RESUME
Objectif: Cette étude a pour objectif de comparer les résultats à court et long terme des anastomoses iléo-coliques isopéristaltiques (IA) et antiperistaltiques (AA) après une colectomie droite ou une résection iléocæcale pour adénocarcinome du côlon droit ou maladie de Crohn. Méthodes: Un essai clinique rétrospectif monocentrique a été mené à l’hôpital Fattouma Bourguiba de Monastir. Les patients atteints de cancer du côlon droit ou de maladie de Crohn iléocæcale ayant subi une résection élective programmée avec IA ou AA ont été inclus. Le critère principal était la fuite anastomotique, tandis que les critères secondaires incluaient la morbidité postopératoire et les résultats à long terme. Résultats: Quatre-vingt-quatorze patients, dont 55 avec un cancer du côlon droit et 39 avec une maladie de Crohn, ont été inclus entre janvier 2016 et juillet 2023. Parmi eux, 48 ont subi une IA et 46 une AA. Les taux de fuite anastomotique étaient similaires entre les deux techniques. Les variables de base et opératoires étaient comparables, sauf pour une prédominance masculine en AA pour la maladie de Crohn et un taux de conversion plus élevé en AA. Aucune différence significative n’a été observée concernant les variables pathologiques, la durée opératoire, la récupération du transit intestinal, ou les complications postopératoires. L’analyse multivariée a montré que l’élévation des globules blancs, la résection R2, et l’adénocarcinome mucineux étaient des facteurs de risque de fuite anastomotique, tandis que les niveaux d’albumine et le renforcement de la ligne d’agrafes étaient des facteurs protecteurs contre la morbidité postopératoire. Conclusion: Les résultats à court et à long terme des techniques IA et AA sont comparables, bien que le taux de conversion soit plus élevé en AA. Des recherches supplémentaires sont nécessaires pour améliorer la sécurité de l’AA.
ABSTRACT
Introduction: Ileocolonic anastomoses are frequent in colorectal surgeries, but anastomotic leakage remains a serious complication associated with increased morbidity and mortality. The optimal peristaltic orientation for anastomosis is still debated. Aim: To evaluate and compare short- and long-term outcomes of isoperistaltic (IA) and antiperistaltic (AA) side-to-side ileocolic anastomoses after right colectomy or ileocecal resection for right-sided adenocarcinoma or Crohn’s disease. Methods: A single-center retrospective clinical trial was conducted at Fattouma Bourguiba University Hospital, Monastir, involving patients with right-sided colon cancer or ileocecal Crohn’s disease who underwent elective resection with either IA or AA. The primary outcome was anastomotic leakage, while secondary outcomes included postoperative morbidity and long-term results. Results: Ninety-four patients, including 55 with right-sided colon cancer and 39 with Crohn’s disease, were analyzed between January 2016 and July 2023. Of these, 48 underwent IA, and 46 underwent AA. Both anastomotic techniques exhibited similar leakage rates. Baseline and operative variables were comparable except for male predominance in AA for Crohn’s disease and a higher conversion rate in AA. No significant differences were noted regarding pathological variables, operative time, bowel transit recovery, oral tolerance, hospital stay, or postoperative complications. Multivariate analysis revealed that elevated white blood cell count, R2 resection, and mucinous adenocarcinoma were risk factors for anastomotic leakage, while albumin levels and staple line reinforcement were protective factors against postoperative morbidity. Conclusion: IA and AA demonstrated comparable safety and feasibility, though AA had a higher conversion rate. Further studies are required to optimize AA safety.
Introduction
Colorectal diseases are an important entity in digestive surgery.
These procedures carry a significant burden of postoperative morbidity and mortality, mainly attributed to anastomotic leaks (1).
Several studies have investigated how to reduce the rate of this complication (2).
It presents some particularities in the context of right colectomy and ileocecal resection that require an ileocolic anastomosis (3 ,4).
These two procedures were indicated essentially in right colon cancer and Crohn’s disease, respectively. Reducing the incidence of anastomosis-related complications is challenging (2).
For these reasons, several varieties of ileocolic anastomosis were suggested (5): end-to-side versus side-to-side, mechanical versus hand-sewn, and intracorporeal versus extracorporeal anastomosis.
Furthermore, for a side-to-side ileocolic anastomosis, one of the additional fundamental points of debate was the direction of reconstruction of the digestive tract according to the peristatic direction: isoperistaltic anastomosis (IA) or antiperistaltic anastomosis (AA) (3).
As this decision can impact postoperative outcomes, these two varieties of side-to-side ileocolic anastomosis were compared with a controversial result (6, 7).
IA has gained favor among certain surgeons due to its reduced need for extensive intestinal mobilization (8).
On the other hand, AA has been preferred by some surgeons because it can mimic a pseudovalvular mechanism at the anastomotic site (7 ).
These disparate results highlight the challenges to reaching a definitive conclusion on the most effective and safest approach to this anastomosis.
Furthermore, the available literature on the effects of different peristaltic orientations on anastomosis was limited by small sample sizes (3).
This restriction makes it challenging to apply the findings to larger populations with relative neglect of long-term outcomes in right colon cancer and Crohn’s disease separately.
Our study compared the short-term and long-term outcomes of isoperistaltic side-to-side anastomosis and antiperistaltic side-to-side anastomosis after right colectomy or ileocecal resection.
Methods
Study design
This study is a single-center retrospective clinical trial of consecutive patients.
Patients were divided into isoperistaltic side-to-side anastomosis and antiperistaltic side-to-side anastomosis.
The study protocol adhered to the methodological index criteria for nonrandomized studies (MINORS) criteria (9).
Populations
Adults (aged over 18 years) with histologically proven right-sided colon adenocarcinoma or ileocecal Crohn’s disease at the Department of Visceral and Digestive Surgery at Fattouma Bourguiba University Hospital in Monastir between January 2016 and July 2023.
For Crohn’s disease, we included all patients with a confirmed gastrointestinal tract lesion of Crohn’s disease with complications: stenosis, fistula, abscess, or Crohn’s disease refractory to medical treatment.
Patients were excluded if the pathological examination resulted in a diagnosis other than colonic adenocarcinoma or Crohn’s disease, or if multiple anastomosis or endto-side anastomosis were performed.
Patients were not included if they underwent emergent surgery, required a defunctioning stoma, patients with multiple primary cancers, synchronous metastases, preoperative chemotherapy or radiation, and patients undergoing proctocolectomy, proctectomy, or segmental colectomy
Surgical procedure
The patients underwent side-to-side ileocolic anastomosis through laparotomy or laparoscopic-assisted surgery with an extracorporeal anastomosis, with occasional conversions to open surgery.
No mechanical bowel preparation or oral decontamination was performed.
General anesthesia was administered.
Intervention group
In this group, an isoperistaltic side-to-side anastomosis(Fig. 1) connected the terminal ileum and transverse colon, aligning with the normal direction of bowel movement.
The stapled anastomosis involved a five-cm overlap in the opposite direction.
An enterotomy and a colotomy were performed five cm distally from the staple line.
The anastomosis was performed using either a hand-sewn suture or an 80 mm mechanical linear stapler.
Sometimes, additional hand sutures were applied for reinforcement in the ileal and colonic staple sections.
Figure 1. Side-to-side isoperistaltic ileocolic anastomosis .

Control group
In the control group, an antiperistaltic side-to-side anastomosis (Fig. 2) connected the terminal ileum and transverse colon with normal bowel movement.
A fivecm overlap was maintained in the same direction.
An enterotomy was performed on the antimesenteric side of the ileum and a colotomy on the colon
We introduced the colon and ileum into the 80mm mechanical linear stapler in the same direction with an overlap of five cm.
Then, the anastomosis was performed.
This anastomosis was terminalized with a second 80-mm mechanical linear stapler to cut the small intestine and colon and free the operative specimen.
Sometimes, additional hand sutures were applied for reinforcement in the ileal and colonic staple sections.
Figure 2. Side-to-side antiperistaltic ileocolic anastomosis .

Endpoints
The main endpoint was an anastomotic leak (AL) that occurred within 30 days after surgery and its risk factors.
Secondary endpoints included operative time, rate of conversion to laparotomy, recovery from bowel transit, satisfactory oral tolerance, readmission,duration of postoperative stay, postoperative morbidity (wound infection, incisional herniation, bleeding, and postoperative medical complications) and its risk factors and long-term outcomes (incisional herniation, anastomotic stenosis, recurrence or metastasis, and malnutrition).
Data extraction
We retrospectively reviewed medical data in our department: demographic data of patients, diseaserelated characteristics, pathological characteristics, surgical details, and short-term and long-term outcomes.
Demographic characteristics included age, sex, body mass index (BMI), American Society of Anesthesiologists(ASA) score, concomitant comorbidities, history of abdominal surgery, and risk factors.
The disease-related characteristics associated with right-sided colon cancer included preoperative carcinoembryonic antigen (CEA),tumor location, tumour grade according to the American Joint Committee on Cancer (10), number of lymph nodes,and length of resected intestine.
For Crohn's disease, we considered various factors, including preoperative medical treatment, location of the disease, and behavior according to the Montreal classification (11).
Operative characteristics encompassed the surgical approach, conversion to laparotomy, type of anastomosis, and operative time.
Short-term results that occurred within 30 days after surgery included recovery from intestinal transit, satisfactory oral tolerance, readmission, hospital stay, and postoperative surgical complications.
Surgical complications were classified according to the Clavien-Dindo classification (12) and included anastomotic leakage, wound infection, incisional herniation, and bleeding.
Furthermore, postoperative medical complications were also evaluated.
Regarding long-term outcomes, patients were followed after hospital discharge in the outpatient department and long-term complications included incisional herniation, anastomotic stenosis, recurrence or metastasis, and malnutrition.
Statistical analysis
Statistical analysis was performed using SPSS software version 22.0.
Graphs and visualizations were generated using Jupyter Notebook 6.5.3 environment, Python 3.9.13 programming language, along with the following libraries: Scipy 1.10.1, Statsmodels 0.13.5, Matplotlib 3.7.1 and Seaborn 0.12.2.
Continuous variables, whether they followed a normal or abnormal distribution, were expressed as the median ± standard deviation and analyzed with a Student’s t test or Mann-Whitney U test, as appropriate.
Categorical variables were presented as percentages and analyzed with Fisher's exact test or a χ2 test, as appropriate.
We performed univariate and multivariate logistic regression analyzes to determine the factors associated with binary outcomes.
We included variables with a p-value of 0.10 or less in the multivariate analysis.
We measured associations using odds ratios (OR) with 95% confidence intervals (CI), considering p-values less than 0.05 as statistically significant.
In multivariate logistic regression to assess risk factors for anastomotic leakage and postoperative morbidity, we standardized numerical features and checked for multicollinearity using the Variance Inflation Factor.
The importance of the characteristics, based on coefficients, was visually represented using bar charts to identify and classify the features (13).
Results
Demographic and clinical characteristics of the study population
Between January 2016 and July 2023, 90 patients were included in this study after excluding 14 patients who did not meet the inclusion criteria.
The flow chart of the retained study population is presented in Fig. 3.
We retained 55 patients (58.51%) operated on for right colon cancer and 39 patients (41.49%) operated on Crohn’s disease.
Within the study population, 48 patients (51.06%) underwent IA, while 46 patients (48.94%) underwent AA.
Examination of these two anastomotic groups revealed no statistically significant disparities in their demographic and clinical characteristics (Table 1).
Figure 3. Flow diagram of the study population .

Among 55 patients with right colon cancer who underwent right colectomy, 26 patients (47.27%) had IA, while 29 patients (52.73%) had AA.

There were no statistically significant differences in preoperative variables between the two groups (Table 2).
Of the 39 patients who underwent elective resection for Crohn's disease, 22 (56.41%) underwent IA, while 17 (43.59%) underwent AA.
In the baseline characteristics of the two groups, there were no statistically significant differences in preoperative demographic and clinical characteristics between IA and AA in Crohn's disease, except for gender,as detailed in Table 2.
Surgical variables and results of the study population
The surgical variables, short-term results, and long-term results are presented in Table 3.
When comparing surgical parameters between the IA and the AA, we did not observe significant differences.
In the univariate analysis, there were no statistical differences between IA and AA in terms of anastomotic leakage (10.41% vs 8.69%, p=1), postoperative bleeding (16.67% vs 21.74%, p=0.71), wound infection (12.5% vs. 10.87%, p=1), incisional herniation (2.08% vs. 0%, p = 1), Clavien-Dindo’s main complications (p = 0.29).

Two patients in the AA group died during the postoperative period: one due to anastomotic leakage and another due to nosocomial pneumonia.
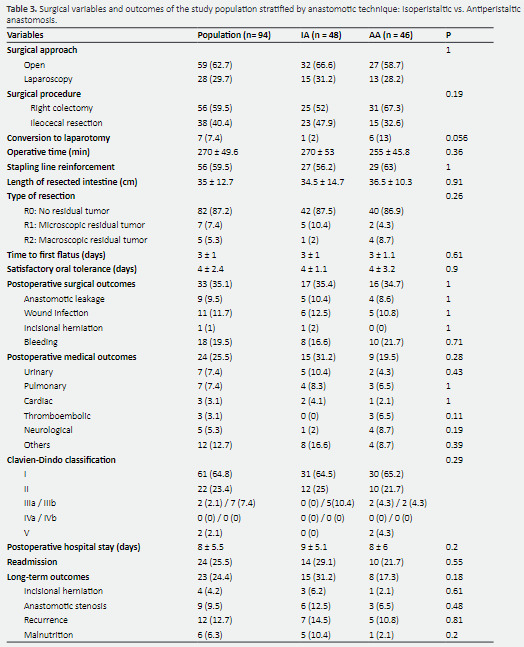
For postoperative medical outcomes, there were no statistical differences between the two groups (31.25% vs. 19.57%, p=0.28).
Furthermore, we did not find any statistical difference between IA and AA in terms of hospital stay (9 ± 5.18 vs. 8 ± 6.01 days, p=0.2), readmission rate (29.17% vs. 21.74%, p = 0.55) and long-term results (31.25% vs. 17.39%, p=0.18).
Regarding surgical variables for patients with right colon cancer(Table 4), the operative time was 270 ± 49.08 min.
In the IA group, 18 patients (69.23%) underwent open surgery and seven patients (26.92%) underwent miniinvasive surgery.
The conversion rate was reported only in one patient (3.85%).
Fourteen patients (53.85%) underwent hand-sewn IA and 12 patients (46.15%) had stapled IA.
For the AA group, 21 patients (72.41%) underwent open surgery and six patients (20.69%) underwent laparoscopy.
The conversion rate was reported in two patients (6.9%).
In particular, all patients in this group underwent stapled AA.
Regarding pathological analysis, the median length of the resected intestine was 40 ± 10.69 cm and the median tumor size was 4.5 ± 10.39 cm.
The number of lymph nodes was 17 ± 10.39.
Lieberkühn adenocarcinoma was the histological variant most frequent in 37 patients(67.27%) followed by mucinous adenocarcinoma in 19 patients (34.55%).
For pathological staging according to the American Joint Committee on Cancer (AJCC), grade II was the most prevalent in 25 patients (45.46%) followed by grade III in 22 patients (40%).
The type of resection was R0 in 52 patients (94.55%).
There were no significant differences between IA and AA in these pathological variables.
ForFor postoperative outcomes, there were no significant differences between the two techniques in terms of postoperative surgical complications (46.15% vs 41.38%, p=0.93), including anastomotic leakage (15.38% vs. 6.89%, p=0.4) or postoperative medical complications(38.46% vs. 31.03%, p=0.76).
Furthermore, there were no differences between the two groups in terms of hospital stay (10 ± 5.29 vs. 8 ± 6.17 days, p=0.09), readmissions(34.62% vs. 24.14%, p=0.57) and long-term results(38.46% vs. 20.69%, p=0.24).
In patients with Crohn’s disease (Table 4), the analysis of surgical and pathological variables revealed that the operative time was 255 ± 50.03 min.
In the IA group, 14 patients (63.64%) underwent open surgery and eight patients (36.36%) underwent laparoscopic surgery.
Among them, 14 patients (63.64%) had a hand-sewn IA and eight patients (36.36%) had a stapled IA.
In contrast, within the AA group, six patients(35.29%) had open surgery and seven patients (41.18%) had laparoscopic surgery.
Among them, only one patient(5.88%) had a hand-sewn AA, while 16 patients (94.12%)had a stapled AA.
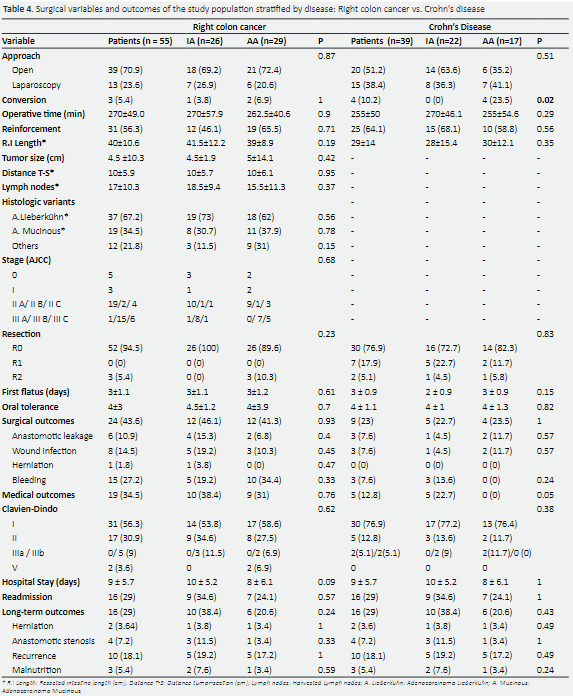
In particular, there was a significant difference in the conversion rate between IA and AA (0% vs. 23.53%,p=0.02).
The length of the resected intestine was 29 ± 14 cm, with a predominant type of resection R0 in 30 patients (76.92%).
For postoperative outcomes, there were no significant differences between IA and AA in the surgical outcomes (22.73% vs. 23.53%, p = 1), including anastomotic leakage (4.55 % vs. 11.76%, p=0.57),postoperative medical complications (22.73% vs. 0%,p=0.056), hospital stay (7 ± 4.84 vs. 8 ± 5.86 days, p=1)and readmission rate (22.73% vs. 17.65%, p=1).
Regarding the long-term results, there were no differences between the two groups (22.73% vs. 11.76%, p=0.43).
Univariate and multivariate analyses of the study population for anastomotic leakage
Univariate and multivariate analyzes were performed for anastomotic leakage in the study population.
The choice between IA and AA did not show statistical significance in univariate or multivariate analyzes (p = 0.522).
White blood cell count emerged as a significant predictor in both univariate (p=0.076) and multivariate analyses(OR=2.888, 95% CI [1.245, 6.699], p=0.013).
Serum albumin levels were not significant in the multivariate analysis (p=0.33), suggesting that AL did not have an independent predictive role when considering other variables.
Furthermore, the type of resection (R2) was identified as a significant predictor of AL (OR=21.094, 95% CI [1.789, 248.708], p=0.015).
In multivariate analyzes of the patients with right colon cancer, only Mucinous adenocarcinoma was associated with an elevated risk of AL occurrence (OR=6.899, 95% CI [1.125, 42.29], p =0.037).
However, in multivariate analyses of patients with Crohn’s disease, no variables were found to be associated with the appearance of AL.
Univariate and multivariate analyses of the study population for postoperative morbidity
In multivariate analyses for postoperative morbidity in the study population, the type of anastomosis did not show an independent association.
However, the reinforcement of the stapling line and the length of the resected intestine were significantly associated with morbidity,with odds ratios of 0.175 (95% CI [0.036, 0.848], p = 0.03) and 2.333 (95% CI [1.037, 5.248], p = 0.041), respectively.
In multivariate analyzes of the patients with right colon cancer to assess postoperative morbidity, albumin levels were found to be a significant protective factor against postoperative morbidity, with an odds ratio of 0.397 (95% CI [0.2, 0.79], p = 0.008).
In the multivariate analysis of patients with Crohn's disease to evaluate postoperative morbidity, the length of the resected intestine was a significant risk factor for postoperative morbidity, with a odds ratio of 2.504 (95% CI [1.031, 6.082], p = 0.043).
Discussion
This controlled clinical trial was conducted in 94 patients with right-sided colon cancer and ileocecal Crohn’s disease.
In all the study population and even in the subgroup analysis, IA and AA were associated with similar anastomotic leak, operative time, recovery from intestinal transit, satisfactory oral tolerance, readmission, duration of postoperative stay, postoperative morbidity(wound infection, incisional herniation, bleeding, and postoperative medical complications) and long-term results (incisional herniation, anastomotic stenosis,recurrence or metastasis, and malnutrition).
AA was associated with a higher rate of conversion.
In the multivariate analysis, we found that elevated white blood cell counts and type R2 were significant risk factors for anastomotic leakage in the general population of the study.
Specifically, patients with right colon cancer had a higher risk of anastomotic leakage when diagnosed with mucinous adenocarcinoma.
For postoperative morbidity, reinforcement of the stapling line was a protective factor, while the greater length of the resected intestine was a risk factor for both the general study population and Crohn's disease patients.
Among patients with right colon cancer, albumin levels were found to be a significant protective factor against postoperative morbidity.
A well-executed anastomosis is crucial.
Despite the existence of numerous anastomotic techniques, the most effective technique remains a topic of ongoing debate.
Traditional end-to-end anastomosis, while a standard procedure to restore intestinal continuity, presents inherent challenges.
These challenges include the risk of stenosis and diameter disparities, particularly in ileocolic anastomosis, and can lead to longer operative time (7).
In contrast, side-to-side anastomosis improved blood flow, increased opening, reduced intraluminal pressure, and reduced the risk of proximal ischemia (8,14).
Stapling devices have revolutionized mechanical anastomosis, offering convenience, stability, and adaptability to variations in the diameter of the intestinal tract (7).
Despite higher costs, stapled anastomosis was chosen for its safety benefits, requiring less surgical skill and resulting in similar anastomotic-related complications to hand-sewn anastomosis (5,15–18).
Regardless of surgical technique, comparing IA and AA in right colectomy and ileocecal resection remains crucial due to the literature gap in the literature on their short-term and long-term results.
Proponents of IA claim that it aligns with natural bowel movement and offers advantages at various anatomical sites (19).
It is especially suitable when there is limited intestinal mobility during right colectomy or ileocecal resection surgeries.
When employing 60-mm linear stapling devices for anastomosis, IA theoretically reduces the required intestinal mobilization by approximately 6 centimeters compared to AA (8)
However, it may lead to some twisting of the terminal ileum mesentery.
In contrast, AA can reduce postoperative ileus by acting as a pseudovalvular mechanism, reducing ileocecal reflux (20, 21).
However, in our study, the postoperative ileus and satisfactory oral tolerance were similar for both anastomotic techniques.
In our study, both IA and AA showed similar operative times.
This concordance was supported by the study by Matsuda et al. (8) study, which reported a median operative time of 215 ± 68 min for IA compared to 203 ± 53 min for AA (p = 0.264).
However, it should be mentioned that the median operative time in our study was longer, at 50 minutes, compared to the study by Matsuda et al. ( 8) study.
This difference could be attributed to the standardized tools used for measuring operative time and the variations in learning curves between the different surgeons in our study
Furthermore, when examining the conversion rate, it was 7.45 % in our study, higher than that reported by Noeli Ibanez et al. (20), who found a conversion rate of 3.7% for IA compared to 5.7% for AA(p=0.5).
Our multivariate analysis for postoperative morbidity showed that the longer resected intestine was a significant risk factor, according to a study by Duan et al. (22) showing that prior intestinal resection in patients with Crohn's disease increases the risk of complications (p=0.019).
Two additional studies (23,24) suggested that extensive resection margins are not necessary to reduce the recurrence of Crohn's disease, favoring bowel preservation procedures to prevent nutritional deficiencies (25 ).
Additionally, reinforcement of the stapling line of the ileal and colon section had a significant reduction in postoperative morbidity by decreasing anastomotic leakage (AL), in line with previous findings (26), where it was found to be an independent protective factor (p < 0.001) in both the univariate and multivariate analysis.
Furthermore, our findings on albumin levels and postoperative morbidity among patients with right colon cancer align with previous research ( 27) that identified malnutrition as a predictor of complications (OR=2.79; p=0.002).
Although our results lacked statistical significance, an association was observed between albumin levels and AL was observed.
A retrospective study by Choudhuri et al. (28) revealed significantly higher AL rates in patients with lower albumin levels, especially when they were below 3.5 g/dl.
Our study extensively evaluated anastomotic leakage (AL), defined by the International Rectal Cancer Study Group as a ‘defect in the intestinal wall at the anastomotic site leading to communication between the intra and extraluminal compartments’ (29).
The absence of a consensus definition has resulted in various incidence reports and categorizations, adding complexity, including simple fistulas, intraperitoneal/extraperitoneal leaks, sepsis-producing/asymptomatic, and early/late leaks (30).
Despite advances in surgical techniques, AL remains a concerning complication in colorectal surgery, with a prevalence ranging from 0% to 20% depending on location.
It leads to increased morbidity, mortality, and healthcare care costs, and affects functional and oncological outcomes (31).
When comparing AL rates between anastomotic techniques, our results align with a previous study (20), which found no significant differences in AL occurrence.
However, the elevated AL rate in our study can be attributed to factors such as inclusion of Crohn's disease patients, a significant risk factor for AL with an odds ratio (OR) of 3.3 (32).
Neary et al. (33) reported AL rates during ileocolectomy for Crohn's disease ranging from 1.6% to 14.3%, depending on associated risk factors. Crowell and Messaris (34) identified preoperative weight loss, prior surgery, and steroid use as risk factors for AL in Crohn's disease.
Furthermore, a systematic review by Eriksen et al. (35) revealed a higher AL rate in patients receiving corticosteroids before surgery (6.77% vs. 3.26% in the non-corticosteroids group).
Expanding on these risk factors, several studies have identified additional factors influencing anastomotic leakage, highlighting the importance of preoperative risk assessment for adapting surgical strategies (26 ,31,36 –39).
Our univariate analysis demonstrated a significant male predominance in AA among Crohn's disease patients, along with a higher rate of AL, potentially explaining this association.
Our multivariate analysis for AL revealed a significant association between preoperative white blood cell count and the occurrence of AL.
In a retrospective study by Paliogiannis et al. (40), which included 1,032 patients, the preoperative white blood cell count did not differ significantly between patients with and without AL.
However, on the fourth postoperative day, those with AL showed a significantly higher white blood cell count (10 for leaks, 7.9 for non-leaks, p < 0.0001).
Furthermore, our results on macroscopic residual disease at the surgical margin (R2) align with a prospective study that included 82 of 2 363 patients who experienced AL (41).
This study found that positive tumor margins at resection (R1 or R2) significantly increased the risk of AL (OR=3.3, 95% CI [1.2–8.8], p=0.019).
Furthermore, among patients with right colon cancer, mucinous adenocarcinoma emerged as a risk factor for AL.
This finding was supported by a retrospective cohort study of 863 of 36,929 patients who experienced early AL, indicating a significant association between AL and the histological presence of poorly differentiated or mucinous adenocarcinoma (42).
Regarding long-term outcomes, few articles have focused on these aspects.
In particular, the same study (20) examined variables such as herniation, intestinal obstruction, and metastasis, reporting a combined occurrence rate of 16.6% in IA compared to 7.4% in AA.
However, our study did not go into diarrhea rates and instead discussed malnutrition as a long-term outcome.
We should mention that our study had several limitations, primarily due to its retrospective nonrandomised singlecenter controlled trial design.
This study relies on existing data, which can result in significant variables going unrecorded, potentially impacting results, and introducing selection bias and confounding.
Achieving a homogeneous baseline for the two anastomotic groups, particularly in the analysis of Crohn’s disease subgroups, was challenging due to a statistical difference in sex.
The propensity matching analysis was not feasible due to the small sample size.
Furthermore, technical variations in additional sutures used for anastomosis reinforcement and non-standard follow-up periods could influence anastomotic leakage rates.
These limitations underscore the need for a multicentric randomized controlled trial(RCT) with a larger sample size to better address the selection criteria for personalized treatment, whether involving isoperistaltic or antiperistaltic anastomosis.
Conclusion
In conclusion, our study examined the short-term and long-term outcomes of isoperistaltic and antiperistaltic side-to-side anastomosis following right colectomy and ileocecal resection.
In general, both techniques were technically feasible and safe, demonstrating similar short-term and long-term outcomes.
Furthermore, in the multivariate analysis, the anastomosis technique did not emerge as a predictive factor for anastomotic leak or morbidity.
Only elevated white blood cell count and type R2 were significantly associated with anastomotic leakage.
Mucinous adenocarcinoma was identified as a risk factor for anastomotic leakage in the population of colon cancer.
Regarding postoperative morbidity, albumin levels and stapling line reinforcement were found to be protective factors, while a longer length of the resected intestine was a risk factor for both the general study population and patients with Crohn's disease.
Although acknowledging the limitations of the study, including its retrospective non-random design, we encourage future randomized controlled trials with larger sample sizes and standardized follow-up periods to provide a more comprehensive evaluation of these anastomosis techniques.
Therefore, it facilitates patient-centered decision making in the field of gastrointestinal surgery and draws definitive conclusions about the most effective and safe approaches to anastomosis procedures.
References
- Liu H, Zeng Z, Zhang H, Wu M, Ma D, Wang Q, et al. Morbidity, mortality, and pathologic outcomes of transanal versus laparoscopic total mesorectal excision for rectal cancer short-term outcomes from a multicenter randomized controlled trial. Annals of Surgery. 2023;277(1):1. doi: 10.1097/SLA.0000000000005523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaouch MA, Kellil T, Jeddi C, Saidani A, Chebbi F, Zouari K. How to prevent anastomotic leak in colorectal surgery? A systematic review. Annals of Coloproctology. 2020;36(4):213. doi: 10.3393/ac.2020.05.14.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Symeonidis D, Karakantas KS, Kissa L, Samara AA, Bompou E, Tepetes K, et al. Isoperistaltic vs antiperistaltic anastomosis after right hemicolectomy: A comprehensive review. World Journal of Clinical Cases. 2023;11(8):1694. doi: 10.12998/wjcc.v11.i8.1694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Celentano V, Pellino G, Spinelli A, Selvaggi F, SICCR Current status of Crohn's disease surgery collaborative, Celentano V, et al. Anastomosis configuration and technique following ileocaecal resection for Crohn's disease: a multicentre study. Updates Surg. 2021;73(1):149–156. doi: 10.1007/s13304-020-00918-z. [DOI] [PubMed] [Google Scholar]
- Puleo S, Sofia M, Trovato MA, Pesce A, Portale TR, Russello D, et al. Ileocolonic anastomosis: preferred techniques in 999 patients. A multicentric study. Surg Today. 2013;43(10):1145–1149. doi: 10.1007/s00595-012-0381-8. [DOI] [PubMed] [Google Scholar]
- Ibáñez N, Abrisqueta J, Luján J, Hernández Q, Rufete MD, Parrilla P. Isoperistaltic versus antiperistaltic ileocolic anastomosis. Does it really matter? Results from a randomised clinical trial (ISOVANTI) Surg Endosc. 2019;33(9):2850–2857. doi: 10.1007/s00464-018-6580-7. [DOI] [PubMed] [Google Scholar]
- Zhang M, Lu Z, Hu X, Zhou H, Zheng Z, Liu Z, et al. Comparison of the short-term outcomes between intracorporeal isoperistaltic and antiperistaltic totally stapled side-to-side anastomosis for right colectomy: A retrospective study on 214 consecutive patients. Surg Open Sci. 2022;9:7–12. doi: 10.1016/j.sopen.2022.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuda A, Miyashita M, Matsumoto S, Sakurazawa N, Takahashi G, Yamada M, et al. Isoperistaltic versus antiperistaltic stapled side-to-side anastomosis for colon cancer surgery: a randomized controlled trial. J Surg Res. 2015;196(1):107–112. doi: 10.1016/j.jss.2015.02.059. [DOI] [PubMed] [Google Scholar]
- Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- Edge SB, American Joint Committee on Cancer . AJCC cancer staging manual. 7th ed. Springer; New York, NY: 2010. 648. [DOI] [PubMed] [Google Scholar]
- Satsangi J, Silverberg MS, Vermeire S, Colombel J. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut. 2006;55(6):749–753. doi: 10.1136/gut.2005.082909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dindo D, Demartines N, Clavien PA. Classification of Surgical Complications. Ann Surg. 2004;240(2):205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brownlee J. How to Calculate Feature Importance With Python. MachineLearningMastery.com. 2020. [2023 Nov 5]. https://machinelearningmastery.com/calculate-feature-importance-with-python/
- Simillis C, Purkayastha S, Yamamoto T, Strong SA, Darzi AW, Tekkis PP. A Meta-Analysis Comparing Conventional End-to-End Anastomosis vs. Other Anastomotic Configurations After Resection in Crohn's Disease. Diseases of the Colon & Rectum. 2007;50(10):1674–1687. doi: 10.1007/s10350-007-9011-8. [DOI] [PubMed] [Google Scholar]
- Choy PYG, Bissett IP, Docherty JG, Parry BR, Merrie A, Fitzgerald A. Stapled versus handsewn methods for ileocolic anastomoses. Cochrane Database Syst Rev. 2011;(9):CD004320. doi: 10.1002/14651858.CD004320.pub3. [DOI] [PubMed] [Google Scholar]
- Kracht M, Hay JM, Fagniez PL, Fingerhut A. Ileocolonic anastomosis after right hemicolectomy for carcinoma: stapled or hand-sewn? A prospective, multicenter, randomized trial. Int J Colorectal Dis. 1993;8(1):29–33. doi: 10.1007/BF00341273. [DOI] [PubMed] [Google Scholar]
- Hashemi M, Novell JR, Lewis AA. Side-to-side stapled anastomosis may delay recurrence in Crohn's disease. Dis Colon Rectum. 1998;41(10):1293–1296. doi: 10.1007/BF02258231. [DOI] [PubMed] [Google Scholar]
- Yamamoto T, Keighley MR. Stapled functional end-to-end anastomosis in Crohn's disease. Surg Today. 1999;29(7):679–681. doi: 10.1007/BF02483001. [DOI] [PubMed] [Google Scholar]
- Tewari M, Shukla HS. Right colectomy with isoperistaltic side-to-side stapled ileocolic anastomosis. J Surg Oncol. 2005;89(2):99–101. doi: 10.1002/jso.20191. [DOI] [PubMed] [Google Scholar]
- Ibáñez N, Abrisqueta J, Luján J, Hernández Q, Rufete MD, Parrilla P. Isoperistaltic versus antiperistaltic ileocolic anastomosis. Does it really matter? Results from a randomised clinical trial (ISOVANTI) Surg Endosc. 2019;33(9):2850–2857. doi: 10.1007/s00464-018-6580-7. [DOI] [PubMed] [Google Scholar]
- Oveson BC, Bergamaschi R. Twisting in the wind: intracorporeal ileocolic anastomosis. Tech Coloproctol. 2016;20(8):511–512. doi: 10.1007/s10151-016-1492-9. [DOI] [PubMed] [Google Scholar]
- Duan Y, Liu Y, Li Y. Previous Intestinal Resection Is Associated with Postoperative Complications in Crohn's Disease: A Cohort Study. Gastroenterol Res Pract. 2020;2020:2194382. doi: 10.1155/2020/2194382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fazio VW, Marchetti F, Church M, Goldblum JR, Lavery C, Hull TL, et al. Effect of resection margins on the recurrence of Crohn's disease in the small bowel. A randomized controlled trial. Ann Surg. 1996;224(4):563–573. doi: 10.1097/00000658-199610000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The minimal bowel resection in Crohn's disease: analysis of prognostic factors on the surgical recurrence. 2003:627–633. [PubMed] [Google Scholar]
- Lee KE, Cantrell S, Shen B, Faye AS. Post-operative prevention and monitoring of Crohn's disease recurrence. Gastroenterology Report. 2022;10:goac070. doi: 10.1093/gastro/goac070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golda T, Lazzara C, Zerpa C, Sobrino L, Fico V, Kreisler E, et al. Risk factors for ileocolic anastomosis dehiscence; a cohort study. The American Journal of Surgery. 2020;220(1):170–177. doi: 10.1016/j.amjsurg.2019.11.020. [DOI] [PubMed] [Google Scholar]
- Schwegler I, von Holzen A, Gutzwiller JP, Schlumpf R, Mühlebach S, Stanga Z. Nutritional risk is a clinical predictor of postoperative mortality and morbidity in surgery for colorectal cancer. British Journal of Surgery. 2010;97(1):92–97. doi: 10.1002/bjs.6805. [DOI] [PubMed] [Google Scholar]
- Choudhuri AH, Uppal R, Kumar M. Influence of non-surgical risk factors on anastomotic leakage after major gastrointestinal surgery: Audit from a tertiary care teaching institute. International Journal of Critical Illness and Injury Science. 2013;3(4):246. doi: 10.4103/2229-5151.124117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahbari NN, Weitz J, Hohenberger W, Heald RJ, Moran B, Ulrich A, et al. Definition and grading of anastomotic leakage following anterior resection of the rectum: a proposal by the International Study Group of Rectal Cancer. Surgery. 2010;147(3):339–351. doi: 10.1016/j.surg.2009.10.012. [DOI] [PubMed] [Google Scholar]
- Ellis CT, Maykel JA. Defining Anastomotic Leak and the Clinical Relevance of Leaks. Clin Colon Rectal Surg. 2021;34(6):359–365. doi: 10.1055/s-0041-1735265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sciuto A, Merola G, De Palma GD, Sodo M, Pirozzi F, Bracale UM. Predictive factors for anastomotic leakage after laparoscopic colorectal surgery. World J Gastroenterol. 2018;24(21):2247–2260. doi: 10.3748/wjg.v24.i21.2247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipska MA, Bissett IP, Parry BR, Merrie AEH. Anastomotic leakage after lower gastrointestinal anastomosis: men are at a higher risk. ANZ J Surg. 2006;76(7):579–585. doi: 10.1111/j.1445-2197.2006.03780.x. [DOI] [PubMed] [Google Scholar]
- Neary PM, Aiello AC, Stocchi L, Shawki S, Hull T, Steele SR. High-Risk Ileocolic Anastomoses for Crohn’s Disease: When Is Diversion Indicated? J Crohns Colitis. 2019;13(7):856–863. doi: 10.1093/ecco-jcc/jjz004. [DOI] [PubMed] [Google Scholar]
- Crowell KT, Messaris E. Risk factors and implications of anastomotic complications after surgery for Crohn’s disease. World J Gastrointest Surg. 2015;7(10):237–242. doi: 10.4240/wjgs.v7.i10.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eriksen TF, Lassen CB, Gögenur I. Treatment with corticosteroids and the risk of anastomotic leakage following lower gastrointestinal surgery: a literature survey. Colorectal Dis. 2014;16(5):O154–O160. doi: 10.1111/codi.12490. [DOI] [PubMed] [Google Scholar]
- Vasiliu ECZ, Zarnescu NO, Costea R, Neagu S. Review of Risk Factors for Anastomotic Leakage in Colorectal Surgery. Chirurgia (Bucur) 2015;110(4):319–326. [PubMed] [Google Scholar]
- McDermott FD, Heeney A, Kelly ME, Steele RJ, Carlson GL, Winter DC. Systematic review of preoperative, intraoperative and postoperative risk factors for colorectal anastomotic leaks. Br J Surg. 2015;102(5):462–479. doi: 10.1002/bjs.9697. [DOI] [PubMed] [Google Scholar]
- Jeganathan NNA, Koltun WA. Special Considerations of Anastomotic Leaks in Crohn’s Disease. Clin Colon Rectal Surg. 2021;34(6):412–416. doi: 10.1055/s-0041-1735273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujita F, Torashima Y, Kuroki T, Eguchi S. The risk factors and predictive factors for anastomotic leakage after resection for colorectal cancer: reappraisal of the literature. Surg Today. 2014;44(9):1595–1602. doi: 10.1007/s00595-013-0685-3. [DOI] [PubMed] [Google Scholar]
- Paliogiannis P, Deidda S, Maslyankov S, Paycheva T, Farag A, Mashhour A. Blood cell count indexes as predictors of anastomotic leakage in elective colorectal surgery: a multicenter study on 1432 patients. World J Surg Onc. 2020;18(1):89. doi: 10.1186/s12957-020-01856-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damen N, Spilsbury K, Levitt M, Makin G, Salama P, Tan P. Anastomotic leaks in colorectal surgery. ANZ Journal of Surgery. 2014;84(10):763–768. doi: 10.1111/ans.12494. [DOI] [PubMed] [Google Scholar]
- Shin US, Kim CW, Yu CS, Kim JC. Delayed anastomotic leakage following sphincter-preserving surgery for rectal cancer. Int J Colorectal Dis. 2010;25(7):843–849. doi: 10.1007/s00384-010-0938-1. [DOI] [PubMed] [Google Scholar]


