ABSTRACT
Objective
To investigate the nature and availability of evidence on the clinical performance of posterior partial coverage restorations (PCR) fabricated from different ceramic materials, outcome definitions, measurement methods, study drop‐outs and follow ups.
Overview
A systematic literature search (inception‐February 2024) was performed through MEDLINE, Scopus, CENTRAL, ClinicalTrials.gov, and the International Clinical Trials Registry Platform to identify clinical studies with a focus on posterior PCRs (onlays, occlusal veneers and partial crowns) with a minimum follow‐up of 1 year. Thirteen of 31 included studies were randomized controlled trials (RCT) and 18 non‐randomized studies of intervention (NRS). Six RCTs compared two different ceramic materials and might be suitable for meta‐analysis. Differences in study design, definition of survival, evaluation methods, and statistical models for survival analysis were identified as reasons for expected heterogeneity among studies. The most common reasons for restoration failures were ceramic fractures and retention loss.
Conclusion
The evidence informing the effect of PCRs varied in definitions of survival and failure, complication classifications, and workflow approaches. RCTs addressing clinical performance of PCRs comparing different ceramic materials are available for conducting systematic reviews and meta‐analyses.
Keywords: ceramics, dental restoration failure, Onlays, partial crowns, survival
1. Introduction
With the evolution of digital technologies monolithic computer‐aided design–computer‐aided manufacturing (CAD‐CAM) materials fabricated from lithium disilicate (LDS), zirconia (Z), and resin matrix ceramics (RMC) were introduced in modern restorative dentistry [1]. Advancements in adhesive technologies fostered the evolution of novel, non‐retentive preparation designs for partial coverage ceramic restorations (PCR), avoiding retentive elements such as isthmus, proximal boxes, or additional circumferential shoulders [2, 3]. Adhesive PCRs can preserve more residual sound tooth structure compared with complete crowns [4]. However, differences among individual studies regarding the preparation design exist up to now [5].
The term “PCR” is an umbrella term to describe restorations with partial cusp coverage. The Glossary of Prosthodontic Terms (GPT10) defines an inlay as “a fixed intracoronal restoration; a dental restoration made outside of a tooth to correspond to the form of the prepared cavity, which is then luted into the tooth” [6]. Different terms have been developed to describe PCRs for the treatment of extended posterior tooth defects. Several authors used the classification by Veneziani [7] dividing these restorations into inlays without any cusp coverage, onlays with partial cusp coverage, and overlays with total cusp coverage. In contrast, the GPT10 defines an onlay as a PCR that restores one or more cusp by covering occlusal surfaces to the entire occlusal surface [6]. In recent years, the term “occlusal veneer” has been further introduced as a type of onlay that is characterized by a non‐retentive preparation design with reduced ceramic thickness [3]. For more extended tooth defects, the term partial coverage crown applies to PCRs that leave at least one or more axial surface uncovered [8].
Many variables affect the treatment success of PCRs, such as preparation design, geometry, properties of ceramic materials, bonding protocol, and occlusal forces [3]. Systematic reviews aim to understand the influence of these variables; however, they face challenges since high‐quality evidence on this topic is scarce [9, 10]. Available primary studies often provide unclear definitions of outcomes, different outcome measures, and a diversity of definitions for the preparation design and type of restoration, which limits the ability to draw sound and clinically relevant conclusions [10, 11, 12]. Most available systematic reviews do not use the Grades of Recommendation, Assessment, Development, and Evaluation approach (GRADE [13]), which prevents clinicians from understanding how much confidence to place in the reported treatment effects (i.e., desirable and undesirable outcomes). Additionally, many systematic reviews on this topic have not used optimal methodological techniques to obtain the best effect estimates to guide clinical decision‐making [12, 14].
The purpose of this scoping review was to investigate the nature and availability of evidence on the clinical performance of PCRs fabricated from different ceramic materials to treat extended posterior tooth defects, outcome definitions, measurement methods, study dropouts, and follow‐ups to guide the conduct of future systematic reviews.
2. Materials and Methods
2.1. Protocol and Registration
The study protocol was registered on Open Science Framework (OSF) and is retrievable at https://www.doi.org/10.17605/OSF.IO/8VU24.
2.2. Eligibility Criteria
The report of this review follows the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses extension for Scoping Reviews (PRISMA‐ScR) [15] statement. The review framework was defined as patients: Patients with extended tooth defects treated with PCRs on posterior teeth; interventions: Ceramic PCRs (Onlays, occlusal veneers, partial crowns [inlays were excluded]); outcomes: Survival, restoration failure, and complications of PCRs; and type of study: RCTs, prospective or retrospective observational studies with at least 1‐year follow‐up.
2.3. Research Questions
The following research questions were posed to guide the search:
What kind and amount of evidence is available investigating the survival, restoration failure, and complications of posterior PCRs fabricated from different ceramic materials?
Is the available body of evidence suitable for performing meta‐analysis comparing different ceramic materials, fabrication techniques, restoration designs, or restoration thicknesses?
2.4. Information Sources
According to Arksey and O'Malley [16], a wide definition of search terms was created to generate a broad coverage of the available evidence. A sensitive search strategy was developed by an experienced information scientist based on a text analysis of 10 relevant PubMed references known to the authors. The search was run from inception of each database to 19 February 2024 (date of last search for all databases) in the following databases and study registers: MEDLINE (via PubMed), the Cochrane Central Register of Controlled Trials (via Cochrane Library), Scopus, WHO International Clinical Trials Registry Platform and ClinicalTrials.gov without restrictions regarding language or publication type. Hand search of the reference lists of the included articles was performed additionally. Search strategies of included databases are presented in Table 1.
TABLE 1.
Search strategies of included databases.
| Search strategy | |
|---|---|
| MEDLINE via PubMed |
#1 crown*[tw] OR onlay*[tw] OR overlay*[tw] OR inlay*[tw] OR veneer*[tw] #2 “Dental Restoration, Permanent”[mh] OR restor*[tw] #3 “Dental Restoration Failure”[mh] OR “Survival Analysis”[mh] OR “Survival Rate”[mh] OR survival[tw] OR fractures[tw] #4 #1 AND #2 AND #3 = 5840 |
| Scopus (advanced search) | TITLE‐ABS‐KEY((crown* OR onlay* OR overlay* OR inlay* OR veneer*) AND restor* AND (failure OR survival OR fractures) AND (random* OR trial OR placebo OR groups) OR (cohort OR (control AND study) OR (control AND group*) OR {follow‐up} OR {follow up} OR {time factors} OR CI)) = 5609 |
| Cochrane Central Register of Controlled Trials (via Cochrane Library) |
|
| ClinicalTrials.gov | ((crown OR crowns OR onlay OR onlays OR overlay OR overlays OR inlay OR inlays OR veneer OR veneers) AND (restore OR restored OR restoring OR restoration OR restorations) AND (failure OR survival OR fractures)) = 219 |
| WHO ICTRP |
((crown* OR onlay* OR overlay* OR inlay* OR veneer*) AND (restor*) AND (failure OR survival OR fractures)) = 30 |
| 10 relevant PubMed records (PMIDs) used to develop the search strategy |
23342329[PMID] OR 26891618[PMID] OR 24600653[PMID] OR 28689915[PMID] OR 33012530[PMID] OR 22372380[PMID] OR 34415434[PMID] OR 34624421[PMID] OR 29214376[PMID] OR 32500864[PMID] |
2.5. Selection of Sources of Evidence
Reviewers participating in the screening process were calibrated to ensure optimal application of eligibility criteria. Two review authors (P.K. and S.P.) independently conducted title and abstract screening to identify studies that met the eligibility criteria (Table 2). Potentially eligible articles from the title and abstract screening were then evaluated using full texts (L.P. and S.P.). Any disagreement was resolved by discussion or by involving a third review author (P.G.).
TABLE 2.
Eligibility criteria.
| Inclusion criteria | Exclusion criteria |
|---|---|
|
|
2.6. Charting the Data
Data extraction was performed independently by two review authors (L.P. and S.P.). Variables for data extraction were: Study design, initial number of patients, final number of patients, number of drop‐outs, tooth vitality, restoration type, restoration material, preparation design and thickness, restoration thickness, workflow, follow‐up time, placed number of restorations, number of restorations in follow‐up, total number of failed units, total number of survived units, definition of survival rate, survival rate, type of statistical model, and different types of complications. Since the aim of this scoping review was to give an overview of the available evidence, a risk of bias analysis was not performed. This is in line with the methodologies proposed for scoping reviews [16, 17].
3. Results
3.1. Selection of Sources of Evidence
A total of 12,592 records were identified by the search. These were deduplicated using Deduklick [18] and resulted in 7,912 records, which were selected for title/abstract screening (Figure 1). 123 full‐text articles remained for full‐text screening, and 92 references were excluded. The main reasons for exclusion were the reporting of aggregated data combining outcomes for inlays and onlays, anterior and posterior restorations or other types of ceramic restorations (n = 51), references identified as interim reports of eligible studies with the same population (n = 16). 31 articles were included in this scoping review (Tables 3a and 3b).
FIGURE 1.
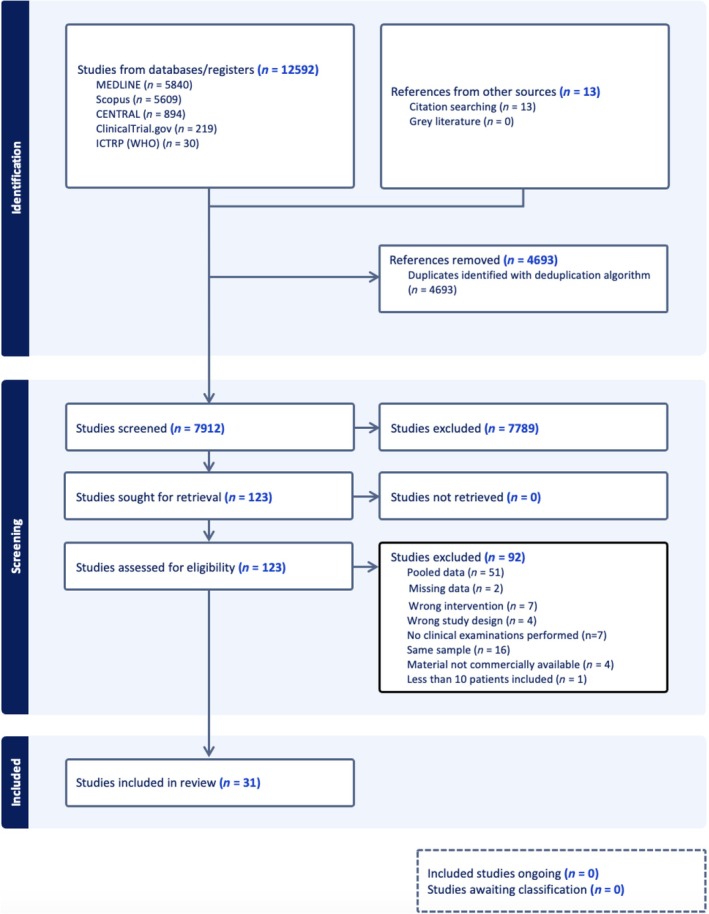
Prisma flow chart for article selection.
TABLE 3a.
Summary of included RCTs.
| No. | Author, year | Study type | Initial no. of patients | Final no. of patients | Drop‐outs | FU (month) | Restoration type | Material | Workflow | Tooth vitality | Placed no. of restorations |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Fasbinder et al. 2020 | RCT | 86 | 86 | 0 | 60 | Onlay | LRGC (IPS Empress CAD, Ivoclar), RMC (Lava Ultimate, 3MESPE) | Digital workflow: CEREC Bluecam, MCX mill (Dentsply Sirona) | Vital | Empress CAD: 60, Lava Ultimate: 60 |
| 2 | Ferrari Cagidiaco et al. 2019 | RCT | 60 | 60 | 0 | 36 | Partial crown | LDS (IPS e.max Press, Ivoclar), LDS (Initial LiSi Press, GC Co.) | Conventional workflow: PVS (Exa'lence, GC Co.), lost‐wax technique | Vital | e.max Press: 30, Initial Lisi Press: 30 |
| 3 | Ferrari Cagidiaco et al. 2020 | RCT | 105 | 96 | 9 | 48 | Partial crown | LDS (IPS e.max Press, Ivoclar), LDS (Initial LiSi Press, GC Co.) | Conventional workflow: PVS (Exa'lence, GC Co.), lost‐wax technique | Vital | e.max Press: 85, Initial Lisi Press: 85 |
| 4 | Ferrari Cagidiaco et al. 2024 | RCT | 120 | 120 | 0 | 48 | Partial crown | LDS (Initial LiSi Press, GC Co.), LDS (Initial LiSi Block, GC Co.) | Conventional and conventional‐digital workflow: PVS (Exa'lence, GC Co.), Fabrication: Initial Lisi Press: conventional (according to manufacturer's instructions); Initial LiSi Block: CAD/CAM (milling machine: n4 Plus) | Vital | Initial LiSi Press: 30, Initial LiSi Block: 30 |
| 5 | Ferrari et al. 2019 | RCT | 120 | 120 | 0 | 36 | Partial crown | LDS (Lisi Press, CG Co.) | Conventional workflow: PVS (Exa'lence, GC Co.), lost‐wax technique | Non‐vital | 120 |
| 6 | Guess et al. 2013 | RCT | 25 | 14 | 11 | 84 | Partial crown | LDS (IPS e.max Press (Ivoclar), LRGC (Pro CAD, Ivoclar) | Conventional and conventional‐digital workflow: Polyether (Permadyne, 3MESPE), fabrication according to manufacturer's instructions (ProCAD: CEREC InLab, e.max Press: lost‐wax technique) | Vital | e.max Press: 40, Pro CAD: 40 |
| 7 | Hassan et al. 2024 | RCT | 20 | 20 | 0 | 24 | Onlay | LDS (IPS e.max CAD, Ivoclar), RMC (Grandio CAD, Voco Dental) | Conventional‐digital workflow: PVS (Elite HD, Zhermack), Milling machine (imes‐icore CORiTEC 350i, imes‐icore GmbH) | Vital | e.max CAD: 20, Grandio CAD: 20 |
| 8 | Pfister et al. 2023 | RCT | 43 | 19 | 24 | 176 | Partial crown | FC (Vita Mark II, Vita Zahnfabrik) | Conventional‐digital workflow: conventional impression (C‐silicone (Silaplast & Silasoft, Detax), scan of impressions and fabrication (CEREC 3, Dentsply Sirona) | nr | 68 |
| 9 | Rinke et al. 2022 | RCT | 45 | 40 | 5 | 56 | Partial crown | LS (Suprinity, Vita Zahnfabrik) | Digital workflow: CEREC Omnicam, MC XL milling unit (Dentsply Sirona) | Vital | 61 |
| 10 | Schlichting et al. 2022 | RCT | 11 | 11 | 0 | 27 | Occlusal veneer | LDS (e. max CAD, Ivoclar), RMC (Lava Ultimate, 3MESPE) | Digital workflow: CEREC Bluecam, inLab software (Dentsply Sirona), milling machine nr | Vital | e. max CAD: 24, Lava Ultimate: 36 |
| 11 | Souza et al. 2021 | RCT | 20 | 20 | 0 | 12 | Onlay | LDS (IPS e.max CAD, Ivoclar), RMC (Lava Ultimate, 3 M Oral Care) | Conventional‐digital workflow: PVS (Express 2 Penta H and Express 2 Light Body, 3 M Oral Care), Fabrication: MCL Compact milling unit (Dentsply Sirona) | Vital | e. max CAD: 20, Lava Ultimate: 20 |
| 12 | van den Breemer et al. 2019 | RCT | 30 | 30 | 0 | 12 | Onlay | LDS (IPS e.max Press, Ivoclar) | Conventional workflow: PVS (Heavy and Ultralight Body Aquasil (Dentsply Sirona), lost wax‐technique | Vital | 60 |
| 13 | Zhang et al. 2022 | RCT | 128 | 121 | 7 | 36 | Onlay | LDS CAD (brand nr), RMC (brand nr) | Digital workflow: CEREC Omnicam, inLab MC XL milling machine (Dentsply Sirona) | Non‐vital | LDS: 66, RMC: 66 |
| No. | No. of restorations in FU | Total no. of failed units | Total no. of survived units | Definition of survival or failure | Survival /failure rate | Type of statistical model | Preparation (occlusal/axial and occlusal) | Preparation thickness | Restoration thickness |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Empress CAD: 60, Lava Ultimate: 60 | Empress CAD: 4, Lava Ultimate: 3 | Empress CAD: 56, Lava Ultimate: 57 | nr | Kaplan–Meier probability for fracture (5 years): Empress CAD: 0.068 (0.026; 0.171), Lava Ultimate: 0.083 (0.036; 0.189) | Kaplan–Meier survival estimation (missing description of statistical methods) | Occlusal and axial | Functional cusp at least 2 mm, non‐functional cusp at least 1.5 mm | nr |
| 2 | e.max Press: 30, Initial Lisi Press: 30 | e.max Press: 0, Initial Lisi Press: 0 | e.max Press: 30, Initial Lisi Press: 30 | Survival was set when the restoration was still in place at the last recall but with biological or technical complications that needed to be treated and/or the crown to be remade. Failure was set when the restoration was not in place anymore at last recall or, because of mechanical or biological complications, needed to be replaced | Survival rate (3 years): e.max Press and Initial Lisi Press: 100% | Mann–Whitney “U” test | Occlusal and axial | Occlusal reduction 1–1.5 mm | nr |
| 3 | e.max Press: 80, Initial Lisi Press: 81 | e.max Press: 5, Initial Lisi Press: 4 | e.max Press: 80, Initial Lisi Press: 81 | Survival was when the restoration was still in place at the last recall but with a biological or technical complication that needed to be treated but without the need to remake the crown | Failure rate (4 years): e.max Press: 6.25%, Initial Lisi Press: 6.17% | Mann–Whitney “U” test | Occlusal and axial | Occlusal clearance ranged between 0.5–1 and 1–1.5 mm | nr |
| 4 | Initial LiSi Press: 30, Initial LiSi Block: 30 | Initial LiSi Press: 0, Initial LiSi Block: 0 | Initial LiSi Press: 30, Initial LiSi Block: 30 | Survival was set when the restoration was still in place at the last recall but with a biological or technical complication that needed to be treated, but without the need to remake the crown. If the restoration was lost at the last recall or, because of mechanical or biological complications, needed to be replaced, it was classified as Failure | Survival rate (4 years): Initial LiSi Press and Initial LiSi Block: 100% | Mann–Whitney “U” test, Cox regression | Occlusal and axial | Occlusal reduction 1–1.5 mm | nr |
| 5 | 120 | 2 | 118 | Survival was defined as the outcome in the absence of absolute failures. The following parameters were considered as failures: [1] post‐debonding [2], post‐fracture [3], vertical or horizontal root fracture [4], crown dislodgement [5], crown fracture [6], periapical lesions not requiring endodontic re‐treatment (…), and [7] periapical lesions requiring endodontic retreatment | Survival rate (3 years): PCCs on molars with and without posts: 100%; PCCs on premolars without post: 93.3%; (2 years): PCCs on premolars with posts: 100% (3 years not given) | Kaplan–Meier survival estimation, Log rank test, Cox regression | nr | Occlusal clearance: 1–1.5 mm | nr |
| 6 | e.max Press: 24, Pro CAD: 24 | e.max Press: 0, Pro CAD: 1 | e.max Press: 24, Pro CAD: 24 | Absolute failure was defined by clinical unacceptable fracture and crack development, which required a replacement of the entire restoration, and/or secondary caries as well as endodontic complications | Survival rate (7 years): e.max Press: 100%, Pro CAD: 97% | Kaplan–Meier survival estimation, Random‐intercept logistic regression model | Occlusal and axial | Occlusal reduction: 2 mm | At least 1.5 mm occlusal thickness |
| 7 | e.max CAD: 18, Grandio CAD: 18 | e.max CAD: 2, Grandio CAD: 2 | e.max CAD: 18, Grandio CAD: 18 | nr | Functional survival rate (2 years): e.max CAD: 90%, Grandio CAD: 90% | Kaplan–Meier survival estimation, Chi‐Square, Fischer Test, MC‐Nemar's test | nr | Occlusal reduction: functional cusps 2 mm, non‐functional cusps 1.5 mm | nr |
| 8 | 32 | 27 | nr | Five reasons for Failure were distinguished: “debonding,” fracture,” “caries,” “endodontic treatment,” and “other reasons” | Survival rate (15 years): 78.1% (±7.3%) PCCs with selective enamel etching, 42.9% (±8.4%) PCCs without selective enamel etching | Kaplan–Meier survival estimation, Log rank test | Occlusal and axial | nr | nr |
| 9 | 54 | Group 0.5–0.74 mm thickness: 5, group 0.75–1.0 mm thickness: 0 | 49 | Survival was defined as the restoration being in situ at the time of the follow‐up examination without signs of a total loss (i.e., the in situ criterion) | Survival rate (5 years): group 0.5–0.74 mm thickness: 83% (95% confidence interval (CI): 0.71–0.96), group 0.75–1.0 mm thickness: 100% | Kaplan–Meier survival estimation, Cox Regression | Occlusal and axial | nr | Minimal thickness in central fissure: 0.5–0.74 or 0.75–1.0 mm |
| 10 | e.max CAD: 24, Lava Ultimate: 36 | e.max CAD: 1, Lava Ultimate: 0 | e.max CAD: 23, Lava Ultimate: 36 | Failure was considered whenever a restoration received a Score 4 or 5. Restorations graded 4 were considered unacceptable but still repairable, while restorations graded 5 were considered failures with immediate need of replacement | Estimated survival rate (3 years): e.max CAD:100%, Lava Ultimate: 84.7%; Pooled survival rate: 88.4% | Kaplan–Meier survival estimation, Log rank test | Occlusal | 0.4–0.6 mm (central groove) to 1.0–1.3 mm (cusp tips) | 0.55 mm at the central groove, 0.89 mm at the internal cusp slope, 1.00 mm at the cusp tip, and 0.78 mm at the marginal ridge |
| 11 | e. max CAD: 20, Lava Ultimate: 20 | e. max CAD: 0, Lava Ultimate: 0 | e. max CAD: 20, Lava Ultimate: 20 | nr | Survival rate (1 years): e.max CAD and Lava Ultimate: 100% | Mann–Whitney U test, Wilcoxon signed‐rank test | nr | Occlusal reduction: at least 1.5–2 mm | Occlusal thickness: at least 1.5–2 mm |
| 12 | 60 | 0 | 60 | nr | Survival rate (1 year): 100% | Chi‐square test, Wilcoxon signed‐rank test | Occlusal and axial | At least 1 mm; cusps were covered (1.5 mm) if the remaining tooth structure wall was < 2 mm thick | Occlusal thickness: at least 1 mm |
| 13 | LDS: 51, RMC: 47 | LDS: 4, RMC: 11 | LDS: 51, RMC: 46 | nr | Survival rate (3 years): LDS: 93.5% (95% CI, 90.4%–96.6%), RMC: 83.1% (95% CI, 78.4%–87.8%) | Kaplan–Meier survival estimation, Log rank test, Mann–Whitney test | Occlusal and axial | 2 mm at functional cusps and at least 1.5 mm at nonfunctional cusps | nr |
Abbreviations: CAD‐CAM, computer‐aided design‐computer‐aided manufacturing; FC, feldspar ceramic; FU, follow‐up; LDS, lithium disilicate; LRGC, leucite‐reinforced glass ceramic; LS, lithium silicate; No, number; nr, not reported; PVS, polyvinyl siloxane; RCT, randomized controlled trial; RMC, resin matrix ceramic.
TABLE 3b.
Summary of included non‐randomized studies of intervention (NRSs).
| No. | Author (year) | Study type | Initial no. of patients | Final no. of patients | Drop‐outs | FU (month) | Restoration type | Material | Workflow | Tooth vitality |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Archibald et al. (2018) | RC | 52 | 30 | 22 | 42 | Onlay | LDS (IPS e.max Press or CAD, Ivoclar) | Digital and conventional‐digital workflow: Bluecam (Dentsply Sirona), PVS (Aquasil, Dentsply Sirona), fabrication: CEREC MC XL machine (Dentsply Sirona) | nr |
| 2 | Arnetzl et al. (2012) | PC | 264 | 244 | 20 | 93 | Overlay | FC (Vitablocs Mark II, Vita Zahnfabrik) | Impression nr, fabrication: CEREC system (Dentsply Sirona) | nr |
| 3 | Chen et al. (2023) | Experimental | 176 | 176 | 0 | 36 | Onlay | LDS (IPS e.max CAD, Ivoclar) | Conventional‐digital workflow: PVS (Express, 3MESPE), CAD/CAM fabrication (machine nr) | Non‐vital |
| 4 | Fabbri et al. (2014) | RC | 312 (combined number for LDS restorations) | 312 (combined number for LDS restorations) | 0 | Onlays: 32.5, Occlusal veneers: 37.5 | Onlay and occlusal veneer | LDS (IPS e.max Press, Ivoclar) | Conventional workflow (impression material and fabrication technique nr) | Vital and non‐vital |
| 5 | Federlin et al. (2010) | Experimental | 29 | 22 | 7 (2 failures included) | 66 | Partial crown | FC (Vita 3D Master CEREC Mark II, Vita Zahnfabrik) | Impression nr, fabrication CEREC 3 (Dentsply Sirona) | nr |
| 6 | Klink et al. (2013) | PC | 35 (combined number for Vita Mark II restorations) | 28 (combined number for Vita Mark II restorations) | 7 (combined number for Vita Mark II restorations) | 49 | Partial crown | FC (Vitablocs Mark II, Vita Zahnfabrik) | Conventional‐digital workflow: Polyether (brand nr), design and fabrication (CEREC inLab software, Dentsply Sirona), milling machine nr | nr |
| 7 | Lindner et al. (2023) | RC | nr | 104 (combined number for inlays and partial crowns) | nr | 71 | Partial crown | LDS (e.max Press, Ivoclar) | nr | Vital and non‐vital |
| 8 | Lu et al. (2018) | Experimental | 93 | 91 | 2 | 36 | Onlay | FC (Vitablocs Mark II, Vita Zahnfabrik), RMC (Enamic, Vita Zahnfabrik) | Digital workflow: CEREC Bluecam, MC XL machine, (Dentsply Sirona) | Non‐vital |
| 9 | Malament et al. (2021) | PC | 304 (combined number for LDS restorations) | 304 (combined number for LDS restorations) | nr | 118 | Onlay | LDS (e.max Press, Ivoclar) | Conventional workflow: Polyether (Impregum; 3MESPE), lost‐wax technique | nr |
| 10 | Murgueitio et al. (2012) | PC | 99 | 99 | 0 | 35 | Onlays and Partial crowns | LRGC (IPS Empress, Ivoclar) | Conventional workflow: PVS (Elite HD, Zhermack), vacuum injection mold technique | Vital and non‐vital |
| 11 | Naeselius et al. (2008) | RC | 91 | 59 | 32 | 49 | Onlay | LRGC (IPS Empress, Ivoclar) | Conventional workflow: Polyether (Impregum, Penta, 3MESPE) or A‐silicone material (Express, 3MESPE or President Coltene/Whaledent), painting technique | Vital and non‐vital |
| 12 | Offer et al. (2022) | RC | 251 | 251 | 0 | 79.2 | Partial crown | LDS (e.max Press, Ivoclar), LRGC (IPS Empress, Ivoclar) | Conventional workflow: Polyether (Impregum, 3MESPE), lost‐wax technique | Vital and non‐vital |
| 13 | Özyoney et al. (2013) | PC | 53 | 53 | nr | 48 | Onlay | LRGC (IPS Empress II, Ivoclar) | Conventional impression: PVS (Permagum, 3MESPE), fabrication nr | Non‐vital |
| 14 | Spitznagel et al. (2018) | PC | 47 (combined number for inlays and PCRs) | 37 (combined number for inlays and PCRs) | 10 (combined number for inlays and PCRs) | 36 | Partial crown | RMC (Enamic, Vita Zahnfabrik) | Conventional‐digital workflow: Vinylsiloxanether (Identium, Kettenbach), fabrication: CEREC inLab MCXL milling unit (Dentsply Sirona) | Vital and non‐vital |
| 15 | Strasding et al. (2020) | PC | 54 (combined number for inlays and onlays) | 36 (combined number for inlays and onlays) | 18 (combined number for inlays and onlays) | 134 | Onlay | LRGC (IPS Empress I, Ivoclar) | Conventional workflow: Polyether (Permadyne, 3 M ESPE), lost‐wax‐technique | Vital and one non‐vital |
| 16 | Wagner et al. (2003) | RC | 22 | 22 | nr | 84 | Partial crown | LRGC (IPS Empress I, Ivoclar) | nr | Vital and non‐vital |
| 17 | Xiao et al. (2020) | Experimental | 120 | 120 | 0 | 24 | Onlay | LDS (e.max Press, Ivoclar) | Conventional workflow: PVS (Express, 3MESPE), lost‐wax technique | Non‐vital |
| 18 | Zimmermann et al. (2018) | PC | 30 | 23 | 7 | 24 | Partial crown | RMC (Lava Ultimate, 3MESPE) | Conventional‐digital workflow: conventional impression (Polyether [Impregum Penta, 3MESPE]), digital quadrant impression of cast (CEREC Bluecam (Dentsply Sirona), fabrication: CEREC MCXL milling unit (Dentsply Sirona) | nr |
| No. | Placed no. of restorations | No. of restorations in FU | Total no. of failed units | Total no. of survived units | Definition of survival or failure | Survival/failure rate | Type of statistical model | Preparation (occlusal/axial and occlusal) | Preparation thickness | Restoration thickness |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 65 | 37 | 5 | 34 | Failures were established as being restorations that were lost or had fractured prior to the evaluation or those that required replacement because of poor marginal quality (Charlie, Delta), secondary caries (Bravo), or endodontic complications | Estimated survival rates (2 years): 96.3%, (4 years): 91.5%; Mean survival rate (6 years): 67.4% (95% CI 62.3–72.5%) | Kaplan–Meier survival estimation and Cox regression, Fisher exact and McNemar test | Occlusal and axial | Nonfunctional cusp minimal 1.5 mm, functional cusp 2 mm | nr |
| 2 | 310 | 286 | 10 | nr | Overlays requiring repair or replacement due to fractures or major defects were classified as Charlie or Delta (technical failures). Onlays associated with sensitivity problems, persistent pain, or cavities were also rated as clinically unacceptable (biological failures) | Survival probability (7.8 years): 96.5% | Kaplan–Meier survival estimation | nr | nr | nr |
| 3 | 180 | 180 | 7 | 173 | Survival was defined as the presence of onlays without biological or technical complications during the entire follow‐up period | Survival rate (3 years): Group O: 98%, Group MO/DO: 96.3%, Group C: 94% | Kaplan–Meier survival estimation, Chi‐square test, Fisher's exact test | Group C: occlusal reduction and boxes, Group O: occlusal reduction and rounded shoulder, Group MO/DO: occlusal reduction and rounded shoulder, prox. boxes without undercut | 1.5–2 mm occlusal reduction | nr |
| 4 | Onlays: 62, Occlusal veneers: 39 | Onlays: 59, Occlusal veneers: 39 | Onlays: 3, Occlusal veneers: 0 | Onlays: 59, Occlusal veneers: 39 | In the case of any mechanical complication, the restoration was considered a failure | Cumulative survival probability (2.7 years): layered onlays: 100%, monolithic onlays: 97.83% (3.1 years): posterior layered and monolithic veneers: 100% | Kaplan–Meier survival estimation, Log rank test | nr | minimal occlusal thickness 2 mm | nr |
| 5 | 29 | 22 | 4 | 21 | All restorations with need of intervention in terms of renewal of the restoration were considered a failure. | Survival rate (5.5 years): 88.8% (±5.9%) | Kaplan Meier survival estimation and Mantel Cox | Occlusal and axial | nr | nr |
| 6 | 25 | 23 | 1 | 22 | Severe adverse event: Severely affecting the restoration or tooth that calls for biologic therapy or technical renewal (used to calculate prevalence of failure); Removal or destruction of restoration, i.e., trepanation through an inlay/onlay (not loss of retention): Survivor function as Kaplan–Meier estimation censored by removal | Cohort prevalence and survival (4 years): Cp (Prevalence of complication): 8.7%, Fp (Prevalence of failure): 4.3%, combined: 1.0 | Kaplan–Meier survival estimation | nr | nr | nr |
| 7 | 114 | nr | 5 | nr | Restorations evaluated with a score of 4 were designated “repair”, and restorations scored 5 were designated “failure” | nr (combined outcome for inlays and partial crowns) | Kaplan–Meier survival estimation | nr | nr | nr |
| 8 | 34 Vitablocs Mark II, 67 Enamic | nr | 3 Vitablocs Mark II, 2 Enamic | nr | nr | Survival rate (3 years): Vitablocs Mark II: 90.7% (95% CI, 85.6%–95.8%); Enamic: 97.0% (95% CI, 94.9%–99.1%) | Kaplan–Meier survival estimation, Log rank test, Fisher exact test | Occlusal and axial | Minimal occlusal reduction: Vitablocs Mark II: minimal 2 mm, Enamic: 1–1.2 mm | nr |
| 9 | 305 | 305 | 3 (type of failure not reported) | 302 | A restoration was recorded as a Failure if it exhibited a fractured ceramic piece that necessitated the restoration be remade. In some instances, the restoration was replaced but not because of failure. These were recorded as replaced, without failure (right censored data) | Survivor Function (9.8 years): 98.3% | Kaplan–Meier survival estimation, Log rank test, Mann–Whitney U test | Occlusal and axial | nr | nr |
| 10 | 210 (no separation of onlays and partial crowns) | 210 (no separation of onlays and partial crowns) | 7 (no separation of onlays and partial crowns) | 203 (no separation of onlays and partial crowns) | Failure modes are classified | Survival rate (3 years): 97.1% (combined outcome for onlays and partial crowns) | Kaplan–Meier survival estimation, Log rank test, Cox regression | Axial and occlusal | Occlusal: 1.5–2 mm | Classification in: thin (1–1.4 mm), medium (1.5–1.9 mm), and thick (2 mm or more) |
| 11 | 130 | 81 | 6 | 75 | A restoration was judged as a Failure when receiving either of the CDA ratings Tango (not acceptable/should be replaced or repaired) or Victor (not acceptable/must be replaced or repaired). All fractures, including surface fractures, were judged as failures | Failure rate (4 years): 7.3% | Descriptive statistics | nr | nr | Minimum thickness of 1 mm |
| 12 | 487 (172 LDS, 315 LRGC) | 487 (172 LDS, 315 LRGC) | 5 | 482 | Irreparable fracture of the ceramic was defined as restoration failure. Additional fracture of the tooth structure was not documented. Debonding was evaluated separately and was not included in the survival rate | Survival rate (5 years): 100%; (10 years): 97.3%; (15 years): 89.5% (no separate survival rate for ceramic materials reported) | Kaplan–Meier survival estimation, Log rank test | Occlusal and axial | nr | nr |
| 13 | 53 | 50 | 3 | 50 | nr | nr | Kaplan–Meier survival estimation, Wilcoxon signed‐rank test | nr | nr | nr |
| 14 | 58 | 44 | 2 | 44 | Absolute failures were defined as clinically unacceptable fracture, which required replacement of the restorations, inacceptable (=Charlie rating) marginal discoloration, marginal adaptation, and secondary caries or debonding | Survival probability (95% CI) (1 year): 100%; (2 years): 97.9% (86.1%–99.7%); (3 years): 95.6% (84.5%–98.9%) | Kaplan–Meier survival estimation, Cox regression | Occlusal and axial (depending on the defect size) | Occlusal at least 1.0–1.5 mm | nr |
| 15 | 27 | 25 | 5 | 20 | Survival rate: All restorations which had no complications (A) or minor complications (B) until the last follow‐up examination. Failure rate: All restorations which showed clinically unacceptable, major complications (C), or fatal complications (D) | Survival rate (11.2 years): 80% | Kaplan–Meier survival estimation, Cox regression | Occlusal and axial | 1.5 mm minimal preparation depth | nr |
| 16 | 42 | 42 | 2 | 40 | nr | Survival rate (7 years): 81% ± 15% | Kaplan–Meier survival estimation, Log rank test | nr | nr | nr |
| 17 | 120 | 115 | 5 | 115 | nr | Survival rate (2 years): 95.83% | Kaplan–Meier survival estimation, Chi‐square test, Fisher exact test | Group S: occlusal and axial, Group B: occlusal with bevel | Occlusal reduction: 1.5–2 mm | nr |
| 18 | 42 | 33 | 5 | nr | Failure: There were three evaluation categories (esthetics, function, biology) each with five subcategories. From best to worst, the subcategories were: (1) clinically excellent, (2) clinically good, (3) clinically sufficient, (4) clinically not sufficient but repairable, and (5) clinically unacceptable. Evaluation with category (5) was rated as a clinical failure | nr (success rate reported) | Wilcoxon‐test | nr | nr | nr |
Abbreviations: CAD‐CAM, computer‐aided design‐computer‐aided manufacturing; FC, feldspar ceramic; FU, follow‐up; LDS, lithium disilicate; LRGC, leucite‐reinforced glass ceramic; LS, lithium silicate; No, number; nr, not reported; PVS, polyvinyl siloxane; RCT, randomized controlled trial; RMC, resin matrix ceramic.
3.2. Characteristics of Sources of Evidence
Thirteen of the included articles were identified as RCTs [19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31] and 18 as non‐randomized studies of interventions (NRS) [32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49]. Six NRSs were conducted retrospectively [32, 33, 34, 35, 36, 37] and 12 prospectively [38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49]. Seven RCTs assessed outcomes of partial crowns [20, 21, 22, 23, 24, 26, 27], five of onlays [19, 25, 29, 30, 31], and one of occlusal veneers [28]. Nine RCTs reported head‐to‐head comparisons among different ceramic materials. Four of them compared RMC with LDS [25, 28, 29, 31], one compared RMC with leucite‐reinforced glass ceramic (LRGC) [19], one compared LRGC with LDS [23], and three compared two types of LDS [20, 21, 24]. Two RCTs investigated ceramic materials with conventional versus CAD‐CAM fabrication techniques [23, 24]. Four RCTs compared partial crowns with or without post‐insertion [22], with and without selective enamel etching [26], with immediate dentin sealing and delayed dentin sealing [30], and with different restoration thicknesses (0.5–0.74 vs. 0.75–1.0 mm) [27]. Seven of the RCTs reported short‐term (1–3 years) [20, 22, 25, 28, 29, 30, 31], four mid‐term (4–6 years) [19, 21, 24, 27], and two long‐term (≥ 7 years) follow‐ups [23, 26]. Seven NRSs investigated the performance of partial crowns [34, 36, 37, 40, 42, 45, 46], eight of onlays [32, 35, 38, 39, 41, 43, 44, 47, 49], and two studies evaluated two types of PCRs (partial crowns and onlays [48]; onlays and occlusal veneers [33]). Five studies investigated the performance of onlays [32, 33, 39, 41, 44] and occlusal veneers [33] fabricated from LDS, one of feldspar ceramic (FC) onlays [38], and three of LRGC onlays [35, 43, 49]. Six studies evaluated partial crowns that were either fabricated from LDS [34], FC [40, 46], LRGC [37], or RMC [42, 45]. Other NRSs compared LRGC and LDS partial crowns [36], FC and RMC onlays [47], or LRGC onlay and partial crown restorations [48]. No PCRs fabricated from zirconia were identified in the included studies. Seven of the included NRSs observed short‐term (1–3 years) [33, 39, 42, 44, 45, 47, 48], six mid‐term (4–6 years) [32, 34, 35, 40, 46, 49], and five long‐term (≥ 7 years) data [36, 37, 38, 41, 43].
3.3. Synthesis of Results
3.3.1. Outcome Characteristics
3.3.1.1. Survival
Different definitions of survival and failure were specified in individual studies. Four studies defined survival when the restoration was still in situ at the final follow‐up visit with or without need of maintenance [20, 21, 24, 27]. In two studies survival was defined as the absence of absolute failures [22, 23]. Four other studies defined failure instead of survival, which was considered when the restoration was lost, removed, and/or remade [32, 40, 41, 46]. Furthermore, failures were considered when the restoration experienced a major complication [33, 43] or whenever a restoration received a score that was considered as clinically unacceptable [28, 34, 35, 38, 45]. In other cases, an irreparable fracture of the restoration was defined as failure [36] or no definition was available, instead events considered as failures were listed [26]. Nine of the 31 included studies did not specify any definition of survival or failure [19, 25, 29, 30, 31, 37, 44, 47, 49]. Kaplan–Meier survival curves in combination with a Cox regression [22, 27, 32, 42, 43, 48], log rank test [22, 26, 28, 31, 33, 36, 37, 41, 47, 48], Wilcoxon‐test [49], or other methods (e.g., Chi‐Square [25, 39, 44], Fischer test [25, 32, 39, 44, 47], Mc‐Nemar's test [25, 32], or Mann–Whitney “U” test [20, 21, 24, 29, 31, 41]) were used for statistical analysis. However, survival was reported either as estimated survival rate [28], mean survival rate [32], survival probability [38, 42], cumulative survival probability [33], pooled survival rate [28] or functional survival rate [25]. In other cases, failure rate [21, 35], prevalence of failure [46], probability of fracture [19], or no rate [49] were specified. Only a few studies described survival rates in % with confidence intervals (95% CI) [31, 32, 42, 47]. The majority of studies reported survival rates in % exclusively [21, 23, 35, 38, 39, 43, 44]. Survival rates of short‐term studies (1–3 years) ranged between 83.1% and 100% [20, 22, 25, 28, 29, 30, 31, 33, 39, 42, 44, 45, 47, 48]. Mid‐term studies (4–6 years) showed a survival rate range of 83%–100% [21, 24, 27, 32, 35, 40, 46] and long‐term studies (7–11.7 years) of 80%–100% [23, 37, 38, 41, 43]. After 15 years, survival rates of 89.5% for LRGC and LDS partial crowns [36] and 78.1% and 42.9% for FC partial crowns with and without selective enamel etching, respectively, were reported [26].
3.3.1.2. Complications
Seventeen of the included studies used modified United States Public Health Service (USPHS) criteria [19, 23, 24, 25, 27, 28, 32, 37, 38, 39, 40, 42, 43, 44, 47, 48, 49], four used World Dental Federation (FDI) criteria [29, 31, 34, 45], three used modified California Dental Association (CDA) criteria [33, 35, 46], two used Functional Index for Teeth (FIT) [20, 21], one study used FDI and modified USPHS [26], and four studies did not report the applied evaluation method [22, 30, 36, 41]. Depending on the definitions, the events were assessed as failures or complications. Complications were grouped either as biological, like endodontic complication, secondary caries, tooth fracture, or technical complication, including ceramic fracture, crack, chipping, loss of retention, or problems with marginal integrity. Fractures and loss of retention were reported to be the most common mechanical causes for failures [19, 21, 23, 25, 26, 27, 31, 32, 33, 34, 35, 37, 38, 39, 40, 42, 44, 45, 46, 47, 48, 49]. However, if the restoration could be recemented and was in situ at the final follow‐up, some of the included studies considered loss of retention as complication exclusively [27, 33, 34, 49]. Endodontic complications and secondary caries were the main classes of biological complications [19, 21, 25, 26, 28, 32, 34, 35, 37, 38, 40, 48, 49]. The majority of studies reported success rates [20, 22, 23, 25, 27, 29, 33, 34, 35, 39, 42, 45, 47, 49]. Due to different assessment methods and different definitions of survival and complications (Tables 3a and 3b), success rates of individual studies did not appear comparable. In a systematic review, numbers of complications can be used for the calculation of complication rates.
3.3.1.3. Patient‐Reported Outcomes
In total, 11 of the 31 included studies reported patient‐reported outcomes either ordinally (categories from less to more satisfied) [28, 29, 31, 33, 34, 38, 43] or continuously via a visual analog scale (VAS) [30, 47]. One study reported the patient satisfaction but did not specify the assessment method [44]. Another study reported that patients were asked about satisfaction; however, no further information was provided [32]. Overall, patient satisfaction was reported to be high across studies.
3.3.2. Preparation Design and Restoration Thickness
Various preparation designs were described in the included studies concerning the geometry, reduction, and extension of the preparation. Four included studies did not provide any detail about the preparation design [34, 37, 46, 49]. Two studies reported an occlusal reduction of at least 2 mm [23, 33], nine studies of 1.5–2 mm [19, 25, 29, 31, 32, 39, 43, 44, 48], and five studies of 1–1.5 mm [20, 22, 24, 30, 42]. Moreover, one study reported a range of 0.5–1.5 mm [21] and one study differentiated between an occlusal reduction of 2 mm for FC and 1–1.2 mm for RMC onlays [47]. The lowest occlusal reduction of 0.4–0.6 mm at the central groove and 1.0–1.3 mm at the cusp tips was performed for occlusal veneers fabricated from RMC and LDS [28]. Only two included studies described non‐retentive preparation designs without an axial preparation [28, 44]. Designs were performed as occlusal reduction exclusively [28] or as an occlusal reduction with bevel [44]. Restoration thickness was reported in six included studies: 1.5–2 mm [29], 1.5 mm [23], a minimum of 1 mm [30, 35], or < 1 mm [27, 28]. Another study performed a classification of thin (1–1.4 mm), medium (1.5–1.9 mm), and thick (2 mm or more) LRGC restorations and concluded that thin and medium thick restorations were more prone to fracture [48]. Three included studies investigated PCRs with minimally invasive (< 1 mm) restoration thicknesses [27, 28, 41]. One RCT provided a detailed description of 0.55 mm at the central groove, 0.89 mm at the internal cusp slope, 1 mm at the cusp tip, and 0.7 mm at the marginal ridge [28]. Another NRS detected no difference between > 1 mm and < 1 mm thick pressed LDS PCRs [41]. One RCT compared lithium silicate (LS) partial crowns of 0.5–0.74 and 0.75–1.0 mm thickness. Five bulk fractures occurred in the 0.5–0.74 mm group, whereas the 0.75–1.0 mm group experienced no fracture [27]. However, only the latter two studies compared different ceramic thicknesses and can therefore provide information regarding the correlation of restoration thickness and ceramic fractures [27, 41].
3.3.3. Conventional Versus Digital Workflow
Six studies applied a digital [19, 27, 28, 31, 32, 47] and 13 studies a conventional workflow [20, 21, 22, 23, 24, 30, 33, 35, 36, 41, 43, 44, 48]. A combined conventional‐digital workflow was used in 10 studies [23, 24, 25, 26, 29, 32, 39, 42, 45, 46]. Three studies compared Press and CAD ceramics [23, 24, 32] and performed conventional [23, 24] or digital impressions [32]. Two studies did not provide any information about the applied impression and fabrication techniques [34, 37]. Two other studies used a CAD‐CAM fabrication, but did not report the impression method [38, 40]. In contrast, another study used a conventional impression, but did not provide any information regarding the fabrication method [49]. Overall, the majority of studies used a conventional impression, whereas the fabrication of restorations was more frequently performed digitally (Tables 3a and 3b).
3.3.4. Tooth Vitality
Ten RCTs were conducted on vital teeth [19, 20, 21, 23, 24, 25, 27, 28, 29, 30], two on non‐vital teeth [22, 31] and one did not report tooth vitality [26]. In contrast, the majority of NRSs included vital and non‐vital teeth [33, 34, 35, 36, 37, 42, 43, 48]. Six studies did not report tooth vitality [32, 38, 40, 41, 45, 46] and four studies investigated PCRs placed on non‐vital teeth [39, 44, 47, 49]. After 3 years of follow‐up, survival rates of 100% were reported for LDS PCRs on vital teeth [20, 28]. Survival rates for LDS PCRs on non‐vital teeth ranged between 93.5% and 100% after 3 years of follow‐up [22, 31, 39]. Since long‐term studies investigating PCRs on non‐vital teeth are lacking, the long‐term performance of PCRs on non‐vital teeth remains uncertain. None of the included studies performed head‐to‐head comparisons among PCRs on vital and non‐vital teeth.
4. Discussion
The studies reviewed varied significantly in their definitions of survival and failure, with some defining survival as restorations remaining in situ. In contrast, others defined it based on the absence of absolute failures or major complications. Statistical analyses to measure survival rates employed diverse methods, including Kaplan–Meier curves and Cox regression. Short‐term survival rates ranged from 83.1% to 100%, with long‐term studies showing similar variation. Complications, mostly mechanical (fractures, loss of retention) or biological (endodontic complications, secondary caries), were frequently reported and differently classified across studies. In most studies, patient‐reported outcomes, showing largely favorable results, were measured using ordinal or visual analog scales. Preparation designs and restoration thicknesses were diverse, with thinner restorations showing higher fracture rates. Both digital and conventional workflows were employed, though digital processes were more frequently used. Survival outcomes differed slightly for vital and non‐vital teeth, with long‐term data on non‐vital teeth remaining uncertain. Overall, there was considerable variation in survival, complication rates, and workflow approaches, underscoring the need for standardized definitions and methodologies in future studies.
Our scoping review concluded that 13 RCTs [19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31] and 18 NRSs (six retrospective [32, 33, 34, 35, 36, 37], 12 prospective [38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49]) are available for the applied research question. Nine of the RCTs performed head‐to‐head comparisons among PCRs fabricated from different ceramic materials [19, 20, 21, 22, 23, 24, 25, 28, 29, 31]. Three of these studies compared two different types of LDS [20, 21, 24] and are not suitable for a meta‐analysis investigating different ceramic materials. In the absence of RCTs, NRSs can inform clinical practice only when there is certainty that no RCTs are currently available [50]. This scoping review identified a substantial body of evidence from RCTs, which does not warrant the inclusion of other lower‐level types of evidence. The other four identified RCTs compared post‐ versus non‐post‐insertion [22], different bonding techniques [26, 30], and restoration thicknesses (0.5–0.74 vs. 0.75–1.0 mm) [27].
The detected similar and wide ranges of survival rates in short, medium, and long‐term might be explained by the heterogeneity of included studies regarding study design (RCTs and NRSs), type of ceramic (all‐ceramic and RMC), different definitions of survival, and applied statistical models for survival analysis. Studies with inadequate or unclear randomization may overestimate treatment effects by up to 40% compared with those using proper randomization [51, 52]. The majority of included studies did not report any ratios, p‐values, or confidence intervals for survival analysis. Survival and complication rates also appear to be too inaccurate due to different evaluation and statistical methods and due to various definitions of survival and failure. Consequently, it is advisable, that statistical calculations are based on the numbers of survived units, failures, or complications instead of survival, success, or complication rates.
Fractures of the ceramic material and loss of retention were the most common mechanical causes for failures [19, 21, 23, 25, 26, 27, 31, 32, 33, 34, 35, 37, 38, 39, 40, 42, 44, 45, 46, 47, 48, 49], whereas endodontic complications and secondary caries were identified as the main classes of biological complications [19, 21, 25, 26, 28, 32, 34, 35, 37, 38, 40, 48, 49]. This is in line with other reviews investigating the performance of PCRs [2, 14]. To confirm these findings, complication rates of included RCTs should be calculated in subsequent systematic reviews. The applied preparation designs differed in the included studies, and no evidence regarding the superiority of a specific preparation design for PCRs was identified. A recently published study on the performance of minimally invasive LDS PCRs analyzed the preparation characteristics (number of cusps and surfaces involved, relative width of the preparation, and surface area in %). It concluded that the preparation characteristics had no significant influence on the survival and success of minimally invasive restorations [53]. However, since the mean evaluation time was limited to 37 months, this conclusion should be viewed with caution. Regarding restoration thickness, one RCT compared LS partial crowns and observed five bulk fractures in the 0.5–0.74 mm group, whereas the 0.75–1.0 mm group experienced no fracture [27]. In contrast, one of the NRSs detected no significant difference between > 1 mm and < 1 mm thick pressed LDS PCRs [41]. An explanation might be the application of different luting agents and bonding techniques, which may have influenced the survival and complications of restorations. In the NRS mentioned above [41], restorations were adhesively luted with a light polymerizing resin cement (Variolink II, Ivoclar). A dual‐curing composite cement with a multi‐bottle bonding and total‐etch technique (Syntac classic and Variolink II, Ivoclar) or a self‐adhesive cement (Relay X Unicem, 3MEspe) were used in the RCT [27]. Further clinical studies on the performance of PCRs with minimally invasive thicknesses and precise descriptions of the applied preparation designs are necessary. Only six of the included studies used a fully digital workflow, while the conventional impression was still the most used method. A previously conducted systematic review reported that the longevity of CAD‐CAM‐fabricated ceramic restorations was lower than that of their conventional counterparts [54]. However, advancements in CAD‐CAM technology may have further improved the properties and longevity of restorative materials [55, 56]. Regarding tooth vitality, it was noticeable that RCTs mostly restricted the inclusion of vital teeth (10 of 13 [19, 20, 21, 23, 24, 25, 27, 28, 29, 30]). In contrast, NRSs were performed on either non‐vital teeth [39, 44, 47, 49], vital and non‐vital teeth [33, 34, 35, 36, 37, 42, 43, 48], or did not report tooth vitality [32, 38, 40, 41, 45, 46]. Although none of the included studies compared vital and non‐vital teeth, PCRs on vital teeth appear to have a more favorable outcome than on non‐vital teeth [31, 48]. This hypothesis can be evaluated by conducting a subgroup analysis in future systematic reviews. Clinical long‐term studies on the performance of PCRs on non‐vital teeth and studies with comparisons of restorations placed on vital and non‐vital teeth are needed.
5. Conclusion
The body of evidence informing the effect of PCRs varied in its definitions of survival and failure, survival rates, complication classifications, and workflow approaches. The review highlighted the need for standardized definitions and methodologies, as well as long‐term outcomes, especially in non‐vital teeth, for which data remains uncertain.
Conflicts of Interest
The authors declare no conflicts of interest.
Acknowledgments
The authors like to thank Maria‐Inti Metzendorf for the development of the search.
Funding: The authors received no specific funding for this work.
P. C. Gierthmuehlen and S. Pieralli contributed equally to this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- 1. Al‐Haj Husain N., Özcan M., Molinero‐Mourelle P., and Joda T., “Clinical Performance of Partial and Full‐Coverage Fixed Dental Restorations Fabricated From Hybrid Polymer and Ceramic CAD/CAM Materials: A Systematic Review and Meta‐Analysis,” Journal of Clinical Medicine 9, no. 7 (2020): 2107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wang B., Fan J., Wang L., Xu B., Wang L., and Chai L., “Onlays/Partial Crowns Versus Full Crowns in Restoring Posterior Teeth: A Systematic Review and Meta‐Analysis,” Head & Face Medicine 18, no. 1 (2022): 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ladino L., Sanjuan M. E., Valdez D. J., and Eslava R. A., “Clinical and Biomechanical Performance of Occlusal Veneers: A Scoping Review,” Journal of Contemporary Dental Practice 22, no. 11 (2021): 1327–1337. [PubMed] [Google Scholar]
- 4. Edelhoff D. and Sorensen J. A., “Tooth Structure Removal Associated With Various Preparation Designs for Posterior Teeth,” International Journal of Periodontics and Restorative Dentistry 22, no. 3 (2002): 241–249. [PubMed] [Google Scholar]
- 5. Sirous S., Navadeh A., Ebrahimgol S., and Atri F., “Effect of Preparation Design on Marginal Adaptation and Fracture Strength of Ceramic Occlusal Veneers: A Systematic Review,” Cllinical and Experimental Dental Research 8, no. 6 (2022): 1391–1403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.“The Glossary of Prosthodontic Terms 2023: Tenth Edition,” Journal of Prosthetic Dentistry 130, no. 4 Suppl 1 (2023): e1–e3. [DOI] [PubMed] [Google Scholar]
- 7. Veneziani M., “Posterior Indirect Adhesive Restorations: Updated Indications and the Morphology Driven Preparation Technique,” International Journal of Esthetic Dentistry 12, no. 2 (2017): 204–230. [PubMed] [Google Scholar]
- 8. H. T. Shillingburg, Jr. , Sather D. A., Wilson E. L., et al., Fundamentals of Fixed Prosthodontics, 4th ed. (Chicago, USA: Quintessence Pub Co, 2012). [Google Scholar]
- 9. Vagropoulou G. I., Klifopoulou G. L., Vlahou S. G., Hirayama H., and Michalakis K., “Complications and Survival Rates of Inlays and Onlays vs Complete Coverage Restorations: A Systematic Review and Analysis of Studies,” Journal of Oral Rehabilitation 45, no. 11 (2018): 903–920. [DOI] [PubMed] [Google Scholar]
- 10. Morimoto S., Rebello de Sampaio F. B., Braga M. M., Sesma N., and Özcan M., “Survival Rate of Resin and Ceramic Inlays, Onlays, and Overlays: A Systematic Review and Meta‐Analysis,” Journal of Dental Research 95, no. 9 (2016): 985–994. [DOI] [PubMed] [Google Scholar]
- 11. Ayres G., Parize H., Mendonça L. M., Kubata B. R., and Tirapelli C., “Is the Digital Workflow More Efficient for Manufacturing Partial‐Coverage Restorations? A Systematic Review,” Journal of Prosthetic Dentistry (2023): S0022‐3913(23)00506‐1. [DOI] [PubMed] [Google Scholar]
- 12. Fathy H., Hamama H. H., El‐Wassefy N., and Mahmoud S. H., “Clinical Performance of Resin‐Matrix Ceramic Partial Coverage Restorations: A Systematic Review,” Clinical Oral Investigations 26, no. 5 (2022): 3807–3822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Santesso N., Glenton C., Dahm P., et al., “GRADE Guidelines 26: Informative Statements to Communicate the Findings of Systematic Reviews of Interventions,” Journal of Clinical Epidemiology 119 (2020): 126–135. [DOI] [PubMed] [Google Scholar]
- 14. Abduo J. and Sambrook R. J., “Longevity of Ceramic Onlays: A Systematic Review,” Journal of Esthetic and Restorative Dentistry 30, no. 3 (2018): 193–215. [DOI] [PubMed] [Google Scholar]
- 15. Tricco A. C., Lillie E., Zarin W., et al., “PRISMA Extension for Scoping Reviews (PRISMA‐ScR): Checklist and Explanation,” Annals of Internal Medicine 169, no. 7 (2018): 467–473. [DOI] [PubMed] [Google Scholar]
- 16. Arksey M. and O'Malley L., “Scoping Studies: Towards a Methodological Framework,” International Journal of Social Research Methodology 8, no. 1 (2005): 19–32. [Google Scholar]
- 17. Peters M. D., Godfrey C. M., Khalil H., McInerney P., Parker D., and Soares C. B., “Guidance for Conducting Systematic Scoping Reviews,” International Journal of Evidence‐Based Healthcare 13, no. 3 (2015): 141–146. [DOI] [PubMed] [Google Scholar]
- 18. Borissov N., Haas Q., Minder B., et al., “Reducing Systematic Review Burden Using Deduklick: A Novel, Automated, Reliable, and Explainable Deduplication Algorithm to Foster Medical Research,” Systematic Reviews 11, no. 1 (2022): 172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Fasbinder D. J., Neiva G. F., Heys D., and Heys R., “Clinical Evaluation of Chairside Computer Assisted Design/Computer Assisted Machining Nano‐Ceramic Restorations: Five‐Year Status,” Journal of Esthetic and Restorative Dentistry 32, no. 2 (2020): 193–203. [DOI] [PubMed] [Google Scholar]
- 20. Cagidiaco E. F., Grandini S., Goracci C., and Joda T., “A Pilot Trial on Lithium Disilicate Partial Crowns Using a Novel Prosthodontic Functional Index for Teeth (FIT),” BMC Oral Health 19, no. 1 (2019): 276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ferrari Cagidiaco E., Sorrentino R., Pontoriero D. I., and Ferrari M., “A Randomized Controlled Clinical Trial of Two Types of Lithium Disilicate Partial Crowns,” American Journal of Dentistry 33, no. 6 (2020): 291–295. [PubMed] [Google Scholar]
- 22. Ferrari M., Ferrari Cagidiaco E., Goracci C., et al., “Posterior Partial Crowns out of Lithium Disilicate (LS2) With or Without Posts: A Randomized Controlled Prospective Clinical Trial With a 3‐Year Follow Up,” Journal of Dentistry 83 (2019): 12–17. [DOI] [PubMed] [Google Scholar]
- 23. Guess P. C., Selz C. F., Steinhart Y. N., Stampf S., and Strub J. R., “Prospective Clinical Split‐Mouth Study of Pressed and CAD/CAM All‐Ceramic Partial‐Coverage Restorations: 7‐Year Results,” International Journal of Prosthodontics 26, no. 1 (2013): 21–25. [DOI] [PubMed] [Google Scholar]
- 24. Ferrari‐Cagidiaco E., Verniani G., Keeling A., et al., “A Randomized Controlled Clinical Trial on Press and Block Lithium Disilicate Partial Crowns: A 4‐Year Recall,” American Journal of Dentistry 37, no. 2 (2024): 85–90. [PubMed] [Google Scholar]
- 25. Hassan A., Hamdi K., Ali A. I., Al‐Zordk W., and Mahmoud S. H., “Clinical Performance Comparison Between Lithium Disilicate and Hybrid Resin Nano‐Ceramic CAD/CAM Onlay Restorations: A Two‐Year Randomized Clinical Split‐Mouth Study,” Odontology 112, no. 2 (2024): 601–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pfister J. L., Federlin M., Hiller K. A., et al., “Randomized Clinical Split‐Mouth Study on Partial Ceramic Crowns Luted With a Self‐Adhesive Resin Cement With or Without Selective Enamel Etching: Long‐Term Results After 15 Years,” Journal of Adhesive Dentistry 25, no. 1 (2023): 177–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rinke S., Zuck T., Hausdörfer T., Leha A., Wassmann T., and Ziebolz D., “Prospective Clinical Evaluation of Chairside‐Fabricated Zirconia‐Reinforced Lithium Silicate Ceramic Partial Crowns‐5‐Year Results,” Clinical Oral Investigations 26, no. 2 (2022): 1593–1603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Schlichting L. H., Resende T. H., Reis K. R., Raybolt Dos Santos A., Correa I. C., and Magne P., “Ultrathin CAD‐CAM Glass‐Ceramic and Composite Resin Occlusal Veneers for the Treatment of Severe Dental Erosion: An up to 3‐Year Randomized Clinical Trial,” Journal of Prosthetic Dentistry 128, no. 2 (2022): 158.e1–158.e12. [DOI] [PubMed] [Google Scholar]
- 29. Souza J., Fuentes M. V., Baena E., and Ceballos L., “One‐Year Clinical Performance of Lithium Disilicate Versus Resin Composite CAD/CAM Onlays,” Odontology 109, no. 1 (2021): 259–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. van den Breemer C., Gresnigt M., Özcan M., Kerdijk W., and Cune M. S., “Prospective Randomized Clinical Trial on the Survival of Lithium Disilicate Posterior Partial Crowns Bonded Using Immediate or Delayed Dentin Sealing: Short‐Term Results on Tooth Sensitivity and Patient Satisfaction,” Operative Dentistry 44, no. 5 (2019): E212–e222. [DOI] [PubMed] [Google Scholar]
- 31. Zhang L., Hou X. X., Aishan M., Tian M. T., and He H. Y., “A 3‐Year Clinical Evaluation of Endodontically Treated Posterior Teeth Restored With Resin Nanoceramic Computer‐Aided Design/Computer‐Aided Manufacture (CAD/CAM)‐fabricated Partial Crowns,” Medical Science Monitor 28 (2022): e937331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Archibald J. J., G. C. Santos, Jr. , and Moraes Coelho Santos M. J., “Retrospective Clinical Evaluation of Ceramic Onlays Placed by Dental Students,” Journal of Prosthetic Dentistry 119, no. 5 (2018): 743–748.e741. [DOI] [PubMed] [Google Scholar]
- 33. Fabbri G., Zarone F., Dellificorelli G., et al., “Clinical Evaluation of 860 Anterior and Posterior Lithium Disilicate Restorations: Retrospective Study With a Mean Follow‐Up of 3 Years and a Maximum Observational Period of 6 Years,” International Journal of Periodontics and Restorative Dentistry 34, no. 2 (2014): 165–177. [DOI] [PubMed] [Google Scholar]
- 34. Lindner S., Frasheri I., Hickel R., Crispin A., and Kessler A., “Retrospective Clinical Study on the Performance and Aesthetic Outcome of Pressed Lithium Disilicate Restorations in Posterior Teeth up to 8.3 Years,” Clinical Oral Investigations 27, no. 12 (2023): 7383–7393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Naeselius K., Arnelund C. F., and Molin M. K., “Clinical Evaluation of All‐Ceramic Onlays: A 4‐Year Retrospective Study,” International Journal of Prosthodontics 21, no. 1 (2008): 40–44. [PubMed] [Google Scholar]
- 36. Offer K., Kohorst P., and Linsen S., “A Total of 1132 All‐Ceramic Single‐Tooth Restorations Show Acceptable Survival Rates up to 15 Years in a Non‐University Setting,” International Journal of Prosthodontics 35, no. 6 (2022): 815–823. [DOI] [PubMed] [Google Scholar]
- 37. Wagner J., Hiller K. A., and Schmalz G., “Long‐Term Clinical Performance and Longevity of Gold Alloy vs Ceramic Partial Crowns,” Clinical Oral Investigations 7, no. 2 (2003): 80–85. [DOI] [PubMed] [Google Scholar]
- 38. Arnetzl G. V. and Arnetzl G., “Reliability of Nonretentive All‐Ceramic CAD/CAM Overlays,” International Journal of Computerized Dentistry 15, no. 3 (2012): 185–197. [PubMed] [Google Scholar]
- 39. Chen S., Lu M., Zhu Z., and Chen W., “Clinical Performance of Two Onlay Designs for Molars After Root Canal Treatment,” Journal of Oral Science 65, no. 3 (2023): 171–175. [DOI] [PubMed] [Google Scholar]
- 40. Federlin M., Hiller K. A., and Schmalz G., “Controlled, Prospective Clinical Split‐Mouth Study of Cast Gold vs. Ceramic Partial Crowns: 5.5 Year Results,” American Journal of Dentistry 23, no. 3 (2010): 161–167. [PubMed] [Google Scholar]
- 41. Malament K. A., Margvelashvili‐Malament M., Natto Z. S., Thompson V., Rekow D., and Att W., “10.9‐Year Survival of Pressed Acid Etched Monolithic e.Max Lithium Disilicate Glass‐Ceramic Partial Coverage Restorations: Performance and Outcomes as a Function of Tooth Position, Age, Sex, and the Type of Partial Coverage Restoration (Inlay or Onlay),” Journal of Prosthetic Dentistry 126, no. 4 (2021): 523–532. [DOI] [PubMed] [Google Scholar]
- 42. Spitznagel F. A., Scholz K. J., Strub J. R., Vach K., and Gierthmuehlen P. C., “Polymer‐Infiltrated Ceramic CAD/CAM Inlays and Partial Coverage Restorations: 3‐Year Results of a Prospective Clinical Study Over 5 Years,” Clinical Oral Investigations 22, no. 5 (2018): 1973–1983. [DOI] [PubMed] [Google Scholar]
- 43. Strasding M., Sebestyén‐Hüvös E., Studer S., Lehner C., Jung R. E., and Sailer I., “Long‐Term Outcomes of All‐Ceramic Inlays and Onlays After a Mean Observation Time of 11 Years,” Quintessence International 51, no. 7 (2020): 566–576. [DOI] [PubMed] [Google Scholar]
- 44. Xiao W., Chen C., Yang T., and Zhu Z., “Influence of Different Marginal Forms on Endodontically Treated Posterior Teeth Restored With Lithium Disilicate Glass‐Ceramic Onlays: Two‐Year Follow‐Up,” International Journal of Prosthodontics 33, no. 1 (2020): 22–28. [DOI] [PubMed] [Google Scholar]
- 45. Zimmermann M., Koller C., Reymus M., Mehl A., and Hickel R., “Clinical Evaluation of Indirect Particle‐Filled Composite Resin CAD/CAM Partial Crowns After 24 Months,” Journal of Prosthodontics 27, no. 8 (2018): 694–699. [DOI] [PubMed] [Google Scholar]
- 46. Klink A. and Huettig F., “Complication and Survival of Mark II Restorations: 4‐Year Clinical Follow‐Up,” International Journal of Prosthodontics 26, no. 3 (2013): 272–276. [DOI] [PubMed] [Google Scholar]
- 47. Lu T., Peng L., Xiong F., et al., “A 3‐Year Clinical Evaluation of Endodontically Treated Posterior Teeth Restored With Two Different Materials Using the CEREC AC Chair‐Side System,” Journal of Prosthetic Dentistry 119, no. 3 (2018): 363–368. [DOI] [PubMed] [Google Scholar]
- 48. Murgueitio R. and Bernal G., “Three‐Year Clinical Follow‐Up of Posterior Teeth Restored With Leucite‐Reinforced Ips Empress Onlays and Partial Veneer Crowns,” Journal of Prosthodontics 21, no. 5 (2012): 340–345. [DOI] [PubMed] [Google Scholar]
- 49. Ozyoney G., Yan Koglu F., Tagtekin D., and Hayran O., “The Efficacy of Glass‐Ceramic Onlays in the Restoration of Morphologically Compromised and Endodontically Treated Molars,” International Journal of Prosthodontics 26, no. 3 (2013): 230–234. [DOI] [PubMed] [Google Scholar]
- 50. Schunemann H. J., Tugwell P., Reeves B. C., et al., “Non‐randomized Studies as a Source of Complementary, Sequential or Replacement Evidence for Randomized Controlled Trials in Systematic Reviews on the Effects of Interventions,” Research Synthesis Methods 4, no. 1 (2013): 49–62. [DOI] [PubMed] [Google Scholar]
- 51. Schulz K. F. and Grimes D. A., “Allocation Concealment in Randomised Trials: Defending Against Deciphering,” Lancet 359, no. 9306 (2002): 614–618. [DOI] [PubMed] [Google Scholar]
- 52. Kang M., Ragan B. G., and Park J. H., “Issues in Outcomes Research: An Overview of Randomization Techniques for Clinical Trials,” Journal of Athletic Training 43, no. 2 (2008): 215–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Hofsteenge J. W., Bresser R. A., Buijs G. J., et al., “Clinical Performance of Bonded Partial Lithium Disilicate Restorations: The Influence of Preparation Characteristics on Survival and Success,” Journal of Dentistry 142 (2024): 104828. [DOI] [PubMed] [Google Scholar]
- 54. Rodrigues S. B., Franken P., Celeste R. K., Leitune V. C. B., and Collares F. M., “CAD/CAM or Conventional Ceramic Materials Restorations Longevity: A Systematic Review and Meta‐Analysis,” Journal of Prosthodontic Research 63, no. 4 (2019): 389–395. [DOI] [PubMed] [Google Scholar]
- 55. Mostafa N. Z., Ruse N. D., Ford N. L., Carvalho R. M., and Wyatt C. C. L., “Marginal Fit of Lithium Disilicate Crowns Fabricated Using Conventional and Digital Methodology: A Three‐Dimensional Analysis,” Journal of Prosthodontics 27, no. 2 (2018): 145–152. [DOI] [PubMed] [Google Scholar]
- 56. Dolev E., Bitterman Y., and Meirowitz A., “Comparison of Marginal Fit Between CAD‐CAM and Hot‐Press Lithium Disilicate Crowns,” Journal of Prosthetic Dentistry 121, no. 1 (2019): 124–128. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


