Abstract
Objective: To investigate the association between clinical factors, oral dose-volume parameters during radiotherapy for nasopharyngeal carcinoma (NPC), and the development of severe radiation-induced oral mucositis (ROM). It also aims to identify predictive risk factors for severe ROM to support preventive strategies. Methods: Clinical data from 175 NPC patients treated at Jiangxi Cancer Hospital between July 2023 and February 2024 were analyzed. The associations between clinical factors, oral dose-volume parameters, and severe ROM were assessed using univariate and multivariate logistic regression analyses. Results: The incidence of severe ROM was 34.3% (60/175). Univariate analysis demonstrated significant correlations between severe ROM and dose-volume parameters, including V30 (t = 2.497, P = 0.013), V35 (t = 3.348, P = 0.001), V40 (t = 3.344, P = 0.001), V45 (t = 3.289, P = 0.001), V50 (t = 3.291, P = 0.001), and the mean dose (Dmean) (t = 3.863, P < 0.001). Multivariate analysis identified oral mucosal V35 and Dmean as independent risk factors for severe ROM. Receiver operating characteristic (ROC) curve analysis determined a cutoff value of 37.38% for oral V35, with an area under the curve (AUC) of 0.652 (95% CI: 0.565-0.738, P = 0.044). For Dmean, the cutoff value was 3471.4 cGy, with an AUC of 0.666 (95% CI: 0.580-0.751, P < 0.001). Conclusion: The irradiated oral mucosa volume at V35 and Dmean are independent predictors of severe oral mucositis in NPC patients undergoing radiotherapy. These findings highlight the importance of optimizing oral dose constraints to mitigate ROM severity and improve treatment tolerability.
Keywords: Nasopharyngeal carcinoma, radiotherapy, severe oral mucositis, risk factors, dose-volume parameters
Introduction
Nasopharyngeal carcinoma (NPC) is one of the most prevalent malignancies in China, with its incidence demonstrating notable geographical variation worldwide. The highest rates are reported in regions such as Southeast Asia and North Africa, with southern China also recognized as a high-prevalence area [1]. Radiotherapy remains the cornerstone of NPC treatment, playing a critical role in tumor control, metastasis prevention, and improving both survival rates and quality of life [2]. However, radiotherapy is often associated with significant adverse effects, particularly mucositis. Studies show that over 90% of cases develop mucositis to varying degrees during radiotherapy, with nearly all affected when undergoing concurrent chemoradiotherapy [3].
Radiation-induced oral mucositis (ROM) is the most common radiotherapy-related adverse effect, manifesting as inflammation, erythema, swelling, erosion, and ulceration of the oral mucosa. These symptoms severely impair functions such as eating, chewing, swallowing, and speaking. ROM is also associated with complications including malnutrition, pain, infections, and bleeding, all of which collectively diminish patients’ quality of life and compromise treatment outcomes [4,5]. The severity and progression of ROM are influenced by multiple factors, including radiation dose, treatment duration, delivery techniques, and irradiated volume, as well as patient-specific variables such as comorbidities, genetic predisposition, and oral hygiene practices [6].
In recent years, increasing attention has been paid to factors influencing ROM during radiotherapy for nasopharyngeal cancer, particularly the oral irradiated dose. This refers to the radiation absorbed by the oral mucosa, commonly expressed as the mean oral cavity dose (MOCD) or the oral cavity dose-volume histogram (OCDVH). Previous research has demonstrated a strong correlation between higher radiation doses to the oral cavity and increased incidence and severity of ROM [7]. Studies on patients with head and neck malignancies have shown that restricting the cumulative oral cavity radiation dose to below 32 Gray (Gy) significantly reduces the risk of severe mucositis (grade 2: 25%; grade 3: 0%) [8,9]. These findings highlight the importance of optimizing dose constraints to minimize ROM-related morbidity.
Despite these advances, no consensus has been reached regarding the specific dosimetric thresholds that effectively reduce the risk of ROM in NPC patients. This study systematically investigated the influence of oral dose-volume parameters on ROM severity, aiming to identify key dose constraints that could inform and refine radiotherapy protocols. By providing novel insights into the relationship between oral cavity irradiation and ROM, this study seeks to enhance treatment strategies and offer practical guidance for optimizing NPC radiotherapy to improve patient outcomes.
Materials and methods
Source of cases and basic information
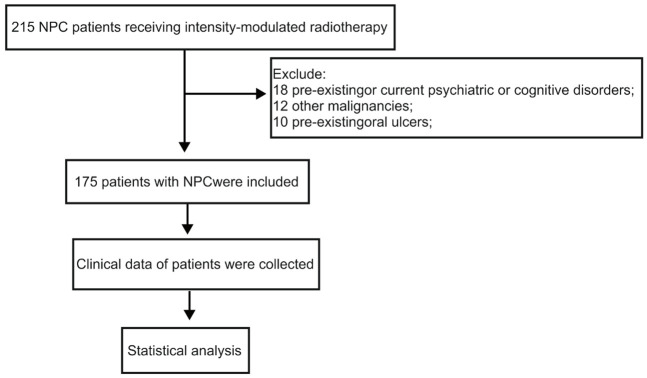
This study enrolled 175 patients with NPC who were admitted to Jiangxi Cancer Hospital between July 2023 and February 2024. All patients underwent CT simulation for radiotherapy planning and received intensity-modulated radiotherapy (IMRT) at a dose of 2.12 Gy per fraction, administered five days per week, for a total dose of 69.96 Gy. Inclusion criteria: age between 18 and 70 years; newly diagnosed, histopathologically confirmed, and previously untreated NPC; an Eastern Cooperative Oncology Group performance status (ECOG PS) score of ≤ 1; and stage I to IVA disease, according to the 8th edition of the Union for International Cancer Control (UICC) staging system [10]. Exclusion criteria: pre-existing or current psychiatric or cognitive disorders; concurrent malignancies; pre-existing oral ulcers before radiotherapy; a history of prior radiotherapy to the head and neck region. A flow chart illustrating the patient selection process is presented in Figure 1. This study was approved by the Ethical Review Committee of Jiangxi Cancer Hospital (Approval No. 2023ky080).
Figure 1.
Patient selection process for this study.
Data extraction
Clinical factors assessed in this study included patient sex, age, body mass index (BMI), smoking history, alcohol consumption history, clinical stage, and whether the patients received induction chemotherapy (IC), concurrent chemotherapy (CCRT), immunotherapy, or targeted therapy. Oral cavity contours were delineated based on contrast-enhanced CT images. The anatomical boundaries of the oral cavity were defined as follows: the hard palate (the upper border), the buccal mucosa surrounding the teeth (the anterior border), the floor of the mouth (the lower border), and the surface of the tongue and the position of the uvula (the posterior border). To evaluate the dosimetric impact on the development of severe oral mucositis (SOM), the following dose-volume parameters were analyzed: V20 (%), V25 (%), V30 (%), V35 (%), V40 (%), V45 (%), and V50 (%), as well as the mean dose to the oral cavity (Dmean, in centigray (cGy)) and the maximum dose (Dmax, cGy).
Outcome measures
The primary outcome was the incidence of severe radiation-induced ROM, defined as grade ≥ 3 according to the Radiation Therapy Oncology Group (RTOG). ROM severity was assessed using the RTOG grading scale for acute radiation injury, which classifies ROM into five grades (0-4). Grade 0: no observable changes; Grade 1: mucosal congestion with mild pain not requiring analgesics; Grade 2: patchy mucositis with inflammatory or bloody exudate, moderate pain, requiring analgesics; Grade 3: confluent fibrinous mucositis, severe pain, requiring narcotic analgesics; Grade 4: ulceration, hemorrhage, and necrosis.
Secondary outcomes included the analysis of dose-volume parameters (V30-V50, Dmean, Dmax) and their association with ROM severity.
Statistical analysis
Statistical analyses were performed using IBM SPSS version 25.0 and GraphPad Prism version 9. Continuous variables that followed a normal distribution were presented as mean ± standard deviation and were analyzed by independent samples t-tests. For data that did not follow a normal distribution, the Mann-Whitney U test (rank-sum test) was applied. Categorical variables were expressed as frequencies and percentages, with group comparisons conducted using the chi-square test. Multivariate analysis was conducted using binary logistic regression. Receiver operating characteristic (ROC) curve analysis was used to determine optimal cutoff values for key dosimetric parameters. A P-value < 0.05 was considered statistically significant.
Results
Incidence of ROM and patient characteristics
Among the 175 patients with NPC, 40 cases experienced mild ROM (grade 0-1), 75 cases developed moderate ROM (grade 2), and 60 cases had severe ROM (grade 3). Notably, no cases of grade 4 ROM were observed. The overall incidence of severe ROM (≥ grade 3) was 34.3% (60/175), underscoring the substantial burden of this adverse effect during radiotherapy. To identify potential risk factors, various clinical parameters were assessed, including sex, age, BMI, T category, N category, clinical stage, IC, CCRT, targeted therapy, immunotherapy, smoking history, and alcohol consumption. The distribution of these variables is detailed in Table 1. Univariate and multivariate logistic regression analyses revealed no significant differences in baseline clinical characteristics between the severe and non-severe ROM groups (all P > 0.05). Specifically, factors such as gender, age, BMI, tumor staging (T and N categories), clinical stage, treatment modalities (IC, CCRT, targeted therapy, and immunotherapy), as well as lifestyle factors like smoking and alcohol consumption, were not significantly associated with the development of severe ROM (Tables 1, 2). These findings suggest that while ROM is a prevalent side effect, its severity may be influenced by factors beyond conventional clinical and demographic parameters.
Table 1.
Associated between clinical factors with severe ROM analyzed by univariate analysis
| Variable | ROM (n = 115) | Severe ROM (n = 60) | χ2 | P value | |
|---|---|---|---|---|---|
| No. (%) | No. (%) | ||||
| Sex | Male | 87 (75.7) | 46 (76.7) | 0.022 | 0.881 |
| Female | 28 (24.3) | 14 (23.3) | |||
| Age (year) | ≤ 52 | 63 (54.8) | 27 (45) | 1.511 | 0.219 |
| > 52 | 52 (45.2) | 33 (55) | |||
| BMI (kg/m2) | < 22.8 | 58 (50.4) | 28 (46.7) | 0.224 | 0.636 |
| ≥ 22.8 | 57 (49.6) | 32 (53.3) | |||
| T category | T1-T2 | 12 (10.4) | 7 (11.7) | 0.062 | 0.804 |
| T3-T4 | 103 (89.6) | 53 (88.3) | |||
| N category | N0-N1 | 67 (58.3) | 38 (63.3) | 0.423 | 0.516 |
| N2-N3 | 48 (41.7) | 22 (36.7) | |||
| Clinical stage | I-III | 60 (52.2) | 29 (48.3) | 0.233 | 0.630 |
| IV | 55 (47.8) | 31 (51.7) | |||
| IC | Yes | 84 (73) | 39 (65) | 1.221 | 0.269 |
| No | 31 (27) | 21 (35) | |||
| CCRT | Yes | 98 (85.2) | 48 (80) | 0.776 | 0.378 |
| No | 17 (14.8) | 12 (20) | |||
| Target therapy | Yes | 89 (77.4) | 48 (80) | 0.158 | 0.691 |
| No | 26 (22.6) | 12 (20) | |||
| Immunotherapy | Yes | 15 (13) | 7 (11.7) | 0.068 | 0.794 |
| No | 100 (87) | 53 (88.3) | |||
| Smoking | Yes | 40 (34.8) | 22 (36.7) | 0.061 | 0.805 |
| No | 75 (65.2) | 38 (63.3) | |||
| Drinking | Yes | 26 (22.6) | 16 (26.7) | 0.365 | 0.551 |
| No | 89 (77.4) | 44 (73.3) | |||
ROM: radiation-induced oral mucositis; BMI: body mass index; IC: induction chemotherapy; CCRT: concurrent chemoradiotherapy.
Table 2.
Univariate and multivariate analyses of factors influencing severe ROM
| Variable | Univariable analyses | Multivariate analyses | |||
|---|---|---|---|---|---|
|
|
|
||||
| OR (95% CI) | P value | OR (95% CI) | P value | ||
| Sex | Male vs. Female | 0.95 (0.45-1.97) | 0.881 | ||
| Age (year) | ≤ 52 vs. > 52 | 1.48 (0.79-2.77) | 0.220 | 1.50 (0.80-2.82) | 0.205 |
| BMI (kg/m2) | < 22.8 vs. ≥ 22.8 | 1.16 (0.62-2.17) | 0.636 | ||
| T category | T1-T2 vs. T3-T4 | 0.88 (0.33-2.37) | 0.804 | ||
| N category | N0-N1 vs. N2-N3 | 0.81 (0.43-1.54) | 0.516 | ||
| Clinical stage | I-III vs. IV | 1.17 (0.62-2.18) | 0.630 | ||
| IC | No vs. Yes | 0.69 (0.35-1.34) | 0.270 | 0.67 (0.34-1.32) | 0.251 |
| CCRT | No vs. Yes | 0.69 (0.31-1.57) | 0.380 | ||
| Target therapy | No vs. Yes | 1.17 (0.54-2.52) | 0.691 | ||
| Immunotherapy | No vs. Yes | 0.88 (0.34-2.29) | 0.794 | ||
| Smoking | No vs. Yes | 1.09 (0.57-2.08) | 0.805 | ||
| Drinking | No vs. Yes | 1.25 (0.61-2.56) | 0.551 | ||
ROM: radiation-induced oral mucositis; BMI: body mass index; IC: induction chemotherapy; CCRT: concurrent chemoradiotherapy.
Effect of dose-volume parameters on severe ROM
Univariate analysis demonstrated a significant association between several oral dose-volume parameters and the development of severe ROM in NPC patients undergoing radiotherapy. Specifically, higher values of V30 (t = 2.497, P = 0.013), V35 (t = 3.348, P = 0.001), V40 (t = 3.344, P = 0.001), V45 (t = 3.289, P = 0.001), V50 (t = 3.291, P = 0.001), and Dmean (t = 3.863, P < 0.001) were significantly correlated with an increased risk of severe ROM (Table 3).
Table 3.
The effect of oral dose volume parameters on severe ROM indicated by univariate analysis (x̅±s)
| Parameters | ROM | Severe ROM | t value | P value |
|---|---|---|---|---|
| V20 (%) | 92.46 ± 8.50 | 94.25 ± 6.64 | 1.415 | 0.159 |
| V25 (%) | 73.96 ± 16.47 | 78.66 ± 16.14 | 1.802 | 0.073 |
| V30 (%) | 55.57 ± 18.12 | 62.78 ± 18.20 | 2.497 | 0.013 |
| V35 (%) | 39.95 ± 15.35 | 48.44 ± 16.99 | 3.348 | 0.001 |
| V40 (%) | 29.08 ± 12.75 | 37.01 ± 15.90 | 3.344 | 0.001 |
| V45 (%) | 21.34 ± 11.09 | 28.52 ± 14.90 | 3.289 | 0.001 |
| V50 (%) | 15.17 ± 9.65 | 21.70 ± 13.68 | 3.291 | 0.001 |
| Dmean (cGy) | 3469.62 ± 461.09 | 3778.60 ± 573.59 | 3.863 | 0.000 |
| Dmax (cGy) | 6872.31 ± 575.39 | 7033.46 ± 564.62 | 1.770 | 0.079 |
Dmean: mean dose to the oral cavity; Dmax: maximum dose to the oral cavity.
Analysis of the mean dose-volume histogram further supported these findings, revealing that patients who developed severe ROM were more likely to have received higher radiation dose volumes. A dose-dependent trend was observed, with the incidence of severe ROM increasing progressively with higher radiation exposure (Figure 2). This pattern underscores the importance of precise dose-volume control in reducing the risk of ROM during radiotherapy.
Figure 2.
Mean dose-volume parameters in the ROM and SROM groups. SROM: severe radiation-induced oral mucositis.
Multivariate analysis provided additional insight, indicating that even small increments in radiation exposure significantly elevated the risk of severe ROM. Specifically, each 1% increase in V35, the risk of severe ROM increased by 0.074-fold (P = 0.015, 95% CI: 1.014-1.137). Likewise, for each additional cGy in Dmean, the likelihood of severe ROM increased by 0.02-fold (P = 0.002, 95% CI: 1.007-1.033) (Table 4). These findings emphasize the critical need for careful radiation dose planning to minimize the risk of severe mucositis and improve patient outcomes.
Table 4.
The effect of oral dose volume parameters on severe ROM indicated by multivariate analysis
| Parameters | Univariable analyses | Multivariate analyses | ||
|---|---|---|---|---|
|
|
|
|||
| OR (95% CI) | P value | OR (95% CI) | P value | |
| V20 (%) | 1.032 (0.988-1.078) | 0.162 | 0.928 (0.831-1.035) | 0.178 |
| V25 (%) | 1.018 (0.998-1.039) | 0.075 | 0.906 (0.799-1.028) | 0.125 |
| V30 (%) | 1.023 (1.004-1.041) | 0.015 | 0.858 (0.714-1.032) | 0.103 |
| V35 (%) | 1.034 (1.013-1.055) | 0.002 | 1.074 (1.014-1.137) | 0.015 |
| V40 (%) | 1.041 (1.017-1.065) | 0.001 | 0.796 (0.454-1.396) | 0.426 |
| V45 (%) | 1.045 (1.018-1.072) | 0.001 | 1.027 (0.481-2.192) | 0.944 |
| V50 (%) | 1.050 (1.021-1.080) | 0.001 | 0.718 (0.412-1.250) | 0.241 |
| Dmean (cGy) | 1.001 (1.001-1.002) | 0.000 | 1.020 (1.007-1.033) | 0.002 |
| Dmax (cGy) | 1.001 (1.000-1.001) | 0.083 | 1.000 (0.999-1.001) | 0.508 |
Dmean: mean dose to the oral cavity; Dmax: maximum dose to the oral cavity.
Volume-response curve analysis
ROC curve analysis identified a critical threshold of 37.38% for oral V35, above which the risk of severe ROM significantly increased. At this cutoff, specificity was 49.6% (57/115), sensitivity reached 78.3% (47/60), and overall accuracy was 59.4% (104/175). The corresponding positive and negative likelihood ratios were 1.554 and 0.437, respectively. The area under the curve (AUC) was 0.652 (P = 0.044, 95% CI: 0.565-0.738), indicating moderate predictive value (Figure 3).
Figure 3.
Predictive performances for V35 and Dmean for severe ROM analyzed using ROC curve. ROM: radiation-induced oral mucositis; ROC: receiver operating characteristic.
Similarly, analysis of Dmean revealed a critical threshold of 3471.4 cGy. Exceeding this value was associated with a specificity of 51.3% (59/115), sensitivity of 75.0% (45/60), and an overall accuracy remained of 59.4% (104/175). The corresponding positive and negative likelihood ratios were 1.540 and 0.487, respectively. The AUC for Dmean was slightly higher at 0.666 (P < 0.001, 95% CI: 0.580-0.751), indicating a stronger predictive capability (Table 5).
Table 5.
The predictive value of V35 for severe ROM
| V35 determination results | Actual number of ROM cases | Total | |
|---|---|---|---|
|
| |||
| ROM | Severe ROM | ||
| ROM | 57 | 13 | 70 |
| Severe ROM | 58 | 47 | 105 |
| Total | 115 | 60 | 175 |
These findings suggest that patients with an oral V35 > 37.38% and a Dmean exceeding 3471.4 cGy are at a significantly elevated risk of developing severe ROM. These thresholds emphasize the importance of careful dose optimization in radiotherapy planning to mitigate ROM severity and improve patient outcomes (Table 6).
Table 6.
The predictive value of Dmean for severe ROM
| Dmean determination results | Actual number of ROM cases | Total | |
|---|---|---|---|
|
| |||
| ROM | Severe ROM | ||
| ROM | 59 | 15 | 74 |
| Severe ROM | 56 | 45 | 101 |
| Total | 115 | 60 | 175 |
Discussion
Nasopharyngeal carcinoma (NPC) is one of the most prevalent head and neck malignancies in China, with radiotherapy serving as the cornerstone of its treatment [11]. However, radiation-induced oral mucositis (ROM) is a frequent and debilitating side effect, significantly impairing patients’ quality of life [12]. Despite advances in radiotherapy techniques, research indicates that nearly all head and neck cancer patients treated with IMRT develop some degree of acute ROM, with approximately half experiencing severe ROM [13-16]. A key contributing factor to the high incidence of ROM is the lack of strict dose constraints for the oral cavity during treatment planning [17]. Additionally, the use of induction and concurrent chemotherapy, immunotherapy, and targeted therapies further exacerbates ROM risk [18]. Identifying reliable predictors for severe ROM is essential for early intervention, optimizing treatment strategies, and improving patient management [19].
Previous studies have identified factors such as age, N stage, and the number of induction chemotherapy cycles as independent predictors of severe ROM [20]. However, in this study, no significant association was found between severe ROM and clinical parameters, including sex, age, BMI, T stage, N stage, clinical stage, smoking history, alcohol consumption history, induction chemotherapy, or concurrent chemotherapy. This discrepancy may be due to the lower relative incidence of severe ROM in our cohort, as well as proactive monitoring and timely management of adverse reactions in our institution. The progression of ROM primarily leads to pain and discomfort, severely impairing oral intake and, in severe cases, causing treatment interruptions [21]. While pain management and nutritional support are critical, identifying predictive factors remains critical to mitigating ROM severity and improving treatment tolerance. Our findings demonstrate that oral dose-volume parameters, particularly V35 and Dmean, are independent risk factors for severe ROM. These findings align with prior research showing a strong correlation between radiation dose, irradiated volume, and ROM severity.
Ebert et al. reported that head and neck cancer patients with grade 3 mucositis had significantly higher Dmax and V30 values compared to those without severe ROM [22]. Similarly, Li et al. found that in patients receiving carbon ion radiotherapy, severe ROM was significantly associated with dosimetric parameters, and proposed dose constraints for Dmax, D10, D15, and D20 [23]. While different studies suggest varying threshold values, our findings identified V35 > 37.38% and Dmean > 3471.4 cGy as critical cutoffs, beyond which the incidence of severe ROM increases significantly. These findings further underscore the importance of optimizing dose-volume parameters to reduce ROM risk while maintaining treatment efficacy.
Several strategies have been explored to mitigate radiotherapy-induced ROM. A randomized clinical trial demonstrated that the probiotic Streptococcus salivarius K12 significantly reduced both the incidence and severity of ROM [24]. Nutritional interventions, such as early oral nutritional supplementation, have also been identified as protective factors against severe ROM [25,26]. Moreover, adjunctive treatments, including Yunnan Baiyao and Kangfuxin solutions, have shown efficacy in suppressing inflammatory responses and alleviating mucositis severity [27]. Emerging evidence also suggests that cognitive behavioral therapy (CBT) may help alleviate radiation-induced toxicities, including xerostomia, fatigue, and insomnia, while improving patients’ psychological well-being [28].
In our study, BMI was not significantly differ between the non-severe and severe ROM groups. This may be attributed to the relatively small sample size, as well as the early implementation of nutritional support and standardized symptomatic management, which likely mitigated significant weight changes. Nevertheless, early intervention remains crucial for improving patient prognosis and minimizing ROM-related complications.
Despite the valuable insights gained, this study has several limitations. First, the relatively small number of cases with severe ROM may have limited the statistical power of our findings. Second, potential selection bias may have occurred during patient enrollment. Third, we only documented the highest grade of mucositis during radiotherapy, without tracking its progression or evaluating post-treatment outcomes. Future large-scale, multi-center studies are needed to validate these findings and further investigate the relationship between predictive factors and the development of severe ROM.
Conclusion
This study investigated the relationship between clinical factors, oral dose-volume parameters, and the risk of severe ROM in NPC patients undergoing radiotherapy. The findings identified V35 and Dmean as independent predictive indicators for severe ROM, reinforcing the importance of dose constraints to the oral mucosa. Optimizing dose-volume parameters during radiotherapy planning may help reduce the incidence of severe ROM, enhance patient tolerability, and improve treatment outcomes. Further research with larger sample sizes and multi-center validation [29] is warranted to refine predictive models and develop targeted intervention strategies.
Disclosure of conflict of interest
None.
References
- 1.Su ZY, Siak PY, Lwin YY, Cheah SC. Epidemiology of nasopharyngeal carcinoma: current insights and future outlook. Cancer Metastasis Rev. 2024;43:919–939. doi: 10.1007/s10555-024-10176-9. [DOI] [PubMed] [Google Scholar]
- 2.Yacoub I, Qian JY, Nashed K, Youssef M, Khalil M, Kallini D, Lee NY. Radiation techniques and advancements in nasopharyngeal carcinoma. Oral Oncol. 2024;159:107060. doi: 10.1016/j.oraloncology.2024.107060. [DOI] [PubMed] [Google Scholar]
- 3.Pulito C, Cristaudo A, Porta C, Zapperi S, Blandino G, Morrone A, Strano S. Oral mucositis: the hidden side of cancer therapy. J Exp Clin Cancer Res. 2020;39:210. doi: 10.1186/s13046-020-01715-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coppini M, Caponio VCA, Mauceri R, Bizzoca ME, Laino L, Lorenzo-Pouso AI, Russo D, Troiano G, Silva FFVE, Lo Muzio L, Campisi G. Efficacy of topical agents in oral mucositis prevention: systematic review and network meta-analysis. Oral Dis. 2024;30:4126–4144. doi: 10.1111/odi.15046. [DOI] [PubMed] [Google Scholar]
- 5.Abdalla-Aslan R, Keegan R, Zadik Y, Yarom N, Elad S. Recent advances in cancer therapy-associated oral mucositis. Oral Dis. 2024 doi: 10.1111/odi.14999. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 6.Goel G, Alice KP, Negi P, Aggarwal N. Factors influencing radiation induced oral mucositis in head and neck cancer. J Cancer Res Ther. 2024;20:1564–1569. doi: 10.4103/jcrt.jcrt_1200_23. [DOI] [PubMed] [Google Scholar]
- 7.Ghosh A, Maitra S, Acharyya S. Buccal mucosa dosimetry as a predictor of acute grade ≥ 3 radiation induced oral mucositis (RIOM) in head neck squamous cell carcinoma treated with conformal radiotherapy: a prospective single institutional study from Eastern India. Clinical Oncology. 2024;36:e361. [Google Scholar]
- 8.Narayan S, Lehmann J, Coleman MA, Vaughan A, Yang CC, Enepekides D, Farwell G, Purdy JA, Laredo G, Nolan K, Pearson FS, Vijayakumar S. Prospective evaluation to establish a dose response for clinical oral mucositis in patients undergoing head-and-neck conformal radiotherapy. Int J Radiat Oncol Biol Phys. 2008;72:756–762. doi: 10.1016/j.ijrobp.2008.01.060. [DOI] [PubMed] [Google Scholar]
- 9.Wang ZH, Zhang SZ, Zhang ZY, Zhang CP, Hu HS, Tu WY, Kirwan J, Mendenhall WM. Protecting the oral mucosa in patients with oral tongue squamous cell carcinoma treated postoperatively with intensity-modulated radiotherapy: a randomized study. Laryngoscope. 2012;122:291–298. doi: 10.1002/lary.22434. [DOI] [PubMed] [Google Scholar]
- 10.Pan XX, Tong LH, Chen YF, Li FL, Tang WB, Liu YJ, Yang W. A simplified T classification based on the 8th edition of the UICC/AJCC staging system for nasopharyngeal carcinoma. Cancer Manag Res. 2019;11:3163–3169. doi: 10.2147/CMAR.S185860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Au KH, Ngan RKC, Ng AWY, Poon DMC, Ng WT, Yuen KT, Lee VHF, Tung SY, Chan ATC, Sze HCK, Cheng ACK, Lee AWM, Kwong DLW, Tam AHP. Treatment outcomes of nasopharyngeal carcinoma in modern era after intensity modulated radiotherapy (IMRT) in Hong Kong: a report of 3328 patients (HKNPCSG 1301 study) Oral Oncol. 2018;77:16–21. doi: 10.1016/j.oraloncology.2017.12.004. [DOI] [PubMed] [Google Scholar]
- 12.Thomas PL, Kaur H, Rishi KS. Radiation induced oral mucositis: onset, severity and associated risk factors among head and neck cancer patients-a prospective observational study. Indian J Public Health Res Develop. 2019;10:355. [Google Scholar]
- 13.Karlsson C, Bohm N, Andersson JS, Finizia C, Almståhl A. Prospective study on health-related quality of life, oral mucositis and oral health on during treatment of head and neck cancer. BMC Oral Health. 2024;24:697. doi: 10.1186/s12903-024-04466-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sroussi HY, Epstein JB, Bensadoun RJ, Saunders DP, Lalla RV, Migliorati CA, Heaivilin N, Zumsteg ZS. Common oral complications of head and neck cancer radiation therapy: mucositis, infections, saliva change, fibrosis, sensory dysfunctions, dental caries, periodontal disease, and osteoradionecrosis. Cancer Med. 2017;6:2918–2931. doi: 10.1002/cam4.1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huang CJ, Huang MY, Fang PT, Chen F, Wang YT, Chen CH, Yuan SS, Huang CM, Luo KH, Chuang HY, Wang YY, Lee HH. Randomized double-blind, placebo-controlled trial evaluating oral glutamine on radiation-induced oral mucositis and dermatitis in head and neck cancer patients. Am J Clin Nutr. 2019;109:606–614. doi: 10.1093/ajcn/nqy329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Elting LS, Cooksley CD, Chambers MS, Garden AS. Risk, outcomes, and costs of radiation-induced oral mucositis among patients with head-and-neck malignancies. Int J Radiat Oncol Biol Phys. 2007;68:1110–1120. doi: 10.1016/j.ijrobp.2007.01.053. [DOI] [PubMed] [Google Scholar]
- 17.Lalla RV, Brennan MT, Gordon SM, Sonis ST, Rosenthal DI, Keefe DM. Oral mucositis due to high-dose chemotherapy and/or head and neck radiation therapy. J Natl Cancer Inst Monogr. 2019;2019:lgz011. doi: 10.1093/jncimonographs/lgz011. [DOI] [PubMed] [Google Scholar]
- 18.Daugėlaitė G, Užkuraitytė K, Jagelavičienė E, Filipauskas A. Prevention and treatment of chemotherapy and radiotherapy induced oral mucositis. Medicina (Kaunas) 2019;55:25. doi: 10.3390/medicina55020025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang Z, Tian L, Liu J, Jiang H, Wang P. Evidence summary on managing radiotherapy-induced oral mucositis in patients with head and neck cancer. Asia Pac J Oncol Nurs. 2024;11:100386. doi: 10.1016/j.apjon.2024.100386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu Z, Huang L, Wang H, Shi Z, Huang Y, Liang L, Wang R, Hu K. Predicting nomogram for severe oral mucositis in patients with nasopharyngeal carcinoma during intensity-modulated radiation therapy: a retrospective cohort study. Curr Oncol. 2022;30:219–232. doi: 10.3390/curroncol30010017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Song X, Su L, Lin Q, Liu S, Zhang W, Hong J. Effect of nutritional status before radiotherapy on radiation-induced acute toxicities in patients with nasopharyngeal carcinoma. Head Neck. 2023;45:620–628. doi: 10.1002/hed.27275. [DOI] [PubMed] [Google Scholar]
- 22.Ebert N, Valentini C, Löcke S, Appold S, Krause M, Baumann M. EP-1311: prediction of oral mucositis in HNSCC by dose-volume parameters. Radiother Oncol. 2015;115:S706–S707. [Google Scholar]
- 23.Li Y, Guan X, Hu C. Impact of dose volume parameters and clinical characteristics on radiation-induced acute oral mucositis for head and neck cancer patients treated with carbon-ion radiotherapy dose volume outcome analysis. Strahlenther Onkol. 2024;200:895–902. doi: 10.1007/s00066-024-02255-1. [DOI] [PubMed] [Google Scholar]
- 24.Peng X, Li Z, Pei Y, Zheng S, Liu J, Wang J, Li R, Xu X. Streptococcus salivarius K12 alleviates oral mucositis in patients undergoing radiotherapy for malignant head and neck tumors: a randomized controlled trial. J. Clin. Oncol. 2024;42:1426–1435. doi: 10.1200/JCO.23.00837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang SA, Zhu YH, Liu WJ, ul Haq I, Gu JY, Qi L, Yang M, Yang JY. Association of nutritional counselling with the severity of radiation-induced oral mucositis in patients with nasopharyngeal carcinoma: a retrospective study. Nutrition Clinique et Métabolisme. 2024;38:244–250. [Google Scholar]
- 26.Su L, Lin QJ, Ma SQ, Song XR, Ye JR, Ni MS, Hong JS. The effect of early oral nutritional supplements on improving nutritional outcomes and radiation-induced oral mucositis for nasopharyngeal carcinoma patients undergoing concurrent chemoradiotherapy. Head Neck. 2023;45:2798–2808. doi: 10.1002/hed.27503. [DOI] [PubMed] [Google Scholar]
- 27.Tang X, Sun J, Deng J, Shi B. Treatment of Yunnan Baiyao plus Kangfuxin solution reduces inflammatory response and prevents patients with nasopharyngeal carcinoma against radiation-induced oral mucositis. J Nanomater. 2021;2021:9973539. [Google Scholar]
- 28.Liu F, Wang H, Jiang C, Wu X, Fan C, Ye X, Li Y, Qiu Y, He L, Xiao S, Zhao Q, Wu W, Tan C, Li Y, He R, Liu W, Chen K. Long term effects of cognitive behavioral therapy on late toxicities, depressive and anxiety symptoms in patients with locoregional advanced nasopharyngeal carcinoma undergoing chemoradiotherapy: a randomized, controlled clinical trial. Int J Radiat Oncol Biol Phys. 2024;120:S37. [Google Scholar]
- 29.Sun Y, Li WF, Chen NY, Zhang N, Hu GQ, Xie FY, Sun Y, Chen XZ, Li JG, Zhu XD, Hu CS, Xu XY, Chen YY, Hu WH, Guo L, Mo HY, Chen L, Mao YP, Sun R, Ai P, Liang SB, Long GX, Zheng BM, Feng XL, Gong XC, Li L, Shen CY, Xu JY, Guo Y, Chen YM, Zhang F, Lin L, Tang LL, Liu MZ, Ma J. Induction chemotherapy plus concurrent chemoradiotherapy versus concurrent chemoradiotherapy alone in locoregionally advanced nasopharyngeal carcinoma: a phase 3, multicentre, randomised controlled trial. Lancet Oncol. 2016;17:1509–1520. doi: 10.1016/S1470-2045(16)30410-7. [DOI] [PubMed] [Google Scholar]