Abstract
Background
Elimination of mother-to-child transmission of HIV is achievable through prevention of mother-to-child transmission (PMTCT) interventions. For HIV-positive mothers to access PMTCT services, they must be identified through HIV testing and counseling. We sought to measure the proportion of mothers with unknown HIV status and to determine associated factors.
Methods
We recruited into a cross-sectional study 400 mothers accompanying their infants for routine immunization at mother-child health clinic (MCH) at Machakos Hospital, Kenya, collected information on HIV testing from their antenatal records, and offered opt-out HIV testing to those with unknown HIV status.
Results
Overall, 304 (76.0%) mothers had unknown status at MCH, of whom 25 (8.6%) tested HIV-positive. HIV positivity was three times higher among mothers who never tested during pregnancy/delivery versus those whose last negative HIV test was >3 months prior to study enrolment (18% versus 6%). Women living more than three kilometers away from the health facility had 2.7-fold greater odds of having unknown status compared to those who lived less than three kilometers (adjusted odds ratio [AOR] 2.7, 95% CI 1.3–5.6). Married women had 3.2-fold greater odds of having unknown status as compared to those who were single (AOR 3.2, 95% CI 1.4–7.0). Those with education had a tenfold reduction in odds of having unknown status compared to those with none (AOR 0.1, 95% CI 0.0–0.2).
Conclusion
Interventions are needed to improve women’s ANC attendance, uptake of HIV testing, and disclosure of HIV status during pregnancy to achieve the elimination of MTCT.
Keywords: HIV, PMTCT, Unknown HIV status, MCH
INTRODUCTION
Mother-to-child transmission of HIV accounts for 90% of infections in children (Joint United Nations Programme on HIV/AIDS (UNAIDS), 2012). In 2017, there were 180,000 children who acquired HIV infection, 90% of whom live in sub-Saharan Africa. In the same year, Kenya was one of 22 priority countries that had the highest burden of HIV-positive pregnant women in need of prevention of mother-to-child transmission. In Kenya it was estimated that 8,000 children became newly infected with HIV in 2017 (Joint United Nations Programme on HIV/AIDS (UNAIDS), 2017, 2018; Sirengo et al., 2015).
Kenya is implementing the UNAIDS strategy aimed at eliminating mother-to-child transmission of HIV, which is defined as achieving a rate of HIV transmission below 5% among infants born to HIV-positive mothers (UNAIDS, 2015). This reduction will be accomplished through several interventions, including screening of women for HIV infection during pregnancy, delivery and postnatal care; initiating highly active antiretroviral therapy (HAART) for all HIV-positive pregnant and lactating mothers; and maintaining these mothers on treatment for life.
HIV-infected pregnant and lactating women need to learn their HIV-positive status in order to access PMTCT interventions. The World Health Organization (WHO) recommends that pregnant mothers be tested at their first antenatal care (ANC) visit and those with HIV-negative results be retested three months later. All women not previously diagnosed with HIV should be retested at delivery. Breastfeeding mothers with unknown HIV status are also tested (WHO, 2015). Targeting HIV testing for PMTCT during the antenatal period in Kenya should be an effective way to diagnose HIV-positive pregnant women because 96% of all pregnant women attend at least one ANC visit, and the proportion of pregnant women who accept HIV testing and counseling services during ANC is also high, at 94% (Kenya National Bureau of Statistics (KNBS), 2014; National AIDS and STI Control Programme (NASCOP), 2012b). However, the remaining 4% of women who do not attend ANC during their pregnancy and 6% of ANC attendees who do not accept HIV testing and counseling during pregnancy represent a group of women with missed opportunities for PMTCT, if they are HIV-infected. Pregnant and breastfeeding women are also at increased risk of HIV infection and of transmitting the virus to their children due to high viral load, hence the importance of retesting women who test HIV-negative at regular intervals during pregnancy and breastfeeding.
The mother-to-child transmission rate in Kenya was high in 2018 at 11.5% (National AIDS Control Council (NACC), 2018b, 2018a), despite adopting and implementing the WHO guidelines since 2012 (NASCOP, 2012a). Identifying factors that impede access to PMTCT services among HIV-positive women is an important step towards implementing appropriate interventions and eliminating mother-to-child transmission of HIV. Although studies have assessed HIV testing practices during the perinatal and maternity period, it is not known how many HIV-positive mothers have unknown HIV status when they present at MCH for their infants’ immunization visits. Therefore, we sought to estimate the proportion of mothers with unknown HIV status presenting for routine infant vaccination. We also sought to identify the time points where the opportunity to test was missed and to identify factors associated with unknown HIV status.
METHODS
Study setting
In 2017, Machakos County, Kenya, had an estimated population of 1.2 million and a HIV prevalence rate of 3.8%. During the same period, it was estimated that 1000 people were infected annually, 18.5% of whom were children (NACC, 2018b). According to the Machakos County HIV profile, only half of all pregnant women attended the recommended four ANC visits, and 31.9% of all HIV-positive pregnant women delivered in a hospital in the same county (National AIDS Control Council (NACC), 2016).
Study design
We conducted a facility-based cross-sectional study in Machakos County Referral Hospital MCH services from July 2014 to January 2015. The first dose of pentavalent vaccine is usually given to infants at six weeks of age. If an infant is born outside a health facility, they should be taken to a health facility to receive the birth oral polio vaccine. All mothers accompanying their infants for either the first dose of pentavalent vaccine or birth oral polio vaccine were eligible and recruited consecutively into the study. After obtaining written consent from participants, we conducted face-to-face interviews using a structured questionnaire to collect self-reported information on the mother’s obstetric history, access to antenatal services and delivery. HIV testing history for antenatal and labor and delivery was abstracted from the ANC mother-baby booklet. The interview was conducted by a clinical officer working in Machakos Hospital who was trained by the investigator. Quality was assured through supervision and record review by the investigator.
The PMTCT Cascade
The PMTCT cascade begins at pregnancy, where all pregnant women with unknown HIV status should be offered opt-out testing at the first ANC visit, and a repeat HIV test (after 3 months) in the third trimester should be offered to all women. Women who decline HIV testing at the first antenatal visit should be offered HIV testing again in subsequent visits. Women presenting in labor without documented HIV testing should have opt-out testing done urgently. HIV counseling and testing should be offered to all women with unknown HIV status at each postnatal visit. For HIV-negative mothers not screened previously during the post-natal period, screening at first child immunization is also recommended. If a woman is diagnosed with HIV at any of these stages then she is linked to HIV care and initiated on ART (National AIDS and STI Control Programme (NASCOP), 2012a).
Measures
We defined an opportunity for HIV testing as occurring at each point in a woman’s pregnancy when she should have been tested for HIV as per national guidelines (National AIDS and STI Control Programme (NASCOP), 2012a). Women were considered to have a known HIV status if they had medical record documentation of HIV-positive status prior to their first ANC visit, were newly-diagnosed with HIV infection during their ANC visits or during delivery, or had HIV-negative status based on tests conducted within three months prior to enrolment in the study. Mothers with unknown HIV status were defined as those women who did not know their HIV status because they self-reported that they had never been tested for HIV or had their last HIV-negative test more than three months prior to enrolment in the study. The time from HIV test was computed as the difference between the recorded date of the last HIV test and date of enrolment into the study.
Sampling procedures
At the time of the survey, 46% of adults in Machakos County had never been tested for HIV. A minimum sample size of 381 mothers was chosen to achieve a 95% confidence interval of +/− 5% for the proportion of women never tested for HIV (46%, based on estimated proportion of adults never tested for HIV in Machakos County). Mothers were enrolled consecutively until the desired sample size was achieved.
Laboratory methods
Service providers who routinely offer HIV testing at MCH conducted HIV testing and counseling for all women enrolled in the study who had either never been tested or had a HIV test more than three months prior to enrolment; testing was offered on an opt-out basis. Rapid HIV testing followed national guidelines and was conducted using the Determine test kit as the screening assay (Abbott Diagnostics, Abbott Park, IL). If the screening assay was reactive, a confirmation test was performed using the Unigold test kit (Trinity Biotech PLC, Ireland). A blood specimen was classified as HIV-positive when it was reactive on both the screening and confirmatory assays. A blood specimen was classified as HIV-negative if non-reactive on the screening assay. For specimens with discrepant screening and confirmatory test results, dry blood spots were collected for confirmatory testing by polymerase chain reaction (PCR). As required in Kenya’s national HIV testing guidelines, we provided pre-test and post-test counseling for all clients, and those who tested HIV-positive were linked to HIV care and HIV-exposed infant follow-up services (Ministry of Health National AIDS and STI Control Program, 2013).
Data analysis
We described study participants by age, marital status, level of education, total number of children, occupation, and distance of residence from health facility. Bivariate analysis compared demographic and clinical characteristics of enrolled women with unknown HIV status to those who knew their HIV status. Variables that were found to be significant (p<0.25) in bivariate analysis or considered to be potential confounders were included in a stepwise logistic regression model to identify independent factors associated with missed opportunity. Variables that remained significant (p<0.05) in the model were considered to be statistically significant. All statistical analyses were performed using STATA version 13 (StataCorp, Texas).
Ethical considerations
The respondents provided written informed consent for study procedures prior to enrolment in the study. The study protocol was reviewed and approved by Kenyatta National Hospital Institutional Review Board in Nairobi, Kenya. Institutional approval for the study was granted by the Machakos County Referral Hospital administration.
RESULTS
A total of 400 mothers were enrolled in the study. No mother refused to participate in the study. Half of mothers were aged below 25 years and 77% were married (Table 1). Seventy-six percent of all mothers had an unknown HIV status at MCH, 19% knew their HIV status, 5% declined to disclose their HIV status. Eighty percent of the mothers with unknown status were in the category because they had their last HIV test more than three months prior to the study, while the remaining 20% had not been tested through the cascade of PMTCT.
Table 1:
Socio – demographics (baseline) characteristics of mothers accompanying infants for immunization at MCH in Machakos County Referral Hospital, Kenya, 2014
| Select variables | All mothers (N400) | Mothers with unknown HIV status (N=304) |
|---|---|---|
| Age (years) | n (%) | n (%) |
| 15–19 | 53 (13.3) | 37 (12.2) |
| 20–24 | 157 (39.3) | 120 (39.5) |
| 25–29 | 90 (22.5) | 72 (23.7) |
| 30 and above | 100 (25) | 75 (24.7) |
| Marital Status | ||
| Single | 90 (22.5) | 89 (23.4) |
| Married | 310 (77.5) | 291 (76.6) |
| Level of Education | ||
| No school | 18 (4.5) | 5 (1.6) |
| Primary school | 154 (38.5) | 115 (37.8) |
| Secondary | 137 (34.3) | 118 (38.8) |
| College/University | 91 (22.8) | 66 (21.7) |
| Occupation | ||
| Housewife/No employment | 217 (54.3) | 158 (52.0) |
| Self-employed/Casual | 65 (16.3) | 50 (16.5) |
| Formal | 62 (15.5) | 53 (17.4) |
| Student | 36 (9) | 33 (10.9) |
| Self-employed/Formal | 20 (5) | 10 (3.3) |
| Distance from health facility | ||
| 1km | 55 (13.8) | 50 (16.5) |
| 2km | 51 (12.8) | 42 (13.8) |
| 3km | 68 (17) | 53 (17.4) |
| 4km | 50 (12.5) | 30 (9.9) |
| More than 5 km | 176 (44.0) | 129 (42.3) |
| No of children | ||
| 1 | 209 (52.3) | 159 (52.3) |
| 2 | 92 (23) | 72 (23.7) |
| 3 | 53 (13.3) | 35 (11.5) |
| >3 | 46 (11.5) | 38 (12.5) |
| HIV status at the time of infant immunization * | ||
| HIV-positive | 14 (14.5) | N/A |
| HIV-negative | 62 (64.6) | N/A |
| Missing¶ | 20 (20.8) | N/A |
Refers to HIV status just prior to study enrolment.
Women who had never previously tested for HIV or whose last HIV-negative test was > 3 months prior.
Women who refused to disclose their HIV status at time of study enrolment
When retesting was done, 5.8% of the mothers without a recent HIV test had an HIV-positive result, while 17.8% of the mothers who had been missed tested HIV-positive (Figure 1).
Figure 1.
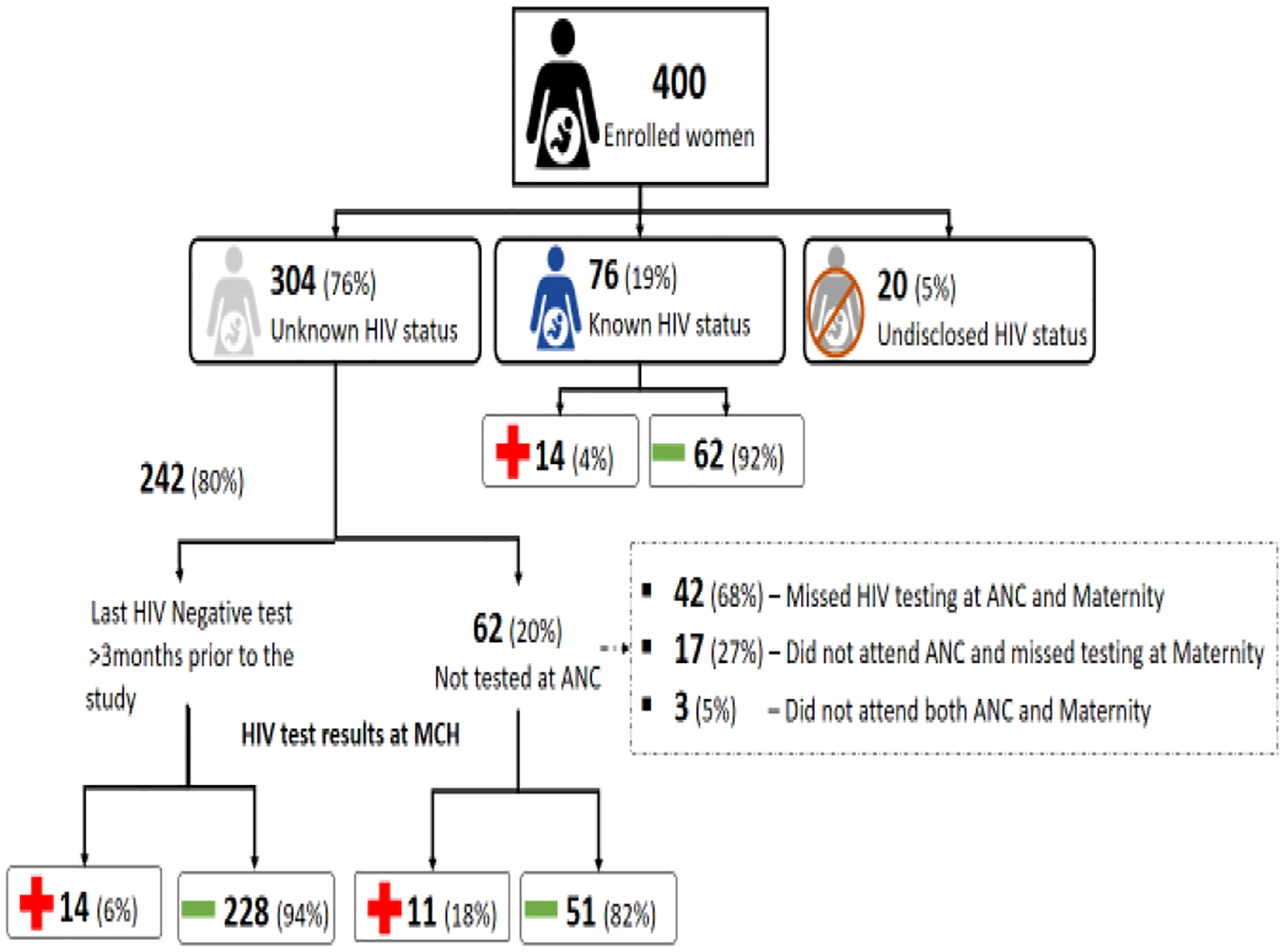
HIV status at enrolment and after testing at MCH among women attending routine child immunization visits, Machakos County Referral Hospital, Kenya, 2014 (n=400)
In total, there were 62 (15.5%) mothers who missed HIV testing at every point during their ANC or maternity care. Two thirds of these mothers were missed either at ANC or maternity while 27% did not attend ANC but were missed at maternity (Figure 1). In the bivariate analysis, among the 304 mothers who had an unknown HIV status at time of infant immunization, 129 (42.4%) were older than 25 years, 299 (98.4%) had at least primary school education, 231 (76.0%) had fewer than 2 children, 159 (52.3%) were living more than 3 kilometers away from the health facility, and 292 (96.0%) had made at least one ANC visit.
In unadjusted analysis, having unknown HIV status was associated with being married, no education and living a long distance from the health facility (Table 2). After adjusting for potential confounders, women who lived more than three kilometers away from the health facility had 2.7 greater odds of having unknown status compared to those who lived less than three kilometers away (AOR 2.7, 95% CI 1.3–5.6). Women who were married had 3.2 greater odds of having unknown status as compared to those who were single (AOR 3.2, 95% CI 1.4–7.0). Finally, women who were educated had a ten-fold reduction in odds of having unknown status compared to those with no education (AOR 0.1, 95% CI 0.0–0.2).
Table 2.
Factors associated with unknown HIV status among women accompanying their infants for immunization at MCH services in Machakos County Referral Hospital, Kenya, 2014
| Select variables | All (N = 380)* | Unknown HIV status (N=304) | Known HIV status (N=76) | Unadjusted | Adjusted |
|---|---|---|---|---|---|
| Age | n (%) | n (%) | n (%) | OR (95% CI) | OR (95% CI) |
| ≥25 years | 213 (47.1) | 175 (57.6) | 38 (50.0) | 1 | |
| <25 years | 167 (52.9) | 129 (42.4) | 38 (50.0) | 1.3 (0.8–2.2) | |
| Marital Status | |||||
| Living Alone | 89 (23.4) | 79 (26.0) | 10 (13.2) | 1 | |
| Living with a Partner | 291 (76.6) | 225 (74.0) | 66 (86.8) | 2.31 (1.3–4.7) | 3.2 (1.4–7.0) |
| Level of Education | |||||
| No education | 17 (4.5) | 5 (1.6) | 12 (15.8) | 1 | |
| Educated | 363 (95.5) | 299 (98.4) | 64 (84.2) | 0.1 (0.0–0.3) | 0.1 (0.0–0.2) |
| Occupation | |||||
| Employed | 141 (37.1) | 113 (37.2) | 28 (36.8) | 1 | |
| Unemployed | 239 (62.9) | 191 (62.8) | 48 (63.2) | 1.0 (0.6–1.7) | |
| Distance from health facility | |||||
| Less than 3 KM | 167 (43.9) | 145 (47.7) | 22 (28.9) | 1 | |
| Above 3 KM | 213 (56.1) | 159 (52.3) | 54 (71.1) | 2.2 (1.3–3.8) | 2.7 (1.3–5.6) |
| No of children | |||||
| More than 2 | 94 (24.7) | 73 (24.0) | 21 (27.6) | 1 | |
| Fewer than 2 | 286 (75.3) | 231 (76.0) | 55 (72.4) | 0.8 (0.5–1.5) | |
| ANC Visits | |||||
| None | 19 (5) | 12 (4.0) | 7 (9.2) | 1 | |
| At least one visit | 361 (95) | 292 (96.0) | 69 (90.8) | 0.4 (0.2–1.1) |
20 women who refused to disclose their HIV status are excluded
DISCUSSION
Although PMTCT interventions have been shown to significantly reduce transmission of HIV to infants, benefits take effect only once the mother has been diagnosed with HIV infection and receives treatment. We found that three quarters of the mothers attending MCH clinic in Machakos Hospital had an unknown HIV status and therefore were eligible for HIV testing. One in five of those mothers with unknown HIV status in MCH had missed an opportunity for HIV testing at every point in the PMTCT cascade, either because they did not attend ANC and maternity, or they were not tested for HIV at either ANC or maternity. This could be an indication of inconsistent implementation of testing guidelines in PMTCT (Rogers et al., 2016). A similar study conducted in South Africa found that a third of mothers missed at least one step in the PMTCT cascade (Woldesenbet et al., 2015).
Eight percent of the mothers in MCH with unknown HIV status and eligible for HIV testing at vaccination tested HIV-positive. HIV positivity among those mothers who had a HIV test greater than three months prior was 6% while it tripled for those who had been missed completely through the cascade. This is similar to the findings in a study conducted in western Kenya that found that pregnant women who had never attended ANC were about 6 times more likely to newly test HIV-positive compared to those who had attended ANC (Ndege, Washington, Kaaria, & Meara, 2016). Although acceptance for HIV testing is high in Kenya, failure to attend ANC remains a barrier to accessing PMTCT services (Delva et al., 2010).
Of the HIV-positive women who were enrolled in our study, 44% were diagnosed at the time of routine infant vaccination. We cannot rule out that some of these women might have already known that they were HIV-infected but did not disclose their HIV status during ANC or maternity care visits in health facilities. Failure to disclose HIV status has been found to be higher among HIV-infected mothers and has been associated with poor use of PMTCT services (Kinuthia et al., 2018; Spangler, Onono, Bukusi, Cohen, & Turan, 2014). Irrespective of reason, the unavailability of HIV status among these HIV-infected mothers in a clinical setting prevents access to PMTCT interventions to reduce the risk of perinatal transmission to their babies. Decreasing stigma and enhancing health education opportunities for pregnant women may help improve disclosure. Antenatal and maternity care is often one of the busiest sectors of the health facility, resulting in short consultations with minimum time available for counseling. These insights provide useful suggestions for improving interventions targeted at eliminating MTCT.
The study found that living more than three kilometers away from a health facility was associated with unknown HIV status, and may relate to ease of access to HIV testing and counseling. Distance has been shown to hinder access to various health services in the region (Asweto, Aluoch, Obonyo, & Ouma, 2014; Golub, Herman-roloff, Hoffman, Jaoko, & Bailey, 2017; Hanson et al., 2015). Addressing the issue of access to a health facility by bringing services closer to the community may help bridge the gaps. Kenya has introduced mobile clinics to address this issue. In contrast to a similar study conducted in Kampala (Namara-Lugolobi EC et al, 2015), our study did not find significant associations between unknown HIV status with age and marital status.
LIMITATIONS
Some of the information collected from mothers was self-reported and vulnerable to recall and social desirability bias. Associations with unknown HIV status were limited to a small number of demographic and clinical variables collected and the relatively small sample size. These findings cannot be generalized beyond the population of pregnant women that attend ANC, maternity, or MCH in Machakos County.
CONCLUSION
We identified a number of HIV-infected mothers who had unknown HIV status at the time of infant vaccination. Maternal child health clinics provide an important avenue for identifying mothers who were missed and linking them and their babies to appropriate care. With adoption of highly active antiretroviral therapy for life, innovative testing and counseling methods need to be used to encourage mothers to test for HIV infection or disclose prior knowledge of HIV-positive status in order to benefit from PMTCT interventions. Community and peer-based interventions can also improve uptake of testing and disclosure.
Interventions to improve ANC attendance, uptake of HIV testing services across the PMTCT cascade, and disclosure of HIV status during pregnancy should be used to optimize PMTCT outcomes in order to accelerate the attainment of the ambitious UNAIDS 90-90-90 goals where we aim to identify 90% of all people living with HIV, put on treatment 90% of those, and achieve viral suppression. These efforts will accelerate elimination of mother-to-child transmission of HIV.
ACKNOWLEDGEMENTS
The authors would like to thank the respondents from Machakos Hospital who participated in the study and Thomas Muthusi, the clinical officer/ HIV counsellor in Machakos Hospital, for providing the services to the mothers. We also wish to acknowledge the technical support from Alfred Musekiwa and Dorothy Southern.
Footnotes
COMPETING INTERESTS
The authors declare that they have no competing interests.
REFERENCES
- Asweto CO, Aluoch JR, Obonyo CO, & Ouma JO (2014). Maternal Autonomy, Distance to Health Care Facility and ANC Attendance: Findings from Madiany Division of Siaya County, Kenya. 2(4), 153–158. 10.12691/ajphr-2-4-5 [DOI] [Google Scholar]
- Delva W, Yard E, Luchters S, Chersich MF, Muigai E, Oyier V, & Temmerman M (2010). A Safe Motherhood project in Kenya: assessment of antenatal attendance, service provision and implications for PMTCT. 15(5), 584–591. 10.1111/j.1365-3156.2010.02499.x [DOI] [PubMed] [Google Scholar]
- Golub G, Herman-roloff A, Hoffman S, Jaoko W, & Bailey RC (2017). The relationship between distance and post-operative visit attendance following medical male circumcision in Nyanza Province, Kenya. 20(11), 2529–2537. 10.1007/sl0461-015-1210-z.The [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanson C, Cox J, Mbaruku G, Manzi F, Gabrysch S, Schellenberg D, … Foundation, M. G. (2015). Maternal mortality and distance to facility-based obstetric care in rural southern Tanzania: a secondary analysis of cross-sectional census data in 226 000 households. The Lancet Global Health, 3(7), e387–e395. 10.1016/S2214-109X(15)00048-0 [DOI] [PubMed] [Google Scholar]
- Joint United Nations Programme on HIV/AIDS (UNAIDS). (2012). Global report: UNAIDS report on the global AIDS epidemic [Google Scholar]
- Joint United Nations Programme on HIV/AIDS (UNAIDS). (2017). Ending AIDS. [PubMed] [Google Scholar]
- Joint United Nations Programme on HIV/AIDS (UNAIDS). (2018). UNAIDS data. [PubMed] [Google Scholar]
- Kenya National Bureau of Statistics (KNBS). (2014). Kenya Demographic and Health Survey (KDHS). [Google Scholar]
- Kinuthia J, Singa B, McGrath CJ, Odeny B, Langat A, Katana A, … John-Stewart G (2018). Prevalence and correlates of non-disclosure of maternal HIV status to male partners: a national survey in Kenya. BMC Public Health, 18(1), 671. 10.1186/s12889-018-5567-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health National AIDS and STI Control Program. (2013). HIV testing guidelines. [Google Scholar]
- Namara-Lugolobi EC et al. (2015). Prevalence and predictors of unknown HIV status among women delivering in Mulago National Referral Hospital, Kampala, Uganda. Afr Health Sci. 2017;17(4):963–973. Doi: 10.4314/Ahs.V17i4.3, 124(3), 235–239. 10.1016/j.ijgo.2013.08.011.Predictors [DOI] [PMC free article] [PubMed] [Google Scholar]
- National AIDS and STI Control Programme (NASCOP). (2012a). Guidelines for Prevention Of Mother To Child Transmission (PMTCT ) of HIV / AIDS in Kenya. [Google Scholar]
- National AIDS and STI Control Programme (NASCOP). (2012b). Kenya AIDS Indicator Survey (KAIS). [Google Scholar]
- National AIDS Control Council (NACC). (2016). Kenya HIV County Profiles 2016. [Google Scholar]
- National AIDS Control Council (NACC). (2018a). Kenya AIDS response progress report 2018. [Google Scholar]
- National AIDS Control Council (NACC). (2018b). Kenya HIV estimates. [Google Scholar]
- Ndege S, Washington S, Kaaria A, & Meara WP (2016). HIV Prevalence and Antenatal Care Attendance among Pregnant Women in a Large Home-Based HIV Counseling and Testing Program in Western Kenya. 995, 1–10. 10.1371/journal.pone.0144618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers AJ, Weke E, Kwena Z, Bukusi EA, Oyaro P, Cohen CR, & Turan JM (2016). Implementation of repeat HIV testing during pregnancy in Kenya: a qualitative study. BMC Pregnancy and Childbirth, 16(1), 151. 10.1186/s12884-016-0936-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirengo M, Muthoni L, Kellogg TA, Kim AA, Katana A, Mwanyumba S, … Study, K. (2015). Mother-to-Child Transmission of HIV in Kenya: Results From a Nationally Representative Study. 66, 66–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spangler SA, Onono M, Bukusi EA, Cohen CR, & Turan JM (2014). HIV-positive status disclosure and use of essential PMTCT and maternal health services in rural Kenya. Journal of Acquired Immune Deficiency Syndromes (1999), 67 Suppl 4(Suppl 4), S235–S242. 10.1097/QAI.0000000000000376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS. (2015). A progress report on the Global Plan towards the elimination of new HIV infections among children by 2015 and keeping their mothers alive. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woldesenbet S, Jackson D, Lombard C, Dinh T-H, Puren A, Sherman G, … Team, S. A. P. E. (SAPMCTE). (2015). Missed Opportunities along the Prevention of Mother-to-Child Transmission Services Cascade in South Africa: Uptake, Determinants, and Attributable Risk (the SAPMTCTE). PloS One, 10(7), e0132425–e0132425. 10.1371/journal.pone.0132425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2015). Consolidated guidelines on HIV testing services. [Google Scholar]


