Abstract
Globally, mental disorders are a significant burden, particularly in low- and middle-income countries, with high prevalence in Rwanda, especially among survivors of the 1994 genocide against Tutsi. Machine learning offers promise in predicting mental health outcomes by identifying patterns missed by traditional methods. However, its application in Rwanda remains under-explored. The study aims to apply machine learning techniques to predict mental health and identify its associated risk factors among Rwandan youth. Mental health data from Rwanda Biomedical Center, collected through the recent Rwanda mental health cross-sectional study and with youth sample of 5221 was used. We used four machine learning models namely logistic regression, Support Vector Machine, Random Forest and Gradient boosting to predict mental health vulnerability among youth. The research findings indicate that the random forest model is the most effective with an accuracy of 88.8% in modeling and predicting factors contributing to mental health vulnerability and 75 % in predicting mental disorders comorbidity. Exposure to traumatic events and violence, heavy drinking and a family history of mental health emerged as the most significant risk factors contributing to the development of mental disorders. While trauma experience, violence experience, affiliation to pro-social group and family history of mental disorders are the main comorbidity drivers. These findings indicate that machine learning can provide insightful results in predicting factors associated with mental health and confirm the role of social and biological factors in mental health. Therefore, it is crucial to consider biological and social factors particularly experience of violence and exposure to traumatic events, when developing mental health interventions and policies in Rwanda. Potential initiatives should prioritize the youth who experience social hardship to strengthen intervention efforts.
Keywords: Machine learning, Prediction, Mental health, Youth, Rwanda
Subject terms: Psychology, Public health
Introduction
Worldwide, one person in eight is suffering from a mental health disorder1. Approximately 75% of the wide burden of mental and behavioral disorders is concentrated in low and lower-middle-income countries, and a substantial majority (76–85%) remain untreated2–4. Mental and behavioral disorders continue to be significant contributors to the global burden, constituting 32.4% of years lived with disability and 13% of disability-adjusted life-years2,5. Individuals with severe mental health issues die prematurely, and this condition causes disability.
Around 20% of the world’s children and teenagers have a mental health condition, with suicide the second driving cause of death among 15–29 year-olds6. Mental health issues’ prevalence seems to be rising in Africa as the population increases, and more people, specifically young people, struggle to cope with crises to earn a living7,8. The recent studies in Rwanda showed that the prevalence of mental disorders is  and the most common are major depressive disorders
and the most common are major depressive disorders  , panic disorders
, panic disorders  and post-traumatic stress disorders
and post-traumatic stress disorders  in general populations; the prevalence among genocide against Tutsi survivors was
in general populations; the prevalence among genocide against Tutsi survivors was  and the most prevalent disorders are major depressive disorders
and the most prevalent disorders are major depressive disorders  , post-traumatic stress disorders
, post-traumatic stress disorders  , and panic disorders
, and panic disorders  )9.
)9.
Given the high prevalence and significant impact of mental health conditions, particularly among vulnerable populations like youth, there is a growing need for innovative approaches to identify those at risk and provide timely interventions10. Novel technologies and Artificial Intelligence enhance practice-oriented research models by integrating research and practice11,12. In this context, leveraging data-driven approaches presents a valuable opportunity. By utilizing survey data and advanced analytical techniques, we can better understand patterns and predictors of mental health issues, enhancing the accuracy of early identification and treatment strategies13,14.
Advancements in machine learning have shown promising potential in predicting mental health outcomes in various contexts15,16. Machine learning, a subset of artificial intelligence, empowers systems to learn from data and improve their performance over time, enabling a wide range of applications that enhance decision-making and automate complex tasks17. The use of Machine Learning (ML) in mental health gained more attention due to the growing availability of digital mental health data and the potential for ML techniques to enhance mental health care delivery18. ML has been applied in various areas, including the detection, diagnosis, prognosis, treatment, and support of mental health problems, as well as in public health, clinical administration, and research15,19. Techniques like natural language processing (NLP) have been used to predict suicide ideation and psychiatric symptoms, aiding in personalized treatment and predictive detection of mental health conditions20,21. Studies have demonstrated the use of ML algorithms, such as classification, regression, and deep learning, to diagnose bipolar disorder and analyze the impact of financial policies on public mental health22,23. The application of ML on longitudinal mobile sensing data has improved the generalizability and predictive performance for mental health symptoms, particularly depression, anxiety, and PTSD during the COVID-19 pandemic24. Moreover, ML models have been employed to predict mental health states across diverse populations, including students and professionals, and to assess mental healthcare service use, revealing both the potential and challenges in resource allocation14,25. Additionally, ML models using passive sensing signals have shown strong performance in predicting mental health risks in individuals with diabetes26. Therefore, ML techniques hold promise for advancing the understanding of mental illness, enhancing diagnostic accuracy, and tailoring interventions to improve outcomes for individuals with mental health conditions27,28.
By leveraging machine-learning algorithms on a large dataset, it is possible to identify patterns and relationships that may not be easily discovered through traditional descriptive and inferential statistics29. ML techniques have been valuable tools for understanding psychiatric disorders and distinguishing and classifying mental health issues among patients for advanced treatments30. Studies identified various machine learning models and assessed their effectiveness in modeling different mental health issues in children, including Attention Deficit/Hyperactivity Disorder (ADHD), major depressive episodes, manic episodes, and anxiety, comparing their performance on different measures of accuracy31. Therefore, ML techniques hold promise for advancing the understanding of mental illness, enhancing diagnostic accuracy, and tailoring interventions to improve outcomes for individuals with mental health conditions27,28.
Several studies have demonstrated the feasibility and effectiveness of machine learning approaches in modeling and predicting mental health outcomes based on behavioral data from specific populations32–34. For instance, Ponce et al.35 integrated sentiment analysis, ML algorithms, and data from social network to develop a mobile application that allowed the early detection and prevention of mental health problems in Peru. This tool enabled timely interventions, contributing positively to public mental health management. Abdul et al.36 employed machine learning techniques to predict mental wellness among university students using health behavior data. Their findings revealed that ML models could accurately predict mental wellness outcomes, outperforming traditional predictive methods. The study highlights the potential of behavior-based ML approaches to be extended and adapted for use in diverse populations beyond the university setting.
However, the use of machine learning in the prediction of mental health in Rwanda is relatively unexplored. This study aims to use machine learning to predict mental health outcomes in youth in Rwanda. Specifically, this study aims to: (a) Build a predictive machine learning model for mental health vulnerability. Design and implement a machine learning predictive model that analyzes various demographic, social, and behavioral factors to identify at-risk youth. Evaluate models based on different evaluation metrics to select the best one. (b) Determine key predictors of mental health status among Rwandan youth. Conduct feature importance analysis to identify the most significant predictors contributing to mental health issues in youth using the best model selected.
Methods
Research design and source of data
This study used recent cross-sectional records from the Rwanda Mental Health Survey (RMHS 2018) which was conducted by the Rwanda Biomedical Center under the Ministry of Health, in collaboration with partner institutions. The survey was conducted from 1st August to 31st August 2018 nationwide and employed multistage sampling methods with the targeted population being people aged 14–65 who lived in Rwanda at the time of the study. The participants of this study are youth, which means those aged between 15 and 24 according to the United Nations’ definition37. This subsample is from across the entire country, ensuring a comprehensive and representative sample and comprised of five thousand two hundred twenty-one  subjects.
subjects.
Data collection tools
The occurrence of common mental disorders was determined using the Mini-International Neuropsychiatric Interview (MINI), version 7.0.238. This diagnostic interview instrument employs a binary response format, where participants respond with either “yes” or “no”.
Moreover, traumatic experiences and heavy drinking were assessed using the MINI component on traumas exposure, and section I for alcohol and section J for drugs . On the other hand, violence exposure was measured using a one dichotomous question (Yes or no) whether the person was exposed to violence, mostly domestic violence.
MINI is widely applied in the field of psychiatry. In previous investigations conducted in Rwanda, Kinyarwanda-translated versions of MINI reflecting the participants’ native language were used to assess mental health conditions and showed satisfactory psychometric properties39–41
Description of variables
Outcome variable
In this study, the outcome variable was any mental health condition classified according to MINI. Mental health status was categorized into two groups: Individuals who screened positive for at least one mental health condition and those who did not test positive for any mental health condition.
Explanatory variables
According to the biopsychosocial model proposed by George Engel42, human experiences are diverse and are shaped by a complex interplay of factors that influence an individual’s life, including biological, psychological, and social determinants that all contribute to shaping a person’s experiences, health and behavior. The explanatory variables associated with any mental health condition were the social and biological factors summarized in Table 1.
Table 1.
Explanatory variables for use in the analysis.
| Variables | Description | Categories |
|---|---|---|
| Sex | Sex of participants | 0: Female, 1: Male |
| Age | Age of participants |
 : Adolescents, : Adolescents,  : Young adults : Young adults |
| Marital status | Marital status of participants | 0: Never married, 1: Married, 2: Separated/divorced |
| Education | Level of education of participants | 0: No education, 1: Primary, 2: Secondary/higher |
| Employment status | Status of employment of participants | 0: Unemployed, 1: Employed |
| Lifetime loss | Participant experienced lifetime loss of someone or something | 0: No, 1: Yes |
| Affiliation to pro-social group | Whether participant is affiliated to a pro-social group | 0: No, 1: Yes |
| Violence experience | Experiencing any kind of violence | 0: No, 1: Yes |
| Religion | Religious beliefs of participants | 0: No religion/others, 1: Muslim, 2: Christian |
| Medical condition | Previous experience of medical condition | 0: No, 1: Yes |
| Heavy drinking | Heavy alcohol consumption | 0: No, 1: Yes |
| Traumatic experience | Experiencing traumatic event | 0: No, 1: Yes |
| Mental health history | Had personal mental health history | 0: No, 1: Yes |
| Family history of mental health | Had history of mental health disorders in family | 0: No, 1: Yes |
Data cleaning and pre-processing
Pre-processing of data involves preparing raw data to make it understandable and suitable for analysis. It consists of various stages, such as data cleaning, integration, transformation, and reduction43. In this study, data cleaning was performed using Python version 3. Key variables for predicting mental health outcomes were selected based on a biopsychosocial theoritical framework that categorizes causes into distant determinants such as social, biological, and psychological factors. The data were slightly imbalanced; therefore, no methods were applied to handle the imbalance. The selection of features was based on the filtering correlation method.
Data transformation
Data transformation involves altering the format or structure of the data to prepare it for analysis. In this study, categorical variables containing non-numeric data were converted into a numerical format through feature encoding. The dummy variables were created to analyze each variable’s contribution.
Machine learning classification algorithms
Machine learning classification algorithms use input training data to predict the likelihood that subsequent data will fall into one of the predetermined categories44. Given  observations
observations  , where
, where  is an element of
is an element of  , and
, and  , where
, where  belongs to
belongs to  . Supervised learning finds a function
. Supervised learning finds a function  or
or  such that
such that  for all pairs
for all pairs  that have the same observations44. For the binary classification problem,
that have the same observations44. For the binary classification problem,  where
where  is labeled as negative and
is labeled as negative and  is labeled as positive observations. In this study, ML algorithms were used, including logistic regression, support vector machine, random forest, and gradient boosting.
is labeled as positive observations. In this study, ML algorithms were used, including logistic regression, support vector machine, random forest, and gradient boosting.
Logistic regression
Logistic regression is a statistical method used for binary classification tasks, aiming to predict the probability that an instance belongs to a specific class45,46. Given a set of predictors  a vector of discrete or continuous variables, a logistic regression models the likelihood that
a vector of discrete or continuous variables, a logistic regression models the likelihood that  falls into a particular category as functions of the predictors. The sigmoid function is used in logistic regression to transform the linear combination of the predictor variables into a probability ranging from
falls into a particular category as functions of the predictors. The sigmoid function is used in logistic regression to transform the linear combination of the predictor variables into a probability ranging from  to
to  .
.
 |
 signifies the probability of the event
signifies the probability of the event  given the predictors
given the predictors  , and the coefficients
, and the coefficients  are estimated by the model using the training data.
are estimated by the model using the training data.
The goal of the logistic regression model is to determine the optimal values of the coefficients  to minimize a loss function. The most common loss function used in logistic regression is the log loss, also known as the cross-entropy loss function, which is defined as:
to minimize a loss function. The most common loss function used in logistic regression is the log loss, also known as the cross-entropy loss function, which is defined as:
 |
where  is the number of observations,
is the number of observations,  is the actual label for observation
is the actual label for observation  , and
, and  is the probability predicted that
is the probability predicted that  for observation
for observation  .
.
Random forest
Random forest is an ensemble method based on decision trees, where each tree is built using a random subset of variables, with the aim of reducing variance. It is inspired by the work of Leo Breiman, Amit, and German’s Lier function47. The random forest may be used for both categorical and continuous variables as classification and regression, respectively48.
Given a vector of random variables  representing the input or predictor variables and
representing the input or predictor variables and  representing the dependent variable with real values, we assume an unknown joint distribution
representing the dependent variable with real values, we assume an unknown joint distribution  . The objective is to determine a prediction function
. The objective is to determine a prediction function  to predict
to predict  .
.
The prediction function is calculated using a loss function  , designed to minimize the expected value of the loss:
, designed to minimize the expected value of the loss:
 |
where  denotes the joint distribution expectation of
denotes the joint distribution expectation of  and
and  . The function
. The function  measures how close
measures how close  is to
is to  , penalizing values of
, penalizing values of  that deviate significantly from
that deviate significantly from  .
.
The loss function  can be defined as:
can be defined as:
 |
ensures that the loss is zero when the prediction matches the true value and penalizes incorrect predictions.
Support vector machine (SVM)
Support vector machine (SVM) is a robust supervised machine learning method used for classification and regression tasks49. Its primary objective is to find the optimal hyperplane that effectively separates the classes in the feature space. SVM achieves this by maximizing the margin between classes based on a set of training data consisting of input vectors  and their corresponding class labels
and their corresponding class labels  . This hyperplane is defined in the high-dimensional feature space and aims to accurately classify new data points by their proximity to this separation boundary.
. This hyperplane is defined in the high-dimensional feature space and aims to accurately classify new data points by their proximity to this separation boundary.
The hyperplane is defined by:
 |
where  is the weight vector perpendicular to the hyperplane, and
is the weight vector perpendicular to the hyperplane, and  is the bias term.
is the bias term.
For linearly separable data, SVM determines the optimal hyperplane by solving the following optimization problem:
 |
subject to the constraints: 
Many real-world datasets are not linearly separable. To handle non-linearly separable data, kernel SVM leverages the concept of kernel functions. Kernel SVM maps the input vector  into a higher-dimensional space using a kernel function
into a higher-dimensional space using a kernel function  , where the data become linearly separable. The optimization problem for kernel SVM becomes:
, where the data become linearly separable. The optimization problem for kernel SVM becomes:
 |
subject to the constraints:  ,
, 
where  are Lagrange multipliers and
are Lagrange multipliers and  is a regularization parameter, balancing the objective of maximizing the margin and minimizing the classification error.
is a regularization parameter, balancing the objective of maximizing the margin and minimizing the classification error.
Gradient boosting
Gradient boosting is an ensemble learning technique used for classification and regression problems, with a wide range of applications due to its accuracy and robustness against overfitting50,51. It combines weak learners during the gradient boosting process to obtain a strong learner. The final result, denoted as  , is obtained by the addition of the results of
, is obtained by the addition of the results of  sequential classifier functions
sequential classifier functions  and is calculated as follows:
and is calculated as follows:
 |
here,  represents a decision tree, and
represents a decision tree, and  is the total number of iterations in the boosting algorithm.
is the total number of iterations in the boosting algorithm.
In these techniques, classification is based on the residuals of the previous iteration, with each feature’s influence being sequentially assessed until a desired accuracy level is achieved. Using a loss function  that is optimized using gradient descent, the residuals are calculated. The expression for the loss function at step
that is optimized using gradient descent, the residuals are calculated. The expression for the loss function at step  is given by:
is given by:
 |
where  represents the regularization term used to compute the loss function
represents the regularization term used to compute the loss function  at step
at step  .
.
Model training
The analysis process started by splitting the processed data set into training and testing sets with a 70–30 ratio, based on the existing literature and proven efficacy in mental health data applications. Four machine algorithms were selected for training, namely logistic regression, gradient boosting, random forest, and SVM. Each model was trained using a 10-fold cross-validation and evaluated based on the evaluation metrics from k-fold cross-validation. Moreover, we checked for overfitting and underfitting by comparing metrics on both the training and test datasets. A grid search was applied to optimize the hyperparameters and explore predefined values to determine the best-performing class-specific feature importance scores by weighting the standardized mean values of features for each class with the feature importance scores derived from the model.
Hyperparameter tuning
Following hyperparameter tuning using grid search, the SVM was optimized with the following parameters:C=10, gamma=1, kernel= bf. Best parameters for the logistic regression were: C = 0.1, class weight = None, penalty = l2, solver = liblinear. Gradient boosting: learning rate=0.01, max-depth=8, n_estimators=300, subsample=0.8, best parameters for random forest=max-depth=10, min_samples_leaf=1, min_samples_split=2, n_estimators=200.
bf. Best parameters for the logistic regression were: C = 0.1, class weight = None, penalty = l2, solver = liblinear. Gradient boosting: learning rate=0.01, max-depth=8, n_estimators=300, subsample=0.8, best parameters for random forest=max-depth=10, min_samples_leaf=1, min_samples_split=2, n_estimators=200.
Model evaluation
Evaluating the performance of a machine learning model is key in any project; this study explores different approaches for evaluating model performance. A number of metrics used include precision, accuracy, recall, F1-score, and area under the curve, which is computed from the confusion matrix, which quantifies correct and incorrect predictions across different classes52,53.
Data analysis
Prevalence of mental health among youth
Figure 1 illustrates the distribution of mental health status among youth, the results highlight the prevalence of mental health conditions in youth is 14.48%. This indicates that 14 individuals out of every 100 have mental health disorders.
Fig. 1.
Prevalence.
Major depressive episode is the most prevalent mental disorder (Table 2), followed by other common conditions such as panic disorder (5.94%), obsessive-compulsive disorder (2.57%), post-traumatic disorder (1.99%), social phobia (1.32%), antisocial personality (1.28%), alcohol use disorder (1.03%), suicidal behavior disorder (0.52%), and substance use disorder (0.34%).
Table 2.
Frequency and prevalence of mental disorders.
| Mental disorder | Frequency | Prevalence (%) |
|---|---|---|
| Major depressive episode | 347 | 6.65 |
| Suicidal behavior disorder | 27 | 0.52 |
| Panic disorder | 310 | 5.94 |
| Social phobia | 69 | 1.32 |
| Obsessive compulsive disorder | 134 | 2.57 |
| Posttraumatic stress disorder | 104 | 1.99 |
| Manic episode | 5 | 0.10 |
| Hypomanic episode | 4 | 0.08 |
| Alcohol use disorder | 54 | 1.03 |
| Substance use disorder | 18 | 0.34 |
| Antisocial personality disorder | 67 | 1.28 |
| Bipolar disorder | 7 | 0.13 |
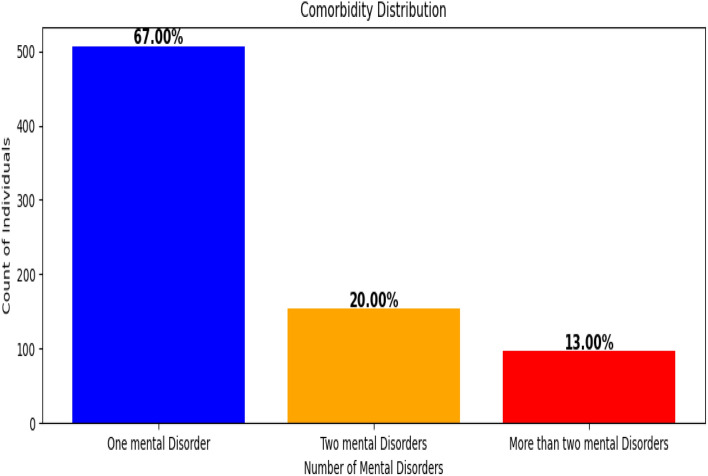
The majority of the individuals (67%) suffer from only one mental disorder (Fig. 2). 153 individuals (20%) have two mental disorders while 96 individuals (13%) have more than two mental disorders. The individuals, who experience severe comorbidity, may require integrated care and specialized treatment for managing multiple disorders.
Fig. 2.
Comorbidity distribution.
Bivariate analysis
A bivariate analysis was performed using Pearson’s chi-square test in a confidence interval of 95% to assess the link between the independent factors and the dependent variable. In this study, a p-value below 0.05 was considered to indicate statistical significance. Table 3 presents a summary of the participants’ background characteristics. A total of 5,221 participants, with females comprising 56.6% of the sample. The data were categorized by age, with the young adults representing the most prevalent age group.
Table 3.
Bivariate analysis of mental health factors.
| Variable | Category | Total (n, %) | No mental disorders (n, %) | Any mental disorders (n, %) | P-value |
|---|---|---|---|---|---|
| Sex | Female | 2956 (56.6) | 2475 (83.7) | 481 (16.3) | 0.000 |
| Male | 2265 (43.4) | 1990 (87.9) | 275 (12.1) | ||
| Education | No education | 541 (10.4) | 430 (79.5) | 111 (20.5) | 0.000 |
| Primary | 2951 (56.5) | 2510 (85.1) | 441 (14.9) | ||
| Secondary/higher | 1729 (33.1) | 1525 (88.2) | 204 (11.8) | ||
| Marital status | Separated | 34 (0.7) | 20 (58.8) | 14 (41.2) | 0.000 |
| Married | 844 (16.2) | 675 (80.0) | 169 (20.0) | ||
| Never married | 4343 (83.2) | 3770 (86.8) | 573 (13.2) | ||
| Employment | Employed | 309 (5.9) | 240 (77.7) | 69 (22.3) | 0.000 |
| Unemployed | 4912 (94.1) | 4225 (86.0) | 687 (14.0) | ||
| Religion | Christian | 4982 (95.4) | 4268 (85.7) | 714 (14.3) | 0.029 |
| Muslim | 126 (2.4) | 110 (87.3) | 16 (12.7) | ||
| Other/None | 113 (2.2) | 87 (77.0) | 26 (23.0) | ||
| Mental health history | Yes | 242 (4.6) | 167 (69.0) | 75 (31.0) | 0.000 |
| No | 4979 (95.4) | 4298 (86.3) | 681 (13.7) | ||
| Medical condition | Yes | 107 (2.0) | 77 (72.0) | 30 (28.0) | 0.000 |
| No | 5114 (98.0) | 4388 (85.8) | 726 (14.2) | ||
| Heavy drinking | Yes | 177 (3.4) | 94 (53.1) | 83 (46.9) | 0.000 |
| No | 5044 (96.6) | 4371 (86.7) | 673 (13.3) | ||
| Violence experience | Yes | 554 (10.6) | 328 (59.2) | 226 (40.8) | 0.000 |
| No | 4667 (89.4) | 4137 (88.6) | 530 (11.4) | ||
| Trauma experience | Yes | 555 (10.6) | 310 (55.9) | 245 (44.1) | 0.000 |
| No | 4666 (89.4) | 4155 (89.0) | 511 (11.0) | ||
| Lifetime loss | Yes | 2250 (43.1) | 1796 (79.8) | 454 (20.2) | 0.000 |
| No | 2971 (56.9) | 2669 (89.8) | 302 (10.2) | ||
| Affiliation with prosocial group | Yes | 1455 (27.9) | 1228 (84.4) | 227 (15.6) | 0.165 |
| No | 3766 (72.1) | 3237 (86.0) | 529 (14.0) | ||
| Family history of mental illness | Yes | 1159 (22.2) | 878 (75.8) | 281 (24.2) | 0.000 |
| No | 4062 (77.8) | 3587 (88.3) | 475 (11.7) | ||
| Age | Adolescent | 2287 (43.8) | 2071 (90.6) | 216 (9.4) | 0.000 |
| Young adults | 2934 (56.2) | 2394 (81.6) | 540 (18.4) |
From the result in Table 3, heavy drinking, trauma experience, being divorced or separated, and violence experience are associated with any mental health vulnerability at 46.9%, 44.1%, 41.2% and 40.8%, respectively. Moreover, medical condition history, having a family history of mental health, having no religion, and being employed are associated with mental health at 28.0%, 24.2%, 23.0% and 22.3% respectively.
Generally, the bivariate analysis shows that most factors are strongly associated with the likelihood of having mental disorders. The most linked categories include sex, education, marital status, employment status, religion, mental health history, medical condition experience, heavy drinking, violence experience, trauma experience, lifetime loss, family history of mental illness, and age. On the other hand, affiliation to pro-social groups was not associated with the likelihood of developing at least one mental health disorder.
Results
Machine learning classification analysis
Table 4 presents the performance metrics of four machine learning models; the performance of each model is evaluated using precision score, recall score, F1 score, and accuracy.
Table 4.
Comparison of evaluation metrics for different models.
| Model | Precision | Recall | F1 score | Accuracy |
|---|---|---|---|---|
| Logistic regression | 0.870 | 0.880 | 0.857 | 0.880 |
| Gradient boosting | 0.859 | 0.872 | 0.844 | 0.872 |
| Random forest | 0.877 | 0.888 | 0.873 | 0.888 |
| SVM | 0.862 | 0.870 | 0.835 | 0.870 |
Significant values are in bold.
Random forest has the highest precision, recall, and accuracy, resulting in the best F1 score among the models. Logistic regression shows a high balance between precision and recall, leading to a solid F1 score; it also has high accuracy. Gradient boosting performs well with a slightly lower precision compared to other models. SVM shows the lowest F1 score and recall, resulting in low accuracy. Random forest has the best overall performance.
The performance of the model shown in Fig. 3 is measured using the ROC-AUC curve. As the graph indicates, the random forest classifier outperforms other models with an AUC of 83.59%. Random forest is quite good and has good discrimination capability, which means it is good at differentiating between those with no mental disorders and those screened with any mental disorders. Feature importance is defined as a method that assigns a score to independent variables based on their predictive utility for a target variable. The achieved scores illustrate which feature may be more important to the objective. The plot created for the feature importance is the output of the random forest classifier.
Fig. 3.
Area under the curve (AUC).
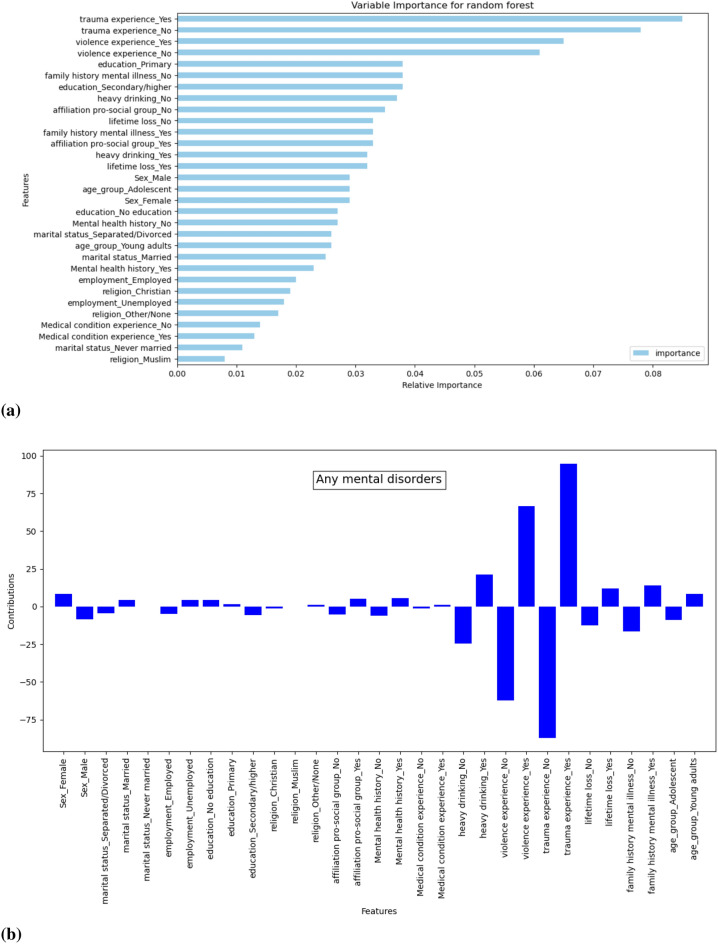
The Fig. 4 displays the feature importance and contributions as determined by the random forest classifier trained on the Rwanda mental health survey youth dataset. The Fig. 4a represents the feature importance where each bar represents a feature from the dataset and its relative importance in predicting those who are screened for at least one mental health disorder. The experiencing traumatic events feature has a high value of relative importance, indicating that trauma experience has a strong influence on the model’s predictions. It is followed by violence experience, heavy drinking, and family history of mental health, as it is illustrated in Fig. 4a . Moreover, we evaluated the contributions of each feature on the target variable. The Fig. 4b highlights experiencing traumatic events and violence has high feature importance scores in predicting any mental health conditions. Other key predictors include heavy drinking, family history of mental illness, and a lifetime loss of a loved one or something significant. Additionally, being female and a young adult are associated with a high likelihood of mental disorders. Conversely, not experiencing these factors significantly reduces the likelihood of having mental health condition.
Fig. 4.
Feature importance and their contributions.
Analysis of factors contributing to the comorbidity
Beyond binary classification, which identifies individuals as positive if they had at least one mental disorder, a multiclass classification approach using the Random Forest model, which outperformed others in the binary, was applied to predict and determine factors associated with comorbidity. Comorbidity was categorised into three levels namely: single mental disorder, two disorders, and multiple ( ) disorders.
) disorders.
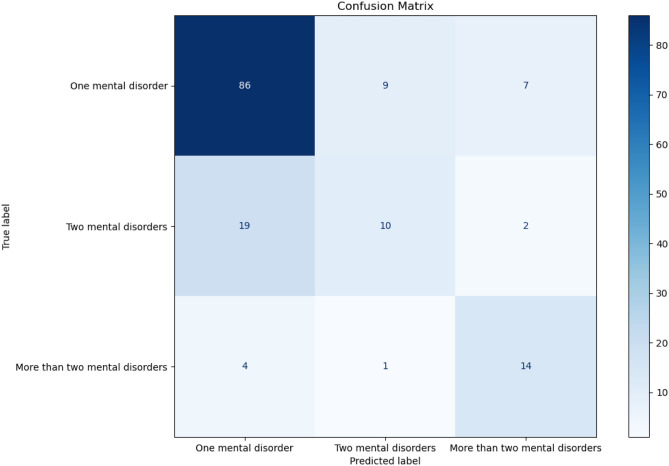
The multiclass modeling using random forest demonstrated an overall solid performance in predicting mental disorder comorbidity among youth, with an accuracy of 75 % and an AUC score of 0.738, indicating a reasonable level of class separability. The precision (0.758) and recall (0.750) reveal that the model makes relatively accurate predictions and successfully identifies a significant proportion of true cases. However, the Fig. 5 and the F1-score point to a slight imbalance in performance across classes.
Fig. 5.
Confusion matrix.
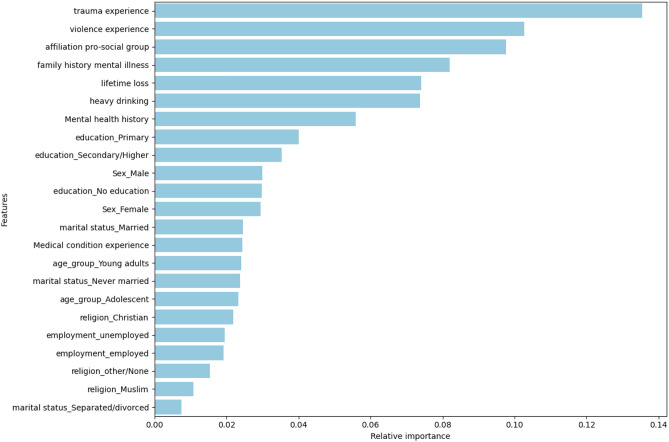
Figure 6 highlights the most influential variables in predicting the level of mental disorder comorbidity among youth. The top contributors include trauma experience, violence experience, affiliation to pro-social group and family history of mental disorders which all show relatively high importance score. These variables show the role of social support systems and adverse life experiences are critical in determining mental health outcomes.
Fig. 6.
Features importances.
Other notable predictor are lifetime loss, heavy drinking and mental health history, emphasizing the role of environmental and behavioral factors. Variables like being divorced/separated, employment status and religion exhibit relatively low importance, which means they may play a lesser role in distinguish levels of comorbidity in this specific dataset.
Discussion
The primary objective of this research was to employ machine learning approaches to predict mental health vulnerability and identify potential contributing factors among youth, using insights derived from cross-sectional survey data. The models were trained on a designated training set, and their performance was evaluated on unseen test data using several metrics, including classification accuracy, confusion matrix, recall, precision, and area under the curve (AUC).
The results revealed that the Random Forest algorithm outperformed other techniques, achieving the highest performance metrics with an accuracy of 88.8% and an AUC of 83.59% in predicting mental health vulnerability. It also showed strong performance in predicting comorbidity, with an accuracy of 75% and an AUC of 0.738. The most influential predictors of mental health vulnerability included traumatic experiences, exposure to violence, heavy drinking, family history of mental illness, lifetime loss, and being female or a young adult. In the context of mental health comorbidity, key contributing factors included traumatic experiences, exposure to violence, affiliation with pro-social groups, family history of mental disorders, experiences of lifetime loss, heavy drinking, and prior mental health conditions.
These findings align with existing literature, where Random Forest has consistently demonstrated high predictive power in mental health studies. For instance, a study focused on international students in the United Kingdom utilized Random Forest to predict depression, identifying important factors such as loan status, gender, age, marital status, financial difficulties, academic stress, homesickness, and loneliness. The model achieved an accuracy of 80%, emphasizing the need for targeted interventions that address the multidimensional aspects of students’ lives54. Similarly, another study evaluated the effectiveness of machine learning in predicting treatment outcomes in a digital mental health intervention targeting depression and anxiety. The Random Forest model achieved high accuracy and highlighted key predictors such as pre-treatment symptoms, self-reported motivation, referral type, and work productivity55. In Southeast Asia, research involving university students developed machine learning classifiers, with Random Forest attaining high accuracy in predicting mental well-being. Key predictors included body mass index, weekly physical activity, GPA, sedentary behavior, and age56. Furthermore, a study on bipolar disorder patients in Colombia demonstrated the potential of ML in predicting hospital admissions and re-admissions using electronic health records. The Random Forest model achieved an accuracy of 95.1% and an AUC of 98%, identifying psychiatric emergency visits, outpatient follow-up appointments, and age as primary predictors57.
Feature importance analysis further confirmed that exposure to traumatic events and experiences of violence were the most significant contributors to screening positive for at least one mental health condition, as illustrated in Fig. 4a. These findings are consistent with existing literature. Traumatic experiences increase vulnerability to mental health disorders, often leading individuals to cope through harmful behaviors such as substance use or self-harm58. Likewise, individuals who have experienced violence are at a significantly higher risk of developing mental health conditions59. Therefore, the present findings support prior evidence indicating that violence and trauma are key drivers of mental health vulnerability.
Limitations
This study offers valuable insights into the use of machine learning for predicting mental health outcomes and serves as a significant resource for exploring factors associated with both mental health conditions and comorbidity among youth. However, several limitations and concerns regarding the generalizability of the findings must be acknowledged. Firstly, the study utilized cross-sectional data, capturing information at a single time point. This approach may not adequately reflect the temporal dynamics and variability of mental health conditions, thereby limiting the model’s capacity to generalize across different real-world scenarios when applied in practice.
Secondly, the analysis was restricted to social and biological factors due to the nature of the dataset. Key psychological and cognitive variables; such as resilience, coping mechanisms, and self-esteem along with other influential factors like family functioning, stigma, discrimination, help-seeking behaviors, digital environment, and cyberbullying, were not included. The omission of these potentially significant variables may introduce selection bias and reduce the comprehensiveness and generalizability of the results.
Thirdly, the external validity of the model may be constrained. Its performance might not translate well to different populations or settings that vary in terms of demographics, resources, social support systems, behavioral norms, or care practices. Moreover, the model’s temporal validity may be affected as health care practices, risk factor prevalence, and population characteristics can evolve over time, further influencing model applicability.
Lastly, although the multiclass classification approach employed in this study provides a more refined analysis than binary classification, it does not account for the exact combinations or co-occurrence patterns of specific mental disorders. Additionally, it does not incorporate the severity or intensity of the conditions, which are critical in understanding the full spectrum of mental health comorbidity. This limitation underscores the need for more detailed clinical data and longitudinal approaches in future research to better capture the complexity of mental health conditions.
Conclusion
This study represents an innovative effort to leverage machine learning techniques to predict mental health outcomes and identify potential risk factors associated with mental health comorbidity among youth, using data from the Rwanda Mental Health Cross-Sectional Survey. The study demonstrated the potential of machine learning in predicting mental health vulnerability. The findings indicate that the random forest model outperformed other models in identifying factors contributing to mental health vulnerability, achieving an accuracy of 87.8% and an AUC of 83.59%. Exposure to traumatic events, violence, heavy drinking, and a family history of mental health issues emerged as the most significant risk factors associated with the development of at least one mental disorder. The random forest model also showed solid performance in predicting mental health comorbidity, with an accuracy of 75% and an AUC of 0.738. However, the F1-score of 71.1% indicates a modest limitation in detecting comorbidity cases, particularly in the context of highly imbalanced data.
Key factors such as traumatic experiences, exposure to violence, affiliation with pro-social groups, family history of mental disorders, experiences of lifetime loss, heavy drinking, and prior mental health conditions were identified as significant predictors of mental health comorbidity. These findings are consistent with existing literature and further underscore the importance of addressing these risk factors in youth mental health interventions.
This study contributes to the existing body of knowledge by demonstrating the applicability of machine learning models in mental health research within the Rwandan context. Moreover, it highlights the importance of identifying and addressing high-risk factors in mental health interventions and policies. The findings emphasize the need for targeted support and tailored strategies for individuals who are at an increased risk of developing mental health conditions.
Acknowledgements
We gratefully acknowledge the contribution of the Rwanda Biomedical Center in Rwanda for providing access to data used in this study. We also extend our sincere appreciation to the University of Rwanda’s Centre for mental health and African Centre of Excellence in Data Science for providing the required resources to execute this project.
Author contributions
This study was conceptualized and designed by FN, VS and CT. FN, VS, CT, JK and JI made contributions to the acquisition of the dataset. FN carried out data analysis, VS, CT, JI, JK, MN, SN contributed to the review of data analysis and the interpretation of the results. MN, IK, MU, SHM, CEN and CT provided critical feedback and helped in revising the manuscript. The overall project was supervised by VS. All authors reviewed and approved the final manuscript.
Funding
We gratefully acknowledge the funding provided by Research training in Data Science for Health in Rwanda under NIH Grant: U2RTW012122-04 in collaboration with the University of Rwanda, The Regional Centre of Excellence in Biomedical Engineering and EHealth, African Institute for Mathematical Sciences and Washington University in Saint Louis. The funder had no involvement in the study design, data acquisition and analysis, decision to publish, or the preparation of the manuscript.
Data availability
The used and/or analysed datasets during this study are available from the corresponding author upon reasonable request.
Code availability
The source code used in this study is available at https://github.com/nfauste/Mental-health-prediction. The code repository includes all scripts necessary to reproduce the analyses and results presented in this work.
Declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Prior to starting the survey, ethical approval was acquired from the Rwanda National Ethics Committee (RNEC) under reference number 0061/RNEC/2018, dated February 15, 2018 and every participant granted informed consent by signing an informed consent form before participating in the survey. All methods were performed in accordance with the relevant guidelines and regulations.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Khune, A. A., Rathod, H. K., Deshmukh, S. P. & Chede, S. B. Mental health, depressive disorder, and its management: A review. GSC Biol. Pharm. Sci.25(2), 1–13 (2023). [Google Scholar]
- 2.Collaborators, G. M. D. et al. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry.9(2), 137–150 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mudiyanselage, K. W. W. et al. The effectiveness of mental health interventions involving non-specialists and digital technology in low-and middle-income countries-a systematic review. J. Psychosomatic Res.169, 111320 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Purgato, M. et al. Promotion, prevention and treatment interventions for mental health in low-and middle-income countries through a task-shifting approach. Epidemiol. Psychiatr. Sci.29, e150 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Consortium WWMHS, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. Jama. 291(21), 2581–2590 (2004). [DOI] [PubMed]
- 6.Kovacevic, R. Mental health: Lessons learned in 2020 for 2021 and forward. World Bank Blogs Retrieved November.7, 2022 (2021). [Google Scholar]
- 7.Sankoh, O., Sevalie, S. & Weston, M. Mental health in Africa. Lancet Glob. Health.6(9), e954–e955 (2018). [DOI] [PubMed] [Google Scholar]
- 8.McNab, S. E. et al. The silent burden: A landscape analysis of common perinatal mental disorders in low-and middle-income countries. BMC Pregnancy Childbirth.22(1), 342 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kayiteshonga, Y., Sezibera, V., Mugabo, L. & Iyamuremye, J. D. Prevalence of mental disorders, associated co-morbidities, health care knowledge and service utilization in Rwanda-towards a blueprint for promoting mental health care services in low-and middle-income countries?. BMC Public Health.22(1), 1–13 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patel, V. et al. The Lancet Commission on global mental health and sustainable development. Lancet.392(10157), 1553–1598 (2018). [DOI] [PubMed] [Google Scholar]
- 11.Atzil-Slonim, D., Penedo, J. M. G. & Lutz, W. Leveraging novel technologies and artificial intelligence to advance practice-oriented research. Administration Policy Mental Health Mental Health Services Res.51(3), 306–317 (2024). [DOI] [PubMed] [Google Scholar]
- 12.Kazdin, A.E. Nonprecsion (standard) psychosocial interventions for the treatment of mental disorders. Int. J. Mental Health Promotion. 24(4), (2022)
- 13.Katiyar, K. AI-based predictive analytics for patients’ psychological disorder. in Predictive Analytics of Psychological Disorders in Healthcare: Data Analytics on Psychological Disorders, 37–53. (Springer, 2022)
- 14.Srividya, M., Mohanavalli, S. & Bhalaji, N. Behavioral modeling for mental health using machine learning algorithms. J. Med. Syst.42, 1–12 (2018). [DOI] [PubMed] [Google Scholar]
- 15.Shatte, A. B., Hutchinson, D. M. & Teague, S. J. Machine learning in mental health: A scoping review of methods and applications. Psychol. Med.49(9), 1426–1448 (2019). [DOI] [PubMed] [Google Scholar]
- 16.Tutun, S. et al. An AI-based decision support system for predicting mental health disorders. Inform. Syst. Front.25(3), 1261–1276 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jordan, M. I. & Mitchell, T. M. Machine learning: Trends, perspectives, and prospects. Science.349(6245), 255–260 (2015). [DOI] [PubMed] [Google Scholar]
- 18.Jiang, T., Gradus, J. L. & Rosellini, A. J. Supervised machine learning: A brief primer. Behav, Therapy.51(5), 675–687 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tiffin, P. A. & Paton, L. W. Rise of the machines? Machine learning approaches and mental health: Opportunities and challenges. Br. J. Psychiatry.213(3), 509–510 (2018). [DOI] [PubMed] [Google Scholar]
- 20.Cook, B. L., Progovac, A. M., Chen, P., Mullin, B., Hou, S., Baca-Garcia, E, et al. Novel use of natural language processing (NLP) to predict suicidal ideation and psychiatric symptoms in a text-based mental health intervention in Madrid. Computational and mathematical methods in medicine. 2016;2016. [DOI] [PMC free article] [PubMed]
- 21.D’Alfonso, S. AI in mental health. Curr. Opin. Psychol. 36, 112–117 (2020). [DOI] [PubMed]
- 22.Jan, Z. et al. The role of machine learning in diagnosing bipolar disorder: Scoping review. J. Med. Internet Res.23(11), e29749 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alanazi, S. A. et al. Public’s mental health monitoring via sentimental analysis of financial text using machine learning techniques. Int. J. Environ. Res. Public Health.19(15), 9695 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Samuelson, K. W. et al. Mental health and resilience during the coronavirus pandemic: A machine learning approach. J. Clin. Psychol.78(5), 821–846 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Van Mens, K. et al. Predicting future service use in Dutch mental healthcare: A machine learning approach. Administration Policy Mental Health Mental Health Services Res.49(1), 116–124 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yu, J. et al. A machine learning approach to passively informed prediction of mental health risk in people with diabetes: Retrospective case-control analysis. J. Med. Internet Res.23(8), e27709 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Graham, S. et al. Artificial intelligence for mental health and mental illnesses: An overview. Curr. Psychiatry Rep.21, 1–18 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dwyer, D. B., Falkai, P. & Koutsouleris, N. Machine learning approaches for clinical psychology and psychiatry. Annu. Rev. Clin. Psychol.14, 91–118 (2018). [DOI] [PubMed] [Google Scholar]
- 29.Dipnall, J. F. et al. Fusing data mining, machine learning and traditional statistics to detect biomarkers associated with depression. PloS One.11(2), e0148195 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chung, J. & Teo, J. Mental health prediction using machine learning: Taxonomy, applications, and challenges. Appl. Comput. Intell. Soft Comput.2022, 1–19 (2022). [Google Scholar]
- 31.Sumathi, M., Poorna, B. Prediction of mental health problems among children using machine learning techniques. Int. J. Adv. Comput. Sci. Appl. 7(1). (2016)
- 32.Dehghan, P., Alashwal, H. & Moustafa, A. A. Applications of machine learning to behavioral sciences focus on categorical data. Discover Psychol.2(1), 22 (2022). [Google Scholar]
- 33.Kim, J. et al. Machine learning for mental health in social media Bibliometric study. J. Med. Internet Res.23(3), e24870 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nilsen, P. et al. Accelerating the impact of artificial intelligence in mental healthcare through implementation science. Implement. Res. Practice.3, 26334895221112030 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ponce, E. K., Cruz, M.F., & Andrade-Arenas, L. Machine learning applied to prevention and mental health care in Peru. Int. J. Adv. Comput. Sci. Appl. 13(1). (2022)
- 36.Abdul Rahman, H., Kwicklis, M., Ottom, M., Amornsriwatanakul, A., H Abdul-Mumin, K., Rosenberg, M, et al. Machine LearningBased prediction of mental WellBeing using health behavior data from University Students. Bioengineering. 10(5), 575. (2023) [DOI] [PMC free article] [PubMed]
- 37.Clark-Kazak, C. R. Towards a working definition and application of social age in international development studies. J. Develop. Stud.45(8), 1307–1324 (2009). [Google Scholar]
- 38.Sheehan, D. V. et al. The MiniInternational Neuropsychiatric Interview MINI: The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry.59(20), 22–33 (1998). [PubMed] [Google Scholar]
- 39.Betancourt, T. et al. Validating the center for epidemiological studies depression scale for children in Rwanda. J. Am. Acad. Child Adolesc. Psychiatry.51(12), 1284–1292 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Munyandamutsa, N., Mahoro Nkubamugisha, P., Gex-Fabry, M. & Eytan, A. Mental and physical health in Rwanda 14 years after the genocide. Social Psychiatry Psychiatric Epidemiol.47, 1753–1761 (2012). [DOI] [PubMed] [Google Scholar]
- 41.Muwonge, J., Umubyeyi, A., Rugema, L. & Krantz, G. Suicidal behaviour and clinical correlates in young adults in Rwanda: A population-based, cross-sectional study. J. Glob. Health Rep.3, e2019080 (2019). [Google Scholar]
- 42.Engel, G. L. The clinical application of the biopsychosocial model. J. Med. Philos.6(2), 101–124 (1981). [DOI] [PubMed] [Google Scholar]
- 43.Maharana, K., Mondal, S. & Nemade, B. A review: Data pre-processing and data augmentation techniques. Glob. Transitions Proc.3(1), 91–99 (2022). [Google Scholar]
- 44.Azencott, C. A. Introduction au Machine Learning-2e éd. Dunod; (2022).
- 45.Agresti, A. Categorical Data Analysis, Vol. 792. (Wiley, 2012).
- 46.Hastie, T., Tibshirani, R., Friedman, J., Hastie, T., Tibshirani, R., & Friedman, J. Unsupervised learning. The elements of statistical learning: Data mining, inference, and prediction. p. 485–585, (2009)
- 47.Biau, G. & Scornet, E. A random forest guided tour. Test.25, 197–227 (2016). [Google Scholar]
- 48.Breiman, L. Random forests. Machine learning.45, 5–32 (2001). [Google Scholar]
- 49.Vapnik, V. The Nature of Statistical Learning Theory. (Springer2Verlag, 1995)
- 50.Bentéjac, C., Csörgő, A. & Martínez-Muñoz, G. A comparative analysis of gradient boosting algorithms. Artif. Intell. Rev.54, 1937–1967 (2021). [Google Scholar]
- 51.Chen, T., & Guestrin, C. Xgboost: A scalable tree boosting system. In: Proceedings of the 22nd acm sigkdd international conference on knowledge discovery and data mining; p. 785–794. (2016)
- 52.Tharwat, A. Classification assessment methods. Appl. Comput. Inform.17(1), 168–192 (2020). [Google Scholar]
- 53.Wardhani, N. W. S. et al. international conference on computer, control, informatics and its applications (IC3INA). IEEE. 2019, 14–18 (2019).
- 54.Rahman, M. A. & Kohli, T. Mental health analysis of international students using machine learning techniques. Plos One.19(6), e0304132 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hornstein, S., Forman-Hoffman, V., Nazander, A., Ranta, K. & Hilbert, K. Predicting therapy outcome in a digital mental health intervention for depression and anxiety A machine learning approach. Digital Health.7, 20552076211060660 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rahman, H. A., Kwicklis, M., Ottom, M., Amornsriwatanakul, A., AbdulMumin, K. H., Rosenberg, M., et al. Prediction Modeling of Mental Well-Being Using Health Behavior Data of College Students. Research Square. (2022)
- 57.Palacios-Ariza, M. A. et al. Prediction of patient admission and readmission in adults from a Colombian cohort with bipolar disorder using artificial intelligence. Front. Psychiatry.14, 1266548 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Butler, L. D., Critelli, F. M. & Rinfrette, E. S. Trauma-informed care and mental health. Directions Psychiatry.31(3), 197–212 (2011). [Google Scholar]
- 59.Patel, D. Violence and Mental Health: Opportunities for Prevention and Early Detection: Proceedings of a Workshop. National Academies Press (2018) [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The used and/or analysed datasets during this study are available from the corresponding author upon reasonable request.
The source code used in this study is available at https://github.com/nfauste/Mental-health-prediction. The code repository includes all scripts necessary to reproduce the analyses and results presented in this work.