Abstract
Inactivation of West Nile virus (WNV) in enzyme-linked immunosorbent assay (ELISA) wash buffer at 37°C was studied, as well as inactivation of WNV in cell culture medium over several days at an ambient temperature (28°C). Aliquots of WNV were removed from the 37°C ELISA wash buffer at 5, 15, 30, and 60 min for the former experiment, while daily aliquots of medium were sampled for the latter experiment. No virus was detected in the wash buffer at 30 and 60 min, while virus was readily detected from cell culture medium over this time. In addition, titers of WNV consistently dropped over a 7-day period at 28°C compared to control suspensions of virus held at 4°C. These observations indicate that WNV is readily inactivated in the presence of detergent-containing buffers. Furthermore, the viability loss at ambient temperature suggests that WNV is easily inactivated during routine transportation and testing of human body fluids such as serum and cerebrospinal fluid.
West Nile virus (WNV), like all flaviviruses, is an enveloped virus with a single-stranded RNA genome. WNV is classified as a biosafety level 3 (BSL3) agent, which, by definition, requires special precautions and physical structures for the containment of the virus in a laboratory setting. The possible presence of WNV in any human serum or cerebrospinal fluid sample raises the issue of inadvertent exposure to this virus during routine laboratory work. Particularly, it has been recommended (2) that during the testing of sera for WNV-specific antibodies, aerosol-producing procedures (e.g., enzyme-linked immunosorbent assay [ELISA] plate rinsing) should be performed in a class 2 biological safety cabinet (BSC2). Although these procedures can also be performed safely inside instruments which provide their own degree of aerosol protection, the operation of an ELISA plate washer in a BSC2 raises serious airflow concerns that may compromise the intended BSL3 safety conditions provided by the BSC2.
To determine the safety of serologic testing for WNV antibodies, we tested the effect of the specimen diluent buffer on WNV viability under normal testing conditions (37°C). The specimen diluent buffer (herein referred to as WNV wash buffer) is a phosphate-buffered saline (PBS) solution containing 0.05% Tween 20. The role of Tween detergents in viral inactivation is well documented for other enveloped viruses, and we sought to determine the deleterious effect of Tween 20 on WNV viability. As reference laboratories often receive specimens shipped unrefrigerated or without cold packs, we also conducted a series of experiments to determine the effect of ambient temperatures (28°C) on WNV viability in the absence of detergent.
For both experiments, a cell-free supernatant from a WNV-infected Vero cell culture was prepared via centrifugation at 8,000 × g for 5 min at an ambient temperature (28°C). The culture was seeded with a WNV isolate obtained from a crow brain in August 2000. The WNV isolate has been verified by reverse transcriptase PCR and immunofluorescent assay procedures.
For the WNV wash buffer inactivation experiment, aliquots of cell-free supernatant containing approximately 108 PFU were diluted in minimal essential medium (MEM) containing 10% fetal bovine serum (FBS), in PBS, or in WNV wash buffer (PBS with 0.05% Tween 20). The dilution factors used were identical to the initial inactivation dilution in the WNV serology protocol, that is, 2.5 μl of serum or virus stock to 1,000 μl of WNV wash buffer (4). All incubations were performed at 37°C. Equal volume aliquots were removed from the MEM and PBS control incubation mixtures at the beginning (time zero) and conclusion (60 min) of the experiment. Equal-volume aliquots were also removed from the experimental WNV wash buffer after 5, 15, 30, and 60 min. The initial aliquot taken from MEM served as the initial time point for the WNV wash buffer inactivation experiment. Following an initial 100-fold dilution in MEM (to reduce the concentration of Tween 20), equal-volume aliquots from each time point were inoculated in triplicate into 25-ml flasks of 1- to 3-day-old Vero cells. Flasks were incubated at 37°C and examined for 7 days for evidence of WNV-induced cytopathic effect (CPE). All experiments were repeated in duplicate.
The MEM and PBS control flasks at time zero and 60 min, as well as the 5-min WNV wash buffer samples, all exhibited WNV-induced CPE within 3 to 4 days postinoculation. This timing of WNV-induced CPE in Vero cells is consistent with previous reports (1). The aliquot taken at 15 min from the WNV wash buffer produced WNV-induced CPE on day 5 postinoculation. Most importantly, samples treated for 30 and 60 min in ELISA wash buffer did not yield viable virus over the 7-day time course of the experiment (Table 1).
TABLE 1.
Effect of ELISA wash buffer (containing 0.05% Tween 20) on WNV viabilitya
| Time (min) in wash buffer at 37°C | CPE with no. of PFU platedb
|
|
|---|---|---|
| 2.75 × 104 | 30 | |
| 0 | + | + |
| 5 | + | + |
| 15 | +c | − |
| 30 | − | − |
| 60 | − | − |
Equal aliquots of virus, mock-treated in cell culture control medium, were CPE positive over the time course of the experiment (not shown).
+, CPE in all three flasks; −, no CPE.
Two of three flasks yielded WNV-induced CPE.
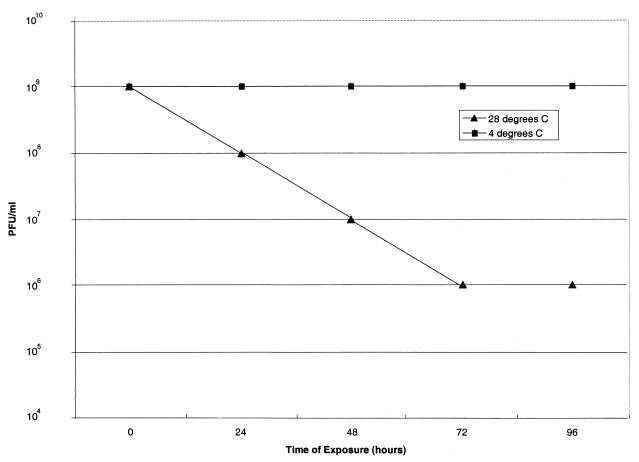
For the temperature experiment, aliquots of the cell-free supernatant were diluted into two tubes containing MEM with 10% FBS. One diluted aliquot was held at 4°C, while the other was placed at ambient temperature (28°C) for 96 h. Beginning at time zero and at 24-h intervals, 1-ml aliquots were removed from each viral suspension and inoculated (in triplicate) into 1- to 3-day-old 25-ml flasks of Vero cells. Flasks were examined for CPE for 7 days. Figure 1 shows the deleterious effects of ambient temperature on WNV survival.
FIG. 1.
Effect of temperature on WNV viability. The results are representative of three individual experiments.
The major findings of this study are twofold. First, the rapid inactivation of WNV in WNV wash buffer suggests that serologic testing of human specimens for WNV might be safely performed without the use of a BSC2. More importantly, perhaps, it adds a level of confidence that such analyses pose little or no safety hazard to those who cannot or do not choose to perform WNV antibody tests in a BSC2. Although we strictly adhere to other CDC recommendations for BSL3 work (i.e., restricted access and the handling of all clinical material under a BSC2), our findings argue against the need for BSC2 confinement in the latter, noninfectious steps of the protocol for the serologic testing of humans. Even though some of these procedures may produce aerosols (i.e., ELISA plate rinsing), the routine testing of blood or sera in hospital or clinical laboratories, be it chemistry, hematology, or serology, is not usually performed under BSC2 confinement conditions. Second, WNV is easily inactivated at temperatures which might be reached during routine shipping and handling of sera.
Further support for our argument can be derived from the nature of the WNV viremia in humans. Clinical specimens submitted for WNV serologic testing are usually collected after a short-lived viremia that precedes the clinical onset of disease (3, 5). It has been reported that of 28 sera tested from immunoglobulin M-positive WNV patients, only four of these cases were also positive by a TaqMan reverse transcriptase PCR protocol with a reported sensitivity of <1 PFU (3).
Our findings suggest that the postinactivation steps in the WNV serologic testing protocol are safe even without BSC2 containment. The WNV wash buffer inactivation experiment clearly illustrates the 100% loss of viability of an aliquot of WNV with several thousand times the possible titer of a human specimen. Coupled with the demonstrated loss of WNV viability at suboptimal temperatures (a 10-fold decrease in titer per 24-h period at 28°C), we conclude that the BSC2 containment of an ELISA plate washer for WNV serologic testing might not be necessary. However, each laboratory should be aware of current CDC recommendations and decide for itself how rigidly these recommendations should be followed.
REFERENCES
- 1.Beckwith, W., S. Sirpenski, R. French, R. Nelson, and D. Mayo. Isolation of eastern equine encephalitis virus and West Nile virus from crows during increased arbovirus surveillance in Connecticut. Am. J. Trop. Med. Hyg., in press. [DOI] [PubMed]
- 2.Centers for Disease Control and Prevention. 2001. Epidemic/epizootic West Nile virus in the United States: revised guidelines for surveillance, prevention, and control. Centers for Disease Control and Prevention, Atlanta, Ga.
- 3.Lanciotti, R. S., A. J. Kerst, R. S. Nasci, M. S. Godsey, C. J. Mitchell, H. M. Savage, N. Komar, N. A. Panella, B. C. Allen, K. E. Volpe, B. S. Davis, and J. T. Roehrig. 2000. Rapid detection of West Nile Virus from human clinical specimens, field-collected mosquitoes, and avian samples by a TaqMan reverse transcriptase-PCR assay. J. Clin. Microbiol. 38:4066-4071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Martin, D. A., D. A. Muth, T. Brown, A. J. Johnson, N. Karabatsos, and J. T. Roehrig. 2000. Standardization of immunoglobulin M capture enzyme-linked immunosorbent assays for routine diagnosis of arboviral infections. J. Clin. Microbiol. 38:1823-1868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Southam, C. M., and A. E. Moore. 1954. Induced virus infections in man by the Egypt isolates of West Nile virus. Am. J. Trop. Med. Hyg. 3:19-50. [DOI] [PubMed] [Google Scholar]