Abstract
Approximately 78.3% of patients with t(8;21) acute myeloid leukemia (AML) express CD19, making it a potential target for chimeric antigen receptor (CAR)-T cell therapy focused on CD19. This prospective phase II trial (NCT03896854) evaluated the safety and efficacy of CD19 CAR-T cell treatment in 10 relapsed CD19-positive t(8;21) AML patients. This study enrolled eight patients with hematologic and two with molecular relapsed AML. The median bone marrow blast percentage was 12.4% (0.1–50.2%), and the blasts exhibited a median CD19 positivity of 55.7% (22.6–97.1%). Genetic profiling revealed TP53 alterations (n = 1), KIT (n = 3) and FLT3-ITD (n = 1) mutations. After lymphodepletion with fludarabine and cyclophosphamide (FC), 5–20 × 106 cells per kilogram of CAR-T cells were administered. All patients experienced grade 3 or higher hematologic toxicities following tumor-reduction chemotherapy and the FC regimen, which were managed for a median of two weeks after CAR-T treatment. Non-hematological toxicities were mild and reversible. Eight patients presented with mild (grade 1–2) cytokine release syndrome (CRS), and one experienced grade 3 CRS. The immune effector cell-associated neurotoxicity syndrome was not observed. All patients achieved complete remission (CR) after CAR-T, with 60% achieving a molecularly MRD-negative CR. RUNX1::RUNX1T1 fusion transcript levels demonstrated a median 2.5-log reduction (range: 0.7–4.5 log; P = 0.002). At a median follow-up of 64.6 months (range: 11.2–88.8 months), the median overall survival and leukemia-free survival were 11.6 and 3.8 months, respectively. The 12-month cumulative incidence of relapse was 53.3%. These findings indicated that CD19 CAR-T was a safe and effective option for relapsed CD19-positive t(8;21) AML.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13045-025-01708-z.
Keywords: Chimeric antigen receptor T cells, CAR-T CD19, t(8;21) translocation, Acute myeloid leukemia, Relapsed
To the editor
Despite the initial response to standard chemotherapy in most t(8;21) acute myeloid leukemia (AML) patients, approximately 35% experience relapse or persistent measurable residual disease (MRD) positivity, conferring a dismal 5-year overall survival rate of ≤ 20% in this setting [1–3]. This poor prognosis stems from the limited therapeutic options available for this molecularly defined subgroup.
Notably, CD19 expression is observed in 78.3% of t(8;21) AML cases [4], representing a potential therapeutic target for CD19-directed chimeric antigen receptor (CAR)-T cell treatment. We first demonstrated the efficacy of CD19 CAR-T cells in two relapsed t(8;21) AML patients, and this finding was subsequently revalidated by Israeli investigators [5, 6]. Based on these early proof-of-concept results, we conducted this prospective trial to evaluate CD19 CAR-T treatment in CD19 + relapsed t(8;21) AML.
This single-center, Phase II trial (NCT03896854, ClinicalTrials.gov) enrolled 10 relapsed t(8;21) AML patients between October 18, 2017, and December 11, 2023, at the First Affiliated Hospital of Soochow University, China. The study protocol received institutional review board approval in accordance with the Declaration of Helsinki guidelines. Baseline characteristics, including prior therapies, cytogenetic/molecular profiles, pre-treatment, blast percentages, CAR-T cell source, CAR-T cell dose, response rates and survival, are tabulated (Table 1). The methodological components, including subject selection criteria, study protocol, CAR construct design, CAR-T cell production procedures, statistical approaches, and endpoint evaluations, were thoroughly documented in the supplementary materials. The study cohort comprised ten patients (eight males and two females). The median age was 31 years (range: 13–52 years). The median follow-up duration was 64.6 months (range: 11.2–88.8 months).
Table 1.
Patient baseline characteristics and treatment outcomes
| Characteristics | N = 10 (%) |
|---|---|
| Median age (range) years | 31 (13–52) |
| Female sex | 2 (20.0%) |
| ECOG performance status ≤ 2 | 10 (100.0%) |
| Median percentage of CD19 positive blasts (%) | 55.7% (22.6–97.1%) |
| Relapsed status | |
| Relapsed after chemotherapy | 8 (80.0%) |
| Relapsed after transplantation | 2 (20.0%) |
| Hematological relapse | 8 (80.0%) |
| Molecular relapse | 2 (20.0%) |
| Molecular Abnormalities | |
| RUNX1::RUNX1T1 | 10 (100.0%) |
| TP53 alteration | 1 (10.0%) |
| KIT mutation | 3 (30.0%) |
| ASXL1 mutation | 4 (40.0%) |
| FLT3-ITD mutation | 1 (10.0%) |
| NRAS mutation | 1 (10.0%) |
| Tumor reduction chemotherapy before CD19 CAR-T infusion | |
| HMA + HAAG | 5 (50.0%) |
| HMA + ECAG | 1 (10.0%) |
| HMA + High dose Ara-C | 1 (10.0%) |
| HMA + Venetoclax + Selinexor | 1 (10.0%) |
| None | 2 (20.0%) |
| Conditioning regimen | |
| FC | 10 (100.0%) |
| Source of CD19 CAR-T | |
| Autologous | 9 (90.0%) |
| Donor | 1 (10.0%) |
| Median CD19 CAR-T dose (range) | 10 (5–20) × 106/kg |
| Clinical responses | |
| CR | 10 (100.0%) |
| CRMRD- | 6 (60.0%) |
| Maintenance therapy | 2 (20.0%) |
| Decitabine alone | 1 (10.0%) |
| Decitabine after allo-HSCT | 1 (10.0%) |
| Survival Status | |
| Alive | 3 (30.0%) |
| Death | 7 (70.0%) |
| - Relapse-related | 6 (85.7%) |
| - GVHD-related | 1 (14.3%) |
| Relapse after CAR-T | |
| - CD19-negative | 5/7 (71.4%) |
Abbreviations: ECOG Eastern Cooperative Oncology Group, HMA Hypomethylating agent, HAAG Homoharringtonine (H), Cytarabine (A), Aclarubicin (A), Granulocyte colony-stimulating factor (G), ECAG Etoposide (E), Cytarabine (C), Aclarubicin (A), Granulocyte colony-stimulating factor (G), Ara-C Cytarabine; FC: Fludarabine (F), Cyclophosphamide (C), CR Complete remission, CRMRD- Measurable residual disease (MRD)-negative complete remission, allo-HSCT Allogeneic hematopoietic stem cell transplantation
All patients experienced grade 3 or higher hematologic toxicities following tumor-reduction chemotherapy and lymphodepletion regimen with fludarabine and cyclophosphamide (FC), including anemia in 8 patients (80%), thrombocytopenia in 8 patients (80%), and neutropenia in 9 patients (90%). The median time of red blood cell transfusions (hemoglobin < 70g/L) was 11 days (range: 8–26 days), and for platelet transfusion independence (platelet counts ≥ 20 × 109/L) was 14 days (range: 0–30 days). The median time to neutrophil recovery (ANC ≥ 0.5 × 109/L) was 12 days (range: 1–24 days). Ultimately, the median time for recovery from all hematologic toxicities was 14 days (range: 1–30 days).
The non-hematological toxicities were transient and manageable, including pulmonary infection (grade 2; n = 1), transient hepatotoxicity (grade 1; n = 1) and hypotension (grade 3; n = 1). Cytokine release syndrome (CRS) occurred in 9 patients (90%), with grades 1 in 4, 2 in 4, and 3 in 1. The grade 3 event was managed with steroid intervention (methylprednisolone 1 mg/kg/day intravenous for 3 days) and supportive care. No immune effector cell-associated neurotoxicity syndrome (ICANS) (ASTCT criteria) [7] was observed.
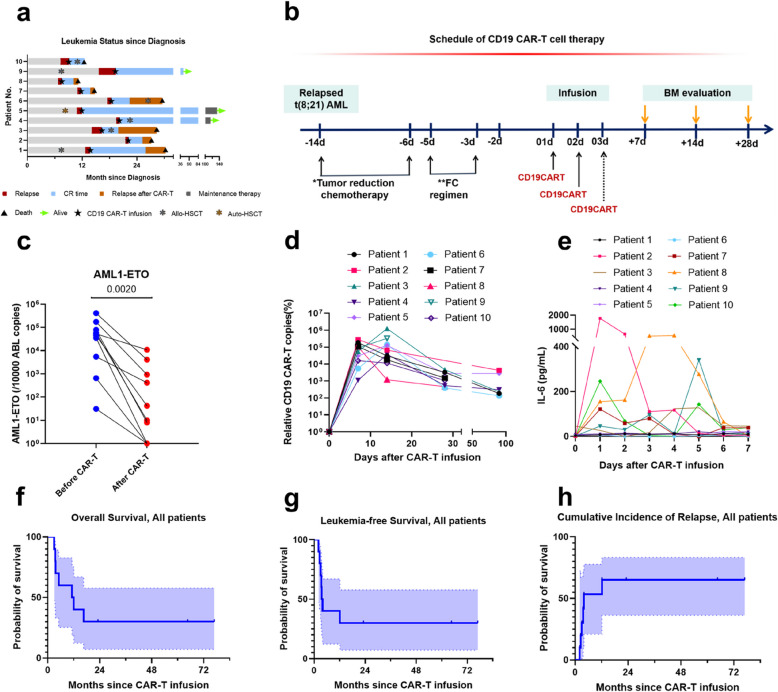
Ten out of 10 patients achieved complete remission (CR) (100% CR rate) post-CAR-T treatment, with 60% attaining molecular MRD-negative CR (CRMRD-) (Fig. 1a, b, Table S2). RUNX1::RUNX1T1 fusion transcript levels showed a median 3.27-log reduction (range: 0.7–4.5 log; P = 0.002) post-CAR-T (Fig. 1c).
Fig. 1.
Treatment Response and Survival of Patients. a Complete remission (CR) status of patients post-CAR-T infusion. Patients 1, 3, 4, 5 and 8 achieved molecular remission. Patients 2, 3, 6, 7 and 8 relapsed within four months, and Patient 1 experienced relapse at 12.2 months after the CD19 CAR-T treatment. b Schedule of the CD19 CAR-T treatment regimen. c Variation in RUNX1::RUNX1T1 fusion gene expression in the bone marrow (BM) measured by quantitative real-time PCR (RT-PCR). d CAR-T cell copy numbers were detected using vector copy numbers (VCN) analysis. e The IL-6 cytokine results during CAR-T cell treatment. f & h 12-month overall survival (OS) and leukemia-free survival (LFS) rates were 45.0% and 46.7%, respectively. h The cumulative incidence of all patients is displayed
The median time to peak levels of CAR-T cells in blood was 8 days after infusion (range: 4–24 days) (Fig. 1d). Longitudinal cytokine profiles (e.g., IL-6) are shown in Fig. 1e and Figure S3. The median peak of IL-6 levels occurred on day 5 (range: 1–10). Figure S1 demonstrated CD19 dynamics and MRD clearance in a representative case (patient 4).
After CAR-T treatment, three patients (patients 3, 4, and 10) underwent allogeneic hematopoietic stem cell transplantation (allo-HSCT), 2 received decitabine-based regimens, and 5 declined further consolidation treatment. Among the three allo-HSCT patients, the patient 10 died of grade IV acute intestinal graft-versus-host disease (GVHD) at 1.5 months post-transplantation, the patient 3 with TP53 alterations succumbed to relapse at 2 months post-transplantation, and the patient 4 receiving decitabine maintenance remained alive in remission. Six patients who underwent allo-HSCT (patients 1, 2, 3, 6, 7, and 8) experienced relapse at a median time of 3.4 months (ranging: 2.1–12.2 months) post-CAR-T therapy. This included five cases of CD19-negative relapse and one case of CD19-positive relapse (patient 8). Several salvage treatments were administered to patients who relapsed after CAR-T, including venetoclax with hypomethylating agent (patients 1, 3), decitabine plus HAAG (Homoharringtonine, Cytarabine, Aclarubicin, combined with Granulocyte colony-stimulating factor) (patient 3), salvage transplantation (patient 6), decitabine combination with CD38 CAR-T (patient 3), and palliative care (patients 2, 7, 8). Finally, seven patients died, and three patients (patients 4, 5, 9) survived after CAR-T treatment. (Figure S2).
The median OS and leukemia-free survival (LFS) were 11.6 months (95% CI, 18.4% to 75.3%) and 3.8 months (95% CI, 18.4% to 75.3%). The 12-month cumulative incidence of relapse (CIR) was 53.3% (95% CI, 20.9% to 77.7%) (Fig. 1f-h). By the last follow-up, three patients were alive (Table S2).
Our study was the first to report the effectiveness of CD19 CAR-T therapy in t(8;21) AML, expanding the research with a larger group, longer follow-up, and a focus on post-CAR-T consolidation. Although all patients achieved CR, the median LFS was only 3.8 months, highlighting the necessity for larger sample sizes and the need for multi-center, collaborative trials to refine treatment strategies. While sequential allo-HSCT or maintenance treatment may help consolidate CAR-T-induced remission, future trials should focus on larger cohorts to evaluate these strategies.
Supplementary Information
Acknowledgements
The authors thank all the study team members, patients, and their families.
Abbreviations
- CAR-T
Chimeric antigen receptor T cell
- allo-HSCT
Allogeneic hematopoietic stem cell transplantation
- CR
Complete remission
- AML
Acute myeloid leukemia
- FC
Fludarabine + cyclophosphamide
- MRD
Measurable residual disease
- OS
Overall survival
- ANC
Absolute neutrophil count
- CRS
Cytokine release syndrome
- CRMRD-
MRD-negative complete remission
- IV
Intravenous
- HAAG
Homoharringtonine (H), Cytarabine (A), Aclarubicin (A), Granulocyte colony-stimulating factor (G)
- ECAG
Etoposide (E), Cytarabine (C), Aclarubicin (A), Granulocyte colony-stimulating factor (G)
- GVHD
Graft-versus-host disease
- LFS
Leukemia-free survival
- CIR
Cumulative incidence of relapse
Authors’ contributions
TXW and WDP were responsible for the concept and design of the study. YJ and CQY collected and analyzed the data and wrote the manuscript. CW and DHP treated the patients and assisted in the data collection. All the authors read and approved the final manuscript.
Funding
This work was supported by research grants from National Natural Science Foundation of China (82070162, 82341209), Frontier Clinical Technical Project of Suzhou Science and Technology plan (SKY2022001), Bethune Charitable Foundation (BCF-IBW-XY-20220930–13), Suzhou diagnosis and treatment project of Clinical Key Diseases (LCZX202201), China International Medical Foundation (Z-2018–31-2102–4), Boxi clinical research project of The First Affiliated Hospital of Soochow University (BXLC005), the Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD).
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
This clinical trial was approved by the Ethics Committee of the First Affiliated Hospital of Soochow University.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jia Yin, Qing-Ya Cui and Hai-Ping Dai contributed equally to this work.
Contributor Information
De-Pei Wu, Email: drwudepei@163.com.
Xiao-Wen Tang, Email: xwtang1020@163.com.
References
- 1.Yin JA, O’Brien MA, Hills RK, Daly SB, Wheatley K, Burnett AK. Minimal residual disease monitoring by quantitative RT-PCR in core binding factor AML allows risk stratification and predicts relapse: results of the United Kingdom MRC AML-15 trial. Blood. 2012;120:2826–35. [DOI] [PubMed] [Google Scholar]
- 2.Marcucci G, Mrózek K, Ruppert AS, et al. Prognostic factors and outcome of core binding factor acute myeloid leukemia patients with t(8;21) differ from those of patients with inv(16): a Cancer and Leukemia Group B study. J Clin Oncol. 2005;23(24):5705–17. [DOI] [PubMed] [Google Scholar]
- 3.Schlenk RF, Benner A, Krauter J, et al. Individual patient data-based meta-analysis of patients aged 16 to 60 years with core binding factor acute myeloid leukemia: a survey of the German Acute Myeloid Leukemia Intergroup. J Clin Oncol. 2004;22(18):3741–50. [DOI] [PubMed] [Google Scholar]
- 4.Kita K, Nakase K, Miwa H, et al. Phenotypical characteristics of acute myelocytic leukemia associated with the t(8;21)(q22;q22) chromosomal abnormality: frequent expression of immature B-cell antigen CD19 together with stem cell antigen CD34. Blood. 1992;80(2):470–7. [PubMed] [Google Scholar]
- 5.Qu C, Li Z, Kang L, Wang Y, Dai H, Yin J, et al. Successful treatment of two relapsed/refractory t(8;21) acute myeloid leukemia patients by CD19-directed chimeric antigen receptor T cells. Bone Marrow Transplant. 2019;54:1138–40. [DOI] [PubMed] [Google Scholar]
- 6.Danylesko I, Jacoby E, Yerushalmi R, et al. Remission of acute myeloid leukemia with t(8;21) following CD19 CAR T-cells. Leukemia. 2020;34(7):1939–42. [DOI] [PubMed] [Google Scholar]
- 7.Lee DW, Santomasso BD, Locke FL, et al. ASTCT Consensus Grading for Cytokine Release Syndrome and Neurologic Toxicity Associated with Immune Effector Cells. Biol Blood Marrow Transplant. 2019;25(4):625–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.