Abstract
Background
Tumours of the parasellar area may engulf the internal carotid artery(ICA) and its branches which may preclude complete resection and may be a risk factor for ischemic complications.
Methods
We present a surgical technique based on a stepwise identification of the arterial branches which may enable a complete resection in selected cases even when complete encasement of the ICA is present on preoperative images.
Conclusion
Resection of tumours encasing the major vascular structures should be systematically attempted while continuously weighing the delicate balance between the risk of vascular injury and the extent of resection.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00701-025-06502-x.
Keywords: Parasellar area, Meningioma, Anterior clinoid, Cavernous sinus
The parasellar region is a complex anatomical area which contains many critical vascular and nervous structures in a very confined space. Due to this close proximity, lesions emerging from the parasellar region render those structures vulnerable to displacement or encasement.
Clinoidal and cavernous sinus meningiomas represent therefore a significant surgical challenge as they imply a high risk of vascular injury. Vascular encasement is a proved risk factor for ischemic complications in sphenoid wing meningiomas [5]. Possible predictive factors for the absence of arachnoid planes in vascular encasement have been described such as vascular narrowing and peritumoral T2 brain edema [1, 3].
We present our surgical technique for the management of vascular encasement in parasellar meningiomas.
Relevant surgical anatomy [6]
In a simplified representation, the parasellar region serves as a pivotal anatomical crossroad for structures of significance, mainly the anterior clinoid process, the optic nerve and the ICA.
The anterior clinoid process is continuous anteriorly with the lesser wing of the sphenoid bone and is medially attached to the body of the sphenoid bone by the anterior root which forms the roof of the optic canal. and the posterior root or the optic strut which separates the optic canal from the superior orbital fissure.
The optic canal contains the ophthalmic artery and the optic nerve, which travels medially to the internal carotid artery to join the contralateral nerve and form the optic chiasm. The superior orbital fissure(SOF) contains the oculomotor nerves and branches of the trigeminal nerve.
The supraclinoid portion of the internal carotid artery courses along the medial side of the anterior clinoid process and below the optic nerve to reach the lateral side of the optic chiasm, bifurcating at the medial end of the sylvian fissure to then give rise to the anterior (ACA) and middle cerebral artery(MCA). During its course, perforators and branches arise from the supraclinoid segment of the internal carotid artery:
the ophthalmic artery, running under and anterolaterally the optic nerve to enter the optic canal.
the superior hypophyseal arteries passing medially below the chiasm toward the tuber cinereum.
the posterior communicating artery(PComA), forming the lateral boundary of the circle of Willis and running slightly above and medial to the oculomotor nerve to reach the posterior cerebral artery(PCA).
the anterior choroidal artery(AChA) coursing along the optic tract towards the choroidal fissure.
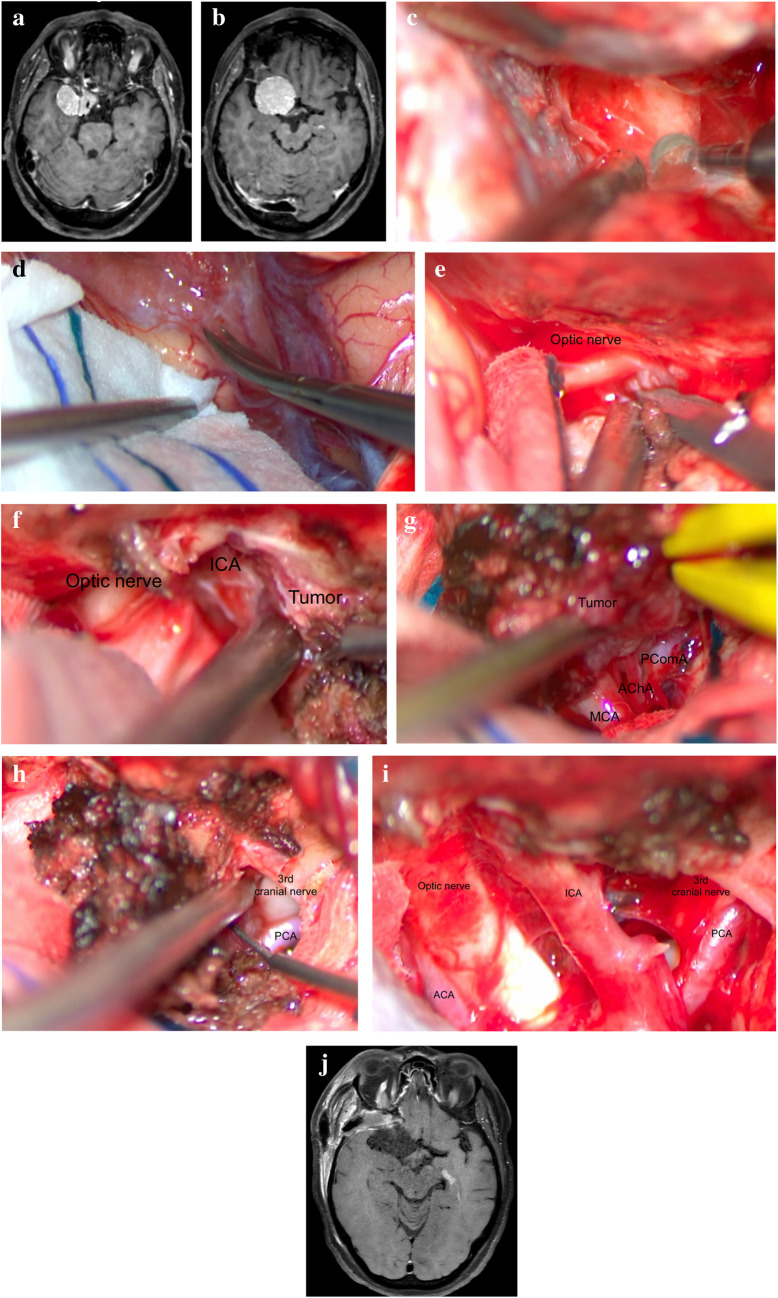
Description of the technique (Fig. 1)
Fig. 1.
a Preoperative Gadolinium enhanced T1 Magnetic Resonance Imaging(MRI) showing a right anterior clinoidal meningioma encasing the supraclinoid ICA. b Preoperative Gadolinium enhanced T1 Magnetic Resonance Imaging(MRI) showing a right anterior clinoidal meningioma encasing the supraclinoid ICA. c Drilling of the right optic canal. d Opening of the right sylvian fissure. e Decompression of the right optic nerve. f Dissection of the supraclinoid ICA. g Dissection of the MCA, PComA and AChA. h Dissection of the PCA and of the third cranial nerve. i Final view at the end of the resection. j Postoperative Gadolinium enhanced T1 (MRI) showing a complete resection of the tumour
-
Positioning:
The patient is positioned supine with the head fixed in a Mayfield with 10–20 degrees of rotation towards the contralateral side of the lesion and the head tilted towards the lesion. Head extension will facilitate a retractorless surgery. Too much head rotation should be avoided in order to preserve a good mental anatomic representation.
-
Choice of approach:
An extended pterional approach associated to a postero-lateral orbitotomy will provide a good access to most parasellar lesions. An orbito pterional or frontotemporal-orbitozygomatic approach may be needed in case of extensive superior development of the tumour.
Extensive drilling of the orbital roof and sphenoid ridge will realise a postero-lateral orbitotomy and allow the exposure of the SOF, the section of the orbito-temporal meningeal band and the peeling of the lateral wall of the cavernous sinus. The last two steps are paramount in order to avoid inadvertent entering the cavernous sinus which could engender neuro vascular lesions.
-
Extradural anterior clinoidectomy and opening of the optic canal [4, 7]
Clinoid pneumatization and the presence of a carotid foramen should be assessed on the pre-operative images.
-
After dural opening, the sylvian fissure and the basal arachnoid cisterns are largely opened.
This manoeuvre allows an early identification of the MCA and a retractorless surgery through dynamic retraction.
Sub-frontal tumour debulking and identification of the optic nerve. The frontal sector of the tumour is the less dangerous. Debulking and dissection should be started in this area. Opening of the falciform ligament and of the optic nerve sheath which may be infiltrated by the tumour allows the identification of the optic nerve and sub sequentially of the ICA at the distal dural ring.
-
Identification of the encased arteries
The arteries should be identified at their enter and exit points. Starting in a retrograde manner, from distal to proximal, might sometimes be easier. The origins of the PcomA and the AchA should be approached carefully as they are often areas of very strong adhesion.
-
Bleeding tolerance
Some bleeding should be tolerated, especially in the area posterior to the ICA and toward the oculomotor triangle until the identification of the AchA, the PcomA and the third cranial nerve. Coagulation should be avoided until all vascular and nervous elements are clearly identified.
-
Tumour sectoring
Tumour sectors [2] should be mentally created and serve as landmarks in order to proceed from known to unknown and from safe to dangerous. Safe triangles are sequentially created as the dissection advances and more anatomical elements are identified.
Indications
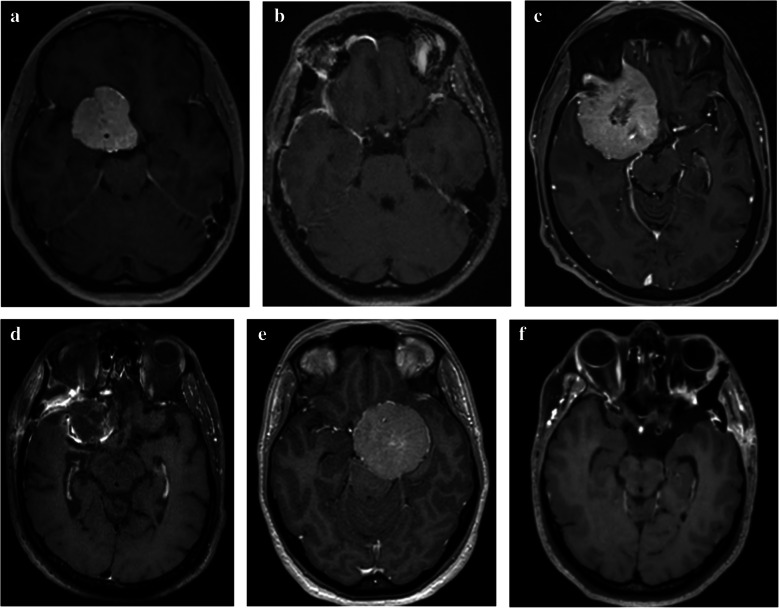
Anterior clinoidal, cavernous sinus and sphenoid wing meningiomas with vascular encasement (Fig. 2).
Fig. 2.
a Preoperative Gadolinium enhanced T1(MRI) showing a right anterior clinical meningioma encasing the supraclinoid ICA. b Postoperative Gadolinium enhanced T1(MRI) showing complete resection of the tumour depicted in Fig. 2a and preservation of the ICA. c Preoperative Gadolinium enhanced T1(MRI) showing a right anterior clinical meningioma encasing the supraclinoid ICA. d Postoperative Gadolinium enhanced T1(MRI) showing complete resection of the tumour depicted in Fig. 2c and preservation of the ICA. e Preoperative Gadolinium enhanced T1(MRI) showing a right cavernous sinus meningioma encasing the supraclinoid ICA. f Postoperative Gadolinium enhanced T1(MRI) showing complete resection of the supratentorial part of the tumour depicted in Fig. 2f and preservation of the ICA
Limitations
Complete surgical resection might not be possible in case of invasion of the vascular adventitia. It is preferable to leave a residue than to create an irreversible neurological deficit.
How to avoid complications
Neuronavigation identification of the encased arteries should be used cautiously and constantly balanced against anatomic landmarks as even a small shift may have catastrophic consequences. Doppler probes might be more reliable for locating encased vascular elements.
Some bleeding should be tolerated until a clear identification of the encased vascular components especially in the supra carotid and retrocarotid sectors o the tumor.
Specific perioperative considerations
Preoperative MRI should be carefully analysed in order to have a clear representation of the lesion and its relationship with the main neurovascular structures.
There are no reliable predictors for the release of encased arteries, but hyper T2 signal of the meningiomas seem to be more favourable for dissection of encased vessels as it predicts a softer lesion.
Specific information to give to the patient about surgery and potential risks
The patient should be informed about the infectious, haemorrhagic and neurological risks.
Key points
Excessive head rotation may disturb the mental representation of the tumor and ‘hide’ the medial neurovascular elements.
Postero-lateral orbitotomy enhances the exposure of the tumor and may avoid the necessity of more extensive osteotomies.
Extradural anterior clinoidectomy allows an early devascularisation of the tumor, decompression of the optic nerve and location of the supraclinoid ICA.
Extensive dissection of the sylvian fissure and arachnoid cisterns.
Sub frontal tumour debulking and identification of the optic nerve, of the ICA and its branches and the 3rd cranial nerve.
Identification of the entry and exit points in the tumor of the ACA, MCA, PComA, AchA.
Tolerate bleeding in the retrocarotid and supra carotid spaces until all vascular and nervous elements have been identified.
T2 hypersignal of the tumor may better predict the chances of freeing the encased vascular elements in our experience.
Vasospasm is possible after extensive vascular dissection. Local use of papaverine and mild postoperative hypertension may mitigate this risk.
It is better to hurt your ego than your patient. A small residue is preferable to an irreversible neurological deficit.
Conclusions
Parasellar meningiomas with vascular encasement represent a great surgical challenge. As no reliable predictive factors for the release of encased arteries have been described, a cautious dissection should be attempted in all cases. Avoiding complications requires a rigorous anatomical knowledge and a meticulous surgical approach.
Supplementary Information
Below is the link to the electronic supplementary material.
Abbreviations
- ICA
Internal carotid artery
- ACA
Anterior cerebral artery
- MCA
Middle cerebral artery
- SOF
Superior orbital fissure
- PCA
Posterior cerebral artery
- PComA
Posterior communicating artery
- AChA
Anterior choroidal artery
Authors’ contributions
S.A. and F.H. acquired and analysed the data. All authors drafted, reviewed and approved the manuscript. Dr Sorin Aldea and Dr Floriana Halimi equally contributed as first co-authors.
S.A, F.H and C.LG drafted, reviewed and approved the manuscript.
Dr Sorin Aldea and Dr Floriana Halimi equally contributed as first co-authors.
Funding
Not applicable.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was conducted in accordance with the guidelines of the Declaration of Helsinki and did not require approval from our Institutional Review Board.
Consent to participate
Written informed consent was obtained from all patients.
Consent for publication
Written informed consent was obtained from all patients.
Conflicts of interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Dhandapani S, Negm HM, Cohen S, Anand VK, Schwartz TH (2015) Endonasal endoscopic transsphenoidal resection of tuberculum Sella meningioma with anterior cerebral artery encasement. Cureus 25 7(8):e311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hendricks BK, Benet A, Lawrence PM, Benner D, Preul MC, Lawton MT (2022) Anatomical triangles for use in skull base surgery: a comprehensive review. World Neurosurg 164:79–92 [DOI] [PubMed] [Google Scholar]
- 3.Kim BW, Kim MS, Kim SW, Chang CH, Kim OL (2011) Peritumoral brain edema in Meningiomas : correlation of radiologic and pathologic features. J Korean Neurosurg Soc 49(1):26–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lemberg J, Krieg SM, Meyer B (2014) Anterior clinoidectomy. Acta Neurochir 156:415–419 [DOI] [PubMed] [Google Scholar]
- 5.McCracken DJ, Higginbotham RA, Boulter JH, Liu Y, Wells JA, Halani SH, Saindane AM, Oyesiku NM, Barrow DL, Olson JJ (2017) Degree of vascular encasement in sphenoid wing Meningiomas predicts postoperative ischemic complications. Neurosurgery 80(6):957–966 [DOI] [PubMed] [Google Scholar]
- 6.Rhoton AL Jr (2002) The supratentorial arteries. Neurosurgery 51(4Suppl):S53-120 [PubMed] [Google Scholar]
- 7.Troude L, Bernard F, Bauchet G, De La Rosa MS, Roche PH (2017) Extradural resection of the anterior clinoid process: How I do it. Neurochirurgie 63(4):336–340 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.