Abstract
Solid cancer contains a complicated communication network between cancer cells and components in the tumor microenvironment (TME), significantly influencing the progression of cancer. Exosomes function as key carriers of signaling molecules in these communications, including the intricate signalings of tumor-associated macrophages (TAMs) on cancer cells and the TME. With their natural lipid bilayer structures and biological activity that relates to their original cell, exosomes have emerged as efficient carriers in studies on cancer therapy. Intrigued by the heterogeneity and plasticity of both macrophages and exosomes, we regard macrophage-derived exosomes in cancer as a double-edged sword. For instance, TAM-derived exosomes, educated by the TME, can promote resistance to cancer therapies, while macrophage-derived exosomes generated in vitro have shown favorable potential in cancer therapy. Here, we depict the reasons for the heterogeneity of TAM-derived exosomes, as well as the manifold roles of TAM-derived exosomes in cancer progression, metastasis, and resistance to cancer therapy. In particular, we emphasize the recent advancements of modified macrophage-derived exosomes in diverse cancer therapies, arguing that these modified exosomes are endowed with unique advantages by their macrophage origin. We outline the challenges in translating these scientific discoveries into clinical cancer therapy, aiming to provide patients with safe and effective treatments.
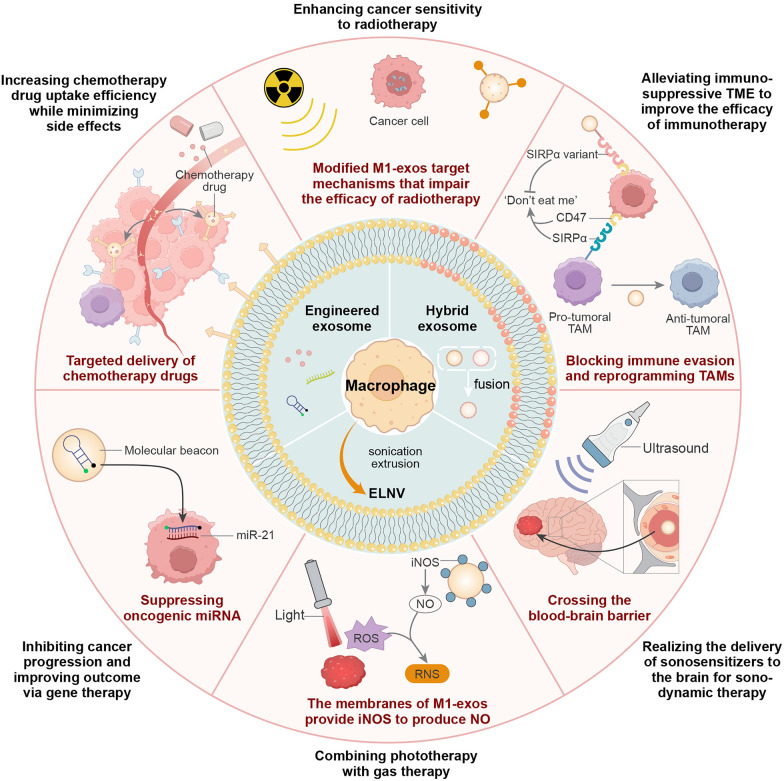
Graphical Abstract
Keywords: Exosomes, Tumor-associated macrophages, Macrophage-derived exosomes, Modified exosomes, Cancer therapy
Introduction
Exosomes, with a general size range of 40 to 150 nm (average 100 nm) in diameter, are a subset of extracellular vesicles (EVs) [1]. All types of cells are capable of secreting exosomes as one of the critical operators in intercellular communications. Exosomes contain diverse bioactive constituents, including proteins, RNA, and DNA, which are packaged within their lipid bilayers [2]. These constituents are released by the cells of origin and taken up by recipient cells [3]. Through these constituents, exosomes mediate plenty of physiologic and pathologic processes, resulting in the maintenance of cellular, tissue, and whole-body homeostasis as well as the generation or promotion of various diseases [2]. Given these structural and functional characteristics, exosomes can serve as a targeted delivery platform for drugs and therapeutic molecules [4].
In cancer, macrophages are one of the main sources of the exosomes in the tumor microenvironment (TME) and pivotal innate immune cells characterized by heterogeneity and plasticity. The classical M1/M2 polarization model has been used to illustrate the heterogeneity of tumor-associated macrophages (TAMs) [5, 6]. In this model, M1 TAMs contribute to the phagocytosis of cancer cells and activation of the immune system, while M2 TAMs boost tumor growth and metastasis, angiogenesis, and immunosuppression [7, 8]. Although the heterogeneity of TAMs is undoubted, a higher TAM proportion is generally related to a worse prognosis, indicating pro-cancer TAMs may be the major types of TAMs [8, 9]. Accordingly, TAMs and TAM-derived exosomes have been found to exert multifaceted pro-cancer functions, including maintaining the malignant phenotypes in cancer cells, inducing immune suppression, and reshaping the extracellular matrix (ECM) [7, 10].
However, the heterogeneity of macrophages makes the anti-cancer role of macrophage-derived exosomes possible. In the absence of cancer context education, macrophage-derived exosomes generated in vitro, especially M1-macrophage-derived exosomes (M1-exos), exhibit significant anti-cancer phenotypes when applied to multiple mouse models of cancer. For instance, M1-exos stimulate anti-cancer inflammation, relieve immune suppression, and reprogram pro-cancer TAMs to anti-cancer TAMs [11–13]. Therefore, macrophage-derived exosomes, these natural bioactive vesicles, are receiving increasing attention owing to their biocompatibility and multiple anti-cancer functions. After modification, macrophage-derived exosomes can act as unique drug delivery systems for various cancer therapies and overcome existing challenges in these therapies, such as lack of targeting, treatment resistance, and limited effect [14–16]. Considering the double-edged role of macrophage-derived exosomes, a comprehensive review of these exosomes in cancer is urgently needed, as it could facilitate the advancement and clinical translation of targeting and harnessing macrophage-derived exosomes in cancer therapies.
In this review, we focus on the roles of macrophage-derived exosomes in cancer, especially the potential in cancer therapy. First, we give an overview of the processes of exosome biogenesis. We also explore the reasons for the heterogeneity of TAM-derived exosomes, exposing the regulators of TAM-derived exosomes in multilayers. Then, we address the crucial roles of TAM-derived exosomes in cancer progression, metastasis, and resistance to cancer therapy. In particular, modified M1 macrophage-derived exosomes in cancer therapy are highlighted, with emphasis on their therapeutic potential and challenges in clinical translation.
The biogenesis of exosomes
Classic exosomes originate from the endocytic pathway and revolve around multivesicular bodies (MVBs) (Fig. 1).
Fig. 1.
Overview of exosome biogenesis. a. Exosome biogenesis starts with the formation of endocytic vesicles, the process whereby the plasma membrane locally invaginates, and is regulated by proteins such as clathrin and caveolin. Endocytic vesicles fuse to form the early endosome, which matures towards MVBs, also known as late endosomes. This progression involves the inward budding of early endosomes, leading to the formation of MVBs that contain ILVs. b. During MVBs maturation, cargoes including proteins, RNA, and DNA are sorted into ILVs. These interactions enrich MVBs with components from multiple intracellular organelles and substances, which is fundamental for the functional heterogeneity of exosomes. c. The fate of MVBs has two potential outcomes: 1. MVBs may be transported to the plus end of microtubules (left) by motor proteins. Following the transport, MVBs bind to the cell membrane and release ILVs as exosomes under the regulation of the SNARE complex. 2. Alternatively, they can be transported towards the minus end of microtubules (right) by motor proteins, bind to lysosomes, and degrade subsequently. MVBs multivesicular bodies, ILV intraluminal vesicles, ER endoplasmic reticulum, TGN trans Golgi network, HOPS homotypic fusion and protein-sorting, Arl8b Rab7-to-Arf-like GTPase 8, SKIP SifA- and kinesin-interacting protein, RILP Rab7-interacting lysosomal protein, BORC BLOC one-related complex, SNARE soluble N-ethylmaleimide-sensitive fusion attachment protein receptor, RBP RNA-binding protein
Within MVBs, intraluminal vesicles (ILVs), widely recognized as precursors for classic exosomes, are generated and transported [1, 2]. Throughout exosome biogenesis, MVBs undergo formation, cargo sorting, fusion with the plasma membrane, and ultimately release ILVs as exosomes [1]. Functioning as carriers for ILVs, MVBs play a crucial role in the whole process of exosome generation and participate in determining the fate of exosomes. In different circumstances, exosomes are formed through a more direct pathway. For example, exosomes can be directly generated from the plasma membranes of erythroleukemia cell lines and T cells [17]. Moreover, activated neutrophils can even release exosomes derived from the nuclear envelope [18]. In this section, we will focus on the biogenesis of the classic exosomes.
MVB formation
The formation of MVBs primarily involves the generation of early endosomes and ILVs. Typically, early endosomes are formed by the fusion of endocytic vesicles derived from the endocytic pathway [19]. These pathways are mediated by several proteins, such as clathrin and caveolin, which respectively form clathrin and caveolin-coated endocytic vesicles with actin cytoskeleton [20, 21]. Furthermore, the uptake of exosomes is also related to clathrin- and caveolin-mediated endocytic pathways [22].
ILVs are generated through the inward budding of the early endosome membrane, leading to the transformation of early endosomes into MVBs that contain multiple ILVs [2]. Mechanisms regulating ILV formation involve both the endosomal sorting complex required for transport (ESCRT)-dependent pathway and the ESCRT-independent pathway. The ESCRT comprises ESCRT-0, -I, -II, and -III subcomplexes, and the ATPase vacuolar protein sorting 4 (VPS4). In the classic ESCRT-dependent pathway, each subcomplex recruits the subsequent one. ESCRT-0 captures ubiquitylated cargo proteins with ubiquitin-binding sites. ATPase VPS4 works together with ESCRT-III to drive constriction and scission of the membrane [23]. Notably, cargo proteins can also be sorted into exosomes via a ubiquitin-independent pathway [24]. Additionally, certain components are capable of recruiting ESCRT-III and ATPase VPS4. These components such as apoptosis-linked gene 2-interacting protein X (ALIX) and his domain protein tyrosine phosphatase (HD-PTP) are the central part of their respective noncanonical ESCRT-dependent pathways. For instance, Syntenin, the adaptor protein of Syndecan, binds to ALIX with LYPX(n)L motifs. After that, ALIX recruits ESCRT-III and ATPase VPS4 to generate ILVs [25]. As for the ESCRT-independent pathway, lipid rafts with high contents of cholesterol, sphingolipids, phosphatidylserine, flotillin, and ceramide are usually involved [26]. For example, active Rab31 drives the formation of ILVs containing epidermal growth factor receptor (EGFR) via the flotillins in lipid rafts, facilitated by cholesterol and ceramide, rather than relying on ESCRT components [27].
Cargo sorting and MVB maturation
During the generation of ILVs, cargoes including proteins, amino acids, lipids, RNA, DNA, and metabolites are sorted into MVBs, some membrane proteins and molecules are also included [2]. The cargoes secreted by exosomes serve as carriers of the information and function in intercellular communication, among which the non-coding RNAs (ncRNAs), including microRNA (miRNA), long non-coding RNA (lncRNA), and circular RNA (circRNA), are most well-studied in various physiologic processes and diseases [17, 28–30]. RNA-binding proteins (RBPs) are involved in many mechanisms of RNA sorting. For instance, Y-box binding protein 1 (YBX1) binds miR-223 with ‘cold shock’ domain and drives miR-223 into exosomes. Notably, miR-223 is enriched in mitochondria and another RBP called YBAP1 mediates the miR-233 transport from mitochondria to exosomes [31]. Heterogeneous nuclear ribonucleoproteins (hnRNPs), a class of RBPs implicated in various stages of cancer progression, are also associated with exosome biogenesis. In colorectal cancer (CRC), a hnRNP called hnRNP-Associated with Lethal Yellow (RALY), an important member of hnRNPs, promotes exosome secretion by enhancing the MVB formation. Increased exosome levels driven by RALY induce M2 macrophage activation, thereby facilitating CRC metastasis, highlighting RALY as a promising target for inhibiting CRC metastasis [32]. The protein sorting is mediated by many components of the ESCRT-dependent and ESCRT-independent pathways, such as ESCRT-III, RAB coupling protein, ALIX, syntenin-1, and ceramides [19]. The ALIX just mentioned stimulates the sorting of the tetraspanins CD9, CD81, and CD63 to MVBs with the presence of lysobisphosphatidic acid (LBPA). Additionally, ALIX, CD9, CD81, and CD63 are widely accepted biomarkers for exosomes [33]. Tetraspanins are also implicated in loading cargoes to MVBs. In ovarian cancer cells, micronuclei collapse introduces nuclear contents including genomic DNA and histone H2B to MVBs, which is proved to be mediated by CD63 [34].
Apart from mitochondrion and micronucleus, MVBs also interact with other organelles and substances. The G protein-coupled receptor class C group 5 member B (GPRC5B) can be trafficked to exosome after the L-type lectin LMAN2-limited and adaptor protein GGA1-dependent transport of endoplasmic reticulum (ER) to the trans Golgi network (TGN) [35]. Inflammasome proteins can also be found in exosomes of stroke patients and traumatic brain injury patients [36, 37]. Through the processes above, MVBs gradually enrich in content and finally mature. More interestingly, in the same type of cells. The exosomes from different organelles of origin can exert different effects, potentially due to variations in membrane protein composition. For example, ER-derived exosomes exhibit better pro-inflammatory and anti-cancer functions than plasma-derived exosomes (Fig. 1) [38]. It provides a new factor to consider when designing exosomes for cancer therapy. The different types and levels of cargoes, along with extensive intracellular interactions, jointly build the foundation for the heterogeneity of exosomes.
MVB transport and ILV release
After maturation, MVBs have the potential to transport to and fuse with either lysosomes for degradation or the plasma membrane for the release of ILVs as exosomes [2]. There are many regulators of MVB transport, among which Rab7 serves as a conserved and crucial component. Rab7 is a member of the Rab small GTPases family, which recruits effector proteins and mediates the fate of vesicles by switching between an inactive GDP-bound (Rab-GDP) and an active GTP-bound (Rab-GTP) state [39].
The transport of MVBs to the plasma membrane involves a Rab7-to-Arf-like GTPase 8 (Arl8b) switch. Arl8b recruits SifA- and kinesin-interacting protein (SKIP), which subsequently recruits the kinesin-1 motor to transport MVBs to the cell periphery (the plus end of microtubules) [40]. Kinesin-3, directly recruited by Arl8, also exerts the same action [41]. Both Arl8b and SKIP are involved in the recruitment of the homotypic fusion and protein-sorting (HOPS) to MVBs. The Arl8b/SKIP/HOPS complex recruits TBC1D15 to inactive and removes Rab7 from MVBs [40]. Active Rab7 interacts with its effector proteins Rab7-interacting lysosomal protein (RILP) and oxysterol-binding protein-related protein 1L (ORP1L) to recruit dynein-dynactin motor complexes, which transport MVBs to the juxtanuclear organizing center (the minus end of microtubules) and lysosomes [42]. Notably, HOPS and Arl8 mediate the transport of MVBs to lysosomes as well. It has been reported that HOPS drives the fusion of MVBs and lysosomes via connecting the Rab2a of MVBs and the BLOC one-related complex (BORC)-anchored Arl8 of lysosomes [41, 43]. The suppression of this fusion can inhibit the degradation of MVBs and promote exosome secretion, which could be used to improve the yield of exosomes in clinical translation [43].
Rab GTPase also coordinates the docking and the fusion with membranes of MVBs. Slp4 (synaptotagmin-like 4 = SYTL4), is one of the effectors of Rab27a for docking MVBs to membranes and interacting with soluble N-ethylmaleimide-sensitive fusion attachment protein receptor (SNARE) complex on the plasma membrane [44]. In hepatocellular carcinoma cells, the highly expressed lncRNA HOX Transcript Antisense RNA (HOTAIR) promotes the docking of MVBs to the plasma membrane by regulating Rab35 and induces SNARE complex formation [45]. SNARE complex is thought to be the main contributor to the fusion of MVB and plasma membrane, known as the last step of exosome release. SNARE protein family comprises the Qa-SNARE, Qb-SNARE, Qc-SNARE, and R-SNARE, distributed on the vesicle membrane (v-SNARE) and the target membrane SNARE (t-SNARE) [46, 47]. The v-SNARE from MVB membranes and the t-SNARE from plasma membranes assemble to form parallel four-helix bundles that drive two membranes into close proximity [48]. SNARE complex in different cells can be assembled by the same or different SNARE family members. In breast cancer cells, HeLa cervical cancer cells, and melanoma cells, syntaxin-4, SNAP-23, and VAMP-7 are responsible for exosome secretion [49]. As for prostate cancer epithelial cells, SNAP29 contributes to exosome release [50].
In the course of exosome biogenesis, ILVs, which are hosted in MVBs, capture diverse cargoes and are released as an intercellular communication tool. This is a complicated multi-step process involving plenty of molecules and mechanisms. The basic outline and classic molecules of the process are mostly illustrated above, but more precise and comprehensive details are still under-explored.
TAM-derived exosomes heterogeneity
Exosome heterogeneity
Exosomes are heterogeneous extracellular vesicles that vary substantially in size, content, and function [2]. The heterogeneity of exosomes arises out of influencing factors from different biological scales, ranging from systemic intrinsic and extrinsic determinants to cellular factors (Fig. 2).
Fig. 2.
Multilevel factors that influence exosome heterogeneity. a. Influences on exosomes can be categorized as systemic intrinsic-/extrinsic-, cellular-, and cellular molecular factors, which shape the heterogeneity of exosomes in their sizes, contents, yield, and ultimately, functions. Notably, influences from distinct biological layers are not isolated, as intrinsic factors are involved in regulating how exosomes respond to extrinsic factors. For example, exosomes derived from Hp-infected mice exhibit gender differences. Exosomes derived from male mice show higher levels of ROS compared to those from female mice. These higher levels of ROS are associated with the development of AS. b. TAMs are one of the key sources of exosomes in the TME. Cancer type determines the features of the TME context, as well as the heterogeneity of TAM-derived exosomes. Specifically, the same kind of microRNA, as an example, miR-223, functions differently in distinct cancer types. MiR-221-3p serves as another example illustrating the significance of cancer context, as it induces similar malignant phenotypes in different cancer types via distinct pathways. Hp Helicobacter pylori, ROS reactive oxygen species, AS atherosclerosis, TAM tumor-associated macrophages, TME tumor microenvironment, GBM Glioblastoma, PDCD4 programmed cell death factor 4, STAT3 signal transducer and activator of transcription 3, GC gastric cancer, PTEN phosphatase and tensin homolog deleted on chromosome ten, PI3K phosphoinositide 3-kinase, FBXW7 F-box and WD repeat domain containing 7, BC breast cancer, Mef2c myocyte enhancer factor 2C, OS osteosarcoma, SOCS3 suppressor of cytokine signaling 3, JAK2 Janus Kinase 2, EOC epithelial ovarian cancer, CDKN1B cyclin-dependent kinase inhibitor 1B
Systemic determinants can be broadly classified as either intrinsic or extrinsic. The systemic intrinsic determinants, such as species, sex, and genetics shape the basal characteristics of exosomes [51–53]. For instance, the yield, size distribution, and antioxidant capacity of plant-derived exosomes vary across different species, providing distinct medicinal value [51]. Moreover, these system intrinsic determinants partly dictate how exosomes react to system extrinsic signals as sensitive responders. A study on Helicobacter pylori (Hp)-infected mice clearly illustrates this phenomenon, showing that exosomes from male, but not female mice, induce a selective increase in reactive oxygen species (ROS) production and endothelial dysfunction. This selective effect is associated with atherosclerosis (AS) development and progression [54]. In addition, other systemic extrinsic factors such as senescence, exercise, and diseases, also contribute to the changes in quantities and contents of exosomes [55–57]. For example, older individuals secrete significantly fewer exosomes and muscle health-associated miRNAs, compared to young individuals, and the disparity in expression levels of these miRNAs can be decreased after resistance exercise training [55]. The upregulated exosomal miR-4732-5p in epithelial ovarian cancer (EOC) patients could be exploited for distinguishing EOC patients from healthy individuals [56]. Similarly, the serum-derived exosomal programmed death-ligand 1 (PD-L1) levels in patients with initially diagnosed osteosarcoma are positively associated with cancer metastasis and death [57]. These differentially expressed cancer-associated biomarkers substantiate exosomes as a promising target in cancer liquid biopsy for early diagnosis, monitoring of cancer progression, and prognosis prediction [58].
The cell of origin and its state are important determinants of exosome heterogeneity. To some extent, exosomes can be viewed as a functional carrier of their original cell. Studies of exosomal programmed cell death protein 1 (PD-1)/PD-L1 indicate that exosomes may serve as respective arms for the war between cancer cells and immune cells. Hepatocellular carcinoma (HCC) cells have the potential to release exosomes with upregulated PD-L1, which is transported to TAMs via exosomes and suppressed CD8+ cells [59]. In contrast, activated T cells generate exosomal PD-1 that binds to PD-L1 on the cell surface and exosomal PD-L1, thereby competitively inhibiting the immunosuppressive effects of PD-L1 [60]. Furthermore, exosome origin is found to be associated with its targeting cell. A study involving several different cancer models demonstrates that TDEs tend to be uptaken by organ-specific cells to prepare the pre-metastatic niche, inducing organ-specific metastasis via corresponding integrins [61]. These examples above underline that the cell of origin plays a dominant role in exosome heterogeneity. However, a certain cell type can exist in different states due to external and internal regulators, resulting in heterogeneity of exosomes. TAM can serve as a presentative example for this and will be discussed further in the next two subsections.
All levels of determinants mentioned above affect the biogenesis of exosomes. Although the biogenesis of exosomes in most types of cells is roughly similar as previously described, the specific regulatory molecules and their functions may vary with the cell types and states, inducing the heterogeneity of exosomes in quantities, structures, and functions. Some regulators may play similar or distinct roles in different cell types. For instance, one of the most critical molecules involved in controlling exosome release is Rab27a, the downregulation or deletion of which significantly reduces exosome levels in various cells [62–64]. However, in hepatocellular carcinoma cells, Rab27a is the one that induces the decrease in exosomes [59]. In fact, our understanding of the regulators in the biogenesis of exosomes is still in its infancy, additional studies will be required to unravel these mysteries.
Exploring the definition of TAM heterogeneity
Macrophages are guardians of homeostasis in all organs with shared responsibilities of phagocytosis and tissue repair. Moreover, macrophages respond to different signals and broadly adapt to varying physiological and pathological circumstances in their ontogeny, resulting in distinct macrophage subsets that differ in phenotype and function between and within tissues [65]. For example, alveolar macrophages in the lung eliminate inhaled particles and pulmonary surfactant, whereas skeletal muscle macrophages facilitate muscle growth and regeneration [66]. Many other functions such as immune surveillance, antigen presentation, and tissue injury repair, are essential responsibilities for macrophages as well [67]. TAMs are converted from bone marrow-derived macrophages (BMDMs) and tissue-resident macrophages (TRMs) through tumor-mediated re-education [5]. Consequently, TAMs display the signature of heterogeneous phenotypes and functions, consistent with the cells they originate from.
Researchers have been trying to define the heterogeneity of macrophages and TAMs for years. Two decades ago, Mills et al. proposed the M1/M2 macrophage polarization paradigm based on different arginase metabolism. They termed macrophages that primarily metabolize arginase to nitric oxide (NO) or ornithine as M1 (tumor-suppressing) or M2 (tumor-promoting), respectively [68]. After that, the M1/M2 paradigm was intermingled with the concept of different activation states of macrophages, which had been defined earlier. By definition, macrophages are classically activated in response to interferon-γ (IFN-γ) and lipopolysaccharide (LPS), and alternatively activated in response to IL-4 and IL-13 [8]. Over the years, with a greater understanding of macrophages, the implications of M1/M2 paradigm have been constantly replenished. Macrophages are considered to exhibit a continuum of phenotypes from M1 to M2. M1 (classically activated) macrophages that are generally stimulated by IFN-γ and LPS, subsequently activate signal transducer and activator of transcription 1 (STAT1) and interferon regulatory factor 1 (IRF1), which results in the production of IFN-γ, IL-1β, and tumor necrosis factor-α (TNF-α). As for M2 (alternatively activated) macrophages, the exposure to IL-4 and IL-13 increases the production of IL-10 and transforming growth factor-β1 (TGF-β1) through the activation of STAT6 and IRF4 [69]. In short, M1 macrophages exhibit a pro-inflammatory and anti-tumor phenotype, whereas M2 macrophages inhibit inflammation and promote tumor progression.
Although the M1/M2 paradigm has a certain value in understanding, discussing, and applying the pre-existing studies, it also has limitations that should be recognized. The M1/M2 paradigm was established on several single in vitro stimuli, and both the TME and the macrophage complexity could not be recapitulated. Specifically, M1-like TAM could show a tumor-promoting phenotype. For instance, M1-like TAMs are capable of promoting the invasion and metastasis of ovarian cancer cells through secreting TNF-α which activates the nuclear factor-kappa B (NF-κB) signaling pathway [70]. In oral squamous cell carcinoma (OSCC), M1-like TAMs induce growth differentiation factor-15 (GDF-15)-mediated erythroblastic leukemia viral oncogene homolog 2 (ErbB2)-phosphorylation, thus enhancing the survival and invasive potential of OSCC cells [71]. M1-like TAMs also significantly contribute to the epithelial-mesenchymal transition (EMT) process and cancer cell stemness via the IL6/STAT3/THBS1 feedback loop in OSCC [72]. Furthermore, M2-like TAMs have been verified to contribute to prostate cancer progression through upregulated IL-6, which is associated with highly expressed Yin Yang 1 (YY1) [73]. More surprisingly, the co-expression of M1 and M2 marker genes and a positive correlation between them in TAM have also been discovered in single-cell studies [74, 75].
In recent years, advances in single-cell technologies have enabled researchers to detect individual TAMs of distinct transcriptome, epigenome, spatial omics, and so on, and thus identify TAMs of different states and spatial distributions (Table 1) [76].
Table 1.
Human TAM subtypes and markers identified by scRNA-seq
| Cancer type | TAM subtype | Characteristic markers | Findings | References | scRNA-seq data |
|---|---|---|---|---|---|
| Breast cancer | Mac: CXCL10 | CXCL10, PD-L1, PD-L2 | Resemble “M1-like” phenotype | [77] | GSE176078 |
| Mac: EGR1 | EGR1 | Resemble “M2-like” phenotype | |||
| Mac: SIGLEC1 | SIGLEC1 | Resemble “M2-like” phenotype | |||
| LAM1: FABP5 | FABP5, TERM2, CCL18, PD-L1, PD-L2 |
Obesity and lipid metabolism Immune regulation and tumor promotion |
|||
| LAM2: APOE | APOE, TERM2, CCL18, PD-L1, PD-L2 |
Obesity and lipid metabolism Immune regulation and tumor promotion |
|||
| Cluster0 (TERM2) | APOE, TREM2, CADM1, SPP1, ISG15, LYZ, FCN1 | Cancer development | [78] | GSE192935,GSE114725 | |
| Cluster1 (TREM2) | APOE, TREM2, SPP1, ISG15, APOC1, CTSD | Cancer development | |||
| Cluster2 (FOLR2) | APOE, FOLR2, SEPP1, SLC40A1, MRC1, LYVE1 |
Tissue-resident macrophages Immune promotion Positively correlate with better prognosis |
|||
| MAC-CXCL2 | C5AR1 | Not reported | [79] | GSE206638 | |
| MAC-FBP1 | MT1X-G-H, FN1 | Not reported | |||
| MAC-FCGBP | FCGBP, CD1A, TACSTD2 | Not reported | |||
| LAM-APOC1 | APOC1, APOE, TREM2, GPNMB, FOLR2, LAG3, PDCD1LG2, CD200 | Lipid metabolism, antigen cross-presentation, IFN-α and -γ signaling pathways | |||
| LAM-STAB1 | STAB1, TREM2, GPNMB, APOE, LYVE-1, FOLR2, CD209, CD276, PDCD1 | Lipid metabolism, tumor promotion, MMP and collagen degradation pathways | |||
| Colorectal cancer | C1QC+ MRC1− macrophage | C1QC+ MRC1− | Not reported | [80] | HRA000979 |
| SPP1+ macrophage | SPP1, FCGR3A, C1QC, MRC1, ITGAM, ANPEP, | Polarization of macrophages, shorter PFS, immunotherapy resistance | |||
| VCAN+ macrophage | VCAN, FCGR3A, MRC1, ANPEP | Not reported | |||
| THBS1+ macrophage | FCGR3A, C1QC1, MRC1, CD209, CMKLR1 | Antigen presentation, the intestinal immune network regulation for IgA production | |||
| S100A9 Mac/Mono | S100A9high | Immunosuppression | [81] | GSE56699,GSE14333,GSE39582,GSE17536,GSE17537,GSE33113,GSE37892 | |
| Cluster0 | STAB1, SIRPα | Immune escape | [82] | GSE178341 | |
| Cluster1 | MACRO, SPP1, SIRPα | Immune escape | |||
| Cluster2 | FTL | Not reported | |||
| Cluster3 | MKI67, SIRPα | Immune escape | |||
| Cluster4 | Not reported | Not reported | |||
| Cluster5 | FOLR2 | Not reported | |||
| OAS+ macrophage | OAS1 | Innate immune response | [83] | HRA003569 | |
| OLR1+ macrophage | OLR1 | G protein-coupled receptor and growth factor receptor binding | |||
| FOLR2+ macrophage | FOLR2 | Tissue-resident macrophage, lipid metabolism, anti-inflammation | |||
| Gastric cancer | Pro-inflammatory macrophage | S100A8, S100A9, IL1B, CXCL8 | Negatively correlated with anti-inflammatory macrophage | [84] | GSE206785 |
| Anti-inflammatory macrophage | APOE, MAF, C1QB, SEPP1 | Reduced survival | |||
| Tissue-resident macrophage | F13A, CCL2, FOLR2, CCL2, LYVE1, SEPP1, F13A1 | Not reported | |||
| Mφ_THBS1 | IL1B, NLRP3, VEGFA, EREG, MITF, NR1H, TFEC | Tissue-resident macrophages | [85] | HRA000704 | |
| Mφ_APOE | APOE, TREM2, C1QA, GPNMB, GRN, CD63, LAMP1 |
Lipid-associated and lysosome functions Tumor progression |
|||
| Glioblastoma | MARCO+ macrophage | MARCO | Tumor progression, poor clinical outcomes, mesenchymal trait, hypoxia | [86] | GSE141383 |
| GPNMB+ macrophage | GPNMB | Promote PN-MES transition and impede T cell activation | [87] | GSE103224, GSE138794,GSE139448,GSE131928 | |
| MPO+ macrophage | MPO | Anti-tumor cytotoxic function | [88] | GSE154795, GSE162631 | |
| Proliferating TAM (C7) | MKI67 | Not reported | [89] | HRA004677 | |
| IL1+ TAM (C6) | IL1 | Inflammatory response pathways, macrophage activation | |||
| Undefined cluster (C5) | Not reported | Not reported | |||
| SIGLEC9+ SEPP1+ TAM (C2) | SIGLEC9, SEPP1 | Immunosuppression, angiogenesis Monocyte-derived macrophage | |||
| SIGLEC9+ MARCO+ TAM (C9) | SIGLEC9, MARCO |
Immunosuppression Monocyte-derived macrophage |
|||
| Hepatocellular carcinoma | TREM2+ TAM (C6) | TREM2 | Anti-inflammation | [90] | GSE149614 |
| MoMF (C16, C26) |
FCN1hi, LYZhi, VCANhi, CD68lo, CD14lo, FCGR3Alo |
Monocyte-derived macrophage | |||
| VEGFA+ TAM (C21) | VEGFA, NFKB1, HSPA1A, HSPA1B | Oxidative stress | |||
| MPP9+ TAM (C23) | CD45+, CD68+, CD11b+, MMP9+, SPP1, ITGAM | Tumor progression, migration, invasion, and angiogenesis, associated with worse overall survival | |||
| SPP1+ macrophage | SPP1, TREM2 | Hypoxia, tumor progression, phagocytosis suppression | [91] | Mendeley Data (skrx2fz79n) | |
| FOLR2+ macrophage | FOLR2, APOE, C2 | Not reported | |||
| CXCL10+ macrophage | APOBEC3A |
Polarization of proinflammatory macrophages Monocyte-derived macrophage |
|||
| CCL3L1+ macrophage | CD74, HLA-DR, HLA-DP, HLA-DQ |
Antigen presentation Monocyte-derived macrophage |
|||
| Proliferating macrophage | Not reported | Not reported | |||
| CXCL10+ TAM | CXCL9, CXCL10, STAT1, IDO1, GBP1 | T cell recruitment, IFN -γ signalling, response to atezo/bev | [92] | EGAS00001007547 | |
| PPT1+ macrophage | Galectin-9hi, CD172ahi, CCR2hi, CD80lo, CCR7lo | High infiltration of T cells but immune exhaustion and immunosuppression, worse clinical outcome | [93] | GSE125449 | |
| TREM2 Macro | TREM2, APOE, APOC1 | Microvascular invasion, similar to LAM, anti-inflammation | [94] | GSE242889 | |
| SCLC | IPF-associated pro-fibrotic macrophage | CD14, CD1, CD81, ITGAX, CSF1R, SPP1, CD74, VSIG4 | ECM deposition and remodeling, immune inhibition | [95] | N/A |
| NSCLC | FABP4-MΦ | FABP4 | Enriched in LUAD, phagocytosis, fatty acids and obesity, | [96] | SCIENCEDB.02028 |
| FCN1-Mφ | FCN1, SPP1 | Enriched in LUAD, phagocytosis | |||
| SPP1-Mφ | SPP1, SELENOP, FCN1 | Enriched in LUSC, proinflammatory and anti-tumor function, tumorigenesis, angiogenesis | |||
| SELENOP-Mφ | SELENOP | Good prognosis, local antioxidant capabilities, lymphocyte activation, nucleoside phosphate metabolism | |||
| Pancreatic cancer | IL1B+ TAM | IL1B, IL1A, NLRP3, PTGS2, CCL3 | Inflammatory response, leukocyte recruitment, angiogenesis | [97] | GSE217847 |
| MKI67+ TAM | MKI67, TOP2A, PCLAF, UBE2C, TK1 | Cell cycle | |||
| FOLR2+ TAM | FOLR2, LYVE1, SELENOP, SLC40A1, MRC1 | Tissue-resident macrophages | |||
| SPP1+ TAM | SPP1, MARCO, FBP1, APOC1, LIPA | Lipid metabolism, phagocytic receptor expression | |||
| HSP+ TAM | HSPA6, SERPINH1, BAG3, HSPB1, HSPD1 | Not reported | |||
| MT+ TAM | MT1H, MT1G, MT1X, MT1E, MT2A | Not reported | |||
| Pancreatic ductal adenocarcinoma | SPP1+ TAM | SPP1, MIF, CXCL8, TREM2 | Tumor infiltrating CD8+ T cell exhaustion | [98] | GSE231535 |
| GRN+ TAM | GRN, APOC1 | Monocyte-derived macrophage, CD8+ T cell exclusion |
MMP matrix metalloproteinases, PFS progression-free survival, PN proneura, MES mesenchymal, atezo/bev atezolizumab/bevacizumab, LAM lipid-associated macrophage, IPF idiopathic pulmonary fibrosis, LUAD lung adenocarcinoma, LUSC lung squamous cell carcinoma, HSP hot-shock protein, MT Metallothionein
.
A review that focuses on TAMs in recent major studies of single-cell omics proposed a new model with seven conserved subsets of TAMs across almost all types of cancers according to their gene expression, signaling pathway, and biological functions in the TME. Of these subsets, interferon-primed TAMs and immune regulatory TAMs are paralogs of M1-like and M2-like macrophages, respectively, but both of them limit anti-tumor immune response in vivo. Conversely, inflammatory cytokine-enriched TAMs recruit immune cells and promote inflammation. In addition, TAMs that are associated with tumor angiogenesis, tumor cell proliferation, EMT, and so on are illustrated in the model as well [99]. The review cited above excellently summarized the main types of TAMs, but cancer-specific subsets are not included. For example, scar-associated macrophages are specific TAMs in liver cancer with gene signatures distinct from that of Kupffer cells [100]. More recently, Bill et al. propose defining TAMs polarization by CXC chemokine ligand 9 (CXCL9) and secreted phosphoprotein 1 (SPP1) expression, which is mostly mutually exclusive in TAMs. Their results suggest that the CXCL9 and SPP1 (CS) ratio, instead of M1 and M2 markers expression, are strongly positively associated with a better prognosis. Additionally, CS polarity in TAMs is related to immune cell infiltration and gene expression in largely all cell types in tumors, both of which regulate tumor control or progression [101]. Taken together, as a precise dichotomy, CS polarity may be a better choice to elaborate TAM heterogeneity. It provides a new approach for designing in vitro experiments of TAMs. Currently, there is a lack of studies that are based on CS TAM polarity, whereas the M1/M2 paradigm has been used for years. Thus, in this review, the M1/M2 paradigm will only be invoked to refer to the experimental design and results in those previous studies.
Factors influencing TAM-derived exosome heterogeneity in cancer
The heterogeneity of TAM-derived exosomes arises from many factors in cancer, such as cancer types (Fig. 2), and the TME. Different tissue or organ origins and mutations characterize cancer types and define how they respond to exosomes. Therefore, the same cargo derived from TAMs in different cancer types may exert different functions, as miR-223 confers invasiveness on breast cancer cells through the Mef2c-β-catenin pathway, but induces resistance to distinct chemotherapeutic drugs in EOC and gastric cancer (GC) through different pathways [102–104]. Likewise, miR-21 elicits resistance to cisplatin resistance in GC while promoting resistance to temozolomide in glioblastoma [105, 106]. Furthermore, the same cargo from TAM-derived exosomes can induce similar phenotypes in different cancer types through distinct mechanisms. Studies focused on M2 TAM-derived exosomal miR-221-3p suggested that miR-221-3p binds to cyclin-dependent kinase inhibitor 1B (CDKN1B) and promotes G1/S transition in EOC cells, but targets suppressor of cytokine signaling 3 (SOCS3) and activates JAK2/STAT3 in osteosarcoma (OS) cells. Though miR-221-3p in both two cancer types contributes to cancer cell proliferation and migration, the distinct mechanisms underline the effect of cancer-specific contexts on TAM-derived exosome heterogeneity in signaling pathways [107, 108].
Moreover, the conditions and contents within the TME, such as hypoxia and lactate, can affect TAM states and their exosomes. Regions of hypoxia are due to the rapid and uncontrolled proliferation of tumors that outgrow the oxygen supply of their surrounding vasculature [109]. Hypoxic TAMs are similar to M2-like phenotype and release exosomes with higher levels of miR-155-5p, which could bind to human antigen R (HuR) in renal cell carcinoma (RCC) cells, thus increasing insulin-like growth factor 1 (IGF1R) mRNA stability. Overall, hypoxia activates IGF1R/PI3K/AKT cascades to promote RCC proliferation and migration through increasing TAM-derived exosomal miR-155-5p [110]. Additionally, in EOC cells, hypoxic TAMs have been found to secrete higher levels of exosomes compared to normoxic TAMs. These exosomes also exhibit an enhanced ability to induce proliferation and resistance to apoptosis in EOC cells [103]. Regardless of whether oxygen is present or not, cancer cells metabolize glucose to lactate by glycolysis, a phenomenon commonly known as the Warburg effect. More interestingly, TAMs are proved to be the most dominant consumers of glucose in the TME, thereby promoting lactate accumulation similarly [111]. Lactate has the potential to upregulate the hypoxia-inducible factor (HIF)−1α-stabilizing long noncoding RNA (HISLA) in both TAMs and their exosomes. In breast cancer cells, HISLA suppresses the hydroxylation and degradation of HIF-1α by binding to prolyl hydroxylase domain 2 (PHD2) and inhibiting the interaction between PHD2 and HIF-1α, which boosts aerobic glycolysis and induces apoptosis resistance in breast cancer cells [112].
Effects of TAM-derived exosomes on cancer progression and metastasis
Solid cancer forms an intricate ecosystem comprising diverse tumor-infiltrating cells and non-cellular components, and interactions among these elements play a crucial role in cancer [113]. In the previous section, we have already discussed the impact of cancers on TAM-derived exosomes. Likewise, recent studies have revealed that TAM-derived exosomes influence cancers directly by interacting with cancer cells, or indirectly, through remodeling the cells and tissue in the TME (Fig. 3). The advances in this area that embody the multifaceted role of TAM-derived exosomes are briefly summarized below. This diverse range of functions suggests that in cancer therapy aiming at suppressing the function of TAMs, directly targeting TAMs could be a better option than targeting TAM-derived exosomes.
Fig. 3.
The contribution of TAM-derived exosomes in cancer progression and metastasis. TAM-derived exosomes contribute to the malignant behavior of cancer cells through ncRNAs such as miRNA, CircRNA, and LncRNA. For instance, miRNA facilitates cancer cell proliferation and metastasis by targeting mRNA to regulate gene expression, while CircRNA functions as a miRNA sponge that modulates gene expression by interacting with miRNA. Moreover, LncRNA LINC01232 facilitates the evasion of cancer cells from CD8 + T cell-mediated immunity attack through degrading and downregulating MHC-I. Furthermore, PD-L1 within exosomes from both TAMs and tumor cells leads to immune suppression by limiting CD8 + T cell activation and proliferation. TAM-derived exosomes also alter the differentiation of naïve CD4 + T cells and the balance of CD4 + T cell subsets, thus aggravating immune suppression. Additionally, TAM-derived exosomes promote the formation of the vascular system through various means, including enhancing vasculogenic mimicry and angiogenesis. ncRNAs non-coding RNA, let-7a lethal-7a, C15orf41 chromosome 15 open reading frame 41, E2F3 E2F transcription factor 3, NBR1 neighbor of breast cancer 1 gene, TCR T cell antigen receptor, PD-L1 programmed death-ligand 1, PD-1 programmed cell death protein 1, Treg Regulatory T cell, Th1 T Helper 1 cell, TIMP2 tissue inhibitor of metal protease 2
TAM-derived exosomes facilitate the malignant phenotypes of cancer cell
TAM-derived exosomes mostly modulate cancer cells by changing gene expression with their ncRNA cargos including miRNA, lncRNA, and circRNA [114]. MiRNAs post-transcriptionally suppress the expression of target genes through binding to target mRNAs and mediating mRNA degradation or translation inhibition [115]. For example, exosomal miRNA lethal-7a (let-7a) released by TAMs targets and downregulates chromosome 15 open reading frame 41 (C15orf41) in OS, thereby promoting the migration and invasion of OS cells. In addition, inhibition of C15orf41 expression activates the PI3K/AKT pathway, which promotes the proliferation of OS cells [116]. LncRNA is a multifunctional regulatory molecule that interacts with DNA, RNA, and proteins to engage in multilevel regulation, encompassing epigenetic modification, transcriptional control, and post-transcriptional regulation [117]. In glioma cells, TAM-derived exosomal lncRNA LINC01231 binds to E2F transcription factor 2 (E2F2) and transports E2F2 to the nucleus, inducing an increase in the neighbor of breast cancer 1 gene (NBR1). NBR1 binds to MHC-I and promotes MHC-I degradation in autophagolysosomes. This leads to the downregulation of MHC-I expression on glioma cells surface and subsequently contributes to the immune escape of glioma cells [118]. The most well-established and characteristic function of circRNA is to serve as miRNA sponges that inhibit corresponding miRNAs suppressing their target mRNAs by binding and sequestering miRNAs [119]. An illustrative instance of this phenomenon is TAM-derived exosomal circ_0020256. E2F3, a target of miR-432-5p, is upregulated in cholangiocarcinoma (CCA) cells as a result of circ_0020256 specifically sponging miR-432-5p. E2F3 overexpression accounts for why TAM-derived exosomal circ_0020256 enhances the proliferation, migration, and invasion of CCA cells [120].
TAM-derived exosomes remodel immune cells and tissue in the TME
Besides direct interactions, TAM-derived exosomes also regulate cancer progression and metastasis via the effect of remodeling TME, such as altering the tumor immune microenvironment and inducing vasculature formation. Recent studies illustrate that TAM-derived exosomes exert both promoting and suppressive activities in anti-tumor immunity. Guo and colleagues confirmed that levels of circulating exosomal PD-L1 in melanoma patients were significantly higher than those in healthy donors, as a result of melanoma cells releasing exosomal PD-L1 [121]. Following this discovery, they also demonstrated that the transition of macrophages to TAMs results in a significant increase in exosomes secretion, along with elevated PD-L1 expression on exosomes [122]. Both types of exosomes collaborate to affect CD8+ T cells through the presence of PD-L1, leading to the inhibition of CD8+ T cell proliferation and activation, thereby suppressing their cytotoxic effects on cancer cells. Added to the direct suppression of antitumor immunity, TAM-derived exosomes also mediate the imbalance among immune cell subsets. Naïve CD4+ T cells have the potential to differentiate into various subsets including T helper 1 (Th1) cells, Th17 cells, and regulatory T cells (Treg) [123]. The cytokines produced by Th1 cells trigger inflammation and promote the anti-tumor immune response, whereas Tregs suppress T cell activation and hinder the anti-tumor immune response in the context of cancer [124, 125]. Whether Th17 cells are pro-tumorigenic or tumor-restraining are context-dependent [126]. In the case of ovarian cancer, the levels of infiltrating Th17 cells and IL-17 they produced predict a favorable prognosis [127]. The Treg/Th17 ratio is verified upregulated in EOC and positively correlated with higher EOC malignancy grades, which can be induced by TAM-derived exosomal miR-29a-3p and miR-21-5p. These miRNAs regulate the differentiation of CD4+ T cells by suppressing the signal transducer and activator of transcription 3 (STAT3), which is pivotal for immunomodulation, including the differentiation and development of immune cells and maintenance of immune homeostasis [128, 129]. Similarly, in malignant pleural effusion of cancer patients, the overexpressed macrophage-derived exosomal miR-4443 triggers CD4+ T cells to differentiate into Treg cells instead of Th1 cells [130]. While these findings suggest that TAM-derived exosomes contribute to shaping an immune-suppressive microenvironment that facilitates cancer progression and metastasis, an interesting observation emerges in CRC: TAM-derived extracellular vesicles, including exosomes, exhibit an M1-like phenotype that induces CD8+ T cells proliferation and activation. In addition, this phenotype is significantly associated with a favorable clinical outcome. More surprisingly, the TAMs that release these EVs display an M2-like signature which is uncorrelated with either a benign or poor prognosis [131].
Angiogenesis is known as a prerequisite for the invasion and metastasis of solid tumors. Cancer cells in hypoxic niches recruit TAMs to release pro-angiogenic growth factors and degrade the extracellular matrix, which stimulates angiogenesis [132]. Recent studies indicate that TAM-derived exosomes have also been implicated in this process. A mouse model of pancreatic ductal adenocarcinoma (PDAC) reveals that miR-155-5p and miR-221-5p from M2 macrophages could decrease E2F2 expression in endothelial cells to promote angiogenesis and growth, thereby enhancing PDAC progression [133]. There also exist other types of vasculature systems in tumors such as vasculogenic mimicry, known as an endothelial cells-independent tumor microcirculation model strongly correlated with tumor invasion, metastasis, and poor prognosis [134]. In a clear-cell renal cell carcinoma (ccRCC) mouse model, TAM-derived exosomal miR-193a-5p target tissue inhibitor of metal protease 2 (TIMP2) and limit its expression in ccRCC cells, thus enhancing vasculogenic mimicry and invasion of ccRCC [135]. This function greatly enhances the metastasis of cancer.
Generating and modifying macrophage-derived exosomes in vitro: potential and challenges in cancer therapy
Advantages of macrophage-derived exosomes in clinical application
An emerging research priority in exosomes is therapeutically exploiting exosomes as “Trojan Horses” for therapeutic molecule delivery [4]. As nano-sized vesicles from endogenous sources, exosomes are characterized by high biocompatibility, low cytotoxicity, and immunogenicity [136]. These advantages have drawn the attention of researchers towards loading therapeutic molecules into exosomes, aiming to directly target and eliminate cancer cells, boost the effectiveness of other cancer therapies, or modulate tumor immunity [137].
Considering different cell sources partly determine the functions and targets of exosomes as previously mentioned, macrophage-derived exosomes possess unique properties such as overcoming the blood–brain barrier (BBB), accumulating in the tumor site, and reactivating antitumor immunity [11–13, 138, 139]. Specifically, due to the presence of the BBB, some of the therapeutic molecules are prevented from arriving at brain lesions [140]. Nevertheless, macrophage-derived exosomes loaded with protein cargo have been proven capable of crossing the BBB through the interaction between the integrin lymphocyte function-associated antigen 1 (LFA-1) on exosomes and the intercellular adhesion molecule 1 (ICAM-1) on human cerebral microvascular endothelial cells [138]. After systemic injection, natural M1 macrophage-derived exosomes (M1-exos) spontaneously home to and accumulate at tumor sites, mirroring the natural accumulation of M1 macrophage in tumors [11, 139]. In the meantime, natural M1-exos also enrich in the lung, liver, and spleen, indicating a lack of specificity for tumors [11]. Furthermore, M1-exos reactive antitumor immunity in various ways. For instance, M1-exos stimulate the activation of NF-κB and the production of inflammatory cytokines in macrophages to elicit inflammation within breast cancer. Meanwhile, these exosomes increase apoptosis in breast cancer cells via increasing caspase-3 activity [11]. Similarly, M1-exos reduce the PD-L1 expression in GC cells and enhance the anti-tumor immunity of T cells in GC by transferring miR-16-5p to GC cells and targeting PD-L1 [12]. In addition, M1-exos have been found capable of mediating the in situ re-polarization of M2-like TAMs to M1-like TAMs that highly express MHC class II and delay tumor growth in vivo [13]. In conclusion, these advantages underscore the therapeutic potential of macrophage-derived exosomes, especially M1-exos, warranting further exploration for their application in cancer therapy.
Other immune cell-derived exosomes also have their unique advantages. For example, dendritic cells (DC)-derived exosomes contain abundant MHC class I/peptide complexes, which can prime T cells and induce anti-tumor responses, making DC-derived exosomes a promising candidate for cancer vaccines [1]. In a mouse model of HCC, DC-derived exosomes modified by α-fetoprotein (AFP) can trigger antigen-specific immune responses and effective tumor suppression, thus providing a feasible approach for HCC immunotherapy [141]. However, some clinical trials using DC-derived exosomes have reported limited T-cell responses, potentially due to the suppression of Tregs, which must be addressed to improve the efficacy of DC-derived exosomes in cancer immunotherapy. Encouragingly, except for T cells, DC-derived exosomes also activate natural killer (NK) cells, highlighting the need for further exploration into their underlying mechanisms and therapeutic potential [142].
Exosomes-based strategies for cancer therapy
To prepare M1-exos for mice models, RAW264.7 or bone marrow cells that are isolated from mice are cultured with LPS or IFN-γ and then polarized to M1-macrophages [11, 16, 143]. After that, M1-exos are collect from the supernatant by ultracentrifugation in most cases. Other methods like ultrafiltration, precipitation, and immunoaffinity capture are also feasible [144]. However, using natural exosomes directly for cancer treatment is infrequent. To achieve multiple goals and maximize the efficacy of exosomes in the war on cancer, researchers have conferred different characteristics to exosomes through different strategies, such as engineered exosomes, hybrid exosomes, and exosome-like nanovesicles (Fig. 4). Notably, combining these strategies is preferred over using them individually, as it provides multiple improvements in efficacy and anti-tumor activity.
Fig. 4.
Modified macrophage-derived exosomes hold promise for cancer therapy. Common exosome-based strategies (inner ring) encompass the engineered exosome with surface decoration and/or inner therapeutic molecules, the ELNV generated through continuous sonication and extrusion of cell membranes, and the hybrid exosome comprised of exosomes and other types of membranes. Existing studies have demonstrated that modified macrophage-derived exosomes possess unique advantages and functions in multiple cancer therapies (middle ring). The specific benefits that these therapies may obtain from modified macrophage-derived exosomes are also listed (outer ring). ELNV exosome-like nanovesicle, M1-exos M1 macrophage-derived exosomes, SIRPα signal regulatory protein
Engineered exosomes
Engineered exosomes refer to exosomes that are applied with surface modifications and/or internally loaded with therapeutic molecules [137]. After intravenous injection, exogenous natural exosomes from several sources are distributed mainly in the liver, spleen, lung, and gastrointestinal tract, where exosomes are actively cleared by macrophages [145]. Consequently, surface modifications to enhance targeting specificity and avoid phagocytosis are crucial. For example, AS1411, a type of aptamer, can efficiently recognize and bind to the nucleolin, which is upregulated on the surface of multiple cancer cells [146]. Thus, AS1411 aptamer-modified exosomes possess the ability to target several cancer cells, such as CRC cells, glioblastoma (GBM) cells, and squamous cell carcinoma (SCC) cells [14, 146, 147]. To resist macrophage-mediated immune phagocytosis, cancer cells overexpress various “don’t eat me” signals, like CD47, which binds to signal regulatory protein α (SIRPα) on the macrophage surface [148]. Likewise, CD47 modification on the surface of engineered exosomes contributes to a longer blood circulation time by invading phagocytosis [16, 149, 150]. Furthermore, CD47 on exosomes competitively binds to SIPRα, thereby repressing CD47/SIPRα between cancer cells and macrophages, and consequently causing more cancer cells phagocytosed [16, 150]. Therapeutic molecules encapsulated within engineered exosomes mainly include chemotherapeutic drugs and nucleic acid [4]. These molecules will be further discussed later in the context of specific treatment modalities.
Exosome-like nanovesicles
Exosome-like nanovesicles (ELNVs) are nanovesicles with exosome-like features such as size, structures, and contents [151]. ELNVs can be generated from the continuous sonication and extrusion of cell membranes. The functions of ELNVs are also consistent with their cells of origin, making ELNVs a suitable substitute for exosomes, whose yield is inadequate for therapeutic strategies [152]. Similar to M1-exos we have mentioned before, M1 macrophages-derived ELNVs can reprogram M2 TAMs to M1 TAMs and increase CD8+ T cell infiltration [152, 153]. The amelioration of immunosuppressive TME improve the efficacy of CD47 blocker, which enhances macrophage-mediate phagocytosis of cancer cells [154]. In this way, these ELNVs inhibit the recurrence and metastasis of malignant melanoma [152].
Hybrid exosomes
Hybrid exosomes are comprised of the fusion of exosomes from different sources, including the fusion of different types of exosomes or ELNVs, as well as the fusion of exosomes with plasma membranes or liposomes [155]. This fusion combines the advantages of multiple membranes. For instance, the hybrid exosomes of CD47-modified TDEs and macrophage-derived exosomes inherit the features of targeting cancer cells, promoting phagocytosis, and mediating repolarization of M2-like TAMs to M1-like macrophages [16]. Additionally, exosomes fused with ELNVs and liposomes compensate for the yield deficiency of natural exosomes [151]. Particularly, a type of hybrid cell is generated by introducing cancer cells nuclear to activated M1-like macrophages. These hybrid cells release exosomes (aMT-exos) that accumulate in lymph nodes and tumor sites after subcutaneous injection, respectively consistent with the feature of macrophages and tumor cells. More importantly, aMT-exos effectively limit primary tumor growth, tumor metastasis, and postsurgical tumor recurrence, likely due to the aMT-exos-mediated immune activation in lymph nodes and the TME [156].
Modified macrophage-derived exosomes-based strategies for cancer therapy
In recent years, many new studies for exosomes have sprung up, as have related M1-exos-based therapies (Table 2). Modified M1-exos provide cancer therapies with specific targeting ability and stable delivery platforms, inducing higher safety and effectiveness (Fig. 4). Below, we discuss how modified macrophage-derived exosomes facilitate current cancer therapies.
Table 2.
Preclinical experiments of modified macrophages-derived exosomes for cancer therapy
| Clinical therapy | Tumor model | Membrane composition | Surface modification | Cargo | References |
|---|---|---|---|---|---|
| Chemotherapy | Breast cancer | Macrophage-derived sEV and synthetic liposome | N/A | Doxorubicin | [157] |
| Breast cancer | M1-exo | N/A | Docetaxel | [158] | |
| Breast cancer | M1-exo | N/A | Paclitaxel | [11] | |
| Breast cancer | Macrophage-derived exosome | N/A | Platinum, HSA, and lecithin | [159] | |
| TNBC | Macrophage-derived exosome | N/A | Doxorubicin | [160] | |
| Pancreatic Cancer | M1-exo | N/A | Gemcitabine and Deferasirox | [161] | |
| Bladder cancer | M1-exo | N/A | Gemcitabine | [162] | |
| Lung cancer | M1-exo | C-Met binding peptide | Cisplatin | [163] | |
| Radiotherapy | Lung cancer | M1-exo | Anti-PD-L1 nanobody | CAT and DNA damage repair inhibitor | [15] |
| Immunotherapy | Breast cancer | M1-exo | IL-4R-binding peptide | NF-κB p50 siRNA and miR-511–3p | [143] |
| Breast cancer | M1-exo | N/A | RSL3 | [139] | |
| TNBC | P-NV, M1-NV, and SαV-C-NV | SIRPα variants | N/A | [152] | |
| Melanoma | M1 macrophages-derived EV | N/A | SiPAK4 and photoactivatable ROS-sensitive polymer | [164] | |
| Sonodynamic Therapy | Glioblastoma | Macrophage-derived exosome | AS1411 aptamer | SiO2 encapsulated CAT and ICG | [14] |
| Chemo-immunotherapy | Breast cancer | TDE and M1-exo | CD47 | DNA-targeting agent (SN38) and STING-agonist (MnO2) | [16] |
| Chemo/gene/ photothermal therapy | Breast cancer | Macrophage-derived exosome | PDA coated Fe3O4 and miR-21-targeting MB | Doxorubicin | [165] |
| Immuno/gas/ photodynamic therapy | Colorectal cancer | M1-exo | N/A | Ce6-loaded upconversion | [166] |
sEV small extracellular vesicle, M1-exo M1 macrophage-derived exosomes, TNBC Triple-negative breast cancer, HSA human serum albumin, c-Met mesenchymal-epithelial transition factor, PD-L1 programmed cell death-ligand 1, CAT catalase, NF-κB nuclear factor kappa-B, NV nanovesicle, P-NV platelet-derived NV, M1-NV M1 macrophage-derived NV, SIRPα signal regulatory protein alpha, SαV-C-NV cancer cell-derived NVs overexpressing high-affinity SIRPα variants, SiPAK4 Small interfering RNA against p21-Activated kinase 4, ROS reactive-oxygen-species, ICG indocyanine green, TDE tumor-derived exosome, SN38 7-Ethyl-10-hydroxycamptothecin, STING stimulator of interferon gene, PDA polydopamine, MB molecular beacon
Chemotherapy
Chemotherapeutic drugs, a conventional therapeutic molecule for cancer therapy, are faced with obstacles including the absence of targeting ability, the potential for side effects, and drug resistance after systemic administration [167]. To overcome these limitations, M1-exos loaded with chemotherapeutic drugs are modified in different ways. For instance, utilizing hybrid exosomes containing TDEs or M1-exos components, as well as biological modifications to endow M1-exos with the capacity to target tumor cells, to avoid the side effects of chemotherapy [11, 16, 157, 160]. Moreover, the simultaneous loading of chemotherapy drug and molecule targeting its corresponding resistance mechanisms has been reported as an exceptional strategy to adverse drug resistance [161].
Targeted peptides are a type of biological modification that can be used to target triple-negative breast cancer (TNBC) cells. Specifically, the expression of cellular-mesenchymal-epithelial transition factor (c-Met) is increased in TNBC cells. Thus, the c-Met binding peptide-modified and doxorubicin (DOX)-load M1-exos avoid damage to main organs and promote the anti-tumor efficiency of DOX [160]. The specific reasons why the anti-tumor efficiency of chemotherapeutic agents loaded to M1-exos is better than that of chemotherapeutic agents alone are manifold. For instance, M1-exos inherently trigger inflammation and activate anti-tumor immune response [11, 158, 163]. Additionally, in a breast cancer model, M0-exos-loaded docetaxel (DTX) also exhibits better anti-tumor ability than DTX alone, suggesting that the absorption efficiency of exosomes is higher than that of bare drug molecules [158, 162]. Another application of M1-exos-based chemotherapies is to reverse drug resistance. For example, to ameliorate the severe chemoresistance of pancreatic cancer to gemcitabine (GEM), GEM and deferasirox (DFX) are loaded to M1-exos at the same time. As an iron chelator, DFX can act as the inhibitor of ribonucleotide reductase M2 (RRM2), whose overexpression is associated with a low sensitivity to GEM and a poor prognosis of pancreatic cancer patients [161].
Radiotherapy
Radiotherapy-mediated cellular damage relies heavily on the DNA damage caused by ionizing radiation (IR) and IR-induced ROS [168]. However, the immunosuppressive TME, hypoxia, and DNA damage repair in solid tumors contribute to limitations in efficacy and resistance to radiotherapy [169]. Targeting of these mechanisms inspires engineering M1-exos to improve tumor sensitivity to radiotherapy. First, PD-L1 antibody-modified outer surfaces and M1-exos-mediated repolarization ameliorate the immunosuppressive TME. Second, catalases that express on the inner surfaces of the membrane catalyze H2O2 to generate O2 and relieve hypoxia. Third, engineered M1-exos loaded DNA damage repair inhibitor to maintain cytotoxicity caused by radiotherapy. Furthermore, in vitro and in vivo experiments prove the safety and effectiveness of M1-exos, which can thus act as a promising radiotherapy sensitizer [15].
Immunotherapy
Immunosuppression is a hallmark of the TME, which allows cancer cells to evade immune surveillance and attack. This immunosuppressive state also reduces the sensitivity of cancer cells to therapeutic interventions, arousing growing interest in immunotherapy. The immune regulation function of modified macrophage-derived exosomes endows them with great potential in immunotherapy. TAMs, as key contributors to the immunosuppressive TME, have also attracted significant research interest, particularly in reversing their cancer-promoting functions to anti-tumor phenotypes [6]. Notably, the feature of M1-exos to repolarize cancer-promoting TAM to anti-cancer phenotype suggests that M1-exos-based strategies can serve as an emerging immunotherapy for cancer. For instance, IL-4-modified M1-exos selectively target IL-4R that is more highly expressed on cancer-promoting TAM instead of anti-tumor macrophages. Moreover, engineered M1-exos are loaded with NF-κB p50 siRNA and miR-511–3p, thereby enhancing cancer-promoting TAMs reprogramming into anti-tumor phenotype and suppressing cancer growth [143]. Furthermore, cyclic guanosine monophosphate-adenosine monophosphate synthase/stimulator of interferon gene (cGAS/STING) can be loaded to M1-exos as well. The activation of STING drives the maturation of the dendritic cells and increases the infiltration of natural killer cells in tumors through releasing IFN [16]. In addition to targeting immune cells, another alternative for M1-exos in immunotherapy is to interact with cancer cells. Specifically, Rao et al. have designed a hybrid NVs (hNVs) that are composed of M1-NVs, platelet-derived NVs (P-NVs), and SIRPα variant-overexpressed cancer cells-derived NVs (SαV-C-NVs). P-NVs confer hNVs the ability to bind to circulating tumor cells (CTCs) and injured tissue. As for SαV-C-NVs, the SIRPα variant promotes the phagocytosis of cancer cells. The specific mechanism is similar to that of overexpressed CD47. Taken together, hNVs target the operation site and regulate immunity, thus suppressing post-surgery recurrence and metastasis of melanoma. Notably, hNVs also successfully avoid immune-related adverse events [152].
Gas-assisted phototherapy
Another interesting fact about M1-exos is that they can produce NO for gas therapy with inducible nitric oxide synthase (iNOS) on their membranes [145]. Gas therapy utilizes gaseous molecules, such as oxygen (O2) and NO, that exhibit therapeutic function or assist other therapies [170]. Among them, the combination of phototherapy and gas therapy can effectively improve phototherapy. Phototherapy for cancer includes two main methods. One is photodynamic therapy (PDT), which relies on the chemical damage, such as ROS, generated by light-activated photosensitizers. The other is photothermal therapy (PTT), in which photothermal agents convert the energy from external light into heat and cause thermal damage within the tumor [171]. One example of PDT in combination with macrophage-derived exosomes-based gas therapy is M1-exos fused with upconversion nanoparticles which are loaded with Ce6, a type of photosensitizer for PDT [166]. Upconversion nanoparticles are capable of transforming near-infrared light to ultraviolet or visible light, thereby activating Ce6 to generate ROS to induce the damage and death of cancer cells [171]. The reaction between ROS and NO produced by M1-exos could generate reactive nitrogen species (RNS), which mediates cancer cell death more efficiently than ROS via stronger peroxidation and nitrification effects [166]. Though the assistant of M1-exos-derived NO to PTT has not been reported yet, macrophage-derived exosomes are still suitable for being a PTT platform combined with other therapies. In a therapy model of breast cancer, macrophage-derived exosomes are loaded with DOX and modified by magnetic nanoparticles that are coated with polydopamine (PDA), a type of photothermal agent. In the presence of an external magnetic field, magnetic nanoparticles target the tumor site, subsequently, near-infrared radiation and PDA induce local heating and the release of molecular beacons and DOX, thereby realizing photothermal therapy-based targeted killing of cancer cells [165]. Gene therapy is also engaged in this model, as macrophage-derived exosomes are coated with molecular beacons that target and silence miR-21, which is engaged in tumorigenesis and development in multiple cancer types [165]. This chemo/gene/photothermal therapy integrates the advantages of various therapies, providing new ideas for future study.
Challenges of modified macrophages-derived exosomes for cancer therapy
Though preclinical experiments in mouse models have preliminarily confirmed the potential of macrophage-derived exosomes-based strategies for cancer therapy, indeed, the application of macrophage-derived exosomes, as well as exosomes or EVs in general, is still in their early stages. There are still many challenges before clinical translation. So far, some exosome-based liquid biopsies and therapies have proven promising in clinical trials, whereas only one small clinical trial, which is still ongoing, is based on macrophage-derived exosomes (NCT05559177). Additionally, allogeneic macrophage-derived exosomes may be preferred in clinical translation to ensure the production of exosomes. However, it remains uncertain whether these exosomes could cause adverse effects, such as immune rejection, immune activation, or allergic reactions, as the immunogenicity and other possible risks of these exosomes have not been fully explored in existing preclinical studies. Characterization and standardized functional assays, with defined quantifiable metrics at the single exosome scale, are also essential to ensure the safety and effectiveness of macrophage-derived exosomes before clinical translation, considering they are highly heterogeneous even when derived from the same type of cells [172]. Moreover, achieving consistent results with macrophage-derived exosomes across different types of cancers is another challenge, considering there may be distinct responses due to differences in genetic expression, TME, and tumor locations. For example, M1-exos mediate the repolarization of M2-like macrophages to M1-like macrophages, M1-exos upregulate the ratio of M1-like/M2-like macrophages, which has been demonstrated beneficial for tumor-suppressive activities in distinct mouse models. However, a recent study of head and neck squamous cell carcinoma has discovered that the correlation is absent between clinical outcome and M1 and M2 markers expression, suggesting that the swift of M2 to M1 does not apply to the therapy for all types of cancers [101]. Thus, to exploit modified macrophage-derived exosomes that are suitable for various types of cancers, it is essential to carefully design their modifications, administration routes, and dosage to target specific cancer types. Above all, more preclinical studies and clinical trials are required to evaluate the effectiveness, safety, and reproducibility of macrophage-derived exosomes in cancer therapy.
In addition to the challenges faced by macrophage-derived exosomes in cancer therapy, the application of exosomes from all sources encounters several common hurdles, mainly including technical issues in standardized production and exploration of treatment regimens. Currently, low productivity, lack of high-purity isolation techniques, and instability in storage hinder exosomes from large-scale and low-cost production [173]. Despite the technical challenges associated with the clinical translation of exosomes, the rapid development of new technologies consistently builds our confidence in overcoming these challenges. Bioreactors and media supplements such as fetal bovine serum make large-scale production possible [174]. The isolation technique of exosomes has always been a focus of research due to its significance to clinical translation and exosome characterization [175]. The conventional isolation methods, such as ultracentrifugation, ultrafiltration, and precipitation, are widely used, but they are time-consuming and low in yield and purity, thus unsuitable for clinical applications [176]. In contrast, emerging methods like size-exclusion chromatography, show promise in clinical translation as they produce exosomes in large-scale and high purity. For instance, a method termed size exclusion–fast protein liquid chromatography (SE-FPLC) enables rapid isolation of exosomes while effectively removing albumin and lipoprotein contaminants, providing a potential solution for high-quality exosome isolation in clinical settings [177].
TAM-derived exosomes reduce the efficacy of cancer therapy
Though the macrophage-derived exosomes generated and modified in vitro show tremendous potential for multiple types of cancer therapy, still some existing studies suggest that TAM-derived exosomes in vivo tend to diminish the efficacy of cancer therapy (Table 3). These studies focused on understanding the molecules and pathways responsible for the resistance to cancer therapy and provide promising biomarkers and therapeutic targets for cancers.
Table 3.
Tumor-associated macrophage-derived exosomes in cancer therapy resistance
| Clinical therapy | Cancer type | Drug | Key cargo | Expression | Mechanisms | References |
|---|---|---|---|---|---|---|
| Chemotherapy | GC | Cisplatin | miR-21 | Up-regulated | Activate PI3K/AKT signaling pathway by down-regulating PTEN to promote cisplatin resistance | [105] |
| GC | Cisplatin | miR-588 | Up-regulated | Target and down-regulate CYLD to promote cisplatin resistance | [178] | |
| GC | Cisplatin | IncRNA CRNDE | Up-regulated | Activate PI3K/AKT signaling pathway by facilitating NEDD4-1-mediated PTEN ubiquitination to promote cisplatin resistance | [179] | |
| GC | Doxorubicin | miR-223 | Up-regulated | Target FBXW7 to impair doxorubicin sensitivity, which may be induced by EMT mechanically | [104] | |
| GC | Oxaliplatin | circ 0008253 | Up-regulated | Probably promote oxaliplatin resistance by up-regulating ABCG2 levels | [180] | |
| EOC | Cisplatin | miR-223 | Up-regulated | Activate PI3K/AKT signaling pathway by down-regulating PTEN to promote cisplatin resistance under hypoxia | [103] | |
| EOC | Cisplatin | miR-221-3p | Up-regulated | Activate AKT signaling pathway by down-regulating ADAMTS6 to promote EOC cell proliferation, adhesion, migration, and multidrug resistance | [181] | |
| PDAC | Gemcitabine | miR-365 | Up-regulated | Up-regulate the triphospho-nucleotide pool and induce the enzyme cytidine deaminase to inactivate gemcitabine | [182] | |
| GBM | Temozolomide | miR-21 | Up-regulated | Activate STAT3/AKT signaling pathway by targeting and down-regulating PDCD4 to promote temozolomide resistance | [106] | |
| LC | Cisplatin | miR-3679-5p | Up-regulated | Suppress NEDD4L-mediated c-Myc ubiquitination to increase aerobic glycolysis and promote cisplatin resistance | [183] | |
| Radiotherapy | EC | N/A | Has_circ_0001610 | Up-regulated | Cyclin B1 levels that are up-regulated by miR-139-5p prevent EC cells from arresting at the G2/M checkpoint thus decreasing the radiosensitivity | [184] |
| LC | N/A | lncRNA AGAP2-AS1 | Up-regulated | Weaken the radiosensitivity through down-regulating miR-296 and upregulating NOTCH2 | [185] | |
| Targeted therapy | NSCLC | Osimertinib | lncRNA MSTRG.292666.16 | Up-regulated | Down-regulate miR-6836-5p and activate MAPK pathway to promote osimertinib resistance | [186] |
| NSCLC | Gefitinib | N/A | N/A | Promote gefitinib resistance through the aberrant activation of the AKT, ERK1/2, and STAT3 pathways | [187] | |
| Immunotherapy | GC/CRC | Anti-PD-1 antibody | ApoE | Up-regulated | Down-regulating MHC-I expression on the cancer cells surface by suppressing BiP | [188] |
| TC | Anti-PD-1 antibody | miR-21-5p | Up-regulated | Down-regulate METTL3 and trigger the demethylation and stabilization of CD70 mRNA, which promotes Tregs infiltration and induces CD8+ T cells exhaustion | [189] | |
| Ferroptosis-based therapy | CC | Erastin | miRNA-660-5p | Up-regulated | Target and inhibit the expression of ALOX15 to suppress erastin-induced ferroptosis | [190] |
GC gastric cancer, EOC epithelial ovarian cancer, PDAC Pancreatic ductal adenocarcinoma, GBM glioblastoma, LC lung cancer, EC endometrial cancer, NSCLC non-small cell lung cancer, CRC colorectal cancer, TC thyroid cancer, CC cervical cancer, PI3K Phosphatidylinositol-3-kinas, PTEN phosphatase and tensin homolog, FBXW7 F-box and WD repeat domain-containing 7, EMT epithelial-to-mesenchymal transition, CYLD cylindromatosis, NEDD4 neuronally expressed developmentally downregulated 4, ABCG2 ATP binding cassette subfamily G member 2, ADAMTS6 a disintegrin and metalloproteinase with thrombospondin motifs 6, STAT3 signal transducer and activator of transcription 3, PDCD4 programmed cell death protein 4, c-Myc cellular-myelocytomatosis viral oncogene, NOTCH2 notch homologous protein 2, MAPK mitogen-activated protein kinase, ERK extracellular regulated protein kinases, ALOX15 arachidonic acid 15-lipoxygenase
Chemotherapy
The most well-studied chemoresistance induced by TAM-derived exosomes is the cisplatin resistance regulated by the PI3K/AKT pathway. The aberrant activation of PI3K/AKT is prevalent in various cancer types, contributing to a range of pro-tumorigenic activities, such as uncontrolled proliferation, survival, and resistance to cancer therapy, depending on the specific downstream molecules of AKT, such as glycogen synthase kinase 3 (GSK3) and mammalian target of rapamycin (mTOR). As an essential upstream negative regulator of the PI3K/AKT pathway, phosphatase and tensin homolog (PTEN) dephosphorylates PI3P and turn it back to PI2P, which antagonizes PI3K-mediated PI2P phosphorylation and thus terminates PI3K signaling [191]. After taken up by GC cells and EOC cells, miR-21, LncRNA CRNDE, and miR-223 within TAM-derived exosomes cause downregulation of PTEN levels and subsequent hyperactivation of PI3K/AKT pathway, leading to cisplatin-resistance in cancer cells [103, 105, 179]. In addition, increased miR-21 levels in GC cells upregulate the expression of B-cell lymphoma-2 (Bcl-2), a decisive anti-apoptotic protein [105]. Evasion from apoptosis also contributes to resistance to treatment in cancer cells [192]. Additionally, it is verified that CD163+ TAM-derived exosomal miR-221-3p in ovarian cancer ascites decrease the level of a disintegrin and metalloproteinase with thrombospondin motifs 6 (ADAMTS6) expression in the peritoneal metastatic sites in EOC patients. Downregulation of ADAMTS6 also increases the cisplatin resistance of EOC cells, probably resulting from the EMT induced by the activation of the EGFR/TGF-β/AKT pathway [181].
The neuronally expressed developmentally downregulated 4 (NEDD4) family is a group of E3 ubiquitin (Ub) ligases that play an integral role in various ubiquitination-mediated pro-tumorigenic activities, including the chemoresistance regulated by TAM-derived exosomes [193]. In GC, the previously mentioned LncRNA CRNDE facilitates NEDD4-1-mediated ubiquitination and subsequent degradation of PTEN, resulting in the activation of the PTEN/PI3K/AKT pathway and resistance to cisplatin [179]. Furthermore, miR-3679-5p found in M2 macrophage-derived exosomes maintains the stability of cellular-myelocytomatosis viral oncogene (c-Myc) and promotes aerobic glycolysis in lung adenocarcinoma. The effect is achieved by limiting NEDD4L expression and preventing NEDD4L-mediated ubiquitination of c-Myc. The increased aerobic glycolysis, in turn, reinforces the resistance to apoptosis and cisplatin in lung adenocarcinoma cells [183].
Radiotherapy
In addition, TAM-derived exosomes play a role in reducing the radiosensitivity of cancer cells. Hsa_circ_0001610 transmitted from TAMs to endometrial cancer (EC) cells through exosomes directly targets and suppresses miR-139-5p, thereby upregulating cyclin B1 levels [184]. Overexpressed cyclin B1 prevents EC cells from arresting at the G2/M checkpoint of the cell cycle and avoids G2/M arrest-induced cell death, thus decreasing the radiosensitivity of EC cells [194]. Another study verifies that lncRNA AGAP2 antisense RNA 1 (AGAP2-AS1) enhances the radioresistance of lung cancer through downregulating miR-296 and upregulating notch homologous protein 2 (NOTCH2). This radioresistance can be mediated by the overexpression AGAP2-AS1 in M2 macrophage-derived exosomes, suggesting that M2-like TAM may be implicated in weakening the radiosensitivity of lung cancer in this way [185].
Targeted therapy
Targeted therapy uses antibodies and small molecules to target the molecular drivers of cancer, such as osimertinib and gefitinib targeting the EGFR, a common mutation in non-small cell lung cancer (NSCLC) [195]. While effective, therapy involving epidermal growth factor receptor tyrosine kinase inhibitors (EGFR-TKIs) faces the challenges of drug resistance [196]. Some known mechanisms of these issues are associated with TAM-derived exosomes [186, 187]. For example, As a third-generation EGFR-TKI, osimertinib is frequently invoked to overcome the acquired resistance induced by first-generation EGFR-TKIs, such as through targeting the acquired T790M resistance mutation [196]. However, researchers have identified that the sensitivity to osimertinib in NSCLC can be decreased by lncRNA MSTRG.292666.16 from TAM-derived exosomes in NSCLC via downregulating miR-6836-5p and activating mitogen-activated protein kinase (MAPK) pathway [186]. Moreover, TAM-derived exosomes have been demonstrated to reduce the efficacy of gefitinib in NSCLC through the aberrant activation of the AKT, extracellular signal-regulated protein kinases 1 and 2 (ERK1/2), and STAT3 pathways [187]. However, the specific mediator within exosomes is still under-discovered.
Immunotherapy
Exosomes serve as key mediators employed by M2-like TAM to inhibit anti-tumor immunity and decrease sensitivity to immunotherapy. For instance, apolipoprotein E (ApoE) within exosomes derived from M2 macrophages has been identified as a contributor to immune checkpoint blockade (ICB) resistance. This occurs through its interaction with a crucial ER chaperone called binding immunoglobulin protein (BiP). The interaction between ApoE and BiP hinders BiP’s function in repairing and loading MHC-I, consequently downregulating MHC-I expression on the cancer cell surface. MHC-I downregulation diminishes the immunogenicity of cancer cells and leads to their escape from the recognition and attack of CD8+ T cells, resulting in weakening the efficacy of anti-PD-1 antibodies. Additionally, the finding that joint use of ApoE ligand and anti-PD-1 antibody ameliorates ApoE-induced anti-PD-1 treatment resistance makes the point that exosomal ApoE can be regarded as a promising target to reverse anti-PD-1 treatment resistance [188].
Ferroptosis-based therapy
Advances in ferroptosis, a regulated cell death induced by iron-dependent lipid peroxides accumulation, have made targeting ferroptosis a potential modality for cancer therapy [197]. In a mouse model of cervical cancer, ferroptosis inducers, such as erastin and RSL3, have exerted tumor-restraining activity; nevertheless, this effect can be suppressed by TAMs. Specifically, TAM-derived exosomal miRNA-660-5p is transferred to cervical cancer cells, where it targets and inhibits the expression of arachidonic acid 15-lipoxygenase (ALOX15) to suppress erastin-induced ferroptosis. Moreover, ALOX15 reduction has also been confirmed to be associated with shorter survival times in cervical cancer patients [190].
Conclusion and future outlook
Exosomes with distinct cell sources and biogenesis processes exhibit heterogenetic features and functions, contributing to the complexity of intercellular communication networks between the components in cancers. This complexity is partly reflected in the tumor-restraining or pro-tumorigenic tendencies of exosomes from macrophages. To be specific, TAM-derived exosomes that are educated by the context of cancers play a crucial role in tumor progression, metastasis, and drug resistance by exerting a direct effect on tumor cells as well as indirectly influencing the fate of the tumor via remodeling the TME. In contrast, exosomes derived from externally generated and modified macrophages, particularly the modified M1-exos, have demonstrated promising as a novel modality for cancer therapy in preclinical studies. The natural advantages of M1-exos and the acquired modification endow the combination of M1-exos-based strategies and existing cancer therapies with distinct benefits. M1-exos inherently enhance anti-cancer immunity and target the cancer cells, even crossing the BBB. In the meanwhile, M1-exos are modified to load therapeutic molecules and target the characteristics of specific cancer therapy, aiming to improve the efficacy of various cancer therapies and reduce side effects.
Although preclinical studies have opened the door to therapeutically harnessing macrophage-derived exosomes, whether these modified exosome-based strategies can achieve the anticipated therapeutic efficacy requires additional clinical trials for validation. Additionally, the technical challenges encountered in large-scale production are shared obstacles in the field of exosome application. The regulation of specific molecules in the biogenesis of exosomes may help [43]. Moreover, the stability and safety of these modified exosomes also need further experiments to validate. There is an urge to tackle the above issues and continue exploring more favorable anti-tumor mechanisms based on macrophage-derived exosomes, propelling the development of these modified exosomes. Furthermore, some emerging techniques, such as CRISPR/Cas9, have proven effective in other types of exosome-based cancer therapy, suggesting future research may explore the application of these promising modifications in macrophage-derived exosomes [198]. Modified macrophage-derived exosomes have the potential to deliver CRISPR/Cas9 to target cells steadily, which helps to overcome the off-target effects. These endeavors may boost the efficacy of current cancer therapies and establish a highly flexible treatment strategy, ultimately improving the clinical prognosis for cancer patients.
Considering the heterogeneity of macrophages and exosomes, the research of TAM-derived exosomes still faces unsolved issues. Current insights derived from the model of CXCL9:SPP1 polarity and single-cell RNA sequencing techniques reveal the limitation of the classical M1/M2 paradigm. However, many studies regard the M2 macrophages that are induced in vitro and subsequently co-cultured with cancer cells as TAM-derived exosomes, probably owing to the difficulties in isolating TAM-derived exosomes from cancer tissues. This approach fails to replicate the intricacies of TME and incorporate the influence of macrophage heterogeneity. Yet, as potential biomarkers and targets in cancer, TAM-derived exosomes may deserve further investigation with more precise models.
Acknowledgements
Not applicable.
Abbreviations
- ADAMTS6
A disintegrin and metalloproteinase with thrombospondin motifs 6
- ALIX
Apoptosis-linked gene 2-interacting protein X
- ALOX15
Arachidonic acid 15-lipoxygenase
- ApoE
Apolipoprotein E
- Arl8b
Rab7-to-Arf-like GTPase 8
- AS
Atherosclerosis
- BBB
Blood–brain barrier
- Bcl-2
B-cell lymphoma-2
- BiP
Binding immunoglobulin protein
- BMDM
Bone marrow-derived macrophage
- BORC
BLOC one-related complex
- C15orf41
Chromosome 15 open reading frame 41
- CCA
Cholangiocarcinoma
- ccRCC
Clear-cell renal cell carcinoma
- CDKN1B
Cyclin-dependent kinase inhibitor 1B
- cGAS
Cyclic guanosine monophosphate-adenosine monophosphate synthase
- circRNA
Circular RNA
- c-Met
Cellular-mesenchymal-epithelial transition factor
- c-Myc
Cellular-myelocytomatosis viral oncogene
- CRC
Colorectal cancer
- CTC
Circulating tumor cell
- CTLA-4
Cytotoxic T lymphocyte associate protein-4
- CXCL9
CXC chemokine ligand 9
- DFX
Deferasirox
- DOX
Doxorubicin
- DTX
Docetaxel
- E2F2
E2F transcription factor 2
- EC
Endometrial cancer
- ECM
Extracellular matrix
- EGFR
Epidermal growth factor receptor
- EGFR-TKI
Epidermal growth factor receptor tyrosine kinase inhibitor
- ELNV
Exosome-like nanovesicle
- EMT
Epithelial-mesenchymal transition
- EOC
Epithelial ovarian cancer
- ER
Endoplasmic reticulum
- ErbB2
Erythroblastic leukemia viral oncogene homolog 2
- ERK1/2
Extracellular signal-regulated protein kinases 1 and 2
- ESCRT
Endosomal sorting complex required for transport
- EV
Extracellular vesicle
- GBM
Glioblastoma
- GC
Gastric cancer
- GDF15
Growth differentiation factor 15
- GEM
Gemcitabine
- GGA1
Golgi associated, gamma adaptin ear containing, ARF binding protein 1
- GPRC5B
G protein-coupled receptor class C group 5 member B
- GSK3
Glycogen synthase kinase 3
- HCC
Hepatocellular carcinoma
- HD-PTP
His domain protein tyrosine phosphatase
- HIF
Hypoxia-inducible factor
- HOPS
Homotypic fusion and protein-sorting
- HOTAIR
HOX Transcript Antisense RNA
- Hp
Helicobacter pylori
- HuR
Human antigen R
- ICAM-1
Intercellular adhesion molecule 1
- ICB
Immune checkpoint blockade
- ICG
Indocyanine green
- IFN-γ
Interferon-γ
- IGF1R
Insulin-like growth factor 1
- ILV
Intraluminal vesicle
- iNOS
Inducible nitric oxide synthase
- IR
Ionizing radiation
- IRF1
Interferon regulatory factor 1
- LBPA
Lysobisphosphatidic acid
- let-7a
Lethal-7a
- LFA-1
Lymphocyte function-associated antigen 1
- LMAN2
Lectin, mannose binding 2
- lncRNA
Long non-coding RNA
- LPS
Lipopolysaccharide
- M1-exo
M1-macrophage-derived exosome
- MAPK
Mitogen-activated protein kinase
- miRNA
MicroRNA
- mTOR
Mammalian target of rapamycin
- MVB
Multivesicular body
- NBR1
Neighbor of breast cancer 1 gene
- ncRNA
Non-coding RNA
- NEDD4
Neuronally expressed developmentally downregulated 4
- NF-κB
Nuclear factor-kappa B
- NO
Nitric oxide
- NOTCH2
Notch homologous protein 2
- NSCLC
Non-small cell lung cancer
- ORP1L
Oxysterol-binding protein-related protein 1L
- OS
Osteosarcoma
- OSCC
Oral squamous cell carcinoma
- PD-1
Programmed cell death protein 1
- PDA
Polydopamine
- PDAC
Pancreatic ductal adenocarcinoma
- PD-L1
Programmed death-ligand 1
- PDT
Photodynamic therapy
- PHD2
Prolyl hydroxylase domain 2
- PTEN
Phosphatase and tensin homolog
- PTT
Photothermal therapy
- RBP
RNA-binding protein
- RCC
Renal cell carcinoma
- RILP
Rab7-interacting lysosomal protein
- RNS
Reactive nitrogen species
- ROS
Reactive oxygen species
- RRM2
Ribonucleotide reductase M2
- SCC
Squamous cell carcinoma
- SDT
Sonodynamic therapy
- SIRPα
Signal regulatory protein α
- SKIP
SifA- and kinesin-interacting protein
- Slp4
Synaptotagmin-like 4 = SYTL4
- SNARE
Soluble N-ethylmaleimide-sensitive fusion attachment protein receptor
- SOCS3
Suppressor of cytokine signaling 3
- SPP1
Secreted phosphoprotein 1
- STAT1
Signal transducer and activator of transcription 1
- STAT3
Signal transducer and activator of transcription 3
- STING
Stimulator of interferon gene
- TAM
Tumor-associated macrophage
- TDE
Tumor-derived exosome
- TGF-β1
Transforming growth factor-β1
- TGN
Trans Golgi network
- Th1
T helper 1
- TIMP2
Tissue inhibitor of metal protease 2
- TME
Tumor microenvironment
- TNBC
Triple-negative breast cancer
- TNF-α
Tumor necrosis factor-α
- Treg
Regulatory T
- TRM
Tissue-resident macrophage
- Ub
Ubiquitin
- VPS4
Vacuolar protein sorting 4
- YBX1
Y-box binding protein 1
- YY1
Yin Yang 1
Author contributions
ZQL and YQR provided direction and guidance throughout the preparation of this manuscript. SYZ, LL, RZW and YQR wrote and edited the manuscript. LL and YQR reviewed and made significant revisions to the manuscript. XWH, and ZQL revised and edited the manuscript. YHB, HX, SYW, YYZ, ANZ, STL, PL, QC, and ZKZ collected and prepared the related papers. All authors read and approved the final manuscript.
Funding
This study was supported by the Major Science and Technology projects of Henan Province (Grant No. 221100310100).
Availability of data and materials
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Long Liu, Siying Zhang, Yuqing Ren and Ruizhi Wang contributed equally and are co–first authors.
Contributor Information
Zaoqu Liu, Email: liuzaoqu@163.com.
Xinwei Han, Email: fcchanxw@zzu.edu.cn.
References
- 1.Kalluri R, McAndrews KM. The role of extracellular vesicles in cancer. Cell. 2023;186(8):1610–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kalluri R, LeBleu VS. The biology, function, and biomedical applications of exosomes. Science. 2020;367(6478):eaau6977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arya SB, Collie SP, Parent CA. The ins-and-outs of exosome biogenesis, secretion, and internalization. Trends Cell Biol. 2023;S0962–8924(23):00129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cheng L, Hill AF. Therapeutically harnessing extracellular vesicles. Nat Rev Drug Discovery. 2022;21(5):379–99. [DOI] [PubMed] [Google Scholar]
- 5.Christofides A, Strauss L, Yeo A, Cao C, Charest A, Boussiotis VA. The complex role of tumor-infiltrating macrophages. Nat Immunol. 2022;23(8):1148–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kloosterman DJ, Akkari L. Macrophages at the interface of the co-evolving cancer ecosystem. Cell. 2023;186(8):1627–51. [DOI] [PubMed] [Google Scholar]
- 7.Mantovani A, Allavena P, Marchesi F, Garlanda C. Macrophages as tools and targets in cancer therapy. Nat Rev Drug Discovery. 2022;21(11):799–820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cassetta L, Pollard JW. A timeline of tumour-associated macrophage biology. Nat Rev Cancer. 2023;23(4):238–57. [DOI] [PubMed] [Google Scholar]
- 9.Pittet MJ, Michielin O, Migliorini D. Clinical relevance of tumour-associated macrophages. Nat Rev Clin Oncol. 2022;19(6):402–21. [DOI] [PubMed] [Google Scholar]
- 10.Zhou M, He X, Mei C, Ou C. Exosome derived from tumor-associated macrophages: biogenesis, functions, and therapeutic implications in human cancers. Biomarker Res. 2023;11(1):100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang P, Wang H, Huang Q, Peng C, Yao L, Chen H, et al. Exosomes from m1-polarized macrophages enhance paclitaxel antitumor activity by activating macrophages-mediated inflammation. Theranostics. 2019;9(6):1714–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li Z, Suo B, Long G, Gao Y, Song J, Zhang M, et al. Exosomal miRNA-16-5p derived from M1 macrophages enhances T cell-dependent immune response by regulating PD-L1 in gastric cancer. Front Cell Dev Biol. 2020;8: 572689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim H, Park H-J, Chang HW, Back JH, Lee SJ, Park YE, et al. Exosome-guided direct reprogramming of tumor-associated macrophages from protumorigenic to antitumorigenic to fight cancer. Bioactive Mater. 2023;25:527–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu T, Liu Y, Cao Y, Liu Z. Engineering macrophage exosome disguised biodegradable nanoplatform for enhanced sonodynamic therapy of glioblastoma. Adv Mater (Deerfield Beach, Fla). 2022;34(15): e2110364. [DOI] [PubMed] [Google Scholar]
- 15.Ma X, Yao M, Gao Y, Yue Y, Li Y, Zhang T, et al. Functional immune cell-derived exosomes engineered for the trilogy of radiotherapy sensitization. Adv Sci. 2022;9(23):e2106031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cheng L, Zhang P, Liu Y, Liu Z, Tang J, Xu L, et al. Multifunctional hybrid exosomes enhanced cancer chemo-immunotherapy by activating the STING pathway. Biomaterials. 2023;301: 122259. [DOI] [PubMed] [Google Scholar]
- 17.Wei H, Chen Q, Lin L, Sha C, Li T, Liu Y, et al. Regulation of exosome production and cargo sorting. Int J Biol Sci. 2021;17(1):163–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arya SB, Chen S, Jordan-Javed F, Parent CA. Ceramide-rich microdomains facilitate nuclear envelope budding for non-conventional exosome formation. Nat Cell Biol. 2022;24(7):1019–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lau NCH, Yam JWP. From exosome biogenesis to absorption: key takeaways for cancer research. Cancers. 2023;15(7):1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Parton RG, McMahon K-A, Wu Y. Caveolae: formation, dynamics, and function. Curr Opin Cell Biol. 2020;65:8–16. [DOI] [PubMed] [Google Scholar]
- 21.Kaksonen M, Roux A. Mechanisms of clathrin-mediated endocytosis. Nat Rev Mol Cell Biol. 2018;19(5):313–26. [DOI] [PubMed] [Google Scholar]
- 22.Krylova SV, Feng D. The machinery of exosomes: biogenesis, release, and uptake. Int J Mol Sci. 2023;24(2):1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vietri M, Radulovic M, Stenmark H. The many functions of ESCRTs. Nat Rev Mol Cell Biol. 2020;21(1):25–42. [DOI] [PubMed] [Google Scholar]
- 24.Huebner AR, Cheng L, Somparn P, Knepper MA, Fenton RA, Pisitkun T. Deubiquitylation of protein cargo is not an essential step in exosome formation. Mol Cell Proteomics MCP. 2016;15(5):1556–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baietti MF, Zhang Z, Mortier E, Melchior A, Degeest G, Geeraerts A, et al. Syndecan-syntenin-ALIX regulates the biogenesis of exosomes. Nat Cell Biol. 2012;14(7):677–85. [DOI] [PubMed] [Google Scholar]
- 26.Han Q-F, Li W-J, Hu K-S, Gao J, Zhai W-L, Yang J-H, et al. Exosome biogenesis: machinery, regulation, and therapeutic implications in cancer. Mol Cancer. 2022;21(1):207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wei D, Zhan W, Gao Y, Huang L, Gong R, Wang W, et al. RAB31 marks and controls an ESCRT-independent exosome pathway. Cell Res. 2021;31(2):157–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li C, Ni Y-Q, Xu H, Xiang Q-Y, Zhao Y, Zhan J-K, et al. Roles and mechanisms of exosomal non-coding RNAs in human health and diseases. Signal Transduct Target Ther. 2021;6(1):383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mori MA, Ludwig RG, Garcia-Martin R, Brandão BB, Kahn CR. Extracellular miRNAs: from biomarkers to mediators of physiology and disease. Cell Metab. 2019;30(4):656–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang Y, Liu J, Ma J, Sun T, Zhou Q, Wang W, et al. Exosomal circRNAs: biogenesis, effect and application in human diseases. Mol Cancer. 2019;18(1):116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ma L, Singh J, Schekman R. Two RNA-binding proteins mediate the sorting of miR223 from mitochondria into exosomes. Elife. 2023;12:e85878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhou J, Li L, Han Y, Ge G, Ji Q, Li H. RNA binding protein RALY facilitates colorectal cancer metastasis via enhancing exosome biogenesis in m6A dependent manner. Int J Biol Macromol. 2024;273(Pt 2): 133112. [DOI] [PubMed] [Google Scholar]
- 33.Larios J, Mercier V, Roux A, Gruenberg J. ALIX- and ESCRT-III-dependent sorting of tetraspanins to exosomes. J Cell Biol. 2020;219(3): e201904113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yokoi A, Villar-Prados A, Oliphint PA, Zhang J, Song X, De Hoff P, et al. Mechanisms of nuclear content loading to exosomes. Sci Adv. 2019;5(11):eaax8849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kwon S-H, Oh S, Nacke M, Mostov KE, Lipschutz JH. Adaptor protein CD2AP and L-type Lectin LMAN2 regulate exosome cargo protein trafficking through the Golgi complex. J Biol Chem. 2016;291(49):25462–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kerr N, García-Contreras M, Abbassi S, Mejias NH, Desousa BR, Ricordi C, et al. Inflammasome proteins in serum and serum-derived extracellular vesicles as biomarkers of stroke. Front Mol Neurosci. 2018;11: 397886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kerr NA, de Rivero Vaccari JP, Umland O, Bullock MR, Conner GE, Dietrich WD, et al. Human lung cell pyroptosis following traumatic brain injury. Cells. 2019;8(1):69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Neupane KR, Aryal SP, Harvey BT, Ramon GS, Chun B, McCorkle JR, et al. Organelle specific macrophage engineered vesicles differentially reprogram macrophage polarization. Adv Healthcare Mater. 2024;13(30): e2401906. [DOI] [PubMed] [Google Scholar]
- 39.Stenmark H. Rab GTPases as coordinators of vesicle traffic. Nat Rev Mol Cell Biol. 2009;10(8):513–25. [DOI] [PubMed] [Google Scholar]
- 40.Jongsma ML, Bakker J, Cabukusta B, Liv N, van Elsland D, Fermie J, et al. SKIP-HOPS recruits TBC1D15 for a Rab7-to-Arl8b identity switch to control late endosome transport. EMBO J. 2020;39(6): e102301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schleinitz A, Pöttgen L-A, Keren-Kaplan T, Pu J, Saftig P, Bonifacino JS, et al. Consecutive functions of small GTPases guide HOPS-mediated tethering of late endosomes and lysosomes. Cell Rep. 2023;42(1): 111969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Johansson M, Rocha N, Zwart W, Jordens I, Janssen L, Kuijl C, et al. Activation of endosomal dynein motors by stepwise assembly of Rab7-RILP-p150Glued, ORP1L, and the receptor betalll spectrin. J Cell Biol. 2007;176(4):459–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shelke GV, Williamson CD, Jarnik M, Bonifacino JS. Inhibition of endolysosome fusion increases exosome secretion. J Cell Biol. 2023;222(6): e202209084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Alnaas AA, Watson-Siriboe A, Tran S, Negussie M, Henderson JA, Osterberg JR, et al. Multivalent lipid targeting by the calcium-independent C2A domain of synaptotagmin-like protein 4/granuphilin. J Biol Chem. 2021;296: 100159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yang L, Peng X, Li Y, Zhang X, Ma Y, Wu C, et al. Long non-coding RNA HOTAIR promotes exosome secretion by regulating RAB35 and SNAP23 in hepatocellular carcinoma. Mol Cancer. 2019;18(1):78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Xu M, Ji J, Jin D, Wu Y, Wu T, Lin R, et al. The biogenesis and secretion of exosomes and multivesicular bodies (MVBs): intercellular shuttles and implications in human diseases. Genes Dis. 2023;10(5):1894–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jahn R, Cafiso DC, Tamm LK. Mechanisms of SNARE proteins in membrane fusion. Nat Rev Mol Cell Biol. 2024;25(2):101–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhang Y, Hughson FM. Chaperoning SNARE folding and assembly. Annu Rev Biochem. 2021;90:581–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Liu C, Liu D, Wang S, Gan L, Yang X, Ma C. Identification of the SNARE complex that mediates the fusion of multivesicular bodies with the plasma membrane in exosome secretion. J Extracell Vesicles. 2023;12(9): e12356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hessvik NP, Sagini K, Romero S, Ramirez-Garrastacho M, Rodriguez M, Tutturen AEV, et al. siRNA screening reveals that SNAP29 contributes to exosome release. Cell Mol Life Sci CMLS. 2023;80(7):177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Viršilė A, Samuolienė G, Laužikė K, Šipailaitė E, Balion Z, Jekabsone A. Species-specific plant-derived nanoparticle characteristics. Plants (Basel). 2022;11(22):3139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Noren Hooten N, Byappanahalli AM, Vannoy M, Omoniyi V, Evans MK. Influences of age, race, and sex on extracellular vesicle characteristics. Theranostics. 2022;12(9):4459–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Orrù V, Virdis F, Marongiu M, Serra V, Schlessinger D, Devoto M, et al. Effect of genetic factors, age and sex on levels of circulating extracellular vesicles and platelets. Int J Mol Sci. 2023;24(8):7183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhang L, Xia X, Wu H, Liu X, Zhu Q, Wang M, et al. Helicobacter pylori infection selectively attenuates endothelial function in male mice via exosomes-mediated ROS production. Front Cell Infect Microbiol. 2023;13:1142387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Xhuti D, Nilsson MI, Manta K, Tarnopolsky MA, Nederveen JP. Circulating exosome-like vesicle and skeletal muscle microRNAs are altered with age and resistance training. J Physiol. 2023. [DOI] [PubMed]
- 56.Liu J, Yoo J, Ho JY, Jung Y, Lee S, Hur SY, et al. Plasma-derived exosomal miR-4732-5p is a promising noninvasive diagnostic biomarker for epithelial ovarian cancer. J Ovarian Res. 2021;14(1):59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wang J, Guo W, Wang X, Tang X, Sun X, Ren T. Circulating exosomal PD-L1 at initial diagnosis predicts outcome and survival of patients with osteosarcoma. Clin Cancer Res. 2023;29(3):659–66. [DOI] [PubMed] [Google Scholar]
- 58.Yu D, Li Y, Wang M, Gu J, Xu W, Cai H, et al. Exosomes as a new frontier of cancer liquid biopsy. Mol Cancer. 2022;21(1):56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Chen J, Lin Z, Liu L, Zhang R, Geng Y, Fan M, et al. GOLM1 exacerbates CD8+ T cell suppression in hepatocellular carcinoma by promoting exosomal PD-L1 transport into tumor-associated macrophages. Signal Transduct Target Ther. 2021;6(1):397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Qiu Y, Yang Y, Yang R, Liu C, Hsu J-M, Jiang Z, et al. Activated T cell-derived exosomal PD-1 attenuates PD-L1-induced immune dysfunction in triple-negative breast cancer. Oncogene. 2021;40(31):4992–5001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hoshino A, Costa-Silva B, Shen T-L, Rodrigues G, Hashimoto A, Tesic Mark M, et al. Tumour exosome integrins determine organotropic metastasis. Nature. 2015;527(7578):329–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Xu G, Xu S, Shi X, Shen C, Zhang D, Zhang T, et al. Foot-and-mouth disease virus degrades Rab27a to suppress the exosome-mediated antiviral immune response. Vet Microbiol. 2020;251:108889. [DOI] [PubMed] [Google Scholar]
- 63.Shimizu A, Sawada K, Kobayashi M, Yamamoto M, Yagi T, Kinose Y, et al. Exosomal CD47 plays an essential role in immune evasion in ovarian cancer. Mol Cancer Res MCR. 2021;19(9):1583. [DOI] [PubMed] [Google Scholar]
- 64.Ma X, Zhao J, Li S, Wang Y, Liu J, Shi Y, et al. Rab27a-dependent exosomes protect against cerebral ischemic injury by reducing endothelial oxidative stress and apoptosis. CNS Neurosci Ther. 2022;28(10):1596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Park MD, Silvin A, Ginhoux F, Merad M. Macrophages in health and disease. Cell. 2022;185(23):4259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wculek SK, Dunphy G, Heras-Murillo I, Mastrangelo A, Sancho D. Metabolism of tissue macrophages in homeostasis and pathology. Cell Mol Immunol. 2022;19(3):384–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chen S, Saeed AFUH, Liu Q, Jiang Q, Xu H, Xiao GG, et al. Macrophages in immunoregulation and therapeutics. Signal Transduct Target Ther. 2023;8(1):207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mills CD, Kincaid K, Alt JM, Heilman MJ, Hill AM. M-1/M-2 macrophages and the Th1/Th2 paradigm. J Immunol. 2000;164(12):6166–73. [DOI] [PubMed] [Google Scholar]
- 69.Strizova Z, Benesova I, Bartolini R, Novysedlak R, Cecrdlova E, Foley LK, et al. M1/M2 macrophages and their overlaps - myth or reality? Clin Sci. 2023;137(15):1067–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Cho U, Kim B, Kim S, Han Y, Song YS. Pro-inflammatory M1 macrophage enhances metastatic potential of ovarian cancer cells through NF-κB activation. Mol Carcinog. 2018;57(2):235–42. [DOI] [PubMed] [Google Scholar]
- 71.Lv C, Li S, Zhao J, Yang P, Yang C. M1 macrophages enhance survival and invasion of oral squamous cell carcinoma by inducing GDF15-mediated ErbB2 phosphorylation. ACS Omega. 2022;7(13):11405–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.You Y, Tian Z, Du Z, Wu K, Xu G, Dai M, et al. M1-like tumor-associated macrophages cascade a mesenchymal/stem-like phenotype of oral squamous cell carcinoma via the IL6/stat3/THBS1 feedback loop. J Exp Clin Cancer Res. 2022;41(1):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chen S, Lu K, Hou Y, You Z, Shu C, Wei X, et al. YY1 complex in M2 macrophage promotes prostate cancer progression by upregulating IL-6. J Immunother Cancer. 2023;11(4): e006020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Azizi E, Carr AJ, Plitas G, Cornish AE, Konopacki C, Prabhakaran S, et al. Single-cell map of diverse immune phenotypes in the breast tumor microenvironment. Cell. 2018;174(5):1293-308.e36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Müller S, Kohanbash G, Liu SJ, Alvarado B, Carrera D, Bhaduri A, et al. Single-cell profiling of human gliomas reveals macrophage ontogeny as a basis for regional differences in macrophage activation in the tumor microenvironment. Genome Biol. 2017;18(1):234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Zhu C, Preissl S, Ren B. Single-cell multimodal omics: the power of many. Nat Methods. 2020;17(1):11–4. [DOI] [PubMed] [Google Scholar]
- 77.Wu SZ, Al-Eryani G, Roden DL, Junankar S, Harvey K, Andersson A, et al. A single-cell and spatially resolved atlas of human breast cancers. Nat Genet. 2021;53(9):1334–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Nalio Ramos R, Missolo-Koussou Y, Gerber-Ferder Y, Bromley CP, Bugatti M, Núñez NG, et al. Tissue-resident FOLR2+ macrophages associate with CD8+ T cell infiltration in human breast cancer. Cell. 2022;185(7):1189-207.e25. [DOI] [PubMed] [Google Scholar]
- 79.Timperi E, Gueguen P, Molgora M, Magagna I, Kieffer Y, Lopez-Lastra S, et al. Lipid-associated macrophages are induced by cancer-associated fibroblasts and mediate immune suppression in breast cancer. Can Res. 2022;82(18):3291–306. [DOI] [PubMed] [Google Scholar]
- 80.Qi J, Sun H, Zhang Y, Wang Z, Xun Z, Li Z, et al. Single-cell and spatial analysis reveal interaction of FAP+ fibroblasts and SPP1+ macrophages in colorectal cancer. Nat Commun. 2022;13(1):1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bao X, Wang D, Dai X, Liu C, Zhang H, Jin Y, et al. An immunometabolism subtyping system identifies S100A9+ macrophage as an immune therapeutic target in colorectal cancer based on multiomics analysis. Cell Rep Med. 2023;4(4): 100987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Roelands J, van der Ploeg M, Ijsselsteijn ME, Dang H, Boonstra JJ, Hardwick JCH, et al. Transcriptomic and immunophenotypic profiling reveals molecular and immunological hallmarks of colorectal cancer tumourigenesis. Gut. 2023;72(7):1326–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Bao X, Li Q, Chen D, Dai X, Liu C, Tian W, et al. A multiomics analysis-assisted deep learning model identifies a macrophage-oriented module as a potential therapeutic target in colorectal cancer. Cell Rep Med. 2024:101399. [DOI] [PMC free article] [PubMed]
- 84.Kang B, Camps J, Fan B, Jiang H, Ibrahim MM, Hu X, et al. Parallel single-cell and bulk transcriptome analyses reveal key features of the gastric tumor microenvironment. Genome Biol. 2022;23(1):265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sun K, Xu R, Ma F, Yang N, Li Y, Sun X, et al. scRNA-seq of gastric tumor shows complex intercellular interaction with an alternative T cell exhaustion trajectory. Nat Commun. 2022;13(1):4943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Chen AX, Gartrell RD, Zhao J, Upadhyayula PS, Zhao W, Yuan J, et al. Single-cell characterization of macrophages in glioblastoma reveals MARCO as a mesenchymal pro-tumor marker. Genome Med. 2021;13(1):88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Xiong A, Zhang J, Chen Y, Zhang Y, Yang F. Integrated single-cell transcriptomic analyses reveal that GPNMB-high macrophages promote PN-MES transition and impede T cell activation in GBM. EBioMedicine. 2022;83: 104239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Karimi E, Yu MW, Maritan SM, Perus LJM, Rezanejad M, Sorin M, et al. Single-cell spatial immune landscapes of primary and metastatic brain tumours. Nature. 2023;614(7948):555–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Mei Y, Wang X, Zhang J, Liu D, He J, Huang C, et al. Siglec-9 acts as an immune-checkpoint molecule on macrophages in glioblastoma, restricting T-cell priming and immunotherapy response. Nat Cancer. 2023;4(9):1273–91. [DOI] [PubMed] [Google Scholar]
- 90.Lu Y, Yang A, Quan C, Pan Y, Zhang H, Li Y, et al. A single-cell atlas of the multicellular ecosystem of primary and metastatic hepatocellular carcinoma. Nat Commun. 2022;13(1):4594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Liu Y, Xun Z, Ma K, Liang S, Li X, Zhou S, et al. Identification of a tumour immune barrier in the HCC microenvironment that determines the efficacy of immunotherapy. J Hepatol. 2023;78(4):770–82. [DOI] [PubMed] [Google Scholar]
- 92.Cappuyns S, Philips G, Vandecaveye V, Boeckx B, Schepers R, Van Brussel T, et al. PD-1- CD45RA+ effector-memory CD8 T cells and CXCL10+ macrophages are associated with response to atezolizumab plus bevacizumab in advanced hepatocellular carcinoma. Nat Commun. 2023;14(1):7825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Weng J, Liu S, Zhou Q, Xu W, Xu M, Gao D, et al. Intratumoral PPT1-positive macrophages determine immunosuppressive contexture and immunotherapy response in hepatocellular carcinoma. J Immunother Cancer. 2023;11(6): e006655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ke L, Rui Z, Fukai W, Yunzheng Z, Fanshuai M, Qingyu L, et al. Single-cell dissection of the multicellular ecosystem and molecular features underlying microvascular invasion in hepatocellular carcinoma. Hepatology (Baltimore, Md). 2023. [DOI] [PMC free article] [PubMed]
- 95.Chan JM, Quintanal-Villalonga Á, Gao VR, Xie Y, Allaj V, Chaudhary O, et al. Signatures of plasticity, metastasis, and immunosuppression in an atlas of human small cell lung cancer. Cancer Cell. 2021;39(11):1479-96.e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Wang C, Yu Q, Song T, Wang Z, Song L, Yang Y, et al. The heterogeneous immune landscape between lung adenocarcinoma and squamous carcinoma revealed by single-cell RNA sequencing. Signal Transduct Target Ther. 2022;7(1):289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Caronni N, La Terza F, Vittoria FM, Barbiera G, Mezzanzanica L, Cuzzola V, et al. IL-1β+ macrophages fuel pathogenic inflammation in pancreatic cancer. Nature. 2023;623(7986):415–22. [DOI] [PubMed] [Google Scholar]
- 98.Oh K, Yoo YJ, Torre-Healy LA, Rao M, Fassler D, Wang P, et al. Coordinated single-cell tumor microenvironment dynamics reinforce pancreatic cancer subtype. Nat Commun. 2023;14(1):5226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ma R-Y, Black A, Qian B-Z. Macrophage diversity in cancer revisited in the era of single-cell omics. Trends Immunol. 2022;43(7):546–63. [DOI] [PubMed] [Google Scholar]
- 100.Massalha H, Bahar Halpern K, Abu-Gazala S, Jana T, Massasa EE, Moor AE, et al. A single cell atlas of the human liver tumor microenvironment. Mol Syst Biol. 2020;16(12): e9682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Bill R, Wirapati P, Messemaker M, Roh W, Zitti B, Duval F, et al. CXCL9:SPP1 macrophage polarity identifies a network of cellular programs that control human cancers. Science (New York, NY). 2023;381(6657):515–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Yang M, Chen J, Su F, Yu B, Su F, Lin L, et al. Microvesicles secreted by macrophages shuttle invasion-potentiating microRNAs into breast cancer cells. Mol Cancer. 2011;10:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Zhu X, Shen H, Yin X, Yang M, Wei H, Chen Q, et al. Macrophages derived exosomes deliver miR-223 to epithelial ovarian cancer cells to elicit a chemoresistant phenotype. J Exp Clin Cancer Res CR. 2019;38:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Gao H, Ma J, Cheng Y, Zheng P. Exosomal transfer of macrophage-derived miR-223 confers doxorubicin resistance in gastric cancer. Onco Targets Ther. 2020;13:12169–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Zheng P, Chen L, Yuan X, Luo Q, Liu Y, Xie G, et al. Exosomal transfer of tumor-associated macrophage-derived miR-21 confers cisplatin resistance in gastric cancer cells. J Exp Clin Cancer Res CR. 2017;36(1):53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Chuang H-Y, Su Y-K, Liu H-W, Chen C-H, Chiu S-C, Cho D-Y, et al. Preclinical evidence of STAT3 inhibitor pacritinib overcoming temozolomide resistance via downregulating miR-21-enriched exosomes from M2 glioblastoma-associated macrophages. J Clin Med. 2019;8(7):959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Li X, Tang M. Exosomes released from M2 macrophages transfer miR-221-3p contributed to EOC progression through targeting CDKN1B. Cancer Med. 2020;9(16):5976–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Liu W, Long Q, Zhang W, Zeng D, Hu B, Liu S, et al. miRNA-221-3p derived from M2-polarized tumor-associated macrophage exosomes aggravates the growth and metastasis of osteosarcoma through SOCS3/JAK2/STAT3 axis. Aging. 2021;13(15):19760–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Jing X, Yang F, Shao C, Wei K, Xie M, Shen H, et al. Role of hypoxia in cancer therapy by regulating the tumor microenvironment. Mol Cancer. 2019;18(1):157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Gu W, Gong L, Wu X, Yao X. Hypoxic TAM-derived exosomal miR-155-5p promotes RCC progression through HuR-dependent IGF1R/AKT/PI3K pathway. Cell Death Discovery. 2021;7(1):147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Reinfeld BI, Madden MZ, Wolf MM, Chytil A, Bader JE, Patterson AR, et al. Cell-programmed nutrient partitioning in the tumour microenvironment. Nature. 2021;593(7858):282–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Chen F, Chen J, Yang L, Liu J, Zhang X, Zhang Y, et al. Extracellular vesicle-packaged HIF-1α-stabilizing lncRNA from tumour-associated macrophages regulates aerobic glycolysis of breast cancer cells. Nat Cell Biol. 2019;21(4):498–510. [DOI] [PubMed] [Google Scholar]
- 113.de Visser KE, Joyce JA. The evolving tumor microenvironment: from cancer initiation to metastatic outgrowth. Cancer Cell. 2023;41(3):374–403. [DOI] [PubMed] [Google Scholar]
- 114.Zhou X, Liu Q, Wang X, Yao X, Zhang B, Wu J, et al. Exosomal ncRNAs facilitate interactive ‘dialogue’ between tumor cells and tumor-associated macrophages. Cancer Lett. 2023;552: 215975. [DOI] [PubMed] [Google Scholar]
- 115.Dragomir MP, Knutsen E, Calin GA. Classical and noncanonical functions of miRNAs in cancers. Trends Genet TIG. 2022;38(4):379–94. [DOI] [PubMed] [Google Scholar]
- 116.Yan C-F, Xia J, Qun W-S, Bing W-Y, Guo W-J, Yong H-G, et al. Tumor-associated macrophages-derived exo-let-7a promotes osteosarcoma metastasis via targeting C15orf41 in osteosarcoma. Environ Toxicol. 2023;38(6):1318–31. [DOI] [PubMed] [Google Scholar]
- 117.Mattick JS, Amaral PP, Carninci P, Carpenter S, Chang HY, Chen L-L, et al. Long non-coding RNAs: definitions, functions, challenges and recommendations. Nat Rev Mol Cell Biol. 2023;24(6):430–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Li J, Wang K, Yang C, Zhu K, Jiang C, Wang M, et al. Tumor-associated macrophage-derived exosomal LINC01232 induces the immune escape in glioma by decreasing surface MHC-I expression. Adv Sci. 2023;10(17):e2207067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kristensen LS, Jakobsen T, Hager H, Kjems J. The emerging roles of circRNAs in cancer and oncology. Nat Rev Clin Oncol. 2022;19(3):188–206. [DOI] [PubMed] [Google Scholar]
- 120.Chen S, Chen Z, Li Z, Li S, Wen Z, Cao L, et al. Tumor-associated macrophages promote cholangiocarcinoma progression via exosomal Circ_0020256. Cell Death Dis. 2022;13(1):94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Chen G, Huang AC, Zhang W, Zhang G, Wu M, Xu W, et al. Exosomal PD-L1 contributes to immunosuppression and is associated with anti-PD-1 response. Nature. 2018;560(7718):382–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Zhong W, Lu Y, Han X, Yang J, Qin Z, Zhang W, et al. Upregulation of exosome secretion from tumor-associated macrophages plays a key role in the suppression of anti-tumor immunity. Cell Rep. 2023;42(10): 113224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Knochelmann HM, Dwyer CJ, Bailey SR, Amaya SM, Elston DM, Mazza-McCrann JM, et al. When worlds collide: Th17 and Treg cells in cancer and autoimmunity. Cell Mol Immunol. 2018;15(5):458–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Basu A, Ramamoorthi G, Albert G, Gallen C, Beyer A, Snyder C, et al. Differentiation and regulation of TH Cells: a balancing act for cancer immunotherapy. Front Immunol. 2021;12: 669474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Shan F, Somasundaram A, Bruno TC, Workman CJ, Vignali DAA. Therapeutic targeting of regulatory T cells in cancer. Trends in Cancer. 2022;8(11):944–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Chang SH. T helper 17 (Th17) cells and interleukin-17 (IL-17) in cancer. Arch Pharmacal Res. 2019;42(7):549–59. [DOI] [PubMed] [Google Scholar]
- 127.Kryczek I, Banerjee M, Cheng P, Vatan L, Szeliga W, Wei S, et al. Phenotype, distribution, generation, and functional and clinical relevance of Th17 cells in the human tumor environments. Blood. 2009;114(6):1141–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Zhou J, Li X, Wu X, Zhang T, Zhu Q, Wang X, et al. Exosomes released from tumor-associated macrophages transfer miRNAs that induce a Treg/Th17 cell imbalance in epithelial ovarian cancer. Cancer Immunol Res. 2018;6(12):1578–92. [DOI] [PubMed] [Google Scholar]
- 129.Xue C, Yao Q, Gu X, Shi Q, Yuan X, Chu Q, et al. Evolving cognition of the JAK-STAT signaling pathway: autoimmune disorders and cancer. Signal Transduct Target Ther. 2023;8(1):204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Shao M-M, Pei X-B, Chen Q-Y, Wang F, Wang Z, Zhai K. Macrophage-derived exosome promotes regulatory T cell differentiation in malignant pleural effusion. Front Immunol. 2023;14:1161375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Cianciaruso C, Beltraminelli T, Duval F, Nassiri S, Hamelin R, Mozes A, et al. Molecular profiling and functional analysis of macrophage-derived tumor extracellular vesicles. Cell Rep. 2019;27(10):3062-80.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.De Palma M, Biziato D, Petrova TV. Microenvironmental regulation of tumour angiogenesis. Nat Rev Cancer. 2017;17(8):457–74. [DOI] [PubMed] [Google Scholar]
- 133.Yang Y, Guo Z, Chen W, Wang X, Cao M, Han X, et al. M2 macrophage-derived exosomes promote angiogenesis and growth of pancreatic ductal adenocarcinoma by targeting E2F2. Mol Ther. 2021;29(3):1226–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Luo Q, Wang J, Zhao W, Peng Z, Liu X, Li B, et al. Vasculogenic mimicry in carcinogenesis and clinical applications. J Hematol Oncol. 2020;13(1):19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Liu Q, Zhao E, Geng B, Gao S, Yu H, He X, et al. Tumor-associated macrophage-derived exosomes transmitting miR-193a-5p promote the progression of renal cell carcinoma via TIMP2-dependent vasculogenic mimicry. Cell Death Dis. 2022;13(4):382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Zhang Y, Liu Q, Zhang X, Huang H, Tang S, Chai Y, et al. Recent advances in exosome-mediated nucleic acid delivery for cancer therapy. J Nanobiotechnol. 2022;20(1):279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Zhang M, Hu S, Liu L, Dang P, Liu Y, Sun Z, et al. Engineered exosomes from different sources for cancer-targeted therapy. Signal Transduct Target Ther. 2023;8(1):124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Yuan D, Zhao Y, Banks WA, Bullock KM, Haney M, Batrakova E, et al. Macrophage exosomes as natural nanocarriers for protein delivery to inflamed brain. Biomaterials. 2017;142:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Wang D, Qiu G, Zhu X, Wang Q, Zhu C, Fang C, et al. Macrophage-inherited exosome excise tumor immunosuppression to expedite immune-activated ferroptosis. J Immunother Cancer. 2023;11(5): e006516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Terstappen GC, Meyer AH, Bell RD, Zhang W. Strategies for delivering therapeutics across the blood-brain barrier. Nat Rev Drug Discovery. 2021;20(5):362–83. [DOI] [PubMed] [Google Scholar]
- 141.Lu Z, Zuo B, Jing R, Gao X, Rao Q, Liu Z, et al. Dendritic cell-derived exosomes elicit tumor regression in autochthonous hepatocellular carcinoma mouse models. J Hepatol. 2017;67(4):739–48. [DOI] [PubMed] [Google Scholar]
- 142.Pitt JM, André F, Amigorena S, Soria J-C, Eggermont A, Kroemer G, et al. Dendritic cell-derived exosomes for cancer therapy. J Clin Investig. 2016;126(4):1224–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Gunassekaran GR, Poongkavithai Vadevoo SM, Baek M-C, Lee B. M1 macrophage exosomes engineered to foster M1 polarization and target the IL-4 receptor inhibit tumor growth by reprogramming tumor-associated macrophages into M1-like macrophages. Biomaterials. 2021;278: 121137. [DOI] [PubMed] [Google Scholar]
- 144.Lai JJ, Chau ZL, Chen S-Y, Hill JJ, Korpany KV, Liang N-W, et al. Exosome processing and characterization approaches for research and technology development. Adv Sci. 2022;9(15):e2103222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Morishita M, Takahashi Y, Nishikawa M, Takakura Y. Pharmacokinetics of exosomes-an important factor for elucidating the biological roles of exosomes and for the development of exosome-based therapeutics. J Pharm Sci. 2017;106(9):2265–9. [DOI] [PubMed] [Google Scholar]
- 146.Hosseini NF, Amini R, Ramezani M, Saidijam M, Hashemi SM, Najafi R. AS1411 aptamer-functionalized exosomes in the targeted delivery of doxorubicin in fighting colorectal cancer. Biomed Pharmacother Biomedecine Pharmacotherapie. 2022;155:113690. [DOI] [PubMed] [Google Scholar]
- 147.Tang Q, Zhang F, Luo L, Duan Y, Zhu T, Ni Y, et al. Ultrasound-induced gold nanoparticle united with acoustic reprogramming of macrophages for enhanced cancer therapy. ACS Appl Mater Interfaces. 2023. [DOI] [PubMed]
- 148.Zhou X, Liu X, Huang L. Macrophage-mediated tumor cell phagocytosis: opportunity for nanomedicine intervention. Adv Func Mater. 2021;31(5):2006220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Kamerkar S, LeBleu VS, Sugimoto H, Yang S, Ruivo CF, Melo SA, et al. Exosomes facilitate therapeutic targeting of oncogenic KRAS in pancreatic cancer. Nature. 2017;546(7659):498–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Cheng L, Zhang X, Tang J, Lv Q, Liu J. Gene-engineered exosomes-thermosensitive liposomes hybrid nanovesicles by the blockade of CD47 signal for combined photothermal therapy and cancer immunotherapy. Biomaterials. 2021;275: 120964. [DOI] [PubMed] [Google Scholar]
- 151.Mondal J, Pillarisetti S, Junnuthula V, Saha M, Hwang SR, Park I-K, et al. Hybrid exosomes, exosome-like nanovesicles and engineered exosomes for therapeutic applications. J Controlled Release. 2023;353:1127–49. [DOI] [PubMed] [Google Scholar]
- 152.Rao L, Wu L, Liu Z, Tian R, Yu G, Zhou Z, et al. Hybrid cellular membrane nanovesicles amplify macrophage immune responses against cancer recurrence and metastasis. Nat Commun. 2020;11(1):4909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Li Q, Yuan M, Jiao X, Huang Y, Li J, Li D, et al. M1 macrophage-derived nanovesicles repolarize M2 macrophages for inhibiting the development of endometriosis. Front Immunol. 2021;12: 707784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Feng M, Jiang W, Kim BYS, Zhang CC, Fu Y-X, Weissman IL. Phagocytosis checkpoints as new targets for cancer immunotherapy. Nat Rev Cancer. 2019;19(10):568–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Sun M, Yang J, Fan Y, Zhang Y, Sun J, Hu M, et al. Beyond extracellular vesicles: hybrid membrane nanovesicles as emerging advanced tools for biomedical applications. Adv Sci. 2023;10:e2303617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Wang S, Li F, Ye T, Wang J, Lyu C, Qing S, et al. Macrophage-tumor chimeric exosomes accumulate in lymph node and tumor to activate the immune response and the tumor microenvironment. Sci Transl Med. 2021;13(615):eabb6981. [DOI] [PubMed] [Google Scholar]
- 157.Rayamajhi S, Nguyen TDT, Marasini R, Aryal S. Macrophage-derived exosome-mimetic hybrid vesicles for tumor targeted drug delivery. Acta Biomater. 2019;94:482–94. [DOI] [PubMed] [Google Scholar]
- 158.Zhao Y, Zheng Y, Zhu Y, Li H, Zhu H, Liu T. Docetaxel-loaded m1 macrophage-derived exosomes for a safe and efficient chemoimmunotherapy of breast cancer. J Nanobiotechnol. 2022;20(1):359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Xiong F, Ling X, Chen X, Chen J, Tan J, Cao W, et al. Pursuing specific chemotherapy of orthotopic breast cancer with lung metastasis from docking nanoparticles driven by bioinspired exosomes. Nano Lett. 2019;19(5):3256–66. [DOI] [PubMed] [Google Scholar]
- 160.Li S, Wu Y, Ding F, Yang J, Li J, Gao X, et al. Engineering macrophage-derived exosomes for targeted chemotherapy of triple-negative breast cancer. Nanoscale. 2020;12(19):10854–62. [DOI] [PubMed] [Google Scholar]
- 161.Zhao Y, Zheng Y, Zhu Y, Zhang Y, Zhu H, Liu T. M1 macrophage-derived exosomes loaded with gemcitabine and deferasirox against chemoresistant pancreatic cancer. Pharmaceutics. 2021;13(9):1493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Tang Z, Tang C, Sun C, Ying X, Shen R. M1 macrophage-derived exosomes synergistically enhance the anti- bladder cancer effect of gemcitabine. Aging. 2022;14(18):7364–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Li J, Li N, Wang J. M1 macrophage-derived exosome-encapsulated cisplatin can enhance its anti-lung cancer effect. Minerva Medica. 2020. [DOI] [PubMed]
- 164.Lu M, Xing H, Shao W, Zhang T, Zhang M, Wang Y, et al. Photoactivatable silencing extracellular vesicle (PASEV) sensitizes cancer immunotherapy. Adv Mater (Deerfield Beach, Fla). 2022;34(35): e2204765. [DOI] [PubMed] [Google Scholar]
- 165.Wang J, Chen P, Dong Y, Xie H, Wang Y, Soto F, et al. Designer exosomes enabling tumor targeted efficient chemo/gene/photothermal therapy. Biomaterials. 2021;276: 121056. [DOI] [PubMed] [Google Scholar]
- 166.Zhang R-Y, Cheng K, Huang Z-Y, Zhang X-S, Li Y, Sun X, et al. M1 macrophage-derived exosome for reprograming M2 macrophages and combining endogenous NO gas therapy with enhanced photodynamic synergistic therapy in colorectal cancer. J Colloid Interface Sci. 2023;654(Pt A):612–25. [DOI] [PubMed] [Google Scholar]
- 167.Anand U, Dey A, Chandel AKS, Sanyal R, Mishra A, Pandey DK, et al. Cancer chemotherapy and beyond: current status, drug candidates, associated risks and progress in targeted therapeutics. Genes Dis. 2023;10(4):1367–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Petroni G, Cantley LC, Santambrogio L, Formenti SC, Galluzzi L. Radiotherapy as a tool to elicit clinically actionable signalling pathways in cancer. Nat Rev Clin Oncol. 2022;19(2):114–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Wu Y, Song Y, Wang R, Wang T. Molecular mechanisms of tumor resistance to radiotherapy. Mol Cancer. 2023;22(1):96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Ghaffari-Bohlouli P, Jafari H, Okoro OV, Alimoradi H, Nie L, Jiang G, et al. Gas therapy: generating, delivery, and biomedical applications. Small Methods. 2024;8(8): e2301349. [DOI] [PubMed] [Google Scholar]
- 171.Li X, Lovell JF, Yoon J, Chen X. Clinical development and potential of photothermal and photodynamic therapies for cancer. Nat Rev Clin Oncol. 2020;17(11):657–74. [DOI] [PubMed] [Google Scholar]
- 172.Carney RP, Mizenko RR, Bozkurt BT, Lowe N, Henson T, Arizzi A, et al. Harnessing extracellular vesicle heterogeneity for diagnostic and therapeutic applications. Nat Nanotechnol. 2024. [DOI] [PMC free article] [PubMed]
- 173.Rezaie J, Feghhi M, Etemadi T. A review on exosomes application in clinical trials: perspective, questions, and challenges. Cell Commun Signal. 2022;20(1):145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Kimiz-Gebologlu I, Oncel SS. Exosomes: Large-scale production, isolation, drug loading efficiency, and biodistribution and uptake. J Controlled Release. 2022;347:533–43. [DOI] [PubMed] [Google Scholar]
- 175.Zhu L, Sun H-T, Wang S, Huang S-L, Zheng Y, Wang C-Q, et al. Isolation and characterization of exosomes for cancer research. J Hematol Oncol. 2020;13(1):152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Chen J, Li P, Zhang T, Xu Z, Huang X, Wang R, et al. Review on strategies and technologies for exosome isolation and purification. Front Bioeng Biotechnol. 2021;9: 811971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Kapoor KS, Harris K, Arian KA, Ma L, Schueng Zancanela B, Church KA, et al. High throughput and rapid isolation of extracellular vesicles and exosomes with purity using size exclusion liquid chromatography. Bioactive Mater. 2024;40:683–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Cui H-Y, Rong J-S, Chen J, Guo J, Zhu J-Q, Ruan M, et al. Exosomal microRNA-588 from M2 polarized macrophages contributes to cisplatin resistance of gastric cancer cells. World J Gastroenterol. 2021;27(36):6079–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Xin L, Zhou L-Q, Liu C, Zeng F, Yuan Y-W, Zhou Q, et al. Transfer of LncRNA CRNDE in TAM-derived exosomes is linked with cisplatin resistance in gastric cancer. EMBO Rep. 2021;22(12): e52124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Yu D, Chang Z, Liu X, Chen P, Zhang H, Qin Y. Macrophage-derived exosomes regulate gastric cancer cell oxaliplatin resistance by wrapping circ 0008253. Cell Cycle (Georgetown, Tex). 2023;22(6):705–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Zhang X, Wang J, Liu N, Wu W, Li H, Chen J, et al. Molecular mechanism of CD163+ tumor-associated macrophage (TAM)-derived exosome-induced cisplatin resistance in ovarian cancer ascites. Ann Transl Med. 2022;10(18):1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Binenbaum Y, Fridman E, Yaari Z, Milman N, Schroeder A, Ben David G, et al. Transfer of miRNA in macrophage-derived exosomes induces drug resistance in pancreatic adenocarcinoma. Can Res. 2018;78(18):5287–99. [DOI] [PubMed] [Google Scholar]
- 183.Wang H, Wang L, Pan H, Wang Y, Shi M, Yu H, et al. Exosomes derived from macrophages enhance aerobic glycolysis and chemoresistance in lung cancer by stabilizing c-Myc via the inhibition of NEDD4L. Front cell Dev Biol. 2021;8:620603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Gu X, Shi Y, Dong M, Jiang L, Yang J, Liu Z. Exosomal transfer of tumor-associated macrophage-derived hsa_circ_0001610 reduces radiosensitivity in endometrial cancer. Cell Death Dis. 2021;12(9):818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Zhang F, Sang Y, Chen D, Wu X, Wang X, Yang W, et al. M2 macrophage-derived exosomal long non-coding RNA AGAP2-AS1 enhances radiotherapy immunity in lung cancer by reducing microRNA-296 and elevating NOTCH2. Cell Death Dis. 2021;12(5):467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Wan X, Xie B, Sun H, Gu W, Wang C, Deng Q, et al. Exosomes derived from M2 type tumor-associated macrophages promote osimertinib resistance in non-small cell lung cancer through MSTRG.292666.16-miR-6836–5p-MAPK8IP3 axis. Cancer Cell Int. 2022;22(1):83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Yuan S, Chen W, Yang J, Zheng Y, Ye W, Xie H, et al. Tumor-associated macrophage-derived exosomes promote EGFR-TKI resistance in non-small cell lung cancer by regulating the AKT, ERK1/2 and STAT3 signaling pathways. Oncol Lett. 2022;24(4):356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Zheng N, Wang T, Luo Q, Liu Y, Yang J, Zhou Y, et al. M2 macrophage-derived exosomes suppress tumor intrinsic immunogenicity to confer immunotherapy resistance. Oncoimmunology. 2023;12(1):2210959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Ning J, Hou X, Hao J, Zhang W, Shi Y, Huang Y, et al. METTL3 inhibition induced by M2 macrophage-derived extracellular vesicles drives anti-PD-1 therapy resistance via M6A-CD70-mediated immune suppression in thyroid cancer. Cell Death Differ. 2023;30(10):2265–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Luo Y, Chen Y, Jin H, Hou B, Li H, Li X, et al. The suppression of cervical cancer ferroptosis by macrophages: the attenuation of ALOX15 in cancer cells by macrophages-derived exosomes. Acta Pharmaceutica Sinica B. 2023;13(6):2645–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.He Y, Sun MM, Zhang GG, Yang J, Chen KS, Xu WW, et al. Targeting PI3K/Akt signal transduction for cancer therapy. Signal Transduct Target Ther. 2021;6(1):425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Zhang L, Lu Z, Zhao X. Targeting Bcl-2 for cancer therapy. Biochim Biophys Acta. 2021;1876(1): 188569. [DOI] [PubMed] [Google Scholar]
- 193.Wang Z-W, Hu X, Ye M, Lin M, Chu M, Shen X. NEDD4 E3 ligase: functions and mechanism in human cancer. Semin Cancer Biol. 2020;67(Pt 2):92–101. [DOI] [PubMed] [Google Scholar]
- 194.Huang R-X, Zhou P-K. DNA damage response signaling pathways and targets for radiotherapy sensitization in cancer. Signal Transduct Target Ther. 2020;5(1):60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Bedard PL, Hyman DM, Davids MS, Siu LL. Small molecules, big impact: 20 years of targeted therapy in oncology. Lancet (London, England). 2020;395(10229):1078–88. [DOI] [PubMed] [Google Scholar]
- 196.Passaro A, Jänne PA, Mok T, Peters S. Overcoming therapy resistance in EGFR-mutant lung cancer. Nat Cancer. 2021;2(4):377–91. [DOI] [PubMed] [Google Scholar]
- 197.Lei G, Zhuang L, Gan B. Targeting ferroptosis as a vulnerability in cancer. Nat Rev Cancer. 2022;22(7):381–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.McAndrews KM, Xiao F, Chronopoulos A, LeBleu VS, Kugeratski FG, Kalluri R. Exosome-mediated delivery of CRISPR/Cas9 for targeting of oncogenic KrasG12D in pancreatic cancer. Life Sci Alliance. 2021;4(9): e202000875. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.