Abstract
Purpose
This study was conducted to estimate proportion of individuals undergoing screening for cardiovascular disease (CVD) and its risk factors and to identify predictors of CVD, blood pressure, and blood cholesterol screening.
Patients and Methods
This cross-sectional study was conducted in 48 primary healthcare centers in Saudi Arabia and 14,239 participants were enrolled. The analysis was performed in SPSS version 26 and adjusted odds ratios (AOR) and 95% Cis were reported.
Results
Blood pressure screening was reported by 35.3%, cholesterol screening by 9.3%, and cardiovascular screening by 3.7%. Significant positive predictors for blood pressure screening included older age (50–75 years: AOR 1.34, 95% CI: 1.20–1.50; ≥75 years: AOR 2.12, 95% CI: 1.84–2.43), being married (AOR: 1.15; 95% CI: 1.04–1.27), non-smoking (AOR: 1.97; 95% CI: 1.79–2.17), physical activity (AOR: 1.16; 95% CI: 1.05–1.28), and diabetes (AOR: 2.14; 95% CI: 1.88–2.44). For cholesterol screening, significant positive predictors were older age (≥75 years: AOR 1.89, 95% CI: 1.56–2.29), unemployment (AOR: 1.26; 95% CI: 1.10–1.45), insurance coverage (AOR: 1.52; 95% CI: 1.33–1.74), smoking (AOR: 1.32; 95% CI: 1.14–1.53), diabetes history (AOR: 1.33; 95% CI: 1.09–1.61), and hypertension (AOR: 1.66; 95% CI: 1.36–2.02). For cardiovascular screening, significant positive predictors included older age (≥75 years: AOR 1.81, 95% CI: 1.35–2.43), unemployment (AOR: 1.53; 95% CI: 1.24–1.88), insurance coverage (AOR: 1.56; 95% CI: 1.27–1.92), smoking (AOR: 1.89; 95% CI: 1.52–2.34), diabetes (AOR: 1.85; 95% CI: 1.41–2.43), and high cholesterol (AOR: 1.76; 95% CI: 1.31–2.36).
Conclusion
A very low proportion of Saudi residents have undergone blood pressure, cholesterol, and CVD screening. Common predictors of screening included older age, insurance coverage, diabetes, hypertension, physical activity, and high cholesterol levels. Low prevalence of screening is alarming, and Saudi Government needs to implement strategies that can help increase proportion of Saudi residents who receive blood pressure, cholesterol, and CVD screening.
Keywords: screening, blood pressure, cholesterol, cardiovascular diseases, Saudi Arabia
Introduction
Cardiovascular diseases (CVDs) are a significant global health concern and a major contributor to mortality.1,2 Globally, CVDs are estimated to be the leading cause of death, accounting for a substantial proportion of all fatalities.1,2 Raised blood pressure and elevated cholesterol levels are well-established and important modifiable risk factors for the development of CVDs.1,2 Effective management of high blood cholesterol and high blood pressure through lifestyle modifications and medical therapy has been shown to reduce the incidence of morbidity and mortality associated with cardiovascular diseases. A fundamental step towards adequately controlling these risk factors is their early detection, which can be achieved through screening programs. Recognizing the substantial and growing burden of CVDs, national guidelines in high-income countries such as the United Kingdom (UK) and the United States of America (USA) recommend screening for cardiovascular risk factors, including high blood cholesterol and high blood pressure.3–6
In the UK, the National Health Service (NHS) recommends regular blood pressure checks for adults at least every five years, or more frequently for individuals with risk factors.7–9 Regarding cholesterol screening, the guidelines are more targeted, often recommending testing for individuals over 40 years of age or those with other CVD risk factors, with the frequency determined by individual risk assessment.7–9 Similarly, in the USA, the US Preventive Services Task Force (USPSTF) recommends routine blood pressure screening for all adults aged 18 years and older.10 For cholesterol screening, the USPSTF recommends routine screening in men aged 35 and older and women aged 45 and older, as well as earlier screening for adults aged 20 to 35 years who have other risk factors for coronary heart disease10 These guidelines in the UK and USA aim to facilitate the early identification and management of key modifiable risk factors for CVD.
Despite the recognition of the importance of screening in high-income countries, data on the prevalence and predictors of blood pressure, cholesterol, and overall cardiovascular screening in Saudi Arabia are limited. To address this gap, baseline data on screening prevalence and its predictors among Saudis in primary healthcare settings are critical for informing public health strategies and improving cardiovascular disease prevention efforts in the Kingdom. Since the burden of non-communicable diseases such as hypertension, diabetes, and cardiovascular diseases is increasing in Saudi Arabia,11,12 there is a need to develop such guidelines for screening. For example, the evidence suggests that non-communicable diseases account for 73% of the disease burden and approximately one-third of the total deaths in Saudi Arabia.13 Given the high burden of cardiovascular diseases in Saudi Arabia, the first step in developing the guidelines is assessing the need assessment of communities for various risk factors of cardiovascular diseases. However, the data on the need assessment, mainly data on screening for modifiable cardiovascular disease risk factors are limited. This study aimed to address this knowledge gap by estimating the proportion of Saudi residents currently undergoing blood pressure and cholesterol screening. We also identified the predictors of blood pressure, cardiovascular screening, and cardiovascular screening among residents of Saudi Arabia.
Materials and Methods
Study Design, Duration, and Setting
This cross-sectional survey was conducted between March and July 2023 as part of a broader health system reform initiative in Saudi Arabia (2021–2022) aimed at transitioning to a health cluster model. The study was carried out in the Riyadh region, which is organized into three health clusters managed by Central Health Services. These clusters encompass both primary healthcare centers (PHCs) and hospitals. For this study, we focused on Health Cluster 2, which serves approximately 3.7 million residents and includes 105 PHCs, due to its diverse population and extensive healthcare infrastructure. From this cluster, a stratified random sampling method was used to select 48 PHCs, ensuring proportional representation of both urban and suburban areas.
Sampling Technique and Study Sample
A multi-stage cluster sampling method was employed to obtain a representative sample of individuals utilizing PHCs within Health Cluster 2 in Riyadh. In the first stage, 48 PHCs were selected using stratified random sampling based on their geographical location (urban/suburban). In the second stage, within each of the selected PHCs, eligible participants were identified using systematic random sampling. Data collectors approached every nth eligible patient presenting to the PHC until the desired sample size was achieved for that center. The sampling interval (n) was determined by dividing the estimated daily patient volume by the target number of participants per PHC.
Eligibility Criteria
The study targeted adults aged 18 years and above who were visiting the selected PHCs, irrespective of their nationality (Saudi or non-Saudi resident). Exclusion criteria included healthcare practitioners and staff working at the PHCs, individuals under 18 years of age, patients with cognitive impairments that would hinder their ability to understand the survey questions, and those who declined to provide informed consent. A total of 14,239 participants completed the electronic survey and were included in the final analysis.
Study Questionnaire and Data Collection
An electronic questionnaire, initially developed from English-language sources, was translated into Arabic and then back-translated into English to ensure accuracy. Prior to data collection, the study objectives and procedures were explained to eligible patients, and written informed consent was obtained from all participants. Data were collected by trained data collectors who were present while participants completed the electronic survey.
The questionnaire included sections on socio-demographic characteristics (eg, age, gender, marital status, education, employment), behavioural characteristics (eg, daily physical activity, alcohol intake, cigarette smoking habits, fast-food consumption), and medical conditions (eg, diabetes, obesity, hypertension, cardiovascular issues, and hypercholesterolemia).
Specifically, regarding screening questions, participants were asked if they had ever been screened for blood pressure, blood cholesterol, and if they had undergone any cardiovascular screening procedures (eg, ECG, stress test). This “ever screened” approach was used to capture the overall prevalence of screening among the study population. Participants were asked to rate their overall current health status using a single, direct question: “In general, would you say your health is.?” with the following response options: 1) Excellent, 2) Very good, 3) Good, 4) Fair, and 5) Poor. This subjective assessment of general health is a widely used measure in population health studies.
Pilot Testing and Validation
The electronic questionnaire underwent pilot testing in the Hail region of Saudi Arabia (a region separate from the study area) with 100 patients to assess clarity, comprehensiveness, and identify any potential difficulties. In the pilot testing, similar to the main study questionnaire, we asked participants if they had ever been screened for blood pressure, blood cholesterol, and if they had undergone any cardiovascular screening procedures. This allowed us to assess the clarity and understanding of these screening-related questions before their deployment in the main study. Based on the feedback from the pilot test, necessary modifications were made to the questionnaire. Subsequently, a focus group meeting was held with 20 key informants from Hail to further refine the questionnaire. To evaluate the test-retest reliability of the revised questionnaire, it was re-administered to the same 100 patients, yielding a reliability coefficient of 0.83. The face validity of the questionnaire was also deemed acceptable by the research team and key informants.
Justification of Independent Variables
The selection of independent variables was guided by prior literature on the predictors of cardiovascular disease risk factors and screening behaviours. Age, gender, marital status, education, and employment status are commonly reported socio-demographic factors associated with health behaviours and access to healthcare. behavioural factors such as physical activity, smoking, and fast-food consumption are established modifiable risk factors for CVD and have been shown to influence health-seeking behaviours, including screening. The inclusion of medical conditions like diabetes, obesity, hypertension, and a history of cardiovascular issues was based on their known association with increased CVD risk and the likelihood of undergoing related screenings.
Statistical Analytical Plan
First, descriptive statistics were calculated to summarize the characteristics of the study sample. For categorical variables such as gender, marital status, work status, education level, health status, history of diabetes, hypertension, cardiovascular diseases, hearing screening, and obesity, frequencies and proportions were presented. The distribution of continuous variables, including age, was assessed for normality using histograms, and measures of central tendency (mean) and dispersion (standard deviation) were reported. To explore the initial associations between individual independent variables and the three primary outcomes of interest (blood pressure screening, cholesterol screening, and cardiovascular screening), univariate logistic regression analyses were conducted. For each independent variable, the odds ratio and corresponding 95% confidence interval were calculated, and statistical significance was determined using a p-value threshold of 0.25. This step identified potential predictors for each screening outcome. Subsequently, multivariable logistic regression models were constructed to determine the independent determinants of each screening outcome among the Saudi participants. The selection of variables for inclusion in these multivariable models was guided by a combination of statistical significance observed in the univariate analyses and established scientific literature on cardiovascular disease risk factors and health-seeking behaviours. The multivariable models allowed us to estimate the adjusted odds ratios (AORs) and their 95% confidence intervals (CIs) for each independent variable, while controlling for the influence of other factors in the model. This provided a more robust understanding of the independent contribution of each predictor to the likelihood of undergoing blood pressure, cholesterol, and cardiovascular screening. We acknowledge the potential for correlation among variables such as diabetes, hypertension, and high cholesterol, recognizing that these conditions often co-occur and share underlying mechanisms. However, our decision to include them simultaneously in the multivariable logistic regression models was driven by the clinical relevance of each as an established and potentially independent risk factor for cardiovascular disease, which could uniquely influence an individual’s likelihood of undergoing screening. Furthermore, treating these interconnected variables as potential confounders is crucial for obtaining less biased estimates of other associations within our models; omitting them could obscure true relationships or lead to misleading findings. For instance, the observed association between a socio-demographic factor and screening might be confounded by the presence of hypertension or diabetes. All statistical analyses were performed using SPSS version 26.0.
Results
Sociodemographic Characteristics of Study Participants
The distribution of age in our sample (N = 14,239) was visually inspected using a histogram (Figure 1). The distribution appears approximately unimodal and somewhat symmetrical, centered around a mean of 59.77 years (Standard Deviation = 16.347). However, there is a slight positive skew, indicating a longer tail towards older ages, and a noticeable peak around the 60–65-year age range. While not perfectly normally distributed, the deviations from normality appear moderate, and given the large sample size, the assumptions of parametric statistical tests are likely reasonably met. Table 1 shows the sociodemographic characteristics of study participants in Saudi Arabia. One-third (34%) of the study participants were < 50 years old and 56.6% of the participants were females. Only 4% of the study participants had attained primary school and more than half (51.5%) reported attending a college or university. Approximately two-thirds (65.3%) were married and 48.6% were unemployed. About a quarter of the study participants (24.3%) had insurance coverage and 27.7% were smokers. About two-thirds (60.7%) reported to be physically active and 5.2% were found to be obese as shown in Table 1.
Figure 1.
Age distribution of the study population attending primary healthcare centers in Riyadh (N = 14,239).
Table 1.
Sociodemographic and Clinical Characteristics of Study Participants (n=14,239)
| Age | n | % |
| < 50 years | 4848 | 34 |
| 50 to 75 years | 6945 | 48.8 |
| At least 75 years | 2446 | 17.2 |
| Education | ||
| Primary | 572 | 4 |
| Up to High School | 3937 | 27.6 |
| College/University | 7336 | 51.5 |
| Others | 2394 | 16.8 |
| Gender | ||
| Female | 8062 | 56.6 |
| Male | 6177 | 43.4 |
| Marital status | ||
| Not married | 4939 | 34.7 |
| Married | 9300 | 65.3 |
| Employment status | ||
| Employed | 7317 | 51.4 |
| Unemployed | 6922 | 48.6 |
| Health status | ||
| Excellent | 4798 | 33.7 |
| Very good | 5076 | 35.6 |
| Good | 2815 | 19.8 |
| Fair | 1256 | 8.8 |
| Poor | 294 | 2.1 |
| Insurance coverage | ||
| Yes | 3457 | 24.3 |
| No | 10782 | 75.7 |
| Smoking | ||
| No | 10297 | 72.3 |
| Yes | 3942 | 27.7 |
| Physical activity | ||
| No | 5598 | 39.3 |
| Yes | 8641 | 60.7 |
| Obesity | ||
| No | 13502 | 94.8 |
| Yes | 737 | 5.2 |
| Blood pressure screening | ||
| No | 9207 | 64.7 |
| Yes | 5032 | 35.3 |
| Cholesterol screening | ||
| No | 12915 | 90.7 |
| Yes | 1324 | 9.3 |
| Cardiovascular screening | ||
| No | 13719 | 96.3 |
| Yes | 520 | 3.7 |
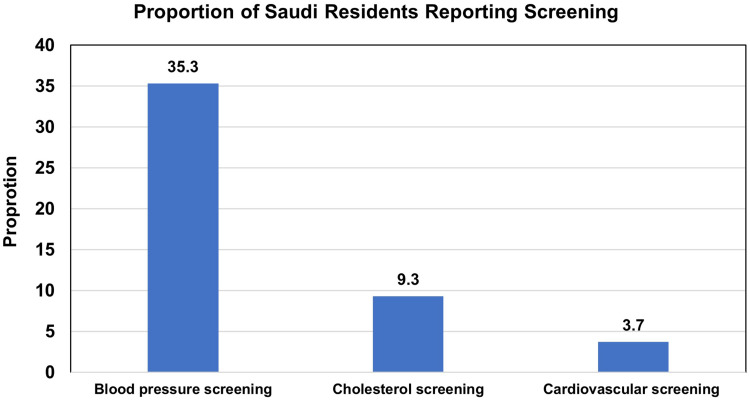
Table 1 also shows the proportion of blood pressure screening among Saudis. The data shows that only one-third of the Saudi study participants (35.3%) reported underwent screening for blood pressure as shown in Table 1. Similarly, the data shows that only 9.3% of the study participants reported undergoing cholesterol screening (Table 1 and Figure 2). The percentage of Saudis undergoing cardiovascular screening was found to be 3.7% as shown in Table 1 and Figure 2.
Figure 2.
Comparison of Blood Pressure, Cholesterol, and Cardiovascular Screening among Saudi residents.
Predictors of Blood Pressure Screening Among Saudis at Primary Healthcare Settings in Riyadh
Table 2 shows the predictors of blood pressure screening among Saudis in primary healthcare settings in Riyadh. We found that compared to younger participants of < 50 years, those who are 50 to 75 years are 1.34 times more likely to go for blood pressure screening (AOR: 1.34; 95% CI: 1.20, 1.50). Also, older participants (at least 75 years) are 2.12 times more likely to undergo blood pressure screening (AOR: 2.12; 95% CI: 1. 84, 2.43). Married Saudi residents had 1.15 times higher odds of undergoing blood pressure screening compared to unmarried residents (AOR: 1.15; 95% CI: 1.04, 1.27). Non-smokers were 1.97 times more likely to screen for blood pressure than smokers (AOR: 1.97; 95% CI: 1.79, 2.16) and physically active Saudi residents were 1.16 times more likely to opt for blood pressure screening than non-physically active (AOR: 1.16; 95% CI: 1.05, 1.28). Those who were diabetic were 2.14 times more likely to undergo high blood pressure screening than non-diabetic individuals (AOR: 2.14; 95% CI: 1.88, 2.44). However, insurance coverage and hypercholesterolemia were not found to be associated with blood pressure screening as illustrated in Table 2.
Table 2.
Predictors of Blood Pressure Screening Among Saudis at Primary Healthcare Settings in Riyadh (n=14,239)
| Predictors | 95% CI | 95% CI | ||||
|---|---|---|---|---|---|---|
| OR | LL | UL | AOR | LL | UL | |
| Age | ||||||
| < 50 years | 1 | 1 | ||||
| 50 to 75 years | 1.58 | 1.46 | 1.71 | 1.34 | 1.20 | 1.50 |
| At least 75 years | 2.56 | 2.31 | 2.83 | 2.12 | 1.84 | 2.43 |
| Education | ||||||
| Primary | 1 | 1 | ||||
| Up to High School | 0.72 | 0.60 | 0.86 | 0.94 | 0.78 | 1.14 |
| College/University | 0.73 | 0.61 | 0.86 | 0.99 | 0.82 | 1.19 |
| Gender | ||||||
| Female | 1 | NA | ||||
| Male | 1.04 | 0.97 | 1.11 | |||
| Marital status | ||||||
| Single | 1 | 1 | ||||
| Married | 1.65 | 1.53 | 1.78 | 1.15 | 1.04 | 1.27 |
| Employment status | ||||||
| Employed | 1.00 | NA | ||||
| Unemployed | 1.01 | 0.95 | 1.09 | |||
| Insurance coverage | ||||||
| No | 1 | 1 | ||||
| Yes | 1.05 | 0.97 | 1.14 | 1.07 | 0.98 | 1.18 |
| Smoking | ||||||
| Yes | 1 | |||||
| No | 1.52 | 1.40 | 1.64 | 1.97 | 1.79 | 2.17 |
| Physical activity | ||||||
| No | 1 | 1 | ||||
| Yes | 1.33 | 1.23 | 1.42 | 1.16 | 1.05 | 1.28 |
| Fast Food consumption | ||||||
| No | 1 | 1 | ||||
| Yes | 1.67 | 1.53 | 1.83 | 2.03 | 1.82 | 2.26 |
| Obesity | ||||||
| No | 1 | 1 | ||||
| Yes | 0.81 | 0.68 | 0.96 | 0.70 | 0.57 | 0.83 |
| Diabetes | ||||||
| No | 1 | 1 | ||||
| Yes | 2.38 | 2.13 | 2.67 | 2.14 | 1.88 | 2.44 |
| High cholesterol | ||||||
| No | 1 | 1 | ||||
| Yes | 1.44 | 1.27 | 1.64 | 1.09 | 0.94 | 1.27 |
Predictors of Cholesterol Screening Among Saudis at Primary Healthcare Settings in Riyadh
Table 3 shows the predictors of cholesterol screening among Saudis in primary healthcare settings in Riyadh. We found that compared to younger participants of < 50 years, those who are older participants (at least 75 years) are 1.89 times more likely to go for blood cholesterol screening (AOR: 1.89; 95% CI: 1.56, 2.29). Compared to employed Saudi residents, unemployed residents were 1.26 times more likely to go for blood cholesterol screening (AOR: 1.26; 95% CI: 1.10, 1.45). Those Saudis who had insurance coverage were 1.52 times more likely to go for blood cholesterol screening (AOR: 1.52; 95% CI: 1.33, 1.74). Smokers were 1.32 times more likely to screen for blood cholesterol than non-smokers (AOR: 1.32; 95% CI: 1.14, 1.53) History of diabetes mellitus (AOR: 1.33; 95% CI: 1.09, 1.61) and hypertension (AOR: 1.65; 95% CI: 1.36, 2.02) was found to be strongly associated with blood cholesterol screening as demonstrated in Table 3.
Table 3.
Predictors of Cholesterol Screening Among Saudis at Primary Healthcare Settings in Riyadh (n=14,239)
| Predictors | 95% CI | 95% CI | ||||
|---|---|---|---|---|---|---|
| OR | LL | UL | AOR | LL | UL | |
| Age | ||||||
| < 50 years | 1 | 1 | ||||
| 50 to 75 years | 2.04 | 1.75 | 2.37 | 1.89 | 1.56 | 2.29 |
| At least 75 years | 3.84 | 3.25 | 4.54 | 3.06 | 2.45 | 3.82 |
| Education | ||||||
| Primary | 1 | 1 | ||||
| Up to High School | 0.52 | 0.40 | 0.67 | 0.78 | 0.59 | 1.02 |
| College/University | 0.60 | 0.47 | 0.77 | 0.91 | 0.69 | 1.18 |
| Gender | ||||||
| Female | 1 | NA | ||||
| Male | 0.96 | 0.86 | 1.08 | |||
| Marital status | ||||||
| Single | 1 | 1 | ||||
| Married | 1.72 | 1.51 | 1.96 | 0.94 | 0.79 | 1.12 |
| Employment status | ||||||
| Employed | 1 | 1 | ||||
| Unemployed | 1.13 | 1.01 | 1.26 | 1.26 | 1.10 | 1.45 |
| Insurance coverage | ||||||
| No | 1 | 1 | ||||
| Yes | 1.50 | 1.33 | 1.70 | 1.52 | 1.33 | 1.74 |
| Smoking | ||||||
| No | 1 | 1 | ||||
| Yes | 1.35 | 1.20 | 1.52 | 1.32 | 1.14 | 1.53 |
| Fast food consumption | ||||||
| No | 1 | |||||
| Yes | 0.83 | 0.72 | 0.95 | 0.76 | 0.64 | 0.89 |
| Physical activity | ||||||
| No | 1 | 1 | ||||
| Yes | 1.21 | 1.07 | 1.36 | 1.10 | 0.94 | 1.29 |
| Obesity | ||||||
| No | 1 | 1 | ||||
| Yes | 1.69 | 1.37 | 2.10 | 1.06 | 0.82 | 1.36 |
| Hypertension | ||||||
| No | 1 | 1 | ||||
| Yes | 2.95 | 2.21 | 3.04 | 1.66 | 1.36 | 2.02 |
| Diabetes | ||||||
| No | 1 | 1 | ||||
| Yes | 2.29 | 1.96 | 2.68 | 1.33 | 1.09 | 1.61 |
Predictors of Cardiovascular Screening Among Saudis at Primary Healthcare Settings in Riyadh
Table 4 shows the predictors of cardiovascular screening among Saudis in primary healthcare settings in Riyadh. We found that compared to younger participants of < 50 years, those who are older participants (at least 75 years) are 1.81 times more likely to go for cardiovascular screening (AOR: 1.81; 95% CI: 1.35, 2.43). Compared to employed Saudi residents, unemployed residents were 1.53 times more likely to go for cardiovascular screening (AOR: 1.53; 95% CI: 1.24, 1.88). Those Saudis who had insurance coverage were 1.56 times more likely to go for cardiovascular screening (AOR: 1.56; 95% CI: 1.27, 1.92). Smokers were 1.89 times more likely to screen for cardiovascular than non-smokers (AOR: 1.89; 95% CI: 1.52, 2.34) Diabetes was found to be strongly associated with cardiovascular screening (AOR: 1.85; 95% CI: 1.41, 2.43). Similarly, we found high cholesterol to be a strong predictor of cardiovascular screening (AOR: 1.76; 95% CI: 1.31, 2.36) as demonstrated in Table 4.
Table 4.
Predictors of Cardiovascular Screening Among Saudis at Primary Healthcare Settings in Riyadh (n=14,239)
| Predictors | 95% CI | 95% CI | ||||
|---|---|---|---|---|---|---|
| OR | LL | UL | AOR | LL | UL | |
| Age | ||||||
| < 50 years | 1.00 | 1 | ||||
| 50 to 75 years | 1.72 | 1.36 | 2.16 | 1.81 | 1.35 | 2.43 |
| At least 75 years | 3.18 | 2.48 | 4.09 | 2.93 | 2.10 | 4.08 |
| Education | ||||||
| Primary | 1 | 1 | ||||
| Up to High School | 0.39 | 0.27 | 0.57 | 0.64 | 0.43 | 0.94 |
| College/University | 0.53 | 0.38 | 0.74 | 0.87 | 0.64 | 1.06 |
| Gender | ||||||
| Female | 1.00 | NA | ||||
| Male | 0.97 | 0.81 | 1.16 | |||
| Marital status | ||||||
| Single | 1.00 | 1 | ||||
| Married | 1.72 | 1.51 | 1.96 | 0.82 | 0.64 | 1.06 |
| Employment status | ||||||
| Employed | 1.00 | 1 | ||||
| Unemployed | 1.28 | 1.08 | 1.53 | 1.53 | 1.24 | 1.88 |
| Insurance coverage | ||||||
| No | 1.00 | 1 | ||||
| Yes | 1.84 | 1.53 | 2.21 | 1.56 | 1.27 | 1.92 |
| Smoking | ||||||
| No | 1.00 | |||||
| Yes | 2.09 | 1.75 | 2.49 | 1.89 | 1.52 | 2.34 |
| Fast food consumption | ||||||
| No | 1.00 | NA | ||||
| Yes | 0.89 | 0.72 | 1.11 | |||
| Physical activity | ||||||
| No | 1.00 | 1 | ||||
| Yes | 1.48 | 1.22 | 1.79 | 1.10 | 0.87 | 1.38 |
| Obesity | ||||||
| No | 1.00 | 1 | ||||
| Yes | 2.41 | 1.82 | 3.20 | 1.15 | 0.82 | 1.61 |
| Diabetes | ||||||
| No | 1.00 | 1 | ||||
| Yes | 3.34 | 2.69 | 4.13 | 1.85 | 1.41 | 2.43 |
| Hypertension | ||||||
| No | 1.00 | 1 | ||||
| Yes | 3.14 | 2.51 | 3.92 | 1.19 | 0.87 | 1.63 |
| High blood cholesterol | ||||||
| No | 1.00 | 1 | ||||
| Yes | 3.55 | 2.84 | 4.44 | 1.76 | 1.32 | 2.36 |
Abbreviations: OR, Odds ratio; AOR, Adjusted Odds ratio; CI, confidence interval.
Discussion
This study was undertaken to estimate the proportion of Saudi residents who underwent blood pressure, blood cholesterol, and cardiovascular screening. We also measured the predictors of blood pressure, blood cholesterol, and cardiovascular screening. Overall, we found that a very small proportion of Saudi residents opted for the above-mentioned three types of screening. The most important cross-cutting predictors included older age, insurance coverage, physical activity, and history of diabetes hypertension, or hypercholesterolemia.
The low prevalence of screening for these risk factors of cardiovascular diseases is not aligned with other studies mainly undertaken in Western countries. For example, a study by Robbins et al, 2011 found that blood pressure and cholesterol screening was received by about 90% and 63.3% of the women in the USA, a very high screening prevalence compared to our study.14 Similarly, another study in the USA reported that about 50 to 70% of women reported underwent screening for blood cholesterol.15 Likewise, one more study from Spain reported that 46 and 34%, respectively, of the individuals from the general population did not undergo screening for cholesterol and blood pressure.16 These variations may reflect differences in the healthcare systems and guidelines available in the two countries. Unlike the health system in Saudi Arabia, the USA Preventive Task Force has made recommendations to screen for modifiable risk factors of cardiovascular diseases. In addition, there is consistency in the recommendations for blood pressure screening across the national USA guidelines.17–19
Moreover, we found differences in the proportion of screening for blood pressure, cholesterol, and cardiovascular diseases among the Saudi population. More specifically, about one-third of Saudi residents underwent screening for blood pressure, however, fewer than 10% underwent screening for blood cholesterol and cardiovascular diseases. This pattern of differences in the screening for various parameters is consistent with Robbins et al, 2011 where authors found that a greater proportion of women underwent blood pressure screening compared to cholesterol screening.14 The higher proportion of blood pressure screening with consistent findings across the regions may be due to the non-invasive procedure (no blood draw) required for screening its availability outside medical infrastructure and very low cost because it does not include additional laboratory expenditure. By contrast, cholesterol and cardiovascular screening are not routine in most healthcare settings. Additional barriers include fasting for 12 hours and blood sample collection to draw blood along with the cost associated with the laboratory. Moreover, unlike blood pressure screening, there are no consistent guidelines to screen high blood cholesterol, which may partly explain the lower rates of blood cholesterol screening compared to blood pressure screening.18,20,21
Additionally, the observed low screening rates in our study likely reflect specific characteristics of the Saudi Arabian healthcare system and prevailing cultural factors. The historical structure of the healthcare system, with its evolving integration of primary care and specialized services, might present challenges in ensuring consistent and proactive screening protocols across all settings. Furthermore, cultural norms around health-seeking behaviour, perceptions of preventative care, and the level of awareness regarding cardiovascular risk factors and the benefits of early screening within the Saudi population could significantly influence the uptake of these essential measures. Future research should explore these systemic and cultural nuances to develop more tailored and effective strategies for improving cardiovascular screening rates in Saudi Arabia.
Regarding the predictors, the current study found that insurance coverage is an important positive predictor of screening for hypertension, high cholesterol, and cardiovascular diseases. This finding is consistent with the study by Robbins et al, 2011 where the authors found that those without insurance were found to have the lowest percentage of blood pressure and cholesterol screening than those who had insurance.14 Health insurance coverage may be an indicator of the socioeconomic status of the individuals and those who had insurance coverage may have access and resources to take benefits from the screening programs. Besides, insured individuals may be likely to even go for regular health checkups. These findings are further supported by the literature where researchers have found that screening for cardiovascular risk factors is less common among individuals with low socio-economic status as measured by income, occupation, education, or health insurance coverage.22–25 However, the same study by Robbins et al, 2011 found a suboptimal screening among those who were hypertensive or pre-diabetic.14 This contrasts with the findings from our study where it was found that diabetic and hypertensive individuals were more likely to go for screening than their counterparts. These differences may reflect variations in sociodemographic backgrounds and behaviour of the residents living in two different geographic areas. Moreover, unlike the current study, the study by Robbins et al, 2011 was conducted only among females, which may in part, explain the differences in the findings between the two studies. We also found that older age was positively associated with the screening for blood pressure, blood cholesterol, and cardiovascular diseases. This finding coincided with the study conducted in Spain and this consistent finding may be explained by the fact that age may be a proxy for the need for screening.16
The findings of our study revealed that non-smokers were more likely to undergo blood pressure screening, whereas smokers were more likely to undergo screening for cholesterol and CVD. Non-smokers might be more health-conscious overall and proactively seek blood pressure checks as a general preventive measure. Conversely, smokers, potentially experiencing or being aware of smoking-related health concerns and often having more frequent interactions with the healthcare system for smoking-related advice or other conditions, might be more likely to undergo cholesterol and broader CVD screening as part of a more comprehensive risk assessment prompted by their smoking status. Similarly, married individuals might benefit from spousal encouragement and shared health behaviours, potentially increasing their likelihood of routine blood pressure screening, while the influence of marital status on the more specific triggers for cholesterol or CVD screening might be less direct and mediated by other factors like age or existing comorbidities. However, these differences need to be further explored in future studies.
Strengths and Limitations
This current cross-sectional study provides valuable insights into the proportion and predictors of two important modifiable risk factors of cardiovascular disease including blood pressure and high cholesterol screening along with the screening of cardiovascular disease. We used a validated and reliable study questionnaire to collect data, and the questionnaire was also pilot tested in a different community before the actual administration of the questionnaire. The findings could guide policymakers and clinicians to devise strategies for introducing screening programs in Saudi Arabia. Besides, we also identified predictors of blood pressure and blood cholesterol screening that may guide policymakers to understand why people with specific characteristics are more likely to undergo screening than others. This could facilitate targeted screening programs by improving access to those who are less likely to undergo screening than others.
However, these findings should be interpreted in the light of some limitations. First, as this was a cross-sectional study, the temporal relationship between predictors and screening behaviours could not be determined. Hence, more longitudinal epidemiological studies are needed in the future to assess the causal relationships between sociodemographic risk factors and various types of screening. Such studies could provide insights into how screening levels change in relation to evolving risk factors and life circumstances. Our cross-sectional study provides a valuable baseline assessment of screening prevalence and associated factors at a specific point in time, and longitudinal research would build upon these findings to offer a more dynamic understanding. Secondly, our study’s reliance on self-reported data for screening history and risk factors introduces the potential for both recall and social desirability biases, which could have influenced our findings. Participants’ difficulty in accurately recalling past screening experiences might have led to either under- or overestimation of actual screening rates. Furthermore, the tendency to present oneself favorably could have resulted in the overreporting of healthy behaviours and screening engagement, potentially inflating the estimated prevalence of cardiovascular screening and the strength of its associated predictors. Additionally, the potential underestimation of obesity prevalence due to the reliance on self-reported weight and height data, susceptible to reporting biases, represents another limitation of our reliance on self-reported information. Third, we did not check the physician’s confirmation or any objective method to confirm the diagnosis of hypertension, hypercholesterolemia, and diabetes mellitus. Another limitation of our study is that participants were recruited from primary healthcare attendees in Riyadh. This may introduce selection bias, as individuals who do not regularly access primary care services might have different screening behaviours and risk factor profiles, potentially limiting the generalizability of our findings to the broader Saudi population. Lastly, we recruited participants from primary healthcare centers within the Riyadh region. Therefore, the results regarding screening prevalence and its predictors may not be fully generalizable to the entire Saudi population, including those who do not regularly utilize primary healthcare facilities or those residing in other regions of the Kingdom. Future research could benefit from broader, population-based sampling strategies to provide a more comprehensive understanding of cardiovascular screening practices across Saudi Arabia.
Conclusion
Overall, our findings reveal a concerningly low uptake of critical cardiovascular disease risk factor screening among primary healthcare attendees in Riyadh, with less than 36% reporting blood pressure screening and less than 10% undergoing cholesterol and cardiovascular screening. Shared predictors of screening across these outcomes included older age, insurance coverage, a history of diabetes or hypertension, physical activity, and high cholesterol levels. This minimal proportion of residents undergoing these essential screenings highlights an urgent need for the Saudi Government to implement targeted measures and strategies to significantly increase screening rates for blood pressure, cholesterol, and cardiovascular diseases. To achieve this, the government could prioritize the seamless integration of these risk assessments into routine primary healthcare visits for eligible individuals, normalizing screening and improving accessibility. Furthermore, implementing targeted subsidies or reducing cost barriers for cholesterol testing and other relevant screenings could significantly improve uptake, particularly among vulnerable populations, ultimately facilitating early detection of modifiable risk factors and reducing the burden of cardiovascular disease. Future research should evaluate the effectiveness of specific interventions aimed at increasing screening uptake within primary healthcare settings and the broader community in Saudi Arabia.
Acknowledgments
Authors are deeply thankful for the Riyadh cluster 2 (King Fahad medical city) for their approval and help in conducting this study.
Funding Statement
There is no funding to report.
Ethics Approval and Consent to Participate
The ethical approval for the current study was taken from the Institutional Review Board of King Fahad medical city (approval # 22-397E). Riyadh Second Health Cluster, Riyadh, Saudi Arabia, is a part of King Fahad Medical City, the main headquarter. The written informed consent to participate were taken from all participants before the data collection process. This study was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Benjamin EJ, Muntner P, Alonso A, et al. Heart disease and stroke statistics-2019 update: a report from the American heart association. Circulation. 2019;139(10):e56–e528. doi: 10.1161/cir.0000000000000659 [DOI] [PubMed] [Google Scholar]
- 2.Patel SA, Winkel M, Ali MK, et al. Cardiovascular mortality associated with 5 leading risk factors: national and state preventable fractions estimated from survey data. Ann Intern Med. 2015;163(4):245–253. doi: 10.7326/m14-1753 [DOI] [PubMed] [Google Scholar]
- 3.Bhatnagar P, Wickramasinghe K, Williams J, et al. The epidemiology of cardiovascular disease in the UK 2014. Heart. 2015;101(15):1182–1189. doi: 10.1136/heartjnl-2015-307516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Joffres M, Falaschetti E, Gillespie C, et al. Hypertension prevalence, awareness, treatment and control in national surveys from England, the USA and Canada, and correlation with stroke and ischaemic heart disease mortality: a cross-sectional study. BMJ Open. 2013;3(8):e003423. doi: 10.1136/bmjopen-2013-003423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Institute for Health and Care Excellence (NICE). Cardiovascular disease: risk assessment and reduction, including lipid modification [CG181]. 2014. Available from: https://www.nice.org.uk/guidance/cg181. Accessed August 8, 2024.
- 6.National Institute for Health and Care Excellence (NICE). Cardiovascular disease: risk assessment and reduction. [CG127]. 2010. Available from: https://www.nice.org.uk/guidance/cg127. Accessed April 1, 2025.
- 7.Life Line Screening. High cholesterol screening. Available from: http://www.lifelinescreening.co.uk/health-screening-services/heart-disease/high-cholesterol.aspx. Accessed April 2, 2025.
- 8.NHS UK. Cholesterol diagnosis. Available from: http://www.nhs.uk/Conditions/Cholesterol/Pages/Diagnosis.aspx. Accessed April 2, 2025.
- 9.Blood pressure UK. blood pressure checks. Available from: http://www.bloodpressureuk.org/microsites/u40/Home/checks. Accessed January 8, 2025.
- 10.Dehmer SP, Maciosek MV, LaFrance AB, et al. Health benefits and cost-effectiveness of asymptomatic screening for hypertension and high cholesterol and aspirin counseling for primary prevention. Ann Fam Med. 2017;15(1):23–36. doi: 10.1370/afm.2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alqunaibet A, Herbst CH, El Saharty S, et al. Noncommunicable Diseases in Saudi Arabia: Toward Effective Interventions for Prevention. Washington, DC: World Bank; 2021. [Google Scholar]
- 12.Hazazi A, Wilson A. Noncommunicable diseases and health system responses in Saudi Arabia: focus on policies and strategies. A qualitative study. Health Res Policy Syst. 2022;20(1):63. doi: 10.1186/s12961-022-00872-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization (WHO). NCD progress monitor 2020. Available from: https://www.who.int/publications/i/item/ncd-progress-monitor-2020. Accessed December 8, 2025.
- 14.Robbins CL, Dietz PM, Bombard JM, et al. Blood pressure and cholesterol screening prevalence among U.S. women of reproductive age: opportunities to improve screening. Am J Prev Med. 2011;41(6):588–595. doi: 10.1016/j.amepre.2011.08.010 [DOI] [PubMed] [Google Scholar]
- 15.Kuklina EV, Yoon PW, Keenan NL. Prevalence of coronary heart disease risk factors and screening for high cholesterol levels among young adults, United States, 1999–2006. Ann Fam Med. 2010;8(4):327–333. doi: 10.1370/afm.1137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rodríguez-Artalejo F, Díez-Gañán L, Artiñano AB, et al. Effectiveness and equity of serum cholesterol and blood pressure testing: a population-based study in Spain. Prev Med. 2003;37(2):82–91. doi: 10.1016/S0091-7435(03)00086-0 [DOI] [PubMed] [Google Scholar]
- 17.Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2571. doi: 10.1161/01.HYP.0000107251.49515.c2 [DOI] [PubMed] [Google Scholar]
- 18.American College of Obstetricians and Gynecologists (ACOG). ACOG committee opinion. primary and preventive care: periodic assessments. Obstet Gynecol. 2003;102(5):1117–1124. doi: 10.1016/j.obstetgynecol.2003.09.033 [DOI] [PubMed] [Google Scholar]
- 19.U.S. Preventive Services Task Force. Screening for high blood pressure. Prev Med. 2003;25(2):159–164. [Google Scholar]
- 20.Bibbins-Domingo K, Grossman DC, Curry SJ, et al. Screening for lipid disorders in children and adolescents: US preventive services task force recommendation statement. JAMA. 2016;316(6):625–633. doi: 10.1001/jama.2016.9852 [DOI] [PubMed] [Google Scholar]
- 21.Robbins CL, Dietz PM, Bombard J, et al. Lifestyle interventions for hypertension and dyslipidemia among women of reproductive age. Prev Chronic Dis. 2011;8(4):A77. [PMC free article] [PubMed] [Google Scholar]
- 22.Broyles RW, Narine L, Brandt EN, et al. Health risks, ability to pay, and the use of primary care: is the distribution of service effective and equitable? Prev Med. 2000;30(6):453–462. doi: 10.1006/pmed.2000.0672 [DOI] [PubMed] [Google Scholar]
- 23.Solberg LI, Brekke ML, Kottke TE. Are physicians less likely to recommend preventive services to low-SES patients? Prev Med. 1997;26(3):350–357. doi: 10.1006/pmed.1997.0150 [DOI] [PubMed] [Google Scholar]
- 24.Carrasquillo O, Lantigua RA, Shea S. Preventive services among medicare beneficiaries with supplemental coverage versus HMO enrollees, Medicaid recipients, and elders with no additional coverage. Med Care. 2001;39(6):616–626. doi: 10.1097/00005650-200106000-00009 [DOI] [PubMed] [Google Scholar]
- 25.Ayanian JZ, Weissman JS, Schneider EC, et al. Unmet health needs of uninsured adults in the United States. JAMA. 2000;284(16):2061–2069. doi: 10.1001/jama.284.16.2061 [DOI] [PubMed] [Google Scholar]