Abstract
Increased phosphorylation of TDP-43 is a pathological hallmark of several neurodegenerative disorders, including amyotrophic lateral sclerosis (ALS) and frontotemporal dementia (FTD). However, the regulation and roles of TDP-43 phosphorylation remain incompletely understood. A variety of techniques have been utilized to understand TDP-43 phosphorylation, including kinase/phosphatase manipulation, phosphomimic variants, and genetic, physical, or chemical inducement in a variety of cell cultures and animal models, and via analyses of post-mortem human tissues. These studies have produced conflicting results: suggesting incongruously that TDP-43 phosphorylation may either drive disease progression or serve a neuroprotective role. In this review, we explore the roles of regulators of TDP-43 phosphorylation including the putative TDP-43 kinases c-Abl, CDC7, CK1, CK2, IKKβ, p38α/MAPK14, MEK1, TTBK1, and TTBK2, and TDP-43 phosphatases PP1, PP2A, and PP2B, in disease. Building on recent studies, we also examine the consequences of TDP-43 phosphorylation on TDP-43 pathology, especially related to TDP-43 mislocalisation, liquid–liquid phase separation, aggregation, and neurotoxicity. By comparing conflicting findings from various techniques and models, this review highlights both the discrepancies and unresolved aspects in the understanding of TDP-43 phosphorylation. We propose that the role of TDP-43 phosphorylation is site and context dependent, and includes regulation of liquid–liquid phase separation, subcellular mislocalisation, and degradation. We further suggest that greater consideration of the normal functions of the regulators of TDP-43 phosphorylation that may be perturbed in disease is warranted. This synthesis aims to build towards a comprehensive understanding of the complex role of TDP-43 phosphorylation in the pathogenesis of neurodegeneration.
Graphical Abstract
TDP-43 is subject to phosphorylation by kinases and dephosphorylation by phosphatases, which variably impacts protein localisation, aggregation, and neurotoxicity in neurodegenerative diseases.
Keywords: TDP-43, Phosphorylation, Amyotrophic lateral sclerosis, Frontotemporal dementia, Post-translational modifications, Neurodegeneration, Kinase, Phosphatase
Background
Amyotrophic lateral sclerosis (ALS), frontotemporal dementia (FTD), and limbic-predominant age-related TDP-43 encephalopathy (LATE) are fatal and devastating neurodegenerative disorders characterised by the cytoplasmic mislocalisation and aggregation of RNA-binding proteins. Among these proteins, TAR DNA-binding protein 43 (TDP-43) is the primary aggregating protein driving pathology in approximately 97% of ALS, 50% of FTD, and all LATE cases [1, 2]. Furthermore, TDP-43-positive aggregates have been observed in a subset of other neurodegenerative disorders including Alzheimer’s disease, Parkinson’s disease, and Huntington’s disease (HD) [3–10]. As a unifying feature among the heterogeneity between and within these disorders, TDP-43 aggregation and abnormal TDP-43 post-translation modifications (PTMs), particularly phosphorylation, has emerged as a key pathological hallmarks of TDP-43 proteinopathy. Despite this, the causes, implications, and contributions of aberrant TDP-43 phosphorylation in disease pathogenesis remain unclear [11–13]. While TDP-43 phosphorylation correlated with disease progression [14–30], emerging evidence suggests that TDP-43 phosphorylation may be part of a neuro-protective mechanism [31–35]. This review discusses the regulators, timing, and roles of TDP-43 phosphorylation to explore whether it is protective or disease-contributing.
TDP-43
Function
TDP-43 is an essential RNA and DNA binding protein encoded by the human TARDBP gene, with vital roles in gene expression and RNA metabolism. This includes critical processes such as transcription, translation, RNA splicing, and mRNA stability (reviewed in [36]). TDP-43 interacts with over 4,000 mRNA transcripts, with high specificity towards UG-rich RNA sequences, and self-regulates expression levels through a negative feedback loop by destabilising its own mRNA [37–39]. TDP-43 plays an important role in RNA splicing, with loss of nuclear TDP-43 causing mis-splicing with emerging implications for neurodegenerative pathology. For example, TDP-43 mislocalisation induces cryptic exon inclusion in genes that regulate neuronal function such as UNC13A and STMN2, leading to decreased expression of their translated proteins [40–44]. TDP-43 also plays a key role in cellular stress responses by regulating mRNA levels, such as G3BP1 [45], to regulate stress granule assembly, apoptosis, axonal transport, and ribonucleoprotein transport [3, 36, 46, 47]. By recruitment to cytoplasmic stress granules in response to cellular stress, TDP-43 also supports stress granule formation and stalling ribosomes [36, 47–49]. TDP-43 is modified by many different PTMs, including acetylation, SUMOylation, ubiquitination, nitrosylation, methylation, C-terminal fragmentation, disulfide bridge formation, citrullination, and phosphorylation [11–13, 50–57]. These modifications likely play crucial roles in regulating TDP-43 function and aggregation propensity [36].
Localisation
TDP-43 is a ubiquitously expressed protein translated in the cytoplasm and transported to the nucleus due to its nuclear localisation signal (NLS). Physiological TDP-43 is primarily localised in the nucleus yet can shuttle between the cytoplasm and nucleus [58]. In Drosophila neurons, TDP-43 forms cytoplasmic mRNP granules that utilize microtubule-dependent transport to deliver target mRNA to distant neuronal compartments [59]. Similarly, in mouse primary hippocampal neurons, TDP-43 associates with mRNP granules and regulates their transport in dendrites to coordinate mRNA localisation and translation [60]. During cellular stress, TDP-43 translocates to the cytoplasm for stress granules assembly [47, 48]. TDP-43 export to the cytoplasm is a passive process, while being actively transported into the nucleus by importins, for example the importin α/β heterodimer, which recognises the NLS of TDP-43 [61, 62]. TDP-43 is also present at low levels inside mitochondria of human motor and cortical neurons, though these levels are increased in post-mortem ALS/FTLD-TDP spinal cord and frontal context tissue, as well as mice and primary rat motor neurons expressing pathological TDP-43 variants [63–65]. This dynamic localisation underscores the role of TDP-43 in responding to cellular conditions and stress.
Structure
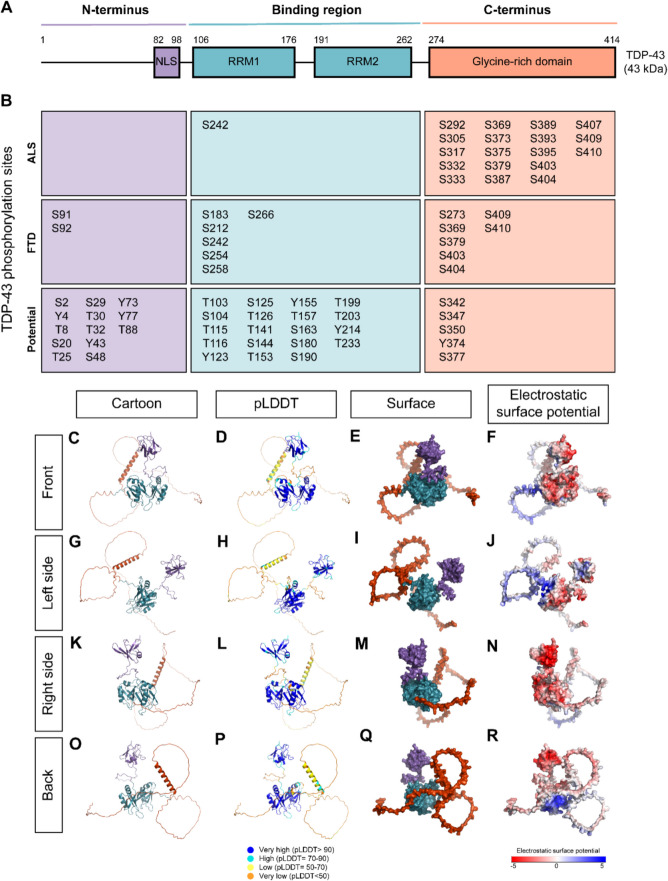
TDP-43 is comprised of 414 amino acids that contain a NLS, two RNA-recognition motifs (RRM1, RRM2), and an intrinsically disordered C-terminal domain (CTD) consisting of glycine-rich and glutamine-asparagine-rich regions [66] (Fig. 1A). The C-terminus lacks a well-defined native structure, as highlighted by its low predicted Local Distance Difference Test (pLDDT) score, a measure of confidence in protein structure predictions, by AlphaFold3, a protein structure prediction tool [67] (Fig. 1D,H,L,P). This low score reflects the structural flexibility of the C-terminus, which enhances its mobility and malleability and allows interaction with a diverse range of molecular partners [68]. The C-terminus is also referred to as a prion-like domain due to its high proclivity for aggregation and the location of many sporadic and familial ALS/FTLD-TDP-associated mutations [69–71]. The N-terminus has been implicated in multiple roles, including its ability to promote TDP-43 oligomerization and DNA binding affinity in vitro and in vivo systems [72–74].
Fig. 1.
TDP-43 structure and phosphorylation sites. A Schematic of TDP-43, showing the N-terminus region (purple) with a nuclear localising signal (NLS), the binding region (blue) with two RNA-recognition motifs (RRM1, RRM2), and the C-terminus region (orange) with a glycine-rich domain. B TDP-43 phosphorylation sites detected in post-mortem ALS and FTLD-TDP brain and spinal cord tissue, along with potential phosphorylation sites [11–13, 52, 75–77]. Sites are listed by amino acid (serine (S), threonine (T), or tyrosine (Y)) and coloured by their localisation (N-terminus, purple; binding region, blue; C-terminus, orange). C-F “front”, (G-J) “left side”, (K-N) “right side”, and (O-R) “back” view of TDP-43 (Q13148) structure as predicted by AlphaFold3 and visualised in PyMOL. TDP-43 is represented in cartoon (C,G,K,O) or surface (E,I,M,Q) form, with the N-terminus in purple, binding region in blue, and the C-terminus in orange. D,H,L,P TDP-43 cartoon coloured by predicted Local Distance Difference Test (pLDDT), which shows regions with very high (dark blue, pLDDT > 90), high (light blue, pLDDT = 70–90), low (yellow, pLDDT = 50–70), and very low (orange, pLDDT < 50) confidence in the predicted structure as calculated by AlphaFold3. F,J,N,R Electrostatic surface potential (ESP) was calculated using APBS Electrostatics Plugin in Pymol where regions coloured red indicates negative potential, while regions indicate neutral potential, and blue indicate positive potential
Pathology
TDP-43 pathology is a progressive process that results in the accumulation of cytoplasmic TDP-43 aggregates. This occurs notably in the upper and lower motor neurons in the motor cortex and spinal cord for ALS, and von Economo neurons and fork cells in the frontoinsular and anterior cingulate cortices in most cases of frontotemporal lobar degeneration with TDP-43 pathology (FTLD-TDP), the pathological entity which causes approximately half of all FTD [78–81] (Fig. 2). An important avenue for future research is mapping the brain regions where specific TDP-43 phosphorylation sites are detected, as selective neuronal vulnerability may be influenced by region-specific phosphorylation patterns. In disease, TDP-43 mislocalises to the cytoplasm, leading to an accumulation of cytoplasmic and loss of nuclear TDP-43 [55, 82]. The mechanisms underlying TDP-43 aggregation are complex, with emerging evidence implicating liquid–liquid phase separation (LLPS) as an intermediate phase in the transition from soluble to aggregated TDP-43 [83–90]. LLPS is the formation of membrane-less protein organelles, also known as liquid droplets, to compartmentalise various biological processes such as the spatiotemporal organisation of RNA processing [91–93]. Recent studies have revealed that TDP-43 undergoes LLPS, forming dynamic and reversible liquid-like assemblies to create specialised cellular microenvironments for RNA processing and metabolism, such as stress granules and paraspeckles [94, 95]. Additionally, TDP-43 can form spherical shells called anisosomes when unable to bind RNA through disease-related mutations or acetylation [89, 96]. Intrinsically disordered regions (IDRs), like the TDP-43 CTD, are a common feature of proteins that undergo LLPS and have been reported to mediate the dynamics of the liquid droplet [97, 98]. LLPS-mediated aggregation has been observed in other neurodegenerative proteins, including α-synuclein, tau, FUS and hnRNPA1 [93–95, 98–104]. When LLPS dynamics are disrupted, TDP-43 liquid droplets can mature into a less dynamic gel-like state before solidifying to form aggregates [36, 83]. These aggregates represent a hallmark of TDP-43 pathology and are observed in post-mortem tissue [11, 55]. Aggregated TDP-43 exhibits several PTMs including acetylation, phosphorylation, SUMOylation, and ubiquitination [11, 51, 55, 82, 105]. Several studies suggest that TDP-43 aggregation and LLPS are driven by its C-terminal IDR, the region which experiences the most pathological phosphorylation [99, 106, 107] (Fig. 1B). Phosphorylated TDP-43 aggregates have also been detected in lysosomes in post-mortem ALS/FTLD pre-frontal cortex tissue, suggesting autophagy plays a role in cytoplasmic TDP-43 accumulation [108].
Fig. 2.
TDP-43 pathology in ALS and FTLD-TDP. Physiological TDP-43 is primarily nuclear with some cytoplasm shuttling and can undergo liquid liquid phase separation (LLPS) to form liquid droplets, membrane-less organelles that provide microenvironments for cellular processes. In disease, TDP-43 mislocalises to the cytoplasm and forms insoluble aggregates, possibly through transition from liquid droplets into less-dynamic gel-like state, then solid state aggregates. This process is toxic to the neurons due to a loss of nuclear TDP-43 and gain of TDP-43 aggregates. The neurotoxicity leads to a loss of neurons including upper and lower motor neurons within the motor cortex and spinal cord for ALS (blue), and von Economo neurons and fork cells in the frontoinsular and anterior cingulate cortices for FTLD-TDP (red). Figure constructed using biorender.com
TDP-43 pathology is hypothesised to drive dual toxicity: a gain-of-function toxicity through the presence of cytoplasmic aggregates and a loss-of-function toxicity due to the depletion of functional nuclear TDP-43 [36, 109–113]. Loss of functional TDP-43 affects various RNA and protein targets, leading to several detrimental events linked with neurodegenerative processes. One notable example is the mis-splicing of UNC13A mRNA due to TDP-43 cytoplasmic mislocalisation, causing reduced UNC13A protein expression, which is implicated in the pathogenesis of ALS and FTLD-TDP [40, 43]. Furthermore, TDP-43 pathology and phosphorylation may be controlled by an unidentified direct or an indirect mechanism, for example the accumulation of TMEM106B, a risk factor for FTD, correlates with insoluble phosphorylated TDP-43 levels in FTLD-TDP type A post-mortem tissue [114]. This evolving understanding of TDP-43 pathology offers valuable insights into the complex interplay of factors, including phosphorylation, which contribute to the pathogenesis of neurodegenerative diseases.
TDP-43 phosphorylation
Phosphorylation is a fundamental and reversible PTM involving the covalent attachment of a negatively charged phosphoryl group to specific amino acids, primarily serine, tyrosine, or threonine in eukaryotes [115, 116]. Structural studies suggest that serine and threonine phosphorylation have distinct conformational effects, with threonine phosphorylation inducing greater rigidity through a process known as pseudocyclization, wherein noncovalent interactions stabilize a constrained backbone conformation that mimics proline’s backbone cyclization [117]. Phosphorylated TDP-43 is a major pathological hallmark, consistently observed in ALS and FTLD-TDP but poorly detected in physiological conditions [11–13]. This suggests that TDP-43 in healthy tissue is either not phosphorylated or experiences low levels of transient phosphorylation due to an equal balance between kinase and phosphatase activity. Notably, phosphorylation at S409/410 is commonly used to identify TDP-43 inclusions in brain and spinal cord as it is highly consistent in disease and due to the development of highly specific and reliable antibodies [11–13]. Of the 64 potential TDP-43 phosphorylation sites, 27 have been detected in ALS or FTLD-TDP via mass spectrometry approaches, with six major pathological sites recognised: S369, S379, S403/404, and S409/410 [11–13, 52, 75–77] (Fig. 1B). Nineteen of these pathological sites are within the C-terminus, potentially owing to the susceptibility of IDRs to PTMs and its role in mediating LLPS [118–121]. The presence of phosphorylated TDP-43 in disease therefore raises the question of whether it contributes to disease progression and neuron loss (i.e., causative) or a cellular defence mechanism (i.e., protective).
Techniques for studying TDP-43 phosphorylation
To investigate the role of TDP-43 phosphorylation in disease, several in vitro and in vivo models and various experimental approaches have been utilised (Table 1). Manipulating the abundance levels of kinases and phosphatases through overexpression, knockdown/out, or pharmacological inhibition have played a prominent role in studying TDP-43 phosphorylation. Overexpression of kinases that target TDP-43 can induce TDP-43 phosphorylation in vitro and in vivo, for example TTBK1 expression in HEK293 cells increased TDP-43 mislocalisation and in C. elegans enhanced TDP-43 cytoplasmic accumulation and negatively impacted locomotion [22, 25]. Conversely, knockdown or knockout approaches, achieved through techniques such as RNA interference or CRISPR/Cas9 gene editing, can assist in identifying the consequences of decreased TDP-43 phosphorylation by targeting specific kinases. For instance, TTBK1 knockdown has been shown to ameliorate neurite length and neuron loss associated with TDP-43 overexpression in iPSC-derived neurons [25]. Similar to kinase manipulation, phosphatase expression can be adjusted to modulate TDP-43 dephosphorylation activity. For instance, knockout of the phosphatase calcineurin led to increased TDP-43 phosphorylation, enhanced TDP-43 accumulation, and exacerbated motor phenotypes in C. elegans [122].
Table 1.
Techniques to study TDP-43 phosphorylation
| Technique | Description | Outcome | Strengths | Limitations | TDP-43 studies |
|---|---|---|---|---|---|
| Kinase overexpression | Increased expression of kinases | ↑ substrate phosphorylation |
• Biologically relevant (increased kinase expression in ALS/FTD) • True phosphorylation • Reversible |
• Off-target effects (enhanced phosphorylation of other substrates) | |
| Kinase inhibition or knockout/down | Eliminate or reduce expression (knockout/down) or activity (therapeutic inhibition) of kinase | ↓ substrate phosphorylation | • True phosphorylation | • Off-target effects (reduced phosphorylation of other substrates) | |
| Phosphatase inhibition or knockout/down | Eliminate or reduce expression (knockout/down) or activity (therapeutic inhibition) of kinase |
↑ substrate phosphorylation (↓ dephosphorylation) |
• True phosphorylation • Biologically relevant (decreased phosphatase expression in ALS/FTD) |
• Off-target effects (enhanced phosphorylation of other substrates) |
In vitro In vivo[122] |
| Phosphomimicry | Amino acid substitution of substrate – replace phosphorylation site (serine/threonine/tyrosine) with aspartate or glutamate to mimic or alanine to prevent phosphorylation | Mimic or prevent phosphorylation |
• Site specific • Substrate specific |
• Irreversible • Alanine loss of hydrogen bond capacity • May not be sufficient replacement for phosphorylation [126, 127, 280] - Charge difference - Smaller steric hindrance |
In vivo [31] |
| In vitro kinase assay | Incubation of recombinant/purified substrate and kinase or phosphatase | Study kinase/phosphatase and substrate interaction | • Purified sample (for direct interaction studies) | • Artificial conditions | [14, 16, 25, 26, 29, 30, 34, 128] |
| Inducement | Physical changes e.g. heat shock | ↑ or ↓ phosphorylation | • Off-target effects | [32] | |
| Inducement | Small molecule/chemical e.g. ethacrynic acid, sodium arsenite | ↑ or ↓ phosphorylation | • Off-target effects | [15, 19, 20, 26, 30, 32, 51, 56, 122, 123, 131, 132] | |
| Inducement | Biological/genetic e.g. TDP-43 optogenetic aggregation, inducible TDP-43 oligomerisation | ↑ or ↓ phosphorylation | • Off-target effects | [28, 173] | |
| Structural experiments | Experimental (e.g. cryoEM) or bioinformatic (e.g. AlphaFold2) approaches to measure TDP-43 structure | Determine how TDP-43 phosphorylation influences its structure |
• High resolution structural data • Provides insight into molecular mechanisms through structural changes |
• Poor reliability for IDRs • Difficult to capture dynamic phosphorylation |
[33] |
| Coarse-grain simulation | Determine how TDP-43 phosphorylation influences TDP-43 dynamics, stability, and interactions |
• Models large-scale dynamics • Useful to generate hypotheses |
• Artificial approach • Low reliability for highly flexibly regions like IDRs • Requires experimental validation • Limited by accuracy of force fields |
[34, 128] |
Since physiological TDP-43 phosphorylation is not typically detectable under basal conditions, these approaches require a model system where TDP-43 phosphorylation can be induced. Such models include using ALS or FTLD-TDP immortalised cells, inducement by cellular stress or glutathione depletion, expression of mutant TDP-43, or TDP-43 overexpression [19, 23, 24, 26, 27, 30, 123]. Manipulating these enzymes may cause off-target effects by altering other cellular pathways. For example, in addition to phosphorylating TDP-43, CK2 has over 350 protein substrates, many of which are involved in spliceosome functions [124, 125]. This makes it challenging to distinguish if pathological changes from kinase or phosphatase manipulation are due primarily to TDP-43 phosphorylation or to secondary effects of other kinase target pathways. Thus, while these approaches are powerful for studying TDP-43 phosphorylation in a disease context, their findings must be validated through complementary approaches.
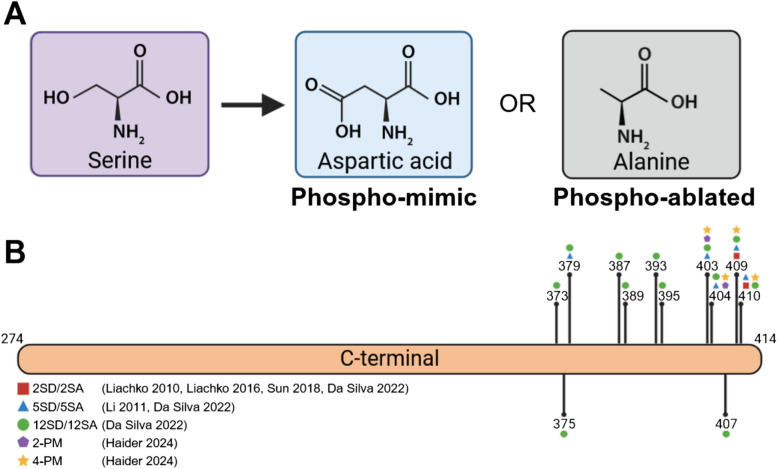
Phosphomimicry is a technique to study the effects of phosphorylation at specific residues, both in vitro and in vivo. This method involves substituting phosphorylation-specific amino acids with either phospho-mimic residues, glutamic acid or aspartic acid, or phospho-ablate residues, such as alanine (Fig. 3). Glutamic acid and aspartic acid carry a negative charge that mimics phosphorylation, while alanine lacks the hydroxyl group of serine, threonine or tyrosine which is necessary for phosphorylation and therefore prevents phosphorylation. This approach allows for precise control of phosphorylation at specific residues and avoids the off-target effects of kinase overexpression. However, conflicting results raise debate as to whether glutamic acid/aspartic acid accurately represent phosphorylation as their charge and steric hinderance is reduced compared to true serine phosphorylation [34, 126, 127]. Phosphomimicry is also a permanent change unaffected by kinase or phosphatase activity, which poses a challenge for studying dynamic processes.
Fig. 3.
Phosphomimic TDP-43 variants used in literature. Amino acid substitution can replace serine (purple) with aspartic acid (blue) to mimic or alanine (grey) to prepare phosphorylation. B Phosphomimic TDP-43 variants used to study C-terminal TDP-43 phosphorylation. Figure constructed using biorender.com
In vitro kinase and phosphatase assays have offered valuable insight into studying the dynamics of phosphorylated TDP-43 and its interactions with kinases and phosphatases. These assays involve the incubation of purified recombinant TDP-43 with a kinase or phosphatase and measuring the levels of phosphorylation or protein behaviour. For example, these assays have demonstrated that several kinases and phosphatases directly phosphorylate or dephosphorylated TDP-43 [11, 14, 15, 29, 35, 56, 122]. They also provide an opportunity to study TDP-43 oligomerisation and LLPS in a simplified environment that lacks regulatory elements [34]. However, this artificial environment is highly influenced by experimental conditions and lacks cellular factors which can influence protein structure, behaviour, and other PTMs. For example, Haider et al. [128] found that LLPS of CTD phosphomimic TDP-43 is dependent on salt concentration, which highlights that experimental conditions can influence findings. In vitro protein assays often do not reflect physiological levels which can lead to results that differ from in vivo conditions. Therefore, while in vitro kinase and phosphatase assays are invaluable for initial mechanistic studies, their findings must be validated in more complex in vitro and in vivo systems to ensure physiological relevance.
Additionally, several studies have reported that certain cellular stresses including impaired RNA binding (e.g. acetylation-mutant TDP-432 KQ), oxidative stress (e.g. glutathione depletion), and heat shock can trigger TDP-43 phosphorylation and accumulation of insoluble TDP-43 [32, 96, 129, 130]. For example, oxidative stress from glutathione depletion caused by ethacrynic acid treatment has been reported to induce TDP-43 phosphorylation at S409/410 in HEK293T and SH-SY5Y cells [19, 26, 30, 122, 131, 132], although the relevance of this chemical stressor to disease contexts remains unclear and may be cell type dependent. These findings provide insight into how environmental factors may contribute to the pathological phosphorylation of TDP-43 and provide models to test pharmaceutical regulators [19, 32, 130].
Bioinformatic approaches may be useful to predict how TDP-43 phosphorylation influences TDP-43 structure and interactions. However, most pathological TDP-43 phosphorylation sites lie within the IDR and have low structural reliability [67, 133], such that structural tools that can predict the impact of PTMs on proteins, such as AlphaFold3, may have limited reliability in defining this region (Fig. 1D,H,L,P). This has also caused challenges for cryogenic electron microscopy and other experimental structural techniques to determine the structure of the TDP-43 CTD. Coarse-grain simulations can model large-scale dynamics and interactions, offering a broader understanding of TDP-43 behaviour influenced by phosphorylation states [34, 128]. While bioinformatic approaches are powerful tools to study many parameters in a simple and cost-effective method, currently experimental validation is vital to ensure the findings are consistent with in vivo conditions.
Possible interdependence of TDP-43 phosphorylation sites
A recent study of tau protein, involved in neurodegeneration, has uncovered a complex network of phosphorylation site interdependence, suggesting that certain phosphorylation sites termed ‘master sites’ influence phosphorylation at other positions within the same protein [134]. A site interdependence screen was performed in HEK293T cells expressing phosphomimic tau variants at 17 sites with or without concomitant expression of 12 different tau kinases, and phospho-epitope-specific tau antibodies targeting 10 different sites were used to detect phosphorylation. Phosphorylation at three specific threonine residues caused the most significant phosphorylation at other sites, and ablation of each of these sites decreased phosphorylation at other sites, suggesting they can control tau hyperphosphorylation [134]. Since tau and TDP-43 both undergo disease-associated hyperphosphorylation and share several kinases, TDP-43 may also have a phosphorylation interdependence network. Indeed, a recent study suggests that TDP-43 phosphorylation sites influence each other as well as the addition of other PTMs. Aikio et al. [56] found that mimicking phosphorylation at S292 independently stimulates phosphorylation at S409/410 in SH-SY5Y cells, and reduced methylation at nearby R293. To date, few TDP-43 phosphorylation sites have been characterised in this manner, largely due to the lack of commercially available TDP-43 phosphorylation antibodies across the different phosphorylation sites. Increased availability of additional phosphorylation-specific TDP-43 antibodies would greatly increase understanding of this process.
Regulators of TDP-43 phosphorylation
Phosphorylation is regulated by kinases and phosphatases, which add and remove phosphate groups from other proteins. Dysfunction in these enzymes occurs in several neurodegenerative disorders and correlates with the increased phosphorylation of aggregation-prone proteins, including α-synuclein, FUS, tau, and TDP-43 [25, 135–141]. For example, the upregulation of casein kinase 1 (CK1) in ALS, FTLD-TDP, and Alzheimer’s disease suggests that enhanced kinase activity may drive the increased phosphorylation of aggregating protein substrates including TDP-43, tau, and α-synuclein [20, 24, 142–144]. At least 9 different kinases have been reported to phosphorylate TDP-43, including c-Abl [29], Cell Division Cycle 7 (CDC7) [14], Casein Kinase 1 (CK1), Casein Kinase 2 (CK2) [11], Inhibitor of nuclear factor kappa-B kinase subunit beta (IKKβ) [35], Mitogen-Activated Protein Kinase 14 (p38α/MAPK14), Mitogen-Activated Protein Kinase Kinase 1 (MEK1) [32], and Tau Tubulin Kinases 1 and 2 (TTBK1/TTBK2) [15], with varying levels of evidence available (Fig. 4, Table 2). To date, no protein-based screen has been performed to identify the full suite of TDP-43 kinases, and whether a single or multiple kinases are most important for driving TDP-43 phosphorylation and how the kinases may influence each other remains largely unexplored.
Fig. 4.

TDP-43 phosphorylation is regulated by kinases and phosphatases. Phosphorylation involves the transfer of the γ-ATP phosphate of ATP to TDP-43 by a kinase (purple). Dephosphorylation is the removal of this phosphate group by a phosphatase (pink). Reported TDP-43 kinases include c-Abl, CDC7, CK1, CK2, IKKβ, p38α/MAPK14, MEK1, TTBK1, and TTBK2 while phosphatases include PP1, PP2A and PP2B. Figure constructed using biorender.com
Table 2.
Reported TDP-43 kinases
| Kinase | Description | Accession | pTDP-43 sites | In vitro assay | TDP-43 studies | Other neurodegeneration substrates | Expression and activity in primary TDP-43 proteinopathies | Expression and activity in other neurodegenerative diseases |
|---|---|---|---|---|---|---|---|---|
| c-Abl | Tyrosine-protein kinase c-Abl | P00519 | Y43 [29] | [29] | [29] |
Parkin, PD [283] |
• ↑ ABL1 RNA in post-mortem sALS spinal motor neurons [149] • ↑ c-Abl protein abundance in rNLS8 TDP-43 mouse model [143] |
|
| CDC7 | Cell Division Cycle 7-related protein kinase | O00311 | S409, S410 [14, 26] | [14, 15] | [14, 173] | |||
| CK1 | Casein Kinase 1 |
P48729 (CK1α) P48730 (CK1δ) P49674 (CK1ε) Q9HCP0 (CK1γ1) P78368 (CK1γ2) Q9Y6M4 (CK1γ3) |
S2, Y4, T25, T88, S91, S92, T116, S183, S242, S254, S273, S292, S305, S342, S347, S350, S369, S375, S377, S379, S387, S389, S393, S395, S403, S404, S407, S409, S410 [11, 167] | [11, 34, 167, 173] | [16, 18, 19, 24, 171, 173, 279, 287] |
• ↑ CSNK1D mRNA in post-mortem sALS spinal cord and frontal cortex [24] • ↑ CSNK1E mRNA levels correlated with pTDP-43 in post-mortem sALS patient tissue [20] • ↑ CK1δ protein abundance in rNLS8 TDP-43 mouse model [143] |
• ↑ > 30-fold CK1δ in post-mortem AD hippocampus [144] • ↑ CSNK1D mRNA in post-mortem AD hippocampus, amygdala, entorhinal cortex and midtemporal gyrus [142] |
|
| CK2 | Casein Kinase 2 |
P68400 (CK2α) P19784 (CK2α’) P67860 (CK2β) |
S379, S409, S410 [11] | [11] | [188] |
APP-β, AD [168] α-synuclein, PD [172, 178–181] Tau, AD [182] |
• ↓ CK2 activity in AD [289] • ↑ CK2 in post-mortem AD hippocampus and temporal cortex [290] |
|
| IKKβ | Inhibitor of nuclear factor kappa-B kinase subunit beta | O14920 | T8, S92, S180 [35] | [35] | [35] | TDP-43, ALS, FTD [35] | • ↑ abundance in post-mortem FTLD-TDP frontal and temporal cortex [193] | |
| MAPK14 | Mitogen-Activated Protein Kinase 14 | Q16539 | S292, S409, S410 [56] | [56] | [32] |
Tau [291] TDP-43 [56] |
||
| MEK1 | Mitogen-Activated Protein Kinase Kinase | Q02750 | T153/Y155 [32] | N/A |
Tau TDP-43 [32] |
|||
| TTBK1 | Tau Tubulin Kinase 1 | Q5TCY1 | S409, S410 [15, 22] | [15, 25] | [15, 22, 25, 30, 279] |
APP-B, AD α-synuclein, PD |
• ↑ TTBK1 levels in ALS post-mortem motor cortex [25] • ↑ TTBK1 in post-mortem FTLD-TDP/FTLD-tau brains [22] • ↑ TTBK1 in rNLS8 TDP-43 mouse model [143] • ↑ TTBK1 RNA in post-mortem FTLD-TDP-43 cerebellum [193] • TTBK1 co-localize with pTDP-43 in ALS spinal cord aggregates [15] • ↑TTBK1 in FTLD post-mortem frontal cortex [15] |
|
| TTBK2 | Tau Tubulin Kinase 2 | Q6IQ55 | S409, S410 [15] | [15] | [15, 22] | TDP-43 [14, 15] | • ↑ TTBK2 in FTLD-TDP/FTLD-tau brains [22] |
Abbreviations: AD Alzheimer’s Disease, PD Parkinson’s Disease, ALS Amyotrophic Lateral Sclerosis, sALS sporadic ALS
Protein Phosphatase 1 (PP1), Protein Phosphatase 2 (PP2A) and Protein Phosphatase 2B (PP2B), also known as calcineurin, have been identified as TDP-43 phosphatases, although few studies have investigated the role of these phosphatases in TDP-43 pathology (Table 3). Understanding the driving forces behind TDP-43 phosphorylation, and possible dephosphorylation, is key to understanding pathology progression.
Table 3.
Reported TDP-43 phosphatases
| Kinase | Description | Accession | pTDP-43 sites | In vitro phosphatase assay | TDP-43 studies | Other neurodegenerative substrates | Expression and activity in primary TDP-43 proteinopathies | Expression and activity in other neurodegenerative diseases |
|---|---|---|---|---|---|---|---|---|
| PP1 | Protein phosphatase 1 |
P62136 (PPP1CA) P62140 (PPP1CB) P36873 (PPP1CC) |
S379, S403, S404, S409, S410 [254] | N/A | [254] |
Tau [292] TDP-43 [254] |
• ↓ PP2A activity in AD brain [293, 294] | |
| PP2A | Protein phosphatase 2 A |
Structural subunit A P30153 (PPP2R1A) P30154 (PPP2R1B) Regulatory subunit B P63151 (PPP2R2A) Q00005 (PPP2R2B) Q9Y2 T4 (PPP2R2C) P56211 (PPP2R2D) Q06190 (PPP2R3 A) Q9Y5P8 (PPP2R3B) Q9 JK24 (PPP2R3C) Q15257 (PPP2R4) Q15172 (PPP2R5A) Q15173 (PPP2R5B) Q13362 (PPP2R5C) Q14738 (PPP2R5D) Q16537 (PPP2R5E) Catalytic subunit C P67775 (PPP2CA) P62714 (PPP2CB) |
N/A |
• ↓ PP2A activity in AD brain [293, 294] • ↓ PP2A mRNA in AD hippocampus [303] • ↓ PP2A expression and activity in frontal and temporal cortices in AD brain [304] |
||||
| PP2B | Protein phosphatases 2B | Q08209 (PPP3CA) P16298 (PPP3CB) P48454 (PPP3CC) P63098 (PPP3R1) Q63811 (PPP3R2) | S409, S410 [122] | [122] | [122] |
TDP-43 [122] |
• ↓ activity in sporadic and familial ALS [260, 261] • ↓ PPP3CA and PP3R1 in FTD and rNLS8 TDP-43 mouse models [143, 193] |
• ↓ PP2B activity in AD brain [293, 294, 307, 308] • ↑ PP2B activity in AD brain [309] |
Abbreviations: AD Alzheimer’s Disease, PD Parkinson’s Disease, ALS Amyotrophic Lateral Sclerosis, sALS sporadic ALS
Putative TDP-43 kinases
Tyrosine-protein kinase ABL1 (c-Abl)
c-Abl is a tyrosine kinase involved in several cellular stress pathways [145], activated by various triggers including oxidative stress, hyperglycaemia, and DNA damage, to drive a signal cascade leading to cell death through apoptosis [146–148]. Increased c-Abl expression has been found in postmortem spinal cord tissue from sporadic ALS cases [149, 150]. Inhibiting c-Abl has shown promising therapeutic effects in iPSC derived motor neurons from ALS patients with SOD1 mutations, TDP-43 mutations, or sporadic ALS, as well as in a SOD1G93A transgenic ALS mouse model [150, 151]. A recent study employing an in vitro kinase assay demonstrated that c-Abl can phosphorylate TDP-43 at tyrosine 43 (Y43), and a direct interaction was supported by co-immunoprecipitation experiments in SH-SY5Y cells [29]. Mimicking phosphorylation at Y43 (Y43E) promoted TDP-43 mislocalisation and stress granule formation in SH-SY5Y cells, and TDP-43 mislocalisation, insolubility, aggregation and neuronal death in primary cortical neurons [29]. However, it should be noted that TDP-43 Y43 phosphorylation has not be detected in post-mortem ALS or FTLD-TDP tissues to date. Notably, c-Abl is the only tyrosine kinase, as opposed to serine/threonine (Ser/Thr) kinases, reported to be able to phosphorylate TDP-43, although evidence for TDP-43 tyrosine phosphorylation in human disease pathology samples remains unclear.
Cell division cycle 7-related protein kinase (CDC7)
CDC7 is a highly conserved Ser/Thr kinase involved in crucial cellular processes such as cell cycle regulation, DNA replication, and DNA repair [152, 153]. Although CDC7 is known for its role in the cell cycle, including regulation by the zinc-finger activator DBF4 [153–158], the function of CDC7 in non-proliferating neurons is not well understood. However, CDC7 was indicated as a TDP-43 kinase through an RNA interference kinome screen in C. elegans based on effects on TDP-43-associated behavioural phenotypes [14]. In vitro kinase assays with wildtype and mutant (M337 V) TDP-43 also showed robust phosphorylation at S409/410 by CDC7, indicating a direct interaction [14, 15]. Inhibition of CDC7 has been observed to decrease, but not eliminate, TDP-43 phosphorylation in a variety of models, including SH-SY5Y cells, ALS and FTLD-TDP immortalized lymphocytes, NSC-34 cells, TDP-43M337V C. elegans, and TDP-43A315T mice [14, 26, 27].
Casein kinase 1 (CK1)
CK1 is a family of Ser/Thr kinases of seven isoforms (α, β, δ, ϵ, γ1, γ2, and γ3) involved in many pathways, including circadian rhythm, vesicular trafficking, cell cycle progression, DNA repair, and signal transduction pathways [159–165]. CK1 α, δ, and ϵ localise to the cytoplasm and nucleus while CK1γ, due to C-terminal palmitoylation, is anchored to the plasma membrane [166]. CK1 was identified as a TDP-43 kinase through an in vitro kinase assay and has since been found to phosphorylate TDP-43 at 29 sites, including S403/404 and S409/410 [11, 167]. CK1 is also implicated in other neurodegenerative disorders, including Alzheimer’s disease and Parkinson’s disease, as it can phosphorylate APP-β [168], tau [169–171], and α-synuclein [171, 172]. Enhanced CK1 expression has also been observed in ALS, FTLD-TDP, and Alzheimer’s disease [20, 24, 142, 144]. TDP-43 itself has been shown to regulate CK1δ and CK1ε expression [20, 173], indicating a complex interplay between CK1 and TDP-43 in disease contexts. Inducible oligomerisation of TDP-43 can enhance CSNK1D (CK1δ gene) and CSNK1E (CK1ε gene) expression in SH-SY5Y cells [173]. Furthermore, enhanced UV crosslinking and immunoprecipitation (eCLIP) of the frontal cortex of sporadic ALS patients found that TDP-43 binds CSNK1E mRNA [20]. In addition, TDP-43 knockdown decreased CSNK1E but not CSNK1D mRNA levels in motor neuron progenitors [20], suggesting that CK1ϵ may be of particular importance in ALS. A recent study highlighted CK1δ and CK1ε as major TDP-43 kinases at S409/410 by comparing the effects of seven small molecule kinase inhibitors on TDP-43 pathology in a SH-SY5Y neuroblastoma cell model [173]. However, this study leaves open the possibility that several kinases drive pathological TDP-43 phosphorylation, since inhibition of these kinases individually decreased but did not eliminate TDP-43 phosphorylation [14, 15, 173]. A recent study explored the effects of CK1ε inhibition in a cytoplasmic TDP-43 mouse model, suggesting that therapeutic inhibition of CK1ε can reduce TDP-43 phosphorylation, lower neurofilament light chain levels, and improve survival [174].
Casein kinase 2 (CK2)
CK2 is a tetrameric Ser/Thr kinase known for its multifaceted roles in cellular processes, ranging from apoptosis and cell survival to RNA and protein synthesis, with over 300 substrates [124, 175]. CK2 comprises two catalytic subunits (α and/or α’) and two regulatory subunits (β), and unlike other kinases is constitutively active [124, 175–177]. CK2 was identified as a TDP-43 kinase alongside CK1 through an in vitro kinase assay with wildtype TDP-43 [11]. To date, no study has comprehensively elucidated all CK2 phosphorylation sites on TDP-43, but probing with phospho-specific antibodies has revealed phosphorylation at S379, S403/404, and S409/410 [11]. Like CK1, CK2 can also phosphorylate APP-β [168], α-synuclein [172, 178–181], and tau [182], suggesting a broad involvement in neurodegenerative diseases.
Inhibitor of nuclear factor kappa-B kinase subunit beta (IKKβ)
IKKβ is a catalytic subunit of IκB kinase (IKK) alongside catalytic IKKα and regulatory IKKγ subunits (reviewed in [183]), controlling inflammation and other immune responses through regulation of NF-κB. A recent study demonstrated that overexpression of IKKβ, but not IKKα or IKKγ, significantly increases NF-kB activity and promotes the proteasomal degradation of cytoplasmic TDP-43 in Neuro2a cells [35]. Using LC–MS/MS analysis, it was revealed that overexpression of IKKβ induces TDP-43 phosphorylation at threonine 8 (T8), serine 92 (S92) and serine 180 (S180), and an in vitro kinase assay demonstrated that IKKβ directly phosphorylates TDP-43 at S92 [35]. Overexpression of IKKβ also decreased TDP-43 aggregation in the hippocampus of a TDP-433A2S mouse model, induced phosphorylation at S92, and decreased neuronal damage. This study suggests that IKKβ plays a role in phosphorylating TDP-43, and also in promoting TDP-43 degradation.
Mitogen-activated protein protein kinase 1 (MEK1)
MEK1, also known as MAP2 K1, is a key kinase in the MAPK/ERK extracellular signalling pathway, which regulates proteome stability, proliferation, differentiation, survival, cell cycle, and apoptosis [184–186]. The potential role of MEK as a TDP-43 kinase was first suggested by Li et al. [32], observing that MEK inhibition prevented TDP-43 phosphorylation at T153/Y155 in response to heat shock in HEK293 and SH-SY5Y cells. Heat shock, a known cellular stressor, can induce TDP-43 phosphorylation, with emerging evidence that heat shock proteins are part of a stress-responsive protective mechanism in disease [143, 187, 188], although the direct relevance of heat shock to neurodegeneration is debatable. Interestingly, overexpression of MEK1 induced TDP-43 phosphorylation in SH-SY5Y cells even in the absence of heat shock [32]. Further, inhibition of ERK, a downstream target of MEK1, did not prevent TDP-43 phosphorylation, suggesting that the downstream MAPK/ERK pathway does not necessarily influence phosphorylation. While these findings hint at a regulatory relationship, the absence of direct evidence from in vitro kinase assays leaves a direct interaction between MEK1 and TDP-43 unexplored. Further research is required to confirm MEK1 as a TDP-43 kinase and to clarify the functional significance of T153/Y155 residue phosphorylation, which is not commonly observed in disease.
Mitogen-activated protein kinase 14 (p38α/MAPK14)
MAPK14, also known as p38α MAPK, is a ubiquitously expressed and highly conserved Ser/Thr kinase in the MAPK family, which plays a role in various cellular processes such as transcription, differentiation, mRNA stability, cell cycle regulation, inflammation, and stress response pathways [189]. MAPK14, along with closely related MAPK11, MAPK12, and MAPK13, is activated by proinflammatory cytokines and other environmental stresses like oxidative stress, mediated by MAPK kinase kinases (MKKs) or autophosphorylation [190]. MAPK14 was first linked to TDP-43 phosphorylation via demonstration that MAPK14 knockdown or pharmacological inhibition decreased phosphorylation of TDP-43M337V at S409/410 in SH-SY5Y cells [56]. Furthermore, expression of MAPK14 with a constitutively activate mutation, but not the wildtype variant, induced TDP-43 phosphorylation and enhanced aggregation and mislocalisation in SH-SY5Y cells. This suggests that MAPK14 may require extracellular signalling or stress conditions to be activated to phosphorylate TDP-43. However, this effect could be indirect due to impaired global nucleocytoplasmic transport function by MAPK14 manipulation. Co-immunoprecipitation experiments in SH-SY5Y cells showed a direct interaction between TDP-43 and MAPK14, suggesting that MAPK14 can directly phosphorylate TDP-43 [56]. Further research is needed to clarify the potential involvement of other regulators of MAPK14 relating to TDP-43 phosphorylation.
Tau-tubulin kinase 1 and 2 (TTBK1, TTBK2)
TTBK1 and TTBK2 are multifunctional Ser/Thr kinases involved in various cellular processes, including microtubule dynamics and neuronal development, with their name stemming from their affinity for microtubules and characterisation as tau kinases [191, 192]. Interestingly, TTBK1 and TTBK2 are the closest evolutionary relative of CK1 and are highly homologous to each other [160]. TTBK2 is ubiquitously expressed, while TTBK1 is neuron specific [191]. TTBK1 and TTBK2 were identified as TDP-43 kinases alongside CDC7 in a RNA interference kinome screen [14]. While TTBK1 and TTBK2 did not phosphorylate TDP-43 during an in vitro kinase assay, a subsequent study demonstrated that they can phosphorylate TDP-43 under conditions of optimised magnesium concentration [15]. A recent in vitro kinase assay using a truncated active form of TTBK1 also indicated that TTBK1 can phosphorylate TDP-43 [25]. Notably, TTBK1 levels are elevated and TTBK1 co-localizes with phosphorylated TDP-43 in ALS and FTLD-TDP post-mortem tissue, and also in a cytoplasmic TDP-43 mouse model [15, 22, 25, 143, 193], and TTBK2 was also elevated in the FTLD-TDP brain [22]. Despite these findings, the specific roles of TTBK1 and TTBK2 and the precise TDP-43 phosphorylation sites targeting by these kinases remain poorly characterised.
Physiological pathways of putative TDP-43 kinases
The reported TDP-43 kinases are involved in many key signalling pathways, including circadian rhythm, Wnt, ERK, NF-κB, p38, microtubule dynamics, and the cell cycle (Fig. 5). These pathways often overlap, creating a complex network that regulate cellular homeostasis, inflammation and cell division. Dysregulation of many of these pathways has been implicated in the pathogenesis of TDP-43 proteinopathies, leading to the overexpression of these kinases, which could potentially be a driving force behind aberrant TDP-43 phosphorylation. While targeting these kinases to modulate TDP-43 phosphorylation may appear to be a promising therapeutic strategy, significant challenges remain. The promiscuity of these kinases and interconnected nature of the pathways means that inhibiting one kinase could have unintended off-target downstream effects. Therefore, while kinase regulation of TDP-43 may be important in neurodegeneration, careful consideration must be given to the broader impact of therapeutic interventions targeting these kinases. Here, we will explore the known biology of the putative TDP-43 kinases focused on biological pathways that may be of relevance to consider as off-target pathways when designing therapeutic interventions to modify TDP-43 phosphorylation.
Fig. 5.
Physiological cellular pathways of putative TDP-43 kinases. Schematic of eight key biological pathways that involve c-Abl, CDC7, CK1, CK2, IKKβ, MAPK14, MEK1, TTBK1 and/or TTBK2. These pathways include 1) circadian rhythm, 2) Wnt pathway, 3) ERK pathway, 4) NF-κB pathway, 5) p38 pathway, 6), microtubule dynamics, 7) PI3K/AKT/mTOR signalling, and 8) cell cycle. Figure constructed using biorender.com
Circadian rhythm
CK1δ and CK1ε play key roles in circadian rhythm, which is an autonomous daily oscillation that maintains body homeostasis and plays important roles in metabolic regulation and memory consolidation. This rhythm is orchestrated by the phosphorylation of PERIOD (PER) by CK1δ and CK1ε, which leads to PER degradation and facilitates nuclear localisation, thereby modulating the length of the circadian period [194, 195]. Of note, circadian rhythm dysfunction has been identified in various neurodegenerative disorders including ALS, Alzheimer’s disease, Parkinson’s disease, Huntington’s disease, and multiple sclerosis (reviewed in [196]). In ALS SOD1G93A transgenic mice, circadian rhythm dysfunction accelerated disease onset and progression through enhanced motor neuron loss, activated gliosis, and NF-κB inflammation [197]. Similar abnormalities are observed in FUS ALS mouse models, preceding cognitive impairment onset [198]. Whether these effects are related to the regulation of TDP-43 phosphorylation by CK1δ and CK1ε remains to be explored.
Wnt pathway
CK1α is involved in the Wnt pathway, which is integral to embryonic development and adult tissue homeostasis. It is involved in both canonical (β-catenin dependent) and non-canonical (β-catenin independent) signalling pathways, modulating various cellular processes [199–201]. Abnormal Wnt signalling has been implicated in ALS, with elevated expression of Wnt ligands, receptors, and co-receptors in ALS spinal cord tissue [202–204]. This suggests Wnt dysfunction which may contribute to disease progression.
ERK pathway
MEK1 kinase is involved in the extracellular signal-regulation kinase (ERK) pathway, a subset of the mitogen-activated protein kinase (MAPK) pathway, which plays a role in cell adhesion, differentiation, proliferation, and apoptosis. This pathway is activated by a series of upstream signals, including mitogens and growth factors, leading to the activation of MEK1/2 (reviewed in [205]). MEK1/2 subsequently phosphorylates and activates ERK1/2, which translocates to the nucleus where it promotes cell proliferation, growth, survival, and cytokines production. Additionally, ERK1/2 phosphorylates PARP- 1, enhancing NF-κB activity through the activation of the IκB kinase (IKK) complex. In ALS, ERK1/2 activation has been associated with disease progression, where its inhibition has been shown to provide protective effects (reviewed in [206]). ERK1/2 signalling plays a role in oligodendrocyte myelination, with emerging evidence highlighting the involvement of oligodendrocyte dysfunction in ALS [207–210]. Collectively, these findings suggest that the activation of MEK1 through the ERK pathway, through its involvement in TDP-43 phosphorylation, neuronal signalling, and oligodendrocyte function, may represent a contributing mechanism underlying ALS pathology and a potential target for therapeutic intervention. Further investigation is required into the upstream pathway of MEK1 activation and how this influences TDP-43 phosphorylation.
NF-κB inflammation
Putative TDP-43 kinase IKKβ is involved in the NF-κB pathway, which is one of the most significant inflammatory pathways associated with TDP-43 pathology. The canonical NF-κB pathway is activated in response to various stimuli, leading to the formation of the IKK complex, composed of catalytic subunits IKKβ, and IKKα, and the regulatory subunit IKKγ, also known as NF-κB essential modulator (NEMO) (reviewed in [211]). This complex phosphorylates Inhibitor of κB (IκB), causing IκB degradation and the release of NF-κB. The free NF-κB translocates to the nucleus to initiate the transcription of genes involved in inflammation, innate immunity, and cell survival (reviewed in [212]). Activation of NF-κB can exacerbate neurodegenerative processes by promoting neuroinflammation [213, 214], and NF-κB mRNA and protein levels are elevated in ALS patient spinal cords, suggesting activation of the NF-kB pathway [215, 216]. TDP-43 itself can regulate NF-κB pathways in both neurons and microglia [215, 217, 218]. Interestingly, neuron inhibition of NF-κB through expression of a super repressor form of IκBα in transgenic TDP-43A315T or TDP-43G348C mice decreased cytoplasmic TDP-43 mislocalisation, improved motor performance and cognition, and reduced motor neuron and gliosis loss [219]. Furthermore, chronic administration of LPS to activate the NF-κB pathway in TDP-43A315T mice exacerbated cytoplasmic TDP-43 accumulation and aggregation [215]. These studies suggest that the NF-κB pathway worsens TDP-43 pathology and may play an important role in regulating disease pathology, potentially involving the TDP-43 kinase IKKβ. Understanding this pathway is important to more fully define the role of neuroinflammation in TDP-43 proteinopathies.
p38 pathway
The TDP-43 kinase MAPK14 is involved in the p38 pathway, which is another type of mitogen-activated protein kinase (MAPK) pathway that promotes inflammation, proliferation, senescence, RNA splicing, apoptosis and differentiation (reviewed in [220]). The pathway is activated by external signals including pro-inflammatory cytokines, heat shock, and UV radiation, or internal signals such as oxidative stress [221–224]. A protein cascade causes phosphorylation and activation of p38 MAPK kinases, including MAPK14, which allows entry to the nucleus. Nuclear MAPK14 inhibits NF-κB activity, promotes several transcription factors to make transcriptional changes, and the p38 pathway has been implicated in ALS pathology, particularly with SOD1 and FUS mutations (reviewed in [205]).
Microtubule dynamics
Putative TDP-43 kinases CK1, TTBK1, and TTBK2 play a role in microtubule dynamics [225–228]. Microtubules are intracellular structures vital for neuron development and maintenance. MTs facilitate axonal transport which is required for mitochondrial recycling, vesicle and mRNA transport, and signalling pathways [229]. Microtubules are particularly important for neurons as they play a role in neurite remodelling, generation of neuronal compartments, and growth cone mechanics [230–232]. Mutations to TUBA4A, a microtubules protein, cause a rare familial form of ALS, highlighting the importance of microtubules for neuron survivability. Additionally, TDP-43 interacts with microtubules for mRNP granule transport, which is vital for proper mRNA localisation and translation in neurons [59, 233]. Disruptions in microtubules dynamics can impair neuronal function and contribute to the pathogenesis of ALS, highlighting the need for further research into the mechanisms regulating MT stability and transport in neurons.
PI3 K/AKT/mTOR signalling pathway
The putative TDP-43 kinase CK2 is involved in the PI3 K/AKT/mTOR pathway, which is an intracellular signalling process important for cellular growth, proliferation, metabolism, and apoptosis. This pathway is activated by upstream cytokines or growth factors, such as fibroblast growth factor (FGF) and platelet-derived growth factor (PDGF), activating PI3K (reviewed in [234]). Once activated, PI3K phosphorylates and activates Protein Kinase B (AKT), leading to several downstream effects, including the activation of mammalian target of rapamycin (mTOR) [234, 235]. Activated mTOR controls macroautophagy, involved in the clearance of many cellular proteins. CK2 plays a pivotal role in this process by regulating AKT activity [236, 237]. In addition to directly phosphorylating AKT, CK2 phosphorylates the phosphatase PTEN to prevent the inhibition of AKT [236, 238, 239]. Overactivation of this pathway has been linked with several cancers, causing abnormal cell growth, proliferation, migration, and chemotherapy resistance [240, 241], suggesting that therapeutic targeting may have unintended consequences in the neurodegenerative disease context.
Cell cycle
Several reported TDP-43 kinases, including CDC7, CK1, MAPK14, MEK1, and IKKβ, play crucial roles in regulation of the cell cycle, particularly in response to cellular stress [228, 242]. While neurons are non-proliferating cells, evidence suggests that neurons can re-enter the cell cycle, which promotes apoptosis [243]. Aberrant neuronal cell cycle re-entry has been highlighted as a major cause of neuronal loss in Alzheimer’s disease [244–246] and ALS [247, 248]. Cell cycle-related abnormalities in ALS include hyperphosphorylation of retinoblastoma protein pRb, increased cyclin D levels, and cytoplasmic redistribution of transcription factor E2F-1 in motor neurons and glia in sporadic ALS post-mortem tissue [247]. Additionally, the cell cycle checkpoint tumor suppressor protein p53 is elevated in motor neurons in the spinal cord but not in the motor cortex in ALS postmortem tissue, further implicating cell cycle dysfuction in ALS pathology [248]. Therefore, further investigations are required to understand the role of the cell cycle in TDP-43 neurodegenerative disorders, and whether this process activates/upregulates TDP-43 kinases to regulate its phosphorylation.
TDP-43 phosphatases
Protein phosphatase 1 (PP1)
PP1 is a class of multimeric Ser/Thr phosphatases responsible for a major portion of eukaryotic protein dephosphorylation [249]. This includes regulation of excitatory synaptic activity, glycogen metabolism, cell progression, cell division, apoptosis, protein synthesis, mitosis, and RNA splicing [250–252]. PP1 consists of a catalytic subunit (PPP1CA, PPP1CB, PPP1CC) and at least one regulatory subunit which confers selectivity, localisation and regulation [253]. Although the catalytic subunits have a similar sequence, the regulatory subunits are diverse and identified by their function. PP1 was found to interact with TDP-43 by co-immunoprecipitation in HEK293 cells [254]. Furthermore, overexpression of PP1α or PP1γ reduced TDP-43 phosphorylation in HEK293 cells, suggesting PP1 is important for TDP-43 dephosphorylation [254]. Notably, while Gu et al. [254] demonstrated that overexpression of wildtype TDP-43 in HEK293T cells is sufficient to detect phosphorylated TDP-43, other HEK293T [25], SH-SY5Y [18], and Drosophila [16] studies did not detect phosphorylation from simply overexpressing TDP-43. This difference could be due to variations in transfection protocols, such as the type of DNA delivery method or the amount of plasmid DNA used, as well as differences in stress conditions during cell culturing, which could influence the cells' response to TDP-43 overexpression. Interestingly, while PPP1 CA is downregulated in ALS/FTD frontal cortical post-mortem tissue [255], PPP1CB and PPP1CC are upregulated in FTD frontal and temporal cortex post-mortem tissue [193].
Protein phosphatase 2 A (PP2A)
PP2A is another class of multimeric Ser/Thr phosphatase that plays a pivotal role in regulating cellular phosphorylation events. While PP2A is ubiquitously expressed, it is most abundant in the heart and brain, with an estimate that it accounts for 71% total phosphatase activity in the human brain [140, 256]. PP2A coimmunoprecipitated with TDP-43 in HEK293 cells, suggesting a direct interaction with TDP-43 [254]. However, no in vitro assays have been performed to investigate whether PP2A is able to dephosphorylate TDP-43 directly.
Protein phosphatase 2B (PP2B)
PP2B, also known as calcineurin, is a conserved heterodimeric calcium/calmodulin dependent Ser/Thr phosphatase important in cellular signalling and stress responses. PP2B consists of two subunits: one of three calcineurin A (CnA) isozymes, a calmodulin-binding catalytic subunit (PPP3CA, PPP3CB, PPP3CC), and one of two calcineurin B (CnB) isozymes (PPP3R1, PPP3R2), a Ca2+-binding regulatory subunit [257]. PP2B plays an important role in postsynaptic structures of central synapses and synaptic endocytosis, and is activated by intracellular Ca2+ concentrations ([258], reviewed in [259]). An in vitro dephosphorylation assay demonstrated that PP2B can dephosphorylate TDP-43 [254]. Additionally, a yeast two-hybrid screen identified PPP3CC as a protein interactor of TDP-43WT, TDP-43A315T, and TDP-43M337V [122]. In disease, PP2B has lower activity in ALS brain and spinal cord tissue [260, 261]. Downregulation of PPP3CA and PPP3R1 has been observed in post-mortem FTD-TDP temporal cortex and in the cortex of the rNLS8 cytoplasmic TDP-43 mouse model [143, 193]. Moreover, PP2B co-localises with TDP-43 aggregates in ALS and FTD post-mortem tissue, suggesting involvement in TDP-43 pathology [122].
TDP-43 phosphorylation: pathology-driving or protective?
The literature on TDP-43 phosphorylation presents contrasting perspectives on whether it acts as a pathology-driving force, a protective mechanism, or both. The following sections will explore key aspects, including the timing of TDP-43 phosphorylation in disease progression and its roles in mislocalisation, aggregation, and neurotoxicity. Additionally, this discussion will compare studies on TDP-43 phosphorylation, highlighting major findings and models for kinase/phosphatase manipulation (Table 4) and phosphomimicry techniques (Table 5).
Table 4.
Effects of altering kinases or phosphatase levels on TDP-43 phosphorylation in different model system
| Approach | Model | Aggregation | Localisation | Neurotoxicity | Other | Reference |
|---|---|---|---|---|---|---|
| In vitro | ||||||
| ↑ kinase | SH-SY5Y | → c-Abl overexpression ↑ cytoplasmic TDP-43 accumulation | → c-Abl overexpression ↑ cytoplasmic TDP-43 | NR | NR | Lee et al. 2022 [29] |
| ↑ kinase | Cultured cortical neurons | NR | → c-Abl overexpression ↑ cytoplasmic TDP-43 | NR | NR | Lee et al. 2022 [29] |
| ↑ kinase | HEK293 cells | → TTBK1 overexpression ↑ insoluble TDP-43 | → TTBK1 overexpression ↑ cytoplasmic TDP-43 | - TTBK1 overexpression does not impact cell death (nuclei count) | NR | Tian et al. 2021 [25] |
| ↑ kinase | SH-SY5Y | → Hyperactive CK1δ ↑ aggregated TDP-43 and ↓ TDP-43 solubility | → Hyperactive CK1δ ↑ cytoplasmic TDP-43 |
→ Hyperactive CK1δ ↓ CFTR exon 9 skipping → Hyperactive CK1δ ↓ HDAC6 mRNA levels |
Nonaka et al. 2016 [18] | |
| ↑ kinase | Yeast | → Hyperactive CK1δ ↑ TDP-43 inclusions | → Hyperactive CK1δ ↑ cytoplasmic TDP-43 | → Hyperactive CK1δ ↑ toxicity | NR | Nonaka et al. 2016 [18] |
| ↑ kinase | Recombinant protein | ← CK1δ ↑ TDP-43 solubility | NR | NR | ← CK1δ ↓ phase separation | Gruijs da Silva et al. 2022 [34] |
| ↑ kinase | SH-SY5Y | NR | → TTBK2 overexpression → cytoplasmic phosphorylated TDP-43 | NR | NR | Liachko et al. 2014 [15] |
| ↑ kinase | Recombinant protein | → CK1δ ↑ oligomerisation | NR | NR | NR | Hasegawa et al. 2008 [11] |
| ↑ kinase | Recombinant protein | → TTBK1 ↑ formation of high molecular TDP-43 species (rescued by TTBK1 inhibition) | NR | NR | NR | Tian et al. 2021 [25] |
| ↑ kinase | iPSC-derived motor neurons | → CK1ε overexpression ↑ aggregation | NR | NR | NR | Krach et al. 2018 [20] |
| ↑ kinase | SH-SY5Y | NR | NR | → ↑ cytotoxicity with incubation with CK1-treated oligomerised TDP-43 compared to non-treated | NR | Choksi et al. 2014 [16] |
| ↑ kinase | HEK293T, Neuro2a | ← CK2α overexpression ↓ insoluble C-terminal TDP-43 fragment (ND251, ND207) | NR | NR | NR | Li et al. 2011 [31] |
| ↑ kinase | Neuro2a | ← IKKβ overexpression ↓ aggregation | NR | ← IKKβ overexpression ↓ toxicity of TDP-43K181E/A321V | NR | Iguchi et al. 2024 [35] |
| ↓ kinase | FTLD immortalised lymphocytes | NR | → CK1δ inhibition ↓ cytoplasmic and ↑ nuclear TDP-43 | → CK1δ partially reverted enhanced proliferation | Alquezar et al. 2016 [19] | |
| ↓ kinase | SH-SH5Y | NR | → CK1δ inhibition ↓ mislocalisation | → CK1δ inhibition ↑ cell survival from ethacrynic acid | Alquezar et al. 2016 [19] | |
| ↓ kinase | SH-SY5Y | → MAPK14 inhibition ↓ aggregation of TDP-43M337V | → MAPK14 inhibition ↓ mislocalisation of TDP-43M337 V | → MAPK14 inhibition or knockdown ↑ survival of TDP-43M337V | Aikio et al. 2025 [56] | |
| ↓ kinase | HEK293T | NR | NR | ← CK1α or CK1δ knockdown, but not TTBK1 or TTBK2, reduced TDP-43WT overexpression cytotoxicity | NR | Deng et al. 2021 [28] |
| ↓ kinase | sALS immortalised lymphoblasts | → CK1δ inhibition ↓ cytoplasmic TDP-43 | Martinez-Gonzalez et al. 2020 [24] | |||
| ↓ kinase | N2a | → TTBK1 knockdown ↓ insoluble TDP-43 and ↓ high molecular TDP-43 species | Tian et al. 2021 [25] | |||
| ↓ kinase | Cultured cortical neurons from c-Abl WT or knockout mice | NR | NR | – no accumulation of insoluble TDP-43 in c-Abl KO | NR | Lee et al. 2022 [29] |
| ↓ kinase | iPSC neurons | NR | NR | → TTBK1 knockdown ↓ TDP-43 overexpression-induced neurite and neuron loss | NR | Tian et al. 2021 [25] |
| ↓ kinase | NSC-34 |
→ CK1 inhibition ↓ aggregation induced by ER stress (tunicamycin) - CK1 inhibition does not influence TDP-43 solubility |
NR | - CK1 inhibition does not influence cell viability from ER stress | NR | Hicks et al. 2020 [123] |
| ↓ kinase | SH-SY5Y | NR | → TTBK1 inhibition ↓ cytoplasmic TDP-43 induced by ethacrynic acid | → TTBK1 inhibition ↓ cell death from ethacrynic acid | NR | Nozal et al. 2022 [30] |
| ↓ kinase | sALS lymphoblasts | NR | → TTBK1 inhibition ↓ cytoplasmic and ↑ nuclear TDP-43 | NR | NR | Nozal et al. 2022 [30] |
| ↓ kinase | ALS immortalised lymphocytes | NR | → CK1δ inhibition ↓ cytoplasmic and ↑ nuclear TDP-43 | NR | NR | Posa et al. 2019 [23] |
| ↓ kinase | SH-SY5Y | NR | → CDC7 inhibition ↓ mislocalisation from ethacrynic acid | → CDC7 inhibition ↓ cell death from ethacrynic acid | NR | Rojas-Prats et al. 2021 [26] |
| ↓ kinase | sALS lymphoblasts | NR | → CDC7 inhibition ↓ cytoplasmic and ↑ nuclear TDP-43 | NR | NR | Vaca et al. 2021 [27] |
| ↓ kinase | FTLD-TDP lymphoblasts (GRN mutation) | NR | → CDC7 inhibition ↓ cytoplasmic and ↑ nuclear TDP-43 | NR | → CDC7 inhibition restored CDK6 mRNA levels | Vaca et al. 2021 [27] |
| In vivo | ||||||
| ↑ kinase | C. elegans | NR | NR | → CDC7 overexpression with M337V or WT TDP-43 ↑ neuron loss |
→ CDC7 and M337V or WT TDP-43 caused paralysis and other severe effects → CDC7 overexpression is synthetic lethal with M337V but not with addition phospho-ablated mutations at S409/410 |
Liachko et al. 2013 [14] |
| ↓ kinase | A315T TDP-43 mouse | NR | NR | → CK1δ inhibition reduced motor neuron loss in spinal cord |
→ CK1δ inhibition significantly delayed weight loss → CK1δ inhibition blocked elevated microglial cells and reduced astrocytes |
Martinez-Gonzalez et al. 2020 [24] |
| ↑ kinase | C. elegans |
→ TTBK1 overexpression ↑ TDP-43 accumulation - TTBK2 overexpression does not influence TDP-43 accumulation |
NR | - TTBK1 overexpression does not influence lifespan |
→ TTBK1 overexpression ↓ locomotion - TTBK2 overexpression does not influence locomotion |
Taylor et al. 2018 [22] |
| ↑ kinase | Drosophila | ← CK2α overexpression ↓ aggregation | NR | NR | NR | Li et al. 2011 [31] |
| ↑ kinase | Drosophila | NR | NR |
→ DBT (CK1ε homolog) enhances TDP-43Q331K toxicity - DBT (CK1ε homolog) no influence on TDP-43WT or TDP-43M337V |
→ DBT (CK1ε homolog) induces TDP-43 fragmentation | Choksi et al. 2014 [16] |
| ↓ kinase | Recombinant protein and simulation approaches |
- C-terminal phosphomimic (2PM, 4PM) TDP-43 LLPS displays biphasic dependence on salt concentration - 4PM forms smaller liquid droplets |
NR | NR | NR | Haider et al. 2024 [128] |
| ↓ kinase | TDP-43A315T mice | NR | NR | → TTBK1 inhibition ↓ motor neuron loss in ventral horn | NR | Nozal et al. 2022 [30] |
| ↓ kinase | TDP-43A315T mice | NR | NR | NR | → CDC7 inhibition ↓ clasping score and ↑ time in rotarod | Rojas-Prats et al. 2021 [26] |
| ↓ kinase | C. elegans | NR | NR | → CDC7 null mutant or inhibition ↓ neuron loss with M337V TDP-43 | → CDC7 knockdown improved motor defects in M337V model | Liachko et al. 2013 [14] |
| ↓ kinase | Drosophila | NR | NR | → CK1δ inhibition ↑ lifespan | Salado et al. 2014 [17] | |
| ↓ kinase | C. elegans | NR | NR | NR | ← Phospho-ablation at S409/410 rescued locomotion deficit, reduced paralysis, and decreased coiling from TDP-43G290A or TDP-43M337V expression | Liachko et al. 2010 [310] |
| ↑ kinase | Mouse | NR | NR | ← IKKβ overexpression ↓ toxicity in TDP-43 cKO model (↓ cleaved caspase 3-positive neurons) | NR | Iguchi et al. 2024 [35] |
| ↓ phosphatase | C. elegans | → PP2B knockout ↑ TDP-43 accumulation | NR | → PP2B knockout exasperated loss of D-type GABAergic neurons of WT and A315T TDP-43 | ← PP2B knockout causes dystrophic neurites, axonal defasciculating and axon degeneration | Liachko et al. 2016 [122] |
Symbols: protective (backward arrow), causative (forward arrow), or neutral (line)
pTDP-43 phosphorylated TDP-43, ICH intracranial haemorrhage, sALS sporadic ALS, NR not reported
Table 5.
Mimicking or preventing TDP-43 phosphorylation in different model system
| Mimic/ablated sites | Model | Aggregation | Localisation | Neurotoxicity | Other | Reference |
|---|---|---|---|---|---|---|
| In vitro | ||||||
| S48 | HEK293 | ← S48E disrupts TDP-43 LLPS and oligomerisation | NR | NR | NR | Wang et al. 2018 [33] |
| 379, 403, 404, 409, 410 | HEK293, Neuro2a | ← 5SD ↓ aggregation and ↑ solubility, 5SA ↑ aggregation and ↓ solubility of C-terminal TDP-43 fragment | NR | NR | NR | Li et al. 2011 [31] |
| S48 | Recombinant protein | S48E disrupts TDP-43 LLPS and oligomerisation | NR | NR | NR | Wang et al. 2018 [33] |
| T88, S91, S92 | Recombinant protein | → Phosphomimic at T88/S91/S92 ↓ affinity for importin α1/β | NR | NR | Doll et al. 2022 [62] | |
| S373, S375, S379, S387, S389, S393, S395, S403, S404, S407, S409, S410 | Recombinant protein |
← CK1δ and 2A, 5A, and 12A condensates have aggregate-like morphology ← 2D, 5D, and 12D condensates are more dynamic and ↓ aggregation |
NR | NR | - 12D and 12 A does not impair RNA regulation | Gruijs da Silva et al. 2022 [34] |
| S373, S375, S379, S387, S389, S393, S395, S403, S404, S407, S409, S410 | HeLa | ← 12SD ↑solubility | - 12SD and 12SA no change in localisation or nuclear import rate | NR | - 12SD and 12SA does not impact TDP-43 autoregulating its own mRNA or splicing regulation | Gruijs da Silva et al. 2022 [34] |
| S373, S375, S379, S387, S389, S393, S395, S403, S404, S407, S409, S410 | U2OS | NR | - 12SD and 12SA no change in localisation | NR | - 12SD and 12SA does not impact TDP-43 autoregulating its own mRNA | Gruijs da Silva et al. 2022 [34] |
| S373, S375, S379, S387, S389, S393, S395, S403, S404, S407, S409, S410 | Primary neurons | ← 12SD ↓ insoluble TDP-43 | ← 12SD ↑ TDP-43 dispersal | NR | - 12SD suppresses stress granule recruitment | Gruijs da Silva et al. 2022 [34] |
| T153, Y155 | HeLa | ← pT153/Y155 increases TDP-43 solubility from heat shock | - pTDP-43 at T153/Y155 recruited to nucleoli | NR | ← pT153/Y155 reduces TDP-43 regulation of splicing by 30% compared to WT and T153E/Y155 A | Li et al. 2017[32] |
| T153, Y155 | SH-SY5Y | - pT153/Y155 did not influence aggregation from heat shock | NR | NR | NR | Li et al. 2017[32] |
| Y43 | SH-SY5Y | NR | NR | NR | ← Y43E ↑ G3BP1-positive stress granules | Lee et al. 2022[29] |
| Y43 | Primary cortical neurons | NR | → Y43E ↑ TDP-43 cytoplasmic localisation | NR | NR | Lee et al. 2022[29] |
| Y43 | Cultured cortical neurons from c-Abl WT or knockout mice | → Y43E ↓ solubility in c-Abl WT or K/O | NR | → Y43E ↑ neuronal cell death in c-Abl K/O model | NR | Lee et al. 2022[29] |
| S409, S410 | Cultured neurons | NR | NR | → S409/410A ↓ neuronal injury from OxyHb treatment | NR | Sun et al. 2018[21] |
| in vivo | ||||||
| S409, S410 | C. elegans | NR | NR | - 2SA with M337V TDP-43 and PP2B knockout did not alter neurodegeneration | - 2SA with M337V TDP-43 and PP2B knockout does not cause locomotion dysfunction | Liachko et al. 2016 [122] |
| 379, 403, 404, 409, 410 | Drosophila | ← 5SE ↓ aggregates and ↑ solubility | NR | NR | NR | Li et al. 2011 [31] |
| S4109, 410 | IHC rats | NR | → S409A/S410A ↓ cytoplasmic mislocalisation | → S409A/S410A ↓autophagy | NR | Sun et al. 2018[21] |
Symbols: protective (backward arrow), causative (forward arrow), or neutral (line)
pTDP-43 phosphorylated TDP-43, ICH intracranial haemorrhage, sALS sporadic ALS, NR not reported
Physiological TDP-43 phosphorylation
Although TDP-43 phosphorylation is strongly associated with pathological processes, some evidence suggests it may also serve a physiological role in TDP-43 function, localisation, and degradation. While phosphorylation is linked to cytoplasmic mislocalization of TDP-43 in disease, physiological TDP-43 also undergoes regulated shuttling between the nucleus and cytoplasm, indicating a potential role for phosphorylation in this dynamic process. Recent studies have identified IKKβ as a kinase capable of phosphorylating TDP-43 at residues T8, S92, S180, and S183 in HEK293T cells [35]. IKKβ overexpression reduced cytoplasmic TDP-43 and facilitated degradation of TDP-433A2S in Neuro2a cells [35]. Specifically, phosphorylation at S92 appears important for TDP-43 degradation, as the phospho-mimic S92D variant degraded significantly faster than control in Neuro2a cells, despite no changes in nuclear-cytoplasmic localization. Additionally, TDP-43 phosphorylation has been observed during cellular stress and in models expressing aggregation-prone or cytoplasm-driven exogenous TDP-43 in HEK293T cells, further supporting its role as a modulator of TDP-43 stability and stress response [96]. These findings highlight the complex interplay between TDP-43 phosphorylation, degradation, and localisation in both physiological contexts and highlights the necessity of exploring all TDP-43 phosphorylation sites.
Timing of phosphorylation
The timing of TDP-43 phosphorylation across the disease course is an understudied area. Emerging evidence suggests TDP-43 phosphorylation is likely not an initial mislocalisation or aggregation-inducing event but rather is triggered by ongoing pathological processes. Li et al. [31] measured a significant increase in phosphorylated TDP-43 over 48 h by expressing an aggregate-prone TDP-43 C-terminal fragment called ND251 in Neuro2a cells. Notably, this study also reported that non-phosphorylated aggregates were primarily small puncta, suggesting phosphorylation occurs after aggregation initiation and maturation. However, it is also possible that phosphorylation-specific TDP-43 antibodies have limited sensitivity, detecting phosphorylated TDP-43 only within dense aggregates. Mann et al. [262] developed a model to spatiotemporally induce TDP-43 oligomerisation in HEK293 cells by expressing TDP-43 tagged with cryptochrome 2 (CRY2), a region that undergoes reversible homo-oligomerisation when exposed to blue light. These ontogenetically induced inclusions were positive for phosphorylated TDP-43 after 4 h of continuous light, indicating that TDP-43 undergoes phosphorylation after aggregation. Another study used CRY2 optogenetics to cause multimerization of G3BP1 to induce stress granule formation in U2OS cells, showing that phosphorylated TDP-43 could be detected after 5 h of stimulated stress granule formation, demonstrating that TDP-43 recruited to stress granules becomes phosphorylated [263]. Ko et al. [173] induced TDP-43 aggregation through doxycycline-inducible expression of full length TDP-43 tagged with N50, an aggregation-inducing sequence, in SH-SY5Y and U2OS cells, inducing aggregates that were phosphorylated. Additionally, both CSNK1D and CSNK1E gene expression was upregulated in these models, suggesting cytoplasmic mislocalisation and/or aggregation triggers TDP-43 phosphorylation by upregulation of CK1δ and CK1ε. These three in vitro studies suggest that TDP-43 is phosphorylated in response to TDP-43 aggregation or stress granule recruitment [173, 262, 263]. This is supported by findings in the rNLS8 cytoplasmic TDP-43 (TDP-43∆NLS) doxycycline-inducible mouse model of ALS [264], in which TDP-43 phosphorylation is first detected in the cortex during early disease stages but after the accumulation of insoluble TDP-43 first begins. A study using Drosophila found that TDP-43 recruited to arsenite-induced or heat-induced foci were phosphorylated at S409/410 [86], but in contrast to the findings of Zhang et al. [263] where the inducement of stress granule formation through the optogenetic oligomerization of G3BP1 caused TDP-43 phosphorylation, phosphorylated TDP-43 was not detected from stress granule recruitment, highlighting how different techniques and models can produce contrasting findings. Collectively, these studies suggest that while TDP-43 phosphorylation is an early event in disease and may occur prior to disease progression, it may be a secondary event to other pathological TDP-43 features such as mislocalisation and aggregation.
Mislocalisation
A prevailing question revolves around whether the pathological cytoplasmic accumulation of TDP-43 results from mechanisms that actively drive TDP-43 out of the nucleus or conversely, prevents nuclear re-entry during normal shuttling. Overexpression of the putative TDP-43 kinases c-Abl, CK1δ, CK1ε, TTBK1, and TTBK2 have been reported to drive TDP-43 mislocalisation in several in vitro models [15, 18, 25, 29]. Similarly, TDP-43 mislocalisation was decreased by CK1 or TTBK1 inhibition in Alzheimer’s disease patient-derived lymphoblasts, CK1 inhibition in ALS patient-derived lymphoblasts, CDC7 inhibition in ethacrynic acid treated SH-SY5Y cells, and CDC7 inhibition in FTD and ALS patient-derived lymphoblasts, [23, 24, 26, 27]. Manipulating kinases might show effects on C-terminal phosphorylation, but phosphorylation at other sites, such as within the NLS, could influence mislocalisation and remain undetected due to the lack of suitable phosphorylation-specific antibodies.
Phosphomimicry of recombinant TDP-43 at putative phosphorylation sites (T88, S91, S92) impaired the NLS region and reduced interaction with importin α1/β, suggesting an impaired ability to re-enter the nucleus [62]. This phenomenon is observed with other aggregate-prone proteins including FUS, of which phosphorylation triggered by DNA damage hinders binding to transportin 1 (TRN1), leading to cytoplasmic accumulation [265]. Gruijs da Silva [34] found that phosphomimic substitutions at 12 C-terminal sites did not affect TDP-43 localisation or nuclear import rate in HeLa cells. These studies suggest that phosphorylation within the NLS may play a more important role than C-terminal sites in influencing cytoplasmic accumulation of TDP-43. TDP-43 phosphorylation has also been implicated in re-localisation to other subcellular compartments, including phosphorylation at T153/Y155 which induces nucleoli recruitment, and phosphomimicry (G298D) at disease-associated mutation G298S which increased TDP-43 mitochondrial localisation [32, 63]. Overall, these studies suggest that TDP-43 phosphorylation impairs nuclear entry, driving mislocalisation to the cytoplasm, although this is not consistent between models and techniques. Intriguingly, this process may serve a protective purpose by sequestering misfolded or abnormal TDP-43 within the cytoplasm where it can undergo clearance mechanisms. Further studies investigating the subcellular localisation and timing of this phosphorylation in TDP-43 pathology are required to help understand whether TDP-43 phosphorylation is a protective mechanism or drives pathology.
LLPS and aggregation
Accumulating evidence suggests that TDP-43 phosphorylation plays a pivotal role in LLPS and aggregate formation. A recent investigation into the role of C-terminal phosphorylation on TDP-43 phase separation dynamics tested recombinant C-terminal phosphomimic variants with varying concentrations of NaCl [128]. The salt concentration plays a role is regulating recombinant protein stability, crystallization, and behaviour by altering the ionic strength of the solvent, where higher salt concentrations support protein stability. This study revealed that phosphorylation increases LLPS in the absence of NaCl and displays a diphasic dependence on salt concentrations wherein phosphorylation decreases LLPS at higher concentrations. Gruijs da Silva et al. [34] mimicked phosphorylation at 2, 5 or 12 pathological sites (Fig. 3) and found phosphorylation reduced LLPS and aggregation to generate more liquid-like and dynamic condensates. Both studies proposed mechanisms based on coarse-grained modelling, with Haider et al. [128] concluding that the electrostatic change of phosphorylation modulates the intermolecular hydrophobic interactions that drive LLPS and Gruijs da Silva et al. [34] suggesting phosphorylation forms more protein-solvent interactions instead of protein–protein interactions.
Several studies have concluded that TDP-43 phosphorylation enhances the propensity of TDP-43 to aggregate. Phosphorylated TDP-43 induced by CK1δ or CK1ε overexpression correlated with TDP-43 aggregation in an in vitro kinase assay [11], in SH-SY5Y cells [18], and in iPSC-derived motor neurons [20]. TTBK1 overexpression decreased TDP-43 solubility in HEK293 cells, suggesting increased aggregation [25]. Additionally, CK1δ inhibition in ER-stressed NSC- 34 cells decreased TDP-43 phosphorylation and aggregation [123]. TTBK1 knockdown or inhibition decreased the abundance of high molecular TDP-43 species in Neuro2a cells [25]. Further, MAPK14 inhibition decreased aggregation in SH-SY5Y cells [56]. Inhibition of TDP-43 phosphatase PP2B increased phosphorylated TDP-43 and aggregation in HEK293 cells [122]. Similarly, PP2B knockout in C. elegans displayed increased TDP-43 aggregation and worse motor control phenotypes [122]. Overall, these studies suggest that TDP-43 phosphorylation exacerbates TDP-43 aggregation, which can be mitigated by decreasing phosphorylation. However, none of these studies show a direct link between phosphorylation and aggregation, since the observed outcomes could potentially be influenced by off-target effects of kinase/phosphatase manipulation.
Conversely, other studies suggest TDP-43 phosphorylation can decrease aggregation. Mimicking phosphorylation at S409/410 (2SD) reduced aggregation and enhanced solubility compared to wildtype TDP-43 in HEK293 cells [266]. Similarity, 5SD (S379/S403/S404/S409/S410D) reduced aggregation and enhanced solubility in TDP-43 C-terminal fragment HEK293T, Neuro2a, and Drosophila models and in in vitro aggregation assay [31, 34]. Preventing phosphorylation at these sites (5SA) enhanced aggregation in Neuro2a cells [31]. Additional C-terminal phosphomimicry (12SD, S373/S375/S379/S387/S389/S393/S395/S403/S404/S407/S409/S410D) in an in vitro aggregation assay had a greater influence on enhancing solubility than 5SD, suggesting additional phosphorylation increases TDP-43’s resistance to aggregation [34]. Overexpression of CK1δ in an in vitro aggregation assay decreased aggregation and CK2α overexpression enhanced the solubility of C-terminal fragmented TDP-43 in HEK293T and Neuro2a cells [31, 34]. Phosphorylation at other sites has also been found to play a role in TDP-43 aggregation and LLPS. Overexpression of IKKβ, a recently identified putative TDP-43 kinase that phosphorylates at T8, S92, S180, and S183, decreased aggregation of wildtype and 3 A2S TDP-43, an aggregate-prone NLS and RRM1 mutant, in Neuro2a cells [35]. Phosphomimicry at S48 disrupted TDP-43 LLPS and polymeric assembly to generate more dynamic assemblies in HEK293 cells [33]. This is consistent with Wang et al. [33] where S48 phosphomimicry of N-terminal recombinant TDP-43 impaired LLPS. Aikio et al. [56] found that phosphomimicry at S292, S409/410 or both enhanced LLPS of recombinant TDP-43. The role of TDP-43 phosphorylation in aggregation and LLPS is complex and context-dependent due to conflicting findings, various models and techniques, and multiple intermediate species. This highlights the need for further research to clarify these mechanisms and their implications for neurodegenerative diseases.
Neurotoxicity
TDP-43 phosphorylation may contribute to neuronal toxicity – defined as mechanisms that lead to cellular dysfunction and death-potentially by influencing TDP-43 mislocalisation and aggregation, as discussed above. However, this remains a topic of debate, with conclusions varying between studies based on different kinases and experimental models. For example, while TTBK1 overexpression enhanced TDP-43 accumulation and decreased locomotion of TDP-43WT overexpressing C. elegans, there were no changes to lifespan [22]. Tian et al. [25] found comparable results in HEK293 cells, where TTBK1 overexpression decreased TDP-43 solubility and enhanced cytoplasmic mislocalisation without influencing cell death. However, this study also reported that TTBK1 knockdown rescued neurite shortening and neuron loss in TDP-43WT overexpressing iPSC neurons and extended the lifespan of TDP-43WT Drosophila. This is consistent with findings of Nozal et al. [30] whereby TTBK1 inhibition prevented cell death induced by ethacrynic acid in SH-SY5Y cells and ameliorated motor neuron loss in the ventral horn in TDP-43A315T mice.
Similar to the effects of TTBK1, CK1 overexpression also enhances, and inhibition ameliorates, TDP-43-mediated toxicity in model systems. Choksi et al. [16] found that SH-SY5Y cell death was enhanced by incubation with oligomerised TDP-43 treated by CK1. Furthermore, overexpression of the CK1ε homolog Doubletime (DBT) in Drosophila enhanced toxicity of TDP-43Q331K, but not TDP-43WT or TDP-43M337V. Nonaka et al. [18] demonstrated that expression of a hyperactive truncated CK1δ variant in yeast increased toxicity. Another study found that inhibition of CK1δ in SH-SY5Y cells decreased toxicity from ethacrynic acid [19]. A different approach found that knockdown of CK1α or CK1δ in TDP-43 overexpressed HEK293 cells prevented cytotoxicity [28]. In a TDP-43A315T mouse model, inhibiting CK1δ prevented motor neuron loss in the spinal cord in addition to delaying weight loss and decreasing neuroinflammation as demonstrated by elevated microglial cells and astrocytes [24].
Liachko et al. [14] showed that the overexpression of TDP-43WT or TDP-43M337V and CDC7 enhances neuron loss in C. elegans and causes behavioural defects. Additionally, CDC7 inhibition prevents neuron loss from TDP-43M337V expression in C. elegans. Another study also found that CDC7 inhibition decreased cell death from TDP-43 pathology induced through ethacrynic acid in SH-SY5Y cells [26]. A further study found that overexpression of IKKβ decreased toxicity of TDP-43K181E/A321V in Neuro2a cells and with TDP-433A2S AAV expression in a TDP-43 knockout mouse model [35]. In contrast, MAPK14 inhibition or knockdown enhanced the survival of SH-SY5Y cells expressing TDP-43M337V. Overall, the phosphorylation of TDP-43 appears to play a role in neuronal toxicity, with effects varying between different kinases and experimental models. These findings underscore the potential for kinase-targeted therapies in mitigating TDP-43-associated neurodegenerative diseases, although further research is needed to fully understand the mechanisms involved. It is also important to consider the off-target effects of kinase/phosphatase manipulation and develop strategies to modulate TDP-43 phosphorylation in a more highly specific manner.
Hypothesised role of TDP-43 phosphorylation
We propose that TDP-43 phosphorylation serves a physiological role in some contexts in promoting TDP-43 LLPS to facilitate cellular processes that rely on phase-separated compartments. However, under pathological conditions, such as cellular stress or other unknown trigger, the upregulation or activation of TDP-43 kinases may drive dramatically increased levels of phosphorylation. Furthermore, TDP-43 itself may regulate its own phosphorylation, as suggested by its binding and regulation of CSNK1E mRNA [20]. In disease, we hypothesize that phosphorylated TDP-43 becomes sequestered in liquid droplet structures, which transition in an irreversible manner to a solid-like state. This solid phase likely traps TDP-43 in a phosphorylated state, shielding it from phosphatases. The phosphorylated TDP-43 detected in post-mortem tissues may thus reflect the TDP-43 post-liquid droplet state. In addition to C-terminal phosphorylation and LLPS, it is likely other TDP-43 phosphorylation sites have different functions. For example, phosphorylation around the NLS has been linked with influencing interactions with importins and thus reducing nuclear entry [62]. Furthermore, phosphorylation at S92, a site phosphorylated by IKKβ, may play a role in TDP-43 degradation [35].
These hypotheses align with similar findings in other neurodegenerative diseases, for example α-synuclein [267, 268], FUS [269, 270], and tau [271] also experience an abnormal increase in phosphorylation in disease. These proteins, like TDP-43, can undergo LLPS [101, 272–274], transition from liquid to solid phases [100, 101], and phosphorylation has been linked with liquid droplet regulation [101, 272, 273, 275, 276]. CK1 has been implicated in the phosphorylation of these proteins, including α-synuclein [172], FUS [277], tau [169, 278], in addition to TDP-43 [11, 167]. The role of CK1 in regulating phosphorylation of multiple neurodegenerative proteins suggests it may represent a shared mechanism driving pathological phase transitions. Understanding the role and regulation of TDP-43 phosphorylation could provide valuable insights into the broader mechanisms of neurodegeneration and inform therapeutic approaches applicable across multiple neurodegenerative diseases.
Conclusion
The current literature on TDP-43 phosphorylation has developed using a variety of models and techniques, resulting in conflicting findings and interpretations that underscore the complexity of these processes in neurodegeneration. While TDP-43 phosphorylation is consistently observed in post-mortem ALS and FTLD-TDP tissue, the influence of TDP-43 phosphorylation on disease progression remains debated. Initially, phosphorylation was hypothesised to exacerbate pathology by promoting TDP-43 mislocalisation, aggregation, and cell death. However, emerging evidence suggests that phosphorylation may modulate LLPS to decrease TDP-43 aggregation and neurotoxicity, suggesting a protective role.
This review has examined the various techniques and models used to study TDP-43 phosphorylation, each with its own strengths and limitations. These methodological differences, along with the uncertainty about the timing of phosphorylation disease, complicate the ability to draw definitive conclusions. Furthermore, the possibility that TDP-43 mislocalisation and/or aggregation itself drives TDP-43 phosphorylation suggests that current approaches may not fully capture the complexity of the disease process. Given these challenges, there is a pressing need to develop new techniques and approaches to accurately assess the timing and consequences of phosphorylation at different TDP-43 sites. This includes developing a more thorough array of well-validated TDP-43 phosphorylation-specific antibodies, targeting sites such as S92 – which has been implicated in TDP-43 degradation – which will be crucial for understanding the role of pathological TDP-43 phosphorylation but may also reveal insights into the potential role of TDP-43 phosphorylation under basal conditions. The development of TDP-43 phosphorylation-specific nanobodies offers a promising method for real-time detection in live cells, helping to uncover the time and location where phosphorylated occurs. Furthermore, the impact of TDP-43 phosphorylation on interactions with other proteins remains largely unexplored. Identifying the phosphorylated TDP-43 proteome will provide valuable insights into its function consequences. Finally, identifying the full suite of TDP-43 kinases, deciphering their regulation mechanisms, and determining the specific sites they target are critical steps toward unravelling the upstream drivers of pathological phosphorylation. For example, it remains unclear whether disease-related alterations in levels of function of TDP-43 kinases has downstream effects on other target proteins which could concurrently affect disease mechanisms. Further research is crucial to understand the driving forces and consequences of TDP-43 phosphorylation and to identify therapeutic targets that can effectively regulate TDP-43 pathology while minimizing off-target effects, ultimately improving neuronal health in ALS and FTLD-TDP.
Acknowledgements
Figures 2–5 and Graphical abstract were created using Biorender.com.
Abbreviations
- AD
Alzheimer’s disease
- ALS
Amyotrophic lateral sclerosis
- FTD
Frontotemporal dementia
- HD
Huntington’s disease
- IDR
Intrinsically disordered region
- LCD
Low-complexity domain
- LLPS
Liquid–liquid phase separation
- NLS
Nuclear localation signal
- PD
Parkinson’s disease
- PTM
Post-translational modification
- RRM
RNA-recognition motif
Authors’ contributions
All authors conceived the ideas and concepts written in this review. E.A.K. conducted the literature search, drafted the manuscript, and created figures/tables. All authors drafted, reviewed, and approved the final manuscript.
Funding
This work was supported by MND Research Australia (Innovator Grant IG2343), the Ross Maclean Fellowship, Brazil Family Program for Neurology, and a FightMND Bill Guest Mid-Career Research Fellowship to A.K.W. A.T.B. was supported by a Race Against Dementia–Dementia Australia Research Foundation (DARF) Fellowship. E.A.K. was supported by a MNDRA PhD Scholarship Top-Up Grant.
Data availability
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Adekunle T. Bademosi, Email: a.bademosi@uq.edu.au
Adam K. Walker, Email: adam.walker@sydney.edu.au
References
- 1.Ling S-C, Polymenidou M, Cleveland DW. Converging Mechanisms in ALS and FTD: Disrupted RNA and Protein Homeostasis. Neuron. 2013;79(3):416–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nelson PT, Dickson DW, Trojanowski JQ, Jack CR, Boyle PA, Arfanakis K, et al. Limbic-predominant age-related TDP-43 encephalopathy (LATE): consensus working group report. Brain. 2019;142(6):1503–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Higashi S, Iseki E, Yamamoto R, Minegishi M, Hino H, Fujisawa K, et al. Concurrence of TDP-43, tau and α-synuclein pathology in brains of Alzheimer’s disease and dementia with Lewy bodies. Brain Res. 2007;1184:284–94. [DOI] [PubMed] [Google Scholar]
- 4.Nakashima-Yasuda H, Uryu K, Robinson J, Xie SX, Hurtig H, Duda JE, et al. Co-morbidity of TDP-43 proteinopathy in Lewy body related diseases. Acta Neuropathol. 2007;114(3):221–9. [DOI] [PubMed] [Google Scholar]
- 5.Josephs KA, Whitwell JL, Knopman DS, Hu WT, Stroh DA, Baker M, et al. Abnormal TDP-43 immunoreactivity in AD modifies clinicopathologic and radiologic phenotype. Neurol. 2008;70(19 Part 2):1850–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lin W-L, Dickson DW. Ultrastructural localization of TDP-43 in filamentous neuronal inclusions in various neurodegenerative diseases. Acta Neuropathol. 2008;116(2):205–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schwab C, Arai T, Hasegawa M, Yu S, McGeer PL. Colocalization of transactivation-responsive DNA-binding protein 43 and huntingtin in inclusions of Huntington disease. J Neuropathol Exp Neurol. 2008;67(12):1159–65. [DOI] [PubMed] [Google Scholar]
- 8.Arai T, Mackenzie IR, Hasegawa M, Nonoka T, Niizato K, Tsuchiya K, et al. Phosphorylated TDP-43 in Alzheimer’s disease and dementia with Lewy bodies. Acta Neuropathol. 2009;117(2):125–36. [DOI] [PubMed] [Google Scholar]
- 9.Nelson PT, Schmitt FA, Lin Y, Abner EL, Jicha GA, Patel E, et al. Hippocampal sclerosis in advanced age: clinical and pathological features. Brain. 2011;134(5):1506–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Josephs KA, Murray ME, Whitwell JL, Parisi JE, Petrucelli L, Jack CR, et al. Staging TDP-43 pathology in Alzheimer’s disease. Acta Neuropathol. 2014;127(3):441–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hasegawa M, Arai T, Nonaka T, Kametani F, Yoshida M, Hashizume Y, et al. Phosphorylated TDP-43 in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Annals of Neurology: Official Journal of the American Neurological Association and the Child Neurology Society. 2008;64(1):60–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Inukai Y, Nonaka T, Arai T, Yoshida M, Hashizume Y, Beach TG, et al. Abnormal phosphorylation of Ser409/410 of TDP-43 in FTLD-U and ALS. FEBS Lett. 2008;582(19):2899–904. [DOI] [PubMed] [Google Scholar]
- 13.Neumann M, Kwong LK, Lee EB, Kremmer E, Flatley A, Xu Y, et al. Phosphorylation of S409/410 of TDP-43 is a consistent feature in all sporadic and familial forms of TDP-43 proteinopathies. Acta Neuropathol. 2009;117(2):137–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liachko NF, McMillan PJ, Guthrie CR, Bird TD, Leverenz JB, Kraemer BC. CDC7 inhibition blocks pathological TDP-43 phosphorylation and neurodegeneration. Ann Neurol. 2013;74(1):39–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liachko NF, McMillan PJ, Strovas TJ, Loomis E, Greenup L, Murrell JR, et al. The tau tubulin kinases TTBK1/2 promote accumulation of pathological TDP-43. PLoS Genet. 2014;10(12): e1004803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Choksi DK, Roy B, Chatterjee S, Yusuff T, Bakhoum MF, Sengupta U, et al. TDP-43 Phosphorylation by casein kinase Iε promotes oligomerization and enhances toxicity in vivo. Hum Mol Genet. 2014;23(4):1025–35. [DOI] [PubMed] [Google Scholar]
- 17.Salado IG, Redondo M, Bello ML, Perez CN, Liachko NF, Kraemer BC, et al. Protein kinase CK-1 inhibitors as new potential drugs for amyotrophic lateral sclerosis. J Med Chem. 2014;57(6):2755–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nonaka T, Suzuki G, Tanaka Y, Kametani F, Hirai S, Okado H, et al. Phosphorylation of TAR DNA-binding protein of 43 kDa (TDP-43) by truncated casein kinase 1δ triggers mislocalization and accumulation of TDP-43. J Biol Chem. 2016;291(11):5473–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alquezar C, Salado IG, de la Encarnación A, Pérez DI, Moreno F, Gil C, et al. Targeting TDP-43 phosphorylation by Casein Kinase-1δ inhibitors: a novel strategy for the treatment of frontotemporal dementia. Mol Neurodegener. 2016;11(1):36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Krach F, Batra R, Wheeler EC, Vu AQ, Wang R, Hutt K, et al. Transcriptome–pathology correlation identifies interplay between TDP-43 and the expression of its kinase CK1E in sporadic ALS. Acta Neuropathol. 2018;136(3):405–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sun L, Zhang K, Zhai W, Li H, Shen H, Yu Z, et al. TAR DNA binding protein-43 loss of function induced by phosphorylation at S409/410 blocks autophagic flux and participates in secondary brain injury after intracerebral hemorrhage. Front Cell Neurosci. 2018;12:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Taylor LM, McMillan PJ, Liachko NF, Strovas TJ, Ghetti B, Bird TD, et al. Pathological phosphorylation of tau and TDP-43 by TTBK1 and TTBK2 drives neurodegeneration. Mol Neurodegener. 2018;13(1):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Posa D, Martínez-González L, Bartolomé F, Nagaraj S, Porras G, Martínez A, et al. Recapitulation of Pathological TDP-43 Features in Immortalized Lymphocytes from Sporadic ALS Patients. Mol Neurobiol. 2019;56(4):2424–32. [DOI] [PubMed] [Google Scholar]
- 24.Martínez-González L, Rodríguez-Cueto C, Cabezudo D, Bartolomé F, Andrés-Benito P, Ferrer I, et al. Motor neuron preservation and decrease of in vivo TDP-43 phosphorylation by protein CK-1δ kinase inhibitor treatment. Sci Rep. 2020;10(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tian Y, Wang Y, Jablonski AM, Hu Y, Sugam JA, Koglin M, et al. Tau-tubulin kinase 1 phosphorylates TDP-43 at disease-relevant sites and exacerbates TDP-43 pathology. Neurobiol Dis. 2021;161: 105548. [DOI] [PubMed] [Google Scholar]
- 26.Rojas-Prats E, Martinez-Gonzalez L, Gonzalo-Consuegra C, Liachko NF, Perez C, Ramírez D, et al. Targeting nuclear protein TDP-43 by cell division cycle kinase 7 inhibitors: A new therapeutic approach for amyotrophic lateral sclerosis. Eur J Med Chem. 2021;210: 112968. [DOI] [PubMed] [Google Scholar]
- 27.Vaca G, Martinez-Gonzalez L, Fernandez A, Rojas-Prats E, Porras G, Cuevas EP, et al. Therapeutic potential of novel Cell Division Cycle Kinase 7 inhibitors on TDP-43-related pathogenesis such as Frontotemporal Lobar Degeneration (FTLD) and amyotrophic lateral sclerosis (ALS). J Neurochem. 2021;156(3):379–90. [DOI] [PubMed] [Google Scholar]
- 28.Deng X, Sun X, Yue W, Duan Y, Hu R, Zhang K, et al. CHMP2B regulates TDP-43 phosphorylation and cytotoxicity independent of autophagy via CK1. J Cell Biol. 2021;221(1): e202103033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee S, Ryu HG, Kweon SH, Kim H, Park H, Lee K-H, et al. c-Abl Regulates the Pathological Deposition of TDP-43 via Tyrosine 43 Phosphorylation. Cells. 2022;11(24):3972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nozal V, Martínez-González L, Gomez-Almeria M, Gonzalo-Consuegra C, Santana P, Chaikuad A, et al. TDP-43 Modulation by Tau-Tubulin Kinase 1 Inhibitors: A New Avenue for Future Amyotrophic Lateral Sclerosis Therapy. J Med Chem. 2022;65(2). [DOI] [PubMed]
- 31.Li HY, Yeh PA, Chiu HC, Tang CY, Tu BPH. Hyperphosphorylation as a defense mechanism to reduce TDP-43 aggregation. PloS one. 2011;6(8):e23075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li W, Reeb AN, Lin B, Subramanian P, Fey EE, Knoverek CR, et al. Heat shock-induced phosphorylation of TAR DNA-binding protein 43 (TDP-43) by MAPK/ERK kinase regulates TDP-43 function. J Biol Chem. 2017;292(12):5089–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang A, Conicella AE, Schmidt HB, Martin EW, Rhoads SN, Reeb AN, et al. A single N-terminal phosphomimic disrupts TDP-43 polymerization, phase separation, and RNA splicing. EMBO J. 2018;37(5): e97452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gruijs da Silva LA, Simonetti F, Hutten S, Riemenschneider H, Sternburg EL, Pietrek LM, et al. Disease-linked TDP-43 hyperphosphorylation suppresses TDP-43 condensation and aggregation. The EMBO Journal. 2022;41(8):e108443. [DOI] [PMC free article] [PubMed]
- 35.Iguchi Y, Takahashi Y, Li J, Araki K, Amakusa Y, Kawakami Y, et al. IκB kinase phosphorylates cytoplasmic TDP-43 and promotes its proteasome degradation. J Cell Biol. 2024;223(2): e202302048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Keating SS, San Gil R, Swanson ME, Scotter EL, Walker AK. TDP-43 pathology: from noxious assembly to therapeutic removal. Progress in Neurobiology. 2022;211:102229. [DOI] [PubMed]
- 37.Ayala YM, De Conti L, Avendaño-Vázquez SE, Dhir A, Romano M, D’ambrogio A, et al. TDP-43 regulates its mRNA levels through a negative feedback loop. EMBO J. 2011;30(2):277–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kuo P-H, Chiang C-H, Wang Y-T, Doudeva LG, Yuan HS. The crystal structure of TDP-43 RRM1-DNA complex reveals the specific recognition for UG-and TG-rich nucleic acids. Nucleic Acids Res. 2014;42(7):4712–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lagier-Tourenne C, Polymenidou M, Cleveland DW. TDP-43 and FUS/TLS: emerging roles in RNA processing and neurodegeneration. Hum Mol Genet. 2010;19(R1):R46–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ma XR, Prudencio M, Koike Y, Vatsavayai SC, Kim G, Harbinski F, et al. TDP-43 represses cryptic exon inclusion in the FTD–ALS gene UNC13A. Nature. 2022;603(7899):124–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Melamed Ze, López-Erauskin J, Baughn MW, Zhang O, Drenner K, Sun Y, et al. Premature polyadenylation-mediated loss of stathmin-2 is a hallmark of TDP-43-dependent neurodegeneration. Nature neuroscience. 2019;22(2):180–90. [DOI] [PMC free article] [PubMed]
- 42.Klim JR, Williams LA, Limone F, Guerra San Juan I, Davis-Dusenbery BN, Mordes DA, et al. ALS-implicated protein TDP-43 sustains levels of STMN2, a mediator of motor neuron growth and repair. Nature neuroscience. 2019;22(2):167–79. [DOI] [PMC free article] [PubMed]
- 43.Brown A-L, Wilkins OG, Keuss MJ, Hill SE, Zanovello M, Lee WC, et al. TDP-43 loss and ALS-risk SNPs drive mis-splicing and depletion of UNC13A. Nature. 2022;603(7899):131–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bademosi AT, Walker AK. Cryptic inclusions UNCover losses driving neurodegeneration. Trends Genet. 2022;38(9):889–91. [DOI] [PubMed] [Google Scholar]
- 45.Sidibé H, Khalfallah Y, Xiao S, Gómez NB, Fakim H, Tank EM, et al. TDP-43 stabilizes G3BP1 mRNA: relevance to amyotrophic lateral sclerosis/frontotemporal dementia. Brain. 2021;144(11):3461–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sephton CF, Cenik C, Kucukural A, Dammer EB, Cenik B, Han Y, et al. Identification of Neuronal RNA Targets of TDP-43-containing Ribonucleoprotein Complexes*♦. J Biol Chem. 2011;286(2):1204–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dewey CM, Cenik B, Sephton CF, Dries DR, Mayer P III, Good SK, et al. TDP-43 is directed to stress granules by sorbitol, a novel physiological osmotic and oxidative stressor. Mol Cell Biol. 2011;31(5):1098–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cohen TJ, Hwang AW, Unger T, Trojanowski JQ, Lee VM. Redox signalling directly regulates TDP-43 via cysteine oxidation and disulphide cross-linking. EMBO J. 2012;31(5):1241–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Khalfallah Y, Kuta R, Grasmuck C, Prat A, Durham HD, Vande VC. TDP-43 regulation of stress granule dynamics in neurodegenerative disease-relevant cell types. Sci Rep. 2018;8(1):7551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Budini M, Buratti E, Morselli E, Criollo A. Autophagy and Its Impact on Neurodegenerative Diseases: New Roles for TDP-43 and C9orf72. Front Mol Neurosci. 2017;10:170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cohen TJ, Hwang AW, Restrepo CR, Yuan C-X, Trojanowski JQ, Lee VM. An acetylation switch controls TDP-43 function and aggregation propensity. Nat Commun. 2015;6(1):5845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cracco L, Doud EH, Hallinan GI, Garringer HJ, Jacobsen MH, Richardson R, et al. Distinguishing post-translational modifications in dominantly inherited FTD: FTLD-TDP Type A (GRN) versus Type B (C9orf72). Neuropathol Appl Neurobiol. 2022:e12836. [DOI] [PMC free article] [PubMed]
- 53.Burke CM, Walsh DJ, Mark KM, Deleault NR, Nishina KA, Agrimi U, et al. Cofactor and glycosylation preferences for in vitro prion conversion are predominantly determined by strain conformation. PLoS Pathog. 2020;16(4): e1008495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Aguilar-Calvo P, Xiao X, Bett C, Eraña H, Soldau K, Castilla J, et al. Post-translational modifications in PrP expand the conformational diversity of prions in vivo. Sci Rep. 2017;7(1):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Neumann M, Sampathu DM, Kwong LK, Truax AC, Micsenyi MC, Chou TT, et al. Ubiquitinated TDP-43 in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Science. 2006;314(5796):130–3. [DOI] [PubMed] [Google Scholar]
- 56.Aikio M, Odeh HM, Wobst HJ, Lee BL, Chan Ú, Mauna JC, et al. Opposing roles of p38α-mediated phosphorylation and PRMT1-mediated arginine methylation in driving TDP-43 proteinopathy. Cell Rep. 2025;44(1): 115205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Saunders CR, Rocha-Rangel PV, Desai R, Quadri Z, Liu H, Hunt Jr JB, et al. Citrullination of TDP-43 is a key post-translation modification associated with structural and functional changes and progressive pathology in TDP-43 mouse models and human proteinopathies. bioRxiv. 2025:2025.02. 28.639952.
- 58.Ayala YM, Zago P, D’Ambrogio A, Xu YF, Petrucelli L, Buratti E, et al. Structural determinants of the cellular localization and shuttling of TDP-43. J Cell Sci. 2008;121(Pt 22):3778–85. [DOI] [PubMed] [Google Scholar]
- 59.Alami NH, Smith RB, Carrasco MA, Williams LA, Winborn CS, Han SS, et al. Axonal transport of TDP-43 mRNA granules is impaired by ALS-causing mutations. Neuron. 2014;81(3):536–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chu J-F, Majumder P, Chatterjee B, Huang S-L, Shen C-KJ. TDP-43 regulates coupled dendritic mRNA transport-translation processes in co-operation with FMRP and Staufen1. Cell reports. 2019;29(10):3118–33. e6. [DOI] [PubMed]
- 61.Pinarbasi ES, Cağatay T, Fung HYJ, Li YC, Chook YM, Thomas PJ. Active nuclear import and passive nuclear export are the primary determinants of TDP-43 localization. Sci Rep. 2018;8(1):7083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Doll SG, Meshkin H, Bryer AJ, Li F, Ko Y-H, Lokareddy RK, et al. Recognition of the TDP-43 nuclear localization signal by importin α1/β. Cell Rep. 2022;39(13): 111007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wang W, Wang L, Lu J, Siedlak SL, Fujioka H, Liang J, et al. The inhibition of TDP-43 mitochondrial localization blocks its neuronal toxicity. Nat Med. 2016;22(8):869–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wang W, Li L, Lin W-L, Dickson DW, Petrucelli L, Zhang T, et al. The ALS disease-associated mutant TDP-43 impairs mitochondrial dynamics and function in motor neurons. Hum Mol Genet. 2013;22(23):4706–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wang W, Arakawa H, Wang L, Okolo O, Siedlak SL, Jiang Y, et al. Motor-coordinative and cognitive dysfunction caused by mutant TDP-43 could be reversed by inhibiting its mitochondrial localization. Mol Ther. 2017;25(1):127–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Buratti E, Baralle FE. The molecular links between TDP-43 dysfunction and neurodegeneration. Adv Genet. 2009;66:1–34. [DOI] [PubMed] [Google Scholar]
- 67.Abramson J, Adler J, Dunger J, Evans R, Green T, Pritzel A, et al. Accurate structure prediction of biomolecular interactions with AlphaFold 3. Nature. 2024;630. [DOI] [PMC free article] [PubMed]
- 68.Rezaei-Ghaleh N, Blackledge M, Zweckstetter M. Intrinsically disordered proteins: from sequence and conformational properties toward drug discovery. ChemBioChem. 2012;13(7):930–50. [DOI] [PubMed] [Google Scholar]
- 69.Sreedharan J, Blair IP, Tripathi VB, Hu X, Vance C, Rogelj B, et al. TDP-43 mutations in familial and sporadic amyotrophic lateral sclerosis. Science. 2008;319(5870):1668–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pesiridis GS, Lee VMY, Trojanowski JQ. Mutations in TDP-43 link glycine-rich domain functions to amyotrophic lateral sclerosis. Human Mole Gene. 2009;18(2):R156–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kabashi E, Valdmanis PN, Dion P, Spiegelman D, McConkey BJ, Velde CV, et al. TARDBP mutations in individuals with sporadic and familial amyotrophic lateral sclerosis. Nat Genet. 2008;40(5):572–4. [DOI] [PubMed] [Google Scholar]
- 72.Chang C-k, Wu T-H, Wu C-Y, Chiang M-h, Toh EK-W, Hsu Y-C, et al. The N-terminus of TDP-43 promotes its oligomerization and enhances DNA binding affinity. Biochemical and biophysical research communications. 2012;425(2):219–24. [DOI] [PubMed]
- 73.Sasaguri H, Chew J, Xu Y-F, Gendron TF, Garrett A, Lee CW, et al. The extreme N-terminus of TDP-43 mediates the cytoplasmic aggregation of TDP-43 and associated toxicity in vivo. Brain Res. 2016;1647:57–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Vivoli-Vega M, Guri P, Chiti F, Bemporad F. Insight into the folding and dimerization mechanisms of the N-terminal domain from human TDP-43. Int J Mol Sci. 2020;21(17):6259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kametani F, Obi T, Shishido T, Akatsu H, Murayama S, Saito Y, et al. Mass spectrometric analysis of accumulated TDP-43 in amyotrophic lateral sclerosis brains. Sci Rep. 2016;6(1):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Laferrière F, Maniecka Z, Pérez-Berlanga M, Hruska-Plochan M, Gilhespy L, Hock E-M, et al. TDP-43 extracted from frontotemporal lobar degeneration subject brains displays distinct aggregate assemblies and neurotoxic effects reflecting disease progression rates. Nat Neurosci. 2019;22(1):65–77. [DOI] [PubMed] [Google Scholar]
- 77.Neumann M, Frick P, Paron F, Kosten J, Buratti E, Mackenzie IR. Correction to: Antibody against TDP-43 phosphorylated at serine 369 suggests conformational differences of TDP-43 aggregates among FTLD-TDP subtypes. Acta Neuropathol. 2021;141(1):137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Burrell JR, Halliday GM, Kril JJ, Ittner LM, Götz J, Kiernan MC, et al. The frontotemporal dementia-motor neuron disease continuum. The Lancet. 2016;388(10047):919–31. [DOI] [PubMed] [Google Scholar]
- 79.Grad LI, Rouleau GA, Ravits J, Cashman NR. Clinical spectrum of amyotrophic lateral sclerosis (ALS). Cold Spring Harb Perspect Med. 2017;7(8): a024117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kim E-J, Sidhu M, Gaus SE, Huang EJ, Hof PR, Miller BL, et al. Selective frontoinsular von Economo neuron and fork cell loss in early behavioral variant frontotemporal dementia. Cereb Cortex. 2012;22(2):251–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Nana AL, Sidhu M, Gaus SE, Hwang JHL, Li L, Park Y, et al. Neurons selectively targeted in frontotemporal dementia reveal early stage TDP-43 pathobiology. Acta Neuropathol. 2019;137:27–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Arai T, Hasegawa M, Akiyama H, Ikeda K, Nonaka T, Mori H, et al. TDP-43 is a component of ubiquitin-positive tau-negative inclusions in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Biochem Biophys Res Commun. 2006;351(3):602–11. [DOI] [PubMed] [Google Scholar]
- 83.Pakravan D, Michiels E, Bratek-Skicki A, De Decker M, Van Lindt J, Alsteens D, et al. Liquid–liquid phase separation enhances TDP-43 LCD aggregation but delays seeded aggregation. Biomolecules. 2021;11(4):548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Gasset-Rosa F, Lu S, Yu H, Chen C, Melamed Ze, Guo L, et al. Cytoplasmic TDP-43 de-mixing independent of stress granules drives inhibition of nuclear import, loss of nuclear TDP-43, and cell death. Neuron. 2019;102(2):339–57 [DOI] [PMC free article] [PubMed]
- 85.Mann JR, Gleixner AM, Mauna JC, Gomes E, DeChellis-Marks MR, Needham PG, et al. RNA binding antagonizes neurotoxic phase transitions of TDP-43. Neuron. 2019;102(2):321–38. e8. [DOI] [PMC free article] [PubMed]
- 86.McGurk L, Gomes E, Guo L, Mojsilovic-Petrovic J, Tran V, Kalb RG, et al. Poly(ADP-Ribose) Prevents Pathological Phase Separation of TDP-43 by Promoting Liquid Demixing and Stress Granule Localization. Mol Cell. 2018;71(5):703-17.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Otte CG, Fortuna TR, Mann JR, Gleixner AM, Ramesh N, Pyles NJ, et al. Optogenetic TDP-43 nucleation induces persistent insoluble species and progressive motor dysfunction in vivo. Neurobiol Dis. 2020;146: 105078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ratti A, Gumina V, Lenzi P, Bossolasco P, Fulceri F, Volpe C, et al. Chronic stress induces formation of stress granules and pathological TDP-43 aggregates in human ALS fibroblasts and iPSC-motoneurons. Neurobiology of Disease. 2020;145. [DOI] [PubMed]
- 89.Yu H, Lu S, Gasior K, Singh D, Vazquez-Sanchez S, Tapia O, et al. HSP70 chaperones RNA-free TDP-43 into anisotropic intranuclear liquid spherical shells. Sci. 2021;371(6529):eabb4309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zhang P, Fan B, Yang P, Temirov J, Messing J, Kim HJ, et al. Chronic optogenetic induction of stress granules is cytotoxic and reveals the evolution of ALS-FTD pathology. Elife. 2019;8: e39578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Boeynaems S, Alberti S, Fawzi NL, Mittag T, Polymenidou M, Rousseau F, et al. Protein phase separation: a new phase in cell biology. Trends Cell Biol. 2018;28(6):420–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Nott TJ, Petsalaki E, Farber P, Jervis D, Fussner E, Plochowietz A, et al. Phase transition of a disordered nuage protein generates environmentally responsive membraneless organelles. Mol Cell. 2015;57(5):936–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Li H-R, Chiang W-C, Chou P-C, Wang W-J, Huang J-r. TAR DNA-binding protein 43 (TDP-43) liquid–liquid phase separation is mediated by just a few aromatic residues. Journal of Biological Chemistry. 2018;293(16):6090–8. [DOI] [PMC free article] [PubMed]
- 94.Conicella AE, Dignon GL, Zerze GH, Schmidt HB, D’Ordine AM, Kim YC, et al. TDP-43 α-helical structure tunes liquid-liquid phase separation and function. Proc Natl Acad Sci U S A. 2020;117(11):5883–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Shin Y, Brangwynne CP. Liquid phase condensation in cell physiology and disease. Science. 2017;357(6357):eaaf4382. [DOI] [PubMed]
- 96.Keating SS, Bademosi AT, San Gil R, Walker AK. Aggregation-prone TDP-43 sequesters and drives pathological transitions of free nuclear TDP-43. Cell Mol Life Sci. 2023;80(4):95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Owen I, Shewmaker F. The role of post-translational modifications in the phase transitions of intrinsically disordered proteins. Int J Mol Sci. 2019;20(21):5501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Molliex A, Temirov J, Lee J, Coughlin M, Kanagaraj AP, Kim HJ, et al. Phase separation by low complexity domains promotes stress granule assembly and drives pathological fibrillization. Cell. 2015;163(1):123–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Conicella AE, Zerze GH, Mittal J, Fawzi NL. ALS mutations disrupt phase separation mediated by α-helical structure in the TDP-43 low-complexity C-terminal domain. Structure. 2016;24(9):1537–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Patel A, Lee HO, Jawerth L, Maharana S, Jahnel M, Hein MY, et al. A liquid-to-solid phase transition of the ALS protein FUS accelerated by disease mutation. Cell. 2015;162(5):1066–77. [DOI] [PubMed] [Google Scholar]
- 101.Wegmann S, Eftekharzadeh B, Tepper K, Zoltowska KM, Bennett RE, Dujardin S, et al. Tau protein liquid–liquid phase separation can initiate tau aggregation. EMBO J. 2018;37(7): e98049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Nedelsky NB, Taylor JP. Bridging biophysics and neurology: aberrant phase transitions in neurodegenerative disease. Nat Rev Neurol. 2019;15(5):272–86. [DOI] [PubMed] [Google Scholar]
- 103.de Oliveira GA, Cordeiro Y, Silva JL, Vieira TC. Liquid-liquid phase transitions and amyloid aggregation in proteins related to cancer and neurodegenerative diseases. Adv Protein Chem Struct Biol. 2019;118:289–331. [DOI] [PubMed] [Google Scholar]
- 104.Lin Y, Protter DS, Rosen MK, Parker R. Formation and maturation of phase-separated liquid droplets by RNA-binding proteins. Mol Cell. 2015;60(2):208–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Seyfried NT, Gozal YM, Dammer EB, Xia Q, Duong DM, Cheng D, et al. Multiplex SILAC analysis of a cellular TDP-43 proteinopathy model reveals protein inclusions associated with SUMOylation and diverse polyubiquitin chains. Mol Cell Proteomics. 2010;9(4):705–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Johnson BS, Snead D, Lee JJ, McCaffery JM, Shorter J, Gitler AD. TDP-43 is intrinsically aggregation-prone, and amyotrophic lateral sclerosis-linked mutations accelerate aggregation and increase toxicity. J Biol Chem. 2009;284(30):20329–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Brangwynne CP, Eckmann CR, Courson DS, Rybarska A, Hoege C, Gharakhani J, et al. Germline P granules are liquid droplets that localize by controlled dissolution/condensation. Science. 2009;324(5935):1729–32. [DOI] [PubMed] [Google Scholar]
- 108.Erwin AL, Chang ML, Fernandez MG, Attili D, Russ JE, Sutanto R, et al. Molecular Visualization of Neuronal TDP43 Pathology In Situ. bioRxiv. 2024.
- 109.Polymenidou M, Lagier-Tourenne C, Hutt KR, Huelga SC, Moran J, Liang TY, et al. Long pre-mRNA depletion and RNA missplicing contribute to neuronal vulnerability from loss of TDP-43. Nat Neurosci. 2011;14(4):459–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Iguchi Y, Katsuno M, Niwa J-i, Takagi S, Ishigaki S, Ikenaka K, et al. Loss of TDP-43 causes age-dependent progressive motor neuron degeneration. Brain. 2013;136(5):1371–82. [DOI] [PubMed]
- 111.Štalekar M, Yin X, Rebolj K, Darovic S, Troakes C, Mayr M, et al. Proteomic analyses reveal that loss of TDP-43 affects RNA processing and intracellular transport. Neuroscience. 2015;293:157–70. [DOI] [PubMed] [Google Scholar]
- 112.Igaz LM, Kwong LK, Lee EB, Chen-Plotkin A, Swanson E, Unger T, et al. Dysregulation of the ALS-associated gene TDP-43 leads to neuronal death and degeneration in mice. J Clin Investig. 2011;121(2):726–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Amlie-Wolf A, Ryvkin P, Tong R, Dragomir I, Suh E, Xu Y, et al. Transcriptomic changes due to cytoplasmic TDP-43 expression reveal dysregulation of histone transcripts and nuclear chromatin. PLoS ONE. 2015;10(10): e0141836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Marks JD, Ayuso VE, Carlomagno Y, Yue M, Todd TW, Hao Y, et al. TMEM106B core deposition associates with TDP-43 pathology and is increased in risk SNP carriers for frontotemporal dementia. Science translational medicine. 2024;16(730):eadf9735. [DOI] [PMC free article] [PubMed]
- 115.Kennelly PJ, Potts M. Fancy meeting you here! A fresh look at" prokaryotic" protein phosphorylation. J Bacteriol. 1996;178(16):4759–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Dinkel H, Chica C, Via A, Gould CM, Jensen LJ, Gibson TJ, et al. Phospho. ELM: a database of phosphorylation sites—update 2011. Nucleic acids research. 2010;39(suppl_1):D261-D7. [DOI] [PMC free article] [PubMed]
- 117.Pandey AK, Ganguly HK, Sinha SK, Daniels KE, Yap GP, Patel S, et al. An inherent difference between serine and threonine phosphorylation: phosphothreonine strongly prefers a highly ordered, compact, cyclic conformation. ACS Chem Biol. 2023;18(9):1938–58. [DOI] [PubMed] [Google Scholar]
- 118.Dyson HJ. Expanding the proteome: disordered and alternatively folded proteins. Q Rev Biophys. 2011;44(4):467–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Iakoucheva LM, Radivojac P, Brown CJ, O’Connor TR, Sikes JG, Obradovic Z, et al. The importance of intrinsic disorder for protein phosphorylation. Nucleic Acids Res. 2004;32(3):1037–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Collins MO, Yu L, Campuzano I, Grant SG, Choudhary JS. Phosphoproteomic analysis of the mouse brain cytosol reveals a predominance of protein phosphorylation in regions of intrinsic sequence disorder. Mol Cell Proteomics. 2008;7(7):1331–48. [DOI] [PubMed] [Google Scholar]
- 121.Bah A, Forman-Kay JD. Modulation of intrinsically disordered protein function by post-translational modifications. J Biol Chem. 2016;291(13):6696–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Liachko NF, Saxton AD, McMillan PJ, Strovas TJ, Currey HN, Taylor LM, et al. The phosphatase calcineurin regulates pathological TDP-43 phosphorylation. Acta Neuropathol. 2016;132(4):545–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Hicks DA, Cross LL, Williamson R, Rattray M. Endoplasmic reticulum stress signalling induces casein kinase 1-dependent formation of cytosolic TDP-43 inclusions in motor neuron-like cells. Neurochem Res. 2020;45(6):1354–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Meggio F, Pinna LA. One-thousand-and-one substrates of protein kinase CK2? FASEB J. 2003;17(3):349–68. [DOI] [PubMed] [Google Scholar]
- 125.Bian Y, Ye M, Wang C, Cheng K, Song C, Dong M, et al. Global screening of CK2 kinase substrates by an integrated phosphoproteomics workflow. Sci Rep. 2013;3(1):3460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Kozeleková A, Náplavová A, Brom T, Gašparik N, Šimek J, Houser J, et al. Phosphorylated and Phosphomimicking Variants May Differ—A Case Study of 14-3-3 Protein. Front Chem. 2022;10: 835733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Paleologou KE, Schmid AW, Rospigliosi CC, Kim H-Y, Lamberto GR, Fredenburg RA, et al. Phosphorylation at Ser-129 but not the phosphomimics S129E/D inhibits the fibrillation of α-synuclein. J Biol Chem. 2008;283(24):16895–905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Haider R, Shipley B, Surewicz K, Hinczewski M, Surewicz WK. Pathological C-terminal phosphomimetic substitutions alter the mechanism of liquid-liquid phase separation of TDP-43 low complexity domain. bioRxiv. 2024. [DOI] [PMC free article] [PubMed]
- 129.Colombrita C, Zennaro E, Fallini C, Weber M, Sommacal A, Buratti E, et al. TDP-43 is recruited to stress granules in conditions of oxidative insult. J Neurochem. 2009;111(4):1051–61. [DOI] [PubMed] [Google Scholar]
- 130.Iguchi Y, Katsuno M, Takagi S, Ishigaki S, Niwa J-i, Hasegawa M, et al. Oxidative stress induced by glutathione depletion reproduces pathological modifications of TDP-43 linked to TDP-43 proteinopathies. Neurobiology of disease. 2012;45(3):862–70. [DOI] [PubMed]
- 131.Martínez-González L, Gonzalo-Consuegra C, Gómez-Almería M, Porras G, de Lago E, Martín-Requero Á, et al. Tideglusib, a non-ATP competitive inhibitor of GSK-3β as a drug candidate for the treatment of amyotrophic lateral sclerosis. Int J Mol Sci. 2021;22(16):8975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Kumar S, Phaneuf D, Cordeau P, Boutej H, Kriz J, Julien J-P. Induction of autophagy mitigates TDP-43 pathology and translational repression of neurofilament mRNAs in mouse models of ALS/FTD. Mol Neurodegener. 2021;16:1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Laurents DV. AlphaFold 2 and NMR spectroscopy: partners to understand protein structure, dynamics and function. Front Mol Biosci. 2022;9: 906437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Stefanoska K, Gajwani M, Tan ARP, Ahel HI, Asih PR, Volkerling A, et al. Alzheimer's disease: Ablating single master site abolishes tau hyperphosphorylation. Science Advances. 2022;8(27):eabl8809. [DOI] [PMC free article] [PubMed]
- 135.Hu JH, Zhang H, Wagey R, Krieger C, Pelech S. Protein kinase and protein phosphatase expression in amyotrophic lateral sclerosis spinal cord. J Neurochem. 2003;85(2):432–42. [DOI] [PubMed] [Google Scholar]
- 136.Vingtdeux V, Davies P, Dickson DW, Marambaud P. AMPK is abnormally activated in tangle-and pre-tangle-bearing neurons in Alzheimer’s disease and other tauopathies. Acta Neuropathol. 2011;121(3):337–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Liu Y-J, Lee L-M, Lai H-L, Chern Y. Aberrant activation of AMP-activated protein kinase contributes to the abnormal distribution of HuR in amyotrophic lateral sclerosis. FEBS Lett. 2015;589(4):432–9. [DOI] [PubMed] [Google Scholar]
- 138.Blalock EM, Geddes JW, Chen KC, Porter NM, Markesbery WR, Landfield PW. Incipient Alzheimer’s disease: microarray correlation analyses reveal major transcriptional and tumor suppressor responses. Proc Natl Acad Sci. 2004;101(7):2173–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Leroy K, Yilmaz Z, Brion JP. Increased level of active GSK-3β in Alzheimer’s disease and accumulation in argyrophilic grains and in neurones at different stages of neurofibrillary degeneration. Neuropathol Appl Neurobiol. 2007;33(1):43–55. [DOI] [PubMed] [Google Scholar]
- 140.Liu F, Grundke-Iqbal I, Iqbal K, Gong CX. Contributions of protein phosphatases PP1, PP2A, PP2B and PP5 to the regulation of tau phosphorylation. Eur J Neurosci. 2005;22(8):1942–50. [DOI] [PubMed] [Google Scholar]
- 141.Choi H-J, Cha SJ, Lee J-W, Kim H-J, Kim K. Recent advances on the role of gsk3β in the pathogenesis of amyotrophic lateral sclerosis. Brain Sci. 2020;10(10):675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Yasojima K, Kuret J, DeMaggio AJ, McGeer E, McGeer PL. Casein kinase 1 delta mRNA is upregulated in Alzheimer disease brain. Brain Res. 2000;865(1):116–20. [DOI] [PubMed] [Google Scholar]
- 143.San Gil R, Pascovici D, Venturato J, Brown-Wright H, Mehta P, Madrid San Martin L, et al. A transient protein folding response targets aggregation in the early phase of TDP-43-mediated disease. bioRxiv. 2023:2023.06. 21.546009. [DOI] [PMC free article] [PubMed]
- 144.Ghoshal N, Smiley JF, DeMaggio AJ, Hoekstra MF, Cochran EJ, Binder LI, et al. A new molecular link between the fibrillar and granulovacuolar lesions of Alzheimer’s disease. Am J Pathol. 1999;155(4):1163–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Siddiqui A, Tumiati M, Joko A, Sandholm J, Roering P, Aakko S, et al. Targeting dna homologous repair proficiency with concomitant topoisomerase ii and c-abl inhibition. Front Oncol. 2021;11: 733700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Sun X, Wu F, Datta R, Kharbanda S, Kufe D. Interaction between protein kinase C δ and the c-Abl tyrosine kinase in the cellular response to oxidative stress. J Biol Chem. 2000;275(11):7470–3. [DOI] [PubMed] [Google Scholar]
- 147.Sun X, Majumder P, Shioya H, Wu F, Kumar S, Weichselbaum R, et al. Activation of the cytoplasmic c-Abl tyrosine kinase by reactive oxygen species. J Biol Chem. 2000;275(23):17237–40. [DOI] [PubMed] [Google Scholar]
- 148.Gonfloni S, Maiani E, Di Bartolomeo C, Diederich M, Cesareni G. Oxidative stress, DNA damage, and c-Abl signaling: At the crossroad in neurodegenerative diseases? International journal of cell biology. 2012;2012(1): 683097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Jiang YM, Yamamoto M, Kobayashi Y, Yoshihara T, Liang Y, Terao S, et al. Gene expression profile of spinal motor neurons in sporadic amyotrophic lateral sclerosis. Ann Neurol. 2005;57(2):236–51. [DOI] [PubMed] [Google Scholar]
- 150.Katsumata R, Ishigaki S, Katsuno M, Kawai K, Sone J, Huang Z, et al. c-Abl inhibition delays motor neuron degeneration in the G93A mouse, an animal model of amyotrophic lateral sclerosis. 2012. [DOI] [PMC free article] [PubMed]
- 151.Imamura K, Izumi Y, Watanabe A, Tsukita K, Woltjen K, Yamamoto T, et al. The Src/c-Abl pathway is a potential therapeutic target in amyotrophic lateral sclerosis. Science Translational Medicine. 2017;9(391):eaaf3962. [DOI] [PubMed]
- 152.Kim JM, Yamada M, Masai H. Functions of mammalian Cdc7 kinase in initiation/monitoring of DNA replication and development. Mutat Res. 2003;532(1–2):29–40. [DOI] [PubMed] [Google Scholar]
- 153.Oshiro G, Owens JC, Shellman Y, Sclafani RA, Li JJ. Cell cycle control of Cdc7p kinase activity through regulation of Dbf4p stability. Mol Cell Biol. 1999;19(7):4888–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Jackson A, Pahl P, Harrison K, Rosamond J, Sclafani R. Cell cycle regulation of the yeast Cdc7 protein kinase by association with the Dbf4 protein. Mol Cell Biol. 1993;13(5):2899–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Weinreich M, Stillman B. Cdc7p–Dbf4p kinase binds to chromatin during S phase and is regulated by both the APC and the RAD53 checkpoint pathway. EMBO J. 1999;18(19):5334–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Montagnoli A, Bosotti R, Villa F, Rialland M, Brotherton D, Mercurio C, et al. Drf1, a novel regulatory subunit for human Cdc7 kinase. EMBO J. 2002;21(12):3171–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Dick SD, Federico S, Hughes SM, Pye VE, O’Reilly N, Cherepanov P. Structural Basis for the Activation and Target Site Specificity of CDC7 Kinase. Structure. 2020;28(8):954-62.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Ferreira MF, Santocanale C, Drury LS, Diffley JF. Dbf4p, an essential S phase-promoting factor, is targeted for degradation by the anaphase-promoting complex. Mol Cell Biol. 2000;20(1):242–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Knippschild U, Gocht A, Wolff S, Huber N, Löhler J, Stöter M. The casein kinase 1 family: participation in multiple cellular processes in eukaryotes. Cell Signal. 2005;17(6):675–89. [DOI] [PubMed] [Google Scholar]
- 160.Cheong JK, Virshup DM. Casein kinase 1: Complexity in the family. Int J Biochem Cell Biol. 2011;43(4):465–9. [DOI] [PubMed] [Google Scholar]
- 161.Schittek B, Sinnberg T. Biological functions of casein kinase 1 isoforms and putative roles in tumorigenesis. Mol Cancer. 2014;13(1):231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Rowles J, Slaughter C, Moomaw C, Hsu J, Cobb MH. Purification of casein kinase I and isolation of cDNAs encoding multiple casein kinase I-like enzymes. Proc Natl Acad Sci USA. 1991;88(21):9548–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Fish KJ, Cegielska A, Getman ME, Landes GM, Virshup DM. Isolation and Characterization of Human Casein Kinase I∊ (CKI), a Novel Member of the CKI Gene Family (∗). J Biol Chem. 1995;270(25):14875–83. [DOI] [PubMed] [Google Scholar]
- 164.Gross SD, Anderson RA. Casein Kinase I: Spatial Organization and Positioning of a Multifunctional Protein Kinase Family. Cell Signal. 1998;10(10):699–711. [DOI] [PubMed] [Google Scholar]
- 165.Zhai L, Graves PR, Robinson LC, Italiano M, Culbertson MR, Rowles J, et al. Casein kinase Iγ subfamily: Molecular cloning, expression, and characterization of three mammalian isoforms and complementation of defects in the Saccharomyces cerevisiae YCK genes. J Biol Chem. 1995;270(21):12717–24. [DOI] [PubMed] [Google Scholar]
- 166.Davidson G, Wu W, Shen J, Bilic J, Fenger U, Stannek P, et al. Casein kinase 1 γ couples Wnt receptor activation to cytoplasmic signal transduction. Nature. 2005;438(7069):867–72. [DOI] [PubMed] [Google Scholar]
- 167.Kametani F, Nonaka T, Suzuki T, Arai T, Dohmae N, Akiyama H, et al. Identification of casein kinase-1 phosphorylation sites on TDP-43. Biochem Biophys Res Commun. 2009;382(2):405–9. [DOI] [PubMed] [Google Scholar]
- 168.Walter J, Schindzielorz A, Hartung B, Haass C. Phosphorylation of the β-Amyloid precursor protein at the cell surface by ectocasein kinases 1 and 2. J Biol Chem. 2000;275(31):23523–9. [DOI] [PubMed] [Google Scholar]
- 169.Hanger DP, Byers HL, Wray S, Leung K-Y, Saxton MJ, Seereeram A, et al. Novel phosphorylation sites in tau from Alzheimer brain support a role for casein kinase 1 in disease pathogenesis. J Biol Chem. 2007;282(32):23645–54. [DOI] [PubMed] [Google Scholar]
- 170.Li G, Yin H, Kuret J. Casein kinase 1 delta phosphorylates tau and disrupts its binding to microtubules. J Biol Chem. 2004;279(16):15938–45. [DOI] [PubMed] [Google Scholar]
- 171.Schwab C, DeMaggio AJ, Ghoshal N, Binder LI, Kuret J, McGeer PL. Casein kinase 1 delta is associated with pathological accumulation of tau in several neurodegenerative diseases. Neurobiol Aging. 2000;21(4):503–10. [DOI] [PubMed] [Google Scholar]
- 172.Okochi M, Walter J, Koyama A, Nakajo S, Baba M, Iwatsubo T, et al. Constitutive phosphorylation of the Parkinson’s disease associated α-synuclein. J Biol Chem. 2000;275(1):390–7. [DOI] [PubMed] [Google Scholar]
- 173.Ko VI, Ong K, Cleveland DW, Yu H, Ravits JM. CK1δ/ε kinases regulate TDP-43 phosphorylation and are therapeutic targets for ALS-related TDP-43 hyperphosphorylation. Neurobiol Dis. 2024;196: 106516. [DOI] [PubMed] [Google Scholar]
- 174.Ko VI, Ong K, Kwon DY, Li X, Pietrasiewicz A, Harvey JS, et al. CK1δ/e-mediated TDP-43 phosphorylation contributes to early motor neuron disease toxicity in amyotrophic lateral sclerosis. 2024. [DOI] [PMC free article] [PubMed]
- 175.Litchfield DW. Protein kinase CK2: structure, regulation and role in cellular decisions of life and death. Biochemical Journal. 2003;369(1):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Ahmad KA, Wang G, Unger G, Slaton J, Ahmed K. Protein kinase CK2-a key suppressor of apoptosis. Adv Enzyme Regul. 2008;48:179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Sarno S, Ghisellini P, Pinna LA. Unique activation mechanism of protein kinase CK2. The N-terminal segment is essential for constitutive activity of the catalytic subunit but not of the holoenzyme. J Biol Chem. 2002;277(25):22509–14. [DOI] [PubMed]
- 178.Ishii A, Nonaka T, Taniguchi S, Saito T, Arai T, Mann D, et al. Casein kinase 2 is the major enzyme in brain that phosphorylates Ser129 of human α-synuclein: implication for α-synucleinopathies. FEBS Lett. 2007;581(24):4711–7. [DOI] [PubMed] [Google Scholar]
- 179.Lee G, Tanaka M, Park K, Lee SS, Kim YM, Junn E, et al. Casein kinase II-mediated phosphorylation regulates α-synuclein/synphilin-1 interaction and inclusion body formation. J Biol Chem. 2004;279(8):6834–9. [DOI] [PubMed] [Google Scholar]
- 180.Sano K, Iwasaki Y, Yamashita Y, Irie K, Hosokawa M, Satoh K, et al. Tyrosine 136 phosphorylation of α-synuclein aggregates in the Lewy body dementia brain: involvement of serine 129 phosphorylation by casein kinase 2. Acta Neuropathol Commun. 2021;9:1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Wu W, Sung CC, Yu P, Li J, Chung KK. S-Nitrosylation of G protein-coupled receptor kinase 6 and Casein kinase 2 alpha modulates their kinase activity toward alpha-synuclein phosphorylation in an animal model of Parkinson’s disease. PLoS ONE. 2020;15(4): e0232019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Greenwood JA, Scott CW, Spreen RC, Caputo CB, Johnson GV. Casein kinase II preferentially phosphorylates human tau isoforms containing an amino-terminal insert. Identification of threonine 39 as the primary phosphate acceptor. Journal of Biological Chemistry. 1994;269(6):4373–80. [PubMed]
- 183.Ghosh S, Hayden MS. New regulators of NF-κB in inflammation. Nat Rev Immunol. 2008;8(11):837–48. [DOI] [PubMed] [Google Scholar]
- 184.Tang Z, Dai S, He Y, Doty RA, Shultz LD, Sampson SB, et al. MEK guards proteome stability and inhibits tumor-suppressive amyloidogenesis via HSF1. Cell. 2015;160(4):729–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Ussar S, Voss T. MEK1 and MEK2, different regulators of the G1/S transition. J Biol Chem. 2004;279(42):43861–9. [DOI] [PubMed] [Google Scholar]
- 186.Shaul YD, Seger R. The MEK/ERK cascade: from signaling specificity to diverse functions. Biochimica et Biophysica Acta (BBA)-Molecular Cell Research. 2007;1773(8):1213–26. [DOI] [PubMed]
- 187.Chen H-J, Mitchell JC, Novoselov S, Miller J, Nishimura AL, Scotter EL, et al. The heat shock response plays an important role in TDP-43 clearance: evidence for dysfunction in amyotrophic lateral sclerosis. Brain. 2016;139(5):1417–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Carlomagno Y, Zhang Y, Davis M, Lin W-L, Cook C, Dunmore J, et al. Casein kinase II induced polymerization of soluble TDP-43 into filaments is inhibited by heat shock proteins. PLoS ONE. 2014;9(3): e90452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Ono K, Han J. The p38 signal transduction pathway activation and function. Cell Signal. 2000;12(1):1–13. [DOI] [PubMed] [Google Scholar]
- 190.Kyriakis JM, Avruch J. Mammalian mitogen-activated protein kinase signal transduction pathways activated by stress and inflammation. Physiol Rev. 2001;81(2):807–69. [DOI] [PubMed] [Google Scholar]
- 191.Sato S, Cerny RL, Buescher JL, Ikezu T. Tau-tubulin kinase 1 (TTBK1), a neuron-specific tau kinase candidate, is involved in tau phosphorylation and aggregation. J Neurochem. 2006;98(5):1573–84. [DOI] [PubMed] [Google Scholar]
- 192.Tomizawa K, Omori A, Ohtake A, Sato K, Takahashi M. Tau-tubulin kinase phosphorylates tau at Ser-208 and Ser-210, sites found in paired helical filament-tau. FEBS Lett. 2001;492(3):221–7. [DOI] [PubMed] [Google Scholar]
- 193.Hasan R, Humphrey J, Bettencourt C, Newcombe J, Consortium NA, Lashley T, et al. Transcriptomic analysis of frontotemporal lobar degeneration with TDP-43 pathology reveals cellular alterations across multiple brain regions. Acta Neuropathologica. 2021:1–19. [DOI] [PMC free article] [PubMed]
- 194.Vielhaber E, Eide E, Rivers A, Gao Z-H, Virshup DM. Nuclear entry of the circadian regulator mPER1 is controlled by mammalian casein kinase I ɛ. Mol Cell Biol. 2000;20(13):4888–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Lee C, Etchegaray J-P, Cagampang FR, Loudon AS, Reppert SM. Posttranslational mechanisms regulate the mammalian circadian clock. Cell. 2001;107(7):855–67. [DOI] [PubMed] [Google Scholar]
- 196.Canever JB, Queiroz LY, Soares ES, de Avelar NCP, Cimarosti HI. Circadian rhythm alterations affecting the pathology of neurodegenerative diseases. Journal of Neurochemistry. 2023. [DOI] [PubMed]
- 197.Huang Z, Liu Q, Peng Y, Dai J, Xie Y, Chen W, et al. Circadian rhythm dysfunction accelerates disease progression in a mouse model with amyotrophic lateral sclerosis. Front Neurol. 2018;9:218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Zhang T, Jiang X, Xu M, Wang H, Sang X, Qin M, et al. Sleep and circadian abnormalities precede cognitive deficits in R521C FUS knockin rats. Neurobiol Aging. 2018;72:159–70. [DOI] [PubMed] [Google Scholar]
- 199.Komiya Y, Habas R. Wnt signal transduction pathways. Organogenesis. 2008;4(2):68–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Liu C, Li Y, Semenov M, Han C, Baeg G-H, Tan Y, et al. Control of β-catenin phosphorylation/degradation by a dual-kinase mechanism. Cell. 2002;108(6):837–47. [DOI] [PubMed] [Google Scholar]
- 201.Amit S, Hatzubai A, Birman Y, Andersen JS, Ben-Shushan E, Mann M, et al. Axin-mediated CKI phosphorylation of β-catenin at Ser 45: a molecular switch for the Wnt pathway. Genes Dev. 2002;16(9):1066–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.González-Fernández C, Gonzalez P, Andres-Benito P, Ferrer I, Rodríguez FJ. Wnt signaling alterations in the human spinal cord of amyotrophic lateral sclerosis cases: spotlight on Fz2 and Wnt5a. Mol Neurobiol. 2019;56:6777–91. [DOI] [PubMed] [Google Scholar]
- 203.Jiang X, Guan Y, Zhao Z, Meng F, Wang X, Gao X, et al. Potential roles of the WNT signaling pathway in amyotrophic lateral sclerosis. Cells. 2021;10(4):839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.González-Fernández C, González P, Rodríguez FJ. New insights into Wnt signaling alterations in amyotrophic lateral sclerosis: a potential therapeutic target? Neural Regen Res. 2020;15(9):1580–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Sahana T, Zhang K. Mitogen-activated protein kinase pathway in amyotrophic lateral sclerosis. Biomedicines. 2021;9(8):969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Sahu R, Upadhayay S, Mehan S. Inhibition of extracellular regulated kinase (ERK)-1/2 signaling pathway in the prevention of ALS: target inhibitors and influences on neurological dysfunctions. Eur J Cell Biol. 2021;100(7–8): 151179. [DOI] [PubMed] [Google Scholar]
- 207.Xiao J, Ferner AH, Wong AW, Denham M, Kilpatrick TJ, Murray SS. Extracellular signal-regulated kinase 1/2 signaling promotes oligodendrocyte myelination in vitro. J Neurochem. 2012;122(6):1167–80. [DOI] [PubMed] [Google Scholar]
- 208.Jeffries MA, Urbanek K, Torres L, Wendell SG, Rubio ME, Fyffe-Maricich SL. ERK1/2 activation in preexisting oligodendrocytes of adult mice drives new myelin synthesis and enhanced CNS function. J Neurosci. 2016;36(35):9186–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Suo N, Guo Ye, He B, Gu H, Xie X. Inhibition of MAPK/ERK pathway promotes oligodendrocytes generation and recovery of demyelinating diseases. Glia. 2019;67(7):1320–32. [DOI] [PMC free article] [PubMed]
- 210.Raffaele S, Boccazzi M, Fumagalli M. Oligodendrocyte dysfunction in amyotrophic lateral sclerosis: mechanisms and therapeutic perspectives. Cells. 2021;10(3):565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Källstig E, McCabe BD, Schneider BL. The Links between ALS and NF-κB. Int J Mol Sci. 2021;22(8):3875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Tilstra JS, Clauson CL, Niedernhofer LJ, Robbins PD. NF-κB in aging and disease. Aging Dis. 2011;2(6):449. [PMC free article] [PubMed] [Google Scholar]
- 213.Kounatidis I, Chtarbanova S, Cao Y, Hayne M, Jayanth D, Ganetzky B, et al. NF-κB immunity in the brain determines fly lifespan in healthy aging and age-related neurodegeneration. Cell Rep. 2017;19(4):836–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Sivandzade F, Prasad S, Bhalerao A, Cucullo L. NRF2 and NF-қB interplay in cerebrovascular and neurodegenerative disorders: molecular mechanisms and possible therapeutic approaches. Redox Biol. 2019;21: 101059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Correia AS, Patel P, Dutta K, Julien J-P. Inflammation induces TDP-43 mislocalization and aggregation. PLoS ONE. 2015;10(10): e0140248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Swarup V, Phaneuf D, Dupré N, Petri S, Strong M, Kriz J, et al. Deregulation of TDP-43 in amyotrophic lateral sclerosis triggers nuclear factor κB–mediated pathogenic pathways. J Exp Med. 2011;208(12):2429–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Zhao W, Beers DR, Bell S, Wang J, Wen S, Baloh RH, et al. TDP-43 activates microglia through NF-κB and NLRP3 inflammasome. Exp Neurol. 2015;273:24–35. [DOI] [PubMed] [Google Scholar]
- 218.Zhu J, Cynader MS, Jia W. TDP-43 inhibits NF-κB activity by blocking p65 nuclear translocation. PLoS ONE. 2015;10(11): e0142296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Dutta K, Thammisetty SS, Boutej H, Bareil C, Julien J-P. Mitigation of ALS pathology by neuron-specific inhibition of nuclear factor kappa B signaling. J Neurosci. 2020;40(26):5137–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Zarubin T, Han J. Activation and signaling of the p38 MAP kinase pathway. Cell Res. 2005;15(1):11–8. [DOI] [PubMed] [Google Scholar]
- 221.Rouse J, Cohen P, Trigon S, Morange M, Alonso-Llamazares A, Zamanillo D, et al. A novel kinase cascade triggered by stress and heat shock that stimulates MAPKAP kinase-2 and phosphorylation of the small heat shock proteins. Cell. 1994;78(6):1027–37. [DOI] [PubMed] [Google Scholar]
- 222.Foltz IN, Lee JC, Young PR, Schrader JW. Hemopoietic growth factors with the exception of interleukin-4 activate the p38 mitogen-activated protein kinase pathway. J Biol Chem. 1997;272(6):3296–301. [DOI] [PubMed] [Google Scholar]
- 223.Bulavin DV, Saito S, Hollander MC, Sakaguchi K, Anderson CW, Appella E, et al. Phosphorylation of human p53 by p38 kinase coordinates N‐terminal phosphorylation and apoptosis in response to UV radiation. The EMBO journal. 1999. [DOI] [PMC free article] [PubMed]
- 224.Obata T, Brown GE, Yaffe MB. MAP kinase pathways activated by stress: the p38 MAPK pathway. Crit Care Med. 2000;28(4):N67–77. [DOI] [PubMed] [Google Scholar]
- 225.Behrend L, Stöter M, Kurth M, Rutter G, Heukeshoven J, Deppert W, et al. Interaction of casein kinase 1 delta (CK1δ) with post-Golgi structures, microtubules and the spindle apparatus. Eur J Cell Biol. 2000;79(4):240–51. [DOI] [PubMed] [Google Scholar]
- 226.Watanabe T, Kakeno M, Matsui T, Sugiyama I, Arimura N, Matsuzawa K, et al. TTBK2 with EB1/3 regulates microtubule dynamics in migrating cells through KIF2A phosphorylation. J Cell Biol. 2015;210(5):737–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Bao C, Bajrami B, Marcotte DJ, Chodaparambil JV, Kerns HM, Henderson J, et al. Mechanisms of regulation and diverse activities of tau-tubulin kinase (TTBK) isoforms. Cell Mol Neurobiol. 2021;41:669–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Roth A, Gihring A, Bischof J, Pan L, Oswald F, Knippschild U. CK1 is a druggable regulator of microtubule dynamics and microtubule-associated processes. Cancers. 2022;14(5):1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Clark JA, Yeaman EJ, Blizzard CA, Chuckowree JA, Dickson TC. A case for microtubule vulnerability in amyotrophic lateral sclerosis: altered dynamics during disease. Front Cell Neurosci. 2016;10:204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Baas PW, Lin S. Hooks and comets: the story of microtubule polarity orientation in the neuron. Dev Neurobiol. 2011;71(6):403–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Sakakibara A, Ando R, Sapir T, Tanaka T. Microtubule dynamics in neuronal morphogenesis. Open Biol. 2013;3(7): 130061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Chen BL, Hall DH, Chklovskii DB. Wiring optimization can relate neuronal structure and function. Proc Natl Acad Sci. 2006;103(12):4723–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Kanai Y, Dohmae N, Hirokawa N. Kinesin transports RNA: isolation and characterization of an RNA-transporting granule. Neuron. 2004;43(4):513–25. [DOI] [PubMed] [Google Scholar]
- 234.Long H-Z, Cheng Y, Zhou Z-W, Luo H-Y, Wen D-D, Gao L-C. PI3K/AKT signal pathway: a target of natural products in the prevention and treatment of Alzheimer’s disease and Parkinson’s disease. Front Pharmacol. 2021;12: 648636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Ojeda L, Gao J, Hooten KG, Wang E, Thonhoff JR, Dunn TJ, et al. Critical role of PI3K/Akt/GSK3β in motoneuron specification from human neural stem cells in response to FGF2 and EGF. PLoS ONE. 2011;6(8): e23414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Di Maira G, Salvi M, Arrigoni G, Marin O, Sarno S, Brustolon F, et al. Protein kinase CK2 phosphorylates and upregulates Akt/PKB. Cell Death Differ. 2005;12(6):668–77. [DOI] [PubMed] [Google Scholar]
- 237.Girardi C, James P, Zanin S, Pinna LA, Ruzzene M. Differential phosphorylation of Akt1 and Akt2 by protein kinase CK2 may account for isoform specific functions. Biochimica et Biophysica Acta (BBA)-Molecular Cell Research. 2014;1843(9):1865–74. [DOI] [PubMed]
- 238.Torres J, Pulido R. The tumor suppressor PTEN is phosphorylated by the protein kinase CK2 at its C terminus: implications for PTEN stability to proteasome-mediated degradation. J Biol Chem. 2001;276(2):993–8. [DOI] [PubMed] [Google Scholar]
- 239.Miller SJ, Lou DY, Seldin DC, Lane WS, Neel BG. Direct identification of PTEN phosphorylation sites. FEBS Lett. 2002;528(1–3):145–53. [DOI] [PubMed] [Google Scholar]
- 240.Paplomata E, O’Regan R. The PI3K/AKT/mTOR pathway in breast cancer: targets, trials and biomarkers. Therapeutic advances in medical oncology. 2014;6(4):154–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Gasparri ML, Besharat ZM, Farooqi AA, Khalid S, Taghavi K, Besharat RA, et al. MiRNAs and their interplay with PI3K/AKT/mTOR pathway in ovarian cancer cells: a potential role in platinum resistance. J Cancer Res Clin Oncol. 2018;144:2313–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Brockman JL, Gross SD, Sussman MR, Anderson RA. Cell cycle-dependent localization of casein kinase I to mitotic spindles. Proc Natl Acad Sci. 1992;89(20):9454–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Nandakumar S, Rozich E, Buttitta L. Cell cycle re-entry in the nervous system: from polyploidy to neurodegeneration. Frontiers in Cell and Developmental Biology. 2021;9: 698661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Yang Y, Geldmacher DS, Herrup K. DNA replication precedes neuronal cell death in Alzheimer’s disease. J Neurosci. 2001;21(8):2661–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Yang Y, Mufson EJ, Herrup K. Neuronal cell death is preceded by cell cycle events at all stages of Alzheimer’s disease. J Neurosci. 2003;23(7):2557–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Koseoglu MM, Norambuena A, Sharlow ER, Lazo JS, Bloom GS. Aberrant neuronal cell cycle re-entry: The pathological confluence of Alzheimer’s disease and brain insulin resistance, and its relation to cancer. J Alzheimers Dis. 2019;67(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Ranganathan S, Bowser R. Alterations in G1 to S phase cell-cycle regulators during amyotrophic lateral sclerosis. Am J Pathol. 2003;162(3):823–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Ranganathan S, Bowser R. p53 and cell cycle proteins participate in spinal motor neuron cell death in ALS. The open pathology journal. 2010;4:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Bollen M, Peti W, Ragusa MJ, Beullens M. The extended PP1 toolkit: designed to create specificity. Trends Biochem Sci. 2010;35(8):450–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Tournebize R, Andersen SS, Verde F, Dorée M, Karsenti E, Hyman AA. Distinct roles of PP1 and PP2A-like phosphatases in control of microtubule dynamics during mitosis. Embo j. 1997;16(18):5537–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Fong NM, Jensen TC, Shah AS, Parekh NN, Saltiel AR, Brady MJ. Identification of Binding Sites on Protein Targeting to Glycogen for Enzymes of Glycogen Metabolism*. J Biol Chem. 2000;275(45):35034–9. [DOI] [PubMed] [Google Scholar]
- 252.Morishita W, Connor JH, Xia H, Quinlan EM, Shenolikar S, Malenka RC. Regulation of synaptic strength by protein phosphatase 1. Neuron. 2001;32(6):1133–48. [DOI] [PubMed] [Google Scholar]
- 253.Virshup DM, Shenolikar S. From promiscuity to precision: protein phosphatases get a makeover. Mol Cell. 2009;33(5):537–45. [DOI] [PubMed] [Google Scholar]
- 254.Gu J, Wang W, Miao S, Chen F, Wu F, Hu W, et al. Protein Phosphatase 1 dephosphorylates TDP-43 and suppresses its function in tau exon 10 inclusion. FEBS Lett. 2018;592(3):402–10. [DOI] [PubMed] [Google Scholar]
- 255.Umoh ME, Dammer EB, Dai J, Duong DM, Lah JJ, Levey AI, et al. A proteomic network approach across the ALS-FTD disease spectrum resolves clinical phenotypes and genetic vulnerability in human brain. EMBO Mol Med. 2018;10(1):48–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Seshacharyulu P, Pandey P, Datta K, Batra SK. Phosphatase: PP2A structural importance, regulation and its aberrant expression in cancer. Cancer Lett. 2013;335(1):9–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Rusnak F, Mertz P. Calcineurin: form and function. Physiol Rev. 2000;80(4):1483–521. [DOI] [PubMed] [Google Scholar]
- 258.Cousin MA, Robinson PJ. The dephosphins: dephosphorylation by calcineurin triggers synaptic vesicle endocytosis. Trends Neurosci. 2001;24(11):659–65. [DOI] [PubMed] [Google Scholar]
- 259.Tarasova E, Gaydukov A, Balezina O. Calcineurin and its role in synaptic transmission. Biochem Mosc. 2018;83:674–89. [DOI] [PubMed] [Google Scholar]
- 260.Ferri A, Nencini M, Battistini S, Giannini F, Siciliano G, Casali C, et al. Activity of protein phosphatase calcineurin is decreased in sporadic and familial amyotrophic lateral sclerosispatients. J Neurochem. 2004;90(5):1237–42. [DOI] [PubMed] [Google Scholar]
- 261.Wagey R, Krieger C, Shaw CA. Abnormal dephosphorylation effect on NMDA receptor regulation in ALS spinal cord. Neurobiol Dis. 1997;4(5):350–5. [DOI] [PubMed] [Google Scholar]
- 262.Mann JR, Gleixner AM, Mauna JC, Gomes E, DeChellis-Marks MR, Needham PG, et al. RNA Binding Antagonizes Neurotoxic Phase Transitions of TDP-43. Neuron. 2019;102(2):321-38.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Zhang P, Fan B, Yang P, Temirov J, Messing J, Kim HJ, et al. Chronic optogenetic induction of stress granules is cytotoxic and reveals the evolution of ALS-FTD pathology. Elife. 2019;8. [DOI] [PMC free article] [PubMed]
- 264.Walker AK, Spiller KJ, Ge G, Zheng A, Xu Y, Zhou M, et al. Functional recovery in new mouse models of ALS/FTLD after clearance of pathological cytoplasmic TDP-43. Acta Neuropathol. 2015;130:643–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Deng Q, Holler CJ, Taylor G, Hudson KF, Watkins W, Gearing M, et al. FUS is phosphorylated by DNA-PK and accumulates in the cytoplasm after DNA damage. J Neurosci. 2014;34(23):7802–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Brady OA, Meng P, Zheng Y, Mao Y, Hu F. Regulation of TDP-43 aggregation by phosphorylation andp62/SQSTM1. J Neurochem. 2011;116(2):248–59. [DOI] [PubMed] [Google Scholar]
- 267.Fujiwara H, Hasegawa M, Dohmae N, Kawashima A, Masliah E, Goldberg MS, et al. α-Synuclein is phosphorylated in synucleinopathy lesions. Nat Cell Biol. 2002;4(2):160–4. [DOI] [PubMed] [Google Scholar]
- 268.Anderson JP, Walker DE, Goldstein JM, De Laat R, Banducci K, Caccavello RJ, et al. Phosphorylation of Ser-129 is the dominant pathological modification of α-synuclein in familial and sporadic Lewy body disease. J Biol Chem. 2006;281(40):29739–52. [DOI] [PubMed] [Google Scholar]
- 269.Gardiner M, Toth R, Vandermoere F, Morrice NA, Rouse J. Identification and characterization of FUS/TLS as a new target of ATM. Biochemical Journal. 2008;415(2):297–307. [DOI] [PubMed] [Google Scholar]
- 270.Rhoads SN, Monahan ZT, Yee DS, Leung AY, Newcombe CG, O’Meally RN, et al. The prionlike domain of FUS is multiphosphorylated following DNA damage without altering nuclear localization. Mol Biol Cell. 2018;29(15):1786–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Hanger DP, Anderton BH, Noble W. Tau phosphorylation: the therapeutic challenge for neurodegenerative disease. Trends Mol Med. 2009;15(3):112–9. [DOI] [PubMed] [Google Scholar]
- 272.Ambadipudi S, Biernat J, Riedel D, Mandelkow E, Zweckstetter M. Liquid–liquid phase separation of the microtubule-binding repeats of the Alzheimer-related protein Tau. Nat Commun. 2017;8(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Kanaan NM, Hamel C, Grabinski T, Combs B. Liquid-liquid phase separation induces pathogenic tau conformations in vitro. Nat Commun. 2020;11(1):1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Ray S, Singh N, Kumar R, Patel K, Pandey S, Datta D, et al. α-Synuclein aggregation nucleates through liquid–liquid phase separation. Nat Chem. 2020;12(8):705–16. [DOI] [PubMed] [Google Scholar]
- 275.Monahan Z, Ryan VH, Janke AM, Burke KA, Rhoads SN, Zerze GH, et al. Phosphorylation of the FUS low-complexity domain disrupts phase separation, aggregation, and toxicity. Embo j. 2017;36(20):2951–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Liu Z, Zhang S, Gu J, Tong Y, Li Y, Gui X, et al. Hsp27 chaperones FUS phase separation under the modulation of stress-induced phosphorylation. Nat Struct Mol Biol. 2020;27(4):363–72. [DOI] [PubMed] [Google Scholar]
- 277.Kishino Y, Matsukawa K, Matsumoto T, Miyazaki R, Wakabayashi T, Nonaka T, et al. Casein kinase 1δ/ε phosphorylates fused in sarcoma (FUS) and ameliorates FUS-mediated neurodegeneration. Journal of Biological Chemistry. 2022;298(8). [DOI] [PMC free article] [PubMed]
- 278.Singh TJ, Grundke-Iqbal I, Iqbal K. Phosphorylation of τ Protein by Casein Kinase-1 Converts It to an Abnormal Alzheimer-Like State. J Neurochem. 1995;64(3):1420–3. [DOI] [PubMed] [Google Scholar]
- 279.Martinez-Gonzalez L, Cuevas EP, Tosat Bitrian C, Nozal V, Gil C, Palomo V, et al. TTBK1 and CK1 inhibitors restore TDP-43 pathology and avoid disease propagation in lymphoblast from Alzheimer’s disease patients. Front Mol Neurosci. 2023;16:1243277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Chen Z, Cole PA. Synthetic approaches to protein phosphorylation. Curr Opin Chem Biol. 2015;28:115–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Brahmachari S, Ge P, Lee SH, Kim D, Karuppagounder SS, Kumar M, et al. Activation of tyrosine kinase c-Abl contributes to α-synuclein–induced neurodegeneration. J Clin Investig. 2016;126(8):2970–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Mahul-Mellier A-L, Fauvet B, Gysbers A, Dikiy I, Oueslati A, Georgeon S, et al. c-Abl phosphorylates α-synuclein and regulates its degradation: implication for α-synuclein clearance and contribution to the pathogenesis of Parkinson’s disease. Hum Mol Genet. 2014;23(11):2858–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Imam SZ, Zhou Q, Yamamoto A, Valente AJ, Ali SF, Bains M, et al. Novel regulation of parkin function through c-Abl-mediated tyrosine phosphorylation: implications for Parkinson’s disease. J Neurosci. 2011;31(1):157–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Derkinderen P, Scales TM, Hanger DP, Leung K-Y, Byers HL, Ward MA, et al. Tyrosine 394 is phosphorylated in Alzheimer’s paired helical filament tau and in fetal tau with c-Abl as the candidate tyrosine kinase. J Neurosci. 2005;25(28):6584–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Tremblay MA, Acker CM, Davies P. Tau phosphorylated at tyrosine 394 is found in Alzheimer’s disease tangles and can be a product of the Abl-related kinase. Arg Journal of Alzheimer’s Disease. 2010;19(2):721–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Vega IE, Cui L, Propst JA, Hutton ML, Lee G, Yen SH. Increase in tau tyrosine phosphorylation correlates with the formation of tau aggregates. Brain Res Mol Brain Res. 2005;138(2):135–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Gu J, Hu W, Tan X, Qu S, Chu D, Gong CX, et al. Elevation of casein kinase 1ε associated with TDP-43 and tau pathologies in Alzheimer’s disease. Brain Pathol. 2020;30(2):283–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Flajolet M, He G, Heiman M, Lin A, Nairn AC, Greengard P. Regulation of Alzheimer’s disease amyloid-β formation by casein kinase I. Proc Natl Acad Sci. 2007;104(10):4159–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Iimoto DS, Masliah E, DeTeresa R, Terry RD, Saitoh T. Aberrant casein kinase II in Alzheimer’s disease. Brain Res. 1990;507(2):273–80. [DOI] [PubMed] [Google Scholar]
- 290.Rosenberger AF, Morrema TH, Gerritsen WH, van Haastert ES, Snkhchyan H, Hilhorst R, et al. Increased occurrence of protein kinase CK2 in astrocytes in Alzheimer’s disease pathology. J Neuroinflammation. 2016;13:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Feijoo C, Campbell DG, Jakes R, Goedert M, Cuenda A. Evidence that phosphorylation of the microtubule-associated protein Tau by SAPK4/p38δ at Thr50 promotes microtubule assembly. J Cell Sci. 2005;118(2):397–408. [DOI] [PubMed] [Google Scholar]
- 292.Gong C-X, Grundke-Iqbal I, Damuni Z, Iqbal K. Dephosphorylation of microtubule-associated protein tau by protein phosphatase-1 and-2C and its implication in Alzheimer disease. FEBS Lett. 1994;341(1):94–8. [DOI] [PubMed] [Google Scholar]
- 293.Gong CX, Singh TJ, Grundke-Iqbal I, Iqbal K. Phosphoprotein phosphatase activities in Alzheimer disease brain. J Neurochem. 1993;61(3):921–7. [DOI] [PubMed] [Google Scholar]
- 294.Gong CX, Shaikh S, Wang JZ, Zaidi T, Grundke-Iqbal I, Iqbal K. Phosphatase activity toward abnormally phosphorylated τ: decrease in Alzheimer disease brain. J Neurochem. 1995;65(2):732–8. [DOI] [PubMed] [Google Scholar]
- 295.Lee K-W, Chen W, Junn E, Im J-Y, Grosso H, Sonsalla PK, et al. Enhanced phosphatase activity attenuates α-synucleinopathy in a mouse model. J Neurosci. 2011;31(19):6963–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Pérez-Revuelta B, Hettich M, Ciociaro A, Rotermund C, Kahle P, Krauss S, et al. Metformin lowers Ser-129 phosphorylated α-synuclein levels via mTOR-dependent protein phosphatase 2A activation. Cell Death Dis. 2014;5(5):e1209-e. [DOI] [PMC free article] [PubMed]
- 297.Gong C-X, Lidsky T, Wegiel J, Zuck L, Grundke-Iqbal I, Iqbal K. Phosphorylation of Microtubule-associated Protein Tau Is Regulated by Protein Phosphatase 2A in Mammalian Brain: implications for neurofibrillary degeneration in alzheimer’s disease*. J Biol Chem. 2000;275(8):5535–44. [DOI] [PubMed] [Google Scholar]
- 298.Drewes G, Mandelkow E-M, Baumann K, Goris J, Merlevede W, Mandelkow E. Dephosphorylation of tau protein and Alzheimer paired helical filaments by calcmeurin and phosphatase-2A. FEBS Lett. 1993;336(3):425–32. [DOI] [PubMed] [Google Scholar]
- 299.Gong C-X, Grundke-Iqbal I, Iqbal K. Dephosphorylation of Alzheimer’s disease abnormally phosphorylated tau by protein phosphatase-2A. Neuroscience. 1994;61(4):765–72. [DOI] [PubMed] [Google Scholar]
- 300.Goedert M, Jakes R, Qi Z, Wang J, Cohen P. Protein Phosphatase 2A Is the Major Enzyme in Brain that Dephosphorylates τ Protein Phosphorylated by Proline-Directed Protein Kinases or Cyclic AMP-Dependent Protein Kinase. J Neurochem. 1995;65(6):2804–7. [DOI] [PubMed] [Google Scholar]
- 301.Wang J-Z, Gong C-X, Zaidi T, Grundke-Iqbal I, Iqbal K. Dephosphorylation of Alzheimer paired helical filaments by protein phosphatase-2A and− 2B. J Biol Chem. 1995;270(9):4854–60. [DOI] [PubMed] [Google Scholar]
- 302.Sontag E, Nunbhakdi-Craig V, Lee G, Bloom GS, Mumby MC. Regulation of the phosphorylation state and microtubule-binding activity of Tau by protein phosphatase 2A. Neuron. 1996;17(6):1201–7. [DOI] [PubMed] [Google Scholar]
- 303.Vogelsberg-Ragaglia V, Schuck T, Trojanowski JQ, Lee VM-Y. PP2A mRNA expression is quantitatively decreased in Alzheimer's disease hippocampus. Experimental neurology. 2001;168(2):402–12. [DOI] [PubMed]
- 304.Sontag E, Luangpirom A, Hladik C, Mudrak I, Ogris E, Speciale S, et al. Altered Expression Levels of the Protein Phosphatase 2A ABαC Enzyme Are Associated with Alzheimer Disease Pathology. J Neuropathol Exp Neurol. 2004;63(4):287–301. [DOI] [PubMed] [Google Scholar]
- 305.Gong CX, Singh TJ, Grundke-Iqbal I, Iqbal K. Alzheimer’s Disease Abnormally Phosphorylated τ Is Dephosphorylated by Protein Phosphatase-2B (Calcineurin). J Neurochem. 1994;62(2):803–6. [DOI] [PubMed] [Google Scholar]
- 306.Rahman A, Grundke-Iqbal I, Iqbal K. PP2B isolated from human brain preferentially dephosphorylates Ser-262 and Ser-396 of the Alzheimer disease abnormally hyperphosphorylated tau. J Neural Transm. 2006;113:219–30. [DOI] [PubMed] [Google Scholar]
- 307.Lian Q, Ladner CJ, Magnuson D, Lee JM. Selective changes of calcineurin (protein phosphatase 2B) activity in Alzheimer’s disease cerebral cortex. Exp Neurol. 2001;167(1):158–65. [DOI] [PubMed] [Google Scholar]
- 308.Ladner CJ, Czech J, Maurice J, Lorens SA, Lee JM. Reduction of Calcineurin Enzymatic Activity in Alzheimer’s Disease: Correlation with Neuropathologic Changes. J Neuropathol Exp Neurol. 1996;55(8):924–31. [DOI] [PubMed] [Google Scholar]
- 309.Qian W, Yin X, Hu W, Shi J, Gu J, Grundke-Iqbal I, et al. Activation of protein phosphatase 2B and hyperphosphorylation of Tau in Alzheimer’s disease. J Alzheimers Dis. 2011;23(4):617–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Liachko NF, Guthrie CR, Kraemer BC. Phosphorylation promotes neurotoxicity in a Caenorhabditis elegans model of TDP-43 proteinopathy. J Neurosci. 2010;30(48):16208–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.