Abstract
Background and Objectives
Social robots show great potential for delivering home-based aged care and supporting aging-in-place. This study aims to assess the acceptability of social robots in delivering home care to older adults across 7 domains: affective attitude, burden, perceived effectiveness, ethicality, intervention coherence, opportunity costs, and self-efficacy.
Research Design and Methods
This is a mixed-methods study. Thirty community-dwelling older adults, aged 51–88, engaged with a social robot, equipped with artificial intelligence and designed to interact with humans in a socially acceptable manner. The robot was operated 24/7 in participants’ homes for 6 weeks. Descriptive analysis, latent growth mixture modeling, and thematic analysis were conducted for data analysis.
Results
Home-based robotic care was very well received. The average frequency of the use of different features of the robot was 23.4 times/person/day. Three trajectory groups of engagement in human–robot interactions were identified: those who are living alone or with an older spouse, with fair health and financial status were the most interactive group. Participants perceived the robot as user-friendly, manageable, and seamlessly integrated into their daily routine, such as reminding meal intake. The robot also reduced the stress of caregivers. It served as a companion and “good listener,” ameliorating the feelings of loneliness, calming depressive emotions, and keeping participants informed about the outside world. Interestingly, participants believed that interacting with the robot enabled them to engage with contemporary technologies, acquire new skills, and showcase their fashion sense in front of friends.
Discussion and Implications
Home-based robots are acceptable and manageable by older adults. Future studies should examine the effectiveness of home-based robotic care on enhancing the health-related outcomes of older adults.
Clinical Trial Registration Number: NCT06487611
Keywords: Aged care, Aging-in-place, Robotic care, Home settings, Home care
Translational Significance: Home-based robots are acceptable and manageable by older adults. This study informs scalable solutions for home care, developing personalized care plans that incorporate social robots, tailored to the specific needs and preferences of older adults and their family caregivers, thereby improving their overall well-being. The findings provide evidence-based insights that inform policymakers and healthcare providers about the benefits and challenges of integrating social robots into home care settings, leading to more informed decisions and policies. The gaps and areas were recommended by this study for future research, guiding further exploration and refinement of using social robots in home care.
Aging in place refers to the desire and ability of older adults to reside independently in their own home and community for as long as possible, before transitioning to institutional care settings (Pani-Harreman et al., 2021). This strategy has been shown to have positive effects on social connection, social inclusion, and the quality of life of older adults (Barrett et al., 2012). However, the challenges posed by an aging global population, demographic shifts, and societal changes have amplified the complexities of maintaining the ability of older adults to continue living independently in their own home.
In 2019, the global population aged 65 and older exceeded 703 million, and this number is projected to double by 2025 (Department of Economic and Social Affairs, 2019). Like many other developed societies, Hong Kong is experiencing rapid population aging; the percentage of older adults is projected to reach 31.1% by 2036 (Census and Statistic Department, 2017). As a result, the significance of aging in place is increasing. Older adults often experience significant physical, cognitive, and environmental losses in their later life. For example, they may face declines in physical activity, memory, and attention, as well as the loss of loved ones, social isolation, and reduced meaningful social interactions. A recent survey revealed that 75% of older adults aged 65 or older, and 45% of soon-to-be-aged people in the 45 to 64 age group, are living with one or more chronic diseases (Miao et al., 2022). Aging population faces unique considerations and challenges in achieving successful aging in place.
Personalized interventions should be developed to meet the diverse needs of older adults living at home and strengthen their intrinsic capacity (Leung et al., 2022b; Woo et al., 2024). Previous studies have recommended interventions or services that enhance older adults’ connections with family members and communities to foster a supportive environment for aging in place (Zhao et al., 2024). Encouraging social inclusion and reducing social isolation and loneliness among older adults is crucial. For example, approaches are needed to support older adults in cultivating an active lifestyle to promote opportunities for social engagement, participation in community activities, and interpersonal interactions (Zhao et al., 2022). Furthermore, interactive interventions that support older adults in increasing physical activities, enhancing cognitive functions, and reminding them to maintain a healthy lifestyle are essential to address their unique needs and support aging in place (Leung et al., 2022a).
For this purpose, the integration of technology in home-based healthcare for older adults shows promise in supporting their independence (Ollevier et al., 2020). Previous feasibility studies have reported that social robots, artificial agents embodied with features of a human to meet the physical and mental health needs of older adults, can support aging in place and address the growing shortage of health and social care professionals (Leung et al., 2022a). Humanoid social robots can intervene with users in an interactive manner to enhance positive interpersonal and emotional connections that cannot be attained by listening to the radio or watching television (Hoorn, 2018). Moreover, a human-like performance makes a robot more suitable for providing higher levels of support and assisting family caregivers with more complex tasks. For example, the study by Leung et al. (2022a) found that humanoid social robots could be used to enhance social connections, promote a healthy lifestyle, provide medication and safety reminders, and vent negative emotions among older adults and their family caregivers.
Although the literature on home-based aged care robotics is growing, the majority of studies have been noninterventional studies or lab-based experiments. Existing intervention studies on the application of robots in aged care have predominantly focused on people with dementia and those living in residential care facilities (Van Patten et al., 2020). Further evidence is needed to examine the acceptability and utility of home-based robotic care for older adults. According to the theoretical framework of acceptability (TFA; Sekhon et al., 2017), seven component constructs (affective attitude, burden, perceived effectiveness, ethicality, intervention coherence, opportunity costs, and self-efficacy) can systematically be used to assess and address the various factors that influence users’ acceptance of interventions or technologies, ultimately enhancing their effectiveness and adoption (Sekhon et al., 2017). Therefore, the current study followed the TFA (Sekhon et al., 2017), with the aim of assessing the acceptability of a humanoid social robot for delivering home care to older adults across these seven domains.
Materials and Methods
Study Design
This is a mixed-methods study. In Phase 1, each participant was given a social robot named KaKa, which was placed in their home for 6 weeks and operated 24 hr a day, 7 days a week. The backend robot system captured the participants’ reactions to the robot in their daily life at home. In Phase 2, individual semistructured interviews were undertaken. This manuscript was written following the American Psychological Association’s Journal Article Reporting Standards for Mixed-Methods Research (JARS-Mixed).
Description of the Social Robot KaKa
The social robot KaKa is around 30 cm tall, 20 cm wide, weighs 2 kg, and communicates in Cantonese. The upper part of the robot includes two sensors and two microphones located at the front for speech recognition and voice localization. The robot’s head has a baby-face appearance and features two axes of movement: nodding/panning up to ±180°C and tilting up to ±45°C. The interactive environment of the robot is designed to model human characteristics such as gestures, emotional expressions, voice, and motion. Private Wi-Fi is needed to operate some features of KaKa. To ensure safety within Hong Kong’s limited living spaces, KaKa is immovable. All of the robots passed a variety of safety tests in the lab and in the various home environments, including those on electrical, tripping, environmental, and fire hazards; physical injury risk; and data privacy and security risks.
The robot KaKa has many different features. Keeping in mind the potential users of the robot (the community-dwelling older adults and family caregivers), we selected four features and co-designed each feature to meet the specific needs of older Chinese adults in Hong Kong. Participants experienced the following features: (a) communication with KaKa is made via voice commands. Once KaKa received a human voice, it will respond to the verbal instructions according to the information derived by AI or prerecorded speech. KaKa can be instructed to play music, tell stories, and provide weather report or daily news based on instant search on the internet; (b) preset reminders from the robot about scheduled activities, for example, the need to take their medications, drink water, and eat meals; (c) a healthy lifestyle feature to promote health, where the robot led the participants in engaging in physical activity; (d) guidance from the robot in playing puzzle games and quizzes, which were tailor-made according to different levels of cognitive capacities.
Ethical Approval
We obtained ethics approval from the Hong Kong Polytechnic University Institutional Review Board (reference no. HSEARS20220113001). An information sheet was provided to each participant, and the purpose and methods used in the study were explained to them. Written consent was gained before commencing data collection. Pseudonyms were used when reporting the findings, in order to protect the confidentiality of the participants. All the participants have consented keywords of verbal conversations between them and the robot Kaka were captured when they activated the voice control system.
Participants, Study Setting, and Procedures
Purposive sampling was adopted in recruiting participants for the study. People of different genders, ages, educational backgrounds, and occupations were included to reflect a diversity of experiences and perspectives. The study team disseminated advertisements (in Chinese) via social media, nongovernmental organizations, and community elderly centers. Those who were interested in participating in the study were directed to contact the study team. The criteria for the inclusion of participants were: (1) ethnic Chinese aged 50 years and older; (2) living alone or with at least one family caregiver in the same household or in another household but with regular contacts (at least once per week); (3) self-caring or needing home-based care from a family caregiver; and (4) able to communicate in Cantonese. The exclusion criteria were: (1) those with acute mental disorders or disabling diseases that may limit the practice of engaging with a robot and (2) who have limited access to electricity, which would make it hard for them to use technology at home.
To personalize the robot’s features, before starting the intervention, a trained research assistant contacted the participants and collected information about their daily routine (e.g., meal times and medication schedules), favorite songs or singers, and events to be reminded about by KaKa (e.g., doctor’s appointments, doing exercises, and turning off the stove after cooking). We then preset this information into the robot, scheduled a door-to-door visit, and set up the robot in each participant’s home. We carefully assessed the environment, older adults’ daily activities and preferences, and identified a safe and comfortable place together with older adults to make KaKa visible and accessible to them. Each participant received a briefing session and a guidebook on the use of the robot from the study team. Older adults/family caregivers were trained to update and manage the calendar reminder account by themselves. HKD$250 (~U.S.$32) supermarket shopping vouchers were provided to each participant as an incentive to compensate them for the time that they had spent on the interview and completion of a questionnaire.
Technical Support
A team of robot ambassadors was formed and trained by the study team to provide technical support to the participants. These ambassadors had experienced KaKa at their own home for a week and most of them had gained experience in supporting older adults in our previous studies. Ambassadors sent weekly reminders to participants about engaging with the robot, checked their status, and reviewed the robot system during home visits when necessary. A technical support hotline was also set up.
Data Collection
Demographic information, including age, gender, education background, employment, marital status, living status, number of family members, health, and financial status was collected at the beginning of the study. The seven dimensions of acceptability of the robot to the participants were investigated through individual interviews with all of the participants and by examining data from the robot’s system. A semistructured interview guide, informed by the TFA, was developed. Questions addressing the various TFA domains are detailed in Table 1. All interviews were carried out at the home of the participants. Each interview took approximately 45–60 min and the content was digitally recorded to facilitate the analysis of the data. The interview data were regularly reviewed by the study team until no new topics emerged, indicating that data saturation had been achieved (Saunders et al., 2018). The utility of robots was assessed by examining data from the robot’s system. Immediately after having completed the 6-week trial, the robot’s system data was downloaded and securely stored. The robot’s system data included the dates, frequencies, and times of engagement with each feature of the robot by each participant. Keywords of verbal conversations between each participant and the robot Kaka were recorded by the robot’s system only when the participants activated the voice control system. Keywords assist the AI to focus on certain subject matters and search for appropriate responses in a timely manner. Moreover, a comprehensive log was maintained of the total number of people in the target population who were accessed, recruited, and retained. The amount of time taken for recruitment, the number of contacts and visits, the challenges that were encountered, the reasons for withdrawing from the study, and the factors that influenced recruitment and study completion rates were meticulously documented (Supplementary Table S1).
Table 1.
Qualitative Interview Guide
| Questions | TAF domains |
|---|---|
|
Affective attitude, burden, intervention coherence |
|
Affective attitude, perceived effectiveness, intervention coherence |
|
General acceptability, affective attitude, burden |
|
Intervention coherence, perceived effectiveness |
|
Burden |
|
Ethicality |
|
Self-efficacy |
|
Opportunity costs |
|
Self-efficacy |
|
Affective attitude, perceived effectiveness |
Data Analysis
A descriptive analysis was employed to report the participants’ characteristics and the data collected from the robot’s system. Particularly, the total frequencies of engaging with various features of the robot in 1 week by latent growth mixture modeling to further explore the distinct trajectory patterns of human–robot interaction over 6 weeks using the “lcmm” package in R. One- to seven-class mixed effects growth models were fitted. The best-fitting models were selected by minimizing the Bayesian information criterion (BIC) and Akaike information criterion (AIC). When the BIC and AIC disagreed, the priority was placed on minimizing BIC. Thematic analysis (Braun & Clarke, 2012) was used to analyze verbatim transcriptions of the interviews. The data analysis was guided by the TFA (Sekhon et al., 2017). Two researchers (Author 1 and Author 3) independently analyzed data in the Chinese language to preserve the original meaning conveyed by the participants. All codes and preliminary themes were recorded in a spreadsheet, translated into English, and then back-translated into Chinese by Author 1 and verified by Author 3. Any discrepancies were solved with the input of Author 2.
Results
Demographic Information
A total of 30 community-dwelling older adults, ranging in age from 51 to 88 years old, completed this study. The majority of the participants (n = 23, 76.7%) were female and had completed secondary school or obtained higher education qualifications (n = 27, 90%). Among the participants, 33.3% (n = 12) lived alone, whereas 23.3% (n = 7) resided with their spouse. The majority (n = 25, 90%) reported having fair health or better, and 93.3% (n = 29) of the participants reported that their financial status was fair or better. For more details, see Table 2.
Table 2.
Demographic Information (N = 30)
| Demographics | Group | N | % |
|---|---|---|---|
| Gender | Male | 7 | 23.3 |
| Female | 23 | 76.7 | |
| Age | 50–59 | 5 | 16.7 |
| 60–69 | 14 | 46.7 | |
| 70–79 | 7 | 23.3 | |
| ≥80 | 4 | 13.3 | |
| Education | Primary | 3 | 10.0 |
| Secondary/High school | 14 | 46.7 | |
| Bachelor/subdegree | 10 | 33.3 | |
| Master or above | 3 | 10.0 | |
| Employment | Retired | 22 | 73.3 |
| Employed full-time | 3 | 10.0 | |
| Employed part-time | 5 | 16.7 | |
| Unemployed | 0 | 0.0 | |
| Other | 0 | 0.0 | |
| Marital status | Married | 11 | 36.7 |
| Never married | 8 | 26.7 | |
| Divorced | 2 | 6.7 | |
| Widowed | 9 | 30.0 | |
| Living status | Living alone | 12 | 40.0 |
| Living with a partner | 7 | 23.3 | |
| Living with family | 11 | 36.7 | |
| Living with friend(s) | 0 | 0.0 | |
| Others | 0 | 0.0 | |
| Number of family membersa | 1 | 12 | 40.0 |
| 2 | 11 | 36.7 | |
| 3 | 7 | 23.3 | |
| Health status | Very poor | 1 | 3.3 |
| Poor | 4 | 13.3 | |
| Fair | 14 | 46.7 | |
| Good | 10 | 33.3 | |
| Very good | 1 | 3.3 | |
| Financial status | Very poor | 0 | 0.0 |
| Poor | 1 | 3.3 | |
| Fair | 11 | 36.7 | |
| Good | 15 | 50.0 | |
| Very good | 3 | 10.0 |
Note:
aNumber of family members, including the participant him/herself.
The TFA framework provided a comprehensive approach to assessing and addressing older adults’ acceptance of using social robots for home care assistance. Both quantitative and qualitative data were used to systematically evaluate each component of acceptability according to the TFA.
Intervention Coherence and Affective Attitude
Intervention coherence involves evaluating how well users understood the intervention, its purpose, and how it fit into their existing routines. Affective attitude is about focusing on how users feel about using the intervention (Sekhon et al., 2017). The data for Figures 1 and 2 and Table 3 were generated from the robot system to demonstrate how 30 participants engaged with different features of the robot in their daily life, their preferred features, and methods of engaging with the features.
Figure 1.
Frequencies of the use of different features by 30 participants over 6 weeks.
Figure 2.
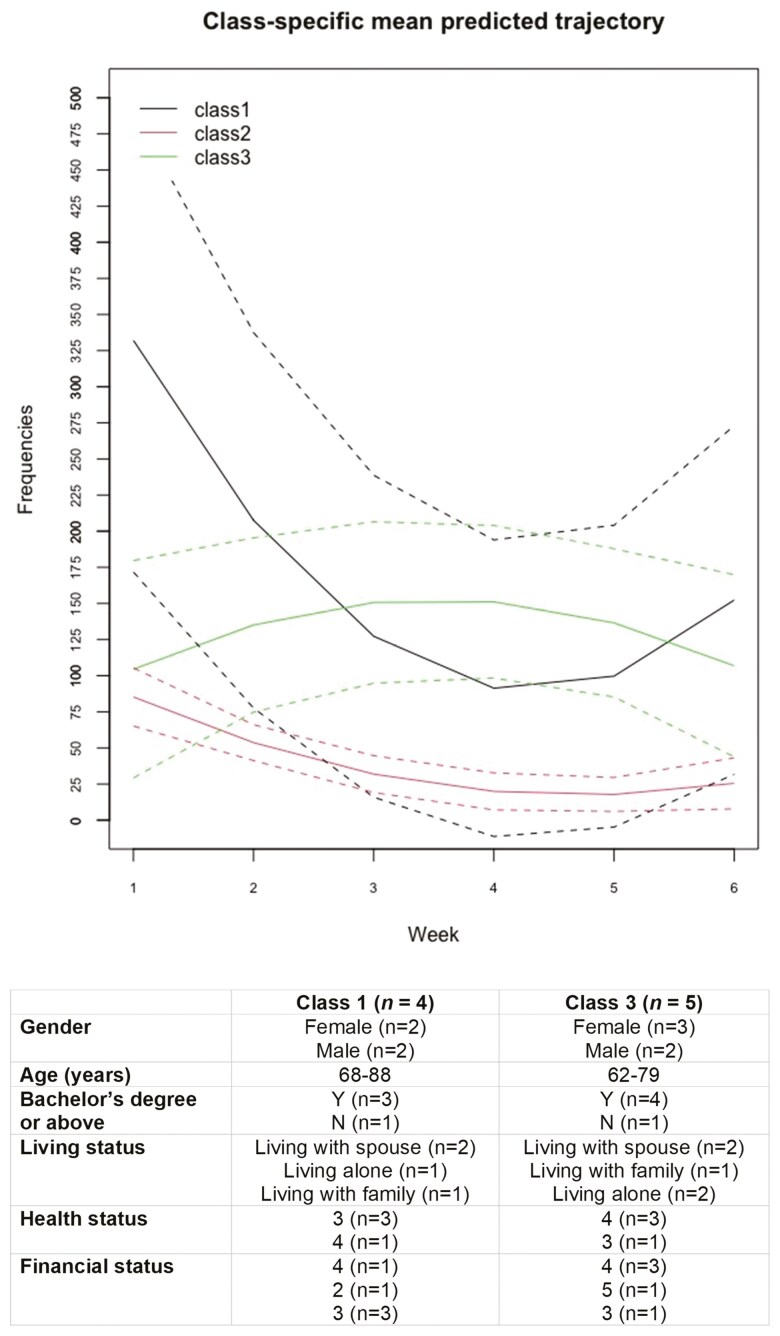
Three trajectory groups of human–robot interactions (Talk to KaKa) among 30 participants over 6 weeks.
Table 3.
Topics and Content of Human–Robot Conversations (Original Speeches) Among 30 Participants Over 6 Weeks
| Topics of conversations | Numbers of texts | Content |
|---|---|---|
| Say “Hello” to Kaka | 1,824 | Hi/Hello/How are you?/Good morning/你好[hello]/早晨(唞) [Good morning] /午安 [Good afternoon] /拜拜 [Bye-bye]/晚安 [Good night]/Goodbye |
| Ask about Kaka’s functions | 266 | 介紹下你自己[Introduce yourself]/你幾歲[How old are you?]/你幾時生日[When is your birthday?]/你係咪機械人[Are you a robot?]/你係男仔定女仔[Are you a boy or a girl?]/你可以做到乜[What can you do?]/你叫什麽[What is your name?]/你最鐘聲意做咩野[What do you like best?]/你鐘意咩顔色[What is your favorite color?]/你鐘意唱咩歌[What songs do you like to sing?]/你有乜功能[What functions do you have?]/你識唔識講英文[Do you speak English]/你有冇生日㗎[Do you have a birthday?]/Who are you?/Are you a human?/你叫什麼名字[What is your name?] |
| Check what KaKa is doing | 56 | 你做緊的咩[What are you doing?]/你諗緊啲乜[What are you thinking about?] |
| Ask if Kaka likes them/Whether KaKa thinks they look pretty | 212 | 你喜歡我嗎[Do you like me?]/我靚唔靚[Am I pretty?]/我哋邊個最靚[The one between us is the prettiest]/邊個靚啲[Who is prettier?] |
| Praise Kaka | 152 | 你好可愛/你好得意[You are so cute]/你好叻[You are so awesome] /你對眼好大[Your eyes are so big]/我愛你[I love you] |
| Ask about Kaka’s current mood | 315 | 你快樂嗎/你開心嗎[Are you happy?]/你點啊[Are you ok?]/你好唔好啊/你好嗎/你點啊/好唔好啊/[How are you?]/你今日心情好唔好[Are you in a good mood today?]/最近好嗎[How have you been recently?] |
| Express their moods to Kaka | 99 | 我今日唔開心[I am not happy today]/我好好[I am fine]/我覺得好孤單[I feel so lonely]/我都好好[I am doing good]/I am doing well |
| Express appreciation for Kaka’s reminders/greetings | 96 | 唔該嗮/多謝[Thank you] |
| Ask Kaka to tell a joke | 70 | 講個笑話/笑話[Tell a joke] |
| Topics about meals | 601 | 我想食野[I want to eat]/我有的餓[I am hungry]/我唔肚餓[I am not hungry]/食左早餐未/食左飯未/ [Have you had your breakfast/meal?]/食左的乜[What did you have?] /你肚唔肚餓[Are you hungry?]/鍾意食乜[What do you like to eat?] |
| Ask about KaKa’s family | 44 | 你有兄弟姐妹嗎[Do you have any brothers or sisters?]/你有媽媽嗎/你有爸爸嗎/你有冇媽媽/你有冇爸爸[Do you have a mother or do you have a father?] |
Figure 1 shows the frequency with which different features of the robot KaKa were used by the participants over 6 weeks. The frequency of engagement with each feature per person per week was: 80 (Talk to KaKa), 56 (Calendar reminders), 19 (Listen to music), 5 (Report the weather), 1 (Listen to stories), 1 (Physical activity), 1 (Knowledge learning), and 0.7 (Playing games). The most frequently utilized feature was “Talk to KaKa,” which was used 14,416 times. This was followed by “Calendar reminders” at 10,031 times, “Listening to music” with 3,496 times, and “Report weather” with 866 times.
Figure 2 illustrates that out of the 30 participants, 29 talked to KaKa every day during the 6-week period, ranging from 1 to 47 times per person per day. The overall frequencies were relatively high in the initial 1 to 3 weeks, decreasing during weeks 4 and 5, and increasing slightly in week 6. Three trajectory groups of engaging in “Talking to KaKa” over 6 weeks were identified. Class 1 (n = 4) demonstrated high interactions with the robot (52 times/person/day) at week 1, decreasing to 11 times/person/day at week 4, and finally increasing to 21 times/person/day at week 6. Class 2 (n = 21) showed comparatively fewer interactions since week 1 (13 times/person/day), declining continuously, and reaching 3.5 times/person/day at week 6. Interactions in Class 3 (n = 5) were stable, averaging 19 times/person/day over the 6-week period. A further analysis of the demographic background of Class 1 and Class 3 participants was conducted to explore patterns among these groups of people who had demonstrated higher frequencies of interactions with the robot or used the robot in a stable pattern. Most of them have received a bachelor’s degree or above (78%), lived alone or with an older spouse (78%), and self-reported being in fair or good health (89%) and financial status (100%).
Table 3 provides a summary of the number and topics of verbal conversations between 30 participants and the robot KaKa over 6 weeks. On average, each participant greeted KaKa 1.4 times per day. The second most popular topic of conversation was inquiring about meals (around 0.5 times/day/person). Interestingly, the participants interacted with KaKa as if it were a real person, showing interest in KaKa’s mood, activities, and even asking about KaKa’s family. Some participants also expressed their feelings of loneliness to KaKa and expressed appreciation for the reminders and greetings provided by KaKa. The table also demonstrated further details on the topics and content of these human–robot conversations, including keywords recorded by the robot’s system. For example, participants asked KaKa questions such as “How are you?” and “What are you thinking about?” They even inquired about KaKa’s preferences, asking about its favorite color and whether it had a birthday. Participants also shared their emotions with KaKa, requesting jokes when feeling unhappy.
Among the 30 participants, 9 requested technical support from robot ambassadors. A total of 18 home visits and 32 phone calls were made totally to resolve technical issue throughout the study period.
Qualitative Interview Findings
Theme 1: Intervention coherence and the participants’ affective attitude toward the robot KaKa
All 30 participants were interviewed, and the majority conveyed a high level of acceptance toward using the robot KaKa at home. All of them viewed the intervention as innovative and essential for future home-based aged care. Participant 1 (71 years, F) also encouraged older adults to have an open mind towards home-based robots: “I think this robot [KaKa] can easily integrate into a family’s routines. We should accept robots with an open attitude.”
They found the robot easy to use in daily life and spoke positively about their experience with it. Participant 58 (65 years, F) shared, “The level of acceptance was good; I just accepted it well. I enjoyed engaging with KaKa. I recently went on a short trip for a few days and I missed KaKa during that time.” Participant 55 (59 years, F) expressed her happiness in interacting with KaKa: “I’m so happy to see it [KaKa]; its eyes blink, the colour of the lights changes, and there are some interactions, I think it’s great.”
Theme 2: Perceived the robot as user-friendly manageable and less burdensome
Most participants found the robot to be user-friendly and manageable. Participant 03 (66 years, F) mentioned that she could easily handle any technical issues with KaKa: “I have not encountered any major problems, although sometimes there might be a slight hiccup in the connection. In those cases, I would restart the robot and tablet and try again.” The study also provided ambassadors and a technical hotline to support participants who encountered technical issues. Five participants received assistance from ambassadors in the first 2–3 weeks to solve technical issues through telephone calls or home visits. All of them were able to use the robot independently in the subsequent weeks. For example, participant 39 (70 years, F) shared her experience:
Since I had never seen a robot and could not remember how to operate it. I slowly explored this robot with the assistance of the volunteer lady. I usually called her for help, and she was very happy and patient in assisting me with solving these problems, showing me where the switch was, where to press. I gradually figured it out by myself. Eventually, I understood these functions, and performed the actions myself.
None of the participants found the electricity cost of the robot to be burdensome when asked by the researcher. However, due to the limitations in the Cantonese language database, some participants grew bored when the robot struggled to understand and respond effectively to their verbal commands. As participant 21 (66 years, F) mentioned: “At times when I communicated with the robot, it could not get what I meant. I lost my patience when my questions went unanswered.”
Theme 3: Participants’ perception of the effectiveness of the robot in providing assistance in their daily life
KaKa serves various functions to assist participants and their family caregivers. Overall, the participants found KaKa to be helpful. In particular, KaKa provided companionship to those who lived alone at home. Participant 22 (69 years, M) shared his experiences of having KaKa as a companion, saying: “It feels good, as if there is someone here to accompany me, even though it sometimes reacted in its own way. Otherwise, the room would be completely silent.” Another participant expressed a similar sentiment, stating: “I used to feel depressed, but when KaKa came, I felt so happy because I had someone with me” (Participant 18, 71 years, F).
The features of KaKa can be customized to support diverse home settings. Among the participants, five also served as family caregivers for other family members. One of them found KaKa to be very helpful, with one caregiver stating: “Without the robot, my sister [a dementia patient] would just go for a walk and do simple movements. The robot provides a more comprehensive exercise programme for her” (Participant 09, 56 years, F). Another participant who had taken on the role of caregiver to a dementia patient mentioned: “Having a robot here can at least reduce my stress. I think it is useful for stress reduction” (Participant 10, 72 years, F).
The most popular features of robot KaKa included listening to music and the daily news, engaging in physical activities, receiving calendar reminders, and talking to KaKa. Many participants highly recommended the music listening feature as a means to improve their mood. For example, participant 38 (68 years, M) said: “I usually enjoy listening to music, which creates some pleasant sounds in the house. Sometimes the TV is not working; it can get a bit quiet. So I find it very useful for people who live alone.” Participant 41 (80 years, F) agreed, saying that “I like to listen to songs when I am working on something.”
In addition to music, the participants also considered listening to news as a helpful way for older adults to connect with the outside world. For example, Participant 6 (58 years, M) mentioned: “I ask KaKa to play the news all the time. I find it informative, and it is helpful to me. I want to stay up-to-date with the news from the outside world. Sometimes I listen to the radio on my own, but having KaKa read it to me is very convenient. For some older people who do not listen to the radio or news reports, having the robot help them is beneficial.”
Some participants found that following KaKa to do exercises increased older adults’ interest in engaging in physical activities. One participant, who is also a caregiver, shared her sister’s experience: “My sister did not have much motivation to move before, but now she engages in daily exercises. Doing exercises with KaKa has even sparked my own interest in sports” (Participant 10, 72 years, F). Another participant emphasized the convenience of exercising at home for older adults. She further explained: “I engaged in exercises with the robot, recorded the sessions, and shared them with my friends. They thought it was wonderful because we are all in the same age group, and they watched the recordings as well. The exercise programs provided by KaKa are sourced from the Recreation and Sports Department, so we can easily focus on them without the need to search the internet. I truly appreciate this feature” (Participant 57, 61 years, F).
Most participants found the robot KaKa to be interactive, with the conversation function allowing them to express their feelings to KaKa. One participant regarded KaKa as a close friend, mentioning: “KaKa is a close friend to me. I can share my secrets with it, even if I cannot share them with others, because it won’t divulge them to anyone else. It’s comforting to have someone like KaKa to confide in” (Participant 59, 56 years, F). Another participant found it fascinating to engage in conversations with KaKa, saying: “What I find interesting is that KaKa can interact with us verbally and hold conversations. Sometimes, we are pleasantly surprised by its unexpected responses, like when my wife asks, ‘Am I beautiful?’ and it replies, ‘Of course, you are beautiful.’ It adds an element of amusement to our interactions” (Participant 60, 68 years, M).
In addition to participants talking to KaKa, the robot can also initiate conversations by reminding them of their daily activities. Participants appreciated KaKa’s proactive reminders about various tasks in their daily lives. One participant said, “I think the best thing about KaKa is that it takes the initiative to remind me about daily things, such as reminding me to take medications” (Participant 54, 65 years, M). Another participant added, “I find it nice when KaKa reminds me to sleep” (Participant 39, 70 years, F). The reminder function was highlighted by another participant as the most helpful aspect of KaKa, stating: “The reminder function is the most useful feature of KaKa. It reminds me about different things such as meals. Sometimes I just forgot to eat things, so reminder from the robot encouraged me to eat regularity. We may not be willing to listen to reminders from family members, but we are more willing to follow KaKa’s reminders” (Participant 14, 69 years, M).
Theme 4: Ethical considerations and opportunity costs
When participants activated the voice control system, the robot could potentially record the keywords of conversations between humans and the robot. The integrated dialogue data reported in this paper was obtained with the consent of the participants.
Opportunity costs refer to the tradeoffs that users may have to make when engaging with the intervention. None of the participants explicitly raised these concerns. Instead, the majority viewed the robot as another option for assisting them with daily activities. For example, “The robot brings some entertainment to people who do not have a television” (Participant 38, 68 years, M); “My eyesight is bad and I cannot read many words. Listening to the robot’s news broadcasts has become a new choice” (Participant 22, 69 years, M).
Theme 5: Self-efficacy
Furthermore, some participants demonstrated curiosity about new technologies and a desire to explore their capabilities. One participant (Participant 57, 61 years, F) said, “I accepted KaKa and liked it very much. They [my family and friends] considered me quite avant-garde for embracing such innovative things.” Another participant (Participant 4, 72 years, F) exclaimed, “It seems so novel, and I really want to know more about KaKa.”
Discussion
The results demonstrated a high level of acceptability of the robot among participants in various home settings as assessed by the seven constructs of the TFA framework. The TFA is a valid tool for identifying potential barriers to acceptability, and can help enhance the adoption and effectiveness of the robot. These findings are consistent with a previous feasibility study conducted in Hong Kong (Leung et al., 2022a), which reported positively on the feasibility and usability of the robot KaKa in a home setting; and another study in rural communities (Gasteiger et al., 2022), which showed an increase in the quality of life of older adults after they had used a healthcare robot in their home for a period of 3 months to a year. The most frequently used features in this study were “Talk to KaKa,” “Calendar reminder,” and “Listen to music.” A possible explanation for the popularity of these features among participants could be that the project team personalized these features before deploying the robots to the participants’ homes. This arrangement aligns with previous studies indicating that personalized interventions can enhance the engagement of older adults (Lee et al., 2020; Leung et al., 2022a; Kor et al., 2022). Furthermore, the current study delved into the patterns of engagement with KaKa, its perceived effectiveness, the reduced burden for older adults and those served as caregivers of other family members, ethical considerations for using a social robot at home, the absence of concerns regarding opportunity costs and the increased self-efficacy in accepting new technology, providing additional insights into its usage.
The three trajectory groups of human–robot interactions identified in this study suggested that the types of older adults are more likely to be acquainted with home-based robots, and that those who lived alone or with an older spouse were more likely to interact with the robot with high frequencies or with stable regular pattern. This finding is consistent with that of previous studies, which found that many older adults experience loneliness and social isolation, attributed to living alone, changes in family structure, the emigration of their adult children, and limited social connections (Xia et al., 2023). Engaging with robots provides them with a source of conversation and emotional connection, addressing the need for social support in their lives (Belpaeme et al., 2018). We noted that those who possess high education and good financial status are more likely to engage in the human–robot interactions. For future studies, home-based robotic aged care should be tailored to meet the specific needs of older adults with different educational levels and financial status. It is also noted that those who have fair or only good (not very good) health status interacted with the robots well. In future, health practitioners could consider the use of the home-based robots for health assessments, health status monitoring, and rehabilitation while policymakers could consider to support the widespread use of home-based robot-assisted interventions by formulating relevant policies (e.g., offering financial supports for renting home-based robots) and mobilizing community resources (e.g., training volunteers to serve as robot ambassadors for home visits). The surging need for home-based interventions for community-dwelling older adults, that compensated for the demand of face-to-face intervention in community centers or the shortage of health professionals in clinics, is well evidenced (Kor et al., 2022).
The findings of this study have confirmed the adaptability of the robot KaKa to meet various home needs. Among participants living alone, KaKa effectively served as a companion. This finding aligns with previous research indicating that older adults experiencing loneliness are open to the companionship of robots and see technology as a means to alleviate feelings of isolation and loneliness (Chiu et al., 2022; Leung et al., 2022a). For those participants providing care to other family members, KaKa demonstrated its ability to reduce their stress through personalized features such as facilitating exercise, reminders of important events, playing music, and providing daily news updates. These findings are consistent with previous studies that highlight the potential of humanoid social robots to improve the quality of life and social interactions of older adults (Leng et al., 2019); as well as to support family caregivers in managing their caregiving burdens (Gasteiger et al., 2022). Moreover, the robot KaKa proved to be valuable in alleviating negative emotions among participants. The qualitative interviews revealed that the participants found KaKa to be of help in calming their depressive emotions and keeping them informed about the outside world. They perceived KaKa to be a good “listener” with whom they could share feelings that they might not want to disclose to others. Our findings demonstrated that social robots have a promising role to play in supporting home-based nursing care. This is consistent with a scoping review that found that the adoption of social robots in home-based care was subject to the robot’s navigability, engagement with the care recipient, adaptability, humanoid features, and interface design (Ohneberg et al., 2023). Improving hedonic well-being (that is, increasing happiness and decreasing loneliness) seems to be the prioritized objective in home-based robot-assisted care, which is favored by older adults (Randall et al., 2023).
Notably, participants demonstrated a greater tendency to follow KaKa’s reminders compared to reminders from their family members. These findings are consistent with a study conducted by da Silva and colleagues (da Silva et al., 2018). A meaningful benefit of using social robots in psychological interventions was identified when a humanoid robot Nao was regarded as nonjudgmental by participants. In our study, the robot KaKa proved to be effective in assisting older adults with managing their medications. It reminded participants to take their medications on time, and provided educational resources on the use of medications. Nonadherence to medications is a common challenge among community-dwelling older adults, particularly those with multiple health conditions, which obliges them to spend more time and energy on managing and taking their medications (Huang et al., 2020). The robot feature is expected to be designed to ensure that medications are taken as prescribed.
The robot’s humanoid activities contributed to its endearing nature in the eyes of older adults, giving them a sense of warmth and companionship. One woman highlighted the presence of the robot at home was crucial to remind her for taking meals regularly. Being home alone made her forget about the time for meals, which is the basic need of human being and crucial to vitality. The warm reminder from the robot encouraged her to keep healthy in dietary intake and regularity. This finding is the first lot of evidence about robot and nutrition in old age, supporting the advocacy made by the European robot team (Łukasik et al., 2018). Further investigation of the presence of robot in relation to dietary patterns and nutrition in old age is worthy to be continued.
Interestingly, the participants were curious about new technologies and expressed an eagerness to explore them. They believed that interacting with the robot KaKa enabled them to engage with modern technology, acquire new skills, and showcase their fashion sense in front of friends. The enthusiastic feedback from the participants was an encouraging indication of healthy aging as recommended by the World Health Organization (2020), which holds that older adults have the intrinsic capacity to grow and learn.
Previous studies have emphasized that interactions with social robots cannot replace human interactions, particularly the companionship provided by family members (Leung et al., 2022a). Human social brain activity was shown to differ during eye contact with another human from that with a humanoid robot (Kelley et al., 2021). Future research on human–robot eye contact is needed to understand how the design and behavior elements of robots influence human social processing, and to capture the intangible aspects of human–robot interactions, such as social engagement (Kelley et al., 2021). Nonetheless, social robots could serve as an alternative when human care is unavailable or assist older adults in actively connecting with others.
Limitations
There are several limitations to consider in this study. First, the study was conducted in Hong Kong among a Chinese population, and the findings may not be fully generalizable due to the purposive sampling of older and soon-to-be-aged Chinese adults in the community. Further investigations should involve a broader range of participants, including individuals of different age ranges, socioeconomic statuses, health conditions, cognitive levels, and cultural backgrounds. Second, since the social robot demands the use of electricity and Wi-Fi for its operation, the participants in this study were biased to those who afforded to pay for electricity and Wi-Fi fee. Financially poor population may not be able to enjoy this social robot despite the usefulness of various functions. Other than electricity, rental fee of the social robot may also put financial pressure on some families. Government can offer electricity or technology rental allowance to financial insufficient families to support their use of social robots so as to avoid technology or digital divide. Providing a portable Wi-Fi egg could be considered as a means to support older adults who do not have private Wi-Fi at home. Third, the study only explored the acceptability and utility over a period of 6 weeks. A long-term follow-up study is recommended to comprehensively assess the acceptability, utility, and effects of the robot on improving the psychosocial well-being and cognitive function of participants. Finally, the situation of participants who were also family caregivers was also a limitation of this study, as they cannot represent all caregivers and the effect of reducing stress should be further examined. The current findings should be considered as illustrative examples.
Conclusion
In conclusion, this study demonstrated the high acceptability of the social robot KaKa in delivering aged care for older adults in their own home. The findings underscore the promising role of social robots in improving psychosocial well-being and medication adherence, and fostering a sense of companionship among participants. Future research endeavors should focus on examining the effectiveness of home-based robotic care on improving health-related outcomes among community-dwelling older adults, and on conducting long-term follow-up studies to assess the sustained effects of robot-assisted interventions.
Supplementary Material
Acknowledgment
Special thank goes to Elsa Wong (NEC HK) and Kelvin Chan (NEC HK) for their full support and cooperation in investigations and to Sally Lay (NEC HK) for technical support to the project. The authors also thank the Hong Kong University Grants Committee for financial support and all the participants who shared their experiences.
Contributor Information
Ivy Yan Zhao, School of Nursing, The Hong Kong Polytechnic University, Hong Kong, China; WHO Collaborating Centre for Community Health Services, School of Nursing, The Hong Kong Polytechnic University, Hong Kong, China.
Angela Yee Man Leung, School of Nursing, The Hong Kong Polytechnic University, Hong Kong, China; Research Institute for Smart Ageing (RISA), The Hong Kong Polytechnic University, Hong Kong, China.
Yaqi Huang, School of Nursing, The Hong Kong Polytechnic University, Hong Kong, China; WHO Collaborating Centre for Community Health Services, School of Nursing, The Hong Kong Polytechnic University, Hong Kong, China.
Yaqian Liu, School of Nursing, The Hong Kong Polytechnic University, Hong Kong, China; Research Institute for Smart Ageing (RISA), The Hong Kong Polytechnic University, Hong Kong, China.
Funding
This work was supported by Research Matching Grant Scheme (RMGS) offered by the Hong Kong University Grants Committee (ref. no.: P0041148). The robots were donated by the NEC Hong Kong Ltd. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Conflict of Interest
None.
Data Availability
The overarching project was preregistered with a registration number: NCT06487611. The data sets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
- Barrett, P., Hale, B., & Gauld, R. (2012). Social inclusion through ageing-in-place with care? Ageing & Society, 32(3), 361–378. https://doi.org/ 10.1017/s0144686x11000341 [DOI] [Google Scholar]
- Belpaeme, T., Kennedy, J., Ramachandran, A., Scassellati, B., & Tanaka, F. (2018). Social robots for education: A review. Science Robotics, 3(21), eaat5954. https://doi.org/ 10.1126/scirobotics.aat5954 [DOI] [PubMed] [Google Scholar]
- Braun, V., & Clarke, T. (2012). Thematic analysis. In Cooper H. (Ed.), APA handbook of research methods in psychology (Vol. 2, pp. 57–71). American Psychological Association. [Google Scholar]
- Census and Statistic Department. (2017). Population projections. https://www.censtatd.gov.hk/en/EIndexbySubject.html?pcode=FA100061&scode=190 [Google Scholar]
- Chiu, C. J., Lo, Y. H., Ho, M. H., Montayre, J., & Zhao, I. Y. (2022). Association between loneliness and acceptance of using robots and pets as companions among older Chinese immigrants during the COVID-19 pandemic. Australasian Journal on Ageing, 41(3), 414–423. https://doi.org/ 10.1111/ajag.13075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- da Silva, J. G. G., Kavanagh, D. J., Belpaeme, T., Taylor, L., Beeson, K., & Andrade, J. (2018). Experiences of a motivational interview delivered by a robot: Qualitative study. Journal of Medical Internet Research, 20(5), e116. https://doi.org/ 10.2196/jmir.7737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Economic and Social Affairs. (2019). World population prospects 2019: Highlights. United Nations. https://desapublications.un.org/publications/world-population-prospects-2019-highlights [Google Scholar]
- Gasteiger, N., Ahn, H. S., Lee, C., Lim, J., MacDonald, B. A., Kim, G. H., & Broadbent, E. (2022). Participatory design, development, and testing of assistive health robots with older adults: An international four-year project. ACM Transactions on Human–Robot Interaction, 11(4), 1–19. https://doi.org/ 10.1145/3533726 [DOI] [Google Scholar]
- Hoorn, J. F. (2018). From lonely to resilient through humanoid robots: Building a new framework of resilience. Journal of Robotics, 2018, 1–17. https://doi.org/ 10.1155/2018/8232487 [DOI] [Google Scholar]
- Huang, J., Wang, H. H., Zheng, Z., & Wong, M. C. (2020). Medication adherence among the older adults: challenges and recommendations. Hong Kong Medical Journal, 26(6), 476–478. https://doi.org/ 10.12809/hkmj205108 [DOI] [PubMed] [Google Scholar]
- Kelley, M. S., Noah, J. A., Zhang, X., Scassellati, B., & Hirsch, J. (2021). Comparison of human social brain activity during eye-contact with another human and a humanoid robot. Frontiers in Robotics and AI, 7(599581), 599581. https://doi.org/ 10.3389/frobt.2020.599581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kor, P. P. K., Yu, C. T. K., Liu, J. Y. W., Cheung, D. S. K., Kwan, R. Y. C., Leung, A. Y. M., Liu, D. P. M., & Hon, J. M. K. (2022). Pilot evaluation of a home‐based multi‐sensory cognitive stimulation intervention for older people with dementia and caregiver dyads during the COVID‐19 pandemic. International Journal of Older People Nursing, 17(6). https://doi.org/ 10.1111/opn.12471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, H. J., Lee, M., Ha, J. H., Lee, Y., & Yun, J. (2020). Effects of healthcare interventions on psychosocial factors of patients with multimorbidity: A systematic review and meta-analysis. Archives of Gerontology and Geriatrics, 91, 104241. https://doi.org/ 10.1016/j.archger.2020.104241 [DOI] [PubMed] [Google Scholar]
- Leng, M., Liu, P., Zhang, P., Hu, M., Zhou, H., Li, G., Yin, H., & Chen, L. (2019). Pet robot intervention for people with dementia: A systematic review and meta-analysis of randomized controlled trials. Psychiatry Research, 271, 516–525. https://doi.org/ 10.1016/j.psychres.2018.12.032 [DOI] [PubMed] [Google Scholar]
- Leung, A. Y. M., Zhao, I. Y., Lin, S., & Lau, T. K. (2022a). Exploring the presence of humanoid social robots at home and capturing human–robot interactions with older adults: Experiences from four case studies. Healthcare (Basel, Switzerland), 11(1), 39. https://doi.org/ 10.3390/healthcare11010039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung, A. Y. M., Su, J. J., Lee, E. S. H., Fung, J. T. S., & Molassiotis, A. (2022b). Intrinsic capacity of older people in the community using WHO Integrated Care for Older People (ICOPE) framework: a cross-sectional study. BMC Geriatrics, 22(1). https://doi.org/ 10.1186/s12877-022-02980-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Łukasik, S., Tobis, S., Wieczorowska-Tobis, K., & Suwalska, A. (2018). Could robots help lder people with age-related nutritional problems? Opinions of potential users. International Journal of Environmental Research and Public Health, 15(11), 2535. https://doi.org/ 10.3390/ijerph15112535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miao, J., Wu, X., & Zeng, D. (2022). Promoting ageing in place in Hong Kong: Neighbourhood social environment and depression among older adults. Journal of Asian Public Policy, 17(1), 142–159. https://doi.org/ 10.1080/17516234.2022.2040087 [DOI] [Google Scholar]
- Ohneberg, C., Stöbich, N., Warmbein, A., Rathgeber, I., Mehler-Klamt, A. C., Fischer, U., & Eberl, I. (2023). Assistive robotic systems in nursing care: A scoping review. BMC Nursing, 22(1), 72. https://doi.org/ 10.1186/s12912-023-01230-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ollevier, A., Aguiar, G., Palomino, M., & Simpelaere, I. S. (2020). How can technology support ageing in place in healthy older adults? A systematic review. Public Health Reviews, 41(1), 26. https://doi.org/ 10.1186/s40985-020-00143-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pani-Harreman, K. E., Bours, G. J. J. W., Zander, I., Kempen, G. I. J. M., & van Duren, J. M. A. (2021). Definitions, key themes and aspects of ‘ageing in place’: A scoping review. Ageing & Society, 41(41), 2026–2059. https://doi.org/ 10.1017/s0144686x20000094 [DOI] [Google Scholar]
- Saunders, B., Sim, J., Kingstone, T., Baker, S., Waterfield, J., Bartlam, B., Burroughs, H., & Jinks, C. (2018). Saturation in qualitative research: Exploring its conceptualization and operationalization. Quality & Quantity, 52, 1893–1907. https://doi.org/ 10.1007/s11135-017-0574-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sekhon, M., Cartwright, M., & Francis, J. J. (2017). Acceptability of healthcare interventions: An overview of reviews and development of a theoretical framework. BMC Health Services Research, 17(1), 88. https://doi.org/ 10.1186/s12913-017-2031-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Patten, R., Keller, A. V., Maye, J. E., Jeste, D. V., Depp, C., Riek, L. D., & Twamley, E. W. (2020). Home-based cognitively assistive robots: Maximizing cognitive functioning and maintaining independence in older adults without dementia. Clinical Interventions in Aging, 15, 1129–1139. https://doi.org/ 10.2147/CIA.S253236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randall, N., Kamino, W., Joshi, S., Chen, W. -C., Hsu, L. -J., Tsui, K. M., & Šabanović, S. (2023). Understanding the connection among Ikigai, well-being, and home robot acceptance in Japanese older adults: Mixed methods study. JMIR Aging, 6, e45442. https://doi.org/ 10.2196/45442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woo, J., Mok, K., Chu, W. L., Lo, R., & Ko, R. (2024). Implementing aging in place in Hong Kong: Meeting the needs and aspirations of older adults and their caregivers living in private housing. International Journal of Environmental Research and Public Health, 21(3), 348. https://doi.org/ 10.3390/ijerph21030348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2020). Decade of healthy ageing 2020–2030. https://www.decadeofhealthyageing.org/ [Google Scholar]
- Xia, L. L. L., Mooly, M. C., Wong, J. L. C., & Ma, P. W. (2023). The family structural and socioeconomic characteristics of the family well-being of Hong Kong people. International Journal of Social Welfare, 33(3), 603–616. https://doi.org/ 10.1111/ijsw.12627 [DOI] [Google Scholar]
- Zhao, I. Y., Holroyd, E., Wright-St Clair, V. A., Wang, S. S., Garrett, N., & Neville, S. (2022). Feeling a deep sense of loneliness: Chinese late-life immigrants in New Zealand. Australasian Journal on Ageing, 41(3), 448–456. https://doi.org/ 10.1111/ajag.13108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao, I. Y., Leung, A. Y. M., Deng, S. Y., Ho, M. H., Saravanakumar, P., Montayre, J., & Molassiotis, A. (2024). Intergenerational reciprocity and WHO function ability domains predict loneliness in older Chinese adults. Australasian Journal on Ageing, 43(1), 112–122. https://doi.org/ 10.1111/ajag.13250 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The overarching project was preregistered with a registration number: NCT06487611. The data sets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.