5901–9. [DOI] [PubMed] [Google Scholar]
- 50.Yoshida K, Matsui Y. The impact of cancer on romantic relationships and marriage postdiagnosis among young adult cancer survivors in Japan: a qualitative study. J Adolesc Young Adult Oncol. 2022;11(2):146–55. [DOI] [PubMed] [Google Scholar]
- 51.Qiu J, et al. Psychological and reproductive decision-making experiences of young women after breast cancer diagnosis: a qualitative study. Support Care Cancer. 2023;31(7):423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Guo X, et al. The relationship between filial piety and the academic achievement and subjective wellbeing of Chinese early adolescents: the moderated mediation effect of educational expectations. Front Psychol. 2022;13: 747296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Stone DS, et al. Young adult cancer survivors and work: a systematic review. J Cancer Surviv. 2017;11(6):765–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Altherr A, et al. Education, employment, and financial outcomes in adolescent and young adult cancer survivors-a systematic review. Curr Oncol. 2023;30(10):8720–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.European Network of Youth Cancer Survivors. European Network of Youth Cancer Survivors. 2025; Available from: https://beatcancer.eu/events/.
- 56.The Economist. Cancer preparedness in Asia-Pacific: Progress towards universal cancer control. The Economist Intelligence Unit 2020; Available from: https://worldcancerinitiative.economist.com/pdf/Roche-cancer-preparedness-in-asia/Roche_Cancer_White_paper.pdf.
- 57.Foundation for Promotion of Cancer Research, J. Cancer statistics in Japan 2021. 2021 [cited 2024 Mar 2]; Available from: https://ganjoho.jp/public/qa_links/report/statistics/pdf/cancer_statistics_2021.pdf.
- 58.Singapore Cancer Society. SCS Return To Work Programme. Available from: https://www.singaporecancersociety.org.sg/scs-return-to-work-programme.html.
- 59.Jong MC, et al., The development and acceptability of a wilderness programme to support the health and well-being of adolescent and young adult cancer survivors: The WAYA Programme. Int J Environ Res Public Health. 2022; 19(19):12012. [DOI] [PMC free article] [PubMed]
- 60.Youth Cancer Europe. STRONG-AYA. 2025 [cited 2025; Available from: https://www.youthcancereurope.org/past_projects/eu-projects/.
- 61.National Cancer Centre Singapore. A unique support system for adolescents and young adults with cancer. [cited 2025; Available from: https://www.nccs.com.sg/patient-care/Pages/a-unique-support-system-for-adolescents-and-young-adults-with-cancer.aspx.
- 62.Hirayama T, et al. A hospital-based online patients support program, online adolescent and young adult Hiroba, for adolescent and young adult cancer patients at a designated cancer center in Japan. J Adolesc Young Adult Oncol. 2022;11(6):588–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Endo M, et al. Returning to work after sick leave due to cancer: a 365-day cohort study of Japanese cancer survivors. J Cancer Surviv. 2016;10(2):320–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kaneko S, et al. Differences in cancer patients’ work-cessation risk, based on gender and type of job: Examination of middle-aged and older adults in super-aged Japan. PLoS ONE. 2020;15(1): e0227792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Koczwara B, et al. Cancer survivorship in the indo-pacific: priorities for progress. JCO Glob Oncol. 2023;9: e2200305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Min HS, Yang HK, Park K. Supporting low-income cancer patients: recommendations for the public financial aid program in the Republic of Korea. Cancer Res Treat. 2018;50(4):1074–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.National Cancer Center. Financial Aid Program for Cancer Patients. [Cited 2024; Available from: https://www.ncc.re.kr/main.ncc?uri=english/sub04_ControlPrograms06.
- 68.Li CK, et al. Care of adolescents and young adults with cancer in Asia: results of an ESMO/SIOPE/SIOP Asia survey. ESMO Open. 2019;4(3): e000467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Warner EL, et al. Social well-being among adolescents and young adults with cancer: A systematic review. Cancer. 2016;122(7):1029–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Osmani V, et al. Prevalence and risk of psychological distress, anxiety and depression in adolescent and young adult (AYA) cancer survivors: A systematic review and meta-analysis. Cancer Med. 2023; 12(7):18354–67. [DOI] [PMC free article] [PubMed]
- 71.Hong YR, Tauscher J, Cardel M. Distrust in health care and cultural factors are associated with uptake of colorectal cancer screening in Hispanic and Asian Americans. Cancer. 2018;124(2):335–45. [DOI] [PubMed] [Google Scholar]
- 72.Patel-Kerai G, et al. The psychosocial experiences of breast cancer amongst Black, South Asian and White survivors: do differences exist between ethnic groups? Psychooncology. 2017;26(4):515–22. [DOI] [PubMed] [Google Scholar]
- 73.Wang JH, et al. Factors associated with Chinese American and White cancer survivors’ physical and psychological functioning. Health Psychol. 2019;38(5):455–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Li T, Cheng S-T, Family, friends, and subjective well-being: a comparison between the west and Asia, in friendship and happiness: across the life-span and Cultures, M. Demir, editors. Springer. Netherlands: Dordrecht; 2015. p. 235–51. [Google Scholar]
- 75.Yeung W-JJ, Alipio C. Transitioning to adulthood in Asia: school, work, and family life. ANNALS Am Acad Pol Soc Sci. 2013;646(1):6–27. [Google Scholar]
- 76.Krauth KA. Family-Oriented Rehabilitation (FOR) and Rehabilitation of Adolescents and Young Adults (AYA) in Pediatric Oncology. Oncol Res Treat. 2017;40(12):752–8. [DOI] [PubMed] [Google Scholar]
- 77.GBD 2021 Fertility and Forecasting Collaborators. Global fertility in 204 countries and territories, 1950–2021, with forecasts to 2100: a comprehensive demographic analysis for the Global Burden of Disease Study 2021. Lancet, 2024; 403(10440):2057–99. [DOI] [PMC free article] [PubMed]
- 78.Nakata K, et al. Cancer in adolescents and young adults in Japan: epidemiology and cancer strategy. Int J Clin Oncol. 2022;27(1):7–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hong Kong Cancer Fund. Fertility Preservation Support Service Programme. [cited 2024; Available from: https://www.cancer-fund.org/en/blog/fertility-preservation-support-service-programme/#:~:text=The%20Fertility%20Preservation%20Clinics%20of,and%20ovarian%20tissue%20freezing%20services.&text=We%20will%20provide%20full%20financial,two%20years%20of%20freez.
- 80.International Labour Organization. C183—Maternity Protection Convention. 2000; Available from: https://www.ilo.org/dyn/normlex/en/f?p=NORMLEXPUB:55:0::NO::P55_TYPE,P55_LANG,P55_DOCUMENT,P55_NODE:REV,en,C183,/Document.
- 81.Government Offices of Sweden. Parental Leave Act. Ministry of Employment. 1995; Available from: https://www.government.se/contentassets/d163a42edcea4638aa112f0f6040202b/sfs-1995584-parental-leave-act/.
- 82.Skaczkowski G, et al. Factors influencing the provision of fertility counseling and impact on quality of life in adolescents and young adults with cancer. J Psychosoc Oncol. 2018;36(4):484–502. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.