Abstract
The coronavirus disease 2019 (COVID-19) pandemic introduced unprecedented challenges to healthcare systems, disrupting the management of chronic conditions such as hypertension. This study examines the impact of the COVID-19 pandemic on hypertension management by emergency medical teams (EMTs) in southeastern Poland. A retrospective analysis was conducted using medical emergency activity cards from EMTs in southeastern Poland. The study included 1795 cases of primary hypertension (International Classification of Diseases, 10th Edition: I-10), comparing data from the pre-pandemic period (April 1, 2019–March 31, 2020) to the pandemic period (April 1, 2020–March 31, 2021). Demographic characteristics, blood pressure measurements, pharmacological interventions, and transport decisions were analyzed using Chi-square tests for categorical variables and t-tests for continuous variables. The frequency of hypertension-related emergency calls remained stable between the pre-pandemic and pandemic periods (P = .805). Women accounted for 68.6% (N = 1232) of cases, and the mean age of patients was 63.4 years (SD = 15.2), with no significant age or sex differences between the 2 periods. The mean initial systolic blood pressure (SBP) was significantly higher before the pandemic (189.85 mm Hg) compared to during the pandemic (185.57 mm Hg, P < .001). The proportion of patients with severe hypertension (SBP ≥ 180 mm Hg) decreased from 70.7% to 66.1%, while mild hypertension cases increased from 5.3% to 7.1% (P = .046). The administration of hydroxyzine increased significantly (38.2% vs 45.1%, P = .003), reflecting a greater focus on managing anxiety-related symptoms. Additionally, EMTs treated more patients at the scene rather than transporting them to the emergency department (76.1% vs 62.4%, P < .001), indicating a shift in EMT decision-making to reduce hospital exposure and optimize resource allocation. The COVID-19 pandemic significantly altered the prehospital management of hypertension, leading to lower initial SBP readings, increased anxiolytic use, and reduced hospital transport rates. Age and sex distribution remained stable across both periods. These findings highlight the need for flexible emergency response protocols that integrate mental health considerations and enhance on-site hypertension management. Future research should assess the long-term outcomes of these adaptations and explore strategies to improve prehospital hypertension care in future public health emergencies.
Keywords: blood pressure, COVID-19, emergency medical teams, healthcare adaptation, hypertension, retrospective study, therapeutic interventions, transport decisions
1. Introduction
Hypertension, or high blood pressure, represents a critical public health issue globally, affecting a significant portion of the adult population.[1] It stands as one of the most crucial modifiable risk factors for a variety of severe health conditions, notably cardiovascular diseases, which remain leading causes of morbidity and mortality worldwide.[2] The pervasive impact of hypertension necessitates continuous efforts in monitoring, managing, and developing effective treatment strategies to mitigate its detrimental effects.[3]
In Poland, hypertension affects approximately 10 million individuals, posing a significant burden on the healthcare system. Before the coronavirus disease 2019 (COVID-19) pandemic, emergency medical teams (EMTs) played a key role in managing hypertensive emergencies, providing prehospital interventions, and deciding whether patients required hospitalization. EMTs operated within a structured healthcare framework where hospital-based care was readily accessible for hypertensive crises.[4]
The COVID-19 pandemic, which began in late 2019, brought unprecedented challenges to healthcare systems worldwide.[5] The sudden surge in COVID-19 cases strained medical resources and facilities, leading to significant disruptions in routine healthcare services. Patients with chronic conditions, such as hypertension, faced new barriers to accessing timely medical care.[6] Lockdowns, social distancing measures, and the overwhelming focus on COVID-19 cases forced many healthcare providers to defer nonurgent consultations and procedures.[6] This shift placed additional burdens on emergency medical services, which had to adapt rapidly to the evolving situation.
Emerging studies have shown that the pandemic exacerbated health disparities, particularly for those with chronic conditions like hypertension. For instance, research conducted in the United States and Italy indicated a substantial decline in hospital admissions for hypertension and other chronic conditions during the early months of the pandemic due to fear of contracting the virus in healthcare settings.[7,8] Additionally, a study in the United Kingdom highlighted delays and disruptions in receiving care for chronic conditions, which negatively impacted patient outcomes.[9]
EMTs found themselves at the forefront of the healthcare response during the pandemic, dealing not only with COVID-19 patients but also ensuring that individuals with other urgent medical needs, including hypertension, received appropriate care. EMTs had to navigate increased call volumes, implement stringent infection control protocols, and manage the added complexity of treating patients in a high-risk environment.[10] These challenges necessitated significant adjustments in their operational procedures and decision-making processes.
The pandemic significantly affected the frequency and nature of hypertension-related emergency calls. There was a need to understand how the heightened pressure on healthcare systems influenced the epidemiology of hypertension and the approaches EMTs took in their therapeutic interventions.[11] Additionally, decisions regarding whether to transport patients to hospitals or treat them on the scene had to be reconsidered in light of the risks associated with COVID-19 exposure and hospital capacity constraints.[12]
Recent studies have also highlighted the psychological impact of the pandemic, contributing to increased stress and anxiety levels, which can adversely affect blood pressure control.[13] The increased use of anxiolytics during the pandemic has been noted, suggesting a direct link between the psychological burden of the pandemic and the management of hypertension.[14]
The aim of this study was to analyze the impact of the COVID-19 pandemic on the epidemiology of hypertension, the therapeutic interventions, and the decisions made by EMTs in southeastern Poland, providing insights that can inform strategies to enhance the resilience of emergency medical services globally. Specifically, the study sought to address how the pandemic affected the frequency of hypertension-related emergency calls and what changes occurred in the therapeutic approaches and transport decisions by EMTs during this period. By comparing data from before and during the pandemic, the study provides a detailed examination of the adaptations in emergency medical responses to hypertension amid a global health crisis.
Southeastern Poland was chosen as the focus of this study due to its unique healthcare infrastructure and EMT operational framework. Unlike previous studies conducted in larger metropolitan areas, this study examines the impact of the pandemic on a region with more decentralized healthcare services, where EMTs play a particularly crucial role in providing timely care for hypertensive emergencies. This regional perspective offers new insights into how emergency medical services adapted to the pandemic in nonmetropolitan settings and highlights potential lessons for similar healthcare environments globally.
The findings from this research are intended to contribute to the broader understanding of the pandemic’s effects on healthcare systems and to provide valuable lessons for improving emergency medical services in future public health emergencies. By examining the specific case of southeastern Poland, this study also offers insights that may be applicable to other regions with similar healthcare infrastructures. The ultimate goal is to enhance the resilience and effectiveness of healthcare delivery in times of crisis, ensuring that patients with chronic conditions like hypertension receive the care they need despite the challenges posed by such unprecedented events.
2. Materials and methods
2.1. Study design, setting, and period
This study was designed as a retrospective analysis of medical documentation, specifically focusing on medical emergency activity cards completed by members of the EMT. The research was conducted in the southeastern region of Poland and spanned a 2-year period from April 1, 2019, to March 31, 2021.
The study period was selected to reflect both the pre-pandemic and pandemic phases. In Poland, the first confirmed case of COVID-19 was reported on March 4, 2020, and the country declared a state of epidemic on March 20, 2020, implementing widespread public health measures. The state of epidemic emergency officially ended on May 16, 2022. The study defined the pre-pandemic period as April 1, 2019–March 31, 2020, and the pandemic period as April 1, 2020–March 31, 2021, aligning with the timeline of significant healthcare disruptions due to the pandemic.
2.2. Inclusion and exclusion criteria
The study focused on adult patients (aged 18 and above) who were diagnosed with primary hypertension (International Classification of Diseases, 10th Edition: I-10) by EMTs during prehospital care. The inclusion criteria required that emergency interventions occurred within the study period (April 1, 2019–March 31, 2021) and that medical records contained at least one noninvasive blood pressure measurement. The study did not distinguish between first-time and previously diagnosed cases of hypertension, as the diagnosis was based on EMT assessment during emergency intervention. Patients were excluded if they were minors, had a systolic blood pressure (SBP) below 140 mm Hg, or had incomplete medical records, including those missing essential clinical data necessary for analysis.
2.3. Data collection
Primary data were collected retrospectively from medical emergency activity cards filled out by EMT personnel during their interventions. A total of 1795 cases were included in the study, each involving a patient diagnosed with primary hypertension. Since a hypertension diagnosis by an EMT required at least one recorded blood pressure reading, all included cases had documented noninvasive blood pressure measurements performed using a monitor-defibrillator during the intervention.
To ensure data quality, a systematic review process was conducted. All medical records were independently verified by 2 researchers to confirm the presence of key variables, including patient demographics, blood pressure readings, therapeutic interventions, and transport decisions. Discrepancies were resolved through discussion, and cases with missing or unclear information were excluded from the dataset to maintain the integrity of the study findings.
2.4. Analyzed variables
The analysis considered several variables to evaluate the impact of the COVID-19 pandemic on emergency calls related to hypertension. These included demographic data (age and gender), blood pressure measurements (systolic and diastolic blood pressure, SBP and DBP) recorded during EMT interventions, pharmacological interventions (use of captopril, furosemide, and hydroxyzine), and EMT transport decisions (whether patients were transported to the emergency department (ED) or left at the scene). These variables were compared between the pre-pandemic period (April 1, 2019–March 31, 2020) and the pandemic period (April 1, 2020–March 31, 2021) to assess changes in hypertension management.
To ensure alignment with the study objectives, the analysis focused on differences in patient characteristics, blood pressure values at the scene, medications administered, and EMT transport decisions before and during the pandemic. Additionally, EMT transport decisions were examined in relation to initial SBP and control SBP following EMT intervention to assess variations in patient management.
Initial Blood Pressure (Initial BP) was defined as the first blood pressure measurement recorded by EMTs at the scene upon patient assessment before any medical intervention. Control Blood Pressure (Control BP) referred to the last recorded blood pressure measurement taken before the EMT completed the intervention, either before transport to the hospital or before leaving the patient at the scene. These measurements provided insight into the immediate effects of EMT-administered treatment and changes in blood pressure management strategies during the pandemic.
2.5. Data management and security
All data were stored in secure, restricted-access systems to ensure confidentiality and data integrity. Only authorized personnel had access to the data, which were used exclusively for scientific purposes. The data management protocols adhered to strict guidelines to protect patient privacy and ensure compliance with ethical standards.
2.6. Statistical analysis
Statistical analyses were conducted using IBM SPSS Statistics version 29.0.0. Given the large sample size of 1795 cases, normal distribution of quantitative variables was assumed. However, to verify this assumption, data distribution was assessed using the Kolmogorov-Smirnov test and Shapiro–Wilk test for normality. Additionally, histograms and Q-Q plots were visually inspected to confirm the distribution pattern. The study groups included patients from the pre-pandemic period (April 1, 2019–March 31, 2020) and the pandemic period (April 1, 2020–March 31, 2021).
Categorical variables (e.g., sex distribution, medication use, and EMT transport decisions) were analyzed using Pearson Chi-squared test. For 2 × 2 contingency tables, Chi-squared test with continuity correction was applied.
Continuous variables (e.g., SBP and DBP) were analyzed using the independent samples t-test to compare mean differences between the 2 study periods.
To assess potential interactions between the pandemic period and EMT transport decisions, a two-way ANOVA (2 × 2 factorial design) was conducted to examine its effects on initial SBP and controlled SBP following EMT intervention.
To assess the adequacy of the study’s sample size, a post hoc power analysis was performed to determine whether the sample size was sufficient for detecting meaningful differences between study groups. The power analysis ensured that the study had a high probability of identifying statistically significant differences where they existed. A significance level of P < .05 was adopted for all statistical tests.
2.7. Ethical considerations
This study adhered to ethical guidelines to ensure participant protection and research integrity. Informed consent was obtained from all participants, and confidentiality was strictly maintained. Ethical approval for the current research was obtained from the Bioethics Committee at the Medical University of Lublin (decision number: KE-0254/150/06/2022), following the Declaration of Helsinki and relevant ethical standards.
3. Results
The study included a total of 1795 cases of emergency calls related to hypertension, with 902 calls recorded before the pandemic and 893 calls during the pandemic. Statistical analysis showed no significant difference in the number of hypertension-related EMT interventions between the 2 periods (P = .832), indicating that the overall demand for emergency hypertension management remained stable despite the challenges posed by COVID-19.
3.1. Participant characteristics and blood pressure levels
The analysis of demographic data showed that women comprised 68.6% (N = 1232) of all patients, with no statistically significant difference in sex distribution between the pre-pandemic and pandemic periods (P = .805). However, there was a significant shift in age distribution. During the pandemic, the proportion of patients aged < 40 and 40 to 59 years increased, while the proportion of those aged ≥ 60 years decreased (P = .003) (Table 1).
Table 1.
Participant characteristics and blood pressure levels before and during the COVID-19 pandemic.
| Variable | Before COVID-19 (N = 936) | During COVID-19 (N = 859) | P-value |
|---|---|---|---|
| Women, n (%) | 640 (68.4%) | 592 (68.9%) | .805 |
| Men, n (%) | 296 (31.6%) | 267 (31.1%) | |
| Age < 40 years, n (%) | 150 (16.0%) | 160 (18.6%) | |
| Age 40–59 years, n (%) | 320 (34.2%) | 340 (39.6%) | |
| Age ≥ 60 years, n (%) | 466 (49.8%) | 359 (41.8%) | .003 |
| Mild Hypertension (SBP 140–159 mm Hg), n (%) | 50 (5.3%) | 61 (7.1%) | |
| Moderate Hypertension (SBP 160–179 mm Hg), n (%) | 224 (23.9%) | 230 (26.8%) | |
| Severe Hypertension (SBP ≥ 180 mm Hg), n (%) | 662 (70.7%) | 568 (66.1%) | .046 |
| Initial SBP, mean ± SD (mm Hg) | 189.85 ± 24.36 | 185.57 ± 21.35 | <.001 |
| Initial DBP, mean ± SD (mm Hg) | 98.5 ± 15.2 | 95.3 ± 13.9 | .003 |
| Control SBP, mean ± SD (mm Hg) | 179.57 ± 25.72 | 172.12 ± 22.3 | <.001 |
| Control DBP, mean ± SD (mm Hg) | 92.1 ± 14.6 | 88.5 ± 12.7 | .002 |
COVID-19 = coronavirus disease 2019, DBP = diastolic blood pressure, SBP = systolic blood pressure.
A statistically significant change was also observed in hypertension severity categories. The proportion of patients with severe hypertension (SBP ≥ 180 mm Hg) decreased from 70.7% before the pandemic to 66.1% during the pandemic, while cases of mild and moderate hypertension increased slightly (P = .046), indicating that more patients were attended by EMTs with lower blood pressure levels during the pandemic.
In terms of blood pressure measurements, the mean initial SBP was significantly higher before the pandemic (189.85 mm Hg) than during the pandemic (185.57 mm Hg, P < .001). Mean DBP also decreased significantly during the pandemic (P = .003). After EMT intervention, mean control SBP and DBP were likewise lower during the pandemic (P < .001 and P = .002, respectively), as shown in Table 1.
3.2. Medication administration and EMT transport decisions
The Analysis of pharmacological interventions revealed no statistically significant changes in the administration rates of captopril (P = .089) or furosemide (P = .210). However, a significant increase was observed in the administration of hydroxyzine, rising from 38.2% before the pandemic to 45.1% during the pandemic (P = .003), indicating a greater focus on managing anxiety-related symptoms (Table 2).
Table 2.
Medication administration and EMT transport decisions before and during the COVID-19 pandemic.
| Variable | Before COVID-19 (N = 936) | During COVID-19 (N = 859) | P-value |
|---|---|---|---|
| Captopril (Administered), n (%) | 573 (61.2%) | 560 (65.2%) | .089 |
| Furosemide (Administered), n (%) | 400 (42.7%) | 379 (44.1%) | .210 |
| Hydroxyzine (Administered), n (%) | 358 (38.2%) | 387 (45.1%) | .003 |
| Left at the Scene, n (%) | 584 (62.4%) | 654 (76.1%) | <.001 |
| Transported to ED, n (%) | 352 (37.6%) | 205 (23.9%) |
COVID-19 = coronavirus disease 2019, ED = emergency department, EMTs = emergency medical teams.
EMT transport decisions also changed significantly during the pandemic. The proportion of patients left at the scene increased from 62.4% to 76.1%, while the number of patients transported to EDs decreased accordingly (P < .001). This suggests a strategic shift in prehospital management to reduce unnecessary hospital exposure during the COVID-19 crisis (Table 2).
3.3. Two-way ANOVA: impact of period and SBP on EMT transport decisions
A two-way ANOVA was conducted to examine the effect of the pandemic period (before vs during COVID-19) and SBP level (initial and control SBP) on EMT transport decisions (transported to ED vs left at the scene).
3.3.1. Initial SBP
The A two-way ANOVA revealed that there was a statistically significant interaction between the effects of pandemic period and EMT transport decision on initial SBP (F(1, 1791) = 4.11, P = .043).
Simple main effects analysis showed that the pandemic period had a statistically significant effect on initial SBP (F(1, 1791) = 10.21, P = .001), with lower initial SBP during the pandemic.
EMT transport decision also had a significant main effect (F(1, 1791) = 81.36, P < .001), with higher initial SBP observed among patients who were transported to the ED compared to those left at the scene.
3.3.2. Controlled SBP
A similar pattern was observed for control SBP. A two-way ANOVA revealed a significant interaction between pandemic period and EMT transport decision (F(1, 1138) = 7.61, P = .006).
Simple main effects analysis showed that the pandemic period had a statistically significant effect on control SBP (F(1, 1138) = 9.02, P = .003), with lower post-intervention SBP during the pandemic.
EMT transport decision also significantly influenced control SBP (F(1, 1138) = 357.93, P < .001), with lower values in patients left at the scene than in those transported to the ED.
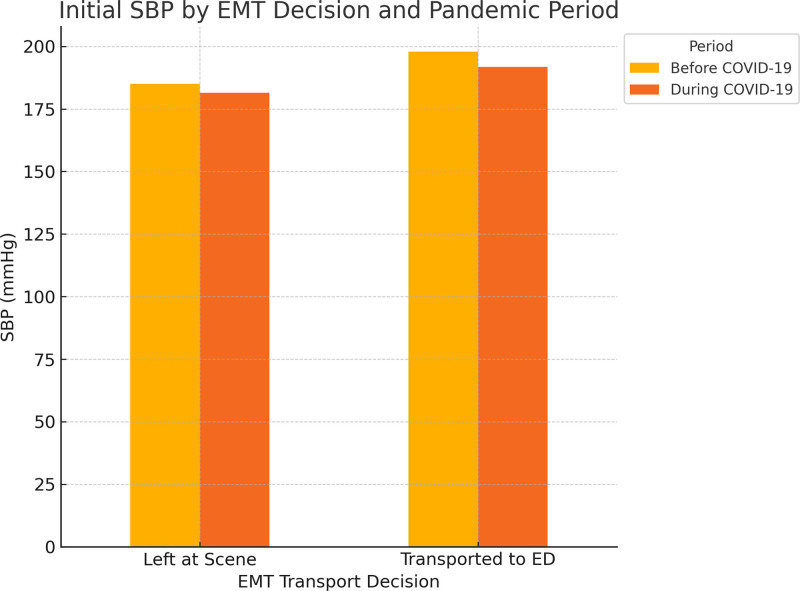
Descriptive statistics for these comparisons are presented in Table 3 and visualized in Figure 1.
Table 3.
Mean SBP Values by EMT transport decision and pandemic period (two-way ANOVA results).
| SBP type | Period | EMT decision | Mean ± SD |
|---|---|---|---|
| Initial SBP | Before COVID-19 | Left at the scene | 184.98 ± 21.70 |
| Transported to ED | 197.93 ± 26.33 | ||
| During COVID-19 | Left at the scene | 181.45 ± 20.5 | |
| Transported to ED | 191.81 ± 24.2 | ||
| Control SBP | Before COVID-19 | Left at the scene | 151.54 ± 16.08 |
| Transported to ED | 179.57 ± 25.72 | ||
| During COVID-19 | Left at the scene | 149.12 ± 15.3 | |
| Transported to ED | 172.12 ± 22.3 |
COVID-19 = coronavirus disease 2019, ED = emergency department, EMTs = emergency medical teams, SBP = systolic blood pressure.
Figure 1.
Initial SBP levels by EMT transport decision and pandemic period. This figure illustrates the differences in SBP levels recorded by EMTs before and during the COVID-19 pandemic. SBP values are displayed based on EMT transport decisions, comparing patients who were left at the scene versus those transported to the ED. The figure highlights a significant shift in SBP levels across both transport groups, reflecting changes in prehospital hypertension management during the pandemic. COVID-19 = coronavirus disease 2019, ED = emergency department, EMT = emergency medical team, SBP = systolic blood pressure.
4. Discussion
This study aimed to evaluate the impact of the COVID-19 pandemic on the prehospital management of hypertension by EMTs. By comparing data from the pre-pandemic and pandemic periods, several key findings emerged. First, the overall frequency of hypertension-related emergency calls remained stable, suggesting that the need for emergency hypertension care persisted despite healthcare disruptions. Second, while gender distribution remained unchanged, there were notable shifts in patient age, with a greater proportion of younger individuals seeking EMT interventions during the pandemic. Third, initial SBP was lower during the pandemic, and a higher proportion of patients presented with lower blood pressure categories. Fourth, the administration of hydroxyzine significantly increased, indicating a greater focus on managing anxiety-related symptoms. Finally, fewer patients were transported to hospitals, reflecting adaptations in EMT triage and decision-making to minimize hospital exposure and optimize resource allocation.
The stable frequency of hypertension-related emergency calls suggests that hypertension remained a persistent and urgent condition requiring EMT intervention, despite pandemic-related healthcare disruptions. This finding aligns with studies conducted in the United States, where the number of hypertension-related ED visits remained stable throughout the pandemic.[15] However, while the overall call volume remained unchanged, it is possible that individual healthcare-seeking behaviors shifted. In particular, older adults, who were at higher risk of severe COVID-19 outcomes, may have been more hesitant to seek emergency care due to fear of infection, leading to a relative increase in younger patients requiring EMT assistance. This aligns with findings from previous research, which indicated that older populations delayed or avoided medical visits during the pandemic.[16] The absence of significant sex-related differences in EMT calls may suggest that both men and women were equally affected by pandemic-related stressors and access limitations, a finding that contrasts with studies reporting gender disparities in healthcare utilization during the pandemic. Future research should explore potential differences in health-seeking behaviors between men and women during public health crises.
A significant shift in blood pressure levels and hypertension severity was observed during the pandemic. Specifically, initial SBP values recorded by EMTs were lower compared to the pre-pandemic period. This is somewhat unexpected, as delays in healthcare-seeking behavior and elevated psychological stress – both common during the pandemic – would typically be associated with increased SBP at the time of emergency intervention. However, a concurrent rise in cases involving mild to moderate hypertension (SBP 140–179 mm Hg) and a decrease in severe hypertension (SBP ≥ 180 mm Hg) suggest that EMTs were dispatched more frequently to patients with less critical blood pressure levels. One possible explanation is that pandemic-related changes in EMT dispatch protocols broadened the scope of emergency responses, allowing for earlier intervention. Additionally, individuals may have sought help at earlier stages due to heightened anxiety and increased public awareness of health risks. While previous studies have linked social isolation, financial pressure, and stress-induced hypertension to worsening cardiovascular outcomes,[17,18] the pattern observed here suggests that EMTs encountered a wider clinical spectrum of hypertension during the pandemic. These findings are consistent with international reports indicating a similar shift in patient severity levels during emergency responses[19] and highlight the need for further research into how such prehospital triage adaptations may affect long-term patient outcomes.
The increased administration of hydroxyzine, an anxiolytic medication, during EMT interventions highlights the growing recognition of psychological distress as a factor in emergency hypertension management. This trend aligns with broader findings indicating a surge in anxiolytic and antidepressant prescriptions during the pandemic, suggesting that stress and anxiety played a significant role in cardiovascular health deterioration.[20] The psychological burden of the pandemic – driven by social isolation, financial instability, and fear of infection – has been widely documented as a contributor to worsening hypertension control.[21] The stable use of captopril and furosemide suggests that core antihypertensive management strategies remained unchanged, with EMTs adapting primarily by incorporating additional anxiolytic treatment to address pandemic-related stress responses. These findings underscore the importance of integrating mental health support into emergency hypertension management protocols, particularly during global health crises.
A major change observed in this study was the shift in EMT transport decisions during the pandemic. EMTs were more likely to leave patients at the scene rather than transport them to EDs, with the proportion of non-transported patients rising from 62.4% before the pandemic to 76.1% during the pandemic. This shift likely reflects efforts to reduce hospital exposure risks, manage ED capacity, and implement updated triage protocols. When comparing patients left at the scene, mean initial and control SBP values were slightly lower during the pandemic (184.98 mm Hg vs 181.45 mm Hg initial SBP; 151.54 mm Hg vs 149.12 mm Hg control SBP), indicating a trend toward attending to patients with less severe hypertension outside of the hospital. Similarly, among patients transported to the ED, both initial and control SBP values decreased during the pandemic (197.93 mm Hg vs 191.81 mm Hg initial SBP; 179.57 mm Hg vs 172.12 mm Hg control SBP), suggesting a broader shift in EMT intervention thresholds. These changes are consistent with findings from other countries where emergency medical systems adapted their care strategies during the pandemic to accommodate shifting resource availability and patient risk levels.[22–24] The observed reductions in SBP within each transport category highlight how EMTs responded to evolving demands while continuing to manage hypertensive patients effectively in both prehospital and hospital-directed care pathways.
Additionally, analysis of the interaction between SBP levels, the pandemic period, and EMT transport decisions provided further insights into emergency care adaptations. Before the pandemic, patients transported to the ED had significantly higher initial SBP compared to those left at the scene. During the pandemic, while this trend persisted, overall SBP values were lower. This suggests that EMTs continued to use SBP severity as a key determinant for hospital transport but may have adjusted hospitalization thresholds based on evolving healthcare constraints. A similar pattern was observed in controlled SBP levels, where EMT-administered interventions resulted in significant reductions in posttreatment SBP, particularly for patients transported to the ED. These changes likely reflect modifications in EMT triage criteria, allowing a broader range of hypertensive patients to be managed on-site rather than being sent to the hospital. This aligns with global efforts to enhance prehospital care and minimize unnecessary hospital visits during the pandemic.[25] Figure 1 provides a visual representation of these interaction effects, illustrating the shift in SBP levels across different EMT decisions before and during the pandemic.
The findings of this study contribute to the growing body of evidence on emergency medical service adaptations during global health crises, reinforcing the need for resilient, data-driven policies that ensure continuity of care for chronic conditions even during periods of extreme healthcare disruption.
5. Strengths and limitations
This study has several notable strengths. It is among the first to comprehensively evaluate hypertension management by EMTs before and during the COVID-19 pandemic, utilizing real-world emergency intervention data. The large dataset ensures robust statistical power, allowing for the identification of significant trends in prehospital hypertension care. Additionally, this study provides detailed insights into EMT transport decisions and pharmacological interventions, aspects that are often overlooked in emergency hypertension research.
Another strength is the inclusion of interaction analyses between SBP levels, EMT decisions, and the pandemic period, offering a nuanced understanding of how emergency care adapted under crisis conditions. These findings contribute to a broader understanding of prehospital emergency system adaptations and underscore the importance of ensuring continuity of care for chronic conditions during public health crises. Future research should expand data collection across multiple regions, incorporate longer follow-up periods, and integrate patient outcomes into the analysis to further assess the impact of these adaptations.
Despite these strengths, the study has some limitations that should be acknowledged. Firstly, the retrospective design relies on existing medical records, which may not capture all relevant details or may contain inconsistencies. The quality of data was dependent on the accuracy of EMT documentation, which could have led to over- or underestimation of findings in cases where subjectivity influenced reporting. However, this limitation was mitigated by applying strict inclusion criteria, ensuring that only complete and verifiable medical records were analyzed.
Another limitation is the variability in data completeness across cases. While blood pressure measurements were recorded, the precise timing of these measurements relative to interventions was inconsistent, which may affect comparisons. Additionally, comorbidities and long-term patient outcomes were not systematically documented, limiting the ability to assess broader health implications beyond emergency care. Future studies should incorporate prospective designs with standardized data collection to improve consistency.
Differences in EMT documentation practices represent another limitation. Variability in experience, training, and workload could have introduced information bias, affecting how therapeutic actions and clinical decisions were recorded. This variability may have resulted in underreporting or misclassification of treatment details. Future research should consider standardized EMT reporting protocols and digital documentation systems to enhance data accuracy.
The regional focus on southeastern Poland also limits the study’s generalizability. While the findings provide insights into local EMT adaptations, they may not fully apply to healthcare systems with different infrastructures and emergency response strategies. Expanding future studies to multiple regions with diverse healthcare models would improve the generalizability of findings.
6. Conclusions
Despite the challenges of the COVID-19 pandemic, the demand for EMT interventions in hypertension remained unchanged. However, the findings highlight important shifts in EMT protocols, including expanded on-site care, increased use of anxiolytics, and reduced hospital transports. These adaptations reflect a broader evolution in emergency care strategies, underscoring the need for flexible response systems. Continued development of EMT procedures is essential to ensure safe and effective prehospital care during future public health emergencies.
7. Recommendations for future emergency medical practices
Building on the study findings, we propose the following recommendations to enhance emergency medical responses for chronic conditions in future public health crises. This study reinforces the growing body of evidence that emergency medical services must adopt resilient, data-driven strategies to ensure continuity of care – even during large-scale disruptions such as the COVID-19 pandemic.
To support this goal, we outline 5 key areas for improvement:
-
Enhancing Adaptive Emergency Protocols
Healthcare systems should develop flexible protocols that allow EMTs to effectively manage chronic conditions like hypertension during crises while minimizing unnecessary hospital admissions.
-
Strengthening Prehospital Care and Training
Expanding EMT training programs in the management of hypertensive emergencies and integrating mental health support strategies could improve patient outcomes and reduce pressure on EDs.[26–28]
-
Longitudinal Research on Emergency Adaptations
Investigating the long-term effects of pandemic-driven adaptations on patient care and health outcomes would help refine prehospital treatment strategies.[29,30]
-
Addressing Psychological Factors in Hypertension Management
Given the increased use of anxiolytics during the pandemic, further studies should explore the psychological burden of crises on chronic disease patients and its influence on healthcare-seeking behaviors.
-
Optimizing Patient Transport Decision Frameworks
Future research should assess the impact of modified EMT triage decisions on patient safety and healthcare system efficiency, ensuring that on-site management strategies remain evidence-based and effective.
By implementing these strategies, emergency medical systems can enhance their preparedness for future public health emergencies, ensuring that chronic disease patients receive timely, high-quality care, regardless of external pressures.
Acknowledgments
The authors would like to extend their appreciation to King Saud University for funding this work through the Researchers Supporting Project number (RSPD2025R649), King Saud University, Riyadh, Saud Arabia.
Author contributions
Conceptualization: Adrian Moskal.
Data curation: Adrian Moskal, Karolina Żak-Kowalska.
Formal analysis: Sebastian Kowalski.
Methodology: Sebastian Kowalski, Karolina Żak-Kowalska.
Supervision: Mariusz Goniewicz.
Validation: Ahmed M. Al-Wathinani, Mariusz Goniewicz.
Writing – original draft: Adrian Moskal, Sebastian Kowalski, Karolina Żak-Kowalska, Ahmed M. Al-Wathinani, Krzysztof Goniewicz, Mariusz Goniewicz.
Writing – review & editing: Ahmed M. Al-Wathinani, Krzysztof Goniewicz.
Abbreviations:
- COVID-19
- coronavirus disease 2019
- DBP
- diastolic blood pressure
- ED
- emergency department
- EMTs
- emergency medical teams
- SBP
- systolic blood pressure
Ethical approval for this research was granted by the Bioethics Committee of the Medical University of Lublin (decision number: KE-0254/150/06/2022).
The authors have no funding and conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
How to cite this article: Moskal A, Kowalski S, Żak-Kowalska K, Al-Wathinani AM, Goniewicz K, Goniewicz M. The impact of the COVID-19 pandemic on hypertension management in southeastern Poland: Challenges and adaptations for emergency medical teams. Medicine 2025;104:19(e42416).
Contributor Information
Adrian Moskal, Email: amoskal.medicine@gmail.com.
Sebastian Kowalski, Email: skowalski.medicine@icloud.com.
Karolina Żak-Kowalska, Email: zak.karolinajagoda@icloud.com.
Ahmed M. Al-Wathinani, Email: ahmalotaibi@ksu.edu.sa.
Mariusz Goniewicz, Email: mariusz.goniewicz@umlub.pl.
References
- [1].Zhou B, Perel P, Mensah GA, Ezzati M. Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nat Rev Cardiol. 2021;18:785–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Adelowo AB. A scoping review of cardio metabolic syndrome: a critical step in mitigating the rising global burden of cardiovascular diseases and diabetes mellitus. Int J Diabetes Metab Disorders. 2022;7:80–6. [Google Scholar]
- [3].Sola J, Cortes M, Perruchoud D, et al. Guidance for the interpretation of continual cuffless blood pressure data for the diagnosis and management of hypertension. Front Med Technol. 2022;4:899143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Goniewicz K, Khorram-Manesh A, Hertelendy AJ, Goniewicz M, Naylor K, Burkle FM, Jr. Current response and management decisions of the European Union to the COVID-19 outbreak: a review. Sustainability. 2020;12:3838. [Google Scholar]
- [5].Bisht R, Saharia R, Sarma J. COVID-19 and the burden of ill-health: a double crisis of disruptions and inequalities. J Soc Econ Devel. 2021;23(Suppl 2):342–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Goniewicz K, Khorram-Manesh A. Maintaining social distancing during the COVID-19 outbreak. Soc Sci. 2021;10:14. [Google Scholar]
- [7].Bress AP, Cohen JB, Anstey DE, et al. Inequities in hypertension control in the United States exposed and exacerbated by COVID‐19 and the role of home blood pressure and virtual health care during and after the COVID‐19 pandemic. J Am Heart Assoc. 2021;10:e020997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Moore JT, Pilkington W, Kumar D. Diseases with health disparities as drivers of COVID‐19 outcome. J Cell Mol Med. 2020;24:11038–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Hayanga B, Stafford M, Bécares L. Ethnic inequalities in multiple long-term health conditions in the United Kingdom: a systematic review and narrative synthesis. BMC Public Health. 2023;23:178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Goniewicz M, Włoszczak-Szubzda A, Al-Wathinani AM, Goniewicz K. Resilience in emergency medicine during COVID-19: evaluating staff expectations and preparedness. J Personalized Med. 2023;13:1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Al-Wathinani A, Hertelendy AJ, Alhurishi S, et al. Increased emergency calls during the COVID-19 pandemic in Saudi Arabia: a national retrospective study. Healthcare (Basel, Switzerland). 2020;9:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Hick JL, Hanfling D, Wynia MK, Pavia AT. Duty to plan: health care, crisis standards of care, and novel coronavirus SARS-CoV-2. Nam Perspect. 2020;2020:10.31478/202003b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Celik M, Yilmaz Y, Karagoz A, et al. Anxiety disorder associated with the COVID-19 pandemic causes deterioration of blood pressure control in primary hypertensive patients. Medeniyet Med J. 2021;36:83–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].de Miranda AS, Macedo DS, Rocha NP, Teixeira AL. Targeting the renin-angiotensin system (RAS) for neuropsychiatric disorders. Curr Neuropharmacol. 2024;22:107–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Giannouchos TV, Biskupiak J, Moss MJ, Brixner D, Andreyeva E, Ukert B. Trends in outpatient emergency department visits during the COVID-19 pandemic at a large, urban, academic hospital system. Am J Emerg Med. 2021;40:20–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Kreutz R, Dobrowolski P, Prejbisz A, et al. Lifestyle, psychological, socioeconomic and environmental factors and their impact on hypertension during the coronavirus disease 2019 pandemic. J Hypertens. 2021;39:1077–89. [DOI] [PubMed] [Google Scholar]
- [17].Catucci A, Scognamiglio U, Rossi L. Lifestyle changes related to eating habits, physical activity, and weight status during COVID-19 quarantine in Italy and some European countries. Front nutr. 2021;8:718877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Fagan HA, Baldwin DS. Pharmacological treatment of generalised anxiety disorder: current practice and future directions. Expert Rev Neurother. 2023;23:535–48. [DOI] [PubMed] [Google Scholar]
- [19].Hussey LJ, Kontopantelis E, Mok PL, et al. Socio‐demographic variation in diagnosis of and prescribing for common mental illnesses among children and young people during the COVID‐19 pandemic: time series analysis of primary care electronic health records. J Child Psychol Psychiatry. 2025;66:16–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Leistner C, Menke A. Hypothalamic–pituitary–adrenal axis and stress. Handbook Clin Neurol. 2020;175:55–64. [DOI] [PubMed] [Google Scholar]
- [21].Wu Q, Xu Z, Song S, et al. Gut microbiota modulates stress-induced hypertension through the HPA axis. Brain Res Bull. 2020;162:49–58. [DOI] [PubMed] [Google Scholar]
- [22].Birkmeyer JD, Barnato A, Birkmeyer N, Bessler R, Skinner J. The impact of the COVID-19 pandemic on hospital admissions in the United States: study examines trends in US hospital admissions during the COVID-19 pandemic. Health Affairs (Project Hope). 2020;39:2010–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Minuz P, Albini FL, Imbalzano E, et al. Telemedicine and digital medicine in the clinical management of hypertension and hypertension-related cardiovascular diseases: a position paper of the Italian Society of Arterial Hypertension (SIIA). High Blood Pressure Cardiovasc Prevent. 2023;30:387–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Dale CE, Takhar R, Carragher R, et al. The adverse impact of COVID-19 pandemic on cardiovascular disease prevention and management in England, Scotland and Wales: a population-scale analysis of trends in medication data. Medrxiv. 2022;2021:12 [Google Scholar]
- [25].Fridell M, Edwin S, Von Schreeb J, Saulnier DD. Health system resilience: what are we talking about? A scoping review mapping characteristics and keywords. Int J Health Policy Manag. 2020;9:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Lerner EB, Newgard CD, Mann NC. Effect of the coronavirus disease 2019 (COVID‐19) pandemic on the US emergency medical services system: a preliminary report. Acad Emerg Med. 2020;27:693–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Chauhan P, Bali A, Kaur S. Breaking barriers for accessible health programs: the role of telemedicine in a global healthcare transformation. In Transformative Approaches to Patient Literacy and Healthcare Innovation 2024. IGI Global: 283–307. [Google Scholar]
- [28].Goniewicz K, Khorram-Manesh A, Burkle FM, Hertelendy AJ, Goniewicz M. The European Union’s post-pandemic strategies for public health, economic recovery, and social resilience. Global Transitions. 2023;5:201–9. [Google Scholar]
- [29].Khorram-Manesh A, Goniewicz K, Burkle FM, Jr. Unleashing the global potential of public health: a framework for future pandemic response. J Infect Public Health. 2024;17:82–95. [DOI] [PubMed] [Google Scholar]
- [30].Goniewicz K, Burkle FM, Khorram-Manesh A. Transforming global public health: climate collaboration, political challenges, and systemic change. J infect public health. 2025;18:102615. [DOI] [PubMed] [Google Scholar]