Abstract
Chronic pain is an extremely prevalent healthcare issue that has a profound impact on individuals and society. Sex and sex hormones regulate the pain threshold differently in males and females in pain processing. However, the regulatory mechanisms of sex differences in response to painful stimuli are still unclear, which contributes to the difficulty of analgesic drug development. Interleukins mediate neuroinflammation and are involved in the development of chronic pain. Recent studies have found that sex and sex hormones are involved in the regulation of pain thresholds by interleukins. Most previous studies used male animals to study the analgesic effects of treatments due to the complexity of estrogen. This review summarizes studies that used only female animals or both sexes to examine the impact of sex on interleukin-regulated chronic pain, to provide a theoretical basis for the development of more targeted precision medicines for pain.
Keywords: sex differences, chronic pain, interleukins, neuroinflammation
1. Introduction
Chronic pain is an extremely prevalent healthcare issue [1]. Estimates suggest that 10% of the world’s population endures chronic pain, and closer to 20–25% in individual countries and regions [2]. Chronic pain can influence the quality of life of patients and impose a substantial financial burden on the healthcare system [3,4]. Although many studies have elucidated the mechanisms underlying the development of pain [5,6,7], currently available treatments for pain are burdened by undesirable side effects. It is worth noting that most preclinical studies used male animals to explore the mechanisms of acute and persistent pain [8,9,10,11]. However, clinical studies reported that women have a higher incidence rate of chronic pain conditions, such as fibromyalgia, migraine, and osteoarthritis (OA) [12,13,14]. In addition, in one laboratory test of healthy volunteers, using various stimuli such as heat, pressure, and chemical irritants, pain thresholds and pain tolerance in women were shown to be lower than in men [15,16,17]. These indicate that women and men may have different underlying physiological mechanisms that contribute to pain. Thus, ignoring sex differences may be one of the reasons for the differences in the efficacy of pain treatment.
The interleukin (IL) family of cytokines has pleiotropic functions in inflammation and acquired immunity [18,19]. ILs can be divided into several families with more than 40 subfamily members [19]. In the nervous system, ILs are produced from many types of cells, which include neurons, glia, immune cells, and other non-neuronal cells [20]. ILs can mediate neuroimmune interaction, triggering abnormal glia activation, immune cell infiltration, and neural activation, and contributing to neuroinflammation [21]. Neuroinflammation can alter the excitability of nerve terminals and regulate pain transduction [21,22,23]. In the past several years, IL-mediated neuroinflammation has been found to participate in acute or chronic pain [22,23,24,25,26], which makes it a potential intervention candidate. Notably, the expression levels and activations of ILs are influenced by sex differences [27,28,29,30]. Furthermore, several ILs were found to exert specific effects on pain modulation in different sexes [30,31]. In this review, we will summarize the various effects of the diverse IL families in pain that are influenced by sex differences and discuss the mechanisms of these ILs in both sexes, with a special focus on females, in the hope of inspiring more individualized treatment strategies for pain.
2. The Influences of Sex Differences in Pain Processing and the Diversity of Estrogen Action
From a biological perspective, sexual differentiation of pain results in large part from organizational and activation effects of gonadal steroid hormones [32]. Although three common kinds of sex hormones (testosterone, estrogen, and progesterone) have been thought to be involved in nociception [32,33,34,35,36,37], their modulative mechanisms in pain processing may be different [38,39]. A previous study found that sex-related differences in spinal alpha (2)-adrenergic receptor-mediated nociception in rats were gonadal hormone-dependent: estrogen attenuated antinociceptive effects in females, whereas testosterone was required for the expression of antinociception in males [38]. This indicates the different roles of gonadal hormones in regulating pain reactivity. Notably, in another research, κ opioid receptor (KOR) antinociception was enhanced by estrogen in the spinal cord of female SD rats [39]. Selective KOR agonists could dose-dependently increase the thermal threshold in proestrus (the phase of the estrous cycle with the highest levels of circulating estradiol) females, but not in intact and ovariectomized (OVX) females or males. Furthermore, estrogen re-injection could dose-dependently enhance the effect of KOR agonist in OVX rats. These two studies reveal an interesting phenomenon: the effect of estrogen on the transmission of pain signals has a dual nature.
Estrogen receptors (ERs) include two classical receptors, ERα and ERβ [40]. A previous study showed that ERβ-selective agonists were effective in promoting allodynia induced by chemotherapy in rats, while the ERα-selective agonists had no effect on chemotherapy-induced pain [41]. This indicates that different ERs can exert different effects on pain modulation. However, the roles of these two receptors are not so absolute, and there is evidence showing that ERα and ERβ might play pro-nociceptive roles [42]. In their research, knockout of either receptor was found to significantly increase the elevated response to mechanical stimuli in female mice. The different effects of ERs are involved in different mechanisms, including protein kinase, inflammatory cytokines, and ion channels [40,43]. In addition, the different distribution of ERs may explain the mechanisms of differences. ERs are ubiquitously expressed by nociceptive system neurons [23]. However, in adult female rat ganglia, ERα expression is restricted to small sensory neurons, while ERβ is widely expressed in most sensory neurons. In the spinal cord, ERα expression appears large and numerous in the superficial dorsal horn (laminaes I–II), but ERβ is mainly expressed in the deeper laminaes (laminaes III–V, VIII, and IX) of the spinal cord [40,44,45]. Moreover, non-classical receptor GPR30 also plays a crucial role in pain modulation [40]. These results further clarify the comprehensive mechanisms of ER signaling pathways in pain processing in females.
In addition, in female rats, estrogen and progesterone regulate pain thresholds depending on their dose, the interaction between these two hormones, and the stage of pain [32,36]. Estradiol and progesterone can attenuate mechanical allodynia dose-dependently [36,46]. In inflammatory pain induced by formalin injection into the rat hind paw [36], estradiol dose-dependently exerted an analgesic effect during phase II (chronic pain) but not phase I (acute pain). Only a high dose of progesterone (500 μg) exerted an analgesic effect during phase I (acute pain) at 1% formalin. However, when co-administration of estradiol (20 μg) and progesterone, a low dose of progesterone (50 μg) could reverse the analgesic effect of estradiol, though this effect was not observed after using its high dose (500 μg). Notably, the levels and activities of estrogen and progesterone can change along with the menstrual cycle, which results in highly equivocal results about sex hormone modulation of nociception in humans and animals [32,36,47].
3. The Influences of Sex Differences in Interleukin Production and Reactivity in the Nervous System
Given the impracticality of treating sex hormones, we will explore other sex-associated mechanisms in pain signaling transmission. Neuroinflammation is critical for pain development [48]. ILs, produced from neurons, glia, immune cells, and other non-neuronal cells [20], play important roles in pain signaling transmission by regulating neuroinflammation [24,25,26]. Sex hormones can affect the production and signaling of interleukins by directly interacting with hormone receptors present in immune cells and neurons, which can alter gene transcription and lead to changes in cytokine expression [40,49,50,51,52]. Sex differences were found to be critical for mediating the immune system [53]. Increasingly, studies have paid attention to the roles of biological sex and sex hormones on changes in these inflammatory markers in the nervous system [54,55]. In the chronic stress model, stress exposure affected the regulation of rat brain IL-1β by the norepinephrine-β-adrenergic receptor pathway in males but not females [56]. In mice brains in which LPS induced proinflammatory cytokine response, IL-1β expression was increased in females but not males [57]. Thus, the production and activation of ILs are influenced by sex and sex hormones in different diseases, which provides important evidence that targeting sex-associated IL activations may provide a potential therapeutic strategy for sex-biased pain.
4. Sex Differences-Associated ILs in Chronic Pain
Chronic pain is characterized by spontaneous, ongoing, or evoked by sensory stimuli [58]. According to the international classification of diseases for chronic pain (CD-11), it can be generally categorized as chronic primary pain syndromes (such as complex regional pain syndromes (CRPS), and fibromyalgia) and chronic secondary pain syndromes [59]. The latter is linked to other diseases as the underlying cause, and it includes chronic neuropathic pain, chronic cancer-related pain, chronic musculoskeletal pain, and others. Neuropathic pain is usually caused by central nerve lesions or peripheral nerve lesions, such as peripheral nerve injury and diabetic neuropathy. Chronic cancer-related pain can be caused by the cancer itself (primary tumor or metastases) or by its treatment (surgery, chemotherapy, and radiotherapy) [58]. Chronic musculoskeletal pain is subdivided into many types according to the various underlying mechanisms, such as persistent inflammation of infectious, autoimmune, or metabolic etiology (e.g., rheumatoid arthritis), or structural changes affecting bones, joints, or muscles (e.g., symptomatic OA). Various animal models of neuropathic pain, musculoskeletal pain, cancer-related pain, and autoimmune dysfunction-induced pain have been established to explore the mechanisms underlying the development of chronic pain [26,30,60,61,62,63,64,65].
Preclinical research found that, despite various causes of different types of chronic pain, neuroinflammation was critical for most pain development [66,67]. ILs, mediators of neuroinflammation, have been well discussed in previous reviews [68,69,70], such as IL-1β [71], IL-6 [70], IL-18 [72], IL-17 [69], IL-23 [73], IL-10 [74], IL-33 [75]. However, the subjects of previous experiments have overwhelmingly been male [11]. Few studies explored the mechanisms of pain development in females or both sexes, and even identified the role of sex differences in pain processing. Thus, the hypotheses were mostly confirmed in males but not in females, indicating that the entire preclinical conclusion may be male-biased. Recently, researchers have been paying more attention to the influences of sex differences in pain development [11]. Increasing studies have focused on various roles of ILs in different sexes. For example, the IL-23/IL-17A axis could regulate female-specific mechanical pain [30]. IL-6 could mediate pain associated with posttraumatic OA in a sex-specific manner [76]. Meanwhile, studies using both sexes found that not all mechanisms contributing to pain development appeared to differ by sex [77,78]. This review focuses on the role of ILs in chronic pain females found from recent preclinical studies that only use female animals and summarizes the similarities and differences in the roles of ILs in studies that used both sexes. (Table 1).
Table 1.
IL-mediated chronic pain in studies using only female animals or both sexes.
| Sex | Interleukin | Mechanism | Effect on Pain | Type of Pain Model | Type of Pain-Like Behavior | Location | Expression Patterns | Reference |
|---|---|---|---|---|---|---|---|---|
| Female and male | IL-1β | Knockout of IL-1 receptor in TRPV1+ nociceptors of DRG prevents the development of inflammatory pain. | Promote | MOG35–55-induced MS, arthritogenic K/BxN serum-induced RA, and MIA-induced OA | Mechanical allodynia | TRPV1+ nociceptors of DRG | Up-regulation | [61] |
| Female and male | IL-1β | Total mRNA expression of IL-1β is higher in females than in males after CCI. NLRP3 and AIM2 are more highly expressed in females, but NLRP1 expression is higher in males. | Promote | CCI-induced pain | Mechanical allodynia | SC | Up-regulation | [79] |
| Female, but not male | IL-1β | IL-1β increases mechanical and thermal pain responsiveness by decreasing PMCA2 levels. | Promote | MOG35–55-induced MS | Mechanical and thermal hyperalgesia | SC | Up-regulation | [65,80] |
| Female | IL-1β | IL-1 receptor antagonists prevent the development of CRPS and reverse the established CRPS by inhibiting microglia activation of dorsal horn. | Promote | CRPS | Mechanical allodynia | plasma, paw, dorsal horn | Up-regulation | [64] |
| Female | IL-1β | IL-1β-mediated glial-neuron crosstalk contributes to the development of fibromyalgia. | Promote | Fibromyalgia | Thermal hyperalgesia, mechanical allodynia | medial prefrontal cortex | Up-regulation | [81] |
| Female and male | IL-1β | Metformin ameliorates fibromyalgia by reducing the increased IL-1β levels in males, but partially decreasing IL-1β levels in the brain of females. | Promote | Fibromyalgia | Thermal hyperalgesia, mechanical allodynia | Brain, SC | Up-regulation | [82] |
| Female and male | IL-6 | CNTF-STAT3-IL-6 axis. | Promote | SNI or CCI-induced pain | Mechanical allodynia, thermal hyperalgesia | DRG, SC | Up-regulation | [83] |
| Male, but not female | IL-6 | IL-6/JAK signaling is a critical mediator of IL-6-induced cartilage catabolism and pain signaling in nociceptive neurons; IL-6/STAT3 signaling is a potent driver of cartilage catabolism; IL-6/ERK signaling is essential for IL-6-induced neurite outgrowth and pain signaling in DRG neurons. | Promote | Post-traumatic OA induced by destabilization of the medial meniscus | Mechanical allodynia | Joint, DRG | Up-regulation | [76] |
| Female | IL-6 | Electroacupuncture treatment and TRPV1 deletion reduce chronic pain by reversing the increase in IL-6. | Promote | fibromyalgia induced by ICS | Mechanical allodynia, thermal hyperalgesia | plasma | Up-regulation | [84] |
| Female | IL-6 | IL-6 induces postmenopausal osteoporotic pain by regulating calcitonin gene-related peptide (CGRP) expression. | Promote | Postmenopausal osteoporotic pain | Mechanical allodynia | Joint, DRG | Up-regulation | [85] |
| Female | IL-6 | IL-6 regulates miRNA-21 expression by STAT3 pathway and results in chronic pelvic pain induced by endometriosis | Promote | Chronic pelvic pain | / | Eutopic and ectopic tissues | Up-regulation | [86] |
| Female | IL-6 | IL-6 upregulates TRPV1 expression and function through JAK/PI3K signaling pathway. | Promote | Cancer-induced bone pain | Mechanical allodynia, thermal hyperalgesia | DRG | Up-regulation | [87] |
| Female | IL-6 | Anti-IL-6 receptor antibody decreases mechanical allodynia by inhibiting microglial activation and proliferation. | Promote | MOG35–55-induced MS | Mechanical allodynia | SC | Up-regulation | [88] |
| Male, but not female | IL-6 | RvD5 can inhibit trigeminal pain by reducing level of IL-6. | Promote | Trigeminal pain induced by CCI-ION | Mechanical allodynia, thermal hyperalgesia | Trigeminal ganglion | Up-regulation | [89] |
| Female | IL-18 | Microglia can maintain advanced-phase cancer pain by producing the proinflammatory cytokine IL-18 to enhance synaptic transmission. | Promote | Cancer-induced bone pain | Mechanical allodynia, thermal hyperalgesia | Microglia in SC | Up-regulation | [90] |
| Female | IL-18 | Gi protein-coupled receptor (GPR109A) attenuates thermal hyperalgesia via suppressing p38 MAPK activity and production of IL-18. | Promote | SLE | Thermal hyperalgesia | Microglia in SC | Up-regulation | [91] |
| Female and male | IL-23 | IL-23 promotes arthritic inflammatory pain induced by GM-CSF, TNF, or CCL17 via COX. | Promote | Zymosan-driven arthritic pain | Pain-like behavior (incapacitance meter) | Joint | Up-regulation | [73,92] |
| Female, but not male | IL-23/IL-17A | Under expression of ERα, IL-23 requires IL-17A release from macrophages to evoke mechanical pain through TRPV1 nociceptor. | Promote | IL-23-induced pain, chemotherapy (paclitaxel)-induced pain, CCI-induced pain, streptozotoxin-induced diabetic neuropathy, formalin-induced pain | Mechanical allodynia, but not thermal hyperalgesia, or cold allodynia | IL-23 in macrophages of DRG, IL-17A in C-fiber nociceptors of DRG | Up-regulation | [30] |
| Female, but not male | IL-23 | Estrogen and IL-23 co-application increases IL-17A release in THP-1 human macrophages and promotes C-fiber-mediated spontaneous pain. | Promote | Blue light-induced spontaneous Pain | Mechanical allodynia | C-fiber nociceptors of DRG | Up-regulation | [31] |
| Female | IL-17A | Chinese medicated gel Long-Teng-Tong-Luo inhibits bone cancer pain by decreasing transient receptor potential channel expression in DRG and spinal astrocyte IL-17A. | Promote | Cancer-induced bone pain | Mechanical allodynia, thermal hyperalgesia | SC | Up-regulation | [93] |
| Female | IL-17 | Electroacupuncture treatment and TRPV1 deletion reduce heat and mechanical hyperalgesia by decreasing IL-17 and IL-17-related signaling pathways (PI3K/Akt, p38, JNK, NF-κB) levels. | Promote | Fibromyalgia induced by ICS | Mechanical allodynia, thermal hyperalgesia | Somatosensory cortex, cerebellum lobe V-VII | Up-regulation | [84] |
| Female | IL-17 | IL-17 promotes the occurrence of MS-associated chronic pain by improving CaMKIIα activation. | Promote | MOG35–55-induced MS | Mechanical allodynia, thermal hyperalgesia | SC | Up-regulation | [94] |
| Female and male | IL-33 | IL-33-TNFα-IL-1β-IFNγ-endothelin 1-prostaglandin (PG) E2 signaling cascade participates in antigen-induced cutaneous and articular hypernociception. | Promote | Antigen-induced pain | Mechanical allodynia | Skin of paw | Up-regulation | [95,96] |
| Female and male | IL-10 | A3-adenosine receptor agonist reverses mechanical allodynia by promoting the IL-10 release of CD4+ T cells in DRG. | Reverse | CCI-induced pain | Mechanical allodynia | CD4+ T cells in DRG | / | [97] |
| Female and male | IL-10 | Sphingosine-1-phosphate antagonists attenuate and reverse neuropathic pain by promoting IL-10 production in astrocytes of spinal cord. | Alleviate, reverse | SNI- and CCI-induced pain | Mechanical allodynia, thermal anti-nociception | Astrocytes in SC | / | [98] |
| Female and male | IL-10 | IL-10 inhibits spinal abnormal synaptic plasticity through β-endorphin expression in microglia. | Alleviate | SNL-induced pain | Mechanical allodynia, thermal hyperalgesia | SC | / | [99] |
| Female and male | IL-10 | Inducible co-stimulatory molecule agonist antibody (ICOSaa) shows a more rapid resolution of mechanical hypersensitivity in females by recruiting T cells and driving IL-10 production. | Alleviate | Chemotherapy (paclitaxel)-induced pain, SNI-induced pain | Mechanical allodynia | T cell in DRG | / | [100] |
| Female and male | IL-10 | IL-13 produced by CD8+ T cells promotes IL-10 release in macrophages of DRG, ameliorating cisplatin-induced mechanical allodynia. | Alleviate | Chemotherapy (cisplatin)-induced pain | Mechanical allodynia | Macrophages of DRG | Up-regulation | [62] |
| Female | IL-10 | Intrathecal IL-10 can effectively reduce cancer-induced bone pain behavior. | Alleviate | Cancer-induced bone pain | Mechanical allodynia | SC | / | [63] |
| Female | IL-10 | IL-10 from GRK+ macrophages promotes resolution of carrageenan-induced mechanical allodynia and thermal hyperalgesia. | Alleviate | Carrageenan-induced pain | Mechanical allodynia, thermal hyperalgesia | Peripheral monocytes/macrophages in DRG | Up-regulation | [101] |
| Male | IL-35 | Intrathecal recombinant IL-35 treatment alleviates mechanical pain by inhibiting microglia activation. | Alleviate | CCI-induced pain | Mechanical allodynia | SC | / | [102] |
| Female | IL-35 | IL-35 reduces mechanical allodynia and spontaneous pain by increasing myelination, upregulating IL-10 expression, and reducing monocyte infiltration. | Alleviate | MOG35–55-induced MS | Mechanical allodynia, spontaneous pain | SC | Down-regulation | [103] |
AIM2, absent in melanoma 2; CCI, chronic constriction injury; CCI-ION, chronic constriction injury of the infraorbital nerve; CCL17, C-C motif ligand 17; DRG, dorsal root ganglion; ERα, estrogen receptor subunit α; GM-CSF, granulocyte macrophage-colony stimulating factor; ICS, intermittent cold stress; JAK, Janus kinase; MIA, monosodium iodoacetate; MOG35–55, myelin oligodendrocyte glycoprotein peptide 35–55; MS, multiple sclerosis; NLRP1, nod-like receptor protein 1; NLRP3, nod-like receptor protein 3; OA, osteoarthritis; PI3K, phosphatidylinositol 3-kinase; RA, rheumatoid arthritis; RvD5, D-series resolvins 5; SC, spinal cord; SLE, systemic lupus erythematosus; SNL, spinal nerve ligation; TNF, tumor necrosis factor; TRPV1, transient receptor potential vanilloid channel type 1.
4.1. IL-1β
IL-1 traditionally includes IL-1α, IL-1β, IL-1Rα, and their receptors are IL-1R1 and IL-1R2 [19]. As a proinflammatory factor, IL-1β is usually regarded as a biomarker of inflammation [104]. Estradiol and progesterone could reduce both IL-1α and IL-1β production in mononuclear leukocytes [105], indicating the effect of sex hormones in the production and activation of IL-1β.
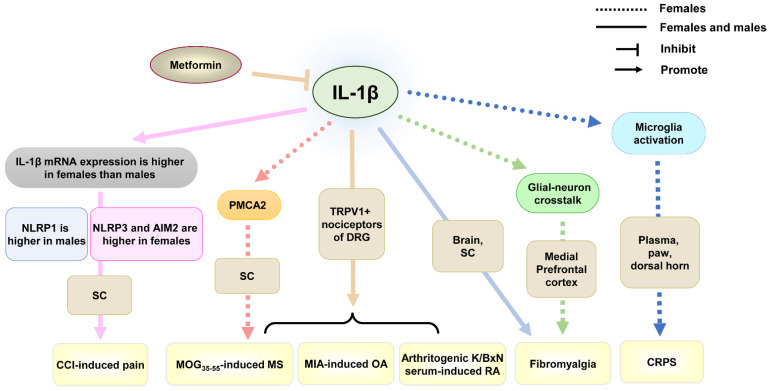
IL-1β was found to promote chronic pain in males, such as neuropathic pain [60,106] and inflammatory pain [61,107]. Similarly, the increased level of IL-1β in females was found in inflammatory pain and neuropathic pain [61,108] (Table 1 and Figure 1). In myelin oligodendrocyte glycoprotein peptide 35–55 (MOG35–55)-induced multiple sclerosis (MS), arthritogenic K/BxN serum-induced rheumatoid arthritis (RA), and monosodium iodoacetate (MIA)-induced OA models of female and male mice, IL-1β-producing myeloid cells were found to infiltrate around IL-1 receptor-expressing nociceptors in DRG. Knockout of IL-1 receptor in transient receptor potential vanilloid 1 positive (TRPV1+) nociceptors of DRG prevented the development of these inflammatory pains in both male and female mice [61]. Though IL-1β can participate in inflammatory pain in both males and females, the mechanisms behind it may be different. In chronic constriction injury (CCI)-induced neuropathic pain in rats, intrathecal IL-1 receptor antagonists reversed the established mechanical allodynia in both sexes. However, there were several differences in the expression level of the gene coding for IL-1β, as well as the four inflammasomes responsible for IL-1β release: nod-like receptor protein 3 (NLRP3), absent in melanoma 2 (AIM2), NLRP1, and NOD-like receptor family CARD-containing 4 protein (NLRC4) in rat spinal cord of different sexes [79]. The total mRNA level of IL-1β was higher in females than in males after CCI. NLRP3 and AIM2 proteins were more highly expressed in females, but NLRP1 expression was higher in males. These indicate that the mechanisms of IL-1β expression and activation are different in both sexes, which provides new insights into therapeutic strategies to compensate for the insufficient efficacy of IL-1 receptor antagonists in males and females. In addition, intrathecal treatment with IL-1α can dose-dependently attenuate symptoms of chronic pain by CCI or chemotherapy in male rats [109,110], which suggests the different effects between IL-1β and IL-1α. The effect of IL-1α in females needs to be further explored.
Figure 1.
The role of IL-1β in chronic pain from studies using females only or both sexes. Abbreviations: CCI, chronic constriction injury; CRPS, complex regional pain syndromes; DRG, dorsal root ganglion; MIA, monosodium iodoacetate; MOG35–55, myelin oligodendrocyte glycoprotein peptide 35–55; MS, multiple sclerosis; NLRP, nod-like receptor protein; OA, osteoarthritis; PMCA2, plasma membrane calcium ATPase 2; RA, rheumatoid arthritis; SC, spinal cord; TRPV1, transient receptor potential vanilloid 1.
In addition, in MOG35–55-induced MS, an autoimmune inflammatory disorder of the nervous system, increased mechanical and thermal pain responsiveness in MS was paralleled by a significant decrease in plasma membrane calcium ATPase 2 (PMCA2) level in the spinal dorsal horn of female mice, but the PMCA2 level remained unaltered in MS mice without the increased pain [65], indicating that PMCA2 plays an important role in pain processing in MS females [80]. Though male mice showed a similar change in PMCA2 level during MS [65], female mutant PMCA2+/− mice were found to be more sensitive to evoked mechanical pain than wild-type controls of the same sex, whereas such a difference was not observed in male PMCA2+/− and PMCA2+/+ mice [80], indicating that the different mechanisms of PMCA2 in MS-associated pain in different sexes. IL-1β, tumor necrosis factor α (TNFα), and IL-6 expressions were robustly increased in the spinal dorsal horn of female mice with MS manifesting pain, whereas these cytokines showed modest increases or no change in female mice with MS in the absence of pain [65]. In vitro, only IL-1β decreased PMCA2 levels in pure spinal cord neuronal cultures, indicating that IL-1β in females can downregulate PMCA2 activation, participating in MS-associated chronic pain.
CRPS is a primary pain condition that typically affects the limb, even associated with motor dysfunction. It is usually triggered by an injury or trauma [111]. CRPS is more prevalent in females than males. In the CRPS female mouse model (Table 1), the levels of IL-1β were increased in plasma and the paw. Using IL-1 receptor antagonists, anakinra, inhibited microglia activation of the dorsal horn, not only preventing the development of CRPS, but also reversing the established CRPS [64]. This indicates that the blockade of the IL-1 receptor can alleviate CRPS in females. However, IL-1β in males was also found to participate in CRPS. The roles of IL-1β in CRPS in both sexes need to be further explored.
Fibromyalgia is a chronic primary condition characterized by widespread pain. Fibromyalgia affects approximately 3–9% of the global population and is significantly more prevalent in females than in males [112]. In the fibromyalgia model (Table 1), IL-1β in microglia of the medial prefrontal cortex of female rats was increased, and injection of IL-1β antibody significantly reduced the expression of group III secretory phospholipase A2 (sPLA2-III) in neurons, alleviating thermal hyperalgesia and mechanical allodynia in the hind paws [81], indicating that IL-1β-mediated glial-neuron crosstalk contributes to the development of fibromyalgia in females. In another study, increased IL-1β levels were found in the brain and spinal cord in both male and female mice, using metformin to ameliorate thermal hyperalgesia and mechanical allodynia. In addition, metformin significantly reduced the increased IL-1β levels in both females and males, but the IL-1β level in the brain of females, rather than males, did not reach a near-normal level [82]. These results suggest that IL-1β in both sexes can participate in the development of fibromyalgia, but the different mechanisms of IL-1β in both sexes need to be further explored.
4.2. IL-6
IL-6, a proinflammatory cytokine, can also participate in inflammation by binding either to the membrane-bound (classic signaling) or the soluble form (trans-signaling) of the IL-6 receptor (IL-6R) [113]. In males, upon aging, IL-6-knockout mice developed more severe spontaneous OA, compared to females [114]. In addition to the influences on IL-6 production [115,116], sex differences can regulate sex-specific responses to IL-6 [117,118,119,120]. In IL-6-knockout old-age mice, myelin basic protein level in the cerebellum was lower in females, and glial fibrillary acidic protein and lipid peroxidation levels in the hippocampus and cerebellum were increased in males, suggesting that IL-6 can exert its effects in aged females and males by regulating different mechanisms [119]. Thus, the effects of IL-6 on diseases in a sex-dependent manner make the researchers focus on sex differences for interventions and treatments in females versus males.
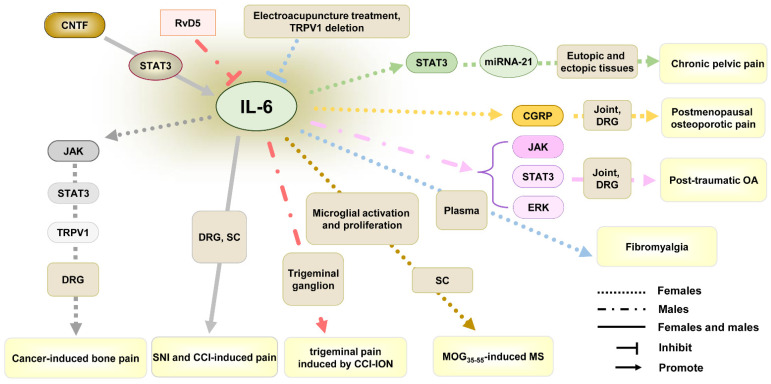
IL-6/IL-6R in DRG and spinal cord were found to play important roles in chronic pain in males and females [121,122]. In cancer-induced bone pain (Table 1 and Figure 2), increased IL-6 in DRG neurons of female rats upregulated expression and activation of TRPV1 through triggering Janus kinase (JAK)/phosphatidylinositol 3-kinase (PI3K) signaling pathway, resulting in mechanical allodynia and thermal hyperalgesia [87]. This indicates that IL-6 can participate in cancer-induced bone pain in females. In neuropathic pain induced by spared sciatic nerve injury (SNI) or CCI, IL-6 participated in ciliary neurotrophic factor (CNTF)-signal transducer and activator of transcription 3 (STAT3) axis-mediated the immune cascades across the Schwann cell-neuron-microglia network in DRG and spinal cord of both males and females [83], indicating the participative roles of IL-6 in SNI or CCI-induced pain in both sexes. However, when D-series resolvins 5 (RvD5) was applied to prevent trigeminal pain induced by chronic constriction injury of the infraorbital nerve (CCI-ION), the lowest dose (3 ng) could promote the antinociceptive effect of RvD5 on heat and mechanical hyperalgesia in male rats. However, only higher doses of RvD5 (10 ng and 30 ng) could decrease chronic pain in females [89], indicating males appear to be more sensitive to RvD5, compared to females. Further research found that IL-6 level was increased in the trigeminal ganglion of male rather than female rats after CCI-ION, and RvD5 could reduce IL-6 level in melas, indicating that sex-associated IL-6 activation may play a crucial role in the efficacy difference in drug on trigeminal pain induced by CCI-ION.
Figure 2.
The role of IL-6 in chronic pain from studies using females only or both sexes. Abbreviations: CCI, chronic constriction injury; CCI-ION, chronic constriction injury of the infraorbital nerve; CGRP, calcitonin gene-related peptide; CNTF, ciliary neurotrophic factor; DRG, dorsal root ganglion; JAK, janus kinase; MOG35–55, myelin oligodendrocyte glycoprotein peptide 35–55; MS, multiple sclerosis; OA, osteoarthritis; RvD5, D-series resolvins 5; SC, spinal cord; STAT3, signal transducer and activator of transcription 3; TRPV1, transient receptor potential vanilloid 1.
In MOG35–55-induced MS, IL-6 expression was robustly increased in the spinal dorsal horn of female mice with MS manifesting pain [65]. Although IL-6 did not influence the PMCA2 level that can be decreased by IL-1β [65], the anti-IL-6 receptor antibody MR16-1 could decrease mechanical allodynia by inhibiting microglial activation and proliferation in the spinal cord of female MS mice [88]. This indicates the role of IL-6 in MS-associated chronic pain in females.
In inflammatory pain induced by OA, a clinical meta-analysis found that women generally reported higher pain-related symptoms [123]. When compared to men, women exhibited greater IL-6 reactivity after exposure to laboratory-evoked pain [124], which might contribute to women’s higher OA-associated pain risk. In OA induced by anterior crucial ligament transaction, IL-6 was found to regulate cartilage matrix anabolism as well as catabolism and participate in the development of OA via retinoic acid receptor-related orphan receptor-α (RORα)/IL-6/STAT3 axis in female mice [125]. However, in post-traumatic OA induced by destabilization of the medial meniscus, genetic ablation of IL-6 in female mice did not inhibit OA-associated cartilage degradation or nociceptive signaling [76]. On the contrary, IL-6 deletion in male mice reduced cartilage degradation through the attenuation of cartilage catabolism and alleviated OA-associated pain. This indicates that, though IL-6 participates in the development of OA by regulating cartilage matrix anabolism and catabolism, it seems uncertain whether IL-6 has an impact on OA-associated pain. In addition, IL-6 exerts its effect on OA not only in a sex-specific manner but also depending on the cause of OA. It should not ignore the effect of IL-6 in males with OA, though the higher level and response of IL-6 in females. Recently, many studies explored the role of JAK signaling and STAT3 signaling in IL-6-induced various types of OA in males [76,126,127]. Based on the similar regulation of IL-6 on STAT3 in females [125], there are more potential roles of IL-6 in females with other types of OA and OA-associated pain that need to be explored.
In the fibromyalgia model induced by intermittent cold stress (ICS), electroacupuncture treatment and TRPV1 deletion reversed the increase in IL-6 in female mice plasma and reduced heat and mechanical hyperalgesia [84], indicating the role of IL-6 in electroacupuncture-treated fibromyalgia. In another sex-associated pain processing, IL-6 was found to participate in postmenopausal osteoporotic pain in female mice, and using an anti-IL-6R antibody could preserve bone health and decrease osteoporotic pain by regulating calcitonin gene-related peptide (CGRP) expression in DRG [85]. In addition, IL-6 could also regulate miRNA-21 expression by STAT3 pathway and result in chronic pelvic pain induced by endometriosis in females [86]. These suggest the important role of IL-6 in chronic pain in favor of females.
4.3. IL-18
IL-18, a member of the IL-1 family, can bind to its specific ligand-binding chain IL-18 receptor α (IL-18Rα) and IL-18Rβ to form a heterotrimeric complex [72]. In the nervous system, IL-18 in microglia can promote neuroinflammation, leading to neurodegeneration [128]. Estradiol-17β treatment was found to improve behavioral scores of spinal cord injury by attenuating NLRP3, IL-1β, IL-18, and caspase-1 expressions [129]. IL-18 was found to be a gene linked to diseases with sex-specific prevalence [130].
An increasing number of studies have demonstrated the important role of IL-18 in the development and maintenance of chronic pain in females and males [72]. In cancer-induced bone pain, microglia in the spinal cord could maintain advanced-phase cancer pain in female rats by producing IL-18 expression to enhance synaptic transmission (Table 1) [90]. Spinal inhibition of the P2X7/p38/IL-18 pathway reduced advanced-phase bone cancer pain. In the female-specific systemic lupus erythematosus (SLE) model, activation of Gi protein-coupled receptor, GPR109A, in spinal microglia of female MRL lupus-prone mice (a well-established mouse model of human SLE) could attenuate thermal hyperalgesia via suppressing p38 activity and IL-18 production [91]. These indicate that IL-18 can participate in chronic pain induced by cancer and SLE. Most studies investigated the role of IL-18 in males [131,132]; however, its effect on chronic pain in females needs to be further explored.
4.4. IL-23/IL-17
IL-23, a member of the IL-12 cytokine family, is a heterodimeric cytokine composed of the IL-23p19 subunit and the IL-12/23p40 subunit [133]. IL-23 is mainly produced by activated macrophages and dendritic cells [134]. It can drive the differentiation and activation of T helper 17 (Th17) cells by binding to IL-23 receptor and IL-12 receptor β1 [133], subsequently promoting releases of IL-17A and IL-17F [134]. Estradiol can suppress IL-17A production from neutrophils and macrophages, which express estrogen receptors, resulting in psoriasis clinical phenotypes by sex-dependent differences, indicating that sex differences make the side effect risk of IL-23 inhibitors higher in females [135].
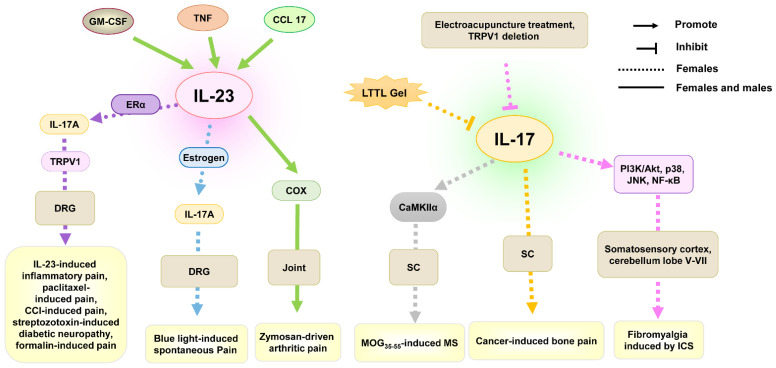
The IL-23/IL-17 axis in joints was found to play an important role in inflammatory arthritis in females and males [136]. The mechanisms of IL-23 in joints of male and female mice participating in zymosan-induced arthritic inflammatory pain were involved in granulocyte macrophage-colony stimulating factor (GM-CSF), TNF, C-C motif ligand 17 (CCL17), and cyclooxygenase (COX), which in turn have themselves been linked in this process [73,92] (Table 1 and Figure 3). Interestingly, IL-23 in the macrophages of mice DRG can induce mechanical allodynia only in females. Previous research found that intraplantar and intrathecal injections of IL-23 resulted in mechanical allodynia, but not thermal hyperalgesia or cold allodynia, in naïve female mice but not male mice in a dose-dependent manner [30]. Similarly, the IL-23/IL-23R axis was found to play an important role in chemotherapy- or CCI-induced neuropathic pain, streptozotoxin-induced diabetic neuropathy, and formalin-induced acute inflammatory pain in female mice [30]. Further research found that IL-23 promoted IL-17A release from macrophages, activating C-fiber nociceptors and TRPV1 to produce mechanical pain in females in the presence of ERα. In addition, intraplantar IL-23 could potentiate blue light-induced pain in females, and intrathecal injection of IL-23 could potentiate low-dose capsaicin-induced spontaneous pain in female but not male mice [31]. In cancer-induced bone pain, treatment with IL-17A antibody in the spinal cord of female rats could also inhibit cancer-induced mechanical allodynia and thermal hyperalgesia [93]. These indicate the importance of IL-23/IL-23R or IL-23/IL-17 axis in generating female-specific mechanical allodynia.
Figure 3.
The role of IL-23/IL-17 in chronic pain from studies using females only or both sexes. Abbreviations: CCL17, C-C motif ligand 17; COX, cyclooxygenase; DRG, dorsal root ganglion; ERα, estrogen receptor α; GM-CSF, granulocyte macrophage-colony stimulating factor; ICS, intermittent cold stress; LTTL gel, gel Long-Teng-Tong-Luo; MOG35–55, myelin oligodendrocyte glycoprotein peptide 35–55; MS, multiple sclerosis; PI3K, phosphatidylinositol 3-kinase; SC, spinal cord; TNF, tumor necrosis factor; TRPV1, transient receptor potential vanilloid 1.
In fibromyalgia induced by ICS, electroacupuncture treatment and TRPV1 deletion decreased IL-17 and IL-17-related signaling pathways (PI3K/Akt, p38, JNK, NF-κB) levels in somatosensory cortex and cerebellum lobe V–VII in female mice and reduced heat and mechanical hyperalgesia [84], indicating the role of IL-17 in electroacupuncture-treated fibromyalgia in females.
In MOG35–55-induced MS, spinal CaMKIIα activity was enhanced in female mice, and CaMKIIα inhibitor or siRNA attenuated mechanical allodynia and thermal hyperalgesia [94]. Further research found that IL-17 induced the occurrence but not the development of mechanical allodynia and thermal hyperalgesia in the MS model, and CaMKIIα was found to participate in IL-17-mediated hyperalgesia by using a CaMKIIα inhibitor. These suggest that IL-17 can promote the occurrence of MS-associated chronic pain by improving CaMKIIα activation in females.
In addition, approximately 60–90% of individuals with psoriasis suffer from pruritus and neuropathic pain in the lesions [137,138]. The IL-23/Th17 immune axis was found to play an important role in the development of psoriasis [139]. However, no preclinical study found the role of IL-23/IL-17 in psoriasis-associated pain. Clinical trials reported that IL-23p19 neutralizing antibody, guselkumab, could reduce the physical component score that includes the bodily pain score of patients with psoriasis [140,141,142]. Psoriasis is a chronic systemic inflammatory cutaneous disease. The psychoneurological system is also influenced during the development of psoriasis [143]. IL-23/IL-17 may participate in psoriasis-associated pain through inflammation. However, the roles and mechanisms of IL23/IL-17 in psoriasis-induced pain need to be explored in females or males.
4.5. IL-33
IL-33, another member of the IL-1 family, is mainly produced by monocytes/macrophages [144]. It uses a receptor complex of ST2 (IL-1 receptor-like 1) and IL-1 receptor accessory protein for its receptor to participate in the inflammatory process [145]. IL-33 is regulated by sexual hormones [146]. In addition, IL-33 can also participate in menopause-induced bone loss in females [146]. Neutralizing antibody to IL-33 is effective for the treatment of endometriosis [147].
In both male and female mice, IL-33 intraplantar injection could induce mechanical hypernociception, and inhibition of TNF-α, CXCL1, or IL-1β reduced IL-33-induced mechanical allodynia [96] (Table 1). Another study explored the regulatory mechanism between IL-33 and these proinflammatory factors [95]. The IL-33/TNFα/IL-1β/IFNγ/endothelin 1-prostaglandin (PG) E2 signaling cascade was found to participate in antigen-induced cutaneous and articular hypernociception. These indicate that IL-33 in both males and females may enjoy a similar mechanism in chronic pain.
4.6. IL-10
IL-10 is a key anti-inflammatory cytokine, which can repress proinflammatory responses and limit unnecessary tissue inflammatory disruptions by binding to the IL-10 receptor [148,149]. IL-10 is produced by macrophages, myeloid dendritic cells, and neutrophils [150]. Sexual hormones can influence the production of IL-10 [151,152]. In the nervous system, LPS stimulation could result in different degrees of cytokine production. Astrocytes of female mice produced less IL-10, compared to those of males [153]. However, the inhibition of female hormones on IL-10 production, IL-10-deficient female mice, but not male mice, displayed increased depressive-like behavior [154], suggesting that the inhibition of female hormones on IL-10 production does not mean the unimportance role of IL-10 in females.
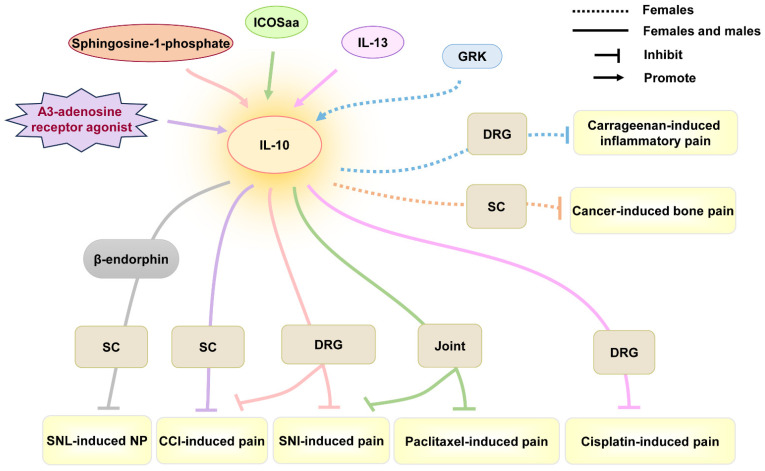
In an anti-inflammatory role, IL-10 has been widely validated in chronic pain. In male and female mice, A3-adenosine receptor agonists promoted CD4+ T cells in DRG to release IL-10, reversing mechano-allodynia induced by CCI [97]. Sphingosine-1-phosphate antagonists could promote IL-10 production of astrocytes in the spinal cord, attenuating and reversing neuropathic pain induced by CCI or SNI in both female and male mice [98]. Similarly, IL-10 reversed spinal abnormal synaptic plasticity of female and male rats through increasing β-endorphin expression in microglia, contributing to the inhibition of hypersensitivity activity in neuropathic pain induced by spinal nerve ligation (SNL) [99]. In chemotherapy-induced pain, IL-13 produced by CD8+ T cells promoted IL-10 release in macrophages of DRG, ameliorating cisplatin-induced mechanical allodynia in both male and female mice [62]. These suggest the anti-inflammatory effect of IL-10 in both sexes (Table 1 and Figure 4). However, the efficiency of IL-10 may be different between the two sexes. Inducible co-stimulatory molecule agonist antibody (ICOSaa) alleviated mechanical hypersensitivity in paclitaxel-induced pain by recruiting IL-10-producing T cells, but ICOSaa applied in female mice showed a more effective pharmacological effect [100]. In addition, intrathecal IL-10 could effectively reduce cancer-induced bone pain behavior in female rats, in a dose-dependent manner [63]. IL-10 produced by peripheral monocytes/macrophages in DRG promoted the resolution of carrageenan-induced mechanical allodynia and thermal hyperalgesia in female mice [101]. Thus, IL-10 can alleviate the development of chronic pain, though slight differences caused by sex differences.
Figure 4.
The role of IL-10 in chronic pain from studies using females only or both sexes. Abbreviations: CCI, chronic constriction injury; DRG, dorsal root ganglion; GRK, G-protein-coupled receptor kinase; ICOSaa, inducible co-stimulatory molecule agonist antibody; NP, neuropathic pain; SC, spinal cord; SNI, sciatic nerve injury; SNL, spinal nerve ligation.
IL-10 was also found to play an anti-inflammation role in MS by decreasing microglial activation, T-cell proliferation, peripheral immune cell infiltration, or IFN-γ secretion [155]. Plasmid construct coding for rat interleukin-10 (pDNA-IL-10F129S) could reduce mechanical allodynia in MS induced by MOG35–55 in male rats. However, the role of IL-10 in MS-associated pain in females needs to be explored. In addition, IL-10 was found to be increased during pharmacological therapy that inhibited pain-like behavior in osteoarthritis in female or male rats [156,157]. Thus, the role of IL-10 in autoimmune disease-associated chronic pain needs to be further explored.
4.7. IL-35
IL-35 is another anti-inflammatory effector cytokine, which plays an immunosuppressive role. IL-35 is released by regulatory T cells, regulatory B cells, and tolerogenic dendritic cells [102]. IL-35 treatment could regulate microglia activation, reducing spinal neuroinflammation and alleviating diabetic neuropathic pain in male rats [158]. In CCI-induced neuropathic pain, intrathecal recombinant IL-35 treatment alleviated mechanical pain in male mice but not female mice [102]. Further research found that IL-35 could inhibit microglia activation in the spinal cord of males but not females, indicating that IL-35 can participate in CCI-induced neuropathic pain in males rather than females (Table 1). However, in MOG35–55-induced MS, IL-35 reduced mechanical allodynia and spontaneous pain and increased myelination of the nociceptive pathway in female mice [103]. Further research found that IL-35 upregulated IL-10 expression and reduced monocyte infiltration in the spinal cord, indicating that IL-35 can attenuate MS-associated pain in females by decreasing neuroinflammation and increasing myelination.
5. Therapeutic Strategy of IL Family
Some strategies have been applied to reverse the effects of the IL family, such as naturally occurring proteins, neutralizing antibodies, or recombinant receptor antagonists [159,160]. These treatments for the IL family in clinical trials showed outstanding therapeutic efficacy [159,160,161,162,163,164]. However, whether these treatments can exert their effects on chronic pain needs to be further explored. Currently, IL-6R inhibitors, such as olokizumab and sirukumab, have been used in efficacy studies in randomized phase III safety trials and demonstrated a significant superiority in primary efficacy outcome in rheumatoid arthritis, compared to the placebo group [165]. Clinical trials reported that IL-23p19 neutralizing antibody, guselkumab, could reduce the physical component score, including the bodily pain score, of patients with psoriasis [140,141,142]. Notably, drugs that target the IL-23/IL-17 pathway showed excellent efficacy for skin disease, efficacy for inflammatory bowel disease, and peripheral arthropathy associated with spondyloarthropathy [166]. However, the female sex increased the risk of drug discontinuation [135,167]. This makes the researchers pay more attention to the influence of sex in drug efficacy and side effects. In addition, preclinical studies showed that, in addition to ILs/IL-Rs itself invention, the upstream of the IL family should be taken into account for pain treatment [90,98,125,168]. However, females and males showed different IL reactivities in pain processing [123,124,169,170] and this review summarized the different effects of ILs in pain transmission in both sexes, especially in females (Table 1). Researchers should focus on sex differences during developing interventions and treatments for chronic pain.
6. The Change in Pain Threshold in Klinefelter Syndrome
Klinefelter syndrome (KS) is the most frequently observed chromosomal disorder in males [157]. The most common form of KS is the regular type (47, XXY), which accounts for 80% of all cases. The other common forms of KS are 47, XX and, der(Y), 47, X, der(X), Y,48, XXXY, 48, XXYY, 49, XXXXY, 47, XXY/46, and XY mosaicism. KS is generally characterized by tall stature, small testes, gynecomastia, and infertility. Serum analysis showed lower testosterone, and higher serum follicle-stimulating hormone and luteinizing hormone levels, which are accompanied by impaired spermatogenesis [171]. Sex hormones affect immune cells and responses, resulting in differences in immune cell compositions and functions in different sexes. Females generally mount stronger immune responses than males [172], and females are much more susceptible to autoimmune diseases. Thus, the additional X-chromosomes make males with KS to develop autoimmune diseases, such as systemic lupus erythematosus, as frequently as women [172,173,174,175]. However, the effect of this type of X chromosome aneuploidies on pain threshold is unclear. Recent clinical research found that, at 30, 60, and 90th min after surgery, visual analog scale pain scores of males with KS were higher than those of males with a normal karyotype [176], indicating that males with KS are more sensitive to painful stimuli. However, the role of KS in chronic pain needs to be further explored.
7. Conclusions
Neuroinflammation plays an important role in pain plasticity, and the IL family plays a crucial regulatory role in this process. Recently, the impact of sex differences on pain processing has been increasingly recognized. Sex and sex hormones can regulate IL production and reactivity. This review summarizes the impacts of sex differences on IL family regulation in chronic pain. The roles and mechanisms of some ILs in chronic pain are different in males and females. In addition, the different causes of chronic pain can influence the effects of ILs in the same sex. These provide insights and considerations for the development of precise therapeutic drugs for chronic pain.
Author Contributions
J.L.: Writing—original draft, writing—review and editing, visualization, conceptualization, funding acquisition. Z.L.: writing—review and editing, visualization. J.J.: validation, supervision. T.C.: validation, supervision. F.G.: writing—review and editing, visualization, validation, supervision, resources, project administration, funding acquisition, and conceptualization. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
This work was supported by the National Natural Science Foundation of China (NSFC) (Grant no. 81974168 and 82101308).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Kennedy J., Roll J.M., Schraudner T., Murphy S., McPherson S. Prevalence of persistent pain in the U.S. adult population: New data from the 2010 national health interview survey. J. Pain. 2014;15:979–984. doi: 10.1016/j.jpain.2014.05.009. [DOI] [PubMed] [Google Scholar]
- 2.Goldberg D.S., McGee S.J. Pain as a global public health priority. BMC Public Health. 2011;11:770. doi: 10.1186/1471-2458-11-770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.van Hecke O., Austin S.K., Khan R.A., Smith B.H., Torrance N. Neuropathic pain in the general population: A systematic review of epidemiological studies. Pain. 2014;155:654–662. doi: 10.1016/j.pain.2013.11.013. [DOI] [PubMed] [Google Scholar]
- 4.Hamood R., Hamood H., Merhasin I., Keinan-Boker L. Chronic pain and other symptoms among breast cancer survivors: Prevalence, predictors, and effects on quality of life. Breast Cancer Res. Treat. 2018;167:157–169. doi: 10.1007/s10549-017-4485-0. [DOI] [PubMed] [Google Scholar]
- 5.Guan X.H., Fu Q.C., Shi D., Bu H.L., Song Z.P., Xiong B.R., Shu B., Xiang H.B., Xu B., Manyande A., et al. Activation of spinal chemokine receptor CXCR3 mediates bone cancer pain through an Akt-ERK crosstalk pathway in rats. Exp. Neurol. 2015;263:39–49. doi: 10.1016/j.expneurol.2014.09.019. [DOI] [PubMed] [Google Scholar]
- 6.Li Z., Li X., Jian W., Xue Q., Liu Z. Roles of Long Non-coding RNAs in the Development of Chronic Pain. Front. Mol. Neurosci. 2021;14:760964. doi: 10.3389/fnmol.2021.760964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Glare P., Aubrey K.R., Myles P.S. Transition from acute to chronic pain after surgery. Lancet. 2019;393:1537–1546. doi: 10.1016/S0140-6736(19)30352-6. [DOI] [PubMed] [Google Scholar]
- 8.Liu Z.Y., Song Z.W., Guo S.W., He J.S., Wang S.Y., Zhu J.G., Yang H.L., Liu J.B. CXCL12/CXCR4 signaling contributes to neuropathic pain via central sensitization mechanisms in a rat spinal nerve ligation model. CNS Neurosci. Ther. 2019;25:922–936. doi: 10.1111/cns.13128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fonseca M.M., Davoli-Ferreira M., Santa-Cecília F., Guimarães R.M., Oliveira F.F.B., Kusuda R., Ferreira D.W., Alves-Filho J.C., Cunha F.Q., Cunha T.M. IL-27 Counteracts Neuropathic Pain Development Through Induction of IL-10. Front. Immunol. 2019;10:3059. doi: 10.3389/fimmu.2019.03059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mogil J.S., Chanda M.L. The case for the inclusion of female subjects in basic science studies of pain. Pain. 2005;117:1–5. doi: 10.1016/j.pain.2005.06.020. [DOI] [PubMed] [Google Scholar]
- 11.Mogil J.S. Qualitative sex differences in pain processing: Emerging evidence of a biased literature. Nat. Rev. Neurosci. 2020;21:353–365. doi: 10.1038/s41583-020-0310-6. [DOI] [PubMed] [Google Scholar]
- 12.Buse D.C., Loder E.W., Gorman J.A., Stewart W.F., Reed M.L., Fanning K.M., Serrano D., Lipton R.B. Sex differences in the prevalence, symptoms, and associated features of migraine, probable migraine and other severe headache: Results of the American Migraine Prevalence and Prevention (AMPP) Study. Headache. 2013;53:1278–1299. doi: 10.1111/head.12150. [DOI] [PubMed] [Google Scholar]
- 13.Fillingim R.B., King C.D., Ribeiro-Dasilva M.C., Rahim-Williams B., Riley J.L., 3rd Sex, gender, and pain: A review of recent clinical and experimental findings. J. Pain. 2009;10:447–485. doi: 10.1016/j.jpain.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mogil J.S. Sex differences in pain and pain inhibition: Multiple explanations of a controversial phenomenon. Nat. Rev. Neurosci. 2012;13:859–866. doi: 10.1038/nrn3360. [DOI] [PubMed] [Google Scholar]
- 15.Chesterton L.S., Barlas P., Foster N.E., Baxter D.G., Wright C.C. Gender differences in pressure pain threshold in healthy humans. Pain. 2003;101:259–266. doi: 10.1016/S0304-3959(02)00330-5. [DOI] [PubMed] [Google Scholar]
- 16.Frot M., Feine J.S., Bushnell C.M. Sex differences in pain perception and anxiety. A psychophysical study with topical capsaicin. Pain. 2004;108:230–236. doi: 10.1016/j.pain.2003.11.017. [DOI] [PubMed] [Google Scholar]
- 17.Sarlani E., Farooq N., Greenspan J.D. Gender and laterality differences in thermosensation throughout the perceptible range. Pain. 2003;106:9–18. doi: 10.1016/S0304-3959(03)00211-2. [DOI] [PubMed] [Google Scholar]
- 18.Vignali D.A., Kuchroo V.K. IL-12 family cytokines: Immunological playmakers. Nat. Immunol. 2012;13:722–728. doi: 10.1038/ni.2366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li J., Huang L., Zhao H., Yan Y., Lu J. The Role of Interleukins in Colorectal Cancer. Int. J. Biol. Sci. 2020;16:2323–2339. doi: 10.7150/ijbs.46651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Salvador A.F., de Lima K.A., Kipnis J. Neuromodulation by the immune system: A focus on cytokines. Nat. Rev. Immunol. 2021;21:526–541. doi: 10.1038/s41577-021-00508-z. [DOI] [PubMed] [Google Scholar]
- 21.Buchheit T., Huh Y., Maixner W., Cheng J., Ji R.R. Neuroimmune modulation of pain and regenerative pain medicine. J. Clin. Investig. 2020;130:2164–2176. doi: 10.1172/JCI134439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Binshtok A.M., Wang H., Zimmermann K., Amaya F., Vardeh D., Shi L., Brenner G.J., Ji R.R., Bean B.P., Woolf C.J., et al. Nociceptors are interleukin-1beta sensors. J. Neurosci. 2008;28:14062–14073. doi: 10.1523/JNEUROSCI.3795-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Richter F., Natura G., Ebbinghaus M., von Banchet G.S., Hensellek S., König C., Bräuer R., Schaible H.G. Interleukin-17 sensitizes joint nociceptors to mechanical stimuli and contributes to arthritic pain through neuronal interleukin-17 receptors in rodents. Arthritis Rheum. 2012;64:4125–4134. doi: 10.1002/art.37695. [DOI] [PubMed] [Google Scholar]
- 24.Yan X., Li F., Maixner D.W., Yadav R., Gao M., Ali M.W., Hooks S.B., Weng H.R. Interleukin-1beta released by microglia initiates the enhanced glutamatergic activity in the spinal dorsal horn during paclitaxel-associated acute pain syndrome. Glia. 2019;67:482–497. doi: 10.1002/glia.23557. [DOI] [PubMed] [Google Scholar]
- 25.Edwards R.R., Kronfli T., Haythornthwaite J.A., Smith M.T., McGuire L., Page G.G. Association of catastrophizing with interleukin-6 responses to acute pain. Pain. 2008;140:135–144. doi: 10.1016/j.pain.2008.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Luo H., Liu H.Z., Zhang W.W., Matsuda M., Lv N., Chen G., Xu Z.Z., Zhang Y.Q. Interleukin-17 Regulates Neuron-Glial Communications, Synaptic Transmission, and Neuropathic Pain after Chemotherapy. Cell Rep. 2019;29:2384–2397.e5. doi: 10.1016/j.celrep.2019.10.085. [DOI] [PubMed] [Google Scholar]
- 27.Kruse J.L., Olmstead R., Hellemann G., Breen E.C., Tye S.J., Brooks J.O., 3rd, Wade B., Congdon E., Espinoza R., Narr K.L., et al. Interleukin-8 and lower severity of depression in females, but not males, with treatment-resistant depression. J. Psychiatr. Res. 2021;140:350–356. doi: 10.1016/j.jpsychires.2021.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mouihate A., Kalakh S. Maternal Interleukin-6 Hampers Hippocampal Neurogenesis in Adult Rat Offspring in a Sex-Dependent Manner. Dev. Neurosci. 2021;43:106–115. doi: 10.1159/000516370. [DOI] [PubMed] [Google Scholar]
- 29.Keckstein S., Pritz S., Amann N., Meister S., Beyer S., Jegen M., Kuhn C., Hutter S., Knabl J., Mahner S., et al. Sex Specific Expression of Interleukin 7, 8 and 15 in Placentas of Women with Gestational Diabetes. Int. J. Mol. Sci. 2020;21:8026. doi: 10.3390/ijms21218026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Luo X., Chen O., Wang Z., Bang S., Ji J., Lee S.H., Huh Y., Furutani K., He Q., Tao X., et al. IL-23/IL-17A/TRPV1 axis produces mechanical pain via macrophage-sensory neuron crosstalk in female mice. Neuron. 2021;109:2691–2706.e5. doi: 10.1016/j.neuron.2021.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ji J., He Q., Luo X., Bang S., Matsuoka Y., McGinnis A., Nackley A.G., Ji R.R. IL-23 Enhances C-Fiber-Mediated and Blue Light-Induced Spontaneous Pain in Female Mice. Front. Immunol. 2021;12:787565. doi: 10.3389/fimmu.2021.787565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Craft R.M. Modulation of pain by estrogens. Pain. 2007;132((Suppl. S1)):S3–S12. doi: 10.1016/j.pain.2007.09.028. [DOI] [PubMed] [Google Scholar]
- 33.Ren K., Wei F., Dubner R., Murphy A., Hoffman G.E. Progesterone attenuates persistent inflammatory hyperalgesia in female rats: Involvement of spinal NMDA receptor mechanisms. Brain Res. 2000;865:272–277. doi: 10.1016/S0006-8993(00)02267-8. [DOI] [PubMed] [Google Scholar]
- 34.Hau M., Dominguez O.A., Evrard H.C. Testosterone reduces responsiveness to nociceptive stimuli in a wild bird. Horm. Behav. 2004;46:165–170. doi: 10.1016/j.yhbeh.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 35.Stoffel E.C., Ulibarri C.M., Folk J.E., Rice K.C., Craft R.M. Gonadal hormone modulation of mu, kappa, and delta opioid antinociception in male and female rats. J. Pain. 2005;6:261–274. doi: 10.1016/j.jpain.2004.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kuba T., Wu H.B., Nazarian A., Festa E.D., Barr G.A., Jenab S., Inturrisi C.E., Quinones-Jenab V. Estradiol and progesterone differentially regulate formalin-induced nociception in ovariectomized female rats. Horm. Behav. 2006;49:441–449. doi: 10.1016/j.yhbeh.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 37.Nag S., Mokha S.S. Testosterone is essential for alpha(2)-adrenoceptor-induced antinociception in the trigeminal region of the male rat. Neurosci. Lett. 2009;467:48–52. doi: 10.1016/j.neulet.2009.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Thompson A.D., Angelotti T., Nag S., Mokha S.S. Sex-specific modulation of spinal nociception by alpha2-adrenoceptors: Differential regulation by estrogen and testosterone. Neurosci. 2008;153:1268–1277. doi: 10.1016/j.neuroscience.2008.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lawson K.P., Nag S., Thompson A.D., Mokha S.S. Sex-specificity and estrogen-dependence of kappa opioid receptor-mediated antinociception and antihyperalgesia. Pain. 2010;151:806–815. doi: 10.1016/j.pain.2010.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chen Q., Zhang W., Sadana N., Chen X. Estrogen receptors in pain modulation: Cellular signaling. Biol. Sex Differ. 2021;12:22. doi: 10.1186/s13293-021-00364-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ma J.N., McFarland K., Olsson R., Burstein E.S. Estrogen Receptor Beta Selective Agonists as Agents to Treat Chemotherapeutic-Induced Neuropathic Pain. ACS Chem. Neurosci. 2016;7:1180–1187. doi: 10.1021/acschemneuro.6b00183. [DOI] [PubMed] [Google Scholar]
- 42.Li L., Fan X., Warner M., Xu X.J., Gustafsson J.A., Wiesenfeld-Hallin Z. Ablation of estrogen receptor alpha or beta eliminates sex differences in mechanical pain threshold in normal and inflamed mice. Pain. 2009;143:37–40. doi: 10.1016/j.pain.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 43.Alexander S.N., Green A.R., Debner E.K., Ramos Freitas L.E., Abdelhadi H.M.K., Szabo-Pardi T.A., Burton M.D. The influence of sex on neuroimmune communication, pain, and physiology. Biol. Sex Differ. 2024;15:82. doi: 10.1186/s13293-024-00660-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Papka R.E., Storey-Workley M., Shughrue P.J., Merchenthaler I., Collins J.J., Usip S., Saunders P.T., Shupnik M. Estrogen receptor-alpha and beta-immunoreactivity and mRNA in neurons of sensory and autonomic ganglia and spinal cord. Cell Tissue Res. 2001;304:193–214. doi: 10.1007/s004410100363. [DOI] [PubMed] [Google Scholar]
- 45.Shughrue P.J., Lane M.V., Merchenthaler I. Comparative distribution of estrogen receptor-alpha and -beta mRNA in the rat central nervous system. J. Comp. Neurol. 1997;388:507–525. doi: 10.1002/(SICI)1096-9861(19971201)388:4<507::AID-CNE1>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 46.Verdi J., Jafari-Sabet M., Mokhtari R., Mesdaghinia A., Banafshe H.R. The effect of progesterone on expression and development of neuropathic pain in a rat model of peripheral neuropathy. Eur. J. Pharmacol. 2013;699:207–212. doi: 10.1016/j.ejphar.2012.11.052. [DOI] [PubMed] [Google Scholar]
- 47.Claiborne J., Nag S., Mokha S.S. Activation of opioid receptor like-1 receptor in the spinal cord produces sex-specific antinociception in the rat: Estrogen attenuates antinociception in the female, whereas testosterone is required for the expression of antinociception in the male. J. Neurosci. 2006;26:13048–13053. doi: 10.1523/JNEUROSCI.4783-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sommer C., Leinders M., Üçeyler N. Inflammation in the pathophysiology of neuropathic pain. Pain. 2018;159:595–602. doi: 10.1097/j.pain.0000000000001122. [DOI] [PubMed] [Google Scholar]
- 49.Watson P.A., Arora V.K., Sawyers C.L. Emerging mechanisms of resistance to androgen receptor inhibitors in prostate cancer. Nature reviews. Cancer. 2015;15:701–711. doi: 10.1038/nrc4016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Li F., Xing X., Jin Q., Wang X.M., Dai P., Han M., Shi H., Zhang Z., Shao X., Peng Y., et al. Sex differences orchestrated by androgens at single-cell resolution. Nature. 2024;629:193–200. doi: 10.1038/s41586-024-07291-6. [DOI] [PubMed] [Google Scholar]
- 51.Zhao T.Z., Ding Q., Hu J., He S.M., Shi F., Ma L.T. GPER expressed on microglia mediates the anti-inflammatory effect of estradiol in ischemic stroke. Brain Behav. 2016;6:e00449. doi: 10.1002/brb3.449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wang J., Hou Y., Zhang L., Liu M., Zhao J., Zhang Z., Ma Y., Hou W. Estrogen Attenuates Traumatic Brain Injury by Inhibiting the Activation of Microglia and Astrocyte-Mediated Neuroinflammatory Responses. Mol. Neurobiol. 2021;58:1052–1061. doi: 10.1007/s12035-020-02171-2. [DOI] [PubMed] [Google Scholar]
- 53.Takahashi T., Iwasaki A. Sex differences in immune responses. Science. 2021;371:347–348. doi: 10.1126/science.abe7199. [DOI] [PubMed] [Google Scholar]
- 54.Xia J., Wang H., Zhang C., Liu B., Li Y., Li K., Li P., Song C. The comparison of sex differences in depression-like behaviors and neuroinflammatory changes in a rat model of depression induced by chronic stress. Front. Behav. Neurosci. 2022;16:1059594. doi: 10.3389/fnbeh.2022.1059594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Parekh S.V., Adams L.O., Barkell G.A., Lysle D.T. Sex-differences in anxiety, neuroinflammatory markers, and enhanced fear learning following chronic heroin withdrawal. Psychopharmacology. 2023;240:347–359. doi: 10.1007/s00213-023-06310-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Barnard D.F., Gabella K.M., Kulp A.C., Parker A.D., Dugan P.B., Johnson J.D. Sex differences in the regulation of brain IL-1β in response to chronic stress. Psychoneuroendocrinology. 2019;103:203–211. doi: 10.1016/j.psyneuen.2019.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Alonaizan R., Alotaibi W.K., Alsulami A., Alkhulaifi F.M., Alomar S. Sex-Differences Influence Depressive-Like Behaviour via Alterations in Microglial Expression of GIF-1, TREM2, and IL-1β in an Acute Lipopolysaccharide-Induced Murine Neuroinflammation Model. Immunol. Investig. 2025;54:317–333. doi: 10.1080/08820139.2024.2440006. [DOI] [PubMed] [Google Scholar]
- 58.Scholz J., Finnerup N.B., Attal N., Aziz Q., Baron R., Bennett M.I., Benoliel R., Cohen M., Cruccu G., Davis K.D., et al. The IASP classification of chronic pain for ICD-11: Chronic neuropathic pain. Pain. 2019;160:53–59. doi: 10.1097/j.pain.0000000000001365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Treede R.D., Rief W., Barke A., Aziz Q., Bennett M.I., Benoliel R., Cohen M., Evers S., Finnerup N.B., First M.B., et al. Chronic pain as a symptom or a disease: The IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11) Pain. 2019;160:19–27. doi: 10.1097/j.pain.0000000000001384. [DOI] [PubMed] [Google Scholar]
- 60.Shao Q., Li Y., Wang Q., Zhao J. IL-10 and IL-1β mediate neuropathic-pain like behavior in the ventrolateral orbital cortex. Neurochem. Res. 2015;40:733–739. doi: 10.1007/s11064-015-1521-5. [DOI] [PubMed] [Google Scholar]
- 61.Mailhot B., Christin M., Tessandier N., Sotoudeh C., Bretheau F., Turmel R., Pellerin È., Wang F., Bories C., Joly-Beauparlant C., et al. Neuronal interleukin-1 receptors mediate pain in chronic inflammatory diseases. J. Exp. Med. 2020;217:e20191430. doi: 10.1084/jem.20191430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Singh S.K., Krukowski K., Laumet G.O., Weis D., Alexander J.F., Heijnen C.J., Kavelaars A. CD8+ T cell-derived IL-13 increases macrophage IL-10 to resolve neuropathic pain. JCI Insight. 2022;7:e154194. doi: 10.1172/jci.insight.154194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kim W.M., Jeong C.W., Lee S.H., Kim Y.O., Cui J.H., Yoon M.H. The intrathecally administered kappa-2 opioid agonist GR89696 and interleukin-10 attenuate bone cancer-induced pain through synergistic interaction. Anesth. Analg. 2011;113:934–940. doi: 10.1213/ANE.0b013e318227824e. [DOI] [PubMed] [Google Scholar]
- 64.Helyes Z., Tékus V., Szentes N., Pohóczky K., Botz B., Kiss T., Kemény Á., Környei Z., Tóth K., Lénárt N., et al. Transfer of complex regional pain syndrome to mice via human autoantibodies is mediated by interleukin-1-induced mechanisms. Proc. Natl. Acad. Sci. USA. 2019;116:13067–13076. doi: 10.1073/pnas.1820168116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mirabelli E., Ni L., Li L., Acioglu C., Heary R.F., Elkabes S. Pathological pain processing in mouse models of multiple sclerosis and spinal cord injury: Contribution of plasma membrane calcium ATPase 2 (PMCA2) J. Neuroinflammation. 2019;16:207. doi: 10.1186/s12974-019-1585-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Li L., Li T., Qu X., Sun G., Fu Q., Han G. Stress/cell death pathways, neuroinflammation, and neuropathic pain. Immunol. Rev. 2024;321:33–51. doi: 10.1111/imr.13275. [DOI] [PubMed] [Google Scholar]
- 67.Vergne-Salle P., Bertin P. Chronic pain and neuroinflammation. Jt. Bone Spine. 2021;88:105222. doi: 10.1016/j.jbspin.2021.105222. [DOI] [PubMed] [Google Scholar]
- 68.Hung A.L., Lim M., Doshi T.L. Targeting cytokines for treatment of neuropathic pain. Scand. J. Pain. 2017;17:287–293. doi: 10.1016/j.sjpain.2017.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Jiang X., Zhou R., Zhang Y., Zhu T., Li Q., Zhang W. Interleukin-17 as a potential therapeutic target for chronic pain. Front. Immunol. 2022;13:999407. doi: 10.3389/fimmu.2022.999407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zhou Y.Q., Liu Z., Liu Z.H., Chen S.P., Li M., Shahveranov A., Ye D.W., Tian Y.K. Interleukin-6: An emerging regulator of pathological pain. J. Neuroinflamm. 2016;13:141. doi: 10.1186/s12974-016-0607-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pillarisetti S. Targeting interleukin-1β for pain. CNS Neurol. Disord. Drug Targets. 2011;10:571–575. doi: 10.2174/187152711796234998. [DOI] [PubMed] [Google Scholar]
- 72.Ju J., Li Z., Jia X., Peng X., Wang J., Gao F. Interleukin-18 in chronic pain: Focus on pathogenic mechanisms and potential therapeutic targets. Pharmacol. Res. 2024;201:107089. doi: 10.1016/j.phrs.2024.107089. [DOI] [PubMed] [Google Scholar]
- 73.Lee K.M., Sherlock J.P., Hamilton J.A. The role of interleukin (IL)-23 in regulating pain in arthritis. Arthritis Res. Ther. 2022;24:89. doi: 10.1186/s13075-022-02777-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Milligan E.D., Penzkover K.R., Soderquist R.G., Mahoney M.J. Spinal interleukin-10 therapy to treat peripheral neuropathic pain. Neuromodulation. 2012;15:520–526, discussion 6. doi: 10.1111/j.1525-1403.2012.00462.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Li P., Yu Q., Nie H., Yin C., Liu B. IL-33/ST2 signaling in pain and itch: Cellular and molecular mechanisms and therapeutic potentials. Biomed. Pharmacother. 2023;165:115143. doi: 10.1016/j.biopha.2023.115143. [DOI] [PubMed] [Google Scholar]
- 76.Liao Y., Ren Y., Luo X., Mirando A.J., Long J.T., Leinroth A., Ji R.R., Hilton M.J. Interleukin-6 signaling mediates cartilage degradation and pain in posttraumatic osteoarthritis in a sex-specific manner. Sci. Signal. 2022;15:eabn7082. doi: 10.1126/scisignal.abn7082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chen G., Luo X., Qadri M.Y., Berta T., Ji R.R. Sex-Dependent Glial Signaling in Pathological Pain: Distinct Roles of Spinal Microglia and Astrocytes. Neurosci. Bull. 2018;34:98–108. doi: 10.1007/s12264-017-0145-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sorge R.E., Mapplebeck J.C., Rosen S., Beggs S., Taves S., Alexander J.K., Martin L.J., Austin J.S., Sotocinal S.G., Chen D., et al. Different immune cells mediate mechanical pain hypersensitivity in male and female mice. Nat. Neurosci. 2015;18:1081–1083. doi: 10.1038/nn.4053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sorge R.E., Mapplebeck J.C., Rosen S., Beggs S., Taves S., Alexander J.K., Martin L.J., Austin J.S., Sotocinal S.G., Chen D., et al. Interleukin-1beta and inflammasome expression in spinal cord following chronic constriction injury in male and female rats. Brain Behav. Immun. 2024;115:157–168. doi: 10.1016/j.bbi.2023.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Khariv V., Ni L., Ratnayake A., Sampath S., Lutz B.M., Tao X.X., Heary R.F., Elkabes S. Impaired sensitivity to pain stimuli in plasma membrane calcium ATPase 2 (PMCA2) heterozygous mice: A possible modality-and sex-specific role for PMCA2 in nociception. FASEB J. 2017;31:224–237. doi: 10.1096/fj.201600541r. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Feng H.N., Zhong L.Q., Xu C.X., Wang T.T., Wu H., Wang L., Traub R.J., Chen X., Cao D.Y. Up-regulation of IL-1β and sPLA2-III in the medial prefrontal cortex contributes to orofacial and somatic hyperalgesia induced by malocclusion via glial-neuron crosstalk. Eur. J. Pharmacol. 2024;982:176933. doi: 10.1016/j.ejphar.2024.176933. [DOI] [PubMed] [Google Scholar]
- 82.AboTaleb H.A., Alturkistani H.A., Abd El-Aziz G.S., Hindi E.A., Halawani M.M., Al-Thepyani M.A., Alghamdi B.S. The Antinociceptive Effects and Sex-Specific Neurotransmitter Modulation of Metformin in a Mouse Model of Fibromyalgia. Cells. 2024;13:1986. doi: 10.3390/cells13231986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hu Z., Deng N., Liu K., Zhou N., Sun Y., Zeng W. CNTF-STAT3-IL-6 Axis Mediates Neuroinflammatory Cascade across Schwann Cell-Neuron-Microglia. Cell Rep. 2020;31:107657. doi: 10.1016/j.celrep.2020.107657. [DOI] [PubMed] [Google Scholar]
- 84.Yeh Y.A., Liao H.Y., Hsiao I.H., Hsu H.C., Lin Y.W. Electroacupuncture Reduced Fibromyalgia-Pain-like Behavior through Inactivating Transient Receptor Potential V1 and Interleukin-17 in Intermittent Cold Stress Mice Model. Brain Sci. 2024;14:869. doi: 10.3390/brainsci14090869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wakabayashi H., Kato S., Nagao N., Miyamura G., Naito Y., Sudo A. Interleukin-6 Inhibitor Suppresses Hyperalgesia Without Improvement in Osteoporosis in a Mouse Pain Model of Osteoporosis. Calcif. Tissue Int. 2019;104:658–666. doi: 10.1007/s00223-019-00521-4. [DOI] [PubMed] [Google Scholar]
- 86.Ochoa Bernal M.A., Song Y., Joshi N., Burns G.W., Paul E.N., Vegter E., Hrbek S., Sempere L.F., Fazleabas A.T. The Regulation of MicroRNA-21 by Interleukin-6 and Its Role in the Development of Fibrosis in Endometriotic Lesions. Int. J. Mol. Sci. 2024;25:8994. doi: 10.3390/ijms25168994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Fang D., Kong L.Y., Cai J., Li S., Liu X.D., Han J.S., Xing G.G. Interleukin-6-mediated functional upregulation of TRPV1 receptors in dorsal root ganglion neurons through the activation of JAK/PI3K signaling pathway: Roles in the development of bone cancer pain in a rat model. Pain. 2015;156:1124–1144. doi: 10.1097/j.pain.0000000000000158. [DOI] [PubMed] [Google Scholar]
- 88.Serizawa K., Tomizawa-Shinohara H., Magi M., Yogo K., Matsumoto Y. Anti-IL-6 receptor antibody improves pain symptoms in mice with experimental autoimmune encephalomyelitis. J. Neuroimmunol. 2018;319:71–79. doi: 10.1016/j.jneuroim.2018.03.017. [DOI] [PubMed] [Google Scholar]
- 89.Baggio D.F., da Luz F.M.R., Lopes R.V., Ferreira L.E.N., Araya E.I., Chichorro J.G. Sex Dimorphism in Resolvin D5-induced Analgesia in Rat Models of Trigeminal Pain. J. Pain. 2023;24:717–729. doi: 10.1016/j.jpain.2022.12.013. [DOI] [PubMed] [Google Scholar]
- 90.Yang Y., Li H., Li T.T., Luo H., Gu X.Y., Lü N., Ji R.R., Zhang Y.Q. Delayed activation of spinal microglia contributes to the maintenance of bone cancer pain in female Wistar rats via P2X7 receptor and IL-18. J. Neurosci. 2015;35:7950–7963. doi: 10.1523/JNEUROSCI.5250-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Viatchenko-Karpinski V., Kong L., Weng H.R. Activation of microglial GPR109A alleviates thermal hyperalgesia in female lupus mice by suppressing IL-18 and glutamatergic synaptic activity. Glia. 2022;70:634–649. doi: 10.1002/glia.24130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Lee K.M., Zhang Z., Achuthan A., Fleetwood A.J., Smith J.E., Hamilton J.A., Cook A.D. IL-23 in arthritic and inflammatory pain development in mice. Arthritis Res. Ther. 2020;22:123. doi: 10.1186/s13075-020-02212-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wang J., Zhang R., Dong C., Jiao L., Xu L., Liu J., Wang Z., Lao L. Transient Receptor Potential Channel and Interleukin-17A Involvement in LTTL Gel Inhibition of Bone Cancer Pain in a Rat Model. Integr. Cancer Ther. 2015;14:381–393. doi: 10.1177/1534735415580677. [DOI] [PubMed] [Google Scholar]
- 94.Hu X., Huang F., Wang Z.J. CaMKIIα Mediates the Effect of IL-17 To Promote Ongoing Spontaneous and Evoked Pain in Multiple Sclerosis. J. Neurosci. 2018;38:232–244. doi: 10.1523/JNEUROSCI.2666-17.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Verri W.A., Jr., Guerrero A.T., Fukada S.Y., Valerio D.A., Cunha T.M., Xu D., Ferreira S.H., Liew F.Y., Cunha F.Q. IL-33 mediates antigen-induced cutaneous and articular hypernociception in mice. Proc. Natl. Acad. Sci. USA. 2008;105:2723–2728. doi: 10.1073/pnas.0712116105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zarpelon A.C., Cunha T.M., Alves-Filho J.C., Pinto L.G., Ferreira S.H., McInnes I.B., Xu D., Liew F.Y., Cunha F.Q., Verri W.A., Jr. IL-33/ST2 signalling contributes to carrageenin-induced innate inflammation and inflammatory pain: Role of cytokines, endothelin-1 and prostaglandin E2. Br. J. Pharmacol. 2013;169:90–101. doi: 10.1111/bph.12110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Durante M., Squillace S., Lauro F., Giancotti L.A., Coppi E., Cherchi F., Di Cesare Mannelli L., Ghelardini C., Kolar G., Wahlman C., et al. Adenosine A3 agonists reverse neuropathic pain via T cell-mediated production of IL-10. J. Clin. Investig. 2021;131:e139299. doi: 10.1172/JCI139299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Chen Z., Doyle T.M., Luongo L., Largent-Milnes T.M., Giancotti L.A., Kolar G., Squillace S., Boccella S., Walker J.K., Pendleton A., et al. Sphingosine-1-phosphate receptor 1 activation in astrocytes contributes to neuropathic pain. Proc. Natl. Acad. Sci. USA. 2019;116:10557–10562. doi: 10.1073/pnas.1820466116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ma L., Peng S., Wei J., Zhao M., Ahmad K.A., Chen J., Wang Y.X. Spinal microglial β-endorphin signaling mediates IL-10 and exenatide-induced inhibition of synaptic plasticity in neuropathic pain. CNS Neurosci. Ther. 2021;27:1157–1172. doi: 10.1111/cns.13694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Sankaranarayanan I., Tavares-Ferreira D., Mwirigi J.M., Mejia G.L., Burton M.D., Price T.J. Inducible co-stimulatory molecule (ICOS) alleviates paclitaxel-induced neuropathic pain via an IL-10-mediated mechanism in female mice. J. Neuroinflamm. 2023;20:32. doi: 10.1186/s12974-023-02719-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Willemen H.L., Eijkelkamp N., Garza Carbajal A., Wang H., Mack M., Zijlstra J., Heijnen C.J., Kavelaars A. Monocytes/Macrophages control resolution of transient inflammatory pain. J. Pain. 2014;15:496–506. doi: 10.1016/j.jpain.2014.01.491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Fiore N.T., Hayes J.P., Williams S.I., Moalem-Taylor G. Interleukin-35 alleviates neuropathic pain and induces an anti-inflammatory shift in spinal microglia in nerve-injured male mice. Brain Behav. Immun. 2024;122:287–300. doi: 10.1016/j.bbi.2024.07.043. [DOI] [PubMed] [Google Scholar]
- 103.Duffy S.S., Keating B.A., Perera C.J., Lees J.G., Tonkin R.S., Makker P.G.S., Carrive P., Butovsky O., Moalem-Taylor G. Regulatory T Cells and Their Derived Cytokine, Interleukin-35, Reduce Pain in Experimental Autoimmune Encephalomyelitis. J. Neurosci. 2019;39:2326–2346. doi: 10.1523/JNEUROSCI.1815-18.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Xiang H.C., Lin L.X., Hu X.F., Zhu H., Li H.P., Zhang R.Y., Hu L., Liu W.T., Zhao Y.L., Shu Y., et al. AMPK activation attenuates inflammatory pain through inhibiting NF-κB activation and IL-1β expression. J. Neuroinflamm. 2019;16:34. doi: 10.1186/s12974-019-1411-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Morishita M., Miyagi M., Iwamoto Y. Effects of sex hormones on production of interleukin-1 by human peripheral monocytes. J. Periodontol. 1999;70:757–760. doi: 10.1902/jop.1999.70.7.757. [DOI] [PubMed] [Google Scholar]
- 106.Pilat D., Rojewska E., Jurga A.M., Piotrowska A., Makuch W., Przewlocka B., Mika J. IL-1 receptor antagonist improves morphine and buprenorphine efficacy in a rat neuropathic pain model. Eur. J. Pharmacol. 2015;764:240–248. doi: 10.1016/j.ejphar.2015.05.058. [DOI] [PubMed] [Google Scholar]
- 107.Souter A.J., Garry M.G., Tanelian D.L. Spinal interleukin-1beta reduces inflammatory pain. Pain. 2000;86:63–68. doi: 10.1016/S0304-3959(99)00315-2. [DOI] [PubMed] [Google Scholar]
- 108.Wen Y., Fan X., Bu H., Ma L., Kong C., Huang C., Xu Y. Downregulation of lncRNA FIRRE relieved the neuropathic pain of female mice by suppressing HMGB1 expression. Mol. Cell. Biochem. 2021;476:841–852. doi: 10.1007/s11010-020-03949-7. [DOI] [PubMed] [Google Scholar]
- 109.Di Cesare Mannelli L., Micheli L., Cervetto C., Toti A., Lucarini E., Parisio C., Marcoli M., Ghelardini C. Neuronal alarmin IL-1α evokes astrocyte-mediated protective signals: Effectiveness in chemotherapy-induced neuropathic pain. Neurobiol. Dis. 2022;168:105716. doi: 10.1016/j.nbd.2022.105716. [DOI] [PubMed] [Google Scholar]
- 110.Mika J., Korostynski M., Kaminska D., Wawrzczak-Bargiela A., Osikowicz M., Makuch W., Przewlocki R., Przewlocka B. Interleukin-1 alpha has antiallodynic and antihyperalgesic activities in a rat neuropathic pain model. Pain. 2008;138:587–597. doi: 10.1016/j.pain.2008.02.015. [DOI] [PubMed] [Google Scholar]
- 111.Goebel A. Complex regional pain syndrome in adults. Rheumatology. 2011;50:1739–1750. doi: 10.1093/rheumatology/ker202. [DOI] [PubMed] [Google Scholar]
- 112.Queiroz L.P. Worldwide epidemiology of fibromyalgia. Curr. Pain Headache Rep. 2013;17:356. doi: 10.1007/s11916-013-0356-5. [DOI] [PubMed] [Google Scholar]
- 113.Garbers C., Rose-John S. Dissecting Interleukin-6 Classic-and Trans-Signaling in Inflammation and Cancer. Methods Mol. Biol. 2018;1725:127–140. doi: 10.1007/978-1-4939-7568-6_11. [DOI] [PubMed] [Google Scholar]
- 114.de Hooge A.S., van de Loo F.A., Bennink M.B., Arntz O.J., de Hooge P., van den Berg W.B. Male IL-6 gene knock out mice developed more advanced osteoarthritis upon aging. Osteoarthr. Cartil. 2005;13:66–73. doi: 10.1016/j.joca.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 115.Su C., Chen M., Huang H., Lin J. Testosterone enhances lipopolysaccharide-induced interleukin-6 and macrophage chemotactic protein-1 expression by activating the extracellular signal-regulated kinase 1/2/nuclear factor-κB signalling pathways in 3T3-L1 adipocytes. Mol. Med. Rep. 2015;12:696–704. doi: 10.3892/mmr.2015.3401. [DOI] [PubMed] [Google Scholar]
- 116.Jankord R., Turk J.R., Schadt J.C., Casati J., Ganjam V.K., Price E.M., Keisler D.H., Laughlin M.H. Sex difference in link between interleukin-6 and stress. Endocrinology. 2007;148:3758–3764. doi: 10.1210/en.2006-1650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Papadopoulos A.D., Wardlaw S.L. Testosterone suppresses the response of the hypothalamic-pituitary-adrenal axis to interleukin-6. Neuroimmunomodulation. 2000;8:39–44. doi: 10.1159/000026451. [DOI] [PubMed] [Google Scholar]
- 118.Elgellaie A., Thomas S.J., Kaelle J., Bartschi J., Larkin T. Pro-inflammatory cytokines IL-1α, IL-6 and TNF-α in major depressive disorder: Sex-specific associations with psychological symptoms. Eur. J. Neurosci. 2023;57:1913–1928. doi: 10.1111/ejn.15992. [DOI] [PubMed] [Google Scholar]
- 119.Miller V.M., Lawrence D.A., Coccaro G.A., Mondal T.K., Andrews K., Dreiem A., Seegal R.F. Sex effects of interleukin-6 deficiency on neuroinflammation in aged C57Bl/6 mice. Brain Res. 2010;1318:11–22. doi: 10.1016/j.brainres.2009.12.091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Silva C., Ines L.S., Nour D., Straub R.H., da Silva J.A. Differential male and female adrenal cortical steroid hormone and cortisol responses to interleukin-6 in humans. Ann. N. Y. Acad. Sci. 2002;966:68–72. doi: 10.1111/j.1749-6632.2002.tb04203.x. [DOI] [PubMed] [Google Scholar]
- 121.Serizawa K., Tomizawa-Shinohara H., Miyake S., Yogo K., Matsumoto Y. Interleukin-6: Evolving role in the management of neuropathic pain in neuroimmunological disorders. Inflamm. Regen. 2021;41:34. doi: 10.1186/s41232-021-00184-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Atzeni F., Nucera V., Masala I.F., Sarzi-Puttini P., Bonitta G. Il-6 Involvement in pain, fatigue and mood disorders in rheumatoid arthritis and the effects of Il-6 inhibitor sarilumab. Pharmacol. Res. 2019;149:104402. doi: 10.1016/j.phrs.2019.104402. [DOI] [PubMed] [Google Scholar]
- 123.Srikanth V.K., Fryer J.L., Zhai G., Winzenberg T.M., Hosmer D., Jones G. A meta-analysis of sex differences prevalence, incidence and severity of osteoarthritis. Osteoarthr. Cartil. 2005;13:769–781. doi: 10.1016/j.joca.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 124.Mun C.J., Letzen J.E., Nance S., Smith M.T., Khanuja H.S., Sterling R.S., Bicket M.C., Haythornthwaite J.A., Jamison R.N., Edwards R.R., et al. Sex Differences in Interleukin-6 Responses Over Time Following Laboratory Pain Testing Among Patients With Knee Osteoarthritis. J. Pain. 2020;21:731–741. doi: 10.1016/j.jpain.2019.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Liang T., Chen T., Qiu J., Gao W., Qiu X., Zhu Y., Wang X., Chen Y., Zhou H., Deng Z., et al. Inhibition of nuclear receptor RORα attenuates cartilage damage in osteoarthritis by modulating IL-6/STAT3 pathway. Cell Death Dis. 2021;12:886. doi: 10.1038/s41419-021-04170-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Makabe K., Okada H., Tachibana N., Ishikura H., Ito N., Tanaka M., Chijimatsu R., Terashima A., Yano F., Asaka M., et al. Baricitinib ameliorates inflammatory and neuropathic pain in collagen antibody-induced arthritis mice by modulating the IL-6/JAK/STAT3 pathway and CSF-1 expression in dorsal root ganglion neurons. Arthritis Res. Ther. 2024;26:121. doi: 10.1186/s13075-024-03354-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Mima Z., Wang K., Liang M., Wang Y., Liu C., Wei X., Luo F., Nie P., Chen X., Xu Y., et al. Blockade of JAK2 retards cartilage degeneration and IL-6-induced pain amplification in osteoarthritis. Int. Immunopharmacol. 2022;113:109340. doi: 10.1016/j.intimp.2022.109340. [DOI] [PubMed] [Google Scholar]
- 128.Bossù P., Ciaramella A., Moro M.L., Bellincampi L., Bernardini S., Federici G., Trequattrini A., Macciardi F., Spoletini I., Di Iulio F., et al. Interleukin 18 gene polymorphisms predict risk and outcome of Alzheimer’s disease. J. Neurol. Neurosurg. Psychiatry. 2007;78:807–811. doi: 10.1136/jnnp.2006.103242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Zendedel A., Mönnink F., Hassanzadeh G., Zaminy A., Ansar M.M., Habib P., Slowik A., Kipp M., Beyer C. Estrogen Attenuates Local Inflammasome Expression and Activation after Spinal Cord Injury. Mol. Neurobiol. 2018;55:1364–1375. doi: 10.1007/s12035-017-0400-2. [DOI] [PubMed] [Google Scholar]
- 130.Gregg C., Zhang J., Butler J.E., Haig D., Dulac C. Sex-specific parent-of-origin allelic expression in the mouse brain. Science. 2010;329:682–685. doi: 10.1126/science.1190831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Miyoshi K., Obata K., Kondo T., Okamura H., Noguchi K. Interleukin-18-mediated microglia/astrocyte interaction in the spinal cord enhances neuropathic pain processing after nerve injury. J. Neurosci. 2008;28:12775–12787. doi: 10.1523/JNEUROSCI.3512-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Pilat D., Piotrowska A., Rojewska E., Jurga A., Ślusarczyk J., Makuch W., Basta-Kaim A., Przewlocka B., Mika J. Blockade of IL-18 signaling diminished neuropathic pain and enhanced the efficacy of morphine and buprenorphine. Mol. Cell. Neurosci. 2016;71:114–124. doi: 10.1016/j.mcn.2015.12.013. [DOI] [PubMed] [Google Scholar]
- 133.Parham C., Chirica M., Timans J., Vaisberg E., Travis M., Cheung J., Pflanz S., Zhang R., Singh K.P., Vega F., et al. A receptor for the heterodimeric cytokine IL-23 is composed of IL-12Rbeta1 and a novel cytokine receptor subunit, IL-23R. J. Immunol. 2002;168:5699–5708. doi: 10.4049/jimmunol.168.11.5699. [DOI] [PubMed] [Google Scholar]
- 134.Schinocca C., Rizzo C., Fasano S., Grasso G., La Barbera L., Ciccia F., Guggino G. Role of the IL-23/IL-17 Pathway in Rheumatic Diseases: An Overview. Front. Immunol. 2021;12:637829. doi: 10.3389/fimmu.2021.637829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Al-Janabi A., Alabas O.A., Yiu Z.Z.N., Foulkes A.C., Eyre S., Khan A.R., Reynolds N.J., Smith C.H., Griffiths C.E.M., Warren R.B., et al. Risk of Paradoxical Eczema in Patients Receiving Biologics for Psoriasis. JAMA Dermatol. 2024;160:71–79. doi: 10.1001/jamadermatol.2023.4846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Lubberts E. The IL-23-IL-17 axis in inflammatory arthritis. Nat. Rev. Rheumatol. 2015;11:415–429. doi: 10.1038/nrrheum.2015.53. [DOI] [PubMed] [Google Scholar]
- 137.Ljosaa T.M., Mork C., Stubhaug A., Moum T., Wahl A.K. Skin pain and skin discomfort is associated with quality of life in patients with psoriasis. J. Eur. Acad. Dermatol. Venereol. 2012;26:29–35. doi: 10.1111/j.1468-3083.2011.04000.x. [DOI] [PubMed] [Google Scholar]
- 138.Elewski B., Alexis A.F., Lebwohl M., Stein Gold L., Pariser D., Del Rosso J., Yosipovitch G. Itch: An under-recognized problem in psoriasis. J. Eur. Acad. Dermatol. Venereol. 2019;33:1465–1476. doi: 10.1111/jdv.15450. [DOI] [PubMed] [Google Scholar]
- 139.Adachi A., Honda T., Egawa G., Kanameishi S., Takimoto R., Miyake T., Hossain M.R., Komine M., Ohtsuki M., Gunzer M., et al. Estradiol suppresses psoriatic inflammation in mice by regulating neutrophil and macrophage functions. J. Allergy Clin. Immunol. 2022;150:909–919.e8. doi: 10.1016/j.jaci.2022.03.028. [DOI] [PubMed] [Google Scholar]
- 140.Deodhar A., Helliwell P.S., Boehncke W.H., Kollmeier A.P., Hsia E.C., Subramanian R.A., Xu X.L., Sheng S., Agarwal P., Zhou B., et al. Guselkumab in patients with active psoriatic arthritis who were biologic-naive or had previously received TNFα inhibitor treatment (DISCOVER-1): A double-blind, randomised, placebo-controlled phase 3 trial. Lancet. 2020;395:1115–1125. doi: 10.1016/S0140-6736(20)30265-8. [DOI] [PubMed] [Google Scholar]
- 141.Mease P.J., Rahman P., Gottlieb A.B., Kollmeier A.P., Hsia E.C., Xu X.L., Sheng S., Agarwal P., Zhou B., Zhuang Y., et al. Guselkumab in biologic-naive patients with active psoriatic arthritis (DISCOVER-2): A double-blind, randomised, placebo-controlled phase 3 trial. Lancet. 2020;395:1126–1136. doi: 10.1016/S0140-6736(20)30263-4. [DOI] [PubMed] [Google Scholar]
- 142.McInnes I.B., Rahman P., Gottlieb A.B., Hsia E.C., Kollmeier A.P., Chakravarty S.D., Xu X.L., Subramanian R.A., Agarwal P., Sheng S., et al. Efficacy and Safety of Guselkumab, an Interleukin-23p19-Specific Monoclonal Antibody, Through One Year in Biologic-Naive Patients With Psoriatic Arthritis. Arthritis Rheumatol. 2021;73:604–616. doi: 10.1002/art.41553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Tang J., Zhao S., Shi H., Li X., Ran L., Cao J., He Y. Effects on peripheral and central nervous system of key inflammatory intercellular signalling peptides and proteins in psoriasis. Exp. Dermatol. 2024;33:e15104. doi: 10.1111/exd.15104. [DOI] [PubMed] [Google Scholar]
- 144.Schmitz J., Owyang A., Oldham E., Song Y., Murphy E., McClanahan T.K., Zurawski G., Moshrefi M., Qin J., Li X., et al. IL-33, an interleukin-1-like cytokine that signals via the IL-1 receptor-related protein ST2 and induces T helper type 2-associated cytokines. Immunity. 2005;23:479–490. doi: 10.1016/j.immuni.2005.09.015. [DOI] [PubMed] [Google Scholar]
- 145.Boraschi D., Tagliabue A. The interleukin-1 receptor family. Semin. Immunol. 2013;25:394–407. doi: 10.1016/j.smim.2013.10.023. [DOI] [PubMed] [Google Scholar]
- 146.Macari S., Madeira M.F.M., Lima I.L.A., Pereira T.S.F., Dias G.J., Cirelli J.A., de Molon R.S., Fukada S.Y., Szawka R.E., Garlet G.P., et al. ST2 regulates bone loss in a site-dependent and estrogen-dependent manner. J. Cell. Biochem. 2018;119:8511–8521. doi: 10.1002/jcb.27080. [DOI] [PubMed] [Google Scholar]
- 147.Kato T., Yasuda K., Matsushita K., Ishii K.J., Hirota S., Yoshimoto T., Shibahara H. Interleukin-1/-33 Signaling Pathways as Therapeutic Targets for Endometriosis. Front. Immunol. 2019;10:2021. doi: 10.3389/fimmu.2019.02021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.York A.G., Skadow M.H., Oh J., Qu R., Zhou Q.D., Hsieh W.Y., Mowel W.K., Brewer J.R., Kaffe E., Williams K.J., et al. IL-10 constrains sphingolipid metabolism to limit inflammation. Nature. 2024;627:628–635. doi: 10.1038/s41586-024-07098-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Ouyang W., Rutz S., Crellin N.K., Valdez P.A., Hymowitz S.G. Regulation and functions of the IL-10 family of cytokines in inflammation and disease. Annu. Rev. Immunol. 2011;29:71–109. doi: 10.1146/annurev-immunol-031210-101312. [DOI] [PubMed] [Google Scholar]
- 150.Saraiva M., O’Garra A. The regulation of IL-10 production by immune cells. Nature reviews. Immunology. 2010;10:170–181. doi: 10.1038/nri2711. [DOI] [PubMed] [Google Scholar]
- 151.Pinzan C.F., Ruas L.P., Casabona-Fortunato A.S., Carvalho F.C., Roque-Barreira M.C. Immunological basis for the gender differences in murine Paracoccidioides brasiliensis infection. PLoS ONE. 2010;5:e10757. doi: 10.1371/journal.pone.0010757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Kahlke V., Angele M.K., Ayala A., Schwacha M.G., Cioffi W.G., Bland K.I., Chaudry I.H. Immune dysfunction following trauma-haemorrhage: Influence of gender and age. Cytokine. 2000;12:69–77. doi: 10.1006/cyto.1999.0511. [DOI] [PubMed] [Google Scholar]
- 153.Chistyakov D.V., Azbukina N.V., Astakhova A.A., Goriainov S.V., Chistyakov V.V., Sergeeva M.G. Sex-Mediated Differences in LPS Induced Alterations of TNFα, IL-10 Expression, and Prostaglandin Synthesis in Primary Astrocytes. Int. J. Mol. Sci. 2018;19:2793. doi: 10.3390/ijms19092793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Mesquita A.R., Correia-Neves M., Roque S., Castro A.G., Vieira P., Pedrosa J., Palha J.A., Sousa N. IL-10 modulates depressive-like behavior. J. Psychiatr. Res. 2008;43:89–97. doi: 10.1016/j.jpsychires.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 155.Sloane E., Ledeboer A., Seibert W., Coats B., van Strien M., Maier S.F., Johnson K.W., Chavez R., Watkins L.R., Leinwand L., et al. Anti-inflammatory cytokine gene therapy decreases sensory and motor dysfunction in experimental Multiple Sclerosis: MOG-EAE behavioral and anatomical symptom treatment with cytokine gene therapy. Brain Behav. Immun. 2009;23:92–100. doi: 10.1016/j.bbi.2008.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Orhan C., Tuzcu M., Durmus A.S., Sahin N., Ozercan I.H., Deeh P.B.D., Morde A., Bhanuse P., Acharya M., Padigaru M., et al. Protective effect of a novel polyherbal formulation on experimentally induced osteoarthritis in a rat model. Biomed. Pharmacother. 2022;151:113052. doi: 10.1016/j.biopha.2022.113052. [DOI] [PubMed] [Google Scholar]
- 157.Groth K.A., Skakkebæk A., Høst C., Gravholt C.H., Bojesen A. Clinical review: Klinefelter syndrome--a clinical update. J. Clin. Endocrinol. Metab. 2013;98:20–30. doi: 10.1210/jc.2012-2382. [DOI] [PubMed] [Google Scholar]
- 158.Jiang Y., Wang J., Li H., Xia L. IL-35 alleviates inflammation progression in a rat model of diabetic neuropathic pain via inhibition of JNK signaling. J. Inflamm. 2019;16:19. doi: 10.1186/s12950-019-0217-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.O’Brien L.C., Mezzaroma E., Van Tassell B.W., Marchetti C., Carbone S., Abbate A., Toldo S. Interleukin-18 as a therapeutic target in acute myocardial infarction and heart failure. Mol. Med. 2014;20:221–229. doi: 10.2119/molmed.2014.00034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Abbate A., Toldo S., Marchetti C., Kron J., Van Tassell B.W., Dinarello C.A. Interleukin-1 and the Inflammasome as Therapeutic Targets in Cardiovascular Disease. Circ. Res. 2020;126:1260–1280. doi: 10.1161/CIRCRESAHA.120.315937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Doberer K., Duerr M., Halloran P.F., Eskandary F., Budde K., Regele H., Reeve J., Borski A., Kozakowski N., Reindl-Schwaighofer R., et al. A Randomized Clinical Trial of Anti-IL-6 Antibody Clazakizumab in Late Antibody-Mediated Kidney Transplant Rejection. J. Am. Soc. Nephrol. 2021;32:708–722. doi: 10.1681/ASN.2020071106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Narazaki M., Tanaka T., Kishimoto T. The role and therapeutic targeting of IL-6 in rheumatoid arthritis. Expert Rev. Clin. Immunol. 2017;13:535–551. doi: 10.1080/1744666X.2017.1295850. [DOI] [PubMed] [Google Scholar]
- 163.Golebski K., Layhadi J.A., Sahiner U., Steveling-Klein E.H., Lenormand M.M., Li R.C.Y., Bal S.M., Heesters B.A., Vilà-Nadal G., Hunewald O., et al. Induction of IL-10-producing type 2 innate lymphoid cells by allergen immunotherapy is associated with clinical response. Immunity. 2021;54:291–307.e7. doi: 10.1016/j.immuni.2020.12.013. [DOI] [PubMed] [Google Scholar]
- 164.Kelsen S.G., Agache I.O., Soong W., Israel E., Chupp G.L., Cheung D.S., Theess W., Yang X., Staton T.L., Choy D.F., et al. Astegolimab (anti-ST2) efficacy and safety in adults with severe asthma: A randomized clinical trial. J. Allergy Clin. Immunol. 2021;148:790–798. doi: 10.1016/j.jaci.2021.03.044. [DOI] [PubMed] [Google Scholar]
- 165.Avci A.B., Feist E., Burmester G.R. Targeting IL-6 or IL-6 Receptor in Rheumatoid Arthritis: What Have We Learned? BioDrugs. 2024;38:61–71. doi: 10.1007/s40259-023-00634-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.McGonagle D., Watad A., Sharif K., Bridgewood C. Why Inhibition of IL-23 Lacked Efficacy in Ankylosing Spondylitis. Front. Immunol. 2021;12:614255. doi: 10.3389/fimmu.2021.614255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Torres T., Puig L., Vender R., Lynde C., Piaserico S., Carrascosa J.M., Gisondi P., Daudén E., Conrad C., Mendes-Bastos P., et al. Drug Survival of IL-12/23, IL-17 and IL-23 Inhibitors for Psoriasis Treatment: A Retrospective Multi-Country, Multicentric Cohort Study. Am. J. Clin. Dermatol. 2021;22:567–579. doi: 10.1007/s40257-021-00598-4. [DOI] [PubMed] [Google Scholar]
- 168.Sorge R.E., LaCroix-Fralish M.L., Tuttle A.H., Sotocinal S.G., Austin J.S., Ritchie J., Chanda M.L., Graham A.C., Topham L., Beggs S., et al. Spinal cord Toll-like receptor 4 mediates inflammatory and neuropathic hypersensitivity in male but not female mice. J. Neurosci. 2011;31:15450–15454. doi: 10.1523/JNEUROSCI.3859-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.McInnis C.M., Thoma M.V., Gianferante D., Hanlin L., Chen X., Breines J.G., Hong S., Rohleder N. Measures of adiposity predict interleukin-6 responses to repeated psychosocial stress. Brain Behav. Immun. 2014;42:33–40. doi: 10.1016/j.bbi.2014.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.von Känel R., Kudielka B.M., Preckel D., Hanebuth D., Fischer J.E. Delayed response and lack of habituation in plasma interleukin-6 to acute mental stress in men. Brain Behav. Immun. 2006;20:40–48. doi: 10.1016/j.bbi.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 171.Lanfranco F., Kamischke A., Zitzmann M., Nieschlag E. Klinefelter’s syndrome. Lancet. 2004;364:273–283. doi: 10.1016/S0140-6736(04)16678-6. [DOI] [PubMed] [Google Scholar]
- 172.Sakkas L.I., Chikanza I.C. Sex bias in immune response: It is time to include the sex variable in studies of autoimmune rheumatic diseases. Rheumatol. Int. 2024;44:203–209. doi: 10.1007/s00296-023-05446-8. [DOI] [PubMed] [Google Scholar]
- 173.Fish E.N. The X-files in immunity: Sex-based differences predispose immune responses. Nat. Rev. Immunol. 2008;8:737–744. doi: 10.1038/nri2394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Kalayci Yigin A., Alay M.T., Uğurlu S., Seven M. The First Case Report of 47,XXY/46,XX/46,XY Mosaic Klinefelter Syndrome Patient With Mixed Connective Tissue Disorder. Am. J. Men’s Health. 2023;17:15579883231165173. doi: 10.1177/15579883231165173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Panimolle F., Tiberti C., Spaziani M., Riitano G., Lucania G., Anzuini A., Lenzi A., Gianfrilli D., Sorice M., Radicioni A.F. Non-organ-specific autoimmunity in adult 47,XXY Klinefelter patients and higher-grade X-chromosome aneuploidies. Clin. Exp. Immunol. 2021;205:316–325. doi: 10.1111/cei.13616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Yığman M., Yığman F., Tangal S., Haliloğlu A.H., Çağlar G.S. Pre-test anxiety levels and postoperative pain in non-obstructive azoospermic patients: Is klinefelter syndrome a predisposing factor? Urol. J. 2022;89:280–284. doi: 10.1177/03915603211025236. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.