Abstract
Objective
To assess the effectiveness of community–home patient-centred care (PCC) in the self-management of type 2 diabetes using a systematic evaluation approach.
Methods
This systematic review and meta-analysis adhered to the PRISMA 2020 guideline. The PubMed, Excerpta Medica Database, Cochrane Library, Web of Science, Chinese Biomedical Literature Database, Chinese Periodicals Full Text Database, CQVIP Chinese Journals Platform and Wanfang databases were searched between database inception and February 2025, with no language limit, using keywords related to type 2 diabetes, PCC and self-management. References of the included studies were reviewed, and citation tracking was used. Eligible studies were English or Chinese peer-reviewed randomised controlled trials (RCTs) involving patients with type 2 diabetes, with PCC applied in the trial group and routine care in the control group, focusing on self-management outcomes. Two reviewers independently screened and extracted data, resolving disagreements through a third reviewer. The Cochrane risk assessment tool was used to assess study quality, with Review Manager 5.3 software used to analyse data using mean difference (MD) and 95%CI via a random-effects model. Heterogeneity was tested, and sensitivity analysis and funnel plots were also used.
Results
A total of 18 RCTs were included, including 6 Chinese and 12 English studies, with 1,893 patients with type 2 diabetes followed up in this study. Following intervention for at least 6 months, compared with routine treatment, PCC reduced fasting blood glucose (FBG) (MD = − 1.27, 95%CI: [− 2.19, − 0.74], I2 = 34%, fixed-effect model) and 2-hour postprandial blood glucose (2hPG) (MD = − 0.76, 95%CI: [− 1.23,−0.28], I2 = 81%, random-effects model), but there was no improvement in body mass index (BMI) (MD = − 0.59, 95%CI: [− 1.31, − 0.13], I2 = 0%, fixed-effect model) or foot care (MD = − 1.51, 95%CI: [− 2.17, − 5.19], I2 = 94%, random-effects model). After 3 months of intervention, compared with the routine treatment, PCC decreased glycosylated haemoglobin A1c (HbA1c) levels (MD = − 0.60, 95%CI: [− 0.88, − 0.32], I2 = 81%, random-effects model), but the BMI did not decrease significantly (MD = − 0.26, 95%CI: [− 1.46, − 0.93], I2 = 0%, fixed-effect model).
Conclusion
Compared with routine nursing, community–home PCC nursing can reduce the levels of FBG, 2-hour plasma glucose (2hPG) and glycated haemoglobin A1c (HbA1c) in patients with type 2 diabetes. A unified PCC protocol could help patients with diabetes control the disease.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12913-025-12539-6.
Keywords: Type 2 diabetes, Patient-centred care, Self-management, Meta-analysis
Introduction
With socio-economic development and aging populations, chronic non-communicable diseases have become the main cause of death, and diabetes, as the third major chronic disease after cardiovascular diseases and tumours, poses a serious threat to the health of the population. In recent years, the situation of diabetes mellitus in China has been bleak, with the number of patients with diabetes reaching 114 million, accounting for one-third of the total number of such patients globally. Furthermore, the prevalence rate continues to grow at an accelerated rate, with type 2 diabetes mellitus, as the main type of the disease, accounting for 90% of the total [1]. Worldwide, diabetes is expected to affect 783.2 million people aged 20–79 years by 2045 [2]. Statistics from the 10th edition of the International Diabetes Federation’s Diabetes Map show that diabetes was responsible for 6.7 million deaths globally in 2021, an average of one death every 5 s, with approximately one-third (32.6%) of all diabetes deaths occurring at less than 60 years of age [2]. Moreover, diabetes contributes to at least US$966 billion in health expenditure globally, an increase of 316% over the past 15 years [2]. China ranks second globally in terms of diabetes health expenditure, indicating an extremely serious situation [3].
As a lifelong chronic metabolic disease, diabetes mellitus mainly occurs due to defective insulin secretion and/or insulin action disorder, and can be divided into type 1 diabetes mellitus, type 2 diabetes mellitus, special types of diabetes mellitus and gestational diabetes mellitus, with type 2 being the dominant type [4]. Type 2 diabetes mellitus is caused by a variety of factors, such as the environment, lifestyle and genetics, and the cause of the disease is complex and difficult to cure [5].
The improvement in the quality of life of patients with diabetes largely depends on the improvement of their self-management ability [5]. Effective self-management of diabetes mellitus is an important way for patients with diabetes to maintain their own health [6]. The self-management of diabetes encompasses a series of reasonable integrated strategies to improve the patient’s confidence in the treatment, improve their quality of life and reduce the risk of complications, which generally includes compliance with medication, regular exercise, dietary control, monitoring of blood glucose and foot care, as well as other aspects focused on the patient’s actions. Health education among the relevant staff can help patients resolve a variety of physical and emotional problems caused by diabetes [7–9]. According to the literature [10], a series of self-management behaviours adopted by patients with diabetes, such as adherence to medication, management of emotions, improvement of lifestyle and management of complications, have been shown to be effective in improving the rate of glycaemic control, reducing cardiovascular risk and decreasing the incidence of diabetic complications [11].
In addition, there are many risk factors for type 2 diabetes, mainly including behavioral or social factors. Patient-centred care (PPC) is based on numerous principles. In biomedicine, blood sugar is regulated and complications are prevented through reasonable diet, exercise and medication, while in psychological terms, the approach involves improving patients’ cognition and mentality and enhancing treatment compliance. Sociologically, with the support of family and community, health promotion activities are conducted to enhance patients’ self-management ability. The approach is considered to be the new direction of medical care, and its patient-centred feature involves paying attention to patients and respecting them by using the model of a biopsychosocial viewpoint. Patient-centred care requires effective patient engagement, targeted individual care plans and patient motivation to adopt self-management behaviours [12]. Thus, PCC has been described as a new model of care tailored to the specific needs, values and preferences of patients [13], and is an important factor in the self-management of patients with type 2 diabetes, one associated with improved quality of life and self-care behaviours [14]. In its consensus report, the American Diabetes Association also advocates PCC to promote patient participation in self-care activities for self-management of type 2 diabetes [15]. Furthermore, community–home care is more likely to increase the continuity of and adherence to management.
Therefore, this study conducts a meta-analysis of randomised control trials (RCTs) examining the effect of community–home PCC on the self-management of patients with type 2 diabetes mellitus to objectively and comprehensively evaluate the effect of the approach in this regard. The aim is to provide evidence-based guidelines for the development of scientific and effective clinical measures to care for such patients.
Materials and methods
Literature search
In compliance with the PRISMA 2020 statement [16], computer searches were performed on PubMed, the Excerpta Medica Database, The Cochrane Library, Web of Science, the Chinese Biomedical Database(CBM), the China National Knowledge Infrastructure(CNKI), the Chinese Journals Platform(CQVIP) and the Wanfang Data Knowledge Service Platform(WANFANG). The search time was limited to the period between the establishment of the database and February 2025 without limiting the language. The database search strategy included the following keywords: ‘diabetes mellitus’ AND ‘type 2 diabetes’ OR ‘Type II Diabetes’ AND ‘Patient-Centered-Care’ OR ‘Person-Oriented-Care’ OR ‘Holistic Care’ OR ‘Self-Management’ OR ‘Self-Care’ AND ‘Community’ OR ‘Home’ AND ‘HbAlc’ OR ‘Self-Care Behaviours’ OR ‘Self-Care Activities’. In addition, the target literature was obtained by reviewing the references of the included studies. Additionally, target articles were obtained by reviewing references from included studies. Contact experts and researchers in related fields as much as possible by telephone or email to find unpublished literature (see Supplementary Materials).
Inclusion and exclusion criteria
The inclusion criteria were as follows: (1) studies published in peer-reviewed journals in English and Chinese; (2) the study population was patients with type 2 diabetes; (3) PCC was applied in the trial group; (4) routine care was applied in the control group; and (5) the result of interest was that the self-disease management indicators of patients with type 2 diabetes include fasting plasma glucose (FPG), 2-hour plasma glucose (2hPG), glycated haemoglobin A1c (HbA1c), body mass index (BMI) or evaluation of foot care in nursing activity summary (using the SDSCA measure); and (6) the study type was an RCT.
The exclusion criteria included (1) the trial group implemented care other than PCC care in community families; (2) study type was conference article, case report or systematic review; (3) inadequate information on outcomes and inability to analyse the data; (4) duplicate reports; and (5) studies for which complete articles were not available.
Literature screening and data extraction
Literature screening was conducted by two researchers individually based on the inclusion and exclusion criteria. Initial screening was first performed by reading the titles and abstracts of the literature before studies that might meet the inclusion criteria were read in full. When a disagreement between the two researchers was encountered, a third researcher was consulted and a discussion was held to reach a consensus. Following the literature screening, data extraction was conducted by two researchers independently according to the standard data extraction form developed. The extracted information included literature information, basic information about the study participants, intervention methods, follow-up time and outcome indicators.
Quality assessment
The Cochrane Collaboration Network Risk Assessment Tool [17] was used for quality assessment. The quality of the literature was evaluated in terms of random allocation methods, allocation scheme concealment, blinding, completeness of outcome data, selective reporting of findings and other sources of bias.
Methods of statistical analyses
Data were analysed using Review Manager 5.3 software. Measures were expressed using mean difference (MD), and 95% confidence intervals (CIs) were used to estimate the range of intervals for effect sizes. As random-effects models are more conservative than fixed-effect models, the former was mainly used to address the possibility of potential differences in effects across studies and populations [18]. Heterogeneity was tested using the Q test and the I2 statistic to determine the presence and magnitude of heterogeneity, and good homogeneity between included studies was considered if I2 ≤ 50% or P ≥ 0.05. The test level was set at 0.05 unless otherwise stated. The one-by-one exclusion method was employed for sensitivity analysis and funnel plots were used to evaluate publication bias.
Results
Basic characteristics of the included studies
After searching publicly available electronic databases, a total of 1893 studies were included in the literature review process, as shown in Fig. 1. After excluding 1077 duplicate studies and 564 irrelevant studies, a total of 252 articles were included in the full-text review process. After reading the full text and screening the full text according to the inclusion and exclusion criteria of this study, a total of 18 [19–36] eligible studies were thus finally included. Published between 2009 and 2022, there were 6 Chinese and 12 English articles, with the research sites from 9 countries, including the United States, China, Denmark and Iran. The 18 studies involved 1,893 patients with type 2 diabetes. See Table 1 for details.
Fig. 1.
Literature screening flow chart
Table 1.
Basic characteristics of eiligible studies
| Study | Country | Study design | Number of follow-up cases | Intervention | Length of follow up (Month) | Outcome index | ||
|---|---|---|---|---|---|---|---|---|
| Basic theory | Mode of delivery | Provider | ||||||
| Zhou Lidan, 2022 [ 19 ] | China | RCT | 100 | NA | Online | Nurse | 3 | FPG, 2 hPG, HbA1c |
| Shi Jieyun, 2021 [ 20 ] | China | RCT | 86 | NA | Face to face | Nurse, Physician | NA | FPG, 2 hPG, HbA1c |
| Li Yuanxiang, 2019 [ 21 ] | China | RCT | 120 | NA | Face to face, Online | Nurse | 6 | FPG, 2 hPG, HbA1c |
| Li Yanfen, 2016 [ 22 ] | China | RCT | 60 | the theory of health education | Face to face, Online, and Telephone | Nurses and family members | 6 | HbA1c |
| Fikadu BH, 2019 [ 23 ] | Norway | RCT | 142 | NA | Face to face | Nurse | 9 | Foot care |
| Li Shuqin, 2014 [ 24 ] | China | RCT | 84 | NA | Face to face, Telephone | Nurse and Psychologist | 6 | HbA1c |
| Hailu FB, 2018 [ 25 ] | Norway | RCT | 142 | NA | Face to face | Nurse | 9 | HbA1c |
| Varming AR, 2019 [ 26 ] | Denmark | RCT | 97 | NA | Face to face | Nurse | 6 | BMI, Foot care |
| Güner TA, 2020 [ 27 ] | Turkey | RCT | 101 | NA | Face to face, Telephone | Nurse, Physician | 6 | HbA1c, BMI |
| Utz SW, 2008 [ 28 ] | USA | RCT | 21 | Social Cognitive Theory | Face to face | Certified, Diabetes, Educator | 6 | HbA1c, Diet control, Foot care |
| Omar MA. 2020 [ 29 ] | UAE | RCT | 164 | NA | Online | Pharmacist | 6 | HbA1c |
| Spencer MS, 2018 [ 30 ] | Canada | RCT | 162 | Empowerment Model | Face to face | Nurse | 18 | HbA1c |
| Pérez-Escamilla R, 2015 [ 31 ] | USA | RCT | 221 | NA | Face to face | Community, health, workers | 18 | HbA1c |
| Yuan C, 2014 [ 32 ] | China | RCT | 88 | NA | Face to face | Nutritionist | 3 | HbA1c, BMI |
| Carter EL, 2011 [ 33 ] | USA | RCT | 47 | NA | Online | Nurse | 9 | HbA1c, Weight |
| Sacco WP, 2009 [ 34 ] | USA | RCT | 48 | NA | Telephone | Psychologist | 6 | HbA1c |
| Golnaz A 2018 [ 35 ] | Iran | RCT | 142 | NA | Face to face | Nurse | 6 | HbA1c, BMI |
| Jutterström L 2016 [ 36 ] | Sweden | RCT | 68 | Hernandez about integration and studies on personal understanding in T2D as well as Illness integration and turning points in T2D | Face to face | Nurse | 12 | HbA1c, BMI |
RCT randomized controlled trials, NA not reported, ADCES7 American Association of Diabetes Educators Diabetes Care and Education Experts 7-Step Method
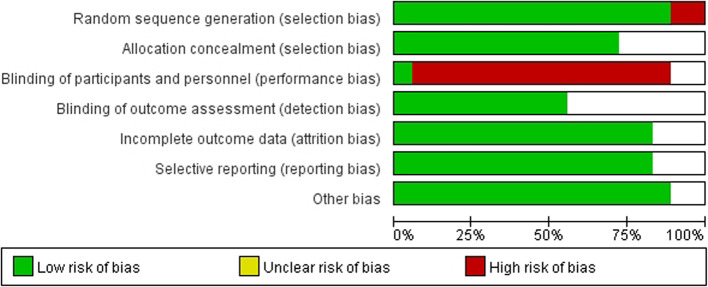
Literature quality assessment
Four studies reported the theoretical model of designing and implementing diabetes self-management intervention [22, 28, 30, 36]. These studies involved intervention in the community and at home. The follow-up period was 3–18 months after intervention. All studies used health education to address patients’ behaviour and cognition. The risk of random distribution method, hidden distribution scheme, integrity of result data and selective reporting was low. But the risk of blindness is higher, generally single-blind, because researchers must know in advance what kind of care the patient will take, and it is very different from the general care of the patient. See Fig. 2 for details.
Fig. 2.
Risk of bias summary
Self-management
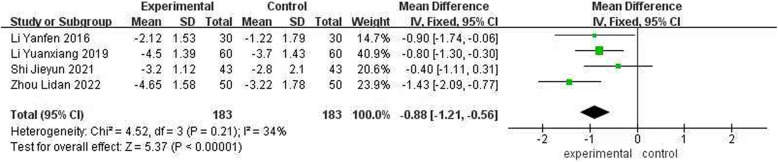
Analysis of the results of the effect of patient-centred care on fasting plasma glucose
Four studies assessed the effect of community–home PCC on FPG. The heterogeneity test result was P = 0.21 and I2 = 34%, indicating that the heterogeneity among the studies was not significant, and the fixed-effect model was thus used for the analysis. The results showed that PCC could reduce the level of FPG in patients with type 2 diabetes compared with routine nursing, and the combined effect was statistically significant (MD = − 0.88, 95%CI: [− 1.21, − 0.56], P < 0.001) (Fig. 3).
Fig. 3.
Forest map of FBG
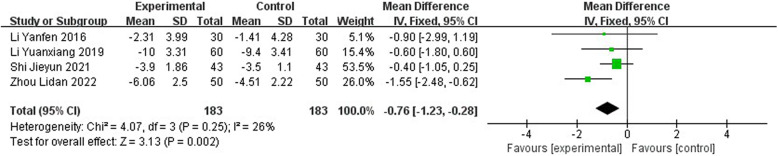
Analysis of the results of the effect of patient-centred care on 2-hour plasma glucose
Four studies evaluated the influence of PCC nursing on 2hPG in community families. The heterogeneity test (P = 0.25, I2 = 26%) showed that the heterogeneity among the studies was not significant, and the fixed-effect model was thus used for the analysis. The results showed that PCC could reduce the level of 2hPG in patients with type 2 diabetes compared with routine nursing, and the combined effect was statistically significant (MD = − 0.76, 95%CI: [− 1.23, − 0.28], P = 0.002) (Fig. 4).
Fig. 4.
Forest map of 2Hpg
Analysis of the results of the effect of patient-centred care on haemoglobin A1c
Fifteen studies evaluated the influence of PCC nursing on HbAlc in community families for 6 months or more. The heterogeneity test result was P < 0.001 and I2 = 81%, which indicated that there was heterogeneity among the studies, and the random-effects model was thus used for the analysis. The results showed that PCC can reduce the level of HbA1c in patients with type 2 diabetes compared with routine nursing, and that its comprehensive effect was statistically significant (MD = − 0.60, 95%CI: [− 0.88, − 0.32], P < 0.001) (Fig. 5).
Fig. 5.
Forest map of HbA1c
Five studies evaluated the influence of PCC nursing on HbAlc in community families for 3 months. The heterogeneity test result was P < 0.001 and I2 = 77%, which indicated that there was heterogeneity among the studies, and the random-effects model was thus used for the analysis. The results showed that PCC can reduce the level of HbA1c in patients with type 2 diabetes compared with routine nursing, and that its comprehensive effect was statistically significant (MD = − 0.45, 95%CI: [− 0.89, − 0.01], P = 0.05) (Fig. 5).
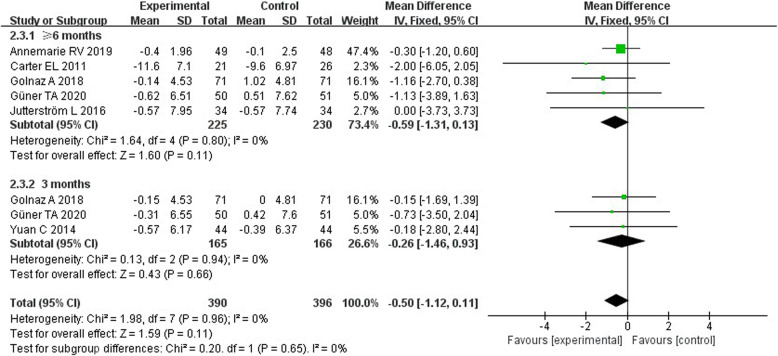
Outcome analysis of the impact of patient-centred care on body mass index
Five studies evaluated the influence of PCC nursing in community families for 6 months or more on the BMI of patients. The heterogeneity test result was P = 0.80 and I2 = 0%, indicating that the heterogeneity among the studies was not significant, and the fixed-effect model was thus used for the analysis. The results showed that, compared with routine nursing, PCC did not significantly reduce the BMI of patients with type 2 diabetes, and that its comprehensive effect was not statistically significant (MD = − 0.59, 95%CI: [− 1.31, − 0.13], P = 0.11).
Three studies evaluated the influence of PCC nursing in community families for 3 months on the BMI of patients. The heterogeneity test result was P = 0.94 and I2 = 0%, indicating that the heterogeneity among the studies was not significant, and the fixed-effect model was thus used for the analysis. The results showed that, compared with routine nursing, PCC did not significantly reduce the BMI of patients with type 2 diabetes, and that its comprehensive effect was not statistically significant (MD = − 0.26, 95%CI: [− 1.46, 0.93], P = 0.66) (Fig. 6).
Fig. 6.
Forest map of BMI
Outcome analysis of the impact of patient-centred care on foot care
Three studies evaluated the heterogeneity of the influence of PCC nursing on foot care in community families. The heterogeneity test result was P < 0.001 and I2 = 94%, which indicated that there was significant heterogeneity among the studies, and the random-effects model was thus used for the analysis. The results showed that PCC did not improve the foot care of patients with type 2 diabetes compared with routine care, and that its comprehensive effect was not statistically significant (MD = − 1.51, 95%CI: [− 2.17, 5.19], P = 0.42) (Fig. 7).
Fig. 7.
Forest map of foot care
Sensitivity analysis
Here, FPG-, 2hPG- and HbAlc-related studies all showed some heterogeneity, and the method of excluding a particular study one by one was used for determination. The results were not significantly changed from the previous results, which were more stable and reliable.
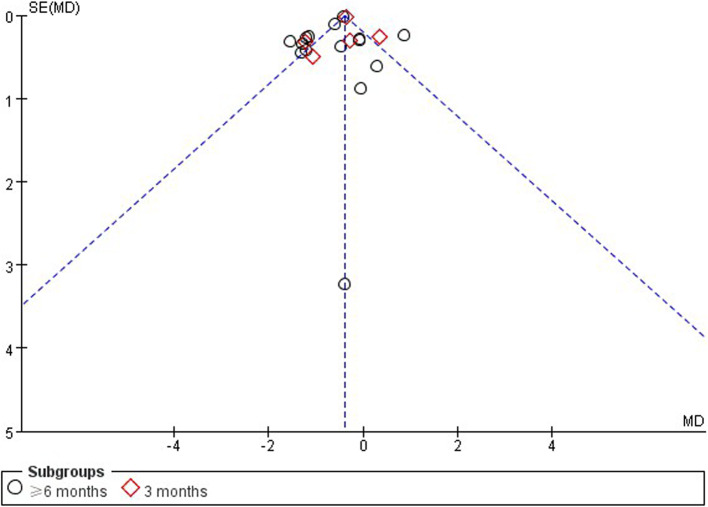
Publication bias analysis
As shown in Fig. 8, using HbA1c as an indicator to draw a funnel plot, all studies exhibited good scatter distribution and symmetry, indicating that the possibility of publication bias in this study is small. Egger’s test showed P = 0.085, indicating that there was no significant publication bias.
Fig. 8.
Publication bias funnel plot
Discussion
Community–home PCC nursing has a significant effect on FPG, 2hPG and HbA1c levels in patients with type 2 diabetes. The results of heterogeneity testing and sensitivity analysis suggested that the literature included in this study was reliable, suggesting that community–home PCC is effective in improving self-management levels in patients with type 2 diabetes mellitus. This is largely because this approach includes aspects of patients’ living habits, dietary procedures and exercise patterns. In the PCC approach, first, care needs to be implemented in accordance with standard procedures to ensure the quality of service. Second, family members are instructed to supervise the patient’s life. Third, the patient’s bad habits are changed, and lastly, a co-operative relationship is established with the patient to ensure continuity of care. As such, community–home PCC can adjust the patient’s lifestyle, reduce their blood glucose level and improve their quality of life [37].
In terms of the effects of community–home PCC on other aspects of patients with type 2 diabetes, study showed that the depression self-assessment scale score of patients in the PCC group was lower than that of the control group, suggesting that the PCC approach can significantly improve the psychological functioning of patients with type 2 diabetes mellitus [24, 34]. The reason for this is that community–home PCC involves comprehensive and systematic health education, which gives patients more psychological support, improves their understanding of diabetes, enhances their cognitive level, promotes healthy behaviours and improves their psychological functioning. Patients with diabetes are usually treated at home and require long-term self-management, which requires strict compliance behaviour. However, the compliance behaviour of patients with diabetes is not satisfactory. Studies have found that community–home PCC can enhance the compliance of patients with diabetes [20, 21]. The reason for this may be that this approach improves patients’ understanding of and attention to diabetes to a certain extent, which is conducive to the formation of good living habits. Patients’ glycaemic control is related to self-management ability, and PCC can help improve patients’ adherence to diet and medication and enhance their self-management ability, thus playing a role in glycaemic control. Moreover, studies found that patients in the community–home PCC group had lower triglyceride levels and significantly higher quality of life than those in the control group [22], suggesting that community–home PCC can help improve patients’ lipid levels and quality of life. This approach can also significantly improve the satisfaction of patients with type 2 diabetes and reduce the incidence of diabetic foot and cardiovascular events [19, 28, 34]. However, the above results were not subjected to meta-analysis due to the paucity of relevant literature, but they are worthy of further study in the future.
Diabetes mellitus cannot be cured clinically, but the implementation of standardised and effective treatment can alleviate or eliminate the clinical symptoms of the disease and maintain the quality of life of patients [38]. However, patients with diabetes tend to have a short hospital stay, lack of professional guidance after discharge, weak diet compliance and self-control, and medication irregularity, while their blood glucose level may rise again [39]. It is necessary for patients with diabetes to receive scientific and standardised care following discharge, and traditional inpatient care is unable to meet this need. In contrast, community–home PCC can provide effective post-discharge care services for patients [40].
Diabetes treatment and management involves a long-term process, wherein patients need to self-manage, meaning healthcare guidance is crucial. Surveys have shown that some patients with type 2 diabetes have a low level of self-management. Good self-management can improve patients’ self-management skills, control metabolic markers and improve their quality of life. The medical model is moving towards a hospital–community–family model, thus providing patients with a high-quality, comprehensive intervention programme. Therefore, community–home PCC is an integral part of the care of patients with type 2 diabetes [41].
The advantages of community–home PCC are as follows. First, the approach organically integrates hospital, community and home care, prompting the participation of medical staff, patients and their families in treatment, deepening patients’ understanding of diabetes knowledge and precautions, and enhancing their self-management ability, which helps to improve metabolic control. Second, regular home follow-up visits by nursing staff assess patients’ disease knowledge, glucose control and insulin use, provide comprehensive health guidance and improve compliance behaviour. Furthermore, the frequency of follow-up visits can be adjusted according to the patient’s level of mastery, and active communication can be used to resolve any problems. Therefore, community–home PCC has unique advantages for patients with type 2 diabetes mellitus, assisting in glycaemic control, improving quality of life, reducing the incidence of complications and ultimately improving the level of comprehensive control to reduce the psychological burden and improve compliance.
This study has some limitations. First, the specific content of the community–home PCC scheme in each study was not exactly the same, the follow-up time was different and the combined results affect the reliability of the conclusion.
In conclusion, community–home PCC can help improve FPG, 2hPG and HbA1c levels in patients with type 2 diabetes mellitus; however, due to the quality limitation of the literature, the above conclusion needs to be further verified. More high-quality clinical studies are recommended at a later stage. A unified PCC protocol has not been identified, and further standardisation of PCC protocols for diabetes may be attempted in the future.
Supplementary Information
Authors’ contributions
Conception and design of the research: Luo Y, Cheng Z, Xiao QY. Acquisition of data: Cheng Z, Xu YF, Tan LY. Analysis and interpretation of the data: Xiao QY, Qu WX, Shen WY. Statistical analysis: Luo Y, Cheng Z, Xiao QY. Obtaining financing: None. Writing of the manuscript: Cheng Z, Xiao QY. Critical revision of the manuscript for intellectual content: Luo Y.
Funding
Shenzhen Bao’an District Science and Technology Innovation Bureau: 2021JD141.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki and approved by the ethics committee of Shenzhen Baoan Shiyan People’s Hospital.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Zhen Cheng and Qingyu Xiao contributed equally to this work.
References
- 1.Liu H, Qiao H. Research progress on the relationship between type 2 diabetes and intestinal flora. Chin J Geriatr Multiple Organ Dis. 2022;21(1):55–8 10.11915/j.issn.1671-5403.2022.01.012. [DOI] [Google Scholar]
- 2.Sun H, Saeedi P, Karuranga S, et al. IDF diabetes atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183:109119. 10.1016/j.diabres.2021.109119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Magliano DJ, Boyko EJ. IDF Diabetes Atlas 10th edition scientific committee. IDF Diabetes Atlas. 10th ed. Brussels: International Diabetes Federation; 2021. [Google Scholar]
- 4.World Health Organization. Definition and diagnosis of diabetes mellitus andintermediate hyperglycemia: report of a WHO/DF consultation, 2006. Geneva: WHO Document Production Services; 2006. [Google Scholar]
- 5.Chinese Medical Association Health Management Branch. Editorial committee of Chinese journal of health management declaration on self health management. Chin J Health Manage. 2015;9(5):331. [Google Scholar]
- 6.Diabetes Branch of Chinese Medical Association. Guidelines for the prevention and treatment of type 2 diabetes in China (2017 Edition). Chin J Diabetes. 2018;10(1):4–67. [Google Scholar]
- 7.Ayele K, Tesfa B, Abebe L, et al. Self care behavior among patients with diabetes in Harari, Eastern Ethiopia: the health belief model perspective. PLoS One. 2012;7(4):e35515. 10.1371/journal.pone.0035515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhong X, Tanasugarn C, Fisher EB, et al. Awareness and practices of self- management and influence factors among individuals with type 2 diabetes in urban community settings in Anhui Province, China. Southeast Asian J Trop Med Public Health. 2011;42(1):185–6 184, 187– 96. [PubMed] [Google Scholar]
- 9.Cosansu G, Erdogan S. Influence of psychosocial factors on self-care behaviors and glycemic control in Turkish patients with type 2 diabetes mellitus. J Transcult Nurs. 2014;25(1):51–9. 10.1177/1043659613504112. [DOI] [PubMed] [Google Scholar]
- 10.van Smoorenburg AN, Hertroijs DFL, Dekkers T, et al. Patients’ perspective on self-management: type 2 diabetes in daily life. BMC Health Serv Res. 2019;19(1):605. 10.1186/s12913-019-4384-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peng X, Guo X, Li H, et al. A qualitative exploration of self-management behaviors and influencing factors in patients with type 2 diabetes. Front Endocrinol (Lausanne). 2022;13:771293. 10.3389/fendo.2022.771293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Al Mahrouqi AS, Mallinson RK, Oh KM, et al. Patients’ and nurses’ perceptions of diabetes self-management in Oman: a qualitative study. Int J Environ Res Public Health. 2022;19(11):6929. 10.3390/ijerph19116929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Delaney LJ. Patient-centred care as an approach to improving health care in Australia. Collegian. 2018;25:119–23. 10.1016/j.colegn.2017.02.005. [Google Scholar]
- 14.Janes R, Titchener J. Using the patient-centred medicine clinical framework to better appreciate and explore the many barriers to care in type 2 diabetes. J Prim Health Care. 2014;6(4):340–8. PMID: 25485333. [PubMed] [Google Scholar]
- 15.Buse JB, Wexler DJ, Tsapas A, et al. 2019 Update to: management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American diabetes association (ADA) and the European association for the study of diabetes (EASD). Diabetes Care. 2020;43(2):487–93. 10.2337/dci19-0066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Higgins J, Altman DG. Chap. 8: Assessing risk of biasin included studies. In: Higgins J, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0. 2008. Available at: http://www.cochrane-handbook.org. Last Accessed 20 Jul 2010.
- 18.Xu C, Furuya-Kanamori L, Zorzela L, Lin L, Vohra S. A proposed framework to guide evidence synthesis practice for meta-analysis with zero-events studies. J Clin Epidemiol. 2021;135:70–8. [DOI] [PubMed] [Google Scholar]
- 19.Zhou LD. Application experience of procedural home care for community-based elderly diabetic patients. Chin Health Care 2022;40(13):136–8. [Google Scholar]
- 20.Shi JY. The effect of community home care on the quality of life of elderly patients with diabetes mellitus. China Health Standard Manage. 2021;12(1):154–6. 10.3969/j.issn.1674-9316.2021.01.058. [Google Scholar]
- 21.Li YX, Zhang YX, Li MY. Analysis of the application effect of home nursing intervention for elderly diabetic patients. China Health Standard Manage. 2019;10(17):143–5. 10.3969/j.issn.1674-9316.2019.17.059. [Google Scholar]
- 22.Li YF, Wang YX. Effect analysis of community home nursing intervention for elderly patients with type 2 diabetes mellitus. J Guangxi Univ Tradit Chin Med 2016. 2016;19(4):59–61. 10.3969/j.issn.2095-4441. [Google Scholar]
- 23.Hailu FB, Moen A, Hjortdahl P. Diabetes Self-Management education (DSME) - effect on knowledge, self-care behavior, and self-efficacy among type 2 diabetes patients in Ethiopia: a controlled clinical trial. Diabetes Metab Syndr Obes. 2019;12:2489–99 PMID: 31819574; PMCID: PMC6890192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li SQ. The effect of home nursing intervention on discharged empty-nested elderly diabetic patients. Qilu Nurs J. 2014(23):78–9. 10.3969/J.issn.1006-7256.2014.23.038.
- 25.Hailu FB, Hjortdahl P, Moen A. Nurse-led diabetes self-management education improves clinical parameters in Ethiopia. Front Public Health. 2018;6:302. 10.3389/fpubh.2018.00302. PMID: 30406070; PMCID: PMC6206899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Varming AR, Rasmussen LB, Husted GR, Olesen K, Grønnegaard C, Willaing I. Improving empowerment, motivation, and medical adherence in patients with poorly controlled type 2 diabetes: a randomized controlled trial of a patient-centered intervention. Patient Educ Couns. 2019;102(12):2238–45 Epub 2019 Jun 13. PMID: 31239180. [DOI] [PubMed] [Google Scholar]
- 27.Güner TA, Coşansu G. The effect of diabetes education and short message service reminders on metabolic control and disease management in patients with type 2 diabetes mellitus. Prim Care Diabetes. 2020;14(5):482–7. 10.1016/j.pcd.2020.04.007. [DOI] [PubMed] [Google Scholar]
- 28.Utz SW, Williams IC, Jones R, et al. Culturally tailored intervention for rural African Americans with type 2 diabetes. Diabetes Educ. 2008;34(5):854–65. 10.1177/0145721708323642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Omar MA, Hasan S, Palaian S, et al. The impact of a self-management educational program coordinated through WhatsApp on diabetes control. Pharm Pract (Granada). 2020;18(2):1841. 10.18549/PharmPract.2020.2.1841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Spencer MS, Kieffer EC, Sinco B, et al. Outcomes at 18 months from a community health worker and peer leader diabetes self-management program for Latino adults. Diabetes Care. 2018;41(7):1414–22. 10.2337/dc17-0978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pérez-Escamilla R, Damio G, Chhabra J, et al. Impact of a community health workers-led structured program on blood glucose control among Latinos with type 2 diabetes: the DIALBEST trial. Diabetes Care. 2015;38(2):197–205. 10.2337/dc14-0327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yuan C, Lai CW, Chan LW, et al. The effect of diabetes self-management education on body weight, glycemic control, and other metabolic markers in patients with type 2 diabetes mellitus. J Diabetes Res. 2014;2014:789761. 10.1155/2014/789761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Carter EL, Nunlee-Bland G, Callender C. A patient-centric, provider-assisted diabetes telehealth self-management intervention for urban minorities. Perspect Health Inf Manag. 2011;8(Winter):1b. [PMC free article] [PubMed] [Google Scholar]
- 34.Sacco WP, Malone JI, Morrison AD, et al. Effect of a brief, regular telephone intervention by paraprofessionals for type 2 diabetes. J Behav Med. 2009;32(4):349–59. 10.1007/s10865-009-9209-4. [DOI] [PubMed] [Google Scholar]
- 35.Golnaz A, Lam SK, Ghazali SS, et al. Effect of a nurse-led diabetes self-management education program on glycosylated hemoglobin among adults with type 2 diabetes. J Diabetes Res. 2018;2018:1–12. 10.1155/2018/4930157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jutterström L, Hörnsten Å, Sandström H, Stenlund H, Isaksson U. Nurse-led patient-centered self-management support improves HbA1c in patients with type 2 diabetes-A randomized study. Patient Educ Couns. 2016;99(11):1821–9. 10.1016/j.pec.2016.06.016. Epub 2016 Jun 17. PMID: 27372525. [DOI] [PubMed] [Google Scholar]
- 37.Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, Thomas J. Updated guidance for trusted systematic reviews: a new edition of the Cochrane handbook for systematic reviews of interventions. Cochrane Database Syst Rev. 2019;10(10):ED000142. 10.1002/14651858.ED000142. PMID: 31643080; PMCID: PMC10284251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhao H, Wang F, Luo GH, Lei H, Peng F, Ren QP, Chen W, Wu YF, Yin LC, Liu JC, Pan SN. Assessment of structural brain changes in patients with type 2 diabetes mellitus using the MRI-based brain atrophy and lesion index. Neural Regen Res. 2022;17(3):618–24. 10.4103/1673-5374.320996. PMID: 34380902; PMCID: PMC8504365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nimer R, Kamel G, Obeidat MA, Dahabiyeh LA. Investigating the molecular structure of plasma in type 2 diabetes mellitus and diabetic nephropathy by synchrotron Fourier-transform infrared microspectroscopy. Spectrochim Acta Mol Biomol Spectrosc. 2022;264:120259. 10.1016/j.saa.2021.120259. Epub 2021 Aug 6. PMID: 34388428. [DOI] [PubMed] [Google Scholar]
- 40.Ferrari F, Moretti A, Villa RF. Hyperglycemia in acute ischemic stroke: physiopathological and therapeutic complexity. Neural Regen Res. 2022;17(2):292–9. 10.4103/1673-5374.317959. PMID: 34269190; PMCID: PMC8463990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xiujuan Z, Wengui C, Xiuwen T. Effect of community nursing intervention on elderly patients with diabetes mellitus. J Qiqihar Med Coll. 2014;35(10):1559–60. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.