Abstract
Background
BCC (BCC) is the most common form of nonmelanocytic skin cancer, particularly prevalent in sun-exposed areas like the head and neck. BCC in the nasal vestibule is rare, with an incidence of only 0.01 %. This case report examines the clinical presentation and management of BCC in this unusual location.
Case presentation
A 65-year-old male with no significant medical history presented with a two-year history of a mass sensation in the left nasal vestibule, accompanied by recurrent epistaxis. Examination revealed a firm, rubbery, and ulcerated 1 cm mass. Histopathologic findings confirmed Micronodular BCC, leading to surgical excision and reconstruction using posterior auricular skin. Despite successful removal, pathological analysis showed positive margins, necessitating careful follow-up.
Discussion
The report discusses the rising global incidence of BCC due to increased solar exposure and an aging population, with 80 % of cases occurring in the head and neck. While the nasal tip and upper lateral surface are common sites, BCC in the nasal vestibule is exceedingly rare. Differential diagnoses include various premalignant and malignant conditions. Surgical excision with adequate margins is the preferred treatment, alongside options like topical agents and Mohs micrographic surgery for less advanced cases. The challenges of tissue reconstruction post-excision are addressed, recommending total skin grafts or specific flaps depending on tissue loss.
Conclusion
This report highlights the rarity and clinical significance of BCC in the nasal vestibule, advocating for increased awareness among healthcare professionals regarding atypical skin cancer presentations and emphasizing the importance of early detection and management.
Keywords: BCC, Nasal vestibule, Surgical oncology, ENT
Highlights
-
•
Rare nasal vestibule BCC: 0.01 % incidence; atypical site needing clinical vigilance for early detection
-
•
Case: 65 M with 2-year nasal mass, recurrent epistaxis; pathology analysis confirmed micronodular BCC.
-
•
Surgical outcome: Excision + auricular graft; positive margins noted post-resection, no recurrence at follow-up.
-
•
BCC trends: Rising global cases linked to UV/aging; 80 % affect head/neck, rare sites demand tailored care.
-
•
Clinical implications: Highlights need for awareness of atypical BCC presentations & research on complex-site therapies.
1. Introduction
BCC (BCC) represents the most prevalent form of nonmelanocytic skin cancer. According to estimates from the American Cancer Society, over 2 million individuals received treatment for non-melanoma skin cancers in 2006, with the majority being diagnosed with BCC. The primary risk factor associated with the development of BCC is exposure to ultraviolet (UV) radiation. This estimation specifically pertains to the United States. Conversely, a recent study conducted in 2019 concluded that the burden of disease associated with non-melanoma skin cancer (NMSC) is expected to either increase or remain at high levels.
Mazeron et al. conducted a study that detailed the anatomical distribution of BCC on the nose, revealing that the majority of cases were located on the external nose, specifically at the ala (26 %), upper lateral surface (18 %), tip (15 %), nasolabial fold (13 %), bridge (12 %), root (11 %), and columella (1 %) [1,2].
According to the classification established by the World Health Organization (WHO), BCC can be categorized into several distinct subtypes, which include: superficial BCC, nodular (solid) BCC, micronodular BCC, infiltrative BCC, fibroepithelial BCC (commonly referred to as Pinkus), BCC with adnexal differentiation, basosquamous carcinoma, and keratotic BCC [3,4]. BCC occurring in the nasal vestibule is exceedingly rare, with an incidence of only 0.01 % [5].
BCC of the nasal vestibule, although infrequent, presents distinct clinical challenges due to its anatomically complex location and the nonspecific nature of its early symptoms, as highlighted by various case reports. Bajoghli and Gassmann [15] emphasize the condition's tendency for misdiagnosis, often mimicking benign lesions, which can result in treatment delays and an increased risk of local invasion. Case studies by Arnaud et al. and B. Khademi et al. [16,17] illustrate the potential for aggressive tumor behavior, including intranasal extension, necessitating careful surgical interventions such as full-thickness skin grafts or Mohs micrographic surgery to preserve functional integrity and reduce recurrence rates.
The increasing global prevalence of BCC, attributed to aging demographics and cumulative UV exposure [13], highlights the importance of identifying uncommon manifestations, such as those occurring in the nasal vestibule. These cases necessitate specialized management strategies to effectively navigate the associated diagnostic and therapeutic challenges [15,16].
This report presents a case of BCC located in the left nasal vestibule of a 65-year-old male patient, who sought medical attention primarily due to bleeding associated with an ovoid mass formation within his nasal cavity.
2. Case presentation
A 65-year-old male with no significant medical history, including a lack of chronic sun exposure, smoking, and drug abuse, presented to our institution with a primary complaint of a mass sensation located on the medial aspect of his nasal vestibule. This sensation had been persistent for two years prior to his admission. The patient did not seek medical attention until he was referred to our clinic.
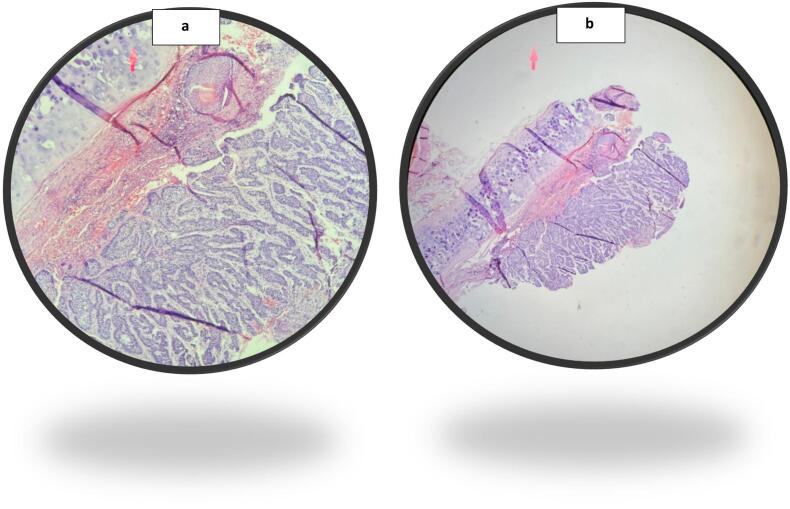
He reported a mass-like formation in the nasal vestibule, which was associated with progressive and recurrent episodes of bleeding (epistaxis). Notably, he denied any additional nasal symptoms such as nasal obstruction, rhinorrhea, or pain. Physical examination revealed a firm, rubbery, and ulcerated mass measuring 1 × 1 cm in the left vestibule of the nose. Subsequent evaluations included a fine needle aspiration (FNA), which showed clinical characteristics of BCC. Finally, the biopsy sample obtained post-resection confirmed the presence of Micronodular BCC, measuring 7.5 × 0.5 × 0.2 mm, located in the left nasal vestibule (see Fig. 1a and b).
Fig. 1.
a and b. Illustrates The neoplastic infiltrate observed in basaloid squamous cell carcinoma (BSCC) is primarily characterized by the presence of basaloid cells, which exhibit pleomorphic and hyperchromatic nuclei, an elevated nuclear-to-cytoplasmic ratio, and heightened mitotic activity. This includes atypical mitoses and nuclear palisading at the periphery of the neoplastic lobule, notably without accompanying stromal retraction. Furthermore, a distinctive feature of BSCC is the occurrence of comedonecrosis within the central regions of the neoplastic lobules. Additionally, this area demonstrates pronounced cytoplasmic alterations.
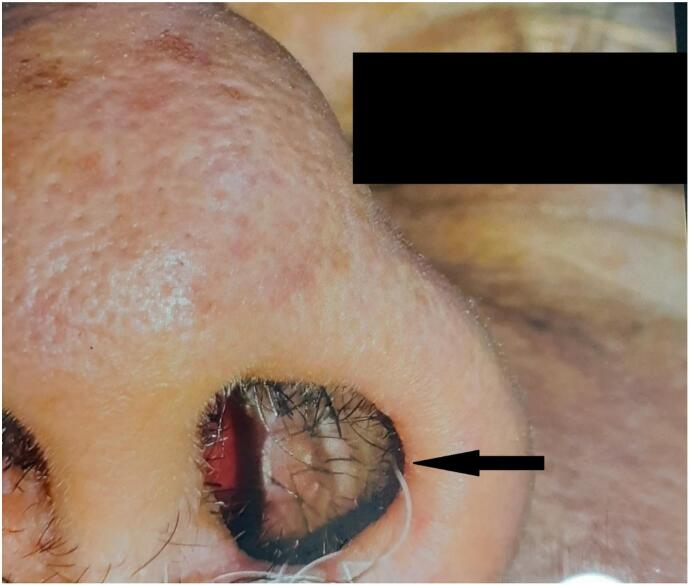
Following the diagnosis, the patient underwent surgical excision of the mass (Fig. 2). The procedure involved utilizing posterior auricular skin to reconstruct the defect created by the resection of the vestibular skin and cartilage. More specifically, the mass located within the nasal cavity primarily affected the skin, while the cartilaginous structures of the nasal alae remained intact. As a result, the tumor resection was performed with relative ease, and no additional surgical interventions, such as the use of flaps, were required, as the integrity of the alar and cartilaginous tissues was preserved.
Fig. 2.
Demonstrates the successful resection of the tumor with the absence of recurrence within a follow-up period of three months.
A biopsy was submitted to the pathology department, which further confirmed the diagnosis of BCC of the nasal vestibule. However, margin resection results indicated positive margins. Upon discharge, the patient was scheduled for a follow-up appointment three months' post-operation, which demonstrated no evidence of recurrence. Additionally, the patient has been rescheduled for a second follow-up appointment in three months to closely monitor any potential tumor recurrence and to assess the need for adjuvant therapy.
3. Methods
This study was conducted following SCARE Guidelines Criteria [12].
4. Discussion
The prevalence of BCC (BCC) is on the rise globally, attributed to heightened exposure to solar ultraviolet radiation and the aging population [2,6]. Approximately 80 % of all BCC cases are located in the head and neck region, with 25–30 % of these cases specifically occurring on the nose [2,7].
The most frequently affected areas of the nose include the nasal tip, the upper lateral surface, and the ala nasi [14]. Notably, fewer than 1 % of BCC located on the nose arise in the nasal vestibule. The differential diagnoses for these lesions encompass premalignant conditions, such as actinic keratosis and keratoacanthoma, as well as malignant neoplasms, including melanoma and squamous cell carcinoma [2,5,6].
Surgical excision with an adequate margin is recommended as the preferred treatment modality for BCC. The primary objective of this treatment is to achieve complete tumor resection while maintaining both functional integrity and aesthetic appearance. A range of surgical and medical interventions are available for the management of BCC. Surgical excision is typically indicated for lesions that are not in advanced stages. Alternative treatment options, which are utilized less frequently, include topical agents such as 5-fluorouracil (5-FU) and imiquimod, as well as cryosurgery, intralesional injections, photodynamic therapy, and Mohs micrographic surgery. Additionally, radiation therapy may be considered in cases where surgical intervention is contraindicated or when resection margins are found to be positive [6,8,9].
The reconstruction of the nasal vestibule requires a sophisticated methodology tailored to the specific characteristics of the defect, including its location, depth, and individual patient factors. For superficial defects limited to the cutaneous layers, primary closure or full-thickness skin grafts (FTSGs) are generally sufficient, as they provide reliable aesthetic and functional outcomes with minimal associated morbidity. In contrast, in cases where tumors infiltrate deeper structures, such as cartilage or the nasal alar framework—commonly observed in advanced BCCs—the use of local flaps, such as paramedian forehead flaps (PMFFs), becomes essential [10,11].
These flaps offer significant vascularity and structural integrity for multi-layered defects, adhering to the principles of subunit-based reconstruction [16]. This perspective is supported by case reports indicating that forehead flaps are particularly advantageous for composite defects involving both skin and cartilage, while simpler cutaneous defects may be effectively managed through conservative excision and primary repair [15].
5. Conclusion
Our case involving a 65-year-old male highlights the necessity for increased awareness among healthcare professionals regarding atypical manifestations of BCC, particularly in less common anatomical sites. The successful diagnosis and surgical treatment of this case emphasize the critical role of early detection and the implementation of appropriate management strategies to achieve optimal patient outcomes. In light of the rising incidence of BCC attributed to factors such as UV exposure and an aging demographic, there is a pressing need for further research to investigate effective treatment options and reconstructive techniques specifically designed for lesions in anatomically challenging areas like the nasal vestibule.
Institution of the study
Khalili Hospital, ENT Department, Shiraz University of medical sciences.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
This research was deemed exempt from ethical approval in accordance with the regulations set forth by Shiraz medical university’ Ethical Committee.
Funding
None.
Author contribution
Reza Kaboodkhani developed the conceptual framework for the study, while, Sajjad Soltani and Alireza Yousefi performed the surgical procedures, and cured the data. Shayan Yousufzai was responsible for project administration, visualization, initial draft composition, review and revision. Negar Fatehi assisted in investigation; Mahsan Nadgaran assisted in surgical procedure, conducted patient interview and assessed the patient's follow-up.
Guarantor
Alireza Yousefi and Shayan Yousufzai.
Declaration of competing interest
The authors declare no competing interest.
References
- 1.Veness M.J., Chong L., Tiver K., Gebski V. BCC of the nose: an Australian and New Zealand radiation oncology patterns-of-practice study. J. Med. Imaging Radiat. Oncol. 2008;52(4):382–393. doi: 10.1111/j.1440-1673.2008.01974.x. Aug. (PMID: 18811764) [DOI] [PubMed] [Google Scholar]
- 2.Wollina U., Bennewitz A., Langner D. BCC of the outer nose: overview on surgical techniques and analysis of 312 patients. J Cutan Aesthet Surg. 2014;7(3):143–150. doi: 10.4103/0974-2077.146660. Jul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peris K., Fargnoli M.C., Garbe C., Kaufmann R., Bastholt L., Seguin N.B., Bataille V., Marmol V.D., Dummer R., Harwood C.A., Hauschild A., Höller C., Haedersdal M., Malvehy J., Middleton M.R., Morton C.A., Nagore E., Stratigos A.J., Szeimies R.M., Tagliaferri L., Trakatelli M., Zalaudek I., Eggermont A., Grob J.J., European Dermatology Forum (EDF), the European Association of Dermato-Oncology (EADO) and the European Organization for Research and Treatment of Cancer (EORTC) Diagnosis and treatment of BCC: European consensus-based interdisciplinary guidelines. Eur. J. Cancer. 2019;118:10–34. doi: 10.1016/j.ejca.2019.06.003. Sep. Epub 2019 Jul 6. PMID: 31288208. [DOI] [PubMed] [Google Scholar]
- 4.Alter M., Hillen U., Leiter U., Sachse M., Gutzmer R. Current diagnosis and treatment of BCC. J. Dtsch. Dermatol. Ges. 2015;13(9):863–874. doi: 10.1111/ddg.12798. Sep. quiz 875. (PMID: 26882375) [DOI] [PubMed] [Google Scholar]
- 5.Mazeron J.J., Chassagne D., Crook J., Bachelot F., Brochet F., Brune D., Brunin F., Bunescu U., Daly N., Danczak S., et al. Radiation therapy of carcinomas of the skin of nose and nasal vestibule: a report of 1676 cases by the Groupe Europeen de Curiethérapie. Radiother. Oncol. 1988;13(3):165–173. doi: 10.1016/0167-8140(88)90052-7. Nov. (PMID: 3146781) [DOI] [PubMed] [Google Scholar]
- 6.Kim Y.J., Cho H.H., Kim S.O., Lee J.B., Lee S.C. Reconstruction algorithm for nasal BCC with skin involvement only: analysis of 221 cases repaired by minor surgery. Clin. Exp. Dermatol. 2015;40(7):728–734. doi: 10.1111/ced.12676. Oct. Epub 2015 May 11. PMID: 25959078. [DOI] [PubMed] [Google Scholar]
- 7.Yigider A.P., Kayhan F.T., Yigit O., Kavak A., Cingi C. Skin diseases of the nose. Am. J. Rhinol. Allergy. 2016;30(3):83–90. doi: 10.2500/ajra.2016.30.4318. May. (PMID: 27216341) [DOI] [PubMed] [Google Scholar]
- 8.Levendag PC, Nijdam WM, van Moolenburgh SE, Tan L, Noever I, van Rooy P, Mureau MA, Jansen PP, Munte K, Hofer SO. Interstitial radiation therapy for early-stage nasal vestibule cancer: a continuing quest for optimal tumor control and cosmesis. Int. J. Radiat. Oncol. Biol. Phys. 2006 Sep 1;66(1):160–9. doi: 10.1016/j.ijrobp.2006.03.041. Epub 2006 Jul 12. PMID: 16839706. [DOI] [PubMed]
- 9.Takata Pontes L., Fantelli Stelini R., Cintra M.L., Magalhães R.F., Velho P.E., Moraes A.M. The importance of superficial BCC in a retrospective study of 139 patients who underwent Mohs micrographic surgery in a Brazilian university hospital. Clinics (Sao Paulo) 2015;70(11):721–725. doi: 10.6061/clinics/2015(11)01. Nov. PMID: 26602517; PMCID: PMC4642494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.El Mazouz S., Fejjal N., Hafidi J., Cherkab L., Mejjati H., Belfqih R., Gharib N., Abbassi A. La Greffe de Peau dans le Traitement des Sequelles de la Main Brulee. A Propos de 152 Cas - Experience du Service de Chirurgie Plastique du Centre Hospitalier Universitaire Ibn-Sina, Rabat, Maroc [Skin grafting in the treatment of hand burns sequelae in relation to 152 cases. Report from Department of Plastic Surgery, University Hospital Ibn Sina] Ann Burns Fire Disasters. 2010;23(1):39–42. Mar 31. French. PMID: 21991196; PMCID: PMC3188241. [PMC free article] [PubMed] [Google Scholar]
- 11.Martin D., Barthélémy I., Mondie J.M., Grangier Y., Pélissier P., Loddé J.P. Les épithéliomas faciaux: considérations générales, moyens et indications chirurgicales [Facial epitheliomas: general considerations, surgical techniques and indications] Ann. Chir. Plast. Esthet. 1998;43(4):311–364. Aug. French. PMID: 9926468. [PubMed] [Google Scholar]
- 12.Sohrabi C., Mathew G., Maria N., Kerwan A., Franchi T., Agha R.A. The SCARE 2023 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. Lond. Engl. 2023;109(5):1136. doi: 10.1097/JS9.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hu W., Fang L., Ni R., Zhang H., Pan G. Changing trends in the disease burden of non-melanoma skin cancer globally from 1990 to 2019 and its predicted level in 25 years. BMC Cancer. 2022;22(1):836. doi: 10.1186/s12885-022-09940-3. Jul 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hasan A., Kandil A.M., Al-Ghamdi H.S., Alghamdi M.A., Nasr M., Naeem S.A., Abd-Elhay W.M., Mohamed O.K.E., Ibrahim H.S.A., Ahmed E.M., Abdrabo A.E.M., Elgohary S.A. Sun-exposed versus sun-protected cutaneous basal cell carcinoma: Clinico-pathological profile and p16 immunostaining. Diagnostics (Basel). 2023;13(7):1271. doi: 10.3390/diagnostics13071271. Mar 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bajoghli A.A., Gassmann K. Basal cell carcinoma in the nasal vestibule. J. Drugs Dermatol. 2020;19(3):333–334. Mar 1. (PMID: 32550683) [PubMed] [Google Scholar]
- 16.Arnaud K., Jibbe A., Patel P., Clayton A. Basal cell carcinoma of nasal vestibule with significant intranasal extension. Dermatologic Surg. 2022;48(7):780–781. doi: 10.1097/DSS.0000000000003480. Jul 1. Epub 2022 May 24. PMID: 35617084. [DOI] [PubMed] [Google Scholar]
- 17.Khademi B., Soltani S., Yousefi A., Heidari P., Mardani Z., Yousufzai S. Ocular invasion in sinonasal malignant melanoma: A case report and review of literature. Int. J. Surg. Case Rep. 2025;127:110904. doi: 10.1016/j.ijscr.2025.110904. Feb. Epub 2025 Jan 20. PMID: 39842280; PMCID: PMC11788794. [DOI] [PMC free article] [PubMed] [Google Scholar]