Abstract
Background
White spot lesion formation around orthodontic brackets is a major complication associated with fixed orthodontic treatment.
Objective
This review aimed to evaluate the current evidence regarding the differences in white spot lesion formation between self-ligating and conventional ligating brackets.
Methods
Eleven bibliographic databases were searched until January 2025. This review covered parallel-group and split-mouth randomized controlled trials, controlled clinical trials, and cross-sectional studies that investigated the differences in white spot lesion formation between self-ligating and conventional ligating brackets.
Results
Three randomized controlled trials, one controlled clinical trial, and one cross-sectional study were included in this systematic review. Among these, three studies were classified as having a low risk of bias. Four of the five included studies showed no statistically significant difference in white spot lesion formation between the two types of bracket systems (p < 0.05).
Conclusion
There are no potential differences in white spot lesion formation between self-ligating and conventional ligating bracket systems. However, orthodontists must be aware of the other factors affecting white spot lesion formation, with oral hygiene being the most critical factor.
Registration: The protocol was registered in the PROSPERO database (CRD42022353478) on 25 August 2022.
Keywords: Ligation, orthodontic bracket, systematic review, white spot lesion
Introduction
White spot enamel lesion formation around orthodontic brackets is one of the most critical complications experienced by patients following fixed orthodontic treatment. 1 This undesirable condition can cause irreversible tooth structure loss and poor aesthetic outcomes; moreover, in severe cases, the lesion may extend to the dentin tissue, causing tooth sensitivity and endodontic complications. 2 The bacteria in dental biofilms are always metabolically active; some of these bacteria can ferment a carbohydrate substrate to produce acid, causing the pH to fall to below 5 within 1–3 min. Repeated decline in pH may result in decalcification of the tooth surface, leading to the formation of white spot lesion (WSL). 3 WSL appears as an opaque, milky-white colored lesion on the smooth surface of the tooth, which is characterized by the demineralization process of the enamel.4,5 Unfortunately, there is an increased incidence of WSL during orthodontic treatment. A previous study reported that 50% of the orthodontic patients had one or more WSL at the end of treatment. 6
Various materials and approaches have been utilized to manage demineralization of the enamel surface and subsurface following orthodontic treatment. These include fluorides, chicken eggshell paste, infiltrative resins, microabrasion, and restorative approaches.7,8
Orthodontic appliance components, such as brackets, wires, ligatures, elastics, bands, and acrylic expanders, can cause plaque retention and biofilm formation, leading to enamel demineralization.1,6,9 Many factors contribute to this risk, including the retentive nature of multi-bracketed appliances, reduced mechanical cleaning by the cheeks and tongue, and inadequate oral hygiene compliance.1,10,11
Bracket types exhibit various physical characteristics.12,13 Thus, they can directly affect the amount of biofilm formation 14 and plaque retention. 15
Different types of fixed orthodontic appliances are available currently. However, they can be classified into two major categories based on the ligation method. The first category is conventional ligating brackets (CLBs), which rely on either a stainless steel ligature or an elastomeric ring to ensure reliable insertion of the orthodontic wire into the slot.16,17 The second category is self-ligating brackets (SLBs), which have a mechanism for closing and opening the slot and maintaining permanent insertion of the wire inside the slot, thereby eliminating the need for any metal or elastomeric ligature.16,18
Each type of bracket has advantages and disadvantages. According to manufacturers and some studies,19–22 compared with CLBs, SLBs allow better hygiene and are less prone to biofilm formation due to their physical shape and the absence of elastic and metal ligatures, which also promote reductions in the development of WSL. Forsberg et al. 16 and Akin et al. 18 reported that elastomeric ligation was associated with substantial biofilm retention and more accumulation of microorganisms compared with SLB systems, which increase the risk of enamel demineralization. Conversely, several studies23–26 have found no differences in WSL formation and plaque retention between CLBs and SLBs.
The literature has provided conflicting results regarding plaque retention and WSL formation between CLBs and SLBs. It is crucial to have evidence on the best orthodontic bracket system that can help orthodontists achieve treatment goals with minimal biofilm accumulation and enamel demineralization. Several systematic reviews have been conducted to investigate biofilm formation 27 and microbial colonization28,29 around CLBs and SLBs. However, no systematic review has specifically explored WSL formation around these two bracket types. The present systematic review aimed to determine whether there exist any differences in WSL formation between SLB and CLB systems.
Materials and method
Protocol registration
This systematic review adhered to the guidelines of Cochrane handbook for systematic reviews of interventions. 30 This study has been reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement Guidelines 2020. 31 The protocol was registered in the PROSPERO database (CRD42022353478) on 25 August 2022.
Eligibility criteria
This review used the population, intervention, comparison, outcome, and study design (PICOS) framework to define the eligibility criteria: (a) population (P): patients of any age or sex who have received fixed orthodontic appliances on their upper, lower, or both arches, without any dental extraction; (b) intervention (I): patients treated with any SLB system; (c) comparison (C): patients treated with any CLB system; (d) outcome (O): WSL formation; and (e) study design (S): randomized controlled trials (RCTs), controlled clinical trials (CCTs), and cross-sectional studies.
Conversely, case reports, case series, finite element analysis studies, editorials, reviews, personal opinions, abstracts with insufficient data, in vitro studies, animal trials, and other nonclinical studies were excluded from this systematic review.
Search strategy
A comprehensive thorough search was conducted independently by two researchers without language restrictions. The search covered multiple databases from their inception until January 2025, including PubMed, the Cochrane Central Register of Controlled Trials, Trip, CINAHL via EBSCO, Scopus, Web of Science, EMBASE via OVID, Google Scholar, and ProQuest. The ongoing and unpublished trials were electronically identified through the World Health Organization’s International Clinical Trials Registry Platform and Clinical Trials databases.
In addition, a manual search was conducted in the reference lists of the full-text articles eligible for inclusion and relevant systematic reviews. Additional details of the search strategy are provided in Table 1.
Table 1.
Electronic search strategy.
| Database | Search strategy | n |
|---|---|---|
| PubMed® | #1 Self-ligating bracket OR Self-ligation braces OR Self-ligat* OR Self ligat* OR Ligat* OR Conventional bracket OR Traditional braces OR Elastomeric ligation OR Elast* AND #2 White spot lesion OR carious lesions OR carious white spot OR dental caries OR enamel demineralization OR Decalcification OR DMFT Or initial caries lesion. | 610 |
| Cochrane (CENTRAL) | #1 Self-ligating bracket OR Self-ligation braces OR Self-ligat* OR Self ligat* OR Ligat* OR Conventional bracket OR Traditional braces OR Elastomeric ligation OR Elast* AND #2 White spot lesion OR carious lesions OR carious white spot OR dental caries OR enamel demineralization OR Decalcification OR DMFT Or initial caries lesion. | 99 |
| Scopus® | #1TITLE-ABS-KEY (self-ligating AND bracket OR self-ligation AND braces OR self-ligat* OR self AND ligat* OR conventional AND bracket OR traditional AND braces OR elastomeric AND ligature OR ligat* OR elast*). AND #2TITLE-ABS-KEY (white AND spot AND lesion OR carious AND lesions OR carious AND white AND spot OR dental AND caries OR enamel AND demineralization OR decalcification OR DMFT OR initial caries lesion). | 70 |
| Web of Science | #1TS = (Self-ligating bracket OR Self-ligation braces OR Self-ligat* OR Self ligat* OR Ligat* OR Conventional bracket OR Traditional braces OR Elastomeric ligation OR Elast*). #2TS = (White spot lesion OR carious lesions OR carious white spot OR dental caries OR enamel demineralization OR Decalcification OR DMFT OR initial caries lesion). | 588 |
| Google Scholar | Self-ligating brackets OR self-ligation braces OR self-ligat* OR “conventional bracket” OR “traditional braces” OR elastomeric ligature. | 633 |
| Trip | Self-ligating bracket OR Self-ligation braces OR Self-ligat* OR Self ligat* OR Ligat* OR Conventional bracket OR Traditional braces OR Elastomeric ligation OR Elast* AND White spot lesion OR carious lesions OR carious white spot OR dental caries OR enamel demineralization OR Decalcification OR DMFT OR initial caries lesion. | 189 |
| CINAHL | Self-ligating bracket OR Self-ligation braces OR Self-ligat* OR Self ligat* OR Ligat* OR Conventional bracket OR Traditional braces OR Elastomeric ligation OR Elast* AND White spot lesion OR carious lesions OR carious white spot OR dental caries OR enamel demineralization OR Decalcification OR DMFT OR initial caries lesion. | 48 |
| Embase | #1 Self-ligating bracket OR Self-ligation braces OR Self-ligat* OR Self ligat* OR Ligat* OR Conventional bracket OR Traditional braces OR Elastomeric ligation OR Elast* AND #2 White spot lesion OR carious lesions OR carious white spot OR dental caries OR enamel demineralization OR Decalcification OR DMFT OR initial caries lesion. | 242 |
| ProQuest | #1 Self-ligating bracket OR Self-ligation braces OR Self-ligat* OR Self ligat* OR Ligat* OR Conventional bracket OR Traditional braces OR Elastomeric ligation OR Elast* AND #2 White spot lesion OR carious lesions OR carious white spot OR dental caries OR enamel demineralization OR Decalcification OR DMFT OR initial caries lesion. | 376 |
| WHO | Self ligation bracket OR self ligation braces OR self-ligation bracket OR self-ligation braces OR self ligating bracket OR Self-ligating bracket OR Self-ligating braces OR Self Ligating braces OR self-ligat* OR self ligat*. | 11 |
| Clinical Trials | Self ligation bracket OR self ligation braces OR self-ligation bracket OR self-ligation braces OR self ligating bracket OR Self-ligating bracket OR Self-ligating braces OR Self Ligating braces OR self-ligat* OR self ligat*. | 17 |
Study selection and data extraction
The two authors (MII and ASB) independently assessed studies according to the inclusion criteria. In case of difference in their judgment, the author (MYH) was consulted to resolve the matter. Initially, duplicate studies were removed using Endnote software (version X9). Subsequently, the remaining records were screened for relevance by assessing their titles and abstracts using Rayyan® QCRI software.
Finally, the full-text of the remaining studies was evaluated by the same two authors to reach the final decision based on the inclusion criteria. 32
Data items
From the included studies, the following information was extracted: author name, year of publication, study design, sample size, sex and age of the participants, intervention, bracket types, outcome assessment method, evaluation time, and outcome measures.
Effect measure
Methodology, outcome assessment time, assessment method, and outcome measures were taken into account when evaluating the heterogeneity of the included studies. Initially, heterogeneity was assessed clinically. For statistical analysis, the number of WSLs and the degree of decalcification were considered. Mean differences with their associated 95% confidence intervals were used to express data as an effect measure in case of continuous outcomes, and the risk ratio was used in case of dichotomous outcomes.
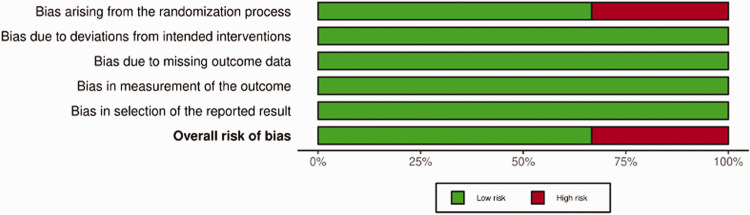
Risk of bias of the included studies
The two authors (MII and ASB) separately assessed the quality of the included studies according to Cochrane guidelines. In case of disagreement between the two authors, the third author (MYH) was asked to resolve the matter. The RoB-2 tool 33 was utilized for the included RCTs. The tool assesses the following five domains: (a) bias arising from the randomization process; (b) bias due to deviations from intended interventions; (c) bias due to missing outcome data; (d) bias in the measurement of the outcome; and (e) bias in the selection of the reported result. Every single domain can be concluded as having a low risk of bias, some concerns, or high risk of bias. The overall judgment of the article was made as follows: (a) low risk of bias if all domains were assessed as a low risk of bias; (b) some concerns if at least one field was evaluated as some concerns, with no domain assessed to be at high risk; or (c) high risk of bias if at least one or more domains were assessed as a high risk of bias.
Furthermore, the ROBINS-I tool 34 was used for CCTs and cross-sectional studies, which assessed the following seven domains: (a) bias due to confounding; (b) bias in the selection of participants; (c) bias in the classification of interventions; (d) bias due to deviations from intended interventions; (e) bias due to missing data; (f) bias in the measurement of outcomes; and (g) bias in the selection of the reported result. Every single domain can be considered to have low, moderate, serious, or critical risk of bias or no information.
Results
Literature search flow and study selection
The search strategy yielded 2883 articles. After removing duplicates, 1743 articles were reviewed. Both independent reviewers (xxx, xxx) applied the exclusion criteria, which led to the exclusion of 1737 articles, which were considered irrelevant to this review. Thus, six articles were considered potentially relevant to the systematic review and chosen for full-text assessment.
Of the six full-text articles assessed, one was excluded, 35 because of the unavailability of the full-text article after journal discontinuation. Therefore, five studies18,23–26 were considered appropriate for the final analysis, including three randomized studies,23–25 one CCT, 26 and one cross-sectional study. 18 The PRISMA flow diagram is presented in Figure 1.
Figure 1.
PRISMA flow chart of the included studies. PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Characteristics of the included studies
Three RCTs,23–25 one CCT, 26 and one cross-sectional study 18 were included in this review. These five included studies were conducted in Turkey, 18 USA, 23 Croatia, 24 UK, 25 and India. 26 A total of 509 patients were included in this review, and the sample size ranged between 13 and 400 patients in each study. Furthermore, the studies had different sex distributions; one study 25 had more males than females, whereas two studies18,23 had more females than males. One study 26 had a similar sex distribution, whereas another study 24 did not mention the sex distribution at all. The patient ages in the included studies ranged between 10 and 35 years.
The study by Buck et al. 23 followed a split-mouth design, whereas the other studies18,24–26 employed a parallel-group design. Two studies24,26 used a Diagnodent pen to measure and detect WSL formation around orthodontic brackets, two studies18,25 depended on digital photographs, and one study 23 utilized both assessment methods.
Furthermore, the included studies varied in the intervention used for teeth. In Buck et al.’s study, 23 the comparison was conducted among four lateral incisors, as an experimental bracket was bonded to a lateral incisor, and a control bracket was bonded to the contralateral incisor. Jurela et al. 24 assessed the incidence of WSL among these teeth (13, 12, 11, 21, 23, 16, 43, 33, and 36). Alshatti et al. 25 studied the incidence and severity of WSL among only the upper lateral incisors. In the CCT of Tiwari et al., 26 the incidence of enamel demineralization was reported among three anterior teeth (13, 11, and 23). In the study by Akin et al., 18 the WSL was scored from the first molar to the first molar on the opposite side for both jaws.
Regarding evaluation time, Jurela et al. 24 assessed the incidence of WSL after 6 months of orthodontic treatment, Buck et al. 23 and Tiwari et al. 26 evaluated the enamel demineralization scores after 12 months of orthodontic treatment, Alshatti et al. 25 assessed the incidence and severity of WSL after 18 months of orthodontic treatment, and Akin et al. 18 assessed the incidence of WSL at the end of orthodontic treatment.
The characteristics of the five included studies are listed in Tables 2 and 3.
Table 2.
Characteristics of the included studies.
| Study (Author, year) | Study design (Country) | Participants (Sample size, male/female) | Participant age | Intervention | Bracket type |
|---|---|---|---|---|---|
| Buck et al. (2011) 23 | RCT(USA) | SP:13 patients (4 males, 9 females) | 12.1–17.2 years | One lateral incisor received SLB, whereas the contralateral incisor received CLB. | IG: SL, 0.022-inch In-Ovation® R, GACCG: standard CLB, 0.022-inch Mini-Ovation®, GAC |
| Akin et al. (2014) 18 | Cross-sectional(Turkey) | IG: 200 (64 males, 136 females)CG: 200 (92 males, 108 females) | 10–18 years | WSL scoring was performed from the first molar to the first molar on the opposite side for both jaws. | IG: (Damon™ 3MX Ormco Glendora, Calif) SLBCG: (Equilibrium® 2, Dentaurum. Phorzeim) CLB |
| Alshatti (2017) 25 | RCT(UK) | IG: 16 patientsCG: 19 patients | IG: 14.82 ± 4.26 yearsCG: 14.47 ± 3.99 years | WSL scoring was performed for only maxillary lateral incisors. | IG: Carriere® SLB, Carlsbad, CACG: pre-adjusted edgewise CLB (PEA) |
| Jurela et al. (2019) 24 | RCT(Croatia) | IG: 21 patientsCG: 21 patients | 15.14 ± 1.66 years | WSL scoring was performed for teeth 13, 12, 11, 21, 23, 16, 43, 33, and 36. | IG: Lotus® Plus, Ortho Technology Inc., Tampa, FLCG: metal C Brackets (Mini Sprint® brackets Forestadent Bernard Forster GmBH) |
| Tiwari et al. (2020) 26 | CCT(India) | IG: 10 patientsCG: 9 patients9 males, 10 females | 20–35 years | WSL scoring was performed for teeth 13, 11, and 23. | IG: SL brackets (Damon™ 3mx Ormco)CG: CLB (3 m™ Gemini 022 MBT brackets) |
RCT: randomized controlled trial; CCT: controlled clinical trial; SP: split-mouth design; IG: intervention group; CG: control group; SLB: self-ligating brackets; CLB: conventional ligating brackets; WSL: white spot lesion
Table 3.
Additional characteristics of the included studies with the main findings.
| Study (Author, year) | Method of outcome assessment | Time of evaluation | Outcome measures | Outcomes and author conclusion |
|---|---|---|---|---|
| Buck et al. (2011) 23 | Photographic records and Diagnodent pen | After 1 year of orthodontic treatment | Analyze WSL formation between CLB and SLB | No differences in WSL formation between the bracket types |
| Akin et al. (2014) 18 | Photographic records | End of the overall treatment | Investigate the incidence of WSL and its relationship with various patient and treatment variables | Incidence of WSL was lower in the SLB group than in the CLB group, but hygiene care was typically an important factor in developing WSL |
| Alshatti (2017) 25 | Intraoral pictures (digital photography) | After 18 months of treatment | Compare the incidence and severity of WSL among CA, SLB, and CLB systems after 9 and 18 month of OT | There were no differences in the incidence and severity of WSL between the two groups |
| Jurela et al. (2019) 24 | Diagnodent pen | Six months after the beginning of fixed orthodontic treatment | Determine the effect of orthodontic therapy on the incidence of WSL | No statistically significant differences were observed in WSL formation between different types of brackets |
| Tiwari et al. (2020) 26 | Diagnodent pen | At 3 and 12 months of orthodontic treatment | Compare ED around SLB and CLB | There were no differences in ED scores at the end of 1 year of OT between SLB and CLB |
WSL: white spot lesion; CLB: conventional ligating brackets; SLB: self-ligating brackets; CA: clear aligners; OT: orthodontic treatment; ED: enamel demineralization
Risk of bias of the included studies
Two RCTs23,25 were assessed as having a low risk of bias, and one RCT 24 was assessed as having a high risk of bias. Bias arising from the randomization process led to the high risk of bias in Jurela et al.’s RCT 24 (Figure 2). The overall risk of bias for each domain is illustrated in Figure 3. Regarding the nonrandomized trials, one study 26 was assessed as having a low risk of bias, and the other 18 was at serious risk of bias. Bias arising from outcome measurement led to the serious risk of bias in Akin et al.’s study 18 (Figure 4). The overall risk of bias for each domain is illustrated in Figure 5. Further details about the reason for each judgment are provided in Supplementary Tables 1 and 2.
Figure 2.
Risk of bias of the included RCTs using the RoB-2 tool. RCTs: randomized controlled trials.
Figure 3.
The overall risk of bias of the included RCTs using the RoB-2 tool. RCTs: randomized controlled trials.
Figure 4.
Risk of bias of the included non-RCTs using the ROBINS-I tool. RCTs: randomized controlled trials.
Figure 5.
The overall risk of bias of the included non-RCTs using the ROBINS-I tool. RCTs: randomized controlled trials.
Effect of intervention
All included studies evaluated WSL formation with SLBs and CLBs. It was not possible to perform a meta-analysis due to several differences among the included studies. There were differences in the WSL assessment times (ranging between 6 and 18 months) and the outcome assessment methods (photograph records and Diagnodent pen).
Four of the five included studies reported no statistically significant difference in WSL formation between SLB and CLB. Buck et al. 23 reported no differences in WSL formation between CLB (0.022-inch Mini-Ovation®, GAC) and SLB (0.022-inch In-Ovation® R, GAC) after 1 year of orthodontic treatment using photographs and Diagnodent pen. Alshatti et al. 25 also used intraoral digital photographs to compare WSL formation among clear aligners, SLB (Carriere® Self-Ligating Bracket, Carlsbad, CA), and CLB (pre-adjusted edgewise). They found no significant differences in the incidence and severity of WSL between SLB and CLB after 18 months of treatment. Jurela et al. 24 used a Diagnodent pen to detect the incidence of WSL among four types of brackets. No statistically significant differences were found between the metal CLB group (Mini Sprint® Bracket, Forestadent Bernard Forster GmBH, Pforzheim, Germany) and the metal SLB group (Lotus® Plus, Ortho Technology Inc., Tampa, FL) after 6 months of orthodontic treatment. Tiwari et al. 26 also used a Diagnodent pen to detect enamel demineralization around SLB (Damon™ 3mx Ormco) and CLB (3m™ Gemini MBT brackets). They found no differences in the enamel demineralization scores after 12 months of orthodontic treatment.
Conversely, the cross-sectional study conducted by Akin et al. 18 utilized photographic records to determine the incidence of WSL in patients treated with SLB (Damon™ 3mx, Ormco, Glendora, Calif) and CLB (Equilibrium® 2, Dentaurum, Phorzeim, Germany). The study showed that SLB led to a lower incidence of WSL than CLB after orthodontic treatment.
Discussion
To the best of our knowledge, this is the first review to evaluate the existing evidence on the difference in WSL formation between CLB and SLB systems. Five studies were included in this systematic review, including three RCTs, one CCT, and one cross-sectional study. It was not possible to conduct a meta-analysis due to several differences among the included studies. There were differences in the assessment times and the methods of outcome assessment.
Four of the five included studies23–26 found no differences in WSL formation between CLBs and SLBs. These results may be attributed to the similar biofilm formation around the two types of brackets, as concluded in a previous systematic review, 27 which showed that there were no significant differences in biofilm formation between elastomeric ligation brackets and self-ligation brackets in patients with fixed orthodontic appliances. Moreover, the systematic review by Nascimento et al. 28 indicated that the type of brackets (conventional or self-ligating) has no influence on microbial colonization and Streptococcus mutans adhesion. Pandis et al. 36 investigated the differences in the microbial contents of saliva samples among these two types of brackets and reported no differences between the two ligation groups.
Akin et al. 18 concluded that the incidence of WSL was lower in the SLB group than in the CLB group. This can be explained by the fact that the hygiene scores of the patients in the two groups during orthodontic treatment were dissimilar. It was observed that the patients’ oral hygiene was comparatively better in the SLB group than in the CLB group. This variance could explain why the SLB group exhibited a lower incidence of WSL than the CLB group. Another factor that may have influenced the results is the assessment method for detecting WSL. They depended only on digital photographs rather than Diagnodent pen, which is the most common tool in the majority of studies on this topic.
Several methods and techniques can be used to detect and characterize WSL, which include clinical examination, photographic records, optical nonfluorescent methods, and optical fluorescent methods, such as Diagnodent. 37 The ideal method should be simple, noninvasive, repeatable, reproducible, and accurate.37,38 However, studies included in this review were dissimilar, as some utilized photographic records and the others depended on Diagnodent pen. Each method has its advantages and disadvantages. However, objective methods, such as Diagnodent pen, are reproducible, repeatable, and expected to have minimal measurement bias compared with photographic records, which do not provide reliable results reflecting the histologic extension of demineralization.26,38,39
Several limitations were observed in the individual studies, which may affect the results obtained. For instance, Buck et al. 23 included only 13 patients, and the WSL outcomes were assessed exclusively on the lateral incisors. Similarly, Alshatti et al. 25 evaluated WSL formation solely on the maxillary lateral incisors, whereas Tiwari et al. 26 restricted their assessment to teeth 13, 11, and 23. In the cross-sectional study by Akin et al. 18 , discrepancies in oral hygiene scores were observed between the two groups, with patients in the SLB group demonstrating better oral hygiene than those in the CLB group. Additionally, in the RCT conducted by Jurela et al. 24 , WSL outcomes were assessed only 6 months after the initiation of orthodontic treatment, which may have impacted the findings.
Regarding potential confounding factors, one study 23 included more than twice as many female patients as males, and two studies24,25 did not report the sex distribution. Furthermore, one study 26 encompassed a broad age range (18–35 years), which could introduce variability in WSL susceptibility.
However, many other factors may affect the incidence and severity of WSL formation around fixed orthodontic brackets, including orthodontic treatment duration, malocclusion type, physical properties and morphological characteristics of the brackets, and proper oral hygiene instructions at every single chairside appointment.
Regarding orthodontic treatment duration, previous studies have demonstrated that the longer the treatment duration, the higher the likelihood of developing WSL.40,41 However, studies included in this review differed on this point. Only one study assessed WSL at the end of orthodontic therapy. 18 In contrast, the other studies measured the outcome after 6–18 months following the adhesion of fixed orthodontic appliances.23–26
Concerning the primary type of malocclusion, it is known that an increase in the severity of teeth crowding is accompanied with a greater accumulation of biofilm, resulting in an increased potential for WSL formation. 42 Unfortunately, none of the five studies clearly reported the type of malocclusion in the patients included in these trials.
With regard to the physical properties and morphological characteristics of the orthodontic braces, it is important to understand that CLBs and SLBs exist in a variety of shapes, sizes, ridges, and retentive surfaces beyond the wings. 43 These characteristics can potentially affect the probability of biofilm formation and may provide an increased number of retention areas around the brackets. However, a wide variety was observed among the brackets utilized in the studies included in this review, as there was no similarity between the studies in terms of either CLBs or SLBs.
However, it is necessary to acknowledge that the most critical factors affecting WSL development during fixed orthodontic therapy are the patient’s oral hygiene and the dental hygienist’s instruction during each treatment appointment.18,40 Consequently, it is imperative for patients and doctors to cooperate in maintaining good oral hygiene during orthodontic therapy.
Limitation
The main limitation of this review was the lack of studies on this topic of clinical practice, as only five were eligible for this systematic review; three of them were RCTs. Moreover, only one study evaluated the outcome after the completion of orthodontic treatment, while in the remaining studies, the outcome was evaluated 6–18 months after the beginning of orthodontic treatment. Furthermore, comparing CLBs with SLBs poses a great challenge because both of them vary widely in terms of shape, size, and retentive surfaces, each with different plaque retention potential.
However, due to the clinical heterogeneity between studies caused by the differences in assessment methods and evaluation times, a meta-analysis was not feasible in this review.
Conclusion
There seem to be no differences in WSL formation between SLBs and CLBs. Therefore, no bracket type is preferred over another with regard to WSL formation. However, because of the small number of studies included in this review, the available evidence was insufficient to determine a strong indication. Therefore, further well-designed RCTs with an adequately calculated sample size should be conducted. Future studies should compare WSL formation between different bracket types at the completion of orthodontic treatment.
Additionally, practitioners should be aware that oral hygiene compliance remains the most influential factor affecting the incidence and severity of WSL, alongside several other contributing factors.
Supplemental Material
Supplemental material, sj-pdf-1-imr-10.1177_03000605251328608 for White spot lesion in self-ligating versus conventional ligating bracket systems: A systematic review by Mohammad I Idris, Ahmad S Burhan, Mohammad Y Hajeer, Ahmad M Alhamwi and Fehmie R Nawaya in Journal of International Medical Research
Supplemental material, sj-pdf-2-imr-10.1177_03000605251328608 for White spot lesion in self-ligating versus conventional ligating bracket systems: A systematic review by Mohammad I Idris, Ahmad S Burhan, Mohammad Y Hajeer, Ahmad M Alhamwi and Fehmie R Nawaya in Journal of International Medical Research
Acknowledgement
Not applicable.
Footnotes
ORCID iD: Mohammad I Idris https://orcid.org/0009-0009-6542-3040
Author’s contributions
MII and ASB searched the literature, examined full-text articles, determined the studies appropriate for inclusion, extracted and processed data, assessed the risk of bias, analyzed and synthesized data both qualitatively and quantitatively, and wrote the initial drafts of this manuscript. ASB helped in formulating the focused review question. MYH supervised the whole procedure, helped resolve disagreements that developed during study selection and risk of bias assessment, and edited the final version of this manuscript. AMA and FRN helped in data entry, data analysis, and preparation of the first draft of this paper. All authors have read and approved the final version of this manuscript.
Availability of data and materials
The datasets associated with this manuscript can be obtained from the corresponding author upon reasonable request.
Clinical trial number of registration
Not applicable (this is a systematic review).
Declaration of conflicting interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate
Not applicable.
Funding
This systematic review was not funded.
Supplementary material
Supplemental material for this article is available online.
References
- 1.Ren Y, Jongsma MA, Mei L, et al. Orthodontic treatment with fixed appliances and biofilm formation–a potential public health threat? Clin Oral Investig 2014; 18: 1711–1718. [DOI] [PubMed] [Google Scholar]
- 2.Al-Blaihed D, El Meligy O, Baghlaf K, et al. White spot lesions in fixed orthodontics: a literature review on etiology, prevention, and treatment. Cureus 2024; 16: e65679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kidd EAM, Fejerskov O. Essentials of dental caries. 4th ed. New York: Oxford University Press, 2016. [Google Scholar]
- 4.Tufekci E, Dixon JS, Gunsolley JC, et al. Prevalence of white spot lesions during orthodontic treatment with fixed appliances. Angle Orthod 2011; 81: 206–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Munjal D, Garg S, Dhindsa A, et al. Assessment of white spot lesions and in-vivo evaluation of the effect of CPP-ACP on white spot lesions in permanent molars of children. J Clin Diagn Res 2016; 10: Zc149–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Al-Ibrahim HM, Hajeer MY, Burhan AS, et al. Evaluation of patient-centered outcomes associated with the acceleration of upper incisor decrowding using self-ligating brackets with or without piezocision in comparison with traditional brackets: a three-arm randomized controlled trial. Cureus 2022; 14: e26467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fathy Abo-Elmahasen MM, Shaaban AM, Elsaharty M, et al. Evaluation of the remineralizing effect of the chicken eggshell paste after removal of the fixed orthodontic appliance: an in vitro study. J Orthod Sci 2024; 13: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Paula AB, Fernandes AR, Coelho AS, et al. Therapies for white spot lesions: a systematic review. J Evid Based Dent Pract 2017; 17: 23–38. [DOI] [PubMed] [Google Scholar]
- 9.Küçükönder A, Hatipoğlu Ö. Comparison between a glass ionomer cement and a compomer concerning bonded acrylic expander retention and white spot formation: a randomized clinical trial. J Orofac Orthop 2023; 84: 157–163. [DOI] [PubMed] [Google Scholar]
- 10.Lucchese A, Bondemark L, Marcolina M, et al. Changes in oral microbiota due to orthodontic appliances: a systematic review. J Oral Microbiol 2018; 10: 1476645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hussein S, Ismail H. Influence of reminder on enhancing compliance in patients with fixed orthodontic appliance treatment (a randomized controlled clinical trial). Patient Prefer Adherence 2023; 17: 1759–1769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anhoury P, Nathanson D, Hughes CV, et al. Microbial profile on metallic and ceramic bracket materials. Angle Orthod 2002; 72: 338–343. [DOI] [PubMed] [Google Scholar]
- 13.Kara-Boulad JM, Burhan AS, Hajeer MY, et al. Evaluation of the oral health-related quality of life (OHRQoL) in patients undergoing lingual versus labial fixed orthodontic appliances: a randomized controlled clinical trial. Cureus 2022; 14: e23379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alexander SA. Effects of orthodontic attachments on the gingival health of permanent second molars. Am J Orthod Dentofacial Orthop 1991; 100: 337–340. [DOI] [PubMed] [Google Scholar]
- 15.Rowshani B, Timmerman MF, Van der Velden U. Plaque development in relation to the periodontal condition and bacterial load of the saliva. J Clin Periodontol 2004; 31: 214–218. [DOI] [PubMed] [Google Scholar]
- 16.Forsberg CM, Brattström V, Malmberg E, et al. Ligature wires and elastomeric rings: two methods of ligation, and their association with microbial colonization of Streptococcus mutans and lactobacilli. Eur J Orthod 1991; 13: 416–420. [DOI] [PubMed] [Google Scholar]
- 17.Alabdullah MM, Burhan AS, Nabawia A, et al. Comparative assessment of dental and basal arch dimensions of passive and active self-ligating versus conventional appliances: a randomized clinical trial. J Orofac Orthop 2023; 84: 74–83. [DOI] [PubMed] [Google Scholar]
- 18.Akin M, Tezcan M, Ileri Z, et al. Incidence of white spot lesions among patients treated with self- and conventional ligation systems. Clin Oral Investig 2015; 19: 1501–1506. [DOI] [PubMed] [Google Scholar]
- 19.Pellegrini P, Sauerwein R, Finlayson T, et al. Plaque retention by self-ligating vs elastomeric orthodontic brackets: quantitative comparison of oral bacteria and detection with adenosine triphosphate-driven bioluminescence. Am J Orthod Dentofacial Orthop 2009; 135: 426.e1–429; discussion 426-427. [DOI] [PubMed] [Google Scholar]
- 20.Damon DH. The rationale, evolution and clinical application of the self-ligating bracket. Clin Orthod Res 1998; 1: 52–61. [DOI] [PubMed] [Google Scholar]
- 21.Shivapuja PK, Berger J. A comparative study of conventional ligation and self-ligation bracket systems. Am J Orthod Dentofacial Orthop 1994; 106: 472–480. [DOI] [PubMed] [Google Scholar]
- 22.Garcez AS, Suzuki SS, Ribeiro MS, et al. Biofilm retention by 3 methods of ligation on orthodontic brackets: a microbiologic and optical coherence tomography analysis. Am J Orthod Dentofacial Orthop 2011; 140: e193–e198. [DOI] [PubMed] [Google Scholar]
- 23.Buck T, Pellegrini P, Sauerwein R, et al. Elastomeric-ligated vs self-ligating appliances: a pilot study examining microbial colonization and white spot lesion formation after 1 year of orthodontic treatment. Orthodontics (Chic) 2011; 12: 108–121. [PubMed] [Google Scholar]
- 24.Jurela A, Sudarević K, Budimir A, et al. Clinical and salivary findings in patients with metal and crystalline conventional and self-ligating orthodontic brackets. Acta Stomatol Croat 2019; 53: 224–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alshatti H. Comparison of white spot lesions among clear aligners, self-ligating brackets and conventional brackets–a randomized controlled clinical trial. Master’s Theses, University of Connecticut ProQuest Dissertations & Theses, 2017; 1111.
- 26.Tiwari A, Jain R. Comparison of enamel demineralisation scores between passive self-ligation brackets and conventional ligation brackets in patients undergoing orthodontic treatment–a laser fluorescence study. Journal of Clinical & Diagnostic Research 2020; 14: ZC16-ZC19. [Google Scholar]
- 27.Skilbeck MG, Mei L, Mohammed H, et al. The effect of ligation methods on biofilm formation in patients undergoing multi-bracketed fixed orthodontic therapy—a systematic review. Orthod Craniofac Res 2022; 25: 14–30. DOI: 10.1111/ocr.12503. [DOI] [PubMed] [Google Scholar]
- 28.Do Nascimento LE, De Souza MM, Azevedo AR, et al. Are self-ligating brackets related to less formation of Streptococcus mutans colonies? A systematic review. Dental Press J Orthod 2014; 19: 60–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Parmar NP, Thompson GL, Atack NE, et al. Microbial colonisation associated with conventional and self-ligating brackets: a systematic review. J Orthod 2022; 49: 151–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cumpston M, Li T, Page MJ, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev 2019; 10: Ed000142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021; 372: n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan—a web and mobile app for systematic reviews. Syst Rev 2016; 5: 210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019; 366: l4898. [DOI] [PubMed] [Google Scholar]
- 34.Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016; 355: i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Polat Ö, Gökçelik A, Arman A, et al. A comparison of white spot lesion formation between a self-ligating bracket and a conventional preadjusted straight wire bracket. World J Orthod 2008; 9: e46–e50. [PubMed] [Google Scholar]
- 36.Pandis N, Papaioannou W, Kontou E, et al. Salivary Streptococcus mutans levels in patients with conventional and self-ligating brackets. Eur J Orthod 2010; 32: 94–99. [DOI] [PubMed] [Google Scholar]
- 37.Vashishta V, Kaul R, Singh A, et al. Evaluation of white spot lesions around orthodontic brackets using different bonding agents–an in vivo study. APOS Trends Apos 2022; 11: 309–316. [Google Scholar]
- 38.Khoroushi M, Kachuie M. Prevention and treatment of white spot lesions in orthodontic patients. Contemp Clin Dent 2017; 8: 11–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Macey R, Walsh T, Riley P, et al. Fluorescence devices for the detection of dental caries. Cochrane Database Syst Rev 2020; 12: Cd013811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Consoli Senno MV, Robles Ruíz JJ. Characteristics of white spot lesions associated with orthodontic treatment: A review. Rev Cient Odontol (Lima) 2023; 11: e168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Talic NF. Adverse effects of orthodontic treatment: a clinical perspective. Saudi Dent J 2011; 23: 55–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sá-Pinto AC, Rego TM, Marques LS, et al. Association between malocclusion and dental caries in adolescents: a systematic review and meta-analysis. Eur Arch Paediatr Dent 2018; 19: 73–82. [DOI] [PubMed] [Google Scholar]
- 43.Choi YY. Relationship between orthodontic treatment and dental caries: results from a national survey. Int Dent J 2020; 70: 38–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-imr-10.1177_03000605251328608 for White spot lesion in self-ligating versus conventional ligating bracket systems: A systematic review by Mohammad I Idris, Ahmad S Burhan, Mohammad Y Hajeer, Ahmad M Alhamwi and Fehmie R Nawaya in Journal of International Medical Research
Supplemental material, sj-pdf-2-imr-10.1177_03000605251328608 for White spot lesion in self-ligating versus conventional ligating bracket systems: A systematic review by Mohammad I Idris, Ahmad S Burhan, Mohammad Y Hajeer, Ahmad M Alhamwi and Fehmie R Nawaya in Journal of International Medical Research
Data Availability Statement
The datasets associated with this manuscript can be obtained from the corresponding author upon reasonable request.