Abstract
Background
Effective palliative care involves managing the many symptoms commonly experienced towards the end-of-life. Appropriate prescribing is key to this care, and ethnic inequalities may lead to unequal treatment and poorer outcomes for minority groups. Understanding these disparities is critical to ensuring equitable care. This rapid systematic review investigates ethnic inequalities in palliative care prescribing amongst adults residing in high-income countries.
Methods
The review was registered with the International Prospective Register of Systematic Reviews (PROSPERO) under registration number CRD42023476977. We conducted searches across three electronic databases (MEDLINE, Embase, and CINAHL) from January 2000 to November 2023. Screening, data extraction and quality assessment were conducted independently by two reviewers. Quality was assessed using various JBI Critical Appraisal tools. Due to the heterogeneity of included studies, a narrative review was undertaken without a meta-analysis.
Results
Out of 7880 studies identified, 10 studies met the inclusion criteria, all conducted in the United States. Overall, five studies were deemed to be high quality and five were fair quality. The studies highlighted ethnic disparities in palliative care prescribing. Minority populations were less likely to receive pain management medications, particularly opioids, compared to non-Hispanic whites. Increased age, female gender, lower socioeconomic status, and place of residence were also related to differences in prescribing practices.
Conclusions
This rapid systematic review suggests that there are ethnic inequalities in palliative care symptom management prescribing, highlighting a possible gap in care for ethnic minority patients. Research beyond the USA is needed to understand if there are international disparities in palliative care prescribing.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12904-025-01742-1.
Keywords: Palliative care, Ethnic inequalities, Prescribing, Symptom management, High-income countries, Rapid systematic review
Background
Palliative care prescribing involves the careful selection and administration of medications to manage symptoms and improve the quality of life for patients with life-limiting illnesses [1]. This approach balances the benefits of the medication with the burdens placed on the patient by taking it [1]. For the purposes of this review, we considered palliative care prescribing to be the prescription of symptom control drugs, and we excluded prescribing of disease modifying drugs, even if prescribed in a palliative care setting. Longstanding problems include dynamic symptoms, individual variability, unlicensed medication use and polypharmacy [2]. Advances in oncological and non-oncological disease management have resulted in patients living longer with increasingly complex symptoms and side effects. As the population ages, living with multimorbidity and organ dysfunction becomes increasingly common [3], both of which impact drug metabolism and efficacy. Tailoring prescriptions to individual needs requires careful assessment and personalised approaches. Furthermore, most people in the last year of life receive multiple medications for various conditions. Balancing symptom control while minimising adverse effects is challenging. Professionals must consider potential interactions and prioritize essential therapies; success relies upon effective utilisation of the expertise of a multi-disciplinary team [4].
Specialist pharmacists can play a critical role in optimizing medication management for individuals receiving palliative care [5]. They may conduct thorough reviews of patients’ medication profiles, assessing appropriateness, interactions, and potential adverse effects [6]. Regular reviews ensure the medication regimen aligns with the patient’s evolving needs. Collaborating with the multidisciplinary team, pharmacists have the expertise to tailor drug regimens for symptom relief. Effective symptom management enhances patients’ quality of life. In addition, pharmacists may educate patients, families, and other healthcare professionals about proper medication use. This includes deprescribing, dosing instructions, administration techniques, and managing side effects.
Ethnic differences in prescribing can arise due to inequalities in access, cultural beliefs, language barriers, and varying responses to medications [7]. To tackle these issues, it is essential to address care inequalities and ensure healthcare providers undergo cultural competence training. Understanding patients’ cultural backgrounds helps tailor treatment plans and ensures respectful communication [8]. Access to interpreters or bilingual healthcare professionals is vital. Clear communication about medications, side effects, and treatment options bridges language gaps. Involving patients and families in decision-making is essential. Healthcare professionals must understand their preferences, beliefs, and concerns [9]. Respect for cultural practices related to health and healing is crucial. Additionally, relying on evidence-based guidelines and pharmaceutical expertise is essential. It is important to recognise that certain ethnic groups may have unique pharmacogenetic variations. By integrating these strategies, healthcare professionals can provide equitable and effective care, regardless of patients’ ethnic backgrounds.
Previous research highlights the need to address ethnic inequality in palliative care experiences, with systematic synthesis of evidence lacking to date [10–12]. Addressing a critical gap in existing research, our rapid review aims to systematically synthesise evidence on ethnic disparities in palliative care prescribing amongst adults in high-income countries. This synthesis offers a foundation for informed decision-making and improved care. Our approach ensures a rigorous examination of the complexities and cumulative effects of social determinants, intersecting identities, and life-course influences on palliative care prescribing practices.
Research aim
This rapid systematic review aims to explore ethnic inequalities in palliative care prescribing amongst adults residing in high-income countries.
Conceptual framework underpinning research
This systematic review uses the Kunonga Framework (see Supplementary Table 1) developed specifically designed to address the complexities of health inequalities and inequities within the context of evidence synthesis [13]. The Kunonga Framework builds upon the established PROGRESS-Plus framework by integrating a focus on intersectionality and the life-course perspective. PROGRESS-Plus serves as an acronym for identifying and analysing the social determinants of health, standing for: Place of residence; Race/ethnicity/culture/language; Occupation; Gender/sex; Religion; Education; Socioeconomic status; and Social capital. The"Plus"element includes additional factors such as age, disability, and sexual orientation [14, 15].
The Kunonga Framework enhances the PROGRESS-Plus framework by reinforcing the critical distinction between health inequality and health inequity, emphasising that not all health differences are inherently inequitable. It advocates for the incorporation of intersectionality within evidence synthesis, which necessitates recognising how multiple social identities and factors such as race, ethnicity, gender, and socioeconomic status interact to create unique and compounded barriers to health [16, 17]. Furthermore, the Kunonga Framework encourages integrating the lifecourse perspective in evidence synthesis, examining how life events and transitions influence outcomes [18, 19]. This perspective will help researchers understand how socioeconomic status, cultural norms, and systemic factors shape ethnic inequalities in palliative care prescribing [19].
Methods
This rapid systematic review was conducted in accordance with Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines [20], with adaptations to expedite the process, including using a limited number of databases and restricting the search to English language studies, as described in rapid review guidelines [21]. Our protocol, initially registered in PROSPERO (CRD42023476977) as a systematic review, was adapted to a rapid review due to policy-driven time constraints, ensuring timely relevance for practice and policy. We also applied the novel Kunonga Framework [13], to explicitly address intersectional nuances of health inequalities and inequities, enhancing our methodological approach beyond the original protocol.
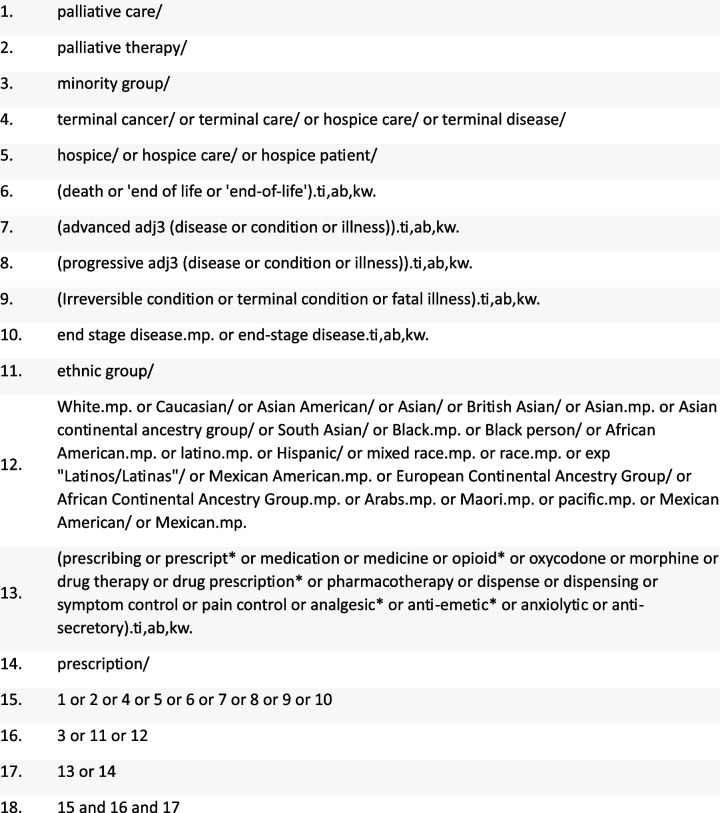
Search strategy
We developed search strategies for MEDLINE, Embase and CINAHL. The search was developed in MEDLINE and adapted for Embase and CINAHL. Medical Subject Headings (MeSH), keywords, and relevant terms, including synonyms for"palliative care,""prescribing,"and"ethnic minorities,"were incorporated into the search strategy. Searches were conducted between January 2000 and November 2023 and were limited to studies published in English. Complete search strategies are provided in Appendices 1 to 3.
Eligibility criteria
The full eligibility criteria for the review are presented in Table 1. Studies were included if they focused on adults receiving palliative care across various settings and examined ethnic inequalities in prescribing symptom relief medication. Palliative care is defined as a holistic approach to improving quality of life for patients with life-limiting illnesses by managing symptoms and addressing their physical, emotional, social, and spiritual needs [22]. Life-limiting illnesses are defined as progressive and incurable conditions that severely affect quality of life and eventually lead to death, such as advanced cancer and chronic obstructive pulmonary disease (COPD) [23]. We defined inequality as measurable differences in palliative care prescribing among ethnic groups that do not consider fairness. Examples include variations in the types and dosages of medications prescribed or the frequency of pain management interventions. Inclusion criteria, predetermined in the protocol, specified studies from Organisation for Economic Cooperation and Development (OECD) high-income countries [24], to ensure comparability and maintain similarity in palliative care standards. Only English language studies published from 2000 onwards were considered to ensure that findings were relevant to current practices and reflect the latest research advancements and trends. Studies were excluded if they involved non-adult populations, were conducted in OECD medium or low-income countries, lacked a specific focus on symptom control medications, dated before 2000, or did not compare prescribing patterns across ethnicities. Abstracts, conference proceedings, dissertations, books, and other forms of grey literature were also excluded to ensure the inclusion of high-quality, peer-reviewed evidence.
Table 1.
Eligibility criteria
| Criterion | Include | Exclude |
|---|---|---|
| Population |
Adults aged 18 + with a life-limiting illness [e.g., advanced cancer and chronic obstructive pulmonary disease (COPD)] with a focus on ethnic minorities Receiving palliative care from generalists or specialists’ providers Taking medicines for symptom control |
Studies carried out on people below the age of 18 People who are not receiving palliative care People who are not taking medicines to control end-of-life symptoms |
| Intervention | Palliative care prescribing of symptom control drugs e.g., pain, agitation, nausea/vomiting |
Non-prescribing practices or interventions Disease modifying drugs |
| Comparator | Comparison of prescribing practices across different ethnic groups, e.g., access to pain medication or symptom management | No comparison across different ethnic groups |
| Outcomes | Ethnic disparities in palliative care prescribing for symptom control | Outcomes not related to disparities in prescribing practices |
| Study design | Randomised control trials, cohort studies, cross-sectional (retrospective or prospective) | Case studies, qualitative studies, reviews, editorials |
| Setting | Studies conducted in Organisation for Economic Co-operation and Development (OECD) high-income countries | Studies conducted in non-OECD countries or low- and middle-income countries |
| Publication type |
Peer-reviewed journal articles Articles published from 2000 onwards |
Abstracts only, conference proceedings, dissertations, books, grey literature Articles published before 2000 |
| Language | Studies published in English | Studies published in languages other than English |
Study screening and selection
The identified studies underwent initial processing through EndNote 21 [25]. Duplicates within the dataset were identified and removed. The remaining studies were imported into Rayyan, a web-based software for systematic reviews, to facilitate screening [26]. To ensure systematic and consistent screening, criteria were developed based on the predetermined inclusion and exclusion guidelines. The criteria were piloted on 10% of the studies to refine their utility and efficacy prior to full-scale implementation. Titles and abstracts were assessed in Rayyan and categorised as ‘included’ or ‘excluded’ based on the criteria. Included studies were exported back to EndNote 21 for full-text examination. Both stages of selection were performed independently by two researchers, with any conflicts resolved through discussion.
Data extraction
A data extraction form was created using Microsoft Excel to capture relevant study characteristics, participant demographics, and pertinent information. Extracted data included author details, publication year, country, participant age, study setting, study design, sample size, ethnic groups, underlying condition, treated symptoms, medications prescribed, inter-ethnic differences, study conclusions and, where reported, other PROGRESS-Plus factors. The extraction form underwent pilot testing with 20% of included studies to refine its structure. The remaining studies were extracted by single researchers, with another checking for accuracy. Any conflicts were resolved through discussion or by a third researcher.
Critical appraisal
We used the JBI critical appraisal tools to systematically assess study quality and relevance [27]. JBI tools were applied to various study designs, including Analytical Cross-Sectional Studies [28], Cohort Studies [28], and Case Control Studies [29]. Critical appraisal was assessed independently by two researchers, with any conflicts resolved through discussion or by a third researcher. In this review, overall risk of bias was assessed based on the percentage of criteria fulfilled: 0–33% of criteria fulfilled indicated high risk of bias; 34–66% of criteria fulfilled indicated fair risk; and 67–100% of criteria fulfilled indicated low risk. No studies were excluded based on their overall risk.
Data synthesis
Due to heterogeneity in the populations, outcomes and analysis methods across studies, we employed a narrative synthesis using the principles of Synthesis Without Meta-analysis [30]. Each synthesis was grouped by PROGRESS-Plus domains and stratified by type of medication. In cases where the medication class was specified, we used the given classification. However, if the medication class was not explicitly stated, we described the medications based on their intended symptom management. A comprehensive list of medications used for each symptom is provided in Appendix 4. Where possible, adjusted analyses reported in the studies were prioritised in the synthesis over unadjusted analyses and frequency data (e.g. Chi2 tests) to account for the potential effects of confounding on effect estimates. We also further ordered the presentation of the data within tables by overall risk of bias assessment. We did not transform data to a standardised metric but used vote counting based on P values and 95% confidence intervals, where appropriate, to determine whether there was an association between ethnicity and prescribing practices. To assess whether there were associations between PROGRESS-Plus domains and palliative care prescribing, two reviewers (TPK and EEJ) independently interpreted each result and resolved conflicts through discussion. The narrative synthesis of medication use, and prescribing for ethnicity was the primary analysis, as it aligned most closely with the overall review question. We tabulated results and provided a brief narrative summary for each analysis. Due to variations in how ethnicity was reported across the original studies, this systematic review used the terminology and classifications from the primary sources. This ensured accuracy, transparency, and preserved the integrity of the original data without oversimplifying complex ethnic identities.
Results
Results of the search
The search identified 10,485 potentially relevant studies. Following deduplication in EndNote 21 and Rayyan, a total of 2605 duplicates were removed. Title and abstract screening was performed on 7880 studies, with 7708 excluded. A total of 172 studies underwent full-text screening, and 162 were excluded. Ten studies met the inclusion criteria and were included in the review [31–40]. The PRISMA flow chart (Fig. 1) summarises the study selection and screening process.
Fig. 1.
Flow diagram of study selection
Study characteristics
Table 2 presents an overview of individual study characteristics. Seven retrospective cohort studies [31, 33, 35, 37–40], two cross-sectional [34, 36], and one case control study [32], all conducted in the United Staes of America (USA), were included. The data sources ranged from large-scale databases such as Surveillance, Epidemiology, and End Results (SEER)-Medicare and Medicaid claims files to specific healthcare settings like cancer centres and nursing homes. Sample sizes ranged from 64 [32] to 318,549 [32] participants, with a focus on older adults, typically aged over 65. Four studies focused on people with specific conditions: pancreatic cancer [31]; lung cancer [39]; ovarian cancer [37]; and AIDS [38]. The remaining six studies included people with a range of health conditions. Figure 2 gives an overview of all conditions within the included studies.
Table 2.
Characteristics of included studies
| Study ID | Country | Age | Setting | Study Design | Sample size | Ethnic Groups | Condition | Symptoms |
|---|---|---|---|---|---|---|---|---|
| Allen et al., 2023 [31] | USA | 93% > 65 years | SEER-Medicare-linked database from 2005 to 2017 | Retrospective cohort study | 74,309 | White (53,893); Black/African American (8,185); Hispanic (7,131); Asian (4,889); American Indian/Alaska Native (211) | Pancreatic cancer | Pain, psychiatric symptoms, depression, anxiety, muscle spasms |
| Booker et al., 2020 [32] | USA | > 65 years | TRIP Cancer Pain Intervention from February 2007 to February 2010 | Case Control | 64 | African Americans (32); Caucasian Americans (32) |
Cancer Cancer diagnosis across all participants (n = 64) Gastrointestinal: 19; ENT: 17; Musculoskeletal: 6; Genitourinary: 5; Lymphatic: 4; Unspecified neoplasms: 2; Endocrine and brain: 1; Missing data: 10 |
Pain |
| Enzinger et al., 2023 [33] | USA | > 65 years | Centers for Medicare & Medicaid Services | Retrospective cohort study | 318,549 | White (272,358); Black (29,555); Hispanic (16,636) |
Cancer Cancer diagnoses across all participants (n = 318,549) Lung: 33.3%; Colorectal or anal: 8%; Pancreas: 6.8%; Esophagogastric: 5%; Liver, gallbladder, biliary: 5.2%; Prostate: 6.6%; Bladder: 2.6%; Kidney: 2.4%; Non-Hodkin lymphomas: 6%; Acute leukaemias: 4.3%; Breast: 5.8%; Ovarian: 2.6%; Uterine: 1.2%; Melanoma: 1.4%; other: 6% |
Pain |
| Haider et al., 2017 [34] | USA | Median (range): 59 (51–67) | MD Anderson Cancer Center’s outpatient palliative care clinic | Cross-sectional | 750 | White (529); Black (84); Hispanic (87); Other (50) |
Cancer Cancer types for total population (n = 750) Breast: 97; GI: 193; Genitourinary: 57; Gynaecologic: 49; Head and neck: 94; Haematologic: 22; Lung: 169; Others: 69 |
Pain |
| Munir et al., 2023 [35] | USA | 66 + | SEER-Medicare database from 2008 to 2016 | Retrospective cohort study | 48,631 | Black (5589), Asian (3089), Hispanic (5862), white (32,374) |
Advanced gastrointestinal cancer Liver: 6551; Pancreas: 13,559; Gastric: 5486; Colorectal: 23,035 |
Pain |
| Reynolds et al., 2008 [36] | USA | Median age (range): 81 (22–103) years | 12 nursing homes in central North Carolina from 2001 to 2004 | Cross-sectional | 1,133 | White 76.7%; ethnic minorities (not specified) |
Dementia: 43.2%; Stroke/Cerebrovascular accident: 28.4%; Congestive heart failure: 23.7%; Diabetes: 19.2%; Chronic obstructive pulmonary disease (COPD): 9.1%; Cancer: 4.8% |
Pain |
| Rolnick et al., 2007 [37] | USA | Mean (range): 67 (20–79) years | Three large health maintenance organisations | Retrospective cohort study | 421 |
White (348); African American (33); Asian (17); Hispanic (18); Native American (1); Unknown (4) |
Epithelial ovarian cancer | Pain |
| Sambamoorthi et al., 2000 [38] | USA | 18 + | New Jersey AIDS Registry, Medicaid claims files for drug and non-drug services, and the Medicaid eligibility file | Retrospective cohort study | 2,131 |
White (505); African American (1,228); Latino/Latina (389) |
AIDS | Pain |
| Saphire et al., 2020 [39] | USA | Mean (SD): 76.8 (6.6) | SEER-Medicare database, January 1, 2008 to December 31, 2014 | Retrospective cohort study | 16,246 |
White, non-Hispanic (13,077); Black, non-Hispanic (1,322); Hispanic (828); Asian, other (1,019) |
Lung cancer Non-small cell lung cancer: 12,898 (79.4%) |
Pain, dyspnoea, emotional distress, fatigue, respiratory secretions, nausea, vomiting, anorexia |
| Tabuyo-Martin et al., 2022 [40] | USA | Mean (range): 58 (21—90) years | Sylvester Comprehensive Cancer Center | Retrospective cohort study | 186 | White (90); African American (46); Latino/Latina (42); Asian (6); Unknown (1) |
Gynecoological cancer Cervix: 42 (22.6%); Ovary: 70 (37.6%); Uterus: 61 (32.8%); Vulva: 13 (7.0%) |
Pain, agitation, nausea/vomiting, lack of appetite, constipation |
Key: SEER The Surveillance, Epidemiology, and End Results, TRIP Translating Research into Practice, ENT Ear, Nose and Throat, COPD Chronic obstructive pulmonary disease; AIDS: Acquired immunodeficiency syndrome
Fig. 2.
Overview of conditions from included studies
Symptoms targeted were predominantly pain, but also included psychiatric symptoms, dyspnoea, emotional distress, fatigue, respiratory secretions, nausea, vomiting, anorexia, constipation, and agitation.
In terms of PROGRESS-Plus variables, seven studies included race/ethnicity/culture/language as a variable in their analyses, six included place of residence and gender/sex, and five included SES or personal characteristics. PROGRESS-Plus domains considered by the studies as part of their analyses are presented in Fig. 3. Six studies considered intersectionality by adjusting for multiple PROGRESS-Plus variables in their analyses [31–33, 35, 38, 39]. Only one study considered a lifecourse perspective in its analysis, accounting for the effects of persistent poverty on outcomes [35].
Fig. 3.
Number of studies including PROGRESS-Plus variables in analyses. Abbreviations: SES = socioeconomic status
Critical appraisal of included studies
Overall, five studies were deemed to be high quality [31, 33, 34, 38, 39], with the remaining five studies judged as fair quality [32, 35–37, 40]. For all studies judged as fair quality, there were some concerns surrounding whether the statistical analyses employed were appropriate and accounted for the effects of confounding. Among the retrospective cohort studies, issues were most frequently related to statistical analysis and the handling of confounding, with some studies also lacking clarity in outcome measurement and follow-up procedures (Table 3). For one cross-sectional study, there were concerns about the clarity of the eligibility criteria and method of exposure measurement (Table 4). For the case-control study, there were concerns about the measurement of the exposure and comparability of cases and controls (Table 5).
Table 3.
Critical appraisal of retrospective cohort studies
| Study ID | Question 1 | Question 2 | Question 3 | Question 4 | Question 5 | Question 6 | Question 7 | Question 8 | Question 9 | Question 10 | Question 11 | Overall Rating |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Allen et al., 2023 [31] | Yes | Yes | Yes | Yes | Yes | N/A | Yes | Yes | N/A | N/A | Yes | High |
| Enzinger et al., 2023 [33] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | N/A | N/A | Yes | High |
| Munir et al., 2023 [35] | Yes | Yes | Unclear | Yes | Yes | Yes | Yes | Unclear | N/A | N/A | Yes | Fair |
| Rolnick et al., 2007 [37] | Yes | Yes | Yes | No | Unclear | Unclear | Yes | Yes | N/A | N/A | Unclear | Fair |
| Sambamoorthi et al., 2000 [38] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | N/A | N/A | Yes | High |
| Saphire et al., 2020 [39] | Yes | Yes | Yes | Unclear | Yes | Yes | Yes | Yes | N/A | N/A | Yes | High |
| Tabuyo-Martin et al., 2022 [40] | Yes | Yes | Yes | No | No | Yes | Yes | Unclear | N/A | N/A | No | Fair |
Table 4.
Critical appraisal of cross-sectional studies
Table 5.
Critical appraisal of case control studies
| Study ID | Question 1 | Question 2 | Question 3 | Question 4 | Question 5 | Question 6 | Question 7 | Question 8 | Question 9 | Question 10 | Overall Rating |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Booker et al., 2020 [32] | No | Yes | Yes | Unclear | Unclear | No | No | Yes | Yes | No | Fair |
Synthesis of findings
Ethnicity
Nine studies reported on receipt of pain medications by ethnic group [31, 33–40]. One study reported on morphine equivalent daily dose (MEDD) across White, Hispanic, Black, and other ethnic groups, finding that Hispanic, Black, and Other racial groups were less likely to receive higher opioid doses compared to White patients [34]. Although a statistically significant P value was provided, it was not clear between which groups this statistically significant association was. For the remaining eight studies, most studies suggested that people from ethnic minority groups may be less likely to receive any pain medication towards end of life, though one study suggested that Hispanic people may be more likely to receive pain medications [31], and two studies suggested no evidence of an association between ethnicity and prescribing [36, 40], (see Table 6 and Supplementary Table 2).
Table 6.
Key: Green = more likely to receive; Red = less likely to receive; Yellow = no evidence of an association
Abbreviations: EOL end of life, MME morphine milligram equivalents, N/A not applicable (not a group reported within study), Ref referent group
Two studies suggested that people from ethnic minority backgrounds were less likely to receive medications for emotional distress medications [39, 40], but the same two studies reported inconsistent associations for receipt of medications for nausea and vomiting. One study reported that people from ethnic minority backgrounds were more likely to receive medication for treating fatigue at end of life compared with white individuals [39]. The same study suggested Black (non-Hispanic), Asian and other ethnic groups were less likely to receive medication for nausea at end of life compared with White individuals, though reported no evidence of an association antiemetics for Hispanic individuals compared with white individuals [39]. The same study suggested that Black non-Hispanic and Asian individuals may be more likely to receive medications for anorexia at end-of-life compared to White individuals, while reporting no evidence of a discrepancy between prescribing for White and Hispanic individuals [39]. One study reported that people from ethnic minorities may be less likely to be prescribed antidepressants, antipsychotics and anxiolytics than White individuals [31]. Finally, one study suggested that Black individuals may be more likely to use appetite stimulants compared to White individuals [40].
Influence of other PROGRESS-Plus factors
Across the studies, various PROGRESS-Plus factors, including gender/sex, place of residence, age, socioeconomic status, and social status, were examined for their influence on access to palliative care and symptom management both in combination with and independent from ethnicity.
Gender
Five studies analysed receipt and use of medication towards end of life by gender while adjusting for the potential confounding effects of ethnicity (see Supplementary Table 3) [33–35, 38, 39]. With regards to receiving pain medications, there were inconsistent results across the five studies. Two studies suggested that men were more likely to be prescribed or use pain medication [33, 34], while three suggested women were more likely to use pain medication [35, 38, 39].
Only one study assessed receipt of medications for anorexia, dyspnoea, emotional distress, fatigue and nausea one month before end of life [39]. The study suggested that females were less likely to receive medications for anorexia and fatigue compared with males but may be more likely to receive medications for dyspnoea, emotional distress and nausea [39].
Place of residence
Four studies analysed receipt and use of medication towards end of life by place of residence while adjusting for the potential confounding effects of ethnicity (see Supplementary Table 4) [33, 35, 38, 39]. Results from these four studies assessing the likelihood of receiving pain medications were inconsistent. One study suggested that there may be no evidence of an association between place of residence and prescribing of medications for dyspnoea and emotional distress, but indicated that people living in less urban areas may be more likely to receive medications for anorexia and nausea [39]. The same study suggested that urban residents were less likely to receive medications for fatigue compared with those living in a large metropolitan statistical area [39].
Personal characteristics: age
Two studies analysed receipt and use of medication towards end of life by age while adjusting for the potential confounding effects of ethnicity (see Supplementary Table 5) [35, 39]. Both studies suggested that receipt of pain medication became less likely with increasing age [35, 39]. One study suggested that there may be no evidence of an association between age and receipt of medications for anorexia, while those older than 66–69 may be more likely to receive medications for emotional distress and nausea. However, the same study presented inconsistent results across age groups in terms of receipt of medications for fatigue and dyspnoea [39].
Personal characteristics: age at diagnosis
One study assessed receipt and use of medication towards end of life by age at diagnosis while adjusting for the potential confounding effects of ethnicity [38], (see Supplementary Table 6), suggesting no evidence of an association between age at diagnosis and the use of pain medication in the last 3 months of life across all age groups [38].
Socioeconomic status
Four studies analysed receipt and use of medication towards end of life by SES while adjusting for the potential confounding effects of ethnicity [33, 35, 38, 39]. SES was assessed using heterogenous measures across the four studies, while two of the studies assessed SES using two different measures [33, 35]. Results of these studies by SES are presented in Supplementary Table 7.
Social capital
One study assessed receipt and use of medication towards end of life by a measure of social capital (marital status) while adjusting for the potential confounding effects of ethnicity [39], presenting inconsistent results (see Supplementary Table 8). The study suggested that unmarried individuals may be less likely to receive medications for anorexia, emotional distress, and nausea, compared to married individuals but there was no evidence of an association between marital status and receipt of medications for dyspnoea, fatigue, or pain [39].
Lifecourse perspective
Only one study incorporated the lifecourse perspective in analysing ethnic inequality in palliative care prescribing [35]. The study found that Black [adjusted odds ratio (aOR) = 0.84; 95% confidence interval (CI): 0.79–0.90], Asian (aOR = 0.86; 95% CI: 0.79–0.94), and Hispanic (aOR = 0.90; 95% CI: 0.84–0.95) patients with advanced gastrointestinal cancer had lower odds of filling an opioid prescription compared to White patients [35]. Additionally, these groups received lower daily doses, with Black patients receiving 16.5 percentage points less and Hispanic patients 19.1 percentage points less. Disparities were somewhat reduced for Asian and Hispanic patients in high-poverty areas but worsened for Black patients [35].
Discussion
Summary of main findings
This rapid systematic review identifies ethnic disparities in palliative care prescribing among adults in high-income countries, with these disparities being further exacerbated by intersecting factors such as gender, place of residence, age, socioeconomic status, and social capital. However, it is important to acknowledge that the robustness of these findings is limited by the relatively small number of studies included in this review. In addition, the generalisability of the results is constrained by the fact that all the studies were conducted in the US, potentially limiting the applicability of the findings to other contexts.
Our review indicates that certain ethnic groups, including Black, Asian, and Hispanic patients, may be less likely to receive pain, emotional distress, and nausea medications, particularly for opioid prescriptions [35, 39, 40]. Gender further compounds these disparities, as women from these ethnic groups often receive less pain management [38, 39]. Additionally, place of residence plays a crucial role, with minorities in less urbanised areas facing heightened barriers, while urban residents encounter distinct challenges [39]. Age also intensifies these disparities, particularly among older ethnic minority patients, who are less likely to receive appropriate palliative care [35, 39]. Socioeconomic status was found to interact with ethnicity to either mitigate or exacerbate these disparities, with some alleviation seen in high-poverty areas for Asian and Hispanic patients, although conditions worsen for Black patients [39]. Furthermore, social capital, such as marital status, appears to influence care receipt, with unmarried individuals generally receiving less comprehensive treatment [39]. The incorporation of a lifecourse perspective, though represented by a single study in this review, revealed how these disparities not only persist, but can worsen over time [35].
Comparison with other work
This rapid systematic review adds to growing reports exploring inequalities in in prescribing across the life course, as well as in the provision of palliative care. Previous research has reinforced the need to reduce inequalities in prescribing, especially for people from ethnic minority backgrounds. One systematic review found significant racial disparities in pain treatment [41]. Specifically, Black/African Americans had a lower likelihood of receiving opioid prescriptions for non-traumatic/non-surgical pain and Hispanics/Latinos also faced disparities for non-traumatic/nonsurgical pain, although not for traumatic/surgical pain [41]. However, another review reported mixed results on racial and ethnic disparities in pain management, with over half of the studies suggesting no significant differences in pain medication receipt [42]. These mixed findings are consistent with our review, which also observed variability in the extent of ethnic disparities, particularly in pain management and access to medications. However further research is needed to explore these patterns globally.
Strengths and limitations
This rapid systematic review adhered to PRISMA guidelines, ensuring a robust and transparent methodological approach [20]. The use of an intersectional lens and lifecourse perspective, as outlined in the Kunonga et al. framework, further strengthens the analysis by providing a nuanced understanding of how social determinants influence disparities in palliative care prescribing. However, this review is not without limitations. Our eligibility criteria, focusing exclusively on prescribing palliative care settings, may inadvertently omit ethnic minority populations who encounter barriers accessing these services. Future research should explicitly explore access barriers to specialist palliative care prescribing for ethnic minorities to further understand and address these disparities. Due to practical constraints typical of rapid reviews, the search strategy was restricted to three commonly used databases (MEDLINE, Embase, and CINAHL), possibly missing relevant studies. Excluding grey literature might have overlooked valuable insights into prescribing practices and disparities. Additionally, restricting inclusion to English-language studies may affect the comprehensiveness and generalisability of findings. Although screening, data extraction, and critical appraisal were done independently by two reviewers, a single reviewer screened most studies at the initial stage. This may have increased the risk of bias or missed studies, despite efforts to minimize this through the double-checking of 20% of the studies by a second reviewer. Regarding the synthesis, we did not transform data to a standardised metric to enable possible comparison between studies. As a result, we relied on narrative synthesis, which, while appropriate for the heterogeneity of the included studies, limits the ability to quantify the overall effect of ethnic inequalities in palliative care prescribing. Furthermore, a limitation of this review arises from the inconsistent reporting of prescription dosage information across studies, such as morphine equivalent daily dose (MEDD) or Defined Daily Doses (DDD). As a result, we were unable to comprehensively analyse prescribing patterns based on standardized dosage metrics in all included studies. This may also affect the generalisability of the findings, as differences in study methodologies and outcomes could obscure potential patterns or associations. Although our eligibility criteria aimed to examine prescribing for symptoms beyond pain, most included studies predominantly addressed pain medication, highlighting a need for further research into prescribing disparities for other prevalent palliative symptoms. It is important to recognise that COVID- 19 (2020–2023) likely influenced palliative care prescribing, with disruptions such as increased anticipatory prescribing, remote consultations, and altered roles for community nurses [43]. These changes may have intensified existing ethnic disparities. As our review did not separately analyse pre- and post-pandemic data, prescribing patterns from 2020 onwards should be interpreted cautiously. Future research should specifically explore pandemic-driven impacts on ethnic prescribing inequalities.
Implications for practice
Pharmacists play a pivotal role in optimizing medication management in both generalist and specialist providers of palliative care [44]. Efforts to integrate pharmacists into multidisciplinary care teams in hospices, care homes and other settings may help mitigate disparities in access to expert pharmacy services and prescribing, particularly for ethnic minority groups [45]. Pharmacists'expertise in medication optimization, can enhance palliative care for all patients [46]. Furthermore, pharmacogenetic research highlights ethnic variations in drug responses, necessitating individualised prescribing approaches under expert supervision [47]. However, underrepresentation of ethnic minorities in clinical trials limits our understanding of optimal medication use in palliative care [47]. Future research focusing on personalized medicine could improve symptom control and align care with patient preferences [48].
More generally, there is increasing acknowledgement of the need to improve equity in palliative care provision, particularly for people from ethnic minority communities. This review suggests that one way to tackle inequities is to target discrepancies in prescribing practices for people with life-limiting illnesses. However, a multi-faceted approach is required to address this broad ranging and complex issue. Cultural competence amongst health and social care professionals is key, so that understanding and respect for the different influences on care preferences and needs becomes the norm.
Implications for research
Incorporating an intersectionality lens [17, 49], and a lifecourse perspective [19], in future research is essential for advancing our understanding of ethnic disparities in palliative care prescribing. By examining how ethnicity intersects with other social determinants such as gender, age, socioeconomic status, and place of residence, researchers can better identify the compounded effects these factors have on prescribing in palliative care. The lifecourse perspective offers valuable insights into how these disparities develop and persist over time, highlighting the cumulative impact of social inequities on access to and quality of palliative care. However, the concentration of research in the US raises critical questions about what is happening in other countries. Additional research is required to explore potential disparities in palliative care prescribing within a broader, global context. Future studies should prioritise multinational collaborations that standardise methodologies, define ethnicity carefully, and account for healthcare system differences. Such efforts would facilitate meaningful cross-country comparisons and help identify both universal and context-specific factors influencing ethnic inequalities in healthcare. Using methodologies, such as multilevel modelling [50], that can effectively capture these complex interactions will be critical for developing targeted interventions aimed at reducing inequities and improving care for underrepresented and vulnerable populations [19].
Conclusion
While medicines are crucial for relieving symptoms in palliative care, our findings suggest potential disparities in prescribing practices, raising concerns about equitable access to palliative care across ethnicities. However, the concentration of research in the US raises critical questions about what is happening in other countries. Further research is needed to investigate potential disparities in palliative care prescribing in a broader, international context.
Supplementary Information
Acknowledgements
None.
Abbreviations
- aOR
Adjusted odds ratio
- JBI
Joanna Briggs Institute
- MEDD
Morphine milligram equivalent daily dose.
- PRISMA
Preferred Reporting Items for Systematic reviews and Meta-Analyses
- PROGRESS plus
Place of residence; Race/ethnicity/culture/language; Occupation; Gender/sex; Religion; Education; Socioeconomic status; and Social capital. The "Plus" element includes additional factors such as age, disability, and sexual orientation
- PROSPERO
International Prospective Register of Systematic Reviews
- SEER
Surveillance, Epidemiology, and End Results
- SES
Socio-economic status
Appendix 1: MEDLINE search strategy
Appendix 2: Embase search strategy
Appendix 3
Table 7.
CINAHL search strategy
| 1. | (MH"Palliative Care") OR"terminal care"or"end of life"or"end-of-life"or death or dying or hospice* OR (MH"Life Support Care") OR"advanced disease"or"advanced condition"or"advanced illness"OR"progressive disease"or"progressive condition"or"progressive illness"OR"irreversible condition"or"terminal condition"or"fatal illness"OR"end stage disease"or"end-stage disease") |
| 2. | ((MH"Minority Groups") OR"ethnic groups"or race or ethnicity OR white or Caucasian or"Asian American"or Asian or Black or"British Asian"or"South Asian"or"African American"or Latino or Latina or Mexican or African or Arabs or Maori or pacific) |
| 3. | ((MH"Pain Management") OR prescribing or prescription* or prescrib* or medication* OR opioid* or “pain management"or oxycodone or morphine or pharmacotherap* or dispens* or"symptom control"or"pain control"or analgesic* or anti-emetic* or anxiolytic or anti-secretory) |
| 4. | 1 AND 2 AND 3 |
Appendix 4
Table 8.
List of medications used for each symptom in the study by Saphire and colleagues [39]
| Condition | Medications |
|---|---|
| Pain | Opioids, Nonopioid Analgesics, Adjuvants |
| Emotional Distress | Antidepressants, Anxiolytics/Sedatives, Antipsychotics |
| Fatigue | Transfusions, Erythropoietin-Stimulating Agents (ESAs), Methylphenidate |
| Dyspnoea | Inhaled Bronchodilators, Inhaled Corticosteroids, Diuretics, Oral COPD/Asthma Medications, Secretion Management Medications |
| Anorexia | Appetite Stimulants |
| Nausea/Vomiting | Serotonin (5-Hydroxytryptamine 3) Antagonists, Neurokinin- 1 Antagonists, Prochlorperazine/Promethazine, Cannabinoids, Metoclopramide |
Author’s contributions
TPK, UD, FD and BH were involved with the original concept and planning the study. TPK, EEJ, UD and EW conducted the screening, data extraction and analysis of the included studies. TPK, EEJ, UD, EW prepared the initial manuscript. All authors read and approved the final manuscript.
Funding
This research is funded through the National Institute for Health and Care Research (NIHR) Policy Research Unit in Older People and Frailty (funding reference PR-PRU- 1217–2150). As of 01.01.24, the unit has been renamed to the NIHR Policy Research Unit in Healthy Ageing (funding reference NIHR206119). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Tafadzwa Patience Kunonga and Eugenie Evelynne Johnson are listed as joint first author.
References
- 1. Twycross R WA, Howard P.: Palliative Care Formulary (PCF8),, 8th Edition edn. Nottingham: Palliativedrugs.com Ltd,; 2022.
- 2.Hagemann V, Bausewein C, Remi C. Off-label use in adult palliative care–more common than expected. A retrospective chart review. Eur J Hospital Pharm. 2022;29(6):329–35. 10.1136/ejhpharm-2020-002554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Valabhji J, Barron E, Pratt A, Hafezparast N, Dunbar-Rees R, Turner EB, Roberts K, Mathews J, Deegan R, Cornelius V. Prevalence of multiple long-term conditions (multimorbidity) in England: a whole population study of over 60 million people. J Royal Soc Med. 2024;117(3):104–17. 10.1177/01410768231206033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.LoPresti MA, Dement F, Gold HT. End-of-life care for people with cancer from ethnic minority groups: a systematic review. American J Hospice Palliative Med. 2016;33(3):291–305. 10.1177/1049909114565658. [DOI] [PubMed] [Google Scholar]
- 5.Geiger J, Enck G, Luciani L, Fudin J, McPherson ML. Evolving roles of palliative care pharmacists. J Pain Symptom Manag. 2022;64(6):e357–61. 10.1016/j.jpainsymman.2022.07.012. [DOI] [PubMed] [Google Scholar]
- 6.Pharmacists ASoH-S: ASHP statement on the pharmacist's role in hospice and palliative care. American journal of health-system pharmacy: AJHP: official journal of the American Society of Health-System Pharmacists 2002, 59(18):1770-1773. 10.1093/ajhp/59.18.1770. [DOI] [PubMed]
- 7.Ellahham S. Communication in health care: impact of language and accent on health care safety, quality, and patient experience. American J Medical Quality. 2021;36(5):355–64. 10.1097/01.JMQ.0000735476.37189.90. [DOI] [PubMed] [Google Scholar]
- 8.Vermeir P, Vandijck D, Degroote S, Peleman R, Verhaeghe R, Mortier E, Hallaert G, Van Daele S, Buylaert W, Vogelaers D. Communication in healthcare: a narrative review of the literature and practical recommendations. International journal of clinical practice. 2015;69(11):1257–67. 10.1111/ijcp.12686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pan CX, Leo-To WF. Cross-cultural health care for older adults: Strategies for pharmacists. The Consultant Pharmacist®. 2014;29(10):645–53. 10.4140/TCP.n.2014.645. [DOI] [PubMed] [Google Scholar]
- 10.Loggers ET, Maciejewski PK, Paulk E, DeSanto-Madeya S, Nilsson M, Viswanath K, Wright AA, Balboni TA, Temel J, Stieglitz H. Racial differences in predictors of intensive end-of-life care in patients with advanced cancer. J Clin Oncol. 2009;27(33):5559. 10.1200/JCO.2009.22.4733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rabow MW, Dibble SL. Ethnic differences in pain among outpatients with terminal and end-stage chronic illness. Pain Medicine. 2005;6(3):235–41. 10.1111/j.1526-4637.2005.05037.x. [DOI] [PubMed] [Google Scholar]
- 12.Koffman J, Bajwah S, Davies JM, Hussain JA. Researching minoritised communities in palliative care: An agenda for change. Palliative Medicine. 2023;37(4):530–42. 10.1177/02692163221132091. [DOI] [PubMed] [Google Scholar]
- 13.Kunonga TP, Addis P, Johnson EE, Bower P, Hanratty B, Craig D: Development of the Kunonga Framework for Extending Approaches in Health Inequality and Inequity Evidence Syntheses. medRxiv 2024:2024.2011.2013.24317273. 10.1101/2024.11.13.24317273
- 14.Cochrane Methods Equity. PROGRESS-Plus. 2024. Available from: https://methods.cochrane.org/equity/projects/evidence-equity/progress-plus.
- 15.O’Neill J, Tabish H, Welch V, Petticrew M, Pottie K, Clarke M, Evans T, Pardo JP, Waters E, White H. Applying an equity lens to interventions: using PROGRESS ensures consideration of socially stratifying factors to illuminate inequities in health. Journal of clinical epidemiology. 2014;67(1):56–64. 10.1016/j.jclinepi.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 16.Calasanti T, Giles S. The Challenge of Intersectionality San Francisco: American Society on Aging; 2017. Available from: https://www.proquest.com/scholarly-journals/challenge-intersectionality/docview/2023382906/se-2.
- 17.Crenshaw K. On Intersectionality: Essential Writings: New Press; 2017.
- 18.Alwin DF. Integrating varieties of life course concepts. The Journals of Gerontology: Series B. 2012;67B(2):206–20. 10.1093/geronb/gbr146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jones NL, Gilman SE, Cheng TL, Drury SS, Hill CV, Geronimus AT. Life course approaches to the causes of health disparities. Am J Public Health. 2019;109(S1):S48–s55. 10.2105/ajph.2018.304738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE: The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Bmj. 2021, 372. 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed]
- 21.Garritty C, Gartlehner G, Nussbaumer-Streit B, King VJ, Hamel C, Kamel C, Affengruber L, Stevens A. Cochrane Rapid Reviews Methods Group offers evidence-informed guidance to conduct rapid reviews. Journal of Clinical Epidemiology. 2021;130:13–22. 10.1016/j.jclinepi.2020.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dewhurst F, Tomkow L, Poole M, McLellan E, Kunonga TP, Damisa E, Stowell M, Todd C, Hanratty B. Unrepresented, unheard and discriminated against: A qualitative exploration of relatives’ and professionals’ views of palliative care experiences of people of African and Caribbean descent during the COVID-19 pandemic. Palliative Medicine. 2023;37(9):1447–60. 10.1177/02692163231188156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pimsen A, Sumpuntharat S, Rodney T, Wirojratana V, Shu B-C. Navigating the Life-Limiting Illness Journey: A Mixed-Method Systematic Review of Advance Care Planning Experiences Among Healthcare Providers, Patients and Family. Journal of Clinical Nursing. 2025;34(2):382–407. 10.1111/jocn.17611. [DOI] [PubMed] [Google Scholar]
- 24.Organisation for Economic Co-operation and Development. List of OECD Member countries - Ratification of the Convention on the OECD: 2024. Available from: https://www.oecd.org/about/document/ratification-oecd-convention.htm.
- 25.The EndNote Team: EndNote. In., EndNote 21 edn. Philadelphia, PA: Clarivate; 2013.
- 26.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Systematic reviews. 2016;5:1–10. 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Barker TH, Stone JC, Sears K, Klugar M, Leonardi-Bee J, Tufanaru C, Aromataris E, Munn Z. Revising the JBI quantitative critical appraisal tools to improve their applicability: an overview of methods and the development process. JBI Evidence Synthesis. 2023;21(3):478–93. 10.11124/JBIES-22-00125. [DOI] [PubMed] [Google Scholar]
- 28.Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R, Currie M, Lisy K, Qureshi R, Mattis P, et al. Systematic reviews of etiology and risk. Joanna Briggs Institute reviewer’s manual 2024. 10.46658/JBIMES-24-06
- 29.Barker TH, Stone JC, Sears K, Klugar M, Tufanaru C, Leonardi-Bee J, Aromataris E, Munn Z. The revised JBI critical appraisal tool for the assessment of risk of bias for randomized controlled trials. JBI Evidence Synthesis. 2023;21(3):494–506. 10.11124/JBIES-22-00430. [DOI] [PubMed] [Google Scholar]
- 30.Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S, Hartmann-Boyce J, Ryan R, Shepperd S, Thomas J, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ. 2020;368: l6890. 10.1136/bmj.l6890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Allen JM, Awunti M, Guo Y, Bian J, Rogers SC, Scarton L, DeRemer DL, Wilkie DJ. Unraveling racial disparities in supportive care medication use among end-of-life pancreatic cancer patients: Focus on pain management and psychiatric therapies. Cancer Epidemiology, Biomarkers and Prevention. 2023;32(12):1675–82. 10.1158/1055-9965.EPI-23-0251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Booker SQ, Herr KA, Garvan CW. Racial differences in pain management for patients receiving hospice care. Oncol Nurs Forum. 2020;2020:228–40. [DOI] [PubMed] [Google Scholar]
- 33.Enzinger AC, Ghosh K, Keating NL, Cutler DM, Clark CR, Florez N, Landrum MB, Wright AA. Racial and ethnic disparities in opioid access and urine drug screening among older patients with poor-prognosis cancer near the end of life. Journal of Clinical Oncology. 2023;41(14):2511–22. 10.1200/JCO.22.01413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Haider A, Zhukovsky DS, Meng YC, Baidoo J, Tanco KC, Stewart HA, Edwards T, Joy MP, Kuriakose L, Lu Z. Opioid prescription trends among patients with cancer referred to outpatient palliative care over a 6-year period. Journal of oncology practice. 2017;13(12):e972–81. 10.1200/JOP.2017.024901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Munir MM, Woldesenbet S, Endo Y, Ejaz A, Cloyd JM, Obeng-Gyasi S, Dillhoff M, Waterman B, Gustin J, Pawlik TM. Association of race/ethnicity, persistent poverty, and opioid access among patients with gastrointestinal cancer near the end of life. Annals of Surgical Oncology. 2023;30(13):8548–58. 10.1245/s10434-023-14218-4. [DOI] [PubMed] [Google Scholar]
- 36.Reynolds KS, Hanson LC, Henderson M, Steinhauser KE. End-of-life care in nursing home settings: do race or age matter? Palliative and Supportive Care. 2008;6(1):21–7. 10.1017/S1478951508000047. [DOI] [PubMed] [Google Scholar]
- 37.Rolnick SJ, Jackson J, Nelson WW, Butani A, Herrinton LJ, Hornbrook M, Neslund-Dudas C, Bachman DJ, Coughlin SS. Pain management in the last six months of life among women who died of ovarian cancer. Journal of pain and symptom management. 2007;33(1):24–31. 10.1016/j.jpainsymman.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 38.Sambamoorthi U, Walkup J, McSpiritt E, Warner L, Castle N, Crystal S. Racial differences in end-of-life care for patients with AIDS. AIDS Public Policy J. 2000;15(3–4):136–48. [PubMed] [Google Scholar]
- 39.Saphire ML, Prsic EH, Canavan ME, Wang S-YJ, Presley CJ, Davidoff AJ. Patterns of symptom management medication receipt at end-of-life among medicare beneficiaries with lung cancer. Journal of pain and symptom management. 2020;59(4):767–77. e761. 10.1016/j.jpainsymman.2019.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tabuyo-Martin A, Torres-Morales A, Pitteloud MJ, Kshetry A, Oltmann C, Pearson JM, Khawand M, Schlumbrecht MP, Sanchez JC. Palliative Medicine Referral and End-of-Life Interventions Among Racial and Ethnic Minority Patients With Advanced or Recurrent Gynecologic Cancer. Cancer Control: Journal of the Moffitt Cancer Center. 2023;30:1–9. 10.1177/10732748231157191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Meghani SH, Byun E, Gallagher RM. Time to Take Stock: A Meta-Analysis and Systematic Review of Analgesic Treatment Disparities for Pain in the United States. Pain Medicine. 2012;13(2):150–74. 10.1111/j.1526-4637.2011.01310.x. [DOI] [PubMed] [Google Scholar]
- 42.Clarke G, Chapman E, Crooks J, Koffman J, Ahmed S, Bennett MI. Does ethnicity affect pain management for people with advanced disease? A mixed methods cross-national systematic review of ‘very high’Human Development Index English-speaking countries. BMC Palliative Care. 2022;21(1):46. 10.1186/s12904-022-00923-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mitchell S, Oliver, P., Gardiner, C., Chapman, H., Khan, D., Boyd, K., Dale, J., Barclay, S., & R Mayland, C.: Community end-of-life care during the COVID-19 pandemic: findings of a UK primary care survey. BJGP Open, 2021, 5(4). 10.3399/BJGPO.2021.0095. [DOI] [PMC free article] [PubMed]
- 44.Zerzan J, Stearns S, Hanson L. Access to palliative care and hospice in nursing homes. Jama. 2000;284(19):2489–94. 10.1001/jama.284.19.2489. [DOI] [PubMed] [Google Scholar]
- 45.Tobin J, Rogers A, Winterburn I, Tullie S, Kalyanasundaram A, Kuhn I, Barclay S. Hospice care access inequalities: a systematic review and narrative synthesis. BMJ supportive and palliative care. 2022;12(2):142–51. 10.1136/bmjspcare-2020-002719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pawłowska I, Pawłowski L, Lichodziejewska-Niemierko M. The role of a pharmacist in a hospice: a nationwide survey among hospice directors, pharmacists and physicians. European Journal of Hospital Pharmacy. 2016;23(2):106–12. 10.1136/ejhpharm-2015-000730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Burroughs VJ, Maxey RW, Levy RA. Racial and ethnic differences in response to medicines: towards individualized pharmaceutical treatment. J Natl Med Assoc. 2002;94(10 Suppl):1–26. [PMC free article] [PubMed] [Google Scholar]
- 48.Barbee Jr J, Kelley S, Andrews J, Harman A. Palliative Care: The Role of the Pharmacist. 2016. Available from: https://www.pharmacytimes.com/view/palliative-care-the-pharmacists-role.
- 49.Kapilashrami A, Hankivsky O. Intersectionality and why it matters to global health. The Lancet. 2018;391(10140):2589–91. 10.1016/S0140-6736(18)31431-4. [DOI] [PubMed] [Google Scholar]
- 50.Evans CR, Leckie G, Subramanian SV, Bell A, Merlo J. A tutorial for conducting intersectional multilevel analysis of individual heterogeneity and discriminatory accuracy (MAIHDA). SSM Popul Health. 2024;26: 101664. 10.1016/j.ssmph.2024.101664. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.