Abstract
Purpose of review
The objective of this review is to provide an overview of the clinical progress, administration methods, efficacy, safety, and treatment-related adverse events associated with antibody–drug conjugates.
Recent findings
Locally advanced or metastatic urothelial carcinoma is an aggressive and lethal malignancy. Cisplatin-based chemotherapy has been the first-line therapy for most patients over the past two decades. However, approximately 50% of patients with locally advanced or metastatic urothelial carcinoma are ineligible for cisplatin-based chemotherapy due to inadequate renal function, poor performance status, or complications. Furthermore, patients who exhibit suboptimal responses or disease progression following platinum-based chemotherapy face therapeutic uncertainty regarding the selection of alternative agents. The emergence of antibody–drug conjugates has provided new options for patients afflicted with this disease, particularly enfortumab vedotin combined with pembrolizumab as a new first-line therapy for advanced urothelial carcinoma or for patients ineligible for platinum-based therapy. Additionally, in the TROPICS-04 trial, sacituzumab govitecan failed to demonstrate significant improvement in overall survival or progression-free survival compared with the physician’s choice of treatment for patients with advanced urothelial carcinoma progressing after platinum-based chemotherapy and PD-(L)1 inhibitor therapy; the FDA withdrew its approval for this indication. ADCs are also being considered for the treatment of muscle-invasive bladder cancer, with ongoing clinical trials.
Keywords: Antibody–drug conjugates (ADCs), Urothelial carcinoma, Treatment-related adverse events (TRAEs), Disitamab vedotin, Enfortumab vedotin, Sacituzumab govitecan
Introduction
Bladder cancer remains a leading cause of global cancer-related mortality, profoundly affecting patient’s quality of life and healthcare costs. According to GLOBOCAN 2020 estimates, bladder cancer accounted for approximately 573,000 new cases worldwide in 2020, with 213,000 deaths attributed to this malignancy. More than three-quarters of newly diagnosed bladder cancer cases occur in men [1]. Bladder cancer ranked as the fourth most common malignancy among men in 2023, accounting for approximately 6% of new cancer diagnoses and 4% of cancer-associated mortality [2]. Based on tumor invasion depth and metastatic status, bladder cancer is classified into three categories: non-muscle invasive bladder cancer (NMIBC), muscle-invasive bladder cancer (MIBC), and metastatic bladder cancer, with urothelial carcinoma (UC) representing 90% of all cases. At initial diagnosis, approximately 70–75% of patients present with NMIBC, 20–25% with MIBC, and 5% with advanced or metastatic disease [3, 4]. Disease progression occurs in 15%–20% of NMIBC cases to MIBC [5], while among those initially diagnosed with localized MIBC, nearly 50% subsequently develop metastatic progression [4].
Over the past two decades, patients with metastatic urothelial carcinoma (mUC) have had limited treatment options, with platinum-based chemotherapy remaining the first-line regimen for most patients until the emergence of the enfortumab vedotin (EV) plus pembrolizumab (Pb) [6, 7]. Platinum-based chemotherapy demonstrates an objective response rate (ORR) ranging from 44.6 to 72% [5, 8], achieving a median survival duration of approximately 13–15 months [4], and survival with carboplatin-containing regimens seemed inferior and limited (8–9 months) [9]. However, nearly 50% of mUC patients are cisplatin ineligible, and 10–15% are platinum ineligible (cisplatin and carboplatin), necessitating alternative treatment options [7]. Immune checkpoint inhibitors (ICIs) have been integrated into practice as first-line therapy for platinum-ineligible patients and as second-/third-line options post-platinum progression in the chemotherapy era [10]. The emergence of targeted therapies, fibroblast growth factor receptor inhibitors, bispecific antibodies, and ADCs has expanded treatment options for patients with la/mUC [3, 7, 11]. ADC, as a prominent research subject, has undergone clinical evaluation in UC management, demonstrating clinically meaningful durable responses with acceptable safety profiles [12, 13]. In particular, disitamab vedotin (DV), EV, and sacituzumab govitecan (SG) have been involved in phase I-III clinical trials and have accumulated substantial clinical evidence in the treatment of patients with la/mUC.
What are ADCs? How do they have an antitumor effect?
In 2000, with the approval of the US Food and Drug Administration (FDA), Mylotarg™ was approved for the treatment of acute myeloid leukemia, marking the introduction of a novel class of precision drugs, ADCs, into oncological clinical practice and heralding a new era of precision medicine in oncology globally [14]. ADCs consist of three components: an antibody, a cytotoxic payload, and a chemical linker. The antibody serves as a navigational guide, recognizing specific antigens expressed on the surface of cancer cells, enabling targeted delivery of the ADC to tumor cells. Antibodies can be categorized into murine antibodies, chimeric antibodies, and humanized antibodies. Owing to severe immunogenicity-related side effects, murine antibodies are gradually replaced by the other two types. The cytotoxic payload functions as the warhead of the ADC, responsible for destroying or killing tumor cells. Chemical linkers act as bridges connecting the antibody and cytotoxic payload, facilitating their conjugation and mediating cytotoxic payload release upon reaching the tumor cell. There are two types of chemical linkers: cleavable and non-cleavable [15]. The antitumor mechanisms and pharmacokinetics of ADCs are highly intricate. Following intravenous administration, ADCs circulate in the bloodstream and specifically target tumor cells through antibody mediated recognition. The antibodies bind to the specific target antigens and are internalized by tumor cells via endocytosis. Acidic, proteases, or redox interactions trigger the release of the cytotoxic payload from the antibody; the liberated cytotoxic payload diffuses into the cytoplasm and throughout the cell to interact with target substrates, ultimately inducing cell death. Hydrophobic drugs can also diffuse into cells through the cell membrane, regardless of whether they express the target antigen, potentially exerting cytotoxic effects on adjacent cells. This “bystander effect” may be a significant factor contributing to the efficacy of ADC in tumors with heterogeneous antigen expression [16]. Thus, ADCs are widely regarded as “biological missiles” for targeted cancer therapy because of their ability to synergistically exert both specific targeting and highly efficient killing of cancer cells. They can not only destroy cancer cells precisely and improve the therapeutic window but also reduce side effects [15].
After decades of research and development, ADCs have achieved remarkable advancements in the treatment of hematological malignancies and solid tumors, emerging as one of the most successful therapeutic strategies in targeted oncology [17, 18]. These include lung cancer [19], breast cancer [20], acute myeloid leukemia [14], and UC [21]. Agents including SG, EV, RC48-ADC, ASG-15ME, and anti-HER2 ADCs have been clinically employed in UC management, with clinical trials demonstrating favorable tolerability and sustained therapeutic responses [22].
Clinical advanced of ADCs in the treatment of urothelial carcinoma
Enfortumab vedotin
EV is an ADC that targets Nectin-4 and consists of a fully human anti-Nectin-4 IgG1 kappa monoclonal antibody conjugated to the microtubule-disrupting agent monomethyl auristatin E (MMAE) via a cleavable linker [23]. Nectin-4 is a transmembrane protein belonging to the Nectin family and plays crucial roles in cell proliferation, migration, and adhesion [24, 25]. It is highly expressed in various malignancies, including bladder, breast, lung, pancreas, ovary, head/neck, and esophageal cancers, especially UC (60%) [23].
In December 2019, the FDA granted accelerated approval to EV for the treatment of la/mUC for the first time. Based on results from an open-label, randomized, multicenter phase 3 study (EV-301), EV received further approval in September 2021 for the treatment of patients with la/mUC who had previously received platinum-based chemotherapy or PD-1/PD-L1 inhibitors [26, 27]. The phase I trial enrolled (N = 155) patients with la/mUC refractory to prior chemotherapy or PD-1/PD-L1 inhibitors, evaluating EV dose escalation from 0.5 to 1.25 mg/kg. Primary endpoints assessed safety, tolerability, and pharmacokinetics, with antitumor activity as a secondary endpoint. In the monotherapy cohort receiving 1.25 mg/kg EV (n = 112), outcomes included an objective response rate (ORR) of 43%, median overall survival (OS) of 12.3 months, and 1-year survival rate of 51.8%. Additionally, the study recommended a dose of 1.25 mg/kg for phase II clinical trials [28]. EV-201 [29] is a global phase II, single-arm study involving 125 patients with mUC. The primary endpoint of the study was the ORR, with a median follow-up duration of 10.2 months; the confirmed ORR was 44%, which included a CR in 12% of patients, and the median response duration was 7.6 months. The phase III [30] trial was a randomized controlled study that involved 86 patients with la/mUC. The patients were randomly assigned at a 1:1 ratio to receive either EV or a commonly used chemotherapy regimen (docetaxel or paclitaxel). With OS as the primary endpoint and PFS, ORR, and safety/tolerability as secondary endpoints. The results revealed that the median OS was 15.18 months in the EV group and 10.55 months in the chemotherapy group. The median PFS was 6.47 months in the EV group and 5.39 months in the chemotherapy group. The confirmed ORR was 34.4% in the EV group and 21.3% in the chemotherapy group. Patients treated with EV demonstrated clinically favorable survival benefits, and compared with those in the chemotherapy group, the incidence of TRAEs in the EV group was lower. EV has completed phase I–III clinical trials, resulting in the accumulation of a substantial amount of clinical data (Table 1) that demonstrate promising efficacy outcomes. Compared with conventional chemotherapy, EV exhibit a superior clinical response [27, 31–35].
Table 1.
Clinical trials of enfortumab vedotin (EV)
| Clinical trials | Trial design | Participants (N) | Primary endpoints | Grade ≥ 3 TRAEs |
|---|---|---|---|---|
| EV-101, Phase I [28] | EVc | la/mUC/155 | Safety/tolerability/pharmacokinetics | 34% |
| Phase I [39] | EVa+SG | la/mUC/23 | Safety/tolerability | 78.3% |
| Phase I [34] | EVb | la/mUC/17 | Safety/tolerability | 58.8% |
| Phase Ib/II [33] | EVa+Pb | la/mUC/45 | Safety | 64.4% |
| EV-201, Phase II [29] | EVb | mUC/125 | 44.0% ORR | 54.4% |
| EV-201, Phase II [27] | EVb | la/mUC/89 | 52.0% ORR | 55.1% |
| EV-103, Phase Ib/II [32] | EVa vs EVa+Pb | la/mUC/149 | 45.2% vs 64.5% ORR | 47.9% vs 63.2% |
| EV-301, Phase 3 [30] | EVb vs chemotherapy | la/mUC/86 | OS 15.18 m vs 10.55 m | 63.9% vs 75% |
| EV-301, Phase 3 [26, 31] | EVb vs chemotherapy | la/mUC/608 | OS 12.88 m vs 8.97 m | 52.4% vs 50.5% |
| EV-302, Phase 3 [36] | EVa+Pb vs chemotherapy | la/mUC/886 |
PFS 12.5 m VS 6.3 m OS 31.5 m VS16.1 m |
55.9% vs 69.5% |
Pb: pembrolizumab, m: month
a1.25 mg/kg, with a maximum of 125 mg per dose, on days 1 and 8 of each 3-week cycle
b1.25 mg/kg; days 1, 8, and 15 of each 4-week cycle
c0.5, 0.75, 1.0, and 1.25 mg/kg escalating doses; infusion on days 1, 8, and 15 of each 4-week cycle
Additionally, in a global, open, randomized trial (EV-302) [36], 886 patients with previously untreated la/mUC were enrolled. Patients were randomly assigned 1:1 to receive EV plus Pb and platinum-based chemotherapy for 3 cycles, respectively. PFS and OS were used as the primary study endpoints. PFS was longer in the EV plus Pb group than the chemotherapy group (median 12.5 and 6.3 months, P < 0.001), as was OS (median 31.5 and 16.1 months, P < 0.001). This trial showed that the use of EV plus Pb significantly improved survival compared with chemotherapy in patients with previously untreated la/mUC, with significant clinical benefit. EV plus Pb has the potential to replace platinum-based chemotherapy as the first-line therapy for patients with aUC or who are platinum ineligible [10, 37, 38].
Although EV can provide clinical benefits to patients, the associated adverse events of the treatment cannot be disregarded, and the incidence of grade ≥ 3 TRAEs ranges from 34 to 78.3% across studies (Table 1). Among EV monotherapy, neutropenia, maculopapular rash, hyperglycemia, anemia, and fatigue were the most common grade ≥ 3 TRAEs. In the EV plus Pb combination group, maculopapular rash, fatigue, neutropenia, peripheral sensory neuropathy, and hyperglycemia were the most common grade ≥ 3 TRAEs. Neutropenia, diarrhea, anemia, fatigue, and infection were the most common grade ≥ 3 TRAEs in the EV + SG dual ADC model (Table 2).
Table 2.
The most common grade ≥ 3 TRAEs of enfortumab vedotin
| TRAEs | EV monotherapy | EV+Pb | EV+SG |
|---|---|---|---|
| Grade ≥ 3 | Grade ≥ 3 | Grade ≥ 3 | |
| Maculopapular rash | + + + | + + + | |
| Hyperglycemia | + + + | + | |
| Neutropenia | + + + + + | + + | + |
| Peripheral sensory neuropathy | + + | + + | |
| Diarrhea | + | + | + |
| Anemia | + + + | + | + |
| Fatigue | + + + | + + + | + |
| Increased lipase | + | + | |
| Decreased appetite | + | ||
| Myelosuppression | + | ||
| Infection | + | + | |
| Renal impairment | + | ||
| Hypertension | + |
The data of TRAEs are based on the clinical trials listed in Table 1. Statistics were conducted on the basis of the most common TRAEs observed in each clinical trial. “ + ” represents one occurrence in the enumeration of the most common TRAEs in the corresponding clinical trial regimens
Sacituzumab govitecan
SG is a novel second-generation ADC that consists of an IgG1 kappa antibody targeting Trop-2 (a surface antigen on trophoblast cells), SN-38 (the active metabolite of irinotecan, a topoisomerase I inhibitor), and a hydrolyzable linker [40–42]. Trop-2 is a transmembrane glycoprotein that is highly expressed on the surface of most epithelial cancer cells. High expression of Trop-2 is associated with a poor prognosis in various tumor types, including mUC [43–45].
In 2015, a clinical study evaluating SG was published, involving 6 patients with mUC refractory to platinum-based regimens and prior systemic therapies who received SG monotherapy. The results revealed clinically significant responses in three patients, with PFS ranging from 6.7 to 8.2 months and OS from 7.5+ to 11.4+ months. These findings indicated initial tolerability of SG in this population and established the rationale for subsequent phase II clinical investigation [46]. In Cohort 1 of a multi-cohort, open-label phase II trial (NCT03547973), the efficacy of SG was evaluated in 113 patients with la or unresectable disease or mUC who had progressed following prior platinum-based chemotherapy and checkpoint inhibitor therapy. With a median follow-up of 9.1 months, the ORR was 27%, with 77% of patients experiencing an improvement; extending follow-up to 10.5 months increased the ORR to 28% [47]. These results supported the FDA’s accelerated approval of SG for the treatment of patients with la/mUC in April 2021 [48]. In Cohorts 2 and 3 of the trial, with median follow-up durations of 9.3 months and 14.8 months, the ORR were 32% [49] and 41% [50], respectively. In cohort 3, the combination of SG + Pb demonstrated a high response rate and an overall manageable toxicity profile in patients with mUC who had progressed after platinum-based chemotherapy, with no new safety signals emerging. These findings provide valuable insights into emerging therapeutic strategies for platinum-refractory bladder cancer and substantiate further investigation of the efficacy of SG combined with checkpoint inhibitors [50]. Pooled analysis across all three cohorts yielded a composite ORR of 30% [45].
In the phase III TROPiCS-04 trial (NCT04527991), 711 patients pretreated with platinum-based chemotherapy and ICIs were enrolled. After a median follow-up of 9.2 months, the primary endpoint was not met (median OS for SG vs. chemotherapy, 10.3 vs. 9.0 months). The results revealed that patients in the SG group had no significant improvement in OS compared with those in the therapy of physician’s choice (paclitaxel, docetaxel, or vinflunine) group [51]. The combination of SG+EV demonstrated a promising ORR of 70% with manageable safety profiles in a phase I trial involving patients who progressed on platinum-based chemotherapy and/or immunotherapy. These findings establish the investigational value of ADC combination regimens in patients with disease progression after prior therapy and warrant further clinical evaluation of this therapeutic strategy [39].
The occurrence of TRAEs is observed in some patients who have undergone ADCs therapy, and TRAEs of grade ≥ 3 can reach 87% in SG+EV (Table 3). Available data from clinical trials demonstrate that the most common grade ≥ 3 TRAEs include neutropenia, leukopenia, anemia, diarrhea, lymphopenia, febrile neutropenia, urinary tract infection, fatigue, flank pain, and bacteremia (Table 3).
Table 3.
Clinical trials of sacituzumab govitecan (SG)
| Clinical trials | Trial design | Participants (N) | Primary endpoints | TRAEs (%) | |
|---|---|---|---|---|---|
| Phase I [46] | SGb | mUC/6 | PFS:6.7 m−8.2 m OS:7.5+m−11.4+m | Grade ≥ 3I, 33.3% | |
| TROPHY-U-01, hase II [47, 48],C1 | SGa | la/mUC/113 | ORR 27% | Grade ≥ 3II, 5% | |
|
TROPHY-U-01, Phase II [49], C2 |
SGa | la/mUC/38 | ORR 32% | Grade ≥ 3III, 87% | |
| TROPHY-U-01, Phase II [50], C3 | SGa+Pb | mUC/41 | ORR 41% | Grade ≥ 3IV, 61% | |
| Phase I [39] | SG+EV | la/mUC/23 | safety/tolerability | Grade ≥ 3V, 78% | |
| TROPiCS-04, Phase III [51] | SG vs chemotherapy | la/mUC/711 | OS (not met) | Grade ≥ 3VI, 67% vs 35% | |
IFlank pain and bacteremia
IINeutropenia, leukopenia, anemia, diarrhea, febrile neutropenia, lymphopenia, and urinary tract infection
IIINeutropenia anemia, leukopenia, fatigue, and diarrhea
IVNeutropenia, leukopenia, and diarrhea
VNeutropenia, diarrhea, anemia, fatigue, infection
VINeutropenia
a10 mg/kg on days 1 and 8 of 21-day cycle
b8 mg/kg, 10 mg/kg, 11 mg/kg, 12 mg/kg, on days 1and 8 of 21-day cycles
Disitamab vedotin
DV, also known as RC48, received approval from China’s National Medical Products Administration on 15 June 2021 for the treatment of locally advanced or metastatic gastric cancer and breast cancer [52]. As the first ADC approved in China, it has demonstrated clinically significant responses and survival benefits in treated patient populations [53]. It is composed of a humanized human epidermal growth factor receptor 2 (HER2) antibody, a cleavable linker (mc-VC-PABC), and a cytotoxic payload MMAE [54]. Studies demonstrate elevated HER2 expression in UC [21], with expression levels positively correlating with clinical stage [55]. UC has emerged as the third type of tumor eligible for ADC therapy, following gastric and breast cancers. In January 2022, on the basis of the findings of the RC48-C009 study [12], DV was granted regulatory approval in China for platinum-refractory mUC patients. Subsequent phase I/II clinical trials have demonstrated significant therapeutic efficacy of DV as second-line therapy in HER2-positive la/mUC patients with prior platinum-based chemotherapy [12, 56–58]. DV has also demonstrated potential in the neoadjuvant therapy of locally advanced bladder cancer. A multicenter real-world study evaluated DV combined with PD-1 inhibitors (tislelizumab/toripalimab) in HER2-positive locally advanced bladder cancer patients. Nine patients with cT2-T4aN0-3M0 disease were enrolled, achieving a confirmed ORR of 88.9% (5 complete responses [CR], 3 partial responses [PR]) at a median follow-up of 12 months. One patient exhibited disease progression with pathological upstaging from T2 N0M0 to T3aN2M0 [59]. A multicenter phase Ib/II study (HOPE-03, ChiCTR2200060153) was conducted to investigate the efficacy and safety of DV combined with tislelizumab in 51 patients with locally advanced or metastatic bladder cancer. Among them, 6 patients were enrolled in phase Ib and 45 patients were enrolled in phase II. The primary endpoints of this study included clinical CR, pathological CR, and safety assessment; the results are being followed up [60]. Additional relevant clinical trials are summarized in Table 4.
Table 4.
Clinical trials of Disitamab vedotin (DV)
| Clinical trials | Participants (cTNM/N) | Primary endpoints | Nation |
|---|---|---|---|
| DVa+PD-1 A | cT2-T4aN0-3M0/9 | 88.9% ORR [59] | China |
| DVa+PD-1 A | cT2-4bN0-3M0-1a/51 | Following [60] | China |
| DVa+PD-1 A | cT2-4aN0-2M0/11 | 81.8% ORR [61] | China |
| DVa+PD-1 A | la/mUC/185 | 62.5% ORR [55] | China |
| DVa | la/mUC/43 | 51.2% ORR [13] | China |
| DVa | la/mUC/107 | 50.5% ORR [12] | China |
| DVa vs DVa+PD-1 A | la/mUC/38 | 63.2% ORR [62] | China |
| DV vs DV+PD-1 A | la/mUC/36 | 38.9% ORR [57] | China |
PD-1 A: programmed death-1 antibody (toripalimab or tislelizumabo or pembrolizumab or envafolimab or sintilimab); la/mUC locally advanced or metastatic urothelial carcinoma
a2 mg/kg, once every 2 weeks
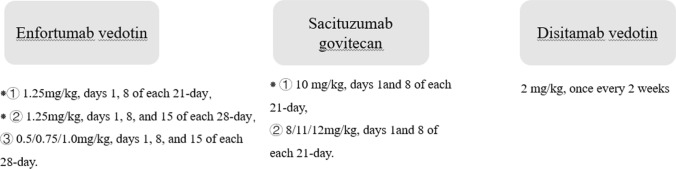
DV can be utilized as monotherapy or in combination with PD-1 inhibitors. The recommended dosage and administration methods for DV are detailed in Table 4 or Fig. 1. Peripheral sensory neuropathy, alopecia, leukopenia, neutropenia, and elevated transaminases were observed as the most common grade 1–2 TRAEs in DV monotherapy. The most common grade ≥ 3 TRAEs in monotherapy were peripheral sensory neuropathy and neutropenia. In combination therapy with DV plus PD-1 antibodies (PD-1 A), gastrointestinal symptoms (decreased appetite/anorexia, nausea/vomiting), peripheral sensory neuropathy, weakness, fatigue, and anemia were the most common grade 1–2 TRAEs. The most common grade ≥ 3 TRAEs associated with this combination were decreased appetite, gastrointestinal bleeding, intestinal obstruction, immune-related pneumonia, and recurrent urinary tract infections (Table 5).
Fig. 1.
The dosages utilized in the clinical trials of DV, EV, and SG, “⁕” is the common recommended dosage and method
Table 5.
Treatment-related adverse events (TRAEs) associated with DV
| TRAEs | DV monotherapy | DV+PD-1 A | ||
|---|---|---|---|---|
| Grade 1–2 | Grade ≥ 3 | Grade1–2 | Grade ≥ 3 | |
| Decreased appetite/anorexia | + | + + + + | + | |
| Rash | + + | |||
| Weak/asthenia/debilitation | + | + + + | ||
| Hypothyroidism | + | |||
| Fatigue | + | + + + | ||
| Gastrointestinal bleeding | + | |||
| Intestinal obstruction | + | |||
| Peripheral sensory neuropath | + + | + + | + + + + | |
| Anemia | + + + | |||
| Immune-related pneumonia | + | |||
| Recurrent urinary tract infection | + | |||
| Alopecia | + + | + + | ||
| Leukopenia | + + | + | ||
| Neutropenia | + + | + + | ||
| Elevated transaminase (AST/ALT) | + + | + | ||
| Bone marrow suppression | + | |||
| Nausea/vomiting | + + + | |||
| Proteinuria | + | |||
| Hypoalbuminemia | + | |||
The data of TRAEs are based on the clinical trials listed in Table 1. Statistical analysis was conducted on the basis of the most common TRAEs observed in each clinical trial. “+” represents one occurrence in the enumeration of the most common TRAEs in the corresponding clinical trial regimens
Other antibody–drug conjugates
Trastuzumab deruxtecan (T-DXd), an ADC approved in the United States, Europe, and Japan for HER2-mutated non-small cell lung cancer. In the phase II clinical trial (DESTINY-PanTumor01), T-DXd was used to treat 102 patients with unresectable or metastatic solid tumors with specific activating HER2 mutations (including UC), and achieved an ORR of 29.4% [63]. In the DESTINY-PanTumor02 trial, T-DXd was evaluated in patients with locally advanced or metastatic HER2-positive solid tumors (immunohistochemistry [IHC] 3+or 2+) who had received ≥ 1 prior systemic therapy or lacked alternative treatment options. Results demonstrated an ORR of 39% in patients with HER2-positive UC, with higher efficacy in the IHC 3+subgroup versus IHC 2+(56.3% vs 35%) [21]. Both trial cohorts achieved durable clinical benefits with meaningful survival outcomes. These findings substantiate T-DXd’s potential as a fourth-line or subsequent therapeutic option for HER2-positive solid tumors, particularly in patients with HER2-activating mutations who have progressed after prior therapies or lack satisfactory alternative therapy. In the DESTINY-PanTumor01 and DESTINY-PanTumor02 trials, the incidences of grade ≥ 3 TRAEs were 51% and 40.8%, respectively. Particular attention should be paid to the risk of drug-related interstitial lung disease associated with this agent. In a clinical trial of trastuzumab plus pertuzumab (NCT02091141), patients with HER2 amplification and/or overexpression and/or mutation solid tumors were treated. The results revealed that trastuzumab plus pertuzumab showed activity in a variety of HER2 amplification and/or overexpression with wild-type KRAS tumors, but the antitumor activity was limited in patients with KRAS mutations, HER2 mutations alone, or 0–1+HER2 expression [64].
In addition, other promising novel ADCs are being developed [10, 65–67]. For example, DS-7300a, a novel ADC that targets B7-H3, highly expressed in bladder cancer, is expected to be a potential therapeutic target for bladder cancer in the future [68].
Opportunities and challenges
The emergence of ADCs has expanded the therapeutic options available for patients with la/mUC. In addition, the extension of their therapeutic application to the therapy of non-metastatic MIBC is also being considered. The cohort L of the EV-103 (EV monotherapy) trial includes platinum-ineligible patients with MIBC (cT2-T4aN1M0 or cT1-T4aN1M0), with pCR as the primary endpoint [69]. The VOLGA trial (EV+durvalumab with or without tremelimumab) for cisplatin-ineligible MIBC patients, the EYNOTE-095/EV-303 trial [70] (EV+Pb) for cisplatin-ineligible patients, and the KEYNOTE-B15/EV-304 trial (EV+Pb) for cisplatin-eligible MIBC patients [66].
What strategies can effectively mitigate the occurrence of TRAEs, particularly fatal drug TRAEs? How can a balance be achieved among dosage, patient tolerability, TRAEs, financial costs, and toxicity? In particular, the combination of EV plus Pb as a new first-line therapy option for patients with la/mUC. The mechanism of resistance to ADCs remains unclear. When resistance or disease progression occurs, what therapeutic approach should be adopted in the next step? Looking for new targets? Or explore dual ADC combinations or combinations with other approved ICIs? Can these agents be used sequentially? Can they be used again if used earlier? The search for new therapeutic targets and research on combination therapies with other agents are already underway, with some having yielded encouraging results. Meanwhile, the application of ADCs in MIBC warrants focused attention.
Acknowledgements
We express our sincere gratitude to the editors and reviewers of our manuscript.
Author contributions
F.H.Z and Q.J.H wrote the main manuscript text, C.T and M.L.J provided the idea, T.D checked the grammar of the manuscript. All authors reviewed the manuscript.
Funding
None.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
This review article is based on previously published studies and does not involve new human or animal research. The work was conducted in accordance with the principles of the Declaration of Helsinki.
Human ethics and consent to participate
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA. 2021;71(3):209–49. [DOI] [PubMed] [Google Scholar]
- 2.Siegel RL, Giaquinto AN, Jemal A. Cancer statistics, 2024. CA. 2024;74(1):12–49. [DOI] [PubMed] [Google Scholar]
- 3.Lopez-Beltran A, Cookson MS, Guercio BJ, Cheng L. Advances in diagnosis and treatment of bladder cancer. BMJ. 2024;384:e076743. [DOI] [PubMed] [Google Scholar]
- 4.Lenis AT, Lec PM, Chamie K, Mshs MD. Bladder cancer: a review. JAMA. 2020;324(19):1980–91. [DOI] [PubMed] [Google Scholar]
- 5.Patel VG, Oh WK, Galsky MD. Treatment of muscle-invasive and advanced bladder cancer in 2020. CA. 2020;70(5):404–23. [DOI] [PubMed] [Google Scholar]
- 6.Von Der Maase H, Hansen SW, Roberts JT, et al. Gemcitabine and cisplatin versus methotrexate, vinblastine, doxorubicin, and cisplatin in advanced or metastatic bladder cancer: results of a large, randomized, multinational, multicenter, phase III study. J Clin Oncol. 2023;41(23):3881–90. [DOI] [PubMed] [Google Scholar]
- 7.Moussa MJ, Campbell MT, Alhalabi O. revisiting treatment of metastatic urothelial cancer: where do cisplatin and platinum ineligibility criteria stand? Biomedicines. 2024. 10.3390/biomedicines12030519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Von Der Maase H, Sengelov L, Roberts JT, et al. Long-term survival results of a randomized trial comparing gemcitabine plus cisplatin, with methotrexate, vinblastine, doxorubicin, plus cisplatin in patients with bladder cancer. J Clin Oncol. 2005;23(21):4602–8. [DOI] [PubMed] [Google Scholar]
- 9.De Santis M, Bellmunt J, Mead G, et al. Randomized phase II/III trial assessing gemcitabine/carboplatin and methotrexate/carboplatin/vinblastine in patients with advanced urothelial cancer who are unfit for cisplatin-based chemotherapy: EORTC study 30986. J Clin Oncol. 2012;30(2):191–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nadal R, Valderrama BP, Bellmunt J. Progress in systemic therapy for advanced-stage urothelial carcinoma. Nat Rev Clin Oncol. 2024. 10.1038/s41571-023-00826-2. [DOI] [PubMed] [Google Scholar]
- 11.Compérat E, Amin MB, Cathomas R, et al. Current best practice for bladder cancer: a narrative review of diagnostics and treatments. Lancet. 2022;400(10364):1712–21. [DOI] [PubMed] [Google Scholar]
- 12.Sheng X, Wang L, He Z, et al. Efficacy and safety of disitamab vedotin in patients with human epidermal growth factor receptor 2-positive locally advanced or metastatic urothelial carcinoma: a combined analysis of two phase II clinical trials. J Clin Oncol. 2024;42(12):1391–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sheng X, Yan X, Wang L, et al. Open-label, multicenter, phase ii study of RC48-ADC, a HER2-targeting antibody-drug conjugate, in patients with locally advanced or metastatic urothelial carcinoma. Clin Cancer Res. 2021;27(1):43–51. [DOI] [PubMed] [Google Scholar]
- 14.Norsworthy KJ, Ko C-W, Lee JE, et al. FDA approval summary: mylotarg for treatment of patients with relapsed or refractory CD33-positive acute myeloid leukemia. Oncologist. 2018;23(9):1103–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fu Z, Li S, Han S, et al. Antibody drug conjugate: the “biological missile” for targeted cancer therapy. Signal Transduct Target Ther. 2022;7(1):93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Drago JZ, Modi S, Chandarlapaty S. Unlocking the potential of antibody-drug conjugates for cancer therapy. Nat Rev Clin Oncol. 2021;18(6):327–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shefet-Carasso L, Benhar I. Antibody-targeted drugs and drug resistance–challenges and solutions. Drug Resist Updat. 2015;18:36–46. [DOI] [PubMed] [Google Scholar]
- 18.Nelson BE, Meric-Bernstam F. Leveraging TROP2 antibody-drug conjugates in solid tumors. Annu Rev Med. 2024;75:31–48. [DOI] [PubMed] [Google Scholar]
- 19.Passaro A, Jänne PA, Peters S. Antibody-drug conjugates in lung cancer: recent advances and implementing strategies. J Clin Oncol. 2023;41(21):3747–61. [DOI] [PubMed] [Google Scholar]
- 20.Chen Y-F, Xu Y-Y, Shao Z-M, Yu K-D. Resistance to antibody-drug conjugates in breast cancer: mechanisms and solutions. Cancer Commun. 2023;43(3):297–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meric-Bernstam F, Makker V, Oaknin A, et al. Efficacy and safety of trastuzumab deruxtecan in patients with HER2-expressing solid tumors: primary results from the DESTINY-PanTumor02 phase ii trial. J Clin Oncol. 2024;42(1):47–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sarfaty M, Rosenberg JE. Antibody-drug conjugates in urothelial carcinomas. Curr Oncol Rep. 2020;22(2):13. [DOI] [PubMed] [Google Scholar]
- 23.Challita-Eid PM, Satpayev D, Yang P, et al. Enfortumab vedotin antibody-drug conjugate targeting nectin-4 is a highly potent therapeutic agent in multiple preclinical cancer models. Can Res. 2016;76(10):3003–13. [DOI] [PubMed] [Google Scholar]
- 24.Liu Y, Han X, Li L, et al. Role of Nectin-4 protein in cancer (Review). Int J Oncol. 2021. 10.3892/ijo.2021.5273. [DOI] [PubMed] [Google Scholar]
- 25.Heath EI, Rosenberg JE. The biology and rationale of targeting nectin-4 in urothelial carcinoma. Nat Rev Urol. 2021. 10.1038/s41585-020-00394-5. [DOI] [PubMed] [Google Scholar]
- 26.Rosenberg JE, Powles T, Sonpavde GP, et al. EV-301 long-term outcomes: 24-month findings from the phase III trial of enfortumab vedotin versus chemotherapy in patients with previously treated advanced urothelial carcinoma. Ann Oncol. 2023;34(11):1047–54. [DOI] [PubMed] [Google Scholar]
- 27.Yu EY, Petrylak DP, O’donnell PH, et al. Enfortumab vedotin after PD-1 or PD-L1 inhibitors in cisplatin-ineligible patients with advanced urothelial carcinoma (EV-201): a multicentre, single-arm, phase 2 trial. Lancet Oncol. 2021;22(6):872–82. [DOI] [PubMed] [Google Scholar]
- 28.Rosenberg J, Sridhar SS, Zhang J, et al. EV-101: a phase I study of single-agent enfortumab vedotin in patients with nectin-4-positive solid tumors, including metastatic urothelial carcinoma. J Clin Oncol. 2020;38(10):1041–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rosenberg O’donnell JEPH, Balar AV, et al. Pivotal trial of enfortumab vedotin in urothelial carcinoma after platinum and anti-programmed death 1/programmed death ligand 1 therapy. J Clin Oncol. 2019;37(29):2592–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Matsubara N, Yonese J, Kojima T, et al. Japanese subgroup analysis of EV-301: an open-label, randomized phase 3 study to evaluate enfortumab vedotin versus chemotherapy in subjects with previously treated locally advanced or metastatic urothelial carcinoma. Cancer Med. 2023;12(3):2761–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Powles T, Rosenberg JE, Sonpavde GP, et al. Enfortumab vedotin in previously treated advanced urothelial carcinoma. N Engl J Med. 2021;384(12):1125–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.O’donnellMilowskyPetrylak PHMIDP, et al. Enfortumab vedotin with or without pembrolizumab in cisplatin-ineligible patients with previously untreated locally advanced or metastatic urothelial cancer. J Clin Oncol. 2023;41(25):4107–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hoimes CJ, Flaig TW, Milowsky MI, et al. Enfortumab vedotin plus pembrolizumab in previously untreated advanced urothelial cancer. J Clin Oncol. 2023;41(1):22–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Takahashi S, Uemura M, Kimura T, et al. A phase I study of enfortumab vedotin in Japanese patients with locally advanced or metastatic urothelial carcinoma. Invest New Drugs. 2020;38(4):1056–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brave MH, Maguire WF, Weinstock C, et al. FDA approval summary: enfortumab vedotin plus pembrolizumab for locally advanced or metastatic urothelial carcinoma. Clin Cancer Res. 2024;30(21):4815–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Powles T, Valderrama BP, Gupta S, et al. Enfortumab vedotin and pembrolizumab in untreated advanced urothelial cancer. N Engl J Med. 2024;390(10):875–88. [DOI] [PubMed] [Google Scholar]
- 37.Mamtani R, Ulloa-Pérez E, Parikh RB, et al. Real-world uptake of enfortumab vedotin plus pembrolizumab after US Food and Drug Administration approval among patients with advanced urothelial cancer. Eur Urol. 2024. 10.1016/j.eururo.2024.08.012. [DOI] [PubMed] [Google Scholar]
- 38.Powles T, Bellmunt J, Comperat E, et al. ESMO Clinical Practice Guideline interim update on first-line therapy in advanced urothelial carcinoma. Ann Oncol. 2024;35(6):485–90. [DOI] [PubMed] [Google Scholar]
- 39.Mcgregor BA, Sonpavde GP, Kwak L, et al. The Double Antibody Drug Conjugate (DAD) phase I trial: sacituzumab govitecan plus enfortumab vedotin for metastatic urothelial carcinoma. Ann Oncol. 2024;35(1):91–7. [DOI] [PubMed] [Google Scholar]
- 40.Moon S-J, Govindan SV, Cardillo TM, et al. Antibody conjugates of 7-ethyl-10-hydroxycamptothecin (SN-38) for targeted cancer chemotherapy. J Med Chem. 2008;51(21):6916–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mathijssen RH, Van Alphen RJ, Verweij J, et al. Clinical pharmacokinetics and metabolism of irinotecan (CPT-11). Clin Cancer Res. 2001;7(8):2182–94. [PubMed] [Google Scholar]
- 42.Goldenberg DM, Cardillo TM, Govindan SV, et al. Trop-2 is a novel target for solid cancer therapy with sacituzumab govitecan (IMMU-132), an antibody-drug conjugate (ADC). Oncotarget. 2015;6(26):22496–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zaman S, Jadid H, Denson AC, Gray JE. Targeting Trop-2 in solid tumors: future prospects. Onco Targets Ther. 2019;12:1781–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Goldenberg DM, Stein R, Sharkey RM. The emergence of trophoblast cell-surface antigen 2 (TROP-2) as a novel cancer. Oncotarget. 2018;9(48):28989–9006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Loriot Y, Balar AV, Petrylak DP, et al. Sacituzumab govitecan demonstrates efficacy across tumor Trop-2 expression levels in patients with advanced urothelial cancer. Clin Cancer. 2024;30(15):3179–88. [DOI] [PubMed] [Google Scholar]
- 46.Faltas B, Goldenberg DM, Ocean AJ, et al. Sacituzumab govitecan, a novel antibody-drug conjugate, in patients with metastatic platinum-resistant urothelial carcinoma. Clin Genitourin Cancer. 2016;14(1):e75–9. [DOI] [PubMed] [Google Scholar]
- 47.Loriot Y, Petrylak DP, Rezazadeh Kalebasty A, et al. TROPHY-U-01, a phase II open-label study of sacituzumab govitecan in patients with metastatic urothelial carcinoma progressing after platinum-based chemotherapy and checkpoint inhibitors: updated safety and efficacy outcomes. Ann Oncol. 2024;35(4):392–401. [DOI] [PubMed] [Google Scholar]
- 48.Tagawa ST, Balar AV, Petrylak DP, et al. TROPHY-U-01: a phase ii open-label study of sacituzumab govitecan in patients with metastatic urothelial carcinoma progressing after platinum-based chemotherapy and checkpoint inhibitors. J Clin Oncol. 2021;39(22):2474–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Petrylak DP, Tagawa ST, Jain RK, et al. TROPHY-U-01 cohort 2: a phase ii study of sacituzumab govitecan in cisplatin-ineligible patients with metastatic urothelial cancer progressing after previous checkpoint inhibitor therapy. J Clin Oncol. 2024;42(29):3410–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Grivas P, Pouessel D, Park CH, et al. Sacituzumab govitecan in combination with pembrolizumab for patients with metastatic urothelial cancer that progressed after platinum-based chemotherapy: TROPHY-U-01 cohort 3. J Clin Oncol. 2024;42(12):1415–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Powles T, Tagawa S, Vulsteke C, et al. Sacituzumab govitecan in advanced urothelial carcinoma: TROPiCS-04, a phase III randomized trial. Ann Oncol. 2025. 10.1016/j.annonc.2025.01.011. [DOI] [PubMed] [Google Scholar]
- 52.Deeks ED. Disitamab vedotin: first approval. Drugs. 2021;81(16):1929–35. [DOI] [PubMed] [Google Scholar]
- 53.Peng Z, Liu T, Wei J, et al. Efficacy and safety of a novel anti-HER2 therapeutic antibody RC48 in patients with HER2-overexpressing, locally advanced or metastatic gastric or gastroesophageal junction cancer: a single-arm phase II study. Cancer Commun. 2021;41(11):1173–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jiang J, Li S, Shan X, et al. Preclinical safety profile of disitamab vedotin: a novel anti-HER2 antibody conjugated with MMAE. Toxicol Lett. 2020;324:30–7. [DOI] [PubMed] [Google Scholar]
- 55.Zhu K, Chang Y, Zhao D, et al. Expression of HER2 in high-grade urothelial carcinoma based on Chinese expert consensus and the clinical effects of disitamab vedotin-tislelizumab combination therapy in the treatment of advanced patients. Front Pharmacol. 2024;15:1355081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yorozu T, Sato S, Kimura T, et al. HER2 status in molecular subtypes of urothelial carcinoma of the renal pelvis and ureter. Clin Genitourin Cancer. 2020;18(4):e443–9. [DOI] [PubMed] [Google Scholar]
- 57.Chen M, Yao K, Cao M, et al. HER2-targeting antibody-drug conjugate RC48 alone or in combination with immunotherapy for locally advanced or metastatic urothelial carcinoma: a multicenter, real-world study. Cancer Immunol Immunother. 2023;72(7):2309–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Shi F, Liu Y, Zhou X, et al. Disitamab vedotin: a novel antibody-drug conjugates for cancer therapy. Drug Delivery. 2022;29(1):1335–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wei Y, Zhang R, Yu C, et al. Disitamab vedotin in combination with immune checkpoint inhibitors for locally and locally advanced bladder urothelial carcinoma: a two-center’s real-world study. Front Pharmacol. 2023;14:1230395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wen F, Lin T, Zhang P, Shen Y. RC48-ADC combined with tislelizumab as neoadjuvant treatment in patients with HER2-positive locally advanced muscle-invasive urothelial bladder cancer: a multi-center phase Ib/II study (HOPE-03). Front Oncol. 2023;13:1233196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wang A, Chen M, Li D, et al. Disitamab vedotin alone or in combination with immune checkpoint inhibitors in bladder-sparing treatment of muscle-invasive bladder cancer: a real-world study. Clin Genitourin Cancer. 2024;22(3):102085. [DOI] [PubMed] [Google Scholar]
- 62.Xu J, Zhang H, Zhang L, et al. Real-world effectiveness and safety of RC48-ADC alone or in combination with PD-1 inhibitors for patients with locally advanced or metastatic urothelial carcinoma: a multicenter, retrospective clinical study. Cancer Med. 2023;12(23):21159–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Li BT, Meric-Bernstam F, Bardia A, et al. Trastuzumab deruxtecan in patients with solid tumours harbouring specific activating HER2 mutations (DESTINY-PanTumor01): an international, phase 2 study. Lancet Oncol. 2024;25(6):707–19. [DOI] [PubMed] [Google Scholar]
- 64.Sweeney CJ, Hainsworth JD, Bose R, et al. MyPathway human epidermal growth factor receptor 2 basket study: pertuzumab + trastuzumab treatment of a tissue-agnostic cohort of patients with human epidermal growth factor receptor 2-altered advanced solid tumors. J Clin Oncol. 2024;42(3):258–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Vlachou E, Johnson BA, Hoffman-Censits J. The role of antibody-drug conjugates in urothelial cancer: a review of recent advances in the treatment of locally advanced and metastatic urothelial cancer. Clin Med Insights Oncol. 2024. 10.1177/11795549241290787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.D’angelo A, Chapman R, Sirico M, et al. An update on antibody-drug conjugates in urothelial carcinoma: state of the art strategies and what comes next. Cancer Chemother Pharmacol. 2022;90(3):191–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Criscitiello C, Morganti S, Curigliano G. Antibody-drug conjugates in solid tumors: a look into novel targets. J Hematol Oncol. 2021;14(1):20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Yamato M, Hasegawa J, Maejima T, et al. DS-7300a, a DNA topoisomerase I inhibitor, DXd-based antibody-drug conjugate targeting B7–H3, exerts potent antitumor activities in preclinical models. Mol Cancer Ther. 2022;21(4):635–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kim KH, Lee HW, Ha HK, Seo HK. Perioperative systemic therapy in muscle invasive bladder cancer: current standard method, biomarkers and emerging strategies. Investig Clin Urol. 2023;64(3):202–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Galsky MD, Hoimes CJ, Necchi A, et al. Perioperative pembrolizumab therapy in muscle-invasive bladder cancer: phase III KEYNOTE-866 and KEYNOTE-905/EV-303. Future Oncol. 2021;17(24):3137–50. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.