Abstract
Background
The relationship between life satisfaction and mental health problems had been confirmed in many existed studies, but the underlying mediating and moderating effect of sleep disturbance and per capita bedroom area (PCBA) behind this association had never been identified. This study aimed to explore the mediating role of sleep disturbance and the moderating effect of PCBA on the association between life satisfaction and mental health problems.
Methods
Multistage cluster random sampling method was used to select the participants and finally 613 migrant older adults with children (MOAC) were included in the survey. A conditional process model was performed to examine the relationship between life satisfaction and mental health problems, as well as the mediating effect of sleep disturbance and the moderating effect of PCBA.
Results
Life satisfaction was negatively associated with mental health problems, and sleep disturbance could mediate their association. Furthermore, the direct effect of life satisfaction on mental health problems and the indirect effect of sleep disturbance in the relationship were moderated by PCBA, but it only moderated the direct effect and the second indirect link (sleep disturbance-mental health problems) of the mediating effect. Both these two effects were stronger for MOAC with a low level of PCBA.
Conclusions
Life satisfaction had negative effect on mental health problems. PCBA moderated the direct effect of life satisfaction on mental health problems and the mediating effect of sleep disturbance on mental health problems. For MOAC with a low level of life satisfaction and high sleep disturbance, particularly those with a low level of PCBA, targeted implication for the community, family members and MOAC were proposed to improve the mental health of MOAC.
Keywords: Mental health problems, Life satisfaction, Sleep disturbance, Per capita bedroom area, Migrant older adults following children, Conditional process analysis
Background
With the fast development of aging and urbanization over the past decades, the migrant population of China reached 376 million in 2020 [1]. Meanwhile, the number of migrant older adults in China also increased rapidly since 2000 and reached 13.4 million in 2015, with the annual average growth rate was 6.6% [2]. Among these migrant older adults, some of them migrated following their children to big cities to take care their grandchildren or reunite with their family, they were defined as migrant older adults with children (MOAC) [3]. MOAC could participate in caring grandchildren, food cooking and household chores to reduce the burden of their children, thus playing an important role in the maintenance of family function and harmonious society. However, the migrant older adults were also the vulnerable populations, since they were suffered from lower healthcare utilization [4, 5], social integration problems [6] and mental health problems [7, 8]. Therefore, to carry out the research on the mental health problems of the MOAC could help identify modifiable risk factors that affected mental health and promoted the improvement in mental health status of MOAC; it was conducive to promoting MOAC’s sense of self-worth and better integration into family and society.
Life satisfaction referred to a subjective assessment of the quality of one’s life [9]. which had been confirmed to be one important determinants of mental health problems [10]. A study among the young adults showed that low life satisfaction was associated with psychological problems [11]. Meanwhile, a study among older adults in US found that most domains of life satisfaction were associated with psychological outcomes [12] and a study among university students in Korea illustrated that better life satisfaction was associated with a lower risk of depression [13]. Thus, the association between life satisfaction and mental health problems did exist, yet the underlying mediating and moderating mechanisms behind this association had not been identified, not mentioned in the MOAC group.
Sleep disturbance was common in older adults [14], which had been confirmed as a risk factor for multiple mental health problems [15–18], and was usually used as an umbrella term to refer to a variety of sleep problems including sleep disorders, insomnia, hypersomnia, poor sleep quality, and inadequate sleep duration [19]. Furthermore, many studies had clarified the effect of life satisfaction on sleep disturbance [20–23], a study among the middle school students in China showed that life satisfaction was negatively correlated with sleep quality [20]. Accordingly, we conjectured that sleep disturbance may be an intermediate process from life satisfaction to mental health problems. To date, the association between life satisfaction and mental health problems via sleep disturbance remained unexplored, let alone such association among the MOAC.
Per capita bedroom area (PCBA) represented the size of the bedroom of MOAC in this study. Previous study showed that housing situation was associated with people’s psychological health [24] and the household crowding was found to be a major risk factor for epidemic disease [25]. Moreover, a study in New Zealand showed the significant association between the housing circumstances and psychological distress [26]. However, no study had clarified the association between PCBA and mental health problems, not mentioned the moderated effect of PCBA between life satisfaction and mental health problems, as well as sleep disturbance and mental health problems in a moderated mediation model.
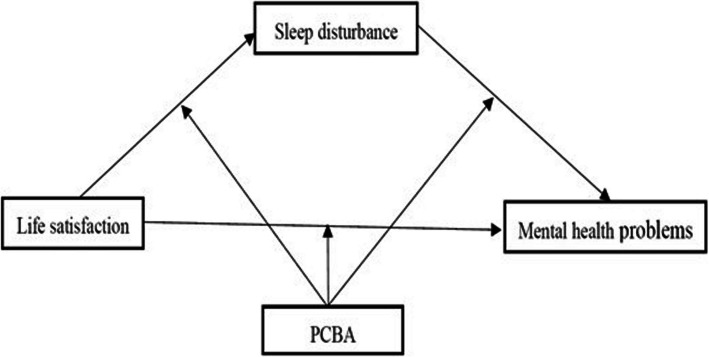
In summary, the first aim of this study was to test whether sleep disturbance mediated the relationship between life satisfaction and mental health problems, the second aim was to investigate the moderated role of PCBA (including the moderated effect on the direct effect in the relationship between life satisfaction and mental health problems, as well as the indirect effect between life satisfaction and mental health problems through sleep disturbance), the third aim was to recommend implications to reduce mental health problems among MOAC and to promote a better life for MOAC in the migrated city. Based on the social ecological model of sleep and social ecological model of sleep and health [27, 28], the conceptual framework of the study was shown in Fig. 1, and three hypotheses were proposed as follow:
Hypothesis 1. Life satisfaction would be negatively and directly associated with mental health problems.
-
Hypothesis 2. Sleep disturbance would mediate the relation between life satisfaction and mental health problems.
Hypothesis 3. PCBA would moderate the effects of life satisfaction and sleep disturbance on mental health problems.
Fig. 1.
The proposed theoretical moderated-mediation model. Note: the first half indirect effect referred to the line from life satisfaction to sleep disturbance; the second half indirect effect referred to the line from sleep disturbance to mental health problems
Methods
Participants
A total of 613 MOAC was selected in Weifang City, China, in August 2021. According to the 7th National census of Weifang City, the total household population of the city was 9.39 million and the population aged 60 and above was 2.04 million, account for 21.7% of the total population, the migrant population in the city was 2.38 million [29].
Multistage cluster random sampling was employed to select the participants. Firstly, four districts were selected as the primary sampling units (PSUs) based on the economic development and geographical location of Weifang city. Secondly, one sub-district from each PSUs were randomly selected as secondary sampling units (SSUs). Thirdly, one community were randomly selected from each of the SSUs. The migrant population aged 60 years or above in the selected communities who came to live in Weifang with their children more than 3 months constituted the whole sample.
The trained investigators conducted face-to-face interviews with each participant for approximately 20 minutes. Initially, 616 MOAC were selected and interviewed. However, three participants were excluded as they answered their questionnaires without logical or incompletely. Ultimately, a total of 613 participants were included in the database.
Assessment and measurements
Mental health problems
Mental health problems was assessed by the Depression Anxiety Stress Scale (DASS- 21) [30, 31], it was proposed by P. F. Lovibond and S. H. Lovibond [32]. It included three subscales-depression, anxiety and stress, totally 21 items, this scale was rated by a 4-point scale (0–3) and the scores of the three subscales and total scale were calculated, with higher scores indicating higher level of negative mental status [33]. The Cronbach's alpha coefficient was 0.865 for DASS- 21 in this study.
Life satisfaction
The Satisfaction with Life Scale (SWLS) was employed to measure life satisfaction, this scale was developed by Diener [34]. It comprised of 5 items and the options for each item ranged from 1 (“strongly disagree”) to 7 (“strongly agree”) and the total score of the scale ranged from 5 to 35 [35]. The Cronbach's alpha coefficient was 0.942 for SWLS in this study.
Sleep disturbance
The Pittsburgh Sleep Quality Index (PSQI) [36] was used to measure the sleep disturbance [37] of the participants in the past month before the survey. It consisted of 19 self-reported items and these items could be divided into seven components. Each component was weighted equally on a scale of 0–3. The PSQI total score ranged from 0 to 21. Individuals with higher scores indicate poorer overall sleep quality [36], meant high sleep disturbance, it was appropriate for use among older adults [38, 39]. The Cronbach's alpha coefficient was 0.773 for PSQI in this study.
PCBA
PCBA was measured by the question: “Your per capita bedroom area?”, the answer was numerical. The higher numeric, indicated the larger PCBA.
Covariates
Covariates included the following parts: gender (male, female) [40], age (60 ~ 65, 66 ~ 70, 71 ~ 80, > 80) [41], marital status (married, single/divorced/separated/widowed) [42], Hukou (rural, urban), education level (not educated, primary school, junior high school, high school/technical secondary school, college degree and bachelor degree or above) [43], employment status (currently employed, retired, unemployed) [44], monthly household income (the first quartile (Q1), the second quartile (Q2), the third quartile (Q3), and the fourth quartile (Q4)) [43]. Q1 was the poorest and Q4 was the richest, time since migration (under five years, five years or above) [45] and chronic disease (without chronic disease, a chronic disease, two chronic diseases, three chronic diseases or above) [43], and the above factors had been confirmed associated with mental health problems.
Statistical analyses
All statistical analyses were performed by using SPSS version 24.0 (SPSS Inc., Chicago, IL, USA). Firstly, descriptive analysis, frequencies and percentages were employed to illustrate the basic characteristics of MOAC. Secondly, Pearson correlation analysis was used to test the correlations of life satisfaction, sleep disturbance, PCBA and mental health problems. Thirdly, PROCESS v3.5 for SPSS developed by Hayes [46] was employed to verify mediation and the moderated mediation hypotheses. The mediating role of sleep disturbance was tested by Model 4 in PROCESS. The mediating effect was deemed statistically significant if the 95% confidence intervals (CI) of the indirect effect did not contain 0. Fourthly, we introduced PCBA as the moderator variable into the model and tested the moderating role of PCBA in possible direct and indirect effects of life satisfaction on mental health problems by using Model 59. Similarly, the moderated mediation effect was approved statistically significant if the 95% CI of the interaction did not contain 0. Both models had the same independent, dependent, and mediating variables, life satisfaction, mental health problems, sleep disturbance, respectively, except for PCBA, which was included as a moderating variable in the moderated mediation model. All the regression coefficients calculated by the Model 4 and Model 59 were both controlled for gender, age, marital status, education level, job before retire, monthly household income, time since migration and chronic disease. The bootstrap sample size was set at 5000, the CI was 95%, and all continuous variables were meant centering. Statistical significance was defined as p-value < 0.05.
Results
Characteristics of the participants
The basic information of MOAC were shown in Table 1. A total of 613 MOAC participated and filled in the questionnaire effectively, among them, 73.08% were female, 55.79% were aged 60 ~ 65, 87.93% were married, 85.64% were from rural areas, 30.18% were educated in primary school, 70.80% were unemployed, 53.83% reported under five years since migration and 57.26% without chronic disease. All above variables were controlled as covariates in the moderated mediation model.
Table 1.
Characteristics of the sample (N = 613)
| Variable | n | % |
|---|---|---|
| Total | 613 | |
| Sex | ||
| Male | 165 | 26.92 |
| Female | 448 | 73.08 |
| Age | ||
| 60 ~ 65 | 342 | 55.79 |
| 66 ~ 70 | 171 | 27.90 |
| 71 ~ 80 | 80 | 13.05 |
| > 80 | 20 | 3.26 |
| Marital status | ||
| Married | 539 | 87.93 |
| Single/divorced/separated/widowed | 74 | 12.07 |
| Hukou | ||
| Rural | 525 | 85.64 |
| Urban | 88 | 14.36 |
| Educational level | ||
| Not educated | 161 | 26.26 |
| Primary school | 185 | 30.18 |
| Junior high school | 158 | 25.77 |
| High school/technical secondary school | 91 | 14.85 |
| College degree, bachelor degree or above | 18 | 2.94 |
| Employment status | ||
| Currently employed | 53 | 8.65 |
| Retired | 126 | 20.55 |
| Unemployed | 434 | 70.80 |
| Monthly household income | ||
| Q1 | 154 | 25.12 |
| Q2 | 152 | 24.80 |
| Q3 | 153 | 24.96 |
| Q4 | 154 | 25.12 |
| Time since migration | ||
| Under five years | 330 | 53.83 |
| Five years or above | 283 | 46.17 |
| Chronic disease | ||
| Without chronic disease | 351 | 57.26 |
| A chronic disease | 170 | 27.73 |
| Two chronic diseases | 70 | 11.42 |
| Three chronic diseases or above | 22 | 3.59 |
Note: Q1: the first quartile, Q2: the second quartile, Q3: the third quartile, Q4: the fourth quartile
Q1 was the poorest and Q4 was the richest
Descriptive analysis and correlation test of main variables
Table 2 showed the mean, standard deviations, and Pearson correlations of the main variables. Life satisfaction was negatively associated with mental health problems (r = − 0.39, P < 0.01) and sleep disturbance (r = − 0.27, P < 0.01), sleep disturbance was positively associated with mental health problems (r = 0.39, P < 0.01). Meanwhile, PCBA was negatively linked with mental health problems (r = − 0.11, P < 0.01) and positively linked with life satisfaction (r = 0.08, P < 0.05), while the correlation between sleep disturbance and PCBA was not statistically significant.
Table 2.
Correlations for the main variables
| Variable | Mean (SD) | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|
| 1. Mental health problems | 7.77 (10.64) | 1 | |||
| 2. Life satisfaction | 27.87 (5.58) | − 0.39** | 1 | ||
| 3. Sleep disturbance | 4.29 (3.60) | 0.39** | − 0.27** | 1 | |
| 4. Per capita bedroom area | 10.76 (5.25) | − 0.11** | 0.08* | − 0.02 | 1 |
Note: SD Standard deviation
**P < 0.01
*P < 0.05
Mediating effect analysis
Table 3 showed the result of mediating effect analysis. After controlling the covariates, the total effects model showed that life satisfaction was negatively associated with mental health problems (Coefficient = − 0.73, t = − 10.14, P < 0.001). As for mediation test, life satisfaction was negatively related to sleep disturbance (Coefficient = − 0.15, t = − 6.20, P < 0.001), and sleep disturbance was positively associated with mental health problems (Coefficient = 0.93, t = 8.25, P < 0.001), life satisfaction was negatively associated with mental health problems (Coefficient = − 0.59, t = − 8.34, P < 0.001). The bias-corrected percentile bootstrap results with 10,000 re-samples showed the 95% CI around direct effect (Effect = − 0. 59, 95%CI, − 0.73, − 0.45) and indirect effect (Effect = − 0.14, 95%CI, − 0.23, − 0.08) did not contain zero (Table 4), implied the association between life satisfaction and mental health problems was partially mediated by the sleep disturbance.
Table 3.
Mediation analysis of sleep disturbance
| Variable | Model 1 (Mental health problems) |
Model 2 (Sleep disturbance) |
Model 3 (Mental health problems) |
|||
|---|---|---|---|---|---|---|
| Coefficient t | Coefficient t | Coefficient t | ||||
| Life satisfaction | − 0.73 | − 10.14*** | − 0.15 | − 6.20*** | − 0.59 | − 8.34*** |
| Sleep disturbance | 0.93 | 8.25*** | ||||
| R2 | 0.17 | 0.13 | 0.25 | |||
| F | 12.37 | 9.00 | 18.69 | |||
Note: adjusted for gender, age, marital status, hukou, education level, employment status, monthly household income time since migration and chronic disease
***P < 0.001
Table 4.
Bootstrap results for effect of life satisfaction on mental health problems
| Item | Effect | SE | LLCI | ULCI |
|---|---|---|---|---|
| Direct effect | − 0.59 | 0.07 | − 0.73 | − 0.45 |
| Indirect effect | − 0.14 | 0.04 | − 0.23 | − 0.08 |
Note: adjusted for gender, age, marital status, hukou, education level, employment status, monthly household income time since migration and chronic disease
LLCI: Lower limit confidence interval 95%, ULCI: Upper limit confidence interval 95% (bias-corrected bootstrap confidence intervals), SE Standard error.
Moderated mediation analyses
The moderated mediation analyses were showed in Table 5. Controlled the covariates, the model with sleep disturbance as outcome (F = 7.567, P < 0.05) and dependent variable model (F = 16.578, P < 0.05) were both statistically significant. Two significant interactions were analyzed to test the moderating role of PCBA. In the sleep disturbance as outcome model, life satisfaction was negatively associated with sleep disturbance (Coefficient = − 0.152, t = − 6.073, P < 0.001), however, the effect of PBCA and the interaction (life satisfaction * PCBA) were not statistically significant (both P > 0.05), implied that PCBA didn’t moderate the first indirect link (life satisfaction -sleep disturbance) of the mediating effect. In the dependent variable model, the interaction effect of life satisfaction and PCBA on mental health problems were significantly (Coefficient = 0.028, t = 2.172, P = 0.030), meanwhile, the interaction effect of sleep disturbance and PCBA on mental health problems were also significantly (Coefficient = − 0.052, t = − 2.583, P = 0.010). These findings illustrated that PCBA was as a moderator in the association between life satisfaction and mental health problems, sleep disturbance and mental health problems.
Table 5.
Regression results of the moderated mediation model (model 59)
| Outcome Variable | ||||
|---|---|---|---|---|
| Outcome variable: sleep disturbance | Coefficient | SE | t | P |
| Constant | − 4.568 | 1.284 | − 3.556 | < 0.001 |
| Life satisfaction | − 0.152 | 0.025 | − 6.073 | < 0.001 |
| PCBA | − 0.025 | 0.027 | − 0.931 | 0.352 |
| Life satisfaction * PCBA | 0.002 | 0.005 | 0.361 | 0.718 |
| R2 | 0.131 | |||
| F | 7.567 | |||
| Outcome variable: Mental health problems | Coefficient | SE | t | P |
| Constant | 7.292 | 3.532 | 2.065 | 0.039 |
| Life satisfaction | − 0.575 | 0.070 | − 8.208 | < 0.001 |
| sleep disturbance | 0.895 | 0.111 | 8.043 | < 0.001 |
| PCBA | − 0.185 | 0.073 | − 2.517 | 0.012 |
| Life satisfaction * PCBA | 0.028 | 0.013 | 2.172 | 0.030 |
| Sleep disturbance * PCBA | − 0.052 | 0.020 | − 2.583 | 0.010 |
| R2 | 0.280 | |||
| F | 16.578 | |||
| Conditional direct effect analysis at different values of PCBA (M ± SD) | Effect | SE | LLCI | ULCI |
| M- 1SD (5.506) | − 0.722 | 0.096 | − 0.911 | − 0.533 |
| M (10.760) | − 0.575 | 0.070 | − 0.713 | − 0.438 |
| M + 1SD (16.014) | − 0.428 | 0.098 | − 0.621 | − 0.235 |
| Conditional indirect effect analysis at different values of PCBA (M ± SD) | Effect | Boot SE | Boot LLCI | Boot ULCI |
| M- 1SD (5.506) | − 0.187 | 0.067 | − 0.331 | − 0.072 |
| M (10.760) | − 0.136 | 0.036 | − 0.215 | − 0.072 |
| M + 1SD (16.014) | − 0.090 | 0.037 | − 0.173 | − 0.029 |
Note: Bootstrap sample size = 5000. *: denoted the product of two variables, representing the interaction term.
SE: Standard error, LLCI: Lower limit confidence interval 95%, ULCI: Upper limit confidence interval 95%, SD: Standard deviation.
If the number of decimal places is the same as in the previous table, some data cannot be fully displayed, so in this table, the number of decimal places is kept to three decimal places
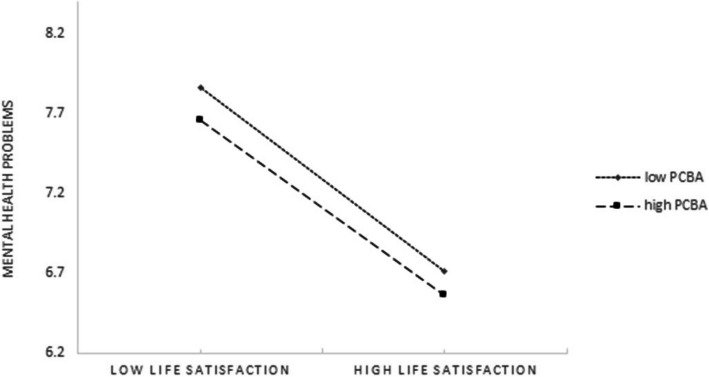
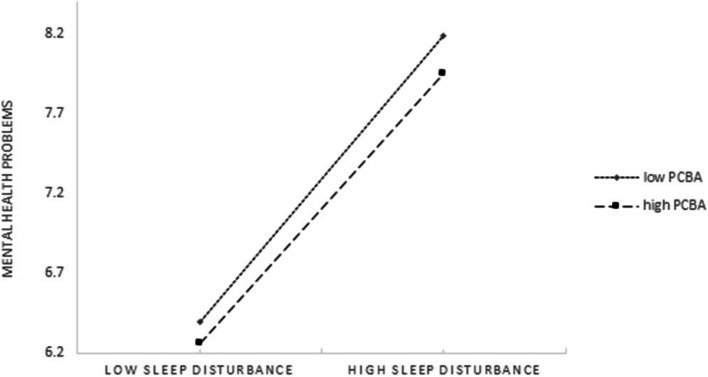
Furthermore, the significant moderated mediation models were tested by analyzing the direct and indirect effects of life satisfaction on mental health problems at different levels of PCBA. PCBA was divided into the high-level group (M + 1SD), moderate (Mean), and low-level group (M- 1SD). The 95% CI in conditional direct and conditional indirect effects showed that the low-level group and the high-level group both did not include zero. The direct effect of life satisfaction on mental health problems and the effect of sleep disturbance on mental health problems were stronger at the low level of PCBA.
The moderating effect could be visualized in Figs. 2 and 3. As shown in Fig. 2, whether high level or low level of PBCA among the MOAC, as the life satisfaction increased, mental health problems decreased significantly. The lower level of PBCA, the more obvious the trend (larger the slope). As shown in Fig. 3, at low levels of sleep disturbance, mental health problems remained low regardless of PBCA. However, when sleep disturbance was high, a low level of PCBA leaded to the higher increase in mental health problems. Furthermore, the direct effect of life satisfaction on mental health problems and the second indirect link (life satisfaction -sleep disturbance) of the mediating effect were more significant for participants with low level of PCBA.
Fig. 2.
Conditional effects of PCBA on association between life satisfaction and mental health problems
Fig. 3.
Conditional effects of PCBA on association between sleep disturbance and mental health problems
Discussion
This study examined the mediating and moderating mechanisms of the sleep disturbance and PCBA underlying the relationship between life satisfaction and mental health problems via a moderated mediation model among the MOAC in Weifang city, China. In this study, the negative association between life satisfaction and mental health problems was found, a partial mediation role of sleep disturbance was also observed in the above association. Furthermore, PCBA moderated the direct effect of life satisfaction on mental health problems, as well as the second half of the indirect effect from sleep disturbance to mental health problems. To be specific, when life satisfaction was low, a low level of PCBA would lead to the direct increase of mental health problems; when life satisfaction was low, a low level of PCBA would result in the indirect increase of mental health problems due to sleep disturbance.
This study found the life satisfaction was negatively associated with the mental health problems, which confirmed the Hypothesis 1 and was consistent with the previous studies [47–49]. In detailed, the higher the life satisfaction, the lower the mental health problems. It was widely acknowledged that the life satisfaction was an individual's comprehensive judgment of their own life, which could affect the individual's emotional experience [50]. The high level of life satisfaction might decrease the negative effects of stress exposure on the individual, due to it could help the individual to recover from negative life events [51] and result in a better mental health.
This study illustrated that the association between life satisfaction and mental health problems was partially mediated by sleep disturbance, which confirmed the Hypothesis 2 and also explained how life satisfaction could indirectly affect mental health problems. None study had illustrated the mediating effect of sleep disturbance on the relationship between life satisfaction and mental health problems, yet Parkerson et. al’s study showed that the high life satisfaction could lead to more sleep among first-year medical students [49], while Eleftheriou et. al’s study found that the more sleep disturbance, the more mental health problems [52].
Based on the moderated mediation analyses, PCBA was found could moderate the direct effect of life satisfaction on mental health problems and the second half of the indirect effect from sleep disturbance to mental health problems, thus partly supported the Hypothesis 3. Existed studies had illustrated that household overcrowding was harmful to individuals'mental health problems [53, 54], yet no study had focused on the association between PCBA and mental health problems, let alone clarifying the moderating effects of PCBA on the relationship between life satisfaction/sleep disturbance and mental health problems. The findings could be explained as follows. Firstly, PCBA could moderate the direct effect of life satisfaction on mental health problems. The negative direct correlation between life satisfaction and mental health problems was higher among those with low PCBA than the high PCBA (as shown in Fig. 2). Previous research illustrated the house mainly represented a safe place for individuals [55], low level of PCBA could not offer an adequate private space for the MOAC to relax and adjust their mood, which furtherly increase low life satisfaction’s negative effect on mental health problems. Secondly, PCBA moderated the indirect link (sleep disturbance-mental health problems) of life satisfaction on mental health problems mediated by sleep disturbance. That is, for the MOAC with a low level of PCBA, the negative effect of life satisfaction on mental health problems was higher when the sleep disturbance increased. In detailed, as shown in Fig. 3, higher indirect link (sleep disturbance-mental health problems) was found among MOAC with a low level of PCBA than those with a high level of PCBA. The explanation might be as follow: the MOAC with low life satisfaction had higher levels of negative emotions than those with high life satisfaction, which furtherly lead to the increase of the sleep disturbance symptoms; to make thing worse, the low level of PCBA would not provide an ideal place for sleep, and finally aggravated the negative effect of lower life satisfaction on mental health problems. This result was in line with the previous studies which also found the bedroom condition was associated with the sleep disturbance and mental health problems [56, 57]. Thirdly, the pandemic of the infectious disease made the duration of the people’s staying at home longer, the smaller private PCBA, together with the social distancing measures would lead to more mental health problems.
Based on the results above in this study, targeted implications on the improvement of life satisfaction, sleep quality, PCBA and mental health among the MOAC were given as follow. Firstly, the children of MOAC should pay more attention on the MOAC’s life satisfaction, sleep quality, and mental health problems, communicated more with MOAC and reduced the burden of MOAC in daily life to reduce physical and mental stress. Secondly, the children of MOAC should try their best to provide a larger private bedroom for MOAC. Thirdly, the community should promote the construction of a communication platform for MOAC, build a platform for them to communicate with their peers, reconstruct the social support and social network, improve life satisfaction and mental health of MOAC. Fourthly, MOAC should keep a positive attitude about life, open heart to children and other family members and keep relax to improve life satisfaction, sleep quality and mental health.
For future studies, follow-up study should be conducted to deeply reveal the correlation and influencing mechanism among life satisfaction, sleep disturbances and mental health problems, meanwhile, to further study the dynamic change of mental health problems among MOAC. Secondly, the regional scope of the study could be expanded, thus to study the differences in mental health problems among MOAC in different cities, furthermore, employing multi-group analysis, explored the influence mechanism of life satisfaction, sleep disturbances, PCBA and mental health problems among MOAC.
There were several limitations in this study. Firstly, the reliance on community staffs’ help on participant recruitment might affect the diversity of the sample and introduce potential bias in the selection of participants, despite the researchers’ efforts to ensure the representation of MOAC across different age groups and geographical locations within the region. Secondly, PCBA was completed by self-reporting, and some MOAC could only know the general PCBA information rather than exact PCBA data, furthermore, the level of housing prices in different parts of the city or whether it is school district housing was not taken into account. Thirdly, there were other factors such as social disintegration and lower healthcare utilization that could mediate the relationship between life satisfaction and mental health problems, however, this study only studied the mediating of sleep disturbances on the association between life satisfaction and mental health problems and resulted the scope of the study was not comprehensive enough. Fourthly, some covariates were regrouped on the basis of the original data, and it might produce bias. Lastly, this study was a cross-sectional study, which made a causal relationship was difficult to be predicted, there might existed the path that life satisfaction mediated the association between sleep disturbance and mental health problems.
Conclusions
To summarize, life satisfaction was negatively associated with mental health problems among the MOAC in Weifang, China; sleep disturbance played a mediating role in the relationship between life satisfaction and mental health problems; the direct effect of life satisfaction on mental health problems and the indirect effect between sleep disturbance and mental health problems were moderated by PCBA. Targeted implication for the community, family members on those MOAC with a low level of life satisfaction, high sleep disturbance and a low level of PCBA, were proposed based on the results above.
Acknowledgements
The research team greatly appreciates the funding support, and the research participants for their cooperation and support.
Abbreviations
- PCBA
Per capita bedroom area
- MOAC
Migrant older adults with children
- PSUs
The primary sampling units
- SSUs
Secondary sampling units
- DASS- 21
Depression Anxiety Stress Scale
- SWLS
The Satisfaction with Life Scale
- PSQI
The Pittsburgh Sleep Quality Index
- CI
Confidence interval
- Q1
The first quartile
- Q2
The second quartile
- Q3
The third quartile
- Q4
The fourth quartile
- SD
Standard deviation
- LLCI
Lower limit confidence interval 95%
- ULCI
Upper limit confidence interval 95%
- SE
Standard error
Authors’ contributions
Conceptualization, F.K. and M.P.; methodology, M.P.; software, M.P.; validation, F.K. and M.P.; formal analysis, M.P.; investigation, F.K., M.P., J.W., H.L., G.L. and X.J.; resources, F.K.; data curation, F.K., M.P., J.W., H.L., G.L., X.J.; writing—original draft preparation, M.P.; writing—review and editing, F.K., M.P. and J.X; visualization, M.P.; supervision, F.K. and S.L.; project administration, F.K.; funding acquisition, F.K. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported and funded by the National Natural Science Foundation of China (No. 71804094), China Postdoctoral Science Foundation (No. 2016 M592161), Natural Science Foundation of Shandong Province (No. ZR2016GB02), Postdoctoral Science Foundation of Shandong Province (No. 201603021), and Fundamental Research Funds for the Central Universities (No. 2022 KJGL01, No. 2018 JC055).
Data availability
Under reasonable requirements, the data and material of this study can be obtained from the corresponding author. The data are not publicly available due to privacy restrictions.
Declarations
Ethics approval and consent to participate
The survey and data use have obtained the written informed consent of all participants. The research program of this was reviewed and approved by the ethical committee of Shandong University (No. 20180225) and was in accordance with the Declaration of Helsinki.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.National Bureau of Statistics of China. The Seventh National Population Census Bulletin (No. 7) - Urban and Rural Population and Mobile Population (in Chinese). China Statistics. 2021;05:13.
- 2.China Migrant Population Development report 2018. http://www.nhc.gov.cn/wjw/xwdt/201812/a32a43b225a740c4bff8f2168b0e9688.shtml
- 3.Fanlei K, Mei K, Cheng L, Sixue L, Jun L. Progress of domestic and international research related to elderly people who move with the family. Chin J Gerontol. 2020;40(11):2443–7. [Google Scholar]
- 4.Xi S, Song Y, Li X, Li M, Lu Z, Yang Y, Wang Y. Local-Migrant Gaps in Healthcare Utilization Between Older Migrants and Local Residents in China. J Am Geriatr Soc. 2020;68(7):1560–7. [DOI] [PubMed] [Google Scholar]
- 5.Tang S, Long C, Wang R, Liu Q, Feng D, Feng Z. Improving the utilization of essential public health services by Chinese elderly migrants: strategies and policy implication. J Glob Health. 2020;10(1): 010807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jinming S. Social work Intervention on urban integration of the rural migrated elderly: Based on the perspective of “active Aging.” People’s Tribune. 2015;36:152–4. [Google Scholar]
- 7.Apak E, Artan T, Ozucelik DN. Evaluation of bio-psycho-social and socio-cultural problems of Syrian elderly living in Turkey. Int J Soc Psychiatry. 2023;69(2):454–66. [DOI] [PubMed]
- 8.Ponizovsky AM, Radomislensky I, Grinshpoon A. Psychological distress and its demographic associations in an immigrant population: findings from the Israeli National Health Survey. Aust N Z J Psychiatry. 2009;43(1):68–75. [DOI] [PubMed] [Google Scholar]
- 9.Sousa L, Lyubomirsky S. Life satisfaction. Encylopedia of Women and Gender: Sex Similarities and Differences and the Impact of Society on Gender. 2001;2:667–76. [Google Scholar]
- 10.Fergusson DM, McLeod GF, Horwood LJ, Swain NR, Chapple S, Poulton R. Life satisfaction and mental health problems (18 to 35 years). Psychol Med. 2015;45(11):2427–36. [DOI] [PubMed] [Google Scholar]
- 11.Park N. The Role of Subjective Well-Being in Positive Youth Development. Ann Am Acad Pol Soc Sci. 2004;591(1):25–39. [Google Scholar]
- 12.Nakamura JS, Delaney SW, Diener E, VanderWeele TJ, Kim ES. Are all domains of life satisfaction equal? Differential associations with health and well-being in older adults. Qual Life Res. 2022;31(4):1043–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seo EH, Kim SG, Kim SH, Kim JH, Park JH, Yoon HJ. Life satisfaction and happiness associated with depressive symptoms among university students: a cross-sectional study in Korea. Ann Gen Psychiatry. 2018;17:52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Piber D, Cho JH, Lee O, Lamkin DM, Olmstead R, Irwin MR. Sleep disturbance and activation of cellular and transcriptional mechanisms of inflammation in older adults. Brain Behav Immun. 2022;106:67–75. [DOI] [PubMed] [Google Scholar]
- 15.Bernert RA, Joiner TE Jr, Cukrowicz KC, Schmidt NB, Krakow B. Suicidality and sleep disturbances. Sleep. 2005;28(9):1135–41. [DOI] [PubMed] [Google Scholar]
- 16.Souilm N, Elsakhy NM, Alotaibi YA, Ali SAO. Effectiveness of emotional freedom techniques (EFT) vs sleep hygiene education group therapy (SHE) in management of sleep disorders among elderly. Sci Rep. 2022;12(1):6521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Batterham PJ, Glozier N, Christensen H. Sleep disturbance, personality and the onset of depression and anxiety: prospective cohort study. Aust N Z J Psychiatry. 2012;46(11):1089–98. [DOI] [PubMed] [Google Scholar]
- 18.Jin T, Sun Y, Wang H, Qiu F, Wang X. Prevalence of depression among Chinese medical students: A systematic review and meta-analysis. Psychol Health Med. 2022;27(10):2212–28. [DOI] [PubMed] [Google Scholar]
- 19.Dolsen EA, Byers AL, Flentje A, Goulet JL, Jasuja GK, Lynch KE, Maguen S, Neylan TC. Sleep disturbance and suicide risk among sexual and gender minority people. Neurobiol Stress. 2022;21: 100488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ling L, Youwei Y, Rongmao L, Xiangdong T, Shanshan L. Relationships of life satisfaction and sleep quality among middle school students in Fuzhou. Chin J School Health. 2011;32(09):1069–71. [Google Scholar]
- 21.Strine TW, Chapman DP, Balluz LS, Moriarty DG, Mokdad AH: The associations between life satisfaction and health-related quality of life, chronic illness, and health behaviors among U.S. community-dwelling adults. J Community Health 2008, 33(1):40–50. [DOI] [PubMed]
- 22.Chiu HF, Xiang YT, Dai J, Chan SS, Leung T, Yu X, Hou ZJ, Ungvari GS, Caine ED. The prevalence of sleep problems and their socio-demographic and clinical correlates in young Chinese rural residents. Psychiatry Res. 2012;200(2–3):789–94. [DOI] [PubMed] [Google Scholar]
- 23.Papi S, Cheraghi M. Relationship between Life Satisfaction and Sleep Quality and Its Dimensions among Older Adults in City of Qom. Iran Soc Work Public Health. 2021;36(4):526–35. [DOI] [PubMed] [Google Scholar]
- 24.Evans GW, Wells NM, Moch A. Housing and Mental Health: A Review of the Evidence and a Methodological and Conceptual Critique. J Soc Issues. 2003;59(3):475–500. [Google Scholar]
- 25.Baker M, McNicholas A, Garrett N, Jones N, Stewart J, Koberstein V, Lennon D. Household crowding a major risk factor for epidemic meningococcal disease in Auckland children. Pediatr Infect Dis J. 2000;19(10):983–90. [DOI] [PubMed] [Google Scholar]
- 26.Pierse N, Carter K, Bierre S, Law D, Howden-Chapman P. Examining the role of tenure, household crowding and housing affordability on psychological distress, using longitudinal data. J Epidemiol Community Health. 2016;70(10):961–6. [DOI] [PubMed] [Google Scholar]
- 27.Grandner MA. Sleep, Health, and Society. Sleep Med Clin. 2017;12(1):1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Consensus Conference P, Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, Dinges DF, Gangwisch J, Grandner MA, et al. Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society on the Recommended Amount of Sleep for a Healthy Adult: Methodology and Discussion. Sleep. 2015;38(8):1161–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Main data of the seventh National Census of Weifang City. http://wfrb.wfnews.com.cn/content/20210610/Articel03008TB.htm
- 30.Zou P, Sun L, Yang W, Zeng Y, Chen Q, Yang H, Zhou N, Zhang G, Liu J, Li Y, et al. Associations between negative life events and anxiety, depressive, and stress symptoms: A cross-sectional study among Chinese male senior college students. Psychiatry Res. 2018;270:26–33. [DOI] [PubMed] [Google Scholar]
- 31.Zahidi F, Khalid M, Surkan PJ, Azadbakht L. Associations Between Food Insecurity and Common Mental Health Problems Among Reproductive-Aged Women in Kabul-Afghanistan. Front Nutr. 2021;8: 794607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. 1995;33(3):335–43. [DOI] [PubMed] [Google Scholar]
- 33.Zhang Z, Wang T, Kuang J, Herold F, Ludyga S, Li J, Hall DL, Taylor A, Healy S, Yeung AS, et al. The roles of exercise tolerance and resilience in the effect of physical activity on emotional states among college students. Int J Clin Health Psychol. 2022;22(3): 100312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Diener E, Emmons RA, Larsen RJ, Griffin S. The Satisfaction With Life Scale. J Pers Assess. 1985;49(1):71–5. [DOI] [PubMed] [Google Scholar]
- 35.Corrigan JD, Kolakowsky-Hayner S, Wright J, Bellon K, Carufel P. The Satisfaction With Life Scale. J Head Trauma Rehabil. 2013;28(6):489–91. [DOI] [PubMed] [Google Scholar]
- 36.Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. [DOI] [PubMed] [Google Scholar]
- 37.Oakes DJ, Pearce HA, Roberts C, Gehrman PG, Lewis C, Jones I, Lewis KJS. Associations between comorbid anxiety and sleep disturbance in people with bipolar disorder: Findings from actigraphy and subjective sleep measures. J Affect Disord. 2022;309:165–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang C, Chang Y, Yun Q, Lu J, Zheng X, Xue Y, Zhao X, Yuan W, Zou J, Zheng J. The impact of chronic diseases on depressive symptoms among the older adults: The role of sleep quality and empty nest status. J Affect Disord. 2022;302:94–100. [DOI] [PubMed] [Google Scholar]
- 39.Li W, Yang S, Li J, Li Z, Yan C, Gui Z, Zhou C. Social capital and self-rated health among Chinese rural empty nesters: A multiple mediation model through sleep quality and psychological distress. J Affect Disord. 2022;298(Pt B):1–9. [DOI] [PubMed] [Google Scholar]
- 40.Abu-Kaf S, Nakash O, Hayat T, Cohen M. Emotional distress among the Bedouin Arab and Jewish elderly in Israel: The roles of gender, discrimination, and self-esteem. Psychiatry Res. 2020;291: 113203. [DOI] [PubMed] [Google Scholar]
- 41.Manandhar K, Risal A, Shrestha O, Manandhar N, Kunwar D, Koju R, Holen A. Prevalence of geriatric depression in the Kavre district, Nepal: Findings from a cross sectional community survey. BMC Psychiatry. 2019;19(1):271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Levkoff SE, MacArthur IW, Bucknall J. Elderly mental health in the developing world. Soc Sci Med. 1995;41(7):983–1003. [DOI] [PubMed] [Google Scholar]
- 43.Al-Butmeh S, Al-Khataib N. Mental health and quality of life of elderly people in the Bethlehem district: a cross-sectional study. Lancet. 2018;391(Suppl 2):S46. [DOI] [PubMed] [Google Scholar]
- 44.Midorikawa H, Tachikawa H, Taguchi T, Shiratori Y, Takahashi A, Takahashi S, Nemoto K, Arai T. Demographics Associated With Stress, Severe Mental Distress, and Anxiety Symptoms During the COVID-19 Pandemic in Japan: Nationwide Cross-sectional Web-Based Survey. JMIR Public Health Surveill. 2021;7(11): e29970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ravens-Sieberer U, Erhart M, Devine J, Gilbert M, Reiss F, Barkmann C, Siegel NA, Simon AM, Hurrelmann K, Schlack R, et al. Child and Adolescent Mental Health During the COVID-19 Pandemic: Results of the Three-Wave Longitudinal COPSY Study. J Adolesc Health. 2022;71(5):570–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, NY, US: Guilford Press; 2013. [Google Scholar]
- 47.Rissanen T, Viinamaki H, Lehto SM, Hintikka J, Honkalampi K, Saharinen T, Koivumaa-Honkanen H. The role of mental health, personality disorders and childhood adversities in relation to life satisfaction in a sample of general population. Nord J Psychiatry. 2013;67(2):109–15. [DOI] [PubMed] [Google Scholar]
- 48.Lombardo P, Jones W, Wang L, Shen X, Goldner EM. The fundamental association between mental health and life satisfaction: results from successive waves of a Canadian national survey. BMC Public Health. 2018;18(1):342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Parkerson GR Jr, Broadhead WE, Tse CK. The health status and life satisfaction of first-year medical students. Acad Med. 1990;65(9):586–8. [DOI] [PubMed] [Google Scholar]
- 50.Munoz RT, Hellman CM, Buster B, Robbins A, Carroll C, Kabbani M, Cassody L, Brahm N, Fox MD. Life Satisfaction, Hope, and Positive Emotions as Antecedents of Health Related Quality of Life Among Homeless Individuals. International Journal of Applied Positive Psychology. 2016;1(1):69–89. [Google Scholar]
- 51.Kim ES, Delaney SW, Tay L, Chen Y, Diener ED, Vanderweele TJ. Life Satisfaction and Subsequent Physical, Behavioral, and Psychosocial Health in Older Adults. Milbank Q. 2021;99(1):209–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Eleftheriou A, Rokou A, Arvaniti A, Nena E, Steiropoulos P. Sleep Quality and Mental Health of Medical Students in Greece During the COVID-19 Pandemic. Front Public Health. 2021;9: 775374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pengcheng L, Longfei Z, Shujuan C, Xiaojie W. Association between household overcrowding and depressive mood among Chinese residents. J Affect Disord. 2021;290:74–80. [DOI] [PubMed] [Google Scholar]
- 54.Hansen CB, Larsen CVL, Bjerregaard P, Riva M. The effect of household crowding and composition on health in an Inuit cohort in Greenland. Scand J Public Health. 2021;49(8):921–30. [DOI] [PubMed] [Google Scholar]
- 55.Mora DC, Quandt SA, Chen H, Arcury TA. Associations of Poor Housing with Mental Health Among North Carolina Latino Migrant Farmworkers. J Agromedicine. 2016;21(4):327–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zhensheng L. On the Bedroom Surroundings and High-quality Sleep. Journal of Zunyi Normal University. 2017;19(03):153–6. [Google Scholar]
- 57.Tachibana H, Izumi T, Honda S, Horiguchi I, Manabe E, Takemoto T. A study of the impact of occupational and domestic factors on insomnia among industrial workers of a manufacturing company in Japan. Occup Med (Lond). 1996;46(3):221–7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Under reasonable requirements, the data and material of this study can be obtained from the corresponding author. The data are not publicly available due to privacy restrictions.