Abstract
A molecular assay for the simultaneous detection of a Staphylococcus aureus-specific gene and the mecA gene, responsible for the resistance to methicillin in staphylococci, was evaluated. The assay included an automated DNA extraction protocol conducted with a MagNA Pure instrument and real-time PCR conducted with a LightCycler instrument. The performance and robustness of the assay were evaluated for a suspension of methicillin-resistant S. aureus (MRSA) strain with a turbidity equivalent to a McFarland standard of 0.5, which was found to be the ideal working concentration. The specificity of the new molecular assay was tested with a panel of 30 gram-negative and gram-positive bacterial strains other than MRSA. No cross-reactivity was observed. In a clinical study, 109 isolates of MRSA were investigated. All clinical MRSA isolates gave positive results for the S. aureus-specific genomic target, and all but one were positive for the mecA gene. In conclusion, the new molecular assay was found to be quick, robust, and laborsaving, and it proved to be suitable for a routine molecular diagnostic laboratory.
Staphylococcus aureus has been known to be a major pathogen causing a wide spectrum of clinical manifestations, such as wound infections, pneumonia, septicemia, and endocarditis, with beta-lactam antibiotics being the drugs of choice for therapy. Since the introduction of methicillin into clinical use in 1961, the occurrence of methicillin-resistant S. aureus (MRSA) has steadily increased and nosocomial infections caused by such isolates have become a serious problem worldwide (2, 14).
The differentiation of MRSA strains from other strains of S. aureus has important implications for the treatment and management of patients with S. aureus infections, and glycopeptides are the drugs of choice for infections caused by MRSA strains. Furthermore, evidence of MRSA requires extensive hygienic precautions to limit the spread of such strains (5, 34).
In the clinical laboratory, S. aureus is identified by growth characteristics and by the subsequent detection of catalase and coagulase activities. Conventional susceptibility testing of S. aureus reliably detects resistance to methicillin or oxacillin if agar dilution tests, disk diffusion tests, or agar screening methods are used according to the standards of the National Committee of Clinical Laboratoy Standards (NCCLS) (16, 17). Standard susceptibility tests, however, are time-consuming. Because the phenotypic expression of methicillin resistance in vitro is heterogeneous and sometimes difficult to induce, false-negative results may be observed (20, 27). Furthermore, S. aureus strains may show a false-negative or noninterpretable result when commercially available kits for coagulase testing (8, 21, 29, 33, 35) are used.
The main mechanism of methicillin resistance is induced by the presence of an additional low-affinity penicillin-binding protein, PBP 2a (encoded by the mecA gene), or, in rare cases, induced by the hyperproduction of β-lactamase (6, 10, 32). Detection of the mecA gene by PCR has been described as a rapid method for the identification of MRSA (1, 4, 11, 13, 15, 23, 24, 28, 36).
In the present study, a molecular assay for the rapid identification of MRSA was established and evaluated. The new assay targeted both the S. aureus gene and the mecA gene within a single PCR and was based on automated DNA isolation and real-time PCR.
MATERIALS AND METHODS
Study design.
A molecular assay for the detection of MRSA based on automated DNA extraction and real-time PCR was established. The new assay was based on automated DNA extraction with a MagNA Pure LC instrument (Roche Molecular Biochemicals, Mannheim, Germany) and real-time PCR with a LightCycler instrument (Roche Diagnostics, Mannheim, Germany).
In the first step, a suspension of the MRSA strain NCTC 10442 (National Collection of Type Cultures and Pathogenic Fungi, Colindale, United Kingdom) with a turbidity equivalent to a McFarland standard of 0.5 (corresponding to 1.5 × 108 CFU per ml) was prepared. The molecular assay based on the automated DNA extraction protocol and real-time PCR on the LightCycler instrument was evaluated. The experiments were repeated five times on different days.
In the second step, the specificity of the new molecular assay was determined with a panel of 30 gram-negative and gram-positive bacterial strains other than MRSA. These included the Escherichia coli standard strain ATCC 25922 (American Type Culture Collection, Manassas, Va.), the Pseudomonas aeruginosa standard strain ATCC 27853, the Enterococcus faecalis standard strain ATCC 29212, and 21 strains of coagulase-negative Staphylococcus spp. (S. saprophyticus, S. epidermidis, S. warneri, and S. haemolyticus) which had been identified in routine diagnostic laboratories. Furthermore, three oxacillin-susceptible S. aureus standard strains (ATCC 29213, ATCC 25923, and NCTC 8325) and three oxacillin-susceptible S. aureus strains which had been isolated in a routine diagnostic laboratory were tested.
In the third step, 109 clinical MRSA isolates were tested. Samples were derived from wounds (49 samples), the respiratory tract (41 samples), and the urinary tract (19 samples). S. aureus strains were identified by their characteristic growth morphologies, Gram stain characteristics, reaction to catalase, coagulase production as detected with the Staphaurex Plus system (Murex Biotech Ltd, Dartford, United Kingdom), the results of the ID32 Staph Apitest (Biomerieux, Marcy l'Etoile, France), and identification with an ID-GPC card (bioMerieux Vitek, Inc., Hazelwood, Mo.) on a VITEK-2 instrument (bioMerieux Vitek, Inc.). Resistance to oxacillin was determined to be indicated by a MIC of ≥4 μg/ml and was tested with the oxacillin Etest (AB Biodisk, Solna, Sweden), according to the guidelines of the NCCLS, and with an AST-P523 card (bioMerieux Vitek, Inc.) on the VITEK-2 instrument. After identification, the strains were stored at −70°C. For molecular testing, clinical specimens were thawed and recultured on blood agar overnight at 37°C. Portions of individual bacterial colonies were suspended in 200 μl of phosphate-buffered saline buffer.
DNA extraction.
The isolation of bacterial DNA was done on a MagNA Pure LC, a benchtop instrument that can extract 32 samples in parallel (12). For DNA extraction, we used a MagNA Pure LC DNA Isolation Kit III (standard protocol; Roche Molecular Biochemicals). The sample volume was 200 μl (a suspension with a turbidity equivalent to a McFarland standard of 0.5); the elution volume was 100 μl. After the completion of the DNA extraction, the MagNA Pure LC cooling block, including the sample carousel with an adequate number of LightCycler capillaries, and the reaction vessels, including the master mix, were placed into the postelution area. After the start of the postelution protocol, which had been programmed prior to the start of the first run, the MagNA Pure LC automatically pipetted 18μl of the master mix and 2 μl of the processed sample into each of the LightCycler capillaries.
Primers and probes.
Oligonucleotide primers and fluorescence-labeled hybridization probes were designed for amplification and sequence-specific detection of both a 188-bp fragment within the mecA gene and a 178-bp fragment within the S. aureus-specific Sa442 gene. The primers and probes were obtained from TIB MolBiol (Berlin, Germany). The nucleotide sequences and positions are listed in Table 1.
TABLE 1.
Oligonucleotide primers and LightCycler hybridization probes used in the PCR assay
| Oligonucleotide | Sequencea | Target gene | Nucleotide positions | GenBank accession no. | Source |
|---|---|---|---|---|---|
| Sa442-F | GTCGGGTACACGATATTCTTCACG | Sa442 | 12-34 | AF033191 | This study |
| Sa442-RS | CTCGTATGACCAGCTTCGGT | Sa442 | 189-168 | AF033191 | This study |
| Sa442-HP-1 | TACTGAAATCTCATTACGTTGCATCGGAA-FAM | Sa442 | 95-123 | AF033191 | Reischl et al. (19) |
| Sa442-HP-2 | Red 705-ATTGTGTTCTGTATGTAAAAGCCGTCTTG-Ph | Sa442 | 126-154 | AF033191 | Reischl et al. (19) |
| Mec-S | CTAGGTGTGGTGAAGATATACCA | mecA | 1596-1619 | X52592 | This study |
| Mec-A | TGAGGTGCGTTAATATTGCCA | mecA | 1783-1763 | X52592 | This study |
| Mec-HP-1 | CAGGTTACGGACAAGGTGAAATACTGATT-FAM | mecA | 1690-1718 | X52592 | Reischl et al. (19) |
| Mec-HP-2 | Red 640-ACCCAGTACAGATCCTTTCAATCTATAGCG-Ph | mecA | 1720-1739 | X52592 | Reischl et al. (19) |
FAM, fluorescein; Red 705, LightCycler Red 705 phosphoramidite; Ph, 3′-phosphate; Red 640, LightCycler Red 640 N-hydroxysuccinimide ester.
The master mixture contained 2 μl of a 10× mixture of LightCycler FastStart DNA master hybridization probes (Roche Diagnostics), 5 mM MgCl2 (final concentration), a 1 μM final concentration of mecA primers, a 0.075 μM final concentration of S. aureus-specific primers, and a 0.2 μM final concentration of hybridization probes.
Real-time PCR.
After the completion of the postelution protocol, the LightCycler capillaries were sealed. Then, the sample carousel with the capillaries was centrifuged in the LightCycler carousel centrifuge and placed into the LightCycler instrument. The cycling protocol consisted of one cycle of 10 min at 95°C followed by 50 cycles consisting of denaturation for 10 s at 97°C, annealing for 10 s at 50°C, and elongation for 15 s at 72°C. After the final cycle, the capillaries were cooled for 2 min at 40°C. Fluorescence curves were analyzed with the LightCycler software (version 3.5.3). Automated calculation of crossing points was done by the second-derivative maximum method. The fluorescence of each capillary was measured at wavelengths of 640 and 705 nm (dual-color option). We selected cycles from 0 to 50 and channel F2/F1 for the mecA gene and channel F3/F1 for the S. aureus-specific gene. Each run contained the MRSA standard strain S. aureus NCTC 10442 and two negative controls (blank reagent and water). Each result was confirmed by the specific peak in the corresponding melting curve.
RESULTS
When a suspension of an MRSA strain with a turbidity equivalent to a McFarland standard of 0.5 was repeatedly tested by a molecular assay based on the automated DNA extraction protocol and real-time PCR on a LightCycler instrument, the crossing points of both targets were always found to be within one cycle. With regard to melting temperatures, no significant differences were observed.
Specificity testing gave negative results for both the mecA gene and the S. aureus-specific gene when we tested the E. coli, P. aeruginosa, and Enterococcus faecalis standard strains. Of all coagulase-negative Staphylococcus strains, the methicillin-resistant strains showed positive results for the mecA gene but negative results for the S. aureus-specific marker. All oxacillin-susceptible S. aureus strains gave positive results for the S. aureus-specific gene but negative results for the mecA gene.
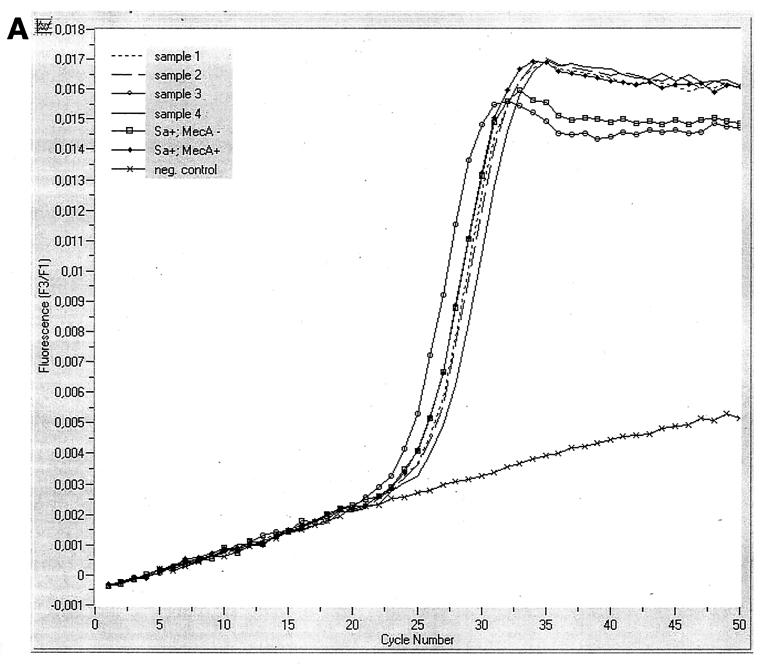
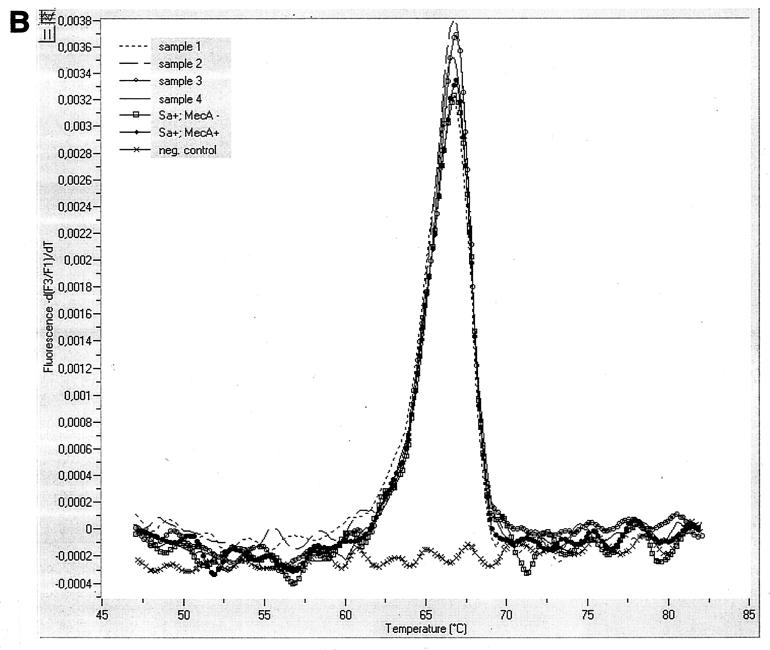
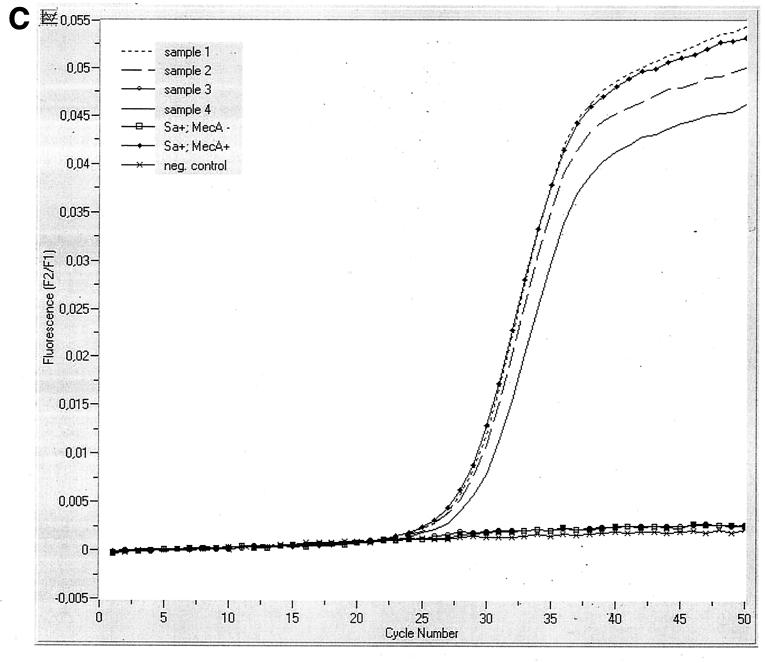
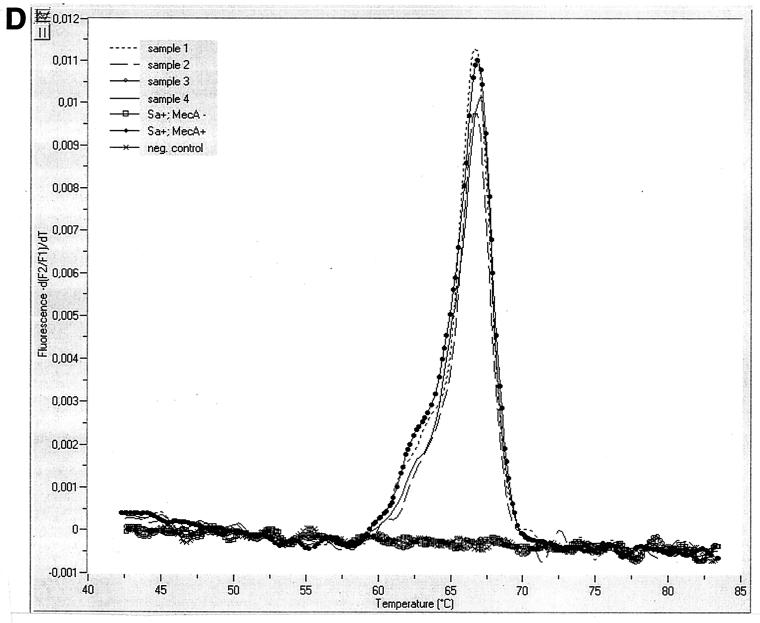
All clinical MRSA isolates showed positive results for the S. aureus-specific gene. Of 109 MRSA strains, 108 gave positive results for the mecA gene; one of the tested MRSA strains gave a negative result for the mecA gene. The melting point curves for each of the targets showed identical product peaks. The results for four clinical samples are shown in Fig. 1.
FIG. 1.
(A) Fluorescence versus cycle number plots (S. aureus-specific genomic fragment Sa442) for clinical samples; (B) melting point curves for the samples in panel A showing identical product peaks; (C) fluorescence versus cycle number plots (mecA gene) of clinical samples; and (D) melting point curves for the samples in panel C showing identical product peaks.
The whole molecular assay was completed within 4 h. The automated DNA extraction with the MagNA Pure LC took 115 min for the extraction of 32 samples. This included a 15-min setup of the MagNA Pure LC. The time required for the postelution protocol was 30 min. After centrifugation, the LC-PCR took another 55 min. No contamination was observed at any time during the study.
DISCUSSION
Since the introduction of semisynthetic penicillins, such as methicillin and oxacillin, for the therapy of infections caused by S. aureus, the occurrence of S. aureus strains resistant to methicillin has steadily increased and MRSA strains have become major nosocomial pathogens (18, 30). Infections with MRSA strains require treatment with glycopeptide antibiotics, which can be nephro- and ototoxic. Additionally, a diagnosis of MRSA infection has important implications for the management of patients since an extensive set of hygienic precautions must be taken to limit the spread of MRSA (3).
Therefore, a rapid and reliable diagnosis of infection by MRSA is of major importance. Although S. aureus is relatively easy to cultivate, conventional identification methods may yield false-positive or false-negative results (9, 31). Standard susceptibility tests are time-consuming. The correct identification of S. aureus and the detection of the mecA gene based on molecular methods have evolved as the method of choice for definitive identification. Earlier studies, however, involved more or less complicated manual DNA extraction protocols, followed by single or multiplex PCR with detection of amplification products on agarose gels (1, 4, 11, 13, 15, 23, 24, 28, 36). Those assays, however, were time-consuming, prone to contamination, and not suitable for routine diagnostic laboratories because of the lack of a hybridization technique.
Recently, a real-time PCR technique for the detection of MRSA with two separate PCRs based on a manual DNA extraction protocol was described (22). In that study, however, no internal control was employed. Reischl et al. (19) described a manual DNA extraction protocol followed by multiplex real-time PCR for the simultaneous detection of the mecA gene and an S. aureus-specific gene which served as an internal control. In comparison to the conditions used in that study, primer compositions and concentrations had to be changed in our study to balance PCR efficiencies for both of the targets by optimization of primer concentrations and product lengths. Because variations in lot-to-lot primer concentrations may exist, it is advisable to adjust the concentrations for each primer lot prior to its first use in routine diagnostics. Following the optimization of the primer concentrations, identical melting point curves for the targets could be shown in this study.
In spite of the growing consensus for the use of molecular methods, they are not yet available in the majority of routine diagnostic laboratories because of their elevated technical requirements. In the present study, a new molecular assay that targets both an S. aureus-specific gene and the mecA gene within a single PCR was established and evaluated. This assay includes an automated DNA extraction protocol on a MagNA Pure instrument and real-time PCR on a LightCycler instrument. Of 109 clinical MRSA strains, 108 could be detected distinctly by the new molecular assay. One isolate showed a negative result for the mecA gene. The reason for this might be one of the rare other mechanisms of methicillin resistance (7, 25, 26).
In conclusion, the new molecular assay was found to be rapid and robust. Because it is a largely automated assay, less hands-on work is needed and it can be incorporated into the workflow of a routine diagnostic laboratory.
Acknowledgments
We gratefully thank Olfert Landt for providing the modified primers and for stimulating discussions.
REFERENCES
- 1.Barski, P., L. Piechowicz, J. Galinski, and J. Kur. 1996. Rapid assay for detection of methicillin-resistant Staphylococcus aureus using multiplex PCR. Mol. Cell. Probes 10:471-475. [DOI] [PubMed] [Google Scholar]
- 2.Benner, E. J., and F. H. Kayser. 1968.. Growing clinical significance of methicillin-resistant Staphylococcus aureus. Lancet ii:741-744. [DOI] [PubMed]
- 3.Boyce, J. M. 2001. MRSA patients: proven methods to treat colonization and infection. J. Hosp. Infect. 48:(Suppl. A):9-14. [DOI] [PubMed]
- 4.Brakstad, O. G., K. Aasbakk, and J. A. Maeland. 1992. Detection of Staphylococcus aureus by polymerase chain reaction amplification of the nuc gene. J. Clin. Microbiol. 30:1654-1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chaix, C., I. Durand-Zaleski, C. Alberti, and C. Brun-Buisson. 1999. Control of endemic methicillin-resistant Staphylococcus aureus: a cost-benefit analysis in an intensive care unit JAMA 18:1745-1751. [DOI] [PubMed] [Google Scholar]
- 6.Chambers, H. F. 1993. Detection of methicillin-resistant staphylococci. Infect. Dis. Clin. N. Am. 7:425-433. [PubMed] [Google Scholar]
- 7.Chambers, H. F. 1997. Methicillin resistance in staphylococci: molecular and biochemical basis and clinical implications. Clin. Microbiol. Rev. 10:781-791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fournier, J. M., A. Boutonnier, and A. Bouvet. 1989. Staphylococcus aureus strains which are not identified by rapid agglutination methods are of capsular serotype 5. J. Clin. Microbiol. 27:1372-1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Frebourg, N. B., D. Nouet, L. Lemée, E. Martin, and J.-F. Lemeland. 1998. Comparison of ATB Staph, Rapid ATB Staph, Vitek, and E-test methods for detection of oxacillin heteroresistance in staphylococci possessing mecA. J. Clin. Microbiol. 36:52-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hartman, B. J., and A. Tomasz. 1984. Low-affinity penicillin-binding protein associated withβ-lactam resistance in Staphylococcus aureus. J. Bacteriol. 158:513-516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kearns, A. M., P. R. Seiders, J. Wheeler, R. Freeman, and M. Steward. 1999. Rapid detection of methicillin-resistant staphylococci by multiplex PCR. J. Hosp. Infect. 43:33-37. [DOI] [PubMed] [Google Scholar]
- 12.Kessler, H. H., G. Muehlbauer, E. Stelzl, E. Daghofer, B. I. Santner, and E. Marth. 2001. Fully automated nucleic acid extraction. MagNA Pure LC. Clin. Chem. 47:1124-1126. [PubMed] [Google Scholar]
- 13.Kohner, P., J. Uhl, C. Kolbert, D. Persing, and F. Cockerill III. 1999. Comparison of susceptibility testing methods with mecA gene analysis for determining oxacillin (methicillin) resistance in clinical isolates of Staphylococcus aureus and coagulase-negative Staphylococcus spp. J. Clin. Microbiol. 37:2952-2961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lowy, F. D. 1998. Staphylococcus aureus infections. N. Engl. J. Med. 339:520-532. [DOI] [PubMed] [Google Scholar]
- 15.Martineau, F., F. J. Picard, P. H. Roy, M. Ouellette, and M. G. Bergeron. 1998. Species-specific and ubiquitous-DNA-based assays for rapid identification of Staphylococcus aureus. J. Clin. Microbiol. 36:618-623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.National Committee for Clinical Laboratory Standards. 1993. Approved standard M2-A5. Performance standards for antimicrobial disk susceptibility tests. National Committee for Clinical Laboratory Standards, Villanova, Pa.
- 17.National Committee for Clinical Laboratory Standards. 1999. Performance standards for antimicrobial susceptibility testing. Ninth informational supplement M100-S9. National Committee for Clinical Laboratory Standards, Wayne, Pa.
- 18.Panlilio, A. L., D. H. Culver, R. P. Gaynes, S. Banerjee, T. S. Henderson, J. S. Tolson, and W. J. Martone. 1992. Methicillin-resistant Staphylococcus aureus in U. S. hospitals, 1975-1991. Infect. Control Hosp. Epidemiol. 13:582-586. [DOI] [PubMed] [Google Scholar]
- 19.Reischl, U., H.-J. Linde, M. Metz, B. Leppmeier, and N. Lehn. 2000. Rapid identification of methicillin-resistant Staphylococcus aureus and simultaneous species confirmation using real-time fluorescence PCR. J. Clin. Microbiol. 38:2429-2433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ribeiro, J., F. D. Vieira, T. King, J. B. D'Arezzo, and J. M. Boyce. 1999. Misclassification of susceptible strains of Staphylococcus aureus as methicillin-resistant S. aureus by a rapid automated susceptibility testing system. J. Clin. Microbiol. 37:1619-1620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ruane, P. J., M. A. Morgan, D. M. Citron, and M. E. Mulligan. 1986. Failure of rapid agglutination methods to detect oxacillin-resistant Staphylococcus aureus. J. Clin. Microbiol. 24:490-492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tan, T. Y., S. Corden, R. Barnes, and B. Cookson. 2001. Rapid identification of methicillin-resistant Staphylococcus aureus from positive blood cultures by real-time fluorescence PCR. J. Clin. Microbiol. 39:4529-4531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tokue, Y., S. Shoji, K. Satoh, A. Watanabe, and M. Motomiya. 1991. Detection of methicillin-resistant Staphylococcus aureus (MRSA) using polymerase chain reaction amplification. J. Exp. Med. 163:31-37. [DOI] [PubMed] [Google Scholar]
- 24.Tokue, Y., S. Shoji, K. Satoh, A. Watanabe, and M. Motomiya. 1992. Comparison of a polymerase chain reaction assay and a conventional microbiolgic method for detection of methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 36:6-9. [DOI] [PMC free article] [PubMed]
- 25.Tomasz, A., H. B. Drugeon, H. M. de Lencastre, D. Jabes, L. McDougall, and J. Bille. 1989. New mechanism for methicillin resistance in Staphylococcus aureus: clinical isolates that lack the PBP 2a gene and contain normal penicillin-binding proteins with modified penicillin-binding capacity. Antimicrob. Agents Chemother. 33:1869-1874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Trees, D. L., and J. J. Iandolo. 1988. Identification of a Staphylococcus aureus transposon (Tn 4291) that carries the methicillin resistance gene(s). J. Bacteriol. 170:149-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ubukata, K., R. Nonoguchi, M. Matsuhashi, and M. Konno. 1989. Expression and inducibility in Staphylococcus aureus of the mecA gene, which encodes a methicillin-resistant S. aureus-specific penicillin-binding protein. J. Bacteriol. 171:2882-2885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ünal, S., J. Hoskins, J. E. Flokowitsch, C. Y. E. Wu, D. A. Preston, and P. L. Skatrud. 1992. Detection of methicillin-resistant staphylococci by using the polymerase chain reaction. J. Clin. Microbiol. 30:1685-1691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ünal, S., K. Werner, P. DeGirolami, F. Barsanti, and G. Eliopoulos. 1994. Comparison of tests for detection of methicillin-resistant Staphylococcus aureus in a clinical microbiology laboratory. Antimicrob. Agents Chemother. 38:345-347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Voss, A., D. Milatovic, C. Wallrauch-Schwarz, V. T. Rosdahl, and I. Braveny. 1994. Methicillin-resistant Staphylococcus aureus in Europe. Eur. J. Clin. Microbiol. Infect. Dis. 13:50-55. [DOI] [PubMed] [Google Scholar]
- 31.Wallet, F., M. Roussel-Delvallez, and R. J. Courcol. 1996. Choice of a routine method for detecting methicillin-resistance in staphylococci. J. Antimicrob. Chemother. 37:901-909. [DOI] [PubMed]
- 32.Waxman, D. J., and J. L. Strominger. 1983. Penicillin-binding proteins and the mechanism of action of beta-lactam antibiotics. Annu. Rev. Biochem. 52:825-869. [DOI] [PubMed] [Google Scholar]
- 33.Weeres-Pothoff, G., C. E. M. Moolhuijzen, and G. P. A. Bongaerts. 1987. Comparison of seven coagulase tests for identification of Staphylococcus aureus. Eur. J. Clin. Microbiol. 6:589-591. [DOI] [PubMed] [Google Scholar]
- 34.Wenzel, R. P., D. R. Reagan, J. S. Bertino, Jr., E. J. Baron, and K. Arias. 1998. Methicillin-resistant Staphylococcus aureus outbreak: a consensus panel's definition and management guidelines. Am. J. Infect. Control 26:102-110. [DOI] [PubMed] [Google Scholar]
- 35.Wilkerson, M., S. McAllister, J. M. Miller, B. J. Heiter, and P. P. Bourbeau. 1997. Comparison of five agglutination tests for identification of Staphylococcus aureus. J. Clin. Microbiol. 35:148-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.York, M. K., L. Gibbs, F. Chehab, and G. F. Brooks. 1996. Comparison of PCR detection of mecA with standard susceptibility testing methods to determine resistance in coagulase-negative staphylococci. J. Clin. Microbiol. 34:249-253. [DOI] [PMC free article] [PubMed] [Google Scholar]