Abstract
As fossil fuel combustion continues to power the global economy, the rate of climate change is accelerating, causing severe respiratory health impacts and large disparities in the degree of human suffering. Hotter and drier climates lead to longer and more severe wildland fire seasons, impairing air quality around the globe. Hotter temperatures lead to higher amounts of ozone and particles, causing the exacerbation of chronic respiratory diseases and premature mortality. Longer pollen seasons and higher pollen concentrations provoke allergic airway diseases. In arid regions, accelerated land degradation and desertification are promoting dust pollution and impairing food production and nutritional content that are essential to respiratory health. Extreme weather events and flooding impede healthcare delivery and can lead to poor indoor air quality due to mold overgrowth. Climate and human activities that harm the environment and ecosystem may also affect the emergence and spread of viral infections, including severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and associated morbidity and mortality exacerbated by air pollution. Children and elderly individuals are more susceptible to the adverse health effects of climate change. Geographical and socioeconomic circumstances, together with a decreased capacity to adapt, collectively increase vulnerability to the adverse effects of climate change. Successful mitigation of anthropogenic climate change is dependent on the commitment of energy-intensive nations to manage greenhouse gas emissions, as well as societal support and response to aggravating factors. In this review, we focus on the respiratory health impacts of global climate change, with an emphasis on susceptible and vulnerable populations and low- and middle-income countries.
Keywords: vulnerable populations, environmental health, SARS-CoV-2, low- and middle-income countries, air pollution
It is no longer a novel concept that climate change is a public health crisis. There have been countless reports documenting the human health implications of warmer temperatures, droughts, heat waves, wildfires, and other environmental changes driven by the rising concentrations of greenhouse gases (GHGs) in the atmosphere (1, 2). In fact, at the time of the 2019 American Thoracic Society conference in Dallas, when the series of topics included in this review was originally presented, a new and unfortunate milestone was reached: the peak concentration of CO2 measured at the Mauna Loa observatory in Hawaii exceeded 415 ppm, with the highest monthly average (414.7 ppm) ever recorded (3). As of this writing, the highest monthly record was measured in June 2022 at Mauna Loa at 420.99 ppm (4). CO2 concentrations in the atmosphere continue to rise as fossil fuel burning continues, largely unabated.
As the topics discussed in this review will demonstrate, climate change harms respiratory health in all parts of the world, with large disparities in the degree and extent of human suffering, as well as the capacity to cope and adapt. High-income countries release a disproportionate fraction of CO2 into the atmosphere and are historically most responsible for global GHG emissions (5). Although high-income countries suffer adverse health effects of climate change, including the consequences of extreme heat, hurricanes, and wildfires, they are also better resourced to tackle this growing public health crisis and move the world’s economy away from fossil fuel use (6). In contrast, low- and middle-income countries (LMICs), with more fragile economies and poor health system infrastructures, are less able to cope with the myriad consequences of major storms and cyclones, flooding, heat waves, and infectious disease transmission brought about by climate change (7). For these countries, adaptation to climate change is a matter of survival.
Susceptibility and Vulnerability to Respiratory Health Effects of Climate Change
The characteristics of the population, such as the degree of development and the demographic structure, are important determinants of susceptibility and vulnerability, which increase the risk that climate change will adversely affect respiratory health (8, 9) (Figure 1). To distinguish these concepts, susceptibility refers to factors inherent to biological predisposition (e.g., genetics) (10), whereas vulnerability refers to external factors (e.g., environmental) and a lack of capacity to anticipate, cope with, and adapt to climate change (8–10). Children and pregnant women, older adults, and persons with chronic medical conditions are more susceptible to climate-related events (10). People who are socially, economically, culturally, politically, institutionally, or otherwise marginalized are disproportionately vulnerable to the detrimental effects of climate change (9–11). However, susceptibility and vulnerability often interact.
Figure 1.
Diagram showing the interactions among climate change–related hazards, vulnerability, and exposure and how they are related to climate and socioeconomic impacts (9).
Children are more susceptible to environmental hazards because they breathe, eat, and drink more for their size and engage in more intense indoor and outdoor physical activity, resulting in greater air pollutant exposure relative to that of adults (12, 13). Because the lungs and other organs of children are still developing, environmental exposures could have long-term health implications that may extend into adulthood. A newborn’s health is affected by the exposure of the mother to climate-related events such as extreme heat, air pollution, malnutrition, and flood-related contaminants during pregnancy. The first consequences are prematurity and low birth weight (<2.5 kg), both of which have been related to impaired respiratory health later in life (14). In childhood, climate-related factors can increase the risk of allergic, respiratory, and infectious diseases, as well as malnutrition (15), which adversely affects respiratory health (16).
Elderly individuals are more biologically susceptible to climate change because of aging (17), and they are more vulnerable to climate effects because of social isolation and reduced ability to quickly mobilize to cooling centers (18). Oxidative stress has been hypothesized to explain the susceptibility of elderly persons, but preexisting morbidity is likely the greatest risk factor (19). Exposure to extreme heat and increased concentrations of air pollutants have been associated with higher risk of cardiopulmonary mortality and morbidity among the elderly, especially those with preexisting disease such as asthma or chronic obstructive pulmonary disease (COPD) (20). Increased infection rates and injuries are also common consequences of climate change in this age group (17). Last, persons with disabilities are less likely to adapt to extreme weather events.
Other vulnerable groups include poor persons, women, vulnerable occupational groups such as workers who are exposed to extreme weather, ethnic minorities, immigrants and refugees, and Indigenous peoples (11, 21). The extent of the impact of climate change on these groups is determined by their exposure, sensitivity, and adaptive capacity. Sensitivity is a function of biological predisposition, whereas adaptive capacity involves the ability to cope with climate hazards and obtain appropriate health care (10, 11).
Healthcare providers play a uniquely valuable role in the societal response to health challenges posed by climate change to their patients, who are disproportionately affected. In terms of research, the complex interactions among environmental exposures, genetic susceptibility, and behavioral risk factors with respect to health may be best studied through consideration of the exposome, which offers a lens through which climate-related impacts on human health may be better understood (13).
The exposome is the totality of individuals’ lifetime environmental exposures, including pollution, toxicants, infections, diet, medications, lifestyle, stress, socioeconomic status, the urban environment, climate factors, social capital, and the internal signals these factors affect in the body (22). Tracking human climate change–induced environmental exposures has led to the development of exposome studies relating internal and external individual exposures over a lifetime to health effects. This has been the case of asthma aggravated by the interactions between air pollution and pollen or between thunderstorms and pollen (13).
Geographical Locations Most Vulnerable to Respiratory Health Effects of Climate Change
A vulnerable geographical location, a low income, and an inability to cope and adapt collectively increase the adverse effects of climate change (8, 17, 23). Regions most likely to be affected by climate change include the Arctic, the Antarctic, island states, the Mediterranean basin, northern high-latitude regions, the Amazon, the southwestern United States, the Tibetan plateau, Central America, Central and West Africa, and South and Southeast Asia (8, 23, 24). However, regions in less temperate zones may experience greater health impacts of global climate because of the cumulative risk associated with the poverty and precarity of those populations (1, 2).
In several regions, a lack of fresh water, increases in local temperature, and decreases in precipitation have negative effects on grain and wheat crop production (25) that will adversely affect inhabitants in 30 countries in Africa and South and Southeast Asia, all highly dependent on grain production (17). Undernourishment and low socioeconomic status increase the risk for chronic airway diseases such as COPD and asthma (16), as well as the risk for respiratory infections including tuberculosis (26).
The risks of death due to heat waves, extreme weather conditions, and respiratory viral infections such as hantavirus and influenza are markedly increased in vulnerable regions (17, 26, 27). There is also more associated risk for desertification, desert dust storms, and health impacts, including greater mortality, emergency department visits, and hospitalization because of respiratory diseases in these areas (1, 28–32).
The number of “climate change migrants” is estimated to rise to 1 billion by 2050, should no significant mitigation of climate change be achieved (1, 17). Forced displacement of people is associated with acute respiratory infection and tuberculosis and sleep-related disorders, and migration from rural to urban areas has been linked to allergic diseases including asthma (33). Vulnerable countries lack the resources to manage the economic losses related to climate change, including those due to respiratory health harms (17). Interference of human activities with the climate system leads to climate change–related hazards, which can pose serious risks to human health. The degree of exposure and the vulnerability of society together determine the climate-related health impacts (Figure 1) (9).
Environmental Justice
The Centers for Disease Control and Prevention describes environmental justice as follows: “All people—regardless of race, color, national origin, or income—are entitled to equal protection from environmental and health hazards and equal access to the development, implementation, and enforcement of environmental laws, regulations, and policies” (34). Populations and communities that are disadvantaged because of poverty, racism, and national origin are the least well protected from the health effects of climate change, such as heat, flooding, landslides, infectious disease, and malnutrition. Although their emissions of GHGs are lower than in high-income countries (5, 35), LMICs “pay the price” (7) and suffer more from negative impacts of global climate change because of lower resilience and capacity to adapt (6, 7). Cumulative losses from anthropogenic extreme heat from 1992 to 2013 were estimated to be between $5 trillion and $29.3 trillion globally. However, losses due to climate change were reported to account for 6.7% of gross domestic product per capita per year for regions in the lower-income decile, whereas this was only 1.5% for regions in the top-income decile (36).
Air pollution is a critical contributor to health inequities worldwide, and individuals living in LMICs experience the highest burden of ambient particulate matter ⩽2.5 μm in aerodynamic diameter (PM2.5), with 55% of the world’s population experiencing increasing degrees of PM2.5 exposure between 2010 and 2016 (37). The annual average population-weighted concentrations of PM2.5 in North America and Europe were reported to have decreased from 12.4 μg/m3 in 2010 to 9.8 μg/m3 in 2016, whereas the concentrations of PM2.5 measured in central and southern Asia increased from 54.8 to 61.5 μg/m3 (37). According to ambient PM2.5 concentrations in 2019, South Asia, the Middle East, North Africa, and sub-Saharan Africa had the highest concentrations, which were 5–10 times higher than those measured in North America (38). In the United States, communities of color, Indigenous communities, and low-income areas are also disproportionately exposed to combustion-related air pollution, including PM2.5, and experience higher rates of pollution-related mortality (39). Furthermore, there is growing evidence suggesting that climate change exacerbates disparities in exposures, both directly through increased exposures to air pollutants and indirectly because of limited adaptation and resilience planning (40). Health equity can be promoted by building community capacity to adapt to climate change, improving healthcare access, and eliminating injustice in the distribution of environmental exposures.
Impact of Climate Change on Pulmonary Health
The World Health Organization report on climate change and health states, “between 2030 and 2050, climate change is expected to cause approximately 250,000 additional deaths per year” (41). Climate change affects respiratory health (Table 1) through impacts on weather and ecosystems. This may occur directly through changes in temperature, humidity, and atmospheric pressure or indirectly through increases in risk factors such as air pollution; distribution of aeroallergens; transmission of respiratory pathogens; desertification; climate change–related hazards such as hurricanes, floods, storms, and wildfires; and the socioeconomic vulnerability of the population. Respiratory health effects of climate change include exacerbations of chronic lung diseases, the development of acute respiratory diseases including infectious diseases, increased allergic response, and premature mortality (Figures 1 and 2).
Table 1.
Summary of potential cardiopulmonary health impacts associated with climate change parameters
| Climate Change–related Parameters | Adverse Health Effects | References |
|---|---|---|
| Direct weather effects (heat stress, cold, drought, humidity, atmospheric pressure) | Increased mortality, emergency department visits, hospitalization because of cardiopulmonary diseases, pulmonary infections, pneumothorax | 1, 17, 20, 28, 29, 31, 41–47, 50 |
| Extreme weather events (hurricanes, cyclones, floods, storms, thunderstorms, wildfires) | Adverse living conditions, injuries, respiratory infections, sleep-related disorders, emergency department visits because of asthma | 21, 27, 33, 49, 50, 64, 65 |
| Allergens, air pollutants | Increased pulmonary mortality and increased emergency department visits, hospitalization because of asthma, COPD, cardiac diseases, and respiratory viral infections including SARS-CoV-2 | 1, 2, 21, 29, 31, 48, 51–56, 58, 66, 67 |
| Dust storms | Increased cardiopulmonary mortality, emergency department visits because of asthma and cardiopulmonary diseases | 24, 28, 29, 31, 32, 61 |
Definition of abbreviations: COPD = chronic obstructive pulmonary disease; SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2.
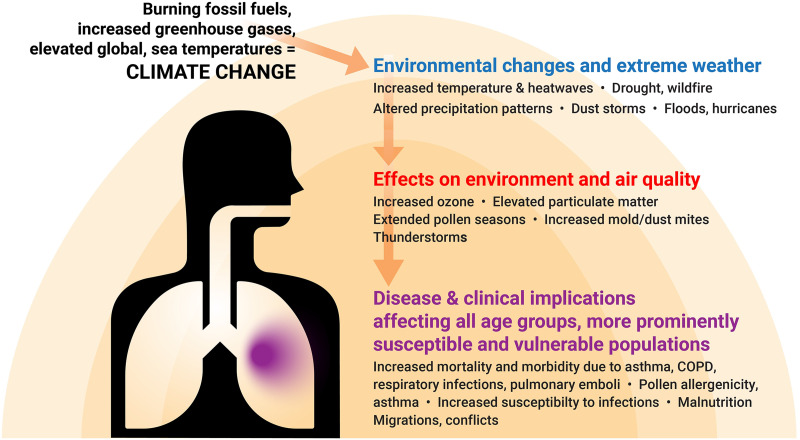
Figure 2.
Implications of greenhouse gas emissions on the climate and weather (blue) and on environment and air quality (red) and their ultimate impacts on respiratory health (purple). COPD = chronic obstructive pulmonary disease.
Direct Effects
Increasing temperatures worldwide have resulted in greater exposure to heat waves, with approximately 125 million vulnerable adults affected between 2006 and 2011 (17). Studies have reported close associations between increased heat and adverse health impacts such as emergency department visits, hospitalizations, and deaths due to cardiopulmonary diseases including asthma, COPD, lower respiratory tract infections, pneumonia, and cardiovascular diseases (1, 28, 29, 31, 42, 43). Similarly, humidity has been associated with asthma and COPD exacerbations (44). Recent studies have reported a significant relationship of increased temperature and atmospheric pressure with spontaneous pneumothorax (45). On the other hand, extreme cold has been associated with an increased risk of acute myocardial infarction and mortality in patients with COPD (46, 47).
Indirect Effects
Extreme Weather Events
Climate change–related weather events have the potential to cause economic devastation leading to unemployment, adverse living conditions (33, 48), injury, and mortality, as well as significant damage to infrastructure and healthcare facilities. Major storms, for example, often displace individuals from their homes, leaving them in crowded living conditions, without shelter or access to health care, and vulnerable to infectious disease including respiratory infections. Climate change is also associated with increases in the frequency and intensity of hurricanes and thunderstorms, resulting in more emergency medical visits for asthma because of the release of pollen and molds caused by thunderstorms and hurricanes, respectively (21, 49, 50).
Allergens and Air Pollutants
Elevated temperatures and humidity arising from climate change have been associated with changes in seasonality and possibly increased allergenicity of pollens and spores and the formation of various types of air pollutants (13). Pollens and spores in the form of bioaerosols, as well as severe events due to climate, such as wildfires, pose further threats to respiratory health (1, 21, 51). Increased ambient allergens and daily variations in pollen bioaerosols have been associated with deaths due to cardiovascular and pulmonary diseases (52).
Robust associations between air pollution and cardiopulmonary mortality and morbidity have been reported (2, 31). Furthermore, wildfires have been increasing in frequency in western North America, Australia, the Iberian peninsula, Brazil, and Russia, resulting in ever higher concentrations of air pollutants that pose threats to respiratory health (51, 53–55). Recent studies suggest that the wildfire season is lengthening, with wildfire smoke having a significant impact on pulmonary morbidity and mortality (56). Wildfire events have had major impacts on air quality around the world. In the United States, PM2.5 emissions from wildfires have undone much of the policy efforts to reduce non–wildfire-related PM2.5 emissions from transportation and electricity generation (57). Moreover, recent studies suggest that wildfire-specific PM2.5 may be more harmful to respiratory health than non–wildfire-related PM2.5 (58). Tropospheric ozone concentration increases in direct relationship to surface temperature. PM2.5 and nitrogen dioxide (NO2) are also increased as the power for air conditioning is generated from the combustion of fossil fuels. On the other hand, warmer weathers may, at least to some extent, reduce energy demand for winter heating in cold areas of the globe (8).
Dust Storms
Desertification and dust storms are well-established consequences of climate change. Higher temperatures tend to extract more moisture from the soil, giving rise to drought-like conditions in affected regions (59). With a rising average global surface temperature, drought-like conditions are projected to significantly increase by 2050. Globally, much of the Sahel and East Africa, the Middle East, India, and parts of northern and western China are projected to be most affected by desertification (24, 30, 32). In the United States, the Mountain West states, stretching from Montana and Wyoming to Arizona and California, are expected to experience the most frequent and severe droughts (60). Studies suggest an increase in the frequency of dust outbreaks in regions such as the Middle East, with a significant impact on health (24, 30, 32).
Desert dust storms are associated with increased emergency department visits, hospitalization, and death due to respiratory diseases including asthma, COPD, respiratory infections, and pulmonary emboli (28, 29, 31, 32, 61). The pulmonary deposition of dust particles can be significant because of fine particulate matter pollution from the lofting of dry crustal materials. The extent of lung injury is dependent on the dose, composition, and size of dust particles. Although more attention has been given to the health effects of PM2.5 from the combustion of fossil fuels in recent years, particulate matter ⩽10 μm in aerodynamic diameter from windblown crustal dust also has significant respiratory toxicity (62), as do fine dust particles (particulate matter ⩽0.1 μm in aerodynamic diameter to PM2.5) that can be transported over large distances across the globe.
Respiratory Infectious Agents Including Severe Acute Respiratory Syndrome Coronavirus 2
Climate change increases the incidence, spread, severity, and pathogenesis of respiratory tract infections in humans after severe weather events or natural disasters, as well as changes in temperature and precipitation (27). Hurricanes have been shown to contribute to an increase in nontuberculous mycobacterial disease. Respiratory infections, such as avian influenza and coccidioidomycosis, are occurring in locations previously unaffected, apparently because of climate change (27). The resulting displacement of inhabitants will lead to increased risk of acute respiratory infection and tuberculosis (33). Indoor air pollution threats anticipated from climate change, including microbial and mold growth secondary to flooding, also result in the displacement of persons and the need for respiratory protection of exposed individuals (49, 63). It is well established that gases such as NO2 and O3 and respirable particulate matter may modify airway permeability, the first line of defense against respiratory viruses (64, 65).
The global pandemic of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has further complicated the scale of health risks related to environmental factors including air pollution. Multiple studies suggest an association between air pollution, which has a close link with climate change, and morbidity and mortality due to coronavirus disease 2019 (COVID-19). High PM2.5 concentrations were positively associated with greater COVID-19 mortality rates at the population level (66) and risk of hospitalization at the individual level (67). Long-term exposure to air pollution can cause airway inflammation as a result of oxidative stress as well as overexpression of angiotensin-converting enzyme 2, which may put patients with COVID-19 at higher risk of severe illness and death (65, 68). It has been observed that SARS-CoV-2 can be present on ambient particulate matter (69), suggesting that the virus could also be transported by particulate matter. However, whether this has an impact on the spread of coronavirus infection remains to be determined. COVID-19 disproportionately affects racial and ethnic minorities and low-income communities, and because these communities experience disproportionate exposure to air pollution (70), increased pollution due to climate change may contribute to these disparities.
Action on Climate Change Mitigation Strategies
The impacts of climate change on humanity in the future will be determined by choices and decisions that are made today. To address the global health crisis of climate change, urgent action is needed at all levels, including intergovernmental regulatory agreements, national policies, local authorities, the private sector, and academia, including the respiratory health medical community.
After the Paris Agreement, the 26th Conference of Parties agreed on carbon markets. This will give certainty and predictability to both market and nonmarket approaches in support of mitigation, as well as adaptation. In addition, the negotiations on the Enhanced Transparency Framework promoted agreed-on tables and formats to account for and report GHG emissions and reduction targets (6). The 26th Conference of Parties agreement indicates that under existing emissions reduction pledges, emissions will be nearly 14% higher by 2030 than in 2010. In response, it was agreed to begin reducing coal-fired power (without carbon capture) and to begin the elimination of subsidies on other fossil fuels. Unfortunately, rather than a phase-out of coal-fired power generation, the agreement only calls for a “phase-down.”
Ambitious national policies are needed to curb CO2 emissions and protect the most vulnerable members of society from the health effects of climate change. The United Kingdom plan for an all-electric new vehicle fleet by 2035 is such an example. In California, the Advanced Clean Cars II regulations also require that all new passenger vehicles sold in the state be zero emission by 2035; income-based incentives will be available to support this transition. California also has a legislative mandate for 100% renewable power generation by 2040. The U.S. Inflation Reduction Act of 2022 has taken the approach of incentivizing innovation and conversion to renewable energy (rather than mandating energy transitions). It remains to be seen if this investment in private-sector solutions will succeed.
Despite resistance in some, many sectors of the economy recognize the current and future challenges posed by climate change, including the associated uncertainties in business and strategic planning. Among these sectors are the military (71), the insurance industry (72), coastal planners (73), and most recently investment ratings; for example, Moody’s is now incorporating climate risk into its ratings assessments (74).
Even as efforts are made to mitigate the worst potential impacts of climate change, societies must become more resilient to those impacts that are now unavoidable. These impacts often disproportionately affect low-income communities and communities of color, reinforcing the need for equitable resilience planning and resource allocation. Examples of resilience policies that are already being implemented in some communities to adapt to extreme heat include the greening of inner-city heat islands and the establishment of cooling/clean air centers. In addition to acute impacts, resilience planning must account for chronic events, such as rising sea levels, worsening air quality, and population migration.
The medical community, especially the respiratory health community, is treating the health consequences of climate change (75). Physicians have a key role as policy advocates to emphasize the health benefits of policies that cut climate-related emissions and reduce disparities in exposure. Physicians must also educate patients to explain how climate change is affecting their health through heat, smoke, allergens, and other exposures (76, 77). Such guidance can help patients protect themselves from the adverse health effects of climate change and improve their understanding of climate change as a health hazard. Multiple nongovernmental organizations are working to educate healthcare providers about the impacts of climate change and respiratory health so that they can better care for their patients. These include professional societies such as the American Thoracic Society, the European Respiratory Society, and the Forum of International Respiratory Societies, as well as health advocacy organizations such as the European Lung Foundation and the American Lung Association. All of these groups have produced publicly available educational materials that provide helpful information about the topic.
Conclusion
Because of inaction by many governments over the past 30 years, we now have a “climate emergency.” GHG emissions have continued to increase, and atmospheric CO2 is now significantly greater than 400 ppm, meaning that the global surface temperature will likely rise by greater than 1.5 °C. This increase in temperature is expected to produce irreversible environmental impacts that pose threats to the way we live and, in particular, to human health worldwide. There is increased urgency to undertake international climate change mitigation efforts to avoid temperature increases in excess of 2 °C, a tipping point with even more serious consequences to the global environment and public health.
Climate change disproportionally affects the poorest countries that contribute the least to GHG emissions. Prompt and effective approaches to mitigation and adaptation can minimize health risks due to climate change (78). A reduction in carbon emissions from the combustion of fossil fuel would have substantial health benefits in reducing global climate change and air pollution, thus leading to reduced cardiopulmonary and other noncommunicable diseases. High-income countries, in particular, have a moral obligation to combat climate change by implementing policies to dramatically reduce fossil fuel use for energy and transportation needs. Healthcare providers in high-income countries can play a critical role in informing and educating their patients, the public, and policy makers about the health implications of climate change and advocate for measures that move the economy away from fossil fuel use.
Climate change and its health impacts are real. The sooner we move to a clean-energy economy, the greater the benefits of mitigation will be on climate change. Most analyses of the costs and benefits of climate change mitigation policies fail to consider the economic and social costs of the adverse health outcomes linked to climate change. When such costs are considered, it is clear that the benefits of climate change mitigation policies can far outweigh the costs of their adoption and implementation (79, 80).
Acknowledgments
Acknowledgment
The authors thank Dr. Rona Marie Silva (Center for Health and the Environment, University of California, Davis) for editing the manuscript.
Footnotes
Supported by National Institute for Occupational Safety and Health (NIOSH) grant U54 OH07550, P30 ES023513, and P51 OD011107.
Author Contributions: H.B. discussed pulmonary health implications in vulnerable regions and low-income countries and organized the topics, writing, and final submission of the manuscript. M.B.R. wrote the introduction and edited the manuscript. W.A. discussed the current condition of climate change and actions on mitigation. M.A.E. focused on the pulmonary health impacts of climate change. M.M. presented the pulmonary health impacts of desert dust storms. I.A.-M. explained the pulmonary health impacts of climate change on susceptible, elderly, and impoverished people; introduced the exposome; and assisted in editing the final manuscript. K.E.P. discussed the situation in developed countries and assisted in editing the final manuscript. J.R.B. prepared the conclusion and edited and modified the manuscript in its final form. All authors contributed to the writing, presentation, and interpretation of the data and the intellectual content of this paper.
CME will be available for this article at https://shop.thoracic.org/collections/cme-moc/ethos-format-type-journal.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1. Romanello M, McGushin A, Di Napoli C, Drummond P, Hughes N, Jamart L, et al. The 2021 report of the Lancet Countdown on health and climate change: code red for a healthy future. Lancet . 2021;398:1619–1662. doi: 10.1016/S0140-6736(21)01787-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rice MB, Thurston GD, Balmes JR, Pinkerton KE. Climate change: a global threat to cardiopulmonary health. Am J Respir Crit Care Med . 2014;189:512–519. doi: 10.1164/rccm.201310-1924PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Oceanic and Atmospheric Administration. https://www.noaa.gov/news/carbon-dioxide-levels-in-atmosphere-hit-record-high-in-may
- 4.Pro Oxygen. Victoria, BC, Canada: Pro Oxygen; 2022. https://www.co2.earth/annual-co2 [Google Scholar]
- 5. Andrews O, Le Quéré C, Kjellstrom T, Lemke B, Haines A. Implications for workability and survivability in populations exposed to extreme heat under climate change: a modelling study. Lancet Planet Health . 2018;2:e540–e547. doi: 10.1016/S2542-5196(18)30240-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.United Nations. Geneva, Switzerland: United Nations; 2021. https://ukcop26.org/the-glasgow-climate-pact/ [Google Scholar]
- 7. Naddaf M. Climate change is costing trillions—and low-income countries are paying the price. Nature . 2022 doi: 10.1038/d41586-022-03573-z. [DOI] [PubMed] [Google Scholar]
- 8.Barros VR, Field CB, Dokken DJ, Mastrandrea MD, Mach KJ, Bilir TE, et al. Cambridge, United Kingdom: Cambridge University Press; 2014. https://www.ipcc.ch/site/assets/uploads/2018/02/WGIIAR5-PartB_FINAL.pdf [Google Scholar]
- 9.Field CB, Barros VR, Dokken DJ, Mach KJ, Mastrandrea MD, Bilir TE, et al. Cambridge, United Kingdom: Cambridge University Press; 2014. https://www.cambridge.org/core/books/climate-change-2014-impacts-adaptation-and-vulnerability-part-a-global-and-sectoral-aspects/1BE4ED76F97CF3A75C64487E6274783A [Google Scholar]
- 10.Kovats S, Ebi KL, Menne B, Campbell-Lendrum D, Canziani OF, Githeko A, et al. Copenhagen, Denmark: The Regional Office for Europe of the World Health Organization; 2003. https://apps.who.int/iris/bitstream/handle/10665/107538/9789289010900-eng.pdf?sequence=1&isAllowed=y [Google Scholar]
- 11. Jessel S, Sawyer S, Hernández D. Energy, poverty, and health in climate change: a comprehensive review of an emerging literature. Front Public Health . 2019;7:357. doi: 10.3389/fpubh.2019.00357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ahdoot SPS. Council on environmental health: global change and children’s health. Pediatrics . 2015;136:e1468–e1484. doi: 10.1542/peds.2015-3233. [DOI] [PubMed] [Google Scholar]
- 13. Cecchi L, D’Amato G, Annesi-Maesano I. External exposome and allergic respiratory and skin diseases. J Allergy Clin Immunol . 2018;141:846–857. doi: 10.1016/j.jaci.2018.01.016. [DOI] [PubMed] [Google Scholar]
- 14. Bush A. Impact of early life exposures on respiratory disease. Paediatr Respir Rev . 2021;40:24–32. doi: 10.1016/j.prrv.2021.05.006. [DOI] [PubMed] [Google Scholar]
- 15. Myers SS, Smith MR, Guth S, Golden CD, Vaitla B, Mueller ND, et al. Climate change and global food systems: potential impacts on food security and undernutrition. Annu Rev Public Health . 2017;38:259–277. doi: 10.1146/annurev-publhealth-031816-044356. [DOI] [PubMed] [Google Scholar]
- 16. Kuiper-Makris C, Selle J, Nüsken E, Dötsch J, Alejandre Alcazar MA. Perinatal nutritional and metabolic pathways: early origins of chronic lung diseases. Front Med (Lausanne) . 2021;8:667315. doi: 10.3389/fmed.2021.667315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Watts N, Amann M, Ayeb-Karlsson S, Belesova K, Bouley T, Boykoff M, et al. The Lancet countdown on health and climate change: from 25 years of inaction to a global transformation for public health. Lancet . 2018;391:581–630. doi: 10.1016/S0140-6736(17)32464-9. [DOI] [PubMed] [Google Scholar]
- 18. Rhoades JL, Gruber JS, Horton B. Developing an in-depth understanding of elderly adult’s vulnerability to climate change. Gerontologist . 2018;58:567–577. doi: 10.1093/geront/gnw167. [DOI] [PubMed] [Google Scholar]
- 19. Numan MS, Brown JP, Michou L. Impact of air pollutants on oxidative stress in common autophagy-mediated aging diseases. Int J Environ Res Public Health . 2015;12:2289–2305. doi: 10.3390/ijerph120202289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Robine JM, Cheung SL, Le Roy S, Van Oyen H, Griffiths C, Michel JP, et al. Death toll exceeded 70,000 in Europe during the summer of 2003. C R Biol . 2008;331:171–178. doi: 10.1016/j.crvi.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 21. Pacheco SE, Guidos G, Annesi-Maesano I, Pawankar R, Amato G, Latour-Staffeld P, et al. American Academy of Allergy, Asthma & Immunology Environmental Exposures and Respiratory Health Climate change and global issues in allergy and immunology. J Allergy Clin Immunol . 2021;148:1366–1377. doi: 10.1016/j.jaci.2021.10.011. [DOI] [PubMed] [Google Scholar]
- 22. Biagioni B, Annesi-Maesano I, D’Amato G, Cecchi L. The rising of allergic respiratory diseases in a changing world: from climate change to migration. Expert Rev Respir Med . 2020;14:973–986. doi: 10.1080/17476348.2020.1794829. [DOI] [PubMed] [Google Scholar]
- 23. Koné B, Oulhote Y, Mustapha A, Olaniyan T, Kouame K, Benmarhnia T, et al. Environmental health research challenges in Africa: insights from symposia organized by the ISEE Africa Chapter at ISES-ISEE 2018. Environ Epidemiol . 2019;3:e074. doi: 10.1097/EE9.0000000000000074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Akpinar-Elci M, Berumen-Flucker B, Bayram H, Al-Taiar A. Climate change, dust storms, vulnerable populations, and health in the Middle East: a review. J Environ Health . 2021;84:8–15. [Google Scholar]
- 25.Parry ML, Canziani OF, Palutikof JP, Adger N, Aggarwal P, Agrawala S, et al. Cambridge, United Kingdom: Cambridge University Press; 2007. https://www.ipcc.ch/site/assets/uploads/2018/02/ar4-wg2-ts-1.pdf [Google Scholar]
- 26. GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet . 2020;396:1223–1249. doi: 10.1016/S0140-6736(20)30752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mirsaeidi M, Motahari H, Taghizadeh Khamesi M, Sharifi A, Campos M, Schraufnagel DE. Climate change and respiratory infections. Ann Am Thorac Soc . 2016;13:1223–1230. doi: 10.1513/AnnalsATS.201511-729PS. [DOI] [PubMed] [Google Scholar]
- 28. Boğan M, Kul S, Al B, Oktay MM, Akpinar Elçi M, Pinkerton KE, et al. Effect of desert dust storms and meteorological factors on respiratory diseases. Allergy . 2022;77:2243–2246. doi: 10.1111/all.15298. [DOI] [PubMed] [Google Scholar]
- 29. Al B, Bogan M, Zengin S, Sabak M, Kul S, Oktay MM, et al. Effects of dust storms and climatological factors on mortality and morbidity of cardiovascular diseases admitted to ED. Emerg Med Int . 2018;2018:3758506. doi: 10.1155/2018/3758506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Goudie AS. Dust storms: recent developments. J Environ Manage . 2009;90:89–94. doi: 10.1016/j.jenvman.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 31. Bayram H, Bauer AK, Abdalati W, Carlsten C, Pinkerton KE, Thurston GD, et al. Environment, global climate change, and cardiopulmonary health. Am J Respir Crit Care Med . 2017;195:718–724. doi: 10.1164/rccm.201604-0687PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bayram H, Öztürk AB. In: Climate change and global public health. Pinkerton KE, Rom WN, editors. Cham, Switzerland: Springer International; 2021. Global climate change, desertification, and its consequences in Turkey and the Middle East; pp. 445–458. [Google Scholar]
- 33. Roman J, Viegi G, Schenker M, Ojeda VD, Pérez-Stable EJ, Nemery B, et al. Research needs on respiratory health in migrant and refugee populations: an official American Thoracic Society and European Respiratory Society workshop report. Ann Am Thorac Soc . 2018;15:1247–1255. doi: 10.1513/AnnalsATS.201807-478ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention. Atlanta, GA: Centers for Disease Control and Prevention; 2022. https://www.cdc.gov/nceh/tracking/topics/EnvironmentalJustice.htm [Google Scholar]
- 35.Global Carbon Project. Global Carbon Project; 2017. https://www.globalcarbonproject.org/carbonbudget/archive/2017/GCP_CarbonBudget_2017.pdf [Google Scholar]
- 36. Callahan CW, Mankin JS. Globally unequal effect of extreme heat on economic growth. Sci Adv . 2022;8:1–12. doi: 10.1126/sciadv.add3726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Shaddick G, Thomas ML, Mudu P, Ruggeri G, Gumy S. Half the world’s population are exposed to increasing air pollution. NPJ Clim Atmos Sci . 2020;3:23. [Google Scholar]
- 38.The World Bank. The global health cost of PM2.5 air pollution: a case for action beyond 2021. Washington, DC: The World Bank; 2022. [Google Scholar]
- 39. Tessum CW, Apte JS, Goodkind AL, Muller NZ, Mullins KA, Paolella DA, et al. Inequity in consumption of goods and services adds to racial-ethnic disparities in air pollution exposure. Proc Natl Acad Sci USA . 2019;116:6001–6006. doi: 10.1073/pnas.1818859116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.American Public Health Association. Washington, DC: American Public Health Association; 2019. https://www.apha.org/policies-and-advocacy/public-health-policy-statements/policy-database/2020/01/14/addressing-environmental-justice-to-achieve-health-equity [Google Scholar]
- 41.World Health Organization. Geneva, Switzerland: World Health Organization; 2021. https://www.who.int/news-room/fact-sheets/detail/climate-change-and-health [Google Scholar]
- 42. Knowlton K, Rotkin-Ellman M, King G, Margolis HG, Smith D, Solomon G, et al. The 2006 California heat wave: impacts on hospitalizations and emergency department visits. Environ Health Perspect . 2009;117:61–67. doi: 10.1289/ehp.11594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Michelozzi P, Accetta G, De Sario M, D’Ippoliti D, Marino C, Baccini M, et al. PHEWE Collaborative Group High temperature and hospitalizations for cardiovascular and respiratory causes in 12 European cities. Am J Respir Crit Care Med . 2009;179:383–389. doi: 10.1164/rccm.200802-217OC. [DOI] [PubMed] [Google Scholar]
- 44. Ayres JG, Forsberg B, Annesi-Maesano I, Dey R, Ebi KL, Helms PJ, et al. Environment and Health Committee of the European Respiratory Society Climate change and respiratory disease: European Respiratory Society position statement. Eur Respir J . 2009;34:295–302. doi: 10.1183/09031936.00003409. [DOI] [PubMed] [Google Scholar]
- 45. Marx T, Bernard N, Kepka S, Gérazime A, Mauny F, Desmettre T. Pneumothorax and the environment: a systematic review of the impact of air pollution and meteorology, and a meta-analysis on meteorology factors. Environ Pollut . 2021;283:117089. doi: 10.1016/j.envpol.2021.117089. [DOI] [PubMed] [Google Scholar]
- 46. Madrigano J, Mittleman MA, Baccarelli A, Goldberg R, Melly S, von Klot S, et al. Temperature, myocardial infarction, and mortality: effect modification by individual- and area-level characteristics. Epidemiology . 2013;24:439–446. doi: 10.1097/EDE.0b013e3182878397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Hansel NN, McCormack MC, Kim V. The effects of air pollution and temperature on COPD. COPD . 2016;13:372–379. doi: 10.3109/15412555.2015.1089846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Akpinar-Elci M, Bidaisee S, Nguyen MT, Elci OC. Occupational exposure and respiratory health problems among nutmeg production workers in Grenada, the Caribbean. Int J Occup Environ Health . 2017;23:20–24. doi: 10.1080/10773525.2017.1280948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Grimsley LF, Chulada PC, Kennedy S, White L, Wildfire J, Cohn RD, et al. Indoor environmental exposures for children with asthma enrolled in the HEAL study, post-Katrina New Orleans. Environ Health Perspect . 2012;120:1600–1606. doi: 10.1289/ehp.1104840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Venkatesan P. Epidemic thunderstorm asthma. Lancet Respir Med . 2022;10:325–326. doi: 10.1016/S2213-2600(22)00083-2. [DOI] [PubMed] [Google Scholar]
- 51. Reid CE, Jerrett M, Tager IB, Petersen ML, Mann JK, Balmes JR. Differential respiratory health effects from the 2008 northern California wildfires: a spatiotemporal approach. Environ Res . 2016;150:227–235. doi: 10.1016/j.envres.2016.06.012. [DOI] [PubMed] [Google Scholar]
- 52. Jaakkola JJK, Kiihamäki SP, Näyhä S, Ryti NRI, Hugg TT, Jaakkola MS. Airborne pollen concentrations and daily mortality from respiratory and cardiovascular causes. Eur J Public Health . 2021;31:722–724. doi: 10.1093/eurpub/ckab034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Balmes JR. Where there’s wildfire, there’s smoke. N Engl J Med . 2018;378:881–883. doi: 10.1056/NEJMp1716846. [DOI] [PubMed] [Google Scholar]
- 54. Nguyen HD, Azzi M, White S, Salter D, Trieu T, Morgan G, et al. The summer 2019–2020 wildfires in East Coast Australia and their impacts on air quality and health in New South Wales, Australia. Int J Environ Res Public Health . 2021;18:3538. doi: 10.3390/ijerph18073538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Requia WJ, Amini H, Mukherjee R, Gold DR, Schwartz JD. Health impacts of wildfire-related air pollution in Brazil: a nationwide study of more than 2 million hospital admissions between 2008 and 2018. Nat Commun . 2021;12:6555. doi: 10.1038/s41467-021-26822-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Rice MB, Henderson SB, Lambert AA, Cromar KR, Hall JA, Cascio WE, et al. Respiratory impacts of wildland fire smoke: future challenges and policy opportunities. An official American Thoracic Society workshop report. Ann Am Thorac Soc . 2021;18:921–930. doi: 10.1513/AnnalsATS.202102-148ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Childs ML, Li J, Wen J, Heft-Neal S, Driscoll A, Wang S, et al. Daily local-level estimates of ambient wildfire smoke PM2.5 for the contiguous US. Environ Sci Technol . 2022;56:13607–13621. doi: 10.1021/acs.est.2c02934. [DOI] [PubMed] [Google Scholar]
- 58. Aguilera R, Corringham T, Gershunov A, Leibel S, Benmarhnia T. Fine particles in wildfire smoke and pediatric respiratory health in California. Pediatrics . 2021;147:e2020027128. doi: 10.1542/peds.2020-027128. [DOI] [PubMed] [Google Scholar]
- 59. Cai WCT, Briggs P, Raupach M. Rising temperature depletes soil moisture and exacerbates severe drought conditions across southeast Australia. Geophys Res Lett . 2009;36:L21709. [Google Scholar]
- 60. Kenneth SGY, James N, Brent B. Characterizing changes in drought risk for the United States from climate change. Environ Res Lett . 2010;5:044012. [Google Scholar]
- 61. Kanatani KT, Ito I, Al-Delaimy WK, Adachi Y, Mathews WC, Ramsdell JW, Toyama Asian Desert Dust and Asthma Study Team Desert dust exposure is associated with increased risk of asthma hospitalization in children. Am J Respir Crit Care Med . 2010;182:1475–1481. doi: 10.1164/rccm.201002-0296OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Derbyshire E. Natural minerogenic dust and human health. Ambio . 2007;36:73–77. doi: 10.1579/0044-7447(2007)36[73:nmdahh]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 63. Poole JA, Barnes CS, Demain JG, Bernstein JA, Padukudru MA, Sheehan WJ, et al. Impact of weather and climate change with indoor and outdoor air quality in asthma: a work group report of the AAAAI Environmental Exposure and Respiratory Health Committee. J Allergy Clin Immunol . 2019;143:1702–1710. doi: 10.1016/j.jaci.2019.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Bayram H, Rusznak C, Khair OA, Sapsford RJ, Abdelaziz MM. Effect of ozone and nitrogen dioxide on the permeability of bronchial epithelial cell cultures of non-asthmatic and asthmatic subjects. Clin Exp Allergy . 2002;32:1285–1292. doi: 10.1046/j.1365-2745.2002.01435.x. [DOI] [PubMed] [Google Scholar]
- 65. Bourdrel T, Annesi-Maesano I, Alahmad B, Maesano CN, Bind MA. The impact of outdoor air pollution on COVID-19: a review of evidence from in vitro, animal, and human studies. Eur Respir Rev . 2021;30:200242. doi: 10.1183/16000617.0242-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Wu X, Nethery RC, Sabath MB, Braun D, Dominici F. Air pollution and COVID-19 mortality in the United States: strengths and limitations of an ecological regression analysis. Sci Adv . 2020;6:eabd4049. doi: 10.1126/sciadv.abd4049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Bowe B, Xie Y, Gibson AK, Cai M, van Donkelaar A, Martin RV, et al. Ambient fine particulate matter air pollution and the risk of hospitalization among COVID-19 positive individuals: cohort study. Environ Int . 2021;154:106564. doi: 10.1016/j.envint.2021.106564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Annesi-Maesano I, Maesano CN, D’Amato M, D’Amato G. Pros and cons for the role of air pollution on COVID-19 development. Allergy . 2021;76:2647–2649. doi: 10.1111/all.14818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Kayalar Ö, Arı A, Babuççu G, Konyalılar N, Doğan Ö, Can F, et al. Existence of SARS-CoV-2 RNA on ambient particulate matter samples: a nationwide study in Turkey. Sci Total Environ . 2021;789:147976. doi: 10.1016/j.scitotenv.2021.147976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Mein SA, Annesi-Maesano I, Rice MB. COVID-19 pandemic: a wake-up call for clean air. Ann Am Thorac Soc . 2021;18:1450–1455. doi: 10.1513/AnnalsATS.202012-1542VP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.U.S. Department of Defense. Washington, DC: U.S. Department of Defense; 2014. [Google Scholar]
- 72. Hope B, Friedman N. Climate change is forcing the insurance industry to recalculate. Wall Street Journal . 2018 [Google Scholar]
- 73. Kettle NP, Dow K. Comparing coastal planner expectations of change to climate science projections. J Environ Policy Plann . 2015;17:475–494. [Google Scholar]
- 74. Flavelle C. Moody’s buys climate data firm, signaling new scrutiny of climate risks. New York Times . 2019 [Google Scholar]
- 75. Shankar HM, Rice MB. Update on climate change: its impact on respiratory health at work, home, and at play. Clin Chest Med . 2020;41:753–761. doi: 10.1016/j.ccm.2020.08.004. [DOI] [PubMed] [Google Scholar]
- 76. Senay E, Sarfaty M, Rice MB. Strategies for clinical discussions about climate change. Ann Intern Med . 2021;174:417–418. doi: 10.7326/M20-6443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Rice MB. Climate change at the bedside? Observations from an ATS membership survey. Ann Am Thorac Soc . 2015;12:245–246. doi: 10.1513/AnnalsATS.201412-590ED. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Tong S, Ebi K. Preventing and mitigating health risks of climate change. Environ Res . 2019;174:9–13. doi: 10.1016/j.envres.2019.04.012. [DOI] [PubMed] [Google Scholar]
- 79. Buonocore JJ, Lambert KF, Burtraw D, Sekar S, Driscoll CT. An analysis of costs and health co-benefits for a U.S. power plant carbon standard. PLoS One . 2016;11:e0156308. doi: 10.1371/journal.pone.0156308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Cromar KR, Anenberg SC, Balmes JR, Fawcett AA, Ghazipura M, Gohlke JM, et al. Global health impacts for economic models of climate change: a systematic review and meta-analysis. Ann Am Thorac Soc . 2022;19:1203–1212. doi: 10.1513/AnnalsATS.202110-1193OC. [DOI] [PMC free article] [PubMed] [Google Scholar]