Abstract
Background
Armed conflicts severely impact survivors psychologically, with effects tied to the trauma's intensity and widespread displacement. From October 2023 to January 2025, the Gaza Strip faced violent conflict, leading to major displacement and suffering. This study examines anxiety, PTSD, and depression among displaced adults from Gaza Strip.
Methods
This cross-sectional study, conducted in November 2024, surveyed 952 displaced adults using the GAD-7, PCL-5, and PHQ-9 instruments and a convenience sampling method. A PTSD diagnosis required having a PCL-5 score ≥ 23 and fulfilling the DSM-5 criteria. The rates and severity of probable anxiety, PTSD, and depression were reported. Then, using SPSS, logistic regression models identified factors associated with each disorder, while multinomial regression models explored associations with the number of comorbidities.
Results
The majority were unemployed (73.7%). Over half of the participants were displaced in camps (55.6%), while 40.4% lived in shelters. Nearly a fifth (20.3%) had lost a first-degree relative, 12.7% were injured, and 4.8% were detained by the military. Moderate or higher levels of anxiety and depression were reported by 79.3% and 84.5%, respectively. The rate of symptomatic PTSD was 67.8% when defined as meeting the DSM-5 criteria for PTSD and having a PCL-5 score ≥ 23, and 88.2% based on the latter criterion alone, while subthreshold PTSD was encountered in 18.1%. Also, 63.1% suffered significant symptoms of all three comorbidities. Significant predictors of anxiety included being female and having PTSD or depression. Significant predictors of PTSD included experiencing more frequent migrations, unemployment or working in the private sector, military detention, or having anxiety or depression. Significant predictors of depression included the death of a first-degree relative, military detention, torture, and having anxiety or PTSD. Additionally, having a higher number of migrations was significantly associated with having one, two, or three disorders compared to having “no disorders,” while those experiencing more forms of harm were significantly more likely to have all three disorders.
Conclusions
The study found very high rates of psychiatric disorders among IDPs in Gaza and identified several risk factors contributing to those rates. Interventions must be prioritized to support society's long-term recovery.
Keywords: depression, anxiety, PTSD, mental health, armed conflicts, gaza strip, refugees, psychological interventions
Introduction
Armed conflicts pose a significant threat to the mental health of affected populations, as traumatic experiences such as loss and injury conspire with socioeconomic stressors like displacement and loss of income. 1 Anxiety, post-traumatic stress disorder (PTSD), and depression are the most identified mental health problems in survivors of armed conflict. Depression is characterized by persistent feelings of sadness, hopelessness, and a lack of interest or pleasure in activities, often with changes in sleep, appetite, and cognitive functioning. Anxiety is characterized by persistent and excessive feelings of fear or anxiety that interfere with daily functioning. It often leads to avoidance behaviors and may be accompanied by physical symptoms such as tension and panic attacks. Posttraumatic stress disorder is a mental health condition that can develop after experiencing or witnessing a traumatic event. PTSD in DSM-5 requires exposure to actual or threatened death, serious injury, or sexual violence (Criterion A), followed by symptoms from four clusters: intrusive symptoms (eg, distressing memories or flashbacks); persistent avoidance of trauma-related stimuli; negative alterations in cognitions and mood; and marked arousal/reactivity changes. These symptoms must persist for more than one month and cause clinically significant distress or functional impairment while not being attributable to substance use or other medical conditions (American Psychiatric Association, 2013). The diagnosis emphasizes both the traumatic exposure and the resulting multifaceted psychological and physiological responses that characterize the disorder. There is a significant overlapping of these three psychiatric comorbidities in war survivors, where the prevalence tends to be proportional to the intensity and frequency of trauma.2–4 Studies from low-income, war-afflicted countries also found that socioeconomic factors such as extreme poverty contributed significantly to mental health issues among war survivors. 5
Forced displacement due to war or conflict constitutes a major traumatic event under DSM-5 Criterion A for PTSD, given its association with actual or threatened death, serious injury, and severe threats to physical integrity—such as exposure to violence, destruction, perilous escape—resulting in profound biopsychosocial impacts, by disrupting access to healthcare, clean water, and education, severing family ties and support networks, and fostering deep feelings of disempowerment and alienation.6,7 Studies and systematic reviews have revealed significantly high prevalence rates of anxiety, PTSD, depression, and other psychiatric disorders among conflict-displaced refugees, even when compared to non-displaced individuals within the same country6–10
The Gaza Strip has been under Israeli military occupation since 1967 and has been subjected to a strict blockade since 2006. It represents an area marked by de-development, chronic conflict, and poverty. Over the past two decades, it has faced repeated military campaigns that have resulted in thousands of deaths and injuries, leaving basic infrastructure and healthcare services trapped in a perpetual cycle of destruction and inadequacy.11,12 Since October 2023, the Gaza Strip has been the epicenter of one of the decade's most notorious and violent wars, representing the latest conflict between the occupied Palestinians and Israel. By November 2024, when this study was conducted, the war had claimed the lives of more than 43000 Palestinians and wounded over 100000 others. It has also caused immense humanitarian suffering, exacerbating the impacts of the nearly two decades of military blockade.13–15 The scale and ferocity of the war have had regional and global consequences and led several countries, as well as human rights and United Nations organizations, to categorize it as genocide.16,17
Forced displacement has been a substantial source of suffering during the Gaza war. 18 A military evacuation order in October 2023 forced the population of the two northern governorates to the southern areas of the Strip. Subsequently, a military corridor dissected the Gaza Strip into two completely isolated cantons, between which the movement and relocation of internally displaced persons (IDPs) was not permitted. 19 The northern canton consisted of the Northern and Gaza Governorates, and the southern of the Middle, Khan Younis, and Rafah Governorates. In November 2024, approximately 1.9 million, ie, nearly 90% of the Gaza Strip's population, were displaced. 20
A recent survey provided an insight into the psychological toll the war has exacted on Palestinians living in the Gaza Strip. 19 In a sample of 339 young adults aged between 18 and 24 years, 93.81%, 79.36%, and 81.71% reported symptoms of moderate or higher depression, anxiety, and stress, respectively, and 63.40% suffered symptoms of PTSD. 19 Those numbers were higher than most previous reports from Palestine prior to the current war and from other regions as well.9,10,21–25 Furthermore, the Gaza Strip's population has already been struggling with a mental health crisis even before the wake of the current war, with high rates of anxiety, PTSD, and depression and insufficient access to mental health services.26,27
Literature is rich with evidence demonstrating the impact of forced displacement and armed conflict on psychiatric disorders. 28 However, except for one study on young adult university students, 19 there are no studies yet exploring the mental well-being of other Gazan population groups during the 2023–2025 war. Additionally, due to the particularly violent and lengthy nature of this war, it is important to document the psychological impacts on the different strata of the community and at different phases of the war. To bridge this gap, the present study aimed to investigate the prevalence of anxiety, PTSD, and depression among adult IDPs in the Gaza Strip and explore the factors predicting these mental health disorders.
Methods
Study Design and Setting
This descriptive, cross-sectional study surveyed the prevalence of probable anxiety, PTSD, and depression among IDPs aged 18 years and older who lived in the southern canton of the Gaza Strip during the war. The study excluded people who were younger than 18, who could not read and write, and who had a known psychiatric condition or dementia. The study settings comprised 15 displacement centers: one school and five displacement camps from the Middle Governorate and six schools and three camps from the Khan Younis Governorate. The geographical distribution of the camps and schools covered the densely populated areas in the southern canton in November 2024. Data collection took place between November 1 and November 20, 2024.
Participants
In November 2024, an estimated 1.9 million IDPs lived in the Gaza Strip.20,29 The majority lived in the southern part of the Strip, having been displaced by military evacuation orders and the ensuing ground invasion of Gaza City and the Northern Governorate in the first weeks of the war. At the time of data collection, Rafah Governorate was evacuated due to the ground invasion that has been ongoing since May 2024. Therefore, the vast majority of the population in the southern canton was condensed to the Middle and Khan Younis Governorates. Most lived in either displacement camps or sought shelter at schools and other public structures. Displacement camps consisted of tents or makeshift structures built from wood and tarpaulin, while families displaced to schools lived in shared classrooms. Living conditions in the camps and schools were comparable and marked by poor conditions, overcrowding, and lack of services.29,30
Sample Size and Sampling
Using the Raosoft, Inc. online calculator, with a 5% margin of error and a 99% confidence interval, the minimally required sample size was calculated as 664 participants. Our study included 952 IDPs. Due to logistical and safety constraints in the conflict zone, a convenience sampling method was utilized. The questionnaire was printed for participants to fill out directly. Senior medical students collected data after explaining the study's design and goals to potential participants in each study setting and obtaining their consent.
Tools and Procedures
Data was collected using a self-administered questionnaire divided into two sections. The first collected sociodemographic data, including age, sex, number of family members, governorate of residence before the war, current governorate, education, job, average monthly income during the preceding three months (reported as multiples of 800 NIS “220 USD”, which was the basic salary distributed to government employees during the war), and current accommodation (tent/shelter/with relatives). Additionally, we investigated seven potential traumatizing experiences of the war, including experiences such as injuries, military detention, torture, house damage, the death of a first-degree relative in the hostilities, loss of income sources, and the number of forced migrations.
The second section comprised the General Anxiety Disorder-7 (GAD-7), Posttraumatic Stress Disorder Checklist for the DSM-5 (PCL-5), and the Patient Health Questionnaire-9 (PHQ-9) scales, which screen for probable anxiety, PTSD, and depression, respectively. We used the Arabic versions of the GAD-7 and PHQ-9, translated and validated by Pfizer Inc., for the GAD-7 and the PHQ-9, while we used the version translated and validated by Ibrahim et al for the PCL-5.31–33
The GAD-7 is a reliable tool used to screen for the prevalence and severity of anxiety symptoms per the DSM-IV-TR in the past two weeks. 34 It comprises seven questions scored between 0 (not at all) and 3 (nearly every day) on a Likert scale. The total score ranges between 0 and 21, with cutoff scores of 5, 10, and 15 signifying minimal, mild, moderate, and severe anxiety symptoms, respectively. 34 We used a cutoff of 8 to distinguish between individuals with anxiety and those without. This cutoff demonstrates high specificity and sensitivity (84% and 83%, respectively). 35
The PCL-5 comprises 20 questions based on the four DSM-5 PTSD symptomatic clusters: reexperiencing, avoidance, negative alterations in cognition and mood, and hyperarousal. 36 It is self-reported and, using a five-point Likert scale (0–4) and a maximum score of 80, assessed the severity of 20 PTSD symptoms over the past month in relation to the worst event experienced during the current war. The cutoff score used in the validated Arabic version was 23 or higher, derived from a cohort of Kurdish and Syrian refugees. 33 For the purpose of the present study, individuals screened positive for PTSD if the participant scored ≥ 23 on the PCL-5 and also reported the minimally required DSM-5 symptoms. This meant endorsing at least one item with moderate or higher severity from DSM-5 criterion B “re-experiencing” (questions 1-5), one item from criterion C “avoidance” (questions 6-7), two items from criterion D “negative alterations in cognition and mood” (questions 8-14), and two items from criterion E “hyperarousal” (questions 15-20). 19 Subthreshold PTSD was diagnosed in participants who endorsed moderate or higher symptoms in any three of the four DSM-5 clusters (B-E). 37
The Patient Health Questionnaire-9 (PHQ-9) is a self-administered tool that employs nine standard questions to screen for depressive symptoms in the past two weeks. The questions represent the criterion symptoms for DSM-IV major depression and are scored on a Likert scale ranging from 0 (not at all) to 3 (nearly every day). The total score ranges between 0 and 27, with 5, 10, 15, and 20 cutoffs representing mild, moderate, moderately severe, and severe depressive symptoms, respectively. 38 A cutoff score of 10 was used to screen for individuals with depression. This cutoff has a sensitivity of 85% and a specificity of 89%. 39 The PHQ-9 score has demonstrated reliability as a screening tool across varying settings in different regions, including in IDPs and veterans.40–42
Ethical Considerations
Ethical approval was obtained from the Institutional Review Board (IRB) at the Islamic University of Gaza (IUG). The research was conducted per the Declaration of Helsinki. Participants gave written informed consent, emphasizing confidentiality and voluntary participation. No identifying information was collected.
Statistical Analysis
Descriptive statistics, including frequencies and percentages, were calculated for categorical variables to provide an overview of the sample characteristics, and means and standard deviations were calculated for continuous variables. Logistic regression models were applied to examine the relationships between sociodemographic characteristics and war-related exposures with mental health outcomes, specifically anxiety, PTSD, and depression. Multinomial regression models were used to explore comorbidities within the sample, with “no disorder” as the reference category and the three disorders as the highest category. Both bivariate and binomial regression analyses were conducted to inform the construction of these models, with detailed results available in the Supplemental material. We tested for the independence of variables, multicollinearity, and the adequacy of the sample size. No violations were found in any of these tests, and the models met the necessary criteria for valid results. Moreover, we used Cronbach's alpha to measure the reliability of the scales. All statistical analyses were performed using STATA 17, while figures were generated using R Studio and Prism GraphPad.
Results
Sociodemographic Characteristics
Of the study's 952 participants, most were female (62%), unemployed (73.7%), and were displaced from the Gaza Governorate (42.3%). The mean age was 32.82 (12.45) years. Table 1 illustrates the sociodemographic characteristics of study participants, and Table 2 breaks down the assessed forms of harm they suffered due to the war.
Table 1.
Descriptive Statistics of the Study Population.
| Item | Frequency | Percent |
|---|---|---|
| Age^ | 32.82 ± 12.45 | |
| Family Size (n)^* | 5.79 ± 2.7 | |
| Sex | ||
| Female | 590 | 62% |
| Male | 362 | 38% |
| Residence Prior to War (Governorate) | ||
| North Gaza | 163 | 17.1% |
| Gaza | 403 | 42.3% |
| Middle Area | 68 | 7.1% |
| Khan Younis | 171 | 18% |
| Rafah | 147 | 15.4% |
| Current Residence | ||
| Middle Area | 397 | 41.8% |
| Khan Younis | 552 | 58.2% |
| Education | ||
| Primary Schooling | 89 | 9.3% |
| Technical-professional Training | 302 | 31.7% |
| Secondary Schooling | 147 | 15.4% |
| Undergraduate Degree | 370 | 38.9% |
| Postgraduate studies | 44 | 4.6% |
| Occupation (during the war) | ||
| Governmental Employee | 113 | 11.9% |
| Private Sector | 51 | 5.4% |
| Freelance | 86 | 9% |
| Unemployed | 702 | 73.7% |
| Current Shelter | ||
| Relative's House | 38 | 4% |
| Displacement Camp | 529 | 55.6% |
| Displacement Center (Schools) | 385 | 40.4% |
| Average Monthly Income (NIS) | ||
| <800 | 736 | 77.4% |
| 800–1600 | 137 | 14.4% |
| >1600 | 78 | 8.2% |
Mean ± Standard Deviation.
Includes the participant's spouse, children, and parents if they shared the same living space.
Table 2.
Assessed Forms of Harm Suffered by Participants.
| Item | Frequency | Percent |
|---|---|---|
| Migration number^ | 5.17 ± 3.09 | |
| Forms of harm^ | 1.44 ± 1.13 | |
| Death of a First-Degree Relative | 193 | 20.3% |
| House Destruction | 601 | 63.1% |
| Personal Injuries | 121 | 12.7% |
| Military Detention | 46 | 4.8% |
| Tortured | 42 | 4.4% |
| Loss of Income Source Due to War | 368 | 38.7% |
^Mean ± Standard Deviation.
Prevalence, Scale Reliability, and Severity of Psychiatric Comorbidities
The internal consistency of the scales was assessed using Cronbach's alpha. The PCL scale exhibited excellent reliability (α = 0.9286), while the PHQ scale and GAD scale both demonstrated good reliability (α = 0.8379 & α = 0.8405, respectively), indicating that all three measures had acceptable to excellent internal consistency.
The median (IQR) GAD-7, PCL-5, and PHQ-9 scores were 14 (10-17), 43 (32-55), and 15 (12-20), respectively. Table 3 illustrates the prevalence and severity of anxiety, PTSD, subthreshold PTSD, and depression. A visual representation of the distribution of the PCL-5 score can be found in the supplement.
Table 3.
Prevalence and Severity of Anxiety, PTSD, and Depression (n = 952).
| Disorder | Frequency | Percent |
|---|---|---|
| Anxiety | ||
| Minimal (<5) | 44 | 4.6% |
| Mild (5–9) | 153 | 16.1% |
| Moderate (10–14) | 311 | 32.7% |
| Severe (≥15) | 444 | 46.6% |
| PTSD | ||
| DSM-5 criteria | 646 | 67.9% |
| PCL-5 ≥ 23 | 840 | 88.2% |
| Fulfils DSM-5 and PCL-5 ≥ 23 | 645 | 67.8% |
| PCL-5 ≥ 33 | 724 | 76.0% |
| Subthreshold PTSD | 173 | 18.1% |
| Depression Severity | ||
| Minimal (<5) | 35 | 3.7% |
| Mild (5–9) | 113 | 11.9% |
| Moderate (10–14) | 274 | 28.8% |
| Moderately Severe (15–19) | 282 | 29.7% |
| Severe (≥20) | 247 | 26% |
| Comorbidities | ||
| None | 65 | 6.8% |
| One Disorder | 84 | 8.8% |
| Two Disorders | 202 | 21.2% |
| Three Disorders | 600 | 63.1% |
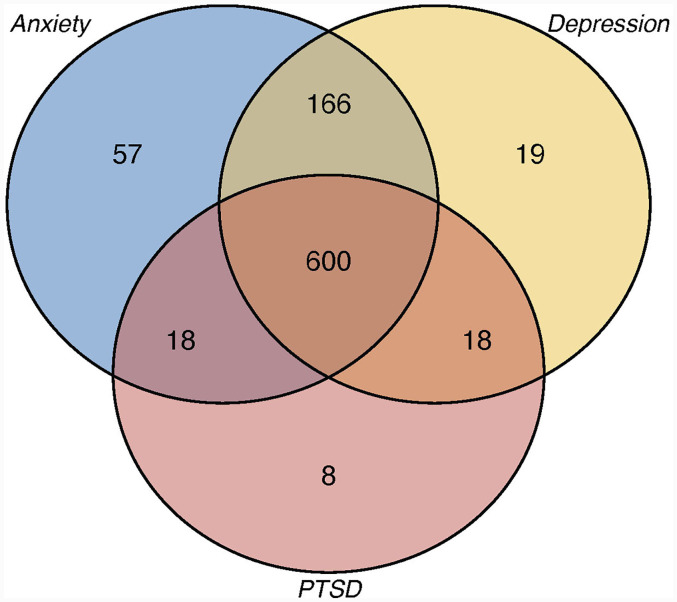
In terms of psychiatric comorbidity, 63.1% suffered significant symptoms of all three screened comorbidities, while only 6.8% did not suffer from any mental health disorder. Figure 1 demonstrates the overlapping of psychiatric comorbidities among participants.
Figure 1.
Overlapping of psychiatric disorders (moderate or higher anxiety, moderate or higher depression, and PTSD fulfilling DSM-5 criteria + PCL-5 score ≥23) among participants (n).
Predictors of Anxiety, PTSD, and Depression
Multivariate logistic regression found that females (OR: 1.91, p-value: 0.0185) and those with PTSD (OR: 3.60, p-value <0.001) or depression (OR: 13.22, p-value < 0.001) were significantly more likely to have moderate or higher symptoms of anxiety. On the other hand, an increased number of migrations (OR: 1.08, p-value = 0.006), unemployment (OR: 1.81, p-value = 0.0249), working in the private sector (OR: 3.11, p-value, 0.015), military detention (OR: 4.61, p-value = 0.046), and having anxiety (OR: 3.50, p-value < 0.001) or depression (OR: 10.40, p-value <0.001) significantly predicted PTSD. Significant predictors of depression were the death of a close relative (OR: 2.27, p-value = 0.0161), military detention (OR: 0.103, p-value = 0.024), torture (OR: 52.65, p-value = 0.0041), and having anxiety (OR: 13.66, p-value < 0.001) or PTSD (OR: 10.72, p-value < 0.001) (Table 4). Multinominal regression found a significant association between the number of migrations and having one, two, or three disorders compared to “no disorders” (respectively, OR: 1.16, p-value = 0.0376; OR: 1.61, p-value = 0.0208; OR: 1.22, p-value = 0.0011) Also, an increased number of the total forms of harm (OR: 1.356, p-value = 0.0267) reported was significantly associated with having three disorders (Table 5).
Table 4.
Multivariate Logistic Regression Models for each Mental Health Disorder.
| Variable | Anxiety | PTSD | Depression | ||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | p | 95% CI | OR | p | 95% CI | OR | p | 95% CI | |
| Age | 1.0058 | 0.5744 | (0.99, 1.03) | 1.0117 | 0.0959 | (1, 1.03) | 0.9965 | 0.7189 | (0.98, 1.02) |
| Number of Migrations | 1 | 0.9999 | (0.91, 1.09) | 1.0849 | 0.006 | (1.02, 1.15) | 1.0429 | 0.3514 | (0.95, 1.14) |
| Sex | |||||||||
| Female | ref | ref | ref | ref | ref | ref | ref | ref | ref |
| Male | 0.5237 | 0.0185 | (0.31, 0.9) | 1.0001 | 0.9997 | (0.7, 1.42) | 1.1178 | 0.6705 | (0.67, 1.87) |
| Occupation | |||||||||
| Governmental Employee | ref | ref | ref | ref | ref | ref | ref | ref | ref |
| Private Sector | 1.3326 | 0.677 | (0.35, 5.15) | 3.1137 | 0.015 | (1.25, 7.78) | 0.5063 | 0.2434 | (0.16, 1.59) |
| Freelance | 0.7916 | 0.6603 | (0.28, 2.24) | 1.3062 | 0.4518 | (0.65, 2.62) | 2.1134 | 0.1837 | (0.7, 6.37) |
| Unemployed | 0.8255 | 0.6232 | (0.38, 1.77) | 1.8118 | 0.0249 | (1.08, 3.05) | 1.0175 | 0.9632 | (0.49, 2.13) |
| Death of Close Relative | |||||||||
| No | ref | ref | ref | ref | ref | ref | ref | ref | ref |
| Yes | 0.5715 | 0.0756 | (0.31, 1.06) | 1.1468 | 0.5145 | (0.76, 1.73) | 2.2726 | 0.0161 | (1.16, 4.43) |
| House Destruction | |||||||||
| No | ref | ref | ref | ref | ref | ref | ref | ref | ref |
| Yes | 1.2288 | 0.4152 | (0.75, 2.02) | 1.3624 | 0.0628 | (0.98, 1.89) | 0.963 | 0.8736 | (0.61, 1.53) |
| Personal Injuries | |||||||||
| No | ref | ref | ref | ref | ref | ref | ref | ref | ref |
| Yes | 1.1602 | 0.7185 | (0.52, 2.6) | 0.85 | 0.5354 | (0.51,1.42) | 0.9764 | 0.9513 | (0.45, 2.1) |
| Military detention | |||||||||
| No | ref | ref | ref | ref | ref | ref | ref | ref | ref |
| Yes | 1.2401 | 0.8074 | (0.22, 6.99) | 4.6058 | 0.0458 | (1.03,20.62) | 0.103 | 0.024 | (0.01, 0.74) |
| Tortured | |||||||||
| No | ref | ref | ref | ref | ref | ref | ref | ref | ref |
| Yes | 0.2488 | 0.15 | (0.04, 1.65) | 0.7519 | 0.7275 | (0.15, 3.74) | 52.651 | 0.0041 | (3.52, 787.48) |
| Loss of Income | |||||||||
| No | ref | ref | ref | ref | ref | ref | ref | ref | ref |
| Yes | 1.4161 | 0.2022 | (0.83, 2.42) | 1.1717 | 0.3575 | (0.84, 1.64) | 0.8504 | 0.5177 | (0.52, 1.39) |
| Anxiety | |||||||||
| No or mild anxiety | - | - | - | ref | ref | ref | ref | ref | ref |
| Moderate anxiety or higher | - | - | - | 3.4909 | <0.001 | (1.97, 6.17) | 13.6572 | <0.001 | (7.88,23.68) |
| PTSD | |||||||||
| No PTSD | ref | ref | ref | - | - | - | ref | ref | ref |
| PTSD | 3.5982 | <0.001 | (2.04, 6.35) | - | - | - | 10.7215 | <0.001 | (6.45, 17.83) |
| Depression | |||||||||
| No or mild depression | ref | ref | ref | ref | ref | ref | - | - | - |
| Moderate depression or higher | 13.2202 | <0.001 | (7.68, 22.76) | 10.3978 | <0.001 | (6.3, 17.17) | - | - | - |
OR: Odds Ratio; P: p-value; CI: Confidence Interval; Ref: reference value.
Table 5.
Multinomial Analyses for Comorbidity (PTSD, Depression, and Anxiety) with “no Disorder” as the Reference Outcome Category.
| Variable | One Disorder versus No Disorder | Two Disorders versus No Disorder | Three Disorders versus No Disorder | ||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | p | 95% CI | OR | p | 95% CI | OR | p | 95% CI | |
| Age | 0.9931 | 0.6538 | (0.96, 1.02) | 0.9968 | 0.8029 | (0.97, 1.02) | 1.0071 | 0.5528 | (0.98, 1.03) |
| Number of Migrations | 1.1624 | 0.0376 | (1.01, 1.34) | 1.1615 | 0.0208 | (1.02, 1.32) | 1.2234 | 0.0011 | (1.08, 1.38) |
| Forms of Harm | 0.98 | 0.908 | (0.7, 1.38) | 1.1153 | 0.461 | (0.83, 1.49) | 1.356 | 0.0267 | (1.04, 1.78) |
| Sex | |||||||||
| Female | ref | ref | ref | ref | ref | ref | ref | ref | ref |
| Male | 0.8897 | 0.7484 | (0.44, 1.82) | 0.8681 | 0.6522 | (0.47, 1.61) | 0.7174 | 0.2531 | (0.41, 1.27) |
| Education | |||||||||
| Primary Schooling | ref | ref | ref | ref | ref | ref | ref | ref | ref |
| Technical-prof Training | 4.5914 | 0.0972 | (0.76, 27.81) | 0.779 | 0.6737 | (0.24, 2.49) | 1.9223 | 0.251 | (0.63, 5.87) |
| Secondary Schooling | 3.2845 | 0.2051 | (0.52, 20.67) | 0.4152 | 0.1522 | (0.12, 1.38) | 0.8816 | 0.828 | (0.28, 2.75) |
| Undergraduate Degree | 3.671 | 0.1428 | (0.64, 20.9) | 0.4824 | 0.1869 | (0.16, 1.42) | 0.7616 | 0.6084 | (0.27, 2.16) |
| Postgraduate studies | 1.4827 | 0.7517 | (0.13, 17.01) | 0.3741 | 0.2322 | (0.07, 1.88) | 0.6702 | 0.6021 | (0.15, 3.02) |
| Occupation | |||||||||
| Governmental Employee | ref | ref | ref | ref | ref | ref | ref | ref | ref |
| Private Sector | 1.7084 | 0.5974 | (0.23, 12.46) | 2.4447 | 0.2919 | (0.46, 12.89) | 3.3446 | 0.1322 | (0.69, 16.11) |
| Freelance | 1.5109 | 0.5863 | (0.34, 6.68) | 1.6875 | 0.4122 | (0.48, 5.89) | 1.9182 | 0.2746 | (0.6, 6.17) |
| Unemployed | 1.3888 | 0.5409 | (0.48, 3.98) | 1.103 | 0.8266 | (0.46, 2.65) | 1.4644 | 0.3546 | (0.65, 3.28) |
OR: Odds Ratio; P: p value; CI: Confidence Interval; Ref: reference value.
Discussion
The present study offers a critical examination of the mental health impact on IDPs in the Gaza Strip in the context of the ongoing war and forced displacement, with findings underscoring the widespread prevalence of anxiety, PTSD, and depression. The high co-occurrence of these three mental health issues is particularly noteworthy, with 63% of participants displaying significant indicators of all three. Furthermore, the prevalence of PTSD is strikingly high, affecting nearly 68% of participants based on DSM-5 criteria and 88% when using the PCL-5 cutoff.
While high rates of anxiety, PTSD, and depression have been consistently observed among IDPs in war settings, the prevalence recorded in this study surpasses previous estimates from Palestine19,21,22 and other war-affected regions. A study in Northwest Ethiopia utilizing the PCL-5 with a cutoff ≥ 33, PHQ-9 with a cutoff ≥ 10, and the anxiety subscale of the DASS-21 instrument found a PTSD prevalence of 40.8% among war survivors. Furthermore, two out of three participants with PTSD also exhibited probable depression and anxiety, in contrast to one in three participants without PTSD. 43 Another recent study on depression among IDPs in two camps in northwestern Ethiopia, utilizing the PHQ-9 instrument with a cutoff score of ≥ 10, found a prevalence rate of 62.2%. 44 A study on displaced Iraqis and Syrians using the PCL-5 reported PTSD rates of 43% and 67.6%, respectively, according to the DSM-V and a cutoff value ≥ 23. 45 Additionally, another study found that the prevalence of PTSD among Yazidi, Christian, and Muslim asylum seekers in Iraqi Kurdistan was 48.7% determined using a PCL-5 ≥ 33, while depressive symptoms ranged from 56% to 68%, assessed using the PHQ-9. 46 Studies from other conflict settings further illustrate the heavy psychological burden of displacement. In Juba, South Sudan, 41.8% of displaced individuals meet the criteria for PTSD as assessed by the Harvard Trauma Questionnaire, while 50% fulfill the criteria for depression based on the Hopkins Symptom Checklist-25. 23 Additionally, using the PCL-C and HSCL-25 scales, 53.4%, 80.7%, and 80.3% of displaced persons in Nepal reported experiencing PTSD, anxiety, and depression, respectively. 24 The use of different scales and cutoff values limits the ability to compare anxiety and depression rates. However, regarding PTSD, and considering that many of these studies applied a single cutoff-based criterion of PCL-5 ≥33 or ≥23, the reported rates are lower than the 88.2% and 76.0% prevalence rates observed in our study using the same cutoff scores, respectively, and are similar to the rate reported among displaced Syrians using the dual criteria employed in our study. 45 This emphasizes the exceptional severity of psychological distress among Gaza's displaced population and aligns with the unprecedented scale of destruction they have experienced.
Several factors likely contribute to this heightened burden of psychiatric comorbidities in Gaza. Unlike many other IDP populations that may eventually find stability or refuge in host communities, displaced Gazans remain trapped in an active war zone, with no opportunity for resettlement, safety, or recovery. Repeated displacements, continuous exposure to aerial bombardment, and the destruction of entire neighborhoods have created an environment in which trauma is both pervasive and ongoing. Additionally, while economic hardship is a common aspect among war-displaced populations, Gaza's prolonged blockade and total infrastructural collapse have left the population with even fewer economic coping mechanisms, thereby exacerbating the psychological toll.
As the war continued to grind on, the population remained exposed to continuous stress and potential trauma with no prospect of respite or recovery. Under such conditions, PTSD symptoms such as hyperarousal and avoidance may no longer be mere remnants of past traumatic experiences but rather adaptive mechanisms necessary for survival. 47 This perspective challenges the conventional conceptualization of PTSD, which assumes that trauma is a discrete event followed by a post-trauma phase. In contexts of protracted conflict, the very notion of “post-traumatic” becomes problematic, as the trauma is ongoing and cumulative. Longitudinal research on Palestinian populations has highlighted the persistence of trauma-related symptoms across decades, prompting some scholars to propose alternative diagnostic frameworks, such as Chronic Traumatic Stress Disorder (CTSD). 48
The diagnostic limitations of PTSD in such settings have been recognized in the ICD-11, which now distinguishes between PTSD and Complex PTSD (CPTSD). 49 CPTSD encompasses the core symptoms of PTSD along with additional disturbances in self-organization, including affective dysregulation, a pervasive sense of worthlessness, and profound difficulties in forming and maintaining interpersonal relationships. 49 These symptoms suggest that war-related psychological distress may not only be limited to PTSD but could also contribute to long-term personality alterations. Indeed, severe and prolonged trauma has been previously associated with an increased risk of personality disorders, particularly among individuals who have experienced chronic exposure to violence.50,51 The implications of this are particularly concerning for Gaza's displaced population, where nearly the entire community has endured multiple forced migrations, loss of family members, and the destruction of their homes, all while remaining under the constant threat of renewed violence.
In this study, several sociodemographic and war-related factors emerged as significant predictors of psychiatric disorders. The findings highlight the disproportionate psychological burden borne by displaced women, a pattern that has been consistently reported in war-affected populations.23,44,52 Women reported significantly higher levels of anxiety and medical staff burnout, respectively, in two recent studies from the Gaza Strip during the war.19,53 Moreover, the impact of forced displacement was reflected in the significant associations between the number of migrations and the severity of psychiatric comorbidities. Each additional displacement increased the risk of PTSD, a finding that aligns with previous research documenting cumulative trauma as a key determinant of persistent post-traumatic stress symptoms. 8 Economic precarity also emerged as a critical factor in mental health outcomes, with unemployment and private-sector employment acting as predictors of PTSD. The war's destruction of economic infrastructure and the consequent loss of livelihood opportunities have left a substantial portion of the population in extreme financial insecurity, exacerbating psychological distress. A correlation between poor income and psychiatric comorbidity has been established in previous studies from the Gaza Strip54,55 and other areas.46,56 Financial instability restricts access to healthcare and basic needs, prolonging the stress response and reinforcing a sense of powerlessness.
Particularly concerning is the strong association between military detention, torture, and the likelihood of developing PTSD and depression. Detention and torture have been well-documented as severe psychological stressors, often resulting in long-term psychiatric sequelae, including PTSD, depressive disorders, and persistent cognitive disturbances. 57 The Gaza war has been marked by reports of mass detentions and allegations of mistreatment, adding another dimension of trauma to an already vulnerable population. 19 The elevated prevalence of psychiatric disorders among those subjected to these experiences in our study underscores the urgent need for targeted mental health interventions for survivors of such extreme violence.
The structural devastation in Gaza has further exacerbated the mental health crisis by limiting access to essential psychological and medical services. The destruction of healthcare infrastructure and the ongoing blockade have significantly restricted access to professional psychiatric care, reinforcing the persistence and severity of untreated mental health conditions.18,26 Given these constraints, alternative community-based mental health support mechanisms must be explored to mitigate the long-term psychological impact of the war and displacement.
Limitations and Future Research Directions
While this study offers valuable insights into the mental health crisis suffered by Gaza's displaced population, several limitations should be acknowledged. The reliance on a convenience sampling method, although dictated by logistical and safety constraints, limits the generalizability of findings beyond the surveyed areas. Additionally, although standardized screening tools were utilized, the study did not incorporate clinical interview-based diagnoses, which is the gold standard diagnostic tool. This may have led to either an overestimation or an underestimation of mental health disorders. Furthermore, considering the protracted nature of the conflict and the ongoing humanitarian crisis, more longitudinal research is necessary to track the long-term mental health trajectories of the displaced population and to inform evidence-based strategies for alleviating the psychiatric consequences of war. Furthermore, given the diagnostic challenges of PTSD in prolonged conflict settings, future research should investigate alternative frameworks, such as CTSD and CPTSD, which could offer a more accurate representation of the enduring psychological burden on affected populations. Lastly, although the vast majority of the Gaza Strip's population has been displaced due to hostilities, a similar study involving non-displaced residents could complement this study's insights into the mental health crisis in Gaza. Despite these limitations, the findings provide a crucial snapshot of the profound psychological distress experienced by Gaza's IDPs, highlighting the urgent need for targeted mental health interventions and broader humanitarian efforts to address the long-term impacts of war and displacement on civilian populations.
Conclusion
The results of this study highlight an unprecedented mental health crisis among displaced individuals in Gaza, with exceptionally high rates of psychiatric comorbidities driven by recurrent displacement, loss of livelihood, and extreme violence. These findings call for an urgent and coordinated response from international humanitarian organizations, local stakeholders, and mental health professionals. To effectively address the psychological suffering of the affected population, we recommend the implementation of scalable and culturally sensitive mental health interventions. These include community-based mental health and psychosocial support (MHPSS) programs, the training of non-specialist health workers through frameworks such as the WHO's mhGAP, and the use of digital mental health platforms to expand access in hard-to-reach areas. Trauma-informed care models should also be integrated across health and social service systems. While challenges such as damaged infrastructure and resource constraints remain, these strategies are feasible through collaboration with local NGOs, the use of existing community networks, and leveraging mobile technologies. Prioritizing these approaches is essential to support long-term mental health recovery in Gaza and other war-affected regions.
Supplemental Material
Supplemental material, sj-jpg-1-css-10.1177_24705470251334943 for The Psychological Toll of War and Forced Displacement in Gaza: A Study on Anxiety, PTSD, and Depression by Belal Aldabbour, Mariam El-Jamal, Amal Abuabada, Aseel Al-Dardasawi, Eman Abusedo, Huda Abu Daff, Hala Al-Saqqa, Doaa Abu Helal, Rawan Abu Radwan, Rola El-Hindawi, Mariam Hamada, Wafaa Abu Khader and Latefa Ali Dardas in Chronic Stress
Supplemental material, sj-docx-2-css-10.1177_24705470251334943 for The Psychological Toll of War and Forced Displacement in Gaza: A Study on Anxiety, PTSD, and Depression by Belal Aldabbour, Mariam El-Jamal, Amal Abuabada, Aseel Al-Dardasawi, Eman Abusedo, Huda Abu Daff, Hala Al-Saqqa, Doaa Abu Helal, Rawan Abu Radwan, Rola El-Hindawi, Mariam Hamada, Wafaa Abu Khader and Latefa Ali Dardas in Chronic Stress
Acknowledgements
The authors acknowledge the contribution of Hossam Elsheikh Khalil, MD, in preparing Figure 1.
Author Biographies
Belal Aldabbour is a board-certified neurologist and an Assistant Professor of Neurology and Neuroscience at the Faculty of Medicine, Islamic University, Gaza, Palestine. His research focuses on generating local data in the fields of neurology, psychiatry, and public health to elevate the underrepresented local community of the Gaza Strip onto the international stage.
Mariam El-Jamal obtained a Master's degree in Public Health/Epidemiology & Biostatistics from the American University of Beirut. She is an independent researcher focusing on mental health.
Amal Abuabada is a double-boarded psychiatrist at the Gaza Community Mental Health Program. Her research is focused on uncovering the mental health impacts of repeated armed conflicts in the Gaza Strip on the community.
Aseel Al-Dardasawi was a 6th-year student at the Islamic University of Gaza Faculty of Medicine who graduated in the February 2025 class.
Eman Abusedo was a 6th-year student at the Islamic University of Gaza Faculty of Medicine who graduated in the February 2025 class.
Huda Abu Daff was a 6th-year student at the Islamic University of Gaza Faculty of Medicine who graduated in the February 2025 class.
Hala Al-Saqqa was a 6th-year student at the Islamic University of Gaza Faculty of Medicine who graduated in the February 2025 class.
Doaa Abu Helal was a 6th-year student at the Islamic University of Gaza Faculty of Medicine who graduated in the February 2025 class.
Rawan Abu Radwan was a 6th-year student at the Islamic University of Gaza Faculty of Medicine who graduated in the February 2025 class.
Rola El-Hindawi was a 6th-year student at the Islamic University of Gaza Faculty of Medicine who graduated in the February 2025 class.
Mariam Hamada was a 6th-year student at the Islamic University of Gaza Faculty of Medicine who graduated in the February 2025 class.
Wafaa Abu Khader was a 6th-year student at the Islamic University of Gaza Faculty of Medicine who graduated in the February 2025 class.
Latefa Ali Dardas is a credentialed psychiatric and mental health nurse specializing in child and adolescent mental health (North Carolina, USA). She is an Associate Professor and Assistant Dean for Quality and Development at the University of Jordan School of Nursing.
ORCID iD: Belal Aldabbour https://orcid.org/0000-0001-9186-4039
Amal Abuabadahttps://orcid.org/0000-0001-7684-8110
Latefa Ali Dardas https://orcid.org/0000-0001-5437-4778
Statements and Declarations
Ethics Approval and Consent to Participate: Ethical approval was obtained from the Institutional Review Board (IRB) at the Islamic University of Gaza (IUG). The research was conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from all participants, emphasizing confidentiality and voluntary participation, and no identifying information was collected. Clinical trial number: not applicable.
Consent for Publication: Not applicable.
Authors’ Contributions: BA and AA conceptualized the study. BA, ME, AA, and LAD contributed to the literature review, study design, and tool development. AAD, EA, HAD, HAS, DAH, RR, REH, MH, and WK collected the data. BA and ME analyzed the data. BA, ME, AA and LD led the writing of the study manuscript. All authors contributed to the manuscript revision and have approved the final version.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Availability of Data and Materials: Available from the corresponding author upon reasonable request.
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Miller KE, Rasmussen A. War exposure, daily stressors, and mental health 15 years on: Implications of an ecological framework for addressing the mental health of conflict-affected populations. Epidemiol Psychiatr Sci. 2024;33:e78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moreno-Chaparro J, Piñeros-Ortiz S, Rodríguez-Ramírez L, Urrego-Mendoza Z, Garzón-Orjuela N, Eslava-Schmalbach J. Mental health consequences of armed conflicts in adults: An overview. Actas Esp Psiquiatr. 2022;50(2):68–91. [PMC free article] [PubMed] [Google Scholar]
- 3.Hoppen TH, Priebe S, Vetter I, Morina N. Global burden of post-traumatic stress disorder and major depression in countries affected by war between 1989 and 2019: a systematic review and meta-analysis. BMJ Glob Health. 2021;6(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murthy RS, Lakshminarayana R. Mental health consequences of war: A brief review of research findings. World Psychiatry. 2006;5(1):25–30. [PMC free article] [PubMed] [Google Scholar]
- 5.Cardozo BL, Bilukha OO, Crawford CA, et al. Mental health, social functioning, and disability in postwar Afghanistan. Jama. 2004;292(5):575–584. [DOI] [PubMed] [Google Scholar]
- 6.Steel Z, Chey T, Silove D, Marnane C, Bryant RA, van Ommeren M. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: A systematic review and meta-analysis. Jama. 2009;302(5):537–549. [DOI] [PubMed] [Google Scholar]
- 7.Manafe N, Ismael-Mulungo H, Ponda F, et al. Prevalence and associated factors of common mental disorders among internally displaced people by armed conflict in Cabo Delgado, Mozambique: a cross-sectional community-based study. Front Public Health. 2024;12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morina N, Stam K, Pollet TV, Priebe S. Prevalence of depression and posttraumatic stress disorder in adult civilian survivors of war who stay in war-afflicted regions. A systematic review and meta-analysis of epidemiological studies. J Affect Disord. 2018;239:328–338. [DOI] [PubMed] [Google Scholar]
- 9.Aysazci-Cakar F, Schroder T, Hunt N. A systematic review of prevalence and correlates of post-traumatic stress disorder, depression and anxiety in displaced Syrian population. Journal of Affective Disorders Reports. 2022;10:100397. [Google Scholar]
- 10.Lushchak O, Velykodna M, Bolman S, Strilbytska O, Berezovskyi V, Storey KB. Prevalence of stress, anxiety, and symptoms of post-traumatic stress disorder among Ukrainians after the first year of Russian invasion: a nationwide cross-sectional study. The Lancet Regional Health – Europe. 2024;36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vaktskjold A, Yaghi M, Balawi U, Iversen B, Venter W. The mortality in Gaza in July—September 2014: A retrospective chart-review study. Confl Health. 2016;10(1):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jebril M, Deakin S. The political economy of health in the Gaza strip: Reversing de-development. J Glob Health. 2022;12:03014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.OCHAOPT. Reported impact snapshot | Gaza Strip (29 October 2024). 2024 29 Oct 2024.
- 14.Alnabih A, Alnabeh N-A, Aljeesh Y, Aldabbour B. Food insecurity and weight loss during wartime: A mixed-design study from the Gaza strip. Journal of Health, Population and Nutrition. 2024;43(1):222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khatib R, McKee M, Yusuf S. Counting the dead in Gaza: Difficult but essential. Lancet. 2024;404(10449):237–238. [DOI] [PubMed] [Google Scholar]
- 16.Amnesty International investigation concludes Israel is committing genocide against Palestinians in Gaza [press release]. AMNESTY, 5/12/2024 2024.
- 17.Application of the Convention on the Prevention and Punishment of the Crime of Genocide in the Gaza Strip (South Africa v. Israel) [press release]. 26/1/2024 2024.
- 18.GCMHP. “There, People Suffer And Die”: A Qualitative Analysis Report 2024. Gaza Community Mental Health Program; 2024.
- 19.Aldabbour B, Abuabada A, Lahlouh A, et al. Psychological impacts of the Gaza war on Palestinian young adults: A cross-sectional study of depression, anxiety, stress, and PTSD symptoms. BMC Psychol. 2024;12(1):696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.UNRWA. UNRWA Situation Report #147 on the Humanitarian Crisis in the Gaza Strip and the West Bank, including East Jerusalem 2024 [Available from: https://www.unrwa.org/resources/reports/unrwa-situation-report-147-situation-gaza-strip-and-west-bank-including-east-jerusalem.
- 21.Marie M, SaadAdeen S, Battat M. Anxiety disorders and PTSD in Palestine: A literature review. BMC Psychiatry. 2020;20(1):509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Agbaria N, Petzold S, Deckert A, et al. Prevalence of post-traumatic stress disorder among Palestinian children and adolescents exposed to political violence: A systematic review and meta-analysis. PLoS One. 2021;16(8):e0256426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Roberts B, Damundu EY, Lomoro O, Sondorp E. Post-conflict mental health needs: A cross-sectional survey of trauma, depression and associated factors in Juba, southern Sudan. BMC Psychiatry. 2009;9(1):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thapa SB, Hauff E. Psychological distress among displaced persons during an armed conflict in Nepal. Soc Psychiatry Psychiatr Epidemiol. 2005;40(8):672–679. [DOI] [PubMed] [Google Scholar]
- 25.Alpak G, Unal A, Bulbul F, et al. Post-traumatic stress disorder among Syrian refugees in Turkey: A cross-sectional study. Int J Psychiatry Clin Pract. 2015;19(1):45–50. [DOI] [PubMed] [Google Scholar]
- 26.Taha AM, Sabet C, Nada SA, Abuzerr S, Nguyen D. Addressing the mental health crisis among children in Gaza. Lancet Psychiatry. 2024;11(4):249–250. [DOI] [PubMed] [Google Scholar]
- 27.Beiraghdar F, Momeni J, Hosseini E, Panahi Y, Negah SS. Health crisis in Gaza: The urgent need for international action. Iran J Public Health. 2023;52(12):2478–2483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Morina N, Akhtar A, Barth J, Schnyder U. Psychiatric Disorders in Refugees and Internally Displaced Persons After Forced Displacement: A Systematic Review. Front Psychiatry. 2018;9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Council NR. Rebuilding Gaza - the paradox of shelter without resources. 2024. 30/10/2024. Contract No.: 11/1/2025.
- 30.OCHAOPT. Gaza Crisis 2023 - Shelter Situation Update, 7th January 2024. OCHA; 2024 10/1/2024.
- 31.Pfizer I. Generalized Anxiety Disorder 7-Item Scale Arabic Version 2010 [Available from: https://www.phqscreeners.com/images/sites/g/files/g10060481/f/201412/GAD7_Arabic%20for%20Tunisia.pdf.
- 32.Pfizer I. The PHQ9 Arabic for Israel 2010 [Available from: https://www.phqscreeners.com/images/sites/g/files/g10060481/f/201412/PHQ9_Arabic%20for%20Israel.pdf.
- 33.Ibrahim H, Ertl V, Catani C, Ismail AA, Neuner F. The validity of posttraumatic stress disorder checklist for DSM-5 (PCL-5) as screening instrument with Kurdish and Arab displaced populations living in the Kurdistan region of Iraq. BMC Psychiatry. 2018;18(1):259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med. 2006;166(10):1092–1097. [DOI] [PubMed] [Google Scholar]
- 35.Plummer F, Manea L, Trepel D, McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: A systematic review and diagnostic metaanalysis. Gen Hosp Psychiatry. 2016;39:24–31. [DOI] [PubMed] [Google Scholar]
- 36.Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. J Trauma Stress. 2015;28(6):489–498. [DOI] [PubMed] [Google Scholar]
- 37.Klein AB, Schnurr PP, Bovin MJ, Friedman MJ, Keane TM, Marx BP. An empirical investigation of definitions of subthreshold posttraumatic stress disorder. J Trauma Stress. 2024;37(1):113–125. [DOI] [PubMed] [Google Scholar]
- 38.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Manea L, Gilbody S, McMillan D. Optimal cut-off score for diagnosing depression with the patient health questionnaire (PHQ-9): A meta-analysis. Cmaj. 2012;184(3):E191–E196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Policastro F, Rossi A, Sulaiman HM, Taib NI. Adaptation, validity, and reliability of the patient health questionnaire (PHQ-9) in the Kurdistan region of Iraq. Healthcare. 2023;11(4):598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Searle AK, Van Hooff M, McFarlane AC, et al. Screening for depression and psychological distress in a currently serving military population: The diagnostic accuracy of the K10 and the PHQ9. Assessment. 2019;26(8):1411–1426. [DOI] [PubMed] [Google Scholar]
- 42.Ahmadi A, Ponder WN, Carbajal J, et al. Validation of the PCL-5, PHQ-9, and GAD-7 in a sample of veterans. J Occup Environ Med. 2023;65(8):643–654. [DOI] [PubMed] [Google Scholar]
- 43.Teshome AA, Abebe EC, Mengstie MA, et al. Post-traumatic stress disorder and associated factors among adult war survivors in northwest Ethiopia: Community-based, cross-sectional study. Front Psychiatry. 2023;14:1083138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tadesse G, Nakie G, Fentahun S, et al. Depressive symptoms and correlations among war-survivor internally displaced persons in two IDP camps in northwest Ethiopia: A cross-sectional survey. BMC Public Health. 2025;25(1):1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ibrahim H, Catani C, Ismail AA, Neuner F. Dimensional structure and cultural invariance of DSM V post-traumatic stress disorder among Iraqi and Syrian displaced people. Front Psychol. 2019;10:1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Richa S, Herdane M, Dwaf A, et al. Trauma exposure and PTSD prevalence among Yazidi, Christian and Muslim asylum seekers and refugees displaced to Iraqi Kurdistan. PLoS One. 2020;15(6):e0233681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McKernan B. ‘Chronic traumatic stress disorder’: the Palestinian psychiatrist challenging western definitions of trauma. The Guardian. 2024. [cited 2025 8/1/2025]. Available from: https://www.theguardian.com/world/2024/apr/14/mental-health-palestine-children. [Google Scholar]
- 48.Altawil MAS, El-Asam A, Khadaroo A. Impact of chronic war trauma exposure on PTSD diagnosis from 2006 −2021: A longitudinal study in Palestine. Middle East Current Psychiatry. 2023;30(1):14. [Google Scholar]
- 49.Karatzias T, Murphy P, Cloitre M, et al. Psychological interventions for ICD-11 complex PTSD symptoms: Systematic review and meta-analysis. Psychol Med. 2019;49(11):1761–1775. [DOI] [PubMed] [Google Scholar]
- 50.Powers A, Petri JM, Sleep C, et al. Distinguishing PTSD, complex PTSD, and borderline personality disorder using exploratory structural equation modeling in a trauma-exposed urban sample. J Anxiety Disord. 2022;88:102558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Munjiza J, Britvic D, Radman M, Crawford MJ. Severe war-related trauma and personality pathology: A case-control study. BMC Psychiatry. 2017;17(1):100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Taha PH, Sijbrandij M. Gender Differences in Traumatic Experiences, PTSD, and Relevant Symptoms among the Iraqi Internally Displaced Persons. Int J Environ Res Public Health. 2021;18(18). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Aldabbour B, Dardas LA, Hamed L, et al. Emotional exhaustion, depersonalization, and personal accomplishment: Exploring burnout in Gaza’s healthcare workforce during the war. Middle East Current Psychiatry. 2025;32(1):25. [Google Scholar]
- 54.Aziz A, Thabet S, Chih A, Huang W. Trauma, PTSD, anxiety, and resilience in Palestinian children in the Gaza strip. British Journal of Education, Society & Behavioural Science. 2015;11:1–13. [Google Scholar]
- 55.Qeshta H, Al_Hawajri A, Aziz A. The Relationship between War Trauma, PTSD, Anxiety and Depression among Adolescents in the Gaza Strip. 2019.
- 56.Amsalem D, Haim-Nachum S, Lazarov A, et al. The effects of war-related experiences on mental health symptoms of individuals living in conflict zones: A longitudinal study. Sci Rep. 2025;15(1):889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.de CWAC, van der Merwe J. The psychological impact of torture. Br J Pain. 2013;7(2):101–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-jpg-1-css-10.1177_24705470251334943 for The Psychological Toll of War and Forced Displacement in Gaza: A Study on Anxiety, PTSD, and Depression by Belal Aldabbour, Mariam El-Jamal, Amal Abuabada, Aseel Al-Dardasawi, Eman Abusedo, Huda Abu Daff, Hala Al-Saqqa, Doaa Abu Helal, Rawan Abu Radwan, Rola El-Hindawi, Mariam Hamada, Wafaa Abu Khader and Latefa Ali Dardas in Chronic Stress
Supplemental material, sj-docx-2-css-10.1177_24705470251334943 for The Psychological Toll of War and Forced Displacement in Gaza: A Study on Anxiety, PTSD, and Depression by Belal Aldabbour, Mariam El-Jamal, Amal Abuabada, Aseel Al-Dardasawi, Eman Abusedo, Huda Abu Daff, Hala Al-Saqqa, Doaa Abu Helal, Rawan Abu Radwan, Rola El-Hindawi, Mariam Hamada, Wafaa Abu Khader and Latefa Ali Dardas in Chronic Stress