Abstract
Purpose
This study aims to identify the risk factors for the progression from pulmonary tuberculosis (PTB) to spinal tuberculosis (STB), which is crucial for early disease intervention, optimizing treatment strategies, and improving patient prognosis.
Methods
A retrospective analysis was conducted on 326 patients diagnosed with PTB between January 2017 and October 2024. Demographic, clinical, and socioeconomic data were collected, including age, gender, body mass index (BMI), Karnofsky Performance Status (KPS), Nutritional Risk Screening 2002 (NRS-2002) score, diabetes, per capita income, smoking status, alcohol consumption, and a history of recurrent PTB. Univariate and multivariate logistic regression analyses were performed to identify significant risk factors for the progression to STB, and interaction effect analysis and risk stratification based on the NRS-2002 score were conducted to assess its predictive value.
Results
Univariate logistic regression revealed that the NRS-2002 score (OR = 2.762, p < 0.001), recurrent PTB (OR = 15.370, p < 0.001), and living in relative poverty (OR = 10.000, p = 0.002) were significant risk factors for the progression from PTB to STB. Multivariate logistic regression confirmed that the NRS-2002 score (OR = 11.22, p < 0.001), recurrent PTB (OR = 5.08, p < 0.001), and living in relative poverty (OR = 2.58, p < 0.001) were independently associated with increased likelihood of STB progression. Stratified analysis revealed a clear dose-response relationship between higher NRS-2002 scores and the risk of progression to STB, with those having scores ≥ 6 exhibiting the highest odds (OR = 91.59, p < 0.001).
Conclusions
This study highlights critical risk factors for the progression from PTB to STB, particularly the NRS-2002 score, recurrent PTB, and socioeconomic status (living in relative poverty). The NRS-2002 score was identified as the most significant predictor, demonstrating a strong dose-response relationship with disease progression. Clinically, early identification of patients with elevated NRS-2002 scores, alongside timely nutritional interventions and efforts to alleviate poverty, can significantly reduce the risk of STB development. These findings can inform clinical decision-making, enhance early intervention strategies, and guide public health policies aimed at preventing STB, particularly in high-risk populations.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13018-025-05848-3.
Keywords: Pulmonary tuberculosis, Spinal tuberculosis, Logistic regression, Recurrent pulmonary tuberculosis, Risk stratification
Introduction
In 2022, the World Health Organization (WHO) reported approximately 10.6 million new cases of tuberculosis (TB) globally [1]. By 2023, the situation had deteriorated further, with an estimated 10.8 million individuals affected by TB, including 8.2 million newly diagnosed cases—marking the highest incidence recorded since global monitoring began in 1995 [2, 3]. Although TB-related mortality slightly decreased from 1.32 million in 2022 to 1.25 million in 2023, TB continues to be the leading cause of death from a single infectious disease [2–4]. The disease remains highly prevalent in regions such as Southeast Asia, Africa, and the Western Pacific, with countries like India, Indonesia, and China shouldering a disproportionate share of the global burden [2–4].
TB caused by the airborne transmission of Mycobacterium TB, is one of the most prevalent infectious diseases globally [5]. Although the lungs are the primary site of infection for Mycobacterium TB, more than 15% of TB cases worldwide are caused by extrapulmonary infections, which can affect any organ system [6]. TB continues to make a significant contribution to global morbidity and mortality [7], causing over one million deaths annually [8, 9]. Due to anatomical vascular supply, the lower thoracic and upper lumbar vertebrae are commonly affected by TB in the spine [10, 11]. The progression of pulmonary tuberculosis (PTB) to spinal tuberculosis (STB) can lead to a series of complications, including chronic back pain, neurological deficits, and kyphotic deformity. In severe cases, it may result in Pott’s paraplegia [10, 11].
There are various risk factors for the progression of PTB to STB. The presence of comorbidities such as diabetes or immunodeficiency diseases (e.g., HIV) is one of the factors contributing to the progression of PTB [12, 13]. Risk factors for the progression of PTBs to STB include socioeconomic factors such as poverty, overcrowding, and malnutrition, which increase the transmission risk of TB [14, 15]. Demographic factors, including age and household conditions, also play a significant role, particularly in individuals aged 20–64 years [12, 13]. Other health conditions, such as alcoholism, substance abuse, and chronic diseases, can impair the immune system, thereby increasing the risk of STB [14, 15].
Nevertheless, the analysis of risk factors for the progression of PTB to STB in existing studies remains limited, particularly in terms of in-depth exploration of specific risk factors such as the Nutritional Risk Screening 2002 (NRS-2002) score. Investigating the identification of risk factors is crucial for early disease intervention, optimizing treatment strategies, and improving patient prognosis. Furthermore, analyzing such studies holds potential value for the formulation of TB control and prevention policies. This study aims to identify the risk factors for the progression of PTB to STB through logistic regression analysis, with a particular focus on risk stratification using the NRS-2002 score, to explore its predictive value in disease progression.
Methods
Patient population
After obtaining approval from the institutional review board, a retrospective analysis was conducted on the demographic and imaging data of patients diagnosed with PTB who visited the outpatient clinic from January 2017 to October 2024. Informed consent was obtained from all participants prior to their inclusion in the study. Diagnosis was confirmed through a comprehensive review of medical records and imaging data. The inclusion criteria were as follows: patients with a confirmed diagnosis of PTB, and the ability to collect the following variables: age, gender, body mass index (BMI), Karnofsky Performance Status (KPS) score, NRS-2002 score (Supplementary Table 1), diabetes, per capita income, history of recurrent PTB, smoking status, alcohol consumption, and family history of TB. Specifically, per capita income, defined as living in relative poverty, refers to an individual’s income being below 60% of the median income in the general population [16]. Smoking was defined as as someone who has smoked at least 100 cigarettes in their lifetime and currently smokes, whether daily or occasionally [17]. The definition of “moderate drinking” provided by the Centers for Disease Control and Prevention (CDC) generally refers to up to 2 alcoholic beverages per day for men and up to 1 alcoholic beverage per day for women.
Patients with incomplete data or insufficient imaging information were excluded from the study. The methodology employed in this study involved a retrospective analysis, with logistic regression used to identify potential factors associated with the progression from PTB to STB among the outpatient cohort.
Statistical analysis
Since the progression of PTB to STB is a binary outcome, we initially applied univariate logistic regression to identify potential risk factors (p < 0.05). Subsequently, multivariate logistic regression was performed to further pinpoint significant risk factors while adjusting for potential confounders. To explore potential interaction effects among variables, an interaction effect analysis was conducted. Additionally, we performed risk stratification analysis on the most prominent risk factors. All statistical analyses were carried out using R software (R version 4.3.3), with a p-value of < 0.05 considered statistically significant.
Results
Patient demographics
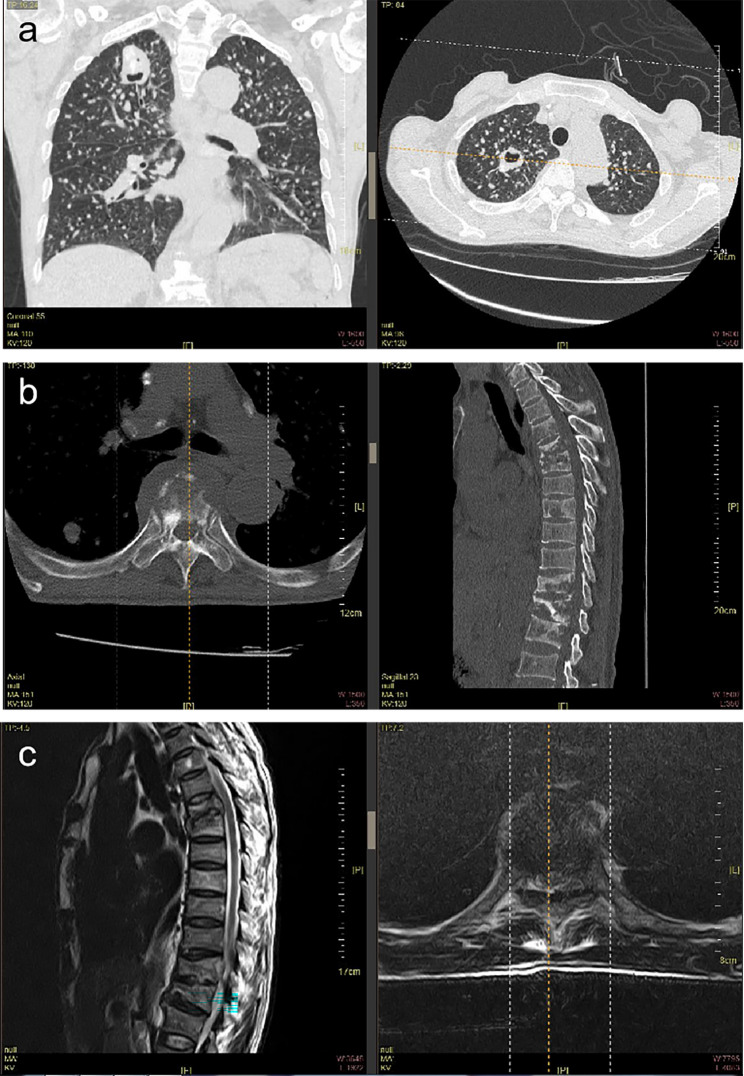
A total of 326 PTB patients were identified (see Table 1), with a mean age of 56.5 ± 15.8 years (range, 16–84). Among these, 16 were diagnosed with STB (Fig. 1). The mean BMI of the cohort was 17.2 ± 0.8. The average KPS score was 50.8 ± 12.1, indicating a moderate level of functional impairment. The mean NRS-2002 score was 2.0 ± 1.7, reflecting the nutritional risk of the patients.
Table 1.
Baseline demographics of 326 outpatients with pulmonary tuberculosis
| Variables | Total(n = 326) |
|---|---|
| 1. Demographic Factors | |
| Age | 56.5 ± 15.8 (range, 16–84) |
| Gender | |
| Male | 202 |
| Female | 124 |
| 2. Clinical Factors | |
| BMI | 17.2 ± 0.8 |
| KPS score | 50.8 ± 12.1 |
| NRS−2002 score | 2.0 ± 1.7 |
| Diabetes | |
| Yes | 46 |
| No | 280 |
| Recurrent Pulmonary Tuberculosis | |
| Yes | 33 |
| No | 293 |
| 3. Socioeconomic and Lifestyle Factors | |
| Per Capita Income (living in relative poverty) | |
| Yes | 10 |
| No | 316 |
| Having a Family Member with Tuberculosis | |
| Yes | 9 |
| No | 317 |
| Smoking | |
| Yes | 193 |
| No | 133 |
| Alcohol Consumption | |
| Yes | 30 |
| No | 296 |
BMI, body mass index; KPS score, Karnofsky Performance Status Score; NRS-2002 score, Nutritional Risk Screening 2002 score
Per Capita Income (living in relative poverty) refers to an individual’s income being below 60% of the median income in society
Smoking was defined as someone who has smoked at least 100 cigarettes in their lifetime and currently smokes, whether daily or occasionally. “Moderate drinking” refers to up to 2 alcoholic beverages per day for men and up to 1 alcoholic beverage per day for women
Fig. 1.
Radiological data of a 65-year-old male patient with pulmonary tuberculosis progressing to spinal tuberculosis. a, b) CT scan images; c) MRI scan image.
Regarding medical history, 33 patients had a history of recurrent PTB, while 293 did not. In terms of socioeconomic and lifestyle factors, 10 patients were classified as living in relative poverty, with a per capita income below 60% of the median national income, whereas 316 patients did not meet this criterion. A family history of TB was reported by 9 patients, while 317 patients did not have a family history of the disease. Smoking was reported by 193 patients, and 133 patients were non-smokers. Alcohol consumption was noted in 30 patients, while 296 patients did not consume alcohol regularly.
Notably, a total of 16 patients progressed from PTB to STB. The mean age was 54.5 ± 9.6 years (range, 40–70). Among them, one patient had comorbid systemic lupus erythematosus and had been maintained on low-dose glucocorticoid therapy for two years. Another patient was diagnosed with rheumatoid arthritis and received nonsteroidal anti-inflammatory drugs (NSAIDs) for symptomatic management over a two-year period without additional immunosuppressive treatment. None of the 16 patients demonstrated characteristics of multidrug-resistant tuberculosis (MDR-TB).
Univariate logistic regression analysis results
Univariate logistic regression was performed to identify factors associated with the progression from PTB to STB. The results are summarized in Table 2. Among the demographic factors, age and gender did not show a statistically significant association with the progression to STB (p > 0.05). Similarly, clinical factors such as BMI, KPS score, diabetes and the NRS-2002 score were assessed. While BMI, diabetes and KPS score did not exhibit a significant relationship with STB progression, the NRS-2002 score was found to be strongly associated with an increased likelihood of progression (OR = 2.762, p < 0.001). In terms of medical history, a history of recurrent PTB was found to be a significant risk factor, with an odds ratio of 15.370 (p < 0.001), suggesting that patients with recurrent PTB are significantly more likely to develop STB. Among the socioeconomic and lifestyle factors, per capita income (living in relative poverty) was also found to be a significant risk factor for the progression to STB (OR = 10.000, p = 0.002). In contrast, having a family member with TB, smoking, and alcohol consumption did not show significant associations with the progression to STB (p > 0.05).
Table 2.
Univariate logistic regression analysis of factors associated with the progression to spinal tuberculosis
| Variables | Estimate | Odds ratio | Std.Error | z value | Pr ( >|z| ) |
|---|---|---|---|---|---|
| 1. Demographic Factors | |||||
| Age | -0.012 | 0.987 | 0.016 | -0.745 | 0.457 |
| Gender (male) | 0.315 | 1.371 | 0.5519 | 0.571 | 0.568 |
| 2. Clinical Factors | |||||
| BMI | 0.332 | 1.393 | 0.235 | 1.414 | 0.157 |
| KPS score | -0.0018 | 0.998 | 0.0212 | -0.085 | 0.932 |
| NRS−2002 score | 1.016 | 2.762 | 0.19 | 5.335 | < 0.001 |
| Diabetes | -0.9350 | 0.3924 | 1.0453 | -0.894 | 0.371 |
| Recurrent Pulmonary Tuberculosis | 2.729 | 15.370 | 0.547 | 4.990 | < 0.001 |
| 3. Socioeconomic and Lifestyle Factors | |||||
| Per Capita Income (living in relative poverty) | 2.302 | 10.000 | 0.746 | 3.085 | 0.002 |
| Having a Family Member with Tuberculosis | 0.923 | 2.517 | 1.093 | 0.844 | 0.399 |
| Smoking | -0.392 | 0.676 | 0.513 | -0.764 | 0.445 |
| Alcohol Consumption | -0.437 | 0.646 | 1.051 | -0.416 | 0.678 |
BMI, body mass index; KPS score, Karnofsky Performance Status Score; NRS-2002 score, Nutritional Risk Screening 2002 score
Multivariate logistic regression analysis results
To further identify independent risk factors for the progression from PTB to STB, a multivariate logistic regression analysis was performed, adjusting for potential confounders (Table 3). The results revealed that three factors were independently associated with an increased likelihood of progression to STB: NRS-2002 score: The NRS-2002 score remained a strong predictor of progression, with an OR of 11.22 (p < 0.001). Patients with a higher NRS-2002 score are over 11 times more likely to develop STB compared to those with a lower score. Recurrent PTB: A history of recurrent PTB was also found to be an independent risk factor, with an odds ratio of 5.08 (p < 0.001). This suggests that patients with recurrent PTB are over five times more likely to develop STB compared to those without a history of recurrence. Per Capita Income (living in relative poverty): Patients living in relative poverty, with a per capita income below 60% of the median national income, had a significantly higher risk of progression to STB (OR = 2.58, p < 0.001).
Table 3.
Multivariate logistic regression analysis of factors associated with the progression to spinal tuberculosis
| Variables | Estimate | Odds ratio | Std.error | Statistic | P value |
|---|---|---|---|---|---|
| (Intercept) | -6.925 | / | 1.03 | -6.72 | < 0.001 |
| NRS−2002 score | 2.419 | 11.22 | 0.676 | 3.581 | < 0.001 |
| Recurrent Pulmonary Tuberculosis | 1.623 | 5.08 | 1.078 | 1.506 | < 0.001 |
| Per Capita Income (living in relative poverty) | 0.947 | 2.58 | 0.208 | 4.562 | < 0.001 |
NRS-2002 score, Nutritional Risk Screening 2002 score
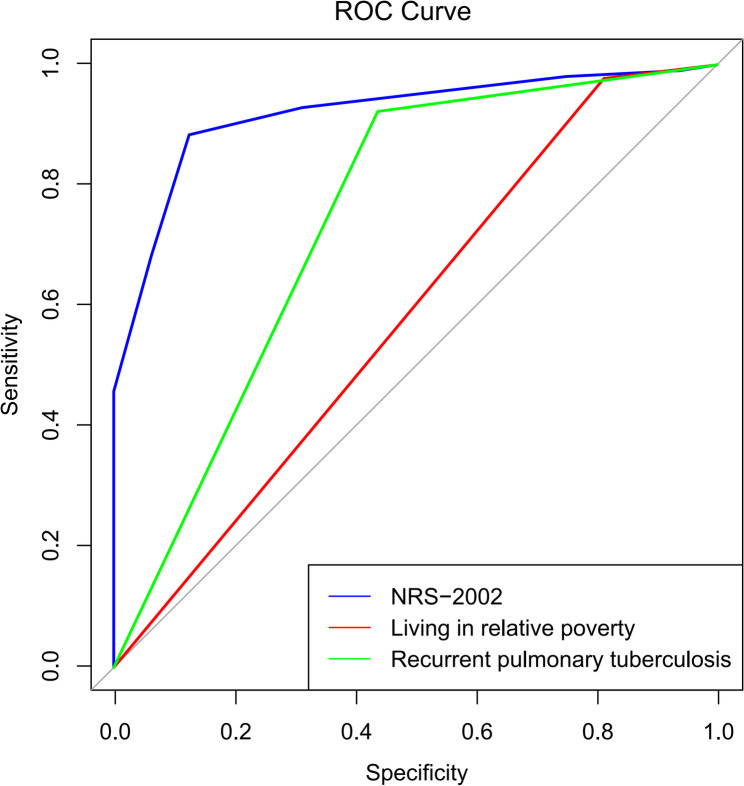
We performed ROC curve analysis to validate the diagnostic efficacy of the NRS-2002 score, recurrent PTB, and living in relative poverty (Fig. 2). All three factors demonstrated diagnostic utility, with the NRS-2002 score showing the highest diagnostic effectiveness.
Fig. 2.
ROC curve
Interaction effect analysis and stratified analysis
To examine potential interaction effects between significant risk factors, interaction terms were incorporated into the multivariate logistic regression model (Table 4). The analysis revealed no significant interactions between the NRS-2002 score and recurrent PTB (p = 0.883), the NRS-2002 score and per capita income (p = 0.337), or recurrent PTB and per capita income (p = 0.992). These findings suggest that the influence of each factor on the progression to STB is independent of the others.
Table 4.
Analysis of interaction effects in the multivariate logistic regression model
| Variables | Estimate | Std.Error | z value | Pr( >|z| ) |
|---|---|---|---|---|
| NRS−2002 score: Recurrent pulmonary tuberculosis | 0.072 | 0.488 | 0.147 | 0.883 |
| NRS−2002 score: Per capita income | −0.599 | 0.624 | −0.96 | 0.337 |
| Recurrent pulmonary tuberculosis: Per capita income | 15.498 | 1696.735 | 0.009 | 0.992 |
NRS-2002 score, Nutritional Risk Screening 2002 score
To further investigate the impact of the NRS-2002 score on the progression to STB, a stratified analysis was performed (Table 5). The results demonstrated a clear dose-response relationship between the NRS-2002 score and the odds of progression (with a baseline defined as an NRS-2002 score of 0–3): For patients with an NRS-2002 score of 4–5, the odds of progression were significantly elevated, with an odds ratio (OR) of 45.98 (p < 0.001). For those with an NRS-2002 score ≥ 6, the odds of progression further increased, with an OR of 91.59 (p < 0.001).
Table 5.
Stratified analysis of the effect of NRS-2002 score on the progression to spinal tuberculosis
| NRS−2002 score | Estimate | Odds ratio | Std.Error | P value |
|---|---|---|---|---|
| 0–3 (baseline) | −4.920 | 0.007 | 0.710 | < 0.001 |
| 4–5 | 3.821 | 45.980 | 0.798 | < 0.001 |
| ≥ 6 | 4.515 | 91.590 | 0.959 | < 0.001 |
NRS-2002 score, Nutritional Risk Screening 2002 score
These findings underscore that a higher NRS-2002 score is strongly associated with an increased risk of progression from PTB to STB, with the risk escalating sharply as the score threshold rises.
Discussion
Statement of principal findings
We performed logistic regression analysis on the baseline data of 326 patients with PTB, adjusting for potential confounders. The results from the multivariate logistic regression identified three primary risk factors associated with the progression from PTB to STB: the NRS-2002 score, recurrent PTB, and per capita income (living in relative poverty). The NRS-2002 score emerged as the most significant predictor of progression, with patients at higher nutritional risk (as indicated by a higher NRS-2002 score) being more than 11 times more likely to develop STB compared to those with lower scores. This underscores the critical role of nutritional status in disease progression. A history of recurrent PTB was identified as a substantial risk factor, with individuals who had experienced recurrent episodes of PTB being over five times more likely to develop STB. Patients with a per capita income below 60% of the median national income, classified as living in relative poverty, were found to be at a significantly higher risk of progressing to STB. These findings highlight the substantial impact of nutritional status, disease recurrence, and socioeconomic factors in the progression from PTB to STB.
NRS-2002 score is a widely utilized tool designed to assess the risk of malnutrition in hospitalized patients [18, 19]. The NRS-2002 score is derived from three main components: (1) Nutritional Status: This is assessed based on BMI, recent weight loss, and food intake over the past week. (2) Severity of Disease: This factor takes into account the increased nutritional needs arising from recent medical conditions or treatments (e.g., surgeries, chronic illnesses). (3) Age Adjustment: An additional point is added for patients aged 70 years or older [19–21]. The total score ranges from 0 to 7, where: 0–3 indicates a low risk of malnutrition, 4–7 suggests a moderate to severe risk of malnutrition [18, 20, 21].
When we performed a stratified analysis of the NRS-2002 score (Table 5), we found that the risk of developing STB in patients with an NRS-2002 score of 4–5 was 46 times higher compared to the baseline group with a score of 0–3. Furthermore, patients with an NRS-2002 score of ≥ 6 had a risk that was 92 times higher than the baseline group.
Comparison with previous studies
Individuals with a history of TB are at an increased risk of recurrence [22, 23]. This is consistent with our findings, as individuals with recurrent PTB are at a higher risk of developing STB. Studies have reported that younger individuals, particularly those in the 25–44 age group, exhibit an elevated risk of recurrence [23, 24]. However, age was not found to be a significant risk factor in our study. Some studies have also identified inadequate supervision during treatment as a risk factor, particularly in cases of poor adherence to prescribed regimens [22, 24]. Our findings support this conclusion. Per Capita Income (living in relative poverty) was identified as a risk factor for the progression of PTB to STB in this study. We hypothesize that poverty, coupled with poor living conditions and long-term malnutrition, increases susceptibility to PTB. Additionally, limited access to educational resources may lead to poorer treatment adherence among these patients, potentially contributing to recurrence.
Clinical significance
Our study highlights the critical role of the NRS-2002 score, recurrent PTB, and per capita income (living in relative poverty) as significant risk factors for the progression from PTB to STB. Among these, the NRS-2002 score stands out as the most impactful predictor, indicating that nutritional status plays a crucial role in the progression of TB. This is clinically significant, as it suggests that early identification and management of malnutrition in PTB patients could serve as a preventive strategy to reduce the risk of developing STB, particularly in those with moderate to high NRS-2002 scores.
Additionally, our findings that a history of recurrent PTB and living in relative poverty are associated with a higher risk of progression underscore the importance of addressing both medical and socioeconomic factors in TB management. These findings could inform healthcare policies, leading to improved TB control strategies that incorporate nutritional support and targeted interventions for individuals with a history of recurrent TB or those living in poverty.
Limitations
Despite the strengths of our study, there are several limitations that should be considered. Firstly, the retrospective design of this study means that causal inferences cannot be made. The identification of risk factors is based on existing clinical records, which may have led to potential biases in data collection and interpretation. This limitation may have affected the robustness of the findings, as retrospective studies are more prone to information bias, selection bias, and recall bias. Additionally, we could not control for all confounders that might influence the progression from PTB to STB, and some relevant factors may have been overlooked. Future prospective studies with a more comprehensive data collection approach could help mitigate these issues and provide stronger evidence on the risk factors identified. Another limitation of this study is the relatively small number of patients who progressed to STB among the 326 patients with PTB. With only 16 cases of progression to STB, the statistical power of the multivariate analysis was limited, which may have affected the reliability of the findings. Although we performed rigorous statistical analysis, including univariate and multivariate logistic regression, the small sample size for the STB group means that the estimates for risk factors, particularly for rarer outcomes, may be less precise. The low number of STB cases also restricts the ability to detect more subtle associations or interactions between variables that might exist. As such, we recommend that future studies with larger sample sizes are needed to confirm these findings and provide more definitive conclusions. Another limitation is the reliance on medical records and self-reported data for variables such as smoking, alcohol consumption, and family history of TB, which may have introduced recall bias or inaccuracies. Moreover, the NRS-2002 score was used to assess nutritional risk, but it does not capture the full complexity of nutritional status, including factors like micronutrient deficiencies or protein-energy malnutrition, which could further influence disease progression.
Conclusion
This study provides clear evidence that the NRS-2002 score, recurrent PTB, and socioeconomic factors (such as living in relative poverty) are significant predictors of the progression from PTB to STB. The NRS-2002 score emerged as the most important predictor, demonstrating a pronounced dose-response relationship with disease progression. These findings have important practical implications for clinical practice: healthcare providers should prioritize the early screening of PTB patients, especially those with high nutritional risk (high NRS-2002 score), a history of recurrent PTB, and low socioeconomic status. Implementing targeted nutritional interventions, alongside efforts to improve living conditions, could significantly reduce the risk of STB development. Furthermore, these results can contribute to the design of more efficient TB control strategies, tailored to address both clinical and socioeconomic vulnerabilities, potentially improving patient outcomes and reducing the burden of TB-related complications.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1: Table 1. NRS-2002 score.
Author contributions
Di Xue, Xue Lin, Xiaolei Chen and Yiqiang Yang participated in the conception and design of the study. All authors read and agreed to the final manuscript and authorship arrangement.
Funding
This study was supported by the National Natural Science Foundation of China Project (82360319); the project of the Central Government guiding local scientific and technological development (2024FRD05048); the Ningxia Natural Science Foundation Project (2024AAC03663, 2024AAC03601); the State Key Laboratory of Pathogenesis, Prevention and Treatment of High Incidence Diseases in Central Asia Fund (SKL-HIDCA-2024-26); the Key Research and Development Program of Ningxia Hui Autonomous Region (2022BEG03126, 2022BEG03169) and the Ningxia Natural Science Foundation Project (2024AAC03665).
Data availability
The raw data supporting the conclusion of this article will be made available on request.
Declarations
Ethics approval and consent to participate
This study was approved by the the Ethics Committee of General Hospital of Ningxia Medical University (KYLL-2024-1633). Informed consent to participate was obtained from all participants prior to their inclusion in the study.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Di Xue and Xiaolei Chen are co-first authors.
Contributor Information
Yiqiang Yang, Email: 18895014581@163.com.
Xue Lin, Email: Lx54257@126.com.
References
- 1.Bagcchi S. WHO’s global tuberculosis report 2022. Lancet Microbe. 2023;4:e20. [DOI] [PubMed] [Google Scholar]
- 2.Farhat MR, Jacobson KR. For tuberculosis, not to screen or not to screen? But who?? And how?? Clin Infect Dis. 2024;78:1677–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO consolidated guidelines on tuberculosis: Module 1: Prevention– Tuberculosis preventive treatment, second edition. 2024. Geneva. [PubMed]
- 4.Goletti D, Meintjes G, Andrade BB, Zumla A, Shan Lee S. Insights from the 2024 WHO global tuberculosis Report - More comprehensive action, innovation, and investments required for achieving WHO end TB goals. Int J Infect Dis. 2025;150:107325. [DOI] [PubMed] [Google Scholar]
- 5.Furin J, Cox H, Pai M, Tuberculosis. Lancet. 2019;393(10181):1642–56. 10.1016/S0140-6736(19)30308-3. [DOI] [PubMed] [Google Scholar]
- 6.Behr MA, Edelstein PH, Ramakrishnan L. Revisiting the timetable of tuberculosis. BMJ. 2018;362:k2738. 10.1136/bmj.k2738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. 10.1016/S0140-6736(20)30925-9 [DOI] [PMC free article] [PubMed]
- 8.Global regional. National sex differences in the global burden of tuberculosis by HIV status, 1990–2019: results from the global burden of disease study 2019. Lancet Infect Dis. 2022;22(2):222–41. 10.1016/S1473-3099(21)00449-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Global regional, national burden of tuberculosis. 1990–2016: results from the global burden of diseases, injuries, and risk factors 2016 study. Lancet Infect Dis. 2018;18(12):1329–49. 10.1016/S1473-3099(18)30625-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leowattana W, Leowattana P, Leowattana T. Tuberculosis of the spine. World J Orthop. 2023;14(5):275–93. 10.5312/wjo.v14.i5.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mann TN, Davis JH, Walzl G, et al. Candidate biomarkers to distinguish spinal tuberculosis from mechanical back pain in a tuberculosis endemic setting. Front Immunol. 2021;12:768040. 10.3389/fimmu.2021.768040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zheng BW, Liu FS, Zheng BY, et al. Risk factors for tuberculous or nontuberculous spondylitis after percutaneous vertebroplasty or kyphoplasty in patients with osteoporotic vertebral compression fracture: A case-control study. Front Surg. 2022;9:962425. 10.3389/fsurg.2022.962425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Glassman I, Nguyen KH, Giess J, Alcantara C, Booth M, Venketaraman V, Pathogenesis. Diagnostic challenges, and risk factors of Pott’s disease. Clin Pract. 2023;13(1):155–65. 10.3390/clinpract13010014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jiang G, Du X, Zhu Y, et al. Value of postoperative serum albumin to predict postoperative complication severity in spinal tuberculosis. Biomed Res Int. 2022;2022:4946848. 10.1155/2022/4946848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kang JH, Lin HC. Comorbidity profile of poliomyelitis survivors in a Chinese population: a population-based study. J Neurol. 2011;258(6):1026–33. 10.1007/s00415-010-5875-y. [DOI] [PubMed] [Google Scholar]
- 16.Yang Y, Zhou L, Zhang C, Luo X, Luo Y, Wang W. Public health services, health human capital, and relative poverty of rural families. Int J Environ Res Public Health. 2022;19:11089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leone A, Landini L, Leone A. What is tobacco smoke? Sociocultural dimensions of the association with cardiovascular risk. Curr Pharm Des. 2010;16:2510–7. [DOI] [PubMed] [Google Scholar]
- 18.Chen X, Li D, Liu Y, Zhu L, Jia Y, Gao Y. Nutritional risk screening 2002 scale and subsequent risk of stroke-associated infection in ischemic stroke: the REMISE study. Front Nutr. 2022;9:895803. 10.3389/fnut.2022.895803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kroc Ł, Fife E, Piechocka-Wochniak E, Sołtysik B, Kostka T. Comparison of nutrition risk screening 2002 and subjective global assessment form as short nutrition assessment tools in older hospitalized adults. Nutrients. 2021;13(1):225. 10.3390/nu13010225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stello BB, Cattani A, Milanez D, Razzera EL, Lima J, Silva FM. Prognostic value of different cut-off points of the NRS-2002 tool to identify nutritional risk in critically ill patients: a longitudinal study. Br J Nutr. 2023;130(8):1357–65. 10.1017/S0007114523000363. [DOI] [PubMed] [Google Scholar]
- 21.Zhu M, Zha Y, Cui L, et al. Assessment of nutritional risk scores (the nutritional risk screening 2002 and modified nutrition risk in critically ill scores) as predictors of mortality in critically ill patients on extracorporeal membrane oxygenation. ASAIO J. 2024;70(6):510–6. 10.1097/MAT.0000000000002142. [DOI] [PubMed] [Google Scholar]
- 22.Cudahy P, Wilson D, Cohen T. Risk factors for recurrent tuberculosis after successful treatment in a high burden setting: a cohort study. BMC Infect Dis. 2020;20(1):789. 10.1186/s12879-020-05515-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li T, Zhang B, Du X, Pei S, Jia Z, Zhao Y. Recurrent pulmonary tuberculosis in China, 2005 to 2021. JAMA Netw Open. 2024;7(8):e2427266. 10.1001/jamanetworkopen.2024.27266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vega V, Cabrera-Sanchez J, Rodríguez S, et al. Risk factors for pulmonary tuberculosis recurrence, relapse and reinfection: a systematic review and meta-analysis. BMJ Open Respir Res. 2024;11(1):e002281. 10.1136/bmjresp-2023-002281. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material 1: Table 1. NRS-2002 score.
Data Availability Statement
The raw data supporting the conclusion of this article will be made available on request.