ABSTRACT
The concomitant presence of esophageal achalasia and esophagogastric junction submucosal leiomyoma is extremely rare. Peroral endoscopic myotomy has been endorsed as one of the primary interventions to manage esophageal achalasia. We present a 49-year-old woman who had initial endoscopic evaluation and diagnosis of achalasia type II then underwent peroral endoscopic myotomy and found to have incidental submucosal leiomyoma at 1 cm distal to esophagogastric junction. It was removed successfully by submucosal tunneling endoscopic resection. This poses the question of whether this is a case of achalasia or pseudoachalasia caused by leiomyoma.
KEYWORDS: achalasia, pseudoachalasia, esophageal leiomyoma, peroral endoscopic myotomy (POEM), submucosal tunneling endoscopic resection (STER), en bloc resection
INTRODUCTION
Achalasia is a rare neurodegenerative disease where there is impairment in the peristaltic motion of the esophageal tube, lower esophageal sphincter, and relaxation.1,2 Esophageal submucosal leiomyomas are benign neoplasms of smooth muscle cells and the most common benign tumors of the esophagus occurring mainly in the lower two-thirds with insidious onset.3,4 The concomitant presence of achalasia and esophagogastric junction (EGJ) leiomyoma is extremely rare. To the best of our knowledge, we found one similar reported case of esophageal achalasia and EGJ leiomyoma coexistence.5 We present a case where clinical assessment, endoscopic, manometric, and radiological evaluation revealed the diagnosis of type II achalasia. Eventually, the patient underwent peroral endoscopic myotomy (POEM) which revealed an incidental leiomyoma that was found at 1 cm distal to EGJ. The leiomyoma was then resected and removed successfully with submucosal tunneling endoscopic resection.
CASE REPORT
A 49-year-old woman presented with long-standing progressive dysphagia to solids and liquids. In the last 6 months, her dysphagia rapidly worsened and lost 20 pounds of weight with associated chest pain and severe regurgitation of undigested food, especially at nighttime. High-resolution esophageal manometry study demonstrated EGJ outflow obstruction with integrated relaxation pressure 29.1, failed peristalsis with all swallows, and 100% panesophageal pressurization suggestive of type II achalasia with Eckardt score of 10. Then, barium esophagram demonstrated dilated esophagus with narrowing at EGJ and generalized dysmotility (Figure 1). The patient was informed of the diagnosis, discussed all management options regarding achalasia, and opted for POEM procedure. Endoluminal functional lumen imaging probe measurements before myotomy reveal EGJ distensibility index of 1.12, 0.88, and 0.99 at 30, 40, and 50 mL fill volume, respectively. Subsequently, upper endoscopy revealed EGJ at 40 cm, retained fluid seen in the esophageal lumen, and no other abnormalities were noted in the esophagus, stomach, and duodenum (Figures 2 and 3). Submucosal tunneling was performed on the anterior wall, which is preferred, however, extended 2 cm into the gastric cardia. A submucosal lesion was seen at 1 cm distal to the EGJ at 41 cm (Figure 4). The submucosal lesion was dissected en bloc from the submucosa and muscularis propria using a triangular tip knife, achieving resection with clear margins (Figure 5). Subsequently, myotomy was done from proximal to distal starting from 33 to 41 cm. In view of incidental finding of submucosal lesion, POEM was accompanied with submucosal tunneling endoscopic resection. The patient tolerated the procedure well, and no complications were noted. Endoluminal functional lumen imaging probe measurements postmyotomy reveal EGJ distensibility index of 6.67 and 12 at 30 mL and 40 mL fill volume, respectively. The following day, barium esophagram demonstrated resolution of distal esophageal dilatation and narrowing at EGJ (Figure 6). Histopathological examination reveals 0.9 × 0.6 × 0.3 cm leiomyoma with clear margin, and immunohistochemistry positive for caldesmon and negative for cluster differentiation 117 and neural marker S100. Office follow-up in 6 weeks reveal symptoms have resolved with Eckardt score of 0.
Figure 1.

Dilated esophagus with narrowing at esophagogastric junction as depicted using barium esophagram.
Figure 2.

An upper endoscopy revealed esophagogastric junction at 40 cm, retained fluid within the esophageal lumen.
Figure 3.

No other abnormalities were noted in the esophagus, stomach, and duodenum during the upper endoscopy.
Figure 4.
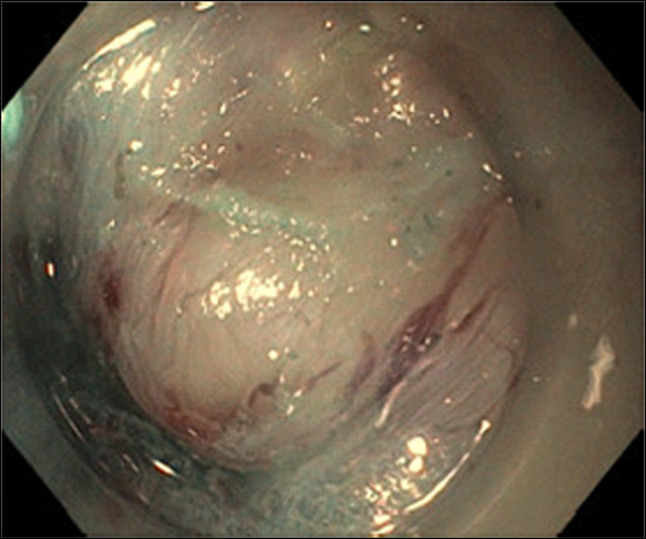
A submucosal lesion distal to the esophagogastric junction.
Figure 5.

The submucosal lesion that was dissected en bloc from the submucosa and muscularis propria using a triangular tip knife.
Figure 6.

The barium esophagram status postresection, which demonstrated resolution of distal esophageal dilatation and narrowing at esophagogastric junction.
DISCUSSION
Esophageal submucosal leiomyomas are the most common benign tumors of the esophagus occurring mainly in the lower two-thirds with insidious onset. However, they are rare and accounts for less than 1% of all esophageal neoplasms.3,4 The initial diagnosis modality is barium esophagram of the upper gastrointestinal tract.6–8 Then, upper endoscopy is used to confirm the diagnosis which can be accompanied with CT scan. Endoscopic ultrasonography (EUS) has become a significant test to perform as it can further delineate the tumor, display any associated mediastinal lymph nodes and the 5-layer structure of the esophageal wall. The patient had CT scans and upper endoscopy which did not reveal any underlying EGJ leiomyoma.
Literature review revealed 1 similar case report of achalasia coexistence with incidental EGJ leiomyoma where they describe a patient with achalasia type 2 and resecting an incidental leiomyoma without performing POEM which resulted in resolution of patient's symptoms.5 Pseudoachalasia can have similar clinical presentation, radiological assessment, and endoscopic findings to achalasia; however, they are usually due to secondary etiologies. Hence, it is important to correctly diagnose the patient as the treatment and prognosis can be different. Moreover, achalasia misdiagnosis has also been reported in those who had incidental underlying esophageal leiomyoma.5,9,10 Therefore, a high index of suspicion should be maintained that pseudoachalasia could be present despite studies suggesting esophageal achalasia. An additional measure we could have performed is EUS; thus, this case presentation may support the use of EUS as a final measure to rule out possible submucosal tumors.11 Our patient initially had the diagnosis of esophageal achalasia type II after extensive performed studies and assessment. Whether our patient had pseudoachalasia or achalasia remains a question and poses the challenge of making the right diagnosis in such similar contexts.
DISCLOSURES
Author contributions: K. Rahima contributed substantially to the conception of the case report and conducted the initial literature review. He participated in drafting the manuscript, compiling clinical data, and revising content critically for intellectual coherence and accuracy. M. Hijazi contributed to data interpretation, helped analyze differential diagnoses, and assisted in preparing the discussion section. He also reviewed and edited the final manuscript for clinical relevance and clarity. M. Kutaiba Albuni contributed to data interpretation, helped analyze differential diagnoses, and assisted in preparing the discussion section. He also reviewed and edited the final manuscript for clinical relevance and clarity. S. Taheri was the primary author responsible for the design, writing, and organization of the manuscript. She coordinated author contributions, conducted an in-depth review of relevant literature, and oversaw all stages of manuscript preparation and submission. V. Muddana was the supervising physician on the case. He provided critical clinical insight, confirmed diagnostic and procedural accuracy, and contributed expert commentary to the discussion. He also reviewed the manuscript for final approval and intellectual content. S. Taheri is the article guarantor.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
Contributor Information
Kenan Rahima, Email: kinan.rahima@gmail.com.
Mohamad Hijazi, Email: mohamad_hijazi@trihealth.com.
Mhd Kutaiba Albuni, Email: mhdkutaiba_albuni@trihealth.com.
Venkata Muddana, Email: venkata_muddana@trihealth.com.
REFERENCES
- 1.Sadowski DC, Ackah F, Jiang B, Svenson LW. Achalasia: Incidence, prevalence and survival. A population-based study. Neurogastroenterol Motil. 2010;22(9):e256–61. [DOI] [PubMed] [Google Scholar]
- 2.Pohl D, Tutuian R. Achalasia: An overview of diagnosis and treatment. J Gastrointestin Liver Dis. 2007;16(3):297–303. [PubMed] [Google Scholar]
- 3.Inderhees S, Tank J, Stein HJ, Dubecz A. Leiomyoma of the esophagus: A further indication for robotic surgery? [in German]. Chirurg. 2019;90(2):125–30. [DOI] [PubMed] [Google Scholar]
- 4.Zhu S, Lin J, Huang S. Successful en bloc endoscopic full-thickness resection of a giant cervical esophageal leiomyoma originating from muscularis propria. J Cardiothorac Surg. 2019;14(1):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Deng B, Gao XF, Sun YY, et al. Case report: Successful resection of a leiomyoma causing pseudoachalasia at the esophagogastric junction by tunnel endoscopy. BMC Gastroenterol. 2016;16:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Perwaiz A, Shaw VK, Singh A, Chaudhary A. Extra-mucosal enucleation is still a safe and feasible treatment option of giant esophageal leiomyomas. Indian J Gastroenterol. 2018;37(1):63–6. [DOI] [PubMed] [Google Scholar]
- 7.Kohli DR, Faigel DO. Esophageal leiomyomas: Making mole hills out of mole hills? Gastrointest Endosc. 2018;87(2):378–9. [DOI] [PubMed] [Google Scholar]
- 8.Lipnickas V, Beiša A, Makūnaitė G, Strupas K. Laparoscopic approach in the treatment of large leiomyoma of the lower third of the esophagus. Wideochir Inne Tech Maloinwazyjne. 2017;12(4):437–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mohamed A. Education and imaging. Gastrointestinal: Pseudoachalasia caused by a lower esophageal stromal tumor. J Gastroenterol Hepatol. 2009;24(6):1152. [DOI] [PubMed] [Google Scholar]
- 10.Carbonari A, Frota M, Colaiacovo R, Rossini L, Nakamura R. Esophageal duplication cyst causing megaesophagus in a young woman presenting with dysphagia. Endoscopy. 2014;46(Suppl 1 UCTN):E201–2. [DOI] [PubMed] [Google Scholar]
- 11.Krishnan K, Lin CY, Keswani R, Pandolfino JE, Kahrilas PJ, Komanduri S. Endoscopic ultrasound as an adjunctive evaluation in patients with esophageal motor disorders subtyped by high-resolution manometry. Neurogastroenterol Motil. 2014;26:1172–8. [DOI] [PMC free article] [PubMed] [Google Scholar]


