Abstract
Objective
Uterine fibroids are prevalent in women of reproductive age and can cause various health issues. This study aimed to explore the association between vitamin D levels and the development of uterine fibroids in Turkish women, a topic on which contradictory findings have been reported.
Methods
This retrospective case–control study was conducted at Osmaniye State Hospital, Turkey, from September 2022 to September 2023. The study group comprised women diagnosed with uterine fibroids, while the control group included women who did not have uterine fibroids. Both groups were compared based on their vitamin D levels, sociodemographic characteristics, obstetric health, clinical characteristics, and imaging findings. The primary focus of the study was on the correlation between vitamin D levels and the presence of uterine fibroids.
Results
The study group involved 954 women with uterine fibroids, and the control group comprised 668 control women. The sociodemographic characteristics of the groups were not significantly different (p > 0.05). However, the median vitamin D level in the study group (9.9 ng/mL) was significantly lower than that in the control group (16.1 ng/mL, p < 0.001). Furthermore, patients with multiple uterine fibroids had significantly lower vitamin D levels than those with a single fibroid (p = 0.032). Women with three or more fibroids had even lower levels of vitamin D than those with fewer than three fibroids (p < 0.001).
Conclusion
The findings indicate a marked association between lower vitamin D levels and the presence of uterine fibroids. Patients with a higher number of fibroids had lower vitamin D levels. These results suggest a potential link between vitamin D deficiency and the development of uterine fibroids. However, more prospective studies are required to determine the exact role of vitamin D in the development and progression of uterine fibroids.
Keywords: Uterine fibroids, 25-hydroxyvitamin D3, vitamin D deficiency, ultrasound imaging
Introduction
Uterine fibroids are benign tumors that are commonly present in women of childbearing age. In addition to heavy menstrual bleeding leading to anemia, uterine fibroids have often been associated with reproductive problems, such as impaired fertility, pregnancy complications, miscarriage, and adverse pregnancy outcomes.1–3 Previous studies have reported various modifiable risk factors, including lifestyle, obesity, and nutritional deficiencies, as risk factors for the development of uterine fibroids.4,5 Controlling these risk factors may offer a cost-effective and feasible method of preventing uterine fibroids or slowing their growth.6,7
The exact cause of uterine fibroids remains unclear. 6 However, considering the immunomodulatory effects of vitamin D on cell growth and cell differentiation, several studies have cited vitamin D deficiency as a potential cause of uterine fibroids.2,4,6,8–10
Although vitamin D deficiency is considered a risk factor for the development of uterine fibroids and significant therapeutic results of vitamin D supplementation with appropriate formulas have been observed in women with vitamin D deficiency, the relationship between vitamin D levels and the risk of uterine fibroids remains controversial.1,11
Studies conducted in Western countries have reported significantly lower vitamin D levels in women with uterine fibroids.4,7,8,12 Similar findings have also been reported in studies conducted in regions with predominantly African–American populations and more sunlight exposure.2,6,9,13–15 The differences between the relevant results of different studies may be attributed to the variations in genetic and environmental factors across these studies.
There is a lack of studies on the relationship between uterine fibroids and vitamin D levels, especially in Turkish women. 15 In this context, this study was performed to assess the relationship between vitamin D levels and uterine fibroids by comparing vitamin D levels in Turkish women with and without uterine fibroids.
Materials and methods
Study design
This study was designed as a retrospective, case–control study. The study protocol was approved by the local ethical committee (Date: 08.02.2023, Number: E-77378720-774.99.221134200). The study was conducted as per the principles of the 1975 Helsinki Declaration, as revised in 2013. Written informed consent was obtained from all study participants. All patient information has been de-identified. The necessary permissions to conduct the study were obtained from the hospital’s institutional review board. The reporting of this study conforms to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines. 16
Study sample
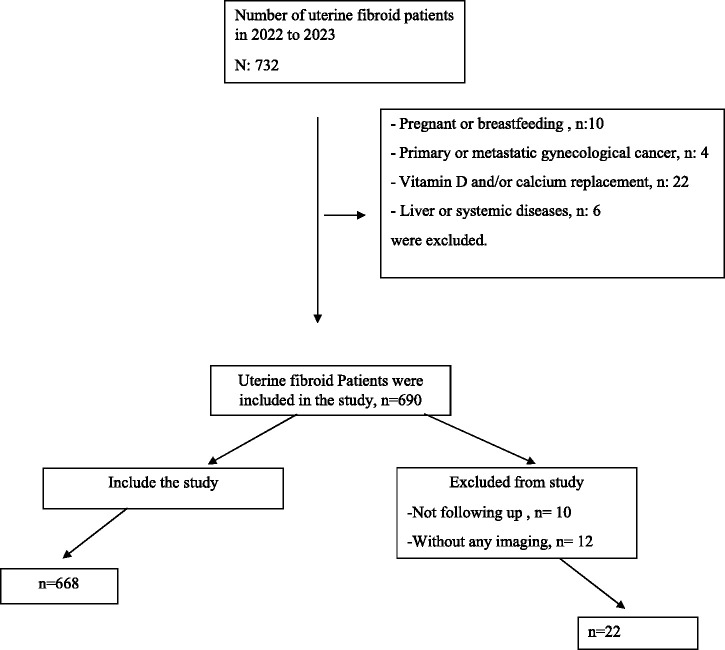
The study population consisted of female patients diagnosed with uterine fibroids at the Department of Obstetrics and Gynecology of Osmaniye State Hospital, Osmaniye, Turkey, between September 2022 and September 2023. The study group comprised patients diagnosed with sonographically confirmed uterine fibroids of any size, and the control group included patients whose routine ultrasound examinations performed during the same period did not reveal any uterine fibroids. The patients in the study and control groups were not matched in terms of age, parity, and body mass index (BMI) values. Women who were pregnant, had any type of mass lesion detected in gynecological organs, had been pregnant within the past 6 months, had been breastfeeding, were using vitamin D or calcium supplements, or had chronic liver disease were excluded from the study 6 (Figure 1).
Figure 1.
Flowchart of the inclusion criteria of patients in the study.
Laboratory investigations
Vitamin D levels were routinely assessed for women who presented to the outpatient clinics with complaints of significant pain, abnormal uterine bleeding, menstrual irregularities, or infertility. Blood samples were obtained from both the study and control groups to measure complete blood counts and serum 25-hydroxy vitamin D3 levels. Enzyme-linked immunosorbent assay kits (Cobas Elecsys 2010, Roche Diagnostics, Mannheim, Germany, 300 microwells, product code: 7725-300) were used to assay patients’ vitamin D levels using the electrochemiluminescence immunoassay (ECLIA) method. Subsequently, the patients in the study and control groups were categorized as per vitamin D deficiency (<10 ng/mL), vitamin D insufficiency (10.0–19.9 ng/mL), and no vitamin D deficiency (≥20 ng/mL).2,6
Imaging studies
Patients were examined sonographically by the attending gynecologists in the outpatient clinics using transabdominal (2–5 MHz convex) and endovaginal (4–8 MHz) probes. Imaging findings, such as the number of uterine fibroids and the maximum uterine fibroid diameter (mm), were noted. 2 The median uterine fibroid diameter in the study group was 68 mm, ranging from 24 to 674 mm.
Data collection and variables
The study and control groups were compared in terms of sociodemographic characteristics (age, education, BMI), obstetric parameters (gravidity, parity), and clinical characteristics (complaints, smoking, comorbidities) as well as the results of laboratory investigations, including vitamin D levels, and imaging.
Statistical analyses
In this study, data analysis was performed using the Jamovi Project (version 2.3.28.0) and JASP (version 0.17.3) software. Continuous variables that followed a normal distribution were expressed as mean ± standard deviation, while non-normally distributed variables were presented as median and range values. Categorical variables were presented as frequencies and percentages. To assess the normality of the data, we applied Shapiro–Wilk, Kolmogorov–Smirnov, and Anderson–Darling tests. We employed the independent samples t-test for comparing normally distributed variables, such as mean hemoglobin levels, and the Mann–Whitney U test for comparing non-normally distributed variables, such as median age, BMI, white blood cell count, and vitamin D levels. For categorical variables, such as patient symptoms, smoking status, educational level, and comorbidities, we used Pearson’s chi-square and Fisher’s exact tests to explore any associations with the presence of uterine fibroids. We considered p-values of ≤0.05 to indicate statistical significance.
Results
The study and control groups consisted of 954 and 668 patients, respectively. There was no significant difference between the groups in terms of age, BMI, and smoking status (p = 0.686, p = 0.894, and p = 0.801, respectively). There were significant differences in the frequency of presenting symptoms (p < 0.001) between the two groups. Accordingly, menorrhagia, menstrual irregularities, and infertility were significantly more prevalent in the study group than in the control group (Table 1). Conversely, the proportions of patients with pain and asymptomatic patients were higher in the control group than in the study group (22.9% vs. 17.7% and 56.9% vs. 19.6%, respectively).
Table 1.
Sociodemographic and clinical characteristics of the patients with and without uterine fibroids.
| Control group (n = 954) | Study group (patients with uterine fibroids) (n = 668) | p | |
|---|---|---|---|
| Age (years)§ | 33.0 (16.0–78.0) | 33.0 (15.0–74.0) | 0.686** |
| Body mass index (kg/m2)§ | 23.3 (16.9–42.3) | 23.2 (16.4–43.3) | 0.894** |
| Patient symptoms‡ | |||
| Pain | 218 (22.9)a | 118 (17.7)b | <0.001* |
| Menorrhagia | 53 (5.6)a | 140 (21.0)b | |
| Menstrual irregularities | 43 (4.5)a | 127 (19.0)b | |
| Infertility | 97 (10.2)a | 152 (22.8)b | |
| Asymptomatic | 543 (56.9)a | 131 (19.6)b | |
| Smoking status‡ | |||
| Nonsmoker | 836 (87.6) | 589 (88.2) | 0.801* |
| Smoker | 118 (12.4) | 79 (11.8) | |
| Level of education‡ | |||
| Illiterate/primary | 700 (73.4)a | 453 (67.8)b | 0.044* |
| High school | 199 (20.9)a | 173 (25.9)b | |
| University | 55 (5.8)a | 42 (6.3)a | |
| Presence of comorbidities‡ | 311 (32.6) | 257 (38.5) | 0.017* |
| Hypertension | 141 (14.8) | 105 (15.7) | 0.654* |
| Asthma | 86 (9.0) | 100 (15.0) | <0.001* |
| Diabetes | 81 (8.5) | 65 (9.7) | 0.441* |
| Hypothyroidism | 30 (3.1) | 23 (3.4) | 0.849* |
| Coronary artery disease | 2 (0.2) | 1 (0.1) | 0.999* |
| Other | 63 (6.6) | 51 (7.6) | 0.483* |
| Obstetric features | |||
| Gravidity§ | 4.0 (0.0–15.0) | 3.0 (0.0–15.0) | <0.001** |
| Number of full-term pregnancies§ | 2.0 (0.0–12.0) | 1.0 (0.0–12.0) | <0.001** |
Table 1 compares sociodemographic and clinical characteristics between control patients and those with uterine fibroids. § represents median values with ranges (minimum–maximum), and ‡ indicates the number and proportion of patients (n (%)). Statistical analysis was conducted using the Mann–Whitney U test (**), Pearson chi-square test, or Fisher’s exact test (*) to assess differences between the two groups. a and b denote significant differences identified in multiple comparisons. The table highlights variations in factors such as age, body mass index, patient symptoms, smoking status, educational level, comorbidities, and obstetric features.
There was a significant difference in the proportion of patients with comorbidities (p < 0.05) between the two groups. However, there was no significant difference between the two groups in terms of the distribution of the comorbidities, except for asthma. Thus, a significantly higher number of patients with comorbidities and asthma were observed in the control group than in the study group (p = 0.017 and p < 0.001, respectively) (Table 1).
The median numbers of gravidity and full-term pregnancies were significantly higher in the control group than in the study group (p < 0.001 for both cases).
The results of the laboratory investigations are presented in Table 2. The median vitamin D level was significantly lower in the study group than in the control group (9.9 vs. 16.1 ng/mL, p < 0.001). The proportion of patients with vitamin D deficiency was significantly higher in the study group than in the control group (51.8% vs. 18.9%). In a similar manner, a significantly higher number of patients with sufficient vitamin D levels were observed in the control group than in the study group (37.6% vs. 8.8%) (p < 0.001).
Table 2.
Laboratory investigations of the groups.
| Control group (n = 954) | Study group (patients with uterine fibroids) (n = 668) | p | |
|---|---|---|---|
| Hemoglobin (g/dL)† | 10.6 ± 1.6 | 10.5 ± 1.6 | 0.062*** |
| White blood cell count (×109)§ | 7005.0 (1050.0–17,800.0) | 7015.0 (3610.0–62,300.0) | 0.878* |
| Vitamin D (ng/mL)§ | 16.1 (2.4–63.6) | 9.9 (1.2–30.8) | <0.001* |
| Vitamin D groups‡ | |||
| Deficient (<10 ng/mL) | 180 (18.9)a | 346 (51.8)b | <0.001** |
| Insufficient (10 to ≤20 ng/mL) | 415 (43.5)a | 263 (39.4)a | |
| Sufficient (≥20 ng/mL) | 359 (37.6)a | 59 (8.8)b |
Table 2 presents laboratory investigations comparing control patients and patients with uterine fibroids. † denotes the mean ± standard deviation, and § indicates median values with ranges (minimum–maximum). The table utilizes the Mann–Whitney U test (*), Pearson chi-square test (**), and independent samples t-test (***) to analyze differences in variables such as hemoglobin levels, white blood cell count, and vitamin D levels. The categorization of vitamin D levels is also included, with a and b indicating significant group differences identified through multiple comparison tests.
Patients with more than one uterine fibroid had significantly lower vitamin D levels than those with only one uterine fibroid (p = 0.032). Patients with three or more uterine fibroids had significantly lower vitamin D levels than those with less than three uterine fibroids (p < 0.001) (Table 3).
Table 3.
Association between vitamin D levels and features of uterine fibroids.
| Vitamin D levels (ng/mL)§ | p* | |
|---|---|---|
| Categorization based on the number of uterine fibroids | ||
| Single (n = 134, 20.1%) | 10.3 (1.2–26.5) | 0.032 |
| Poly (n = 534, 79.9%) | 9.8 (2.3–30.8) | |
| Categorization based on the number of polyps | ||
| <3 (n = 360, 53.9%) | 10.2 (1.2–30.8) | <0.001 |
| ≥3 (n = 308, 46.1%) | 9.3 (2.4–28.5) |
Table 3 explores the association between vitamin D levels and features of uterine fibroids. § signifies median values with their respective ranges (minimum–maximum). The Mann–Whitney U test (*) was used to assess differences in vitamin D levels based on the categorization of the number of uterine fibroids and the number of polyps. This table provides insights into how vitamin D levels are correlated with the characteristics of uterine fibroids in patients.
Discussion
The study revealed a significant relationship between vitamin D deficiency and the development of uterine fibroids. Patients with uterine fibroids had significantly lower vitamin D levels than patients without uterine fibroids. In addition, among patients with uterine fibroids, patients with more uterine fibroids had significantly lower vitamin D levels than those with fewer uterine fibroids. The causality analysis of the relationship between vitamin D deficiency and the development of uterine fibroids could not be performed owing to the retrospective nature of the study. Hence, future prospective studies with extended follow-up periods are needed to confirm the causal relationship between vitamin D deficiency and the occurrence of uterine fibroids.
Several studies have reported an inverse relationship between vitamin D levels and the development of uterine fibroids.2,6,9,13–15 Additionally, several review articles, systematic reviews, and meta-analyses have concluded that vitamin D deficiency is a risk factor for the development of uterine fibroids.4,8,17 In a study conducted among African–American or Black women living in the United States, Harmon et al. 7 showed that vitamin D levels of ≥30 ng/mL were associated with a greater likelihood of fibroid loss, whereas vitamin D levels of ≥20 ng/mL were associated with slower fibroid growth. In the present study, we could not perform such complex investigations on multidimensional relationships between vitamin D levels and the development of uterine fibroids. Nevertheless, our findings are consistent with those reported by other studies.2,6
The relationship between the number of fibroids and vitamin D levels was reportedly less precise than the relationship between the development of uterine fibroids and hypovitaminosis D. 8 In a study conducted among Indian women, Kumari et al. 2 found an inverse correlation between the total volume of fibroids and vitamin D levels. Other researchers have reported similar findings.8,18 Altogether, the findings on the relationship between vitamin D levels and number of fibroids are contradictory. Several studies found no significant correlation between the number and volume of fibroids and vitamin D levels.2,15,19
Nevertheless, a higher number of uterine fibroids were associated with lower vitamin D levels in our study. Intra- and interobserver variability may have restricted the accurate determination of the number of uterine fibroids during sonography. Therefore, we did not attempt to calculate the exact number of fibroids. We categorized the patients as those with less than three uterine fibroids and those with three or more uterine fibroids.
The use of different cutoff values to define vitamin D deficiency may also lead to controversial outcomes. 12 Although some studies have categorized patients into two groups—patients with vitamin D deficiency (<20 ng/mL) and those with sufficient vitamin D (≥20 ng/mL)—other studies have categorized patients into three groups as follows: (a) patients with vitamin D deficiency (<20 ng/mL); (b) patients with insufficient vitamin D (20–30 ng/mL); and (c) patients with sufficient vitamin D (≥30 ng/mL).2,6,7,9,10,12,14,15,20 Vitamin D levels less than 20 ng/mL are commonly considered to indicate vitamin D deficiency and are associated with the risk of bone disease. However, a vitamin D cutoff level of 20 ng/mL has a low specificity in predicting the development of uterine fibroids. 9 Nevertheless, the debate about the optimal vitamin D level being 40–60 ng/mL still continues. 21 In the present study, we categorized patients into three groups as follows: (a) patients with vitamin D deficiency (<10 ng/mL); (b) patients with insufficient vitamin D (10–20 ng/mL); and (c) patients with sufficient vitamin D (≥20 ng/mL).2,6 Using vitamin D cutoff values to define vitamin D deficiency, sufficiency, and insufficiency may be a reason for the discrepancies between study results in terms of the relationship between vitamin D level and the development of uterine fibroids.
Several studies have reported that sociodemographic and obstetric characteristics are associated with vitamin D levels and the development of uterine fibroids.2,6,15 Furthermore, genetic characteristics may be among the underlying factors of vitamin D deficiency. 6 Among other factors that are reported to impact vitamin D metabolism and fibroid development are employment status, number of hours spent outdoors, educational level, career choices, and fertility history.6,15 In the present study, similar to Kaplan’s study conducted in Turkey, we found no significant relationship between sociodemographic characteristics and the development of uterine fibroids. 15 Nevertheless, we found that lower numbers of gravidity and parity were significantly associated with the development of uterine fibroids.
Kumari et al. 2 investigated the effect of exposure to sunlight on the development of uterine fibroids. They concluded that working conditions impact uterine fibroid development via exposure to sunlight.
The relationship between vitamin D supplementation and uterine fibroid development is another issue under debate. 22 Some studies have recommended vitamin D supplementation as a promising and safe treatment method to reduce the size of primary or recurrent uterine fibroids.20,23,24 However, a study reported that vitamin D supplementation has no significant impact on the number of recurrent uterine fibroids. 23 Another study found no significant effect of vitamin D supplementation on the size of uterine fibroids in women with vitamin D insufficiency or deficiency. 10
A recent meta-analysis showed that after 8 weeks of vitamin D supplementation, the size of uterine fibroids decreased significantly compared to that in the placebo group. Moreover, the study also found that vitamin D supplementation significantly increases serum vitamin D levels and reduces the size of uterine fibroids. 25
The antiproliferative and apoptotic effects of 25-hydroxyvitamin D on leiomyomas are achieved by suppressing catechol-O-methyltransferase activity and increasing 25-hydroxyvitamin D receptors in the myometrium while suppressing estrogen and progesterone receptors. 26 If the cause-and-effect relationship is fully understood and if its preventive effect on leiomyoma development and the serum vitamin D level required for this can be determined, vitamin D supplementation and monitoring can be used in the prevention and treatment of fibroids.
In our study, vitamin D levels were significantly low in the uterine fibroids group. As per the results of a previous study 25 and the current study, vitamin D supplementation may decrease the size of fibroids, reduce the clinical symptoms in patients, and reduce the need for most frequently performed surgical procedures for fibroids-related clinical symptoms.
Based on the results of our study and a review of the literature, the following recommendations can be made: exposure to sunlight for a sufficient period of time for optimal health; regular exercise; no alcohol consumption; no smoking; a vitamin D-rich diet, including vegetables and fruits; and avoidance of lifestyle habits that could cause obesity.
Limitations
The primary limitation of this study was its retrospective design. Another limitation was the lack of data on patients’ nutritional habits, dietary intake, sun exposure, and physical activity duration. Potential selection bias due to a lack of randomization, presence of confounding factors, and inability to determine causality due to the nature of the study can be considered additional study limitations. The strength of our study was that our sample size was large. Moreover, to the best of our knowledge, this is the first study conducted among the Turkish population to assess the role of vitamin D in uterine fibroids. Prospective cohort studies with regular monitoring of vitamin D levels and serial ultrasound imaging of uterine morphology are needed to gain a deeper understanding of the role of vitamin D in the development and growth of uterine fibroids.
Conclusion
This study revealed significantly lower vitamin D levels in women with uterine fibroids than in women without uterine fibroids. In addition, vitamin D levels were lower in women with greater number of uterine fibroids than in women with a smaller number of uterine fibroids. This suggests a significant relationship between vitamin D deficiency and the presence of uterine fibroids. However, further prospective research is needed to clarify the causal or inhibitory role of vitamin D in the development and progression of uterine fibroids.
Acknowledgements
The authors wish to acknowledge all study participants, study staff and staff at the health research center, and the study health facilities.
Footnotes
ORCID iD: Özer Birge https://orcid.org/0000-0002-1939-3743
Author contributions
FC, OB, and IK conceived the study, designed the work, acquired and interpreted the data, and drafted the manuscript. OB, IK, and FC were involved in the design of the work, data acquisition, and interpretation of data. OB and IK participated in the design of the work and analysis and interpretation of data. All authors approved the submitted version.
Data availability statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declaration of conflicting interests
Authors have no conflicts of interest to declare.
Ethics statement
The study protocol was approved by the local and ethical clinical research committees of the Osmaniye Provincial Health Directorate of the Ministry of Health of the Republic of Turkey (Approval Date & No: 02.08.2022 & E-77378720-774.99.221134200). The study was conducted in accordance with the principles stated in the 1975 Helsinki Declaration, as revised in 2013.
Funding
The authors declare that this study received no financial support.
Informed consent
Written informed consent was obtained from all participants included in the study.
References
- 1.Guo W, Dai M, Zhong Z, et al. The association between vitamin D and uterine fibroids: a Mendelian randomization study. Front Genet 2022; 13: 1013192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kumari R, Nath B, Gaikwad HS, et al. Association between serum vitamin D level and uterine fibroid in premenopausal women in Indian population. Drug Discov Ther 2022; 16: 8–13. [DOI] [PubMed] [Google Scholar]
- 3.Markowska A, Kurzawa P, Bednarek W, et al. Immunohistochemical expression of vitamin D receptor in uterine fibroids. Nutrients 2022; 14: 3371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sefah N, Ndebele S, Prince L, et al. Uterine fibroids - causes, impact, treatment, and lens to the African perspective. Front Pharmacol 2022; 13: 10457831045783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ali M, Bariani MV, Vafaei S, et al. Prevention of uterine fibroids: molecular mechanisms and potential clinical application. J Endometr Uterine Disord 2023; 1: 100018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tunau KA, Garba JA, Panti AA, et al. Low plasma vitamin D as a predictor of uterine fibroids in a Nigerian population. Niger Postgrad Med J 2021; 28: 181–186. [DOI] [PubMed] [Google Scholar]
- 7.Harmon QE, Patchel SA, Denslow S, et al. Vitamin D and uterine fibroid growth, incidence, and loss: a prospective ultrasound study. Fertil Steril 2022; 118: 1127–1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Combs A, Singh B, Nylander E, et al. A systematic review of vitamin D and fibroids: pathophysiology, prevention, and treatment. Reprod Sci 2023; 30: 1049–1064. [DOI] [PubMed] [Google Scholar]
- 9.Xu F, Li F, Li L, et al. Vitamin D as a risk factor for the presence of asymptomatic uterine fibroids in premenopausal Han Chinese women. Fertil Steril 2021; 115: 1288–1293. [DOI] [PubMed] [Google Scholar]
- 10.Tabrizian K, Shokouhinia R, Davari Tanha F, et al. Effect of two different doses of vitamin D supplementation on uterine myoma on South East Iranian population: a clinical trial. J Family Reprod Health 2021; 15: 248–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ciavattini A, Delli Carpini G, Serri M, et al. Hypovitaminosis D and “small burden” uterine fibroids: opportunity for a vitamin D supplementation. Medicine (Baltimore) 2016; 95: e5698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ciebiera M, Ali M, Prince L, et al. The significance of measuring vitamin D serum levels in women with uterine fibroids. Reprod Sci 2021; 28: 2098–2109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kumari S, Swetha P, Krishnan R S, et al. The association between ferritin and vitamin D levels in premenopausal fibroid uterus cases with anemia. Cureus 2021; 13: e13392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li S, Chen B, Sheng B, et al. The associations between serum vitamin D, calcium and uterine fibroids in Chinese women: a case-controlled study. J Int Med Res 2020; 48: 300060520923492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oskovi Kaplan ZA, Taşçi Y, Topçu HO, et al. 25-Hydroxy vitamin D levels in premenopausal Turkish women with uterine leiomyoma. Gynecol Endocrinol 2018; 34: 261–264. [DOI] [PubMed] [Google Scholar]
- 16.Von Elm E, Altman DG, Egger M; STROBE Initiative et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med 2007; 147: 573–577. [DOI] [PubMed] [Google Scholar]
- 17.Elkafas H, Badary O, Elmorsy E, et al. Endocrine-disrupting chemicals and vitamin D deficiency in the pathogenesis of uterine fibroids. J Adv Pharm Res 2021; 5: 260–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Srivastava P, Gupta HP, Singhi S, et al. Evaluation of 25-hydroxy vitamin D3 levels in patients with a fibroid uterus. J Obstet Gynaecol 2020; 40: 710–714. [DOI] [PubMed] [Google Scholar]
- 19.Paffoni A, Somigliana E, Vigano’ P, et al. Vitamin D status in women with uterine leiomyomas. J Clin Endocrinol Metab 2013; 98: E1374–E1378. [DOI] [PubMed] [Google Scholar]
- 20.Suneja A, Faridi F, Bhatt S, et al. Effect of vitamin D3 supplementation on symptomatic uterine leiomyoma in women with hypovitaminosis D. J Midlife Health 2021; 12: 53–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ciebiera M, Włodarczyk M, Ciebiera M, et al. Vitamin D and uterine fibroids-review of the literature and novel concepts. Int J Mol Sci 2018; 19: 2051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sheng B, Song Y, Liu Y, et al. Association between vitamin D and uterine fibroids: a study protocol of an open-label, randomised controlled trial. BMJ Open 2020; 10: e038709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vahdat M, Allahqoli L, Mirzaei H, et al. The effect of vitamin D on recurrence of uterine fibroids: a randomized, double-blind, placebo-controlled pilot study. Complement Ther Clin Pract 2022; 46: 101536. [DOI] [PubMed] [Google Scholar]
- 24.Davari Tanha F, Feizabad E, Vasheghani Farahani M, et al. The effect of vitamin D deficiency on overgrowth of uterine fibroids: a blinded randomized clinical trial. Int J Fertil Steril 2021; 15: 95–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alsharif SA, Baradwan S, Alshahrani MS, et al. Effect of oral consumption of vitamin D on uterine fibroids: a systematic review and meta-analysis of randomized clinical trials. Nutr Cancer 2024; 76: 226–235. [DOI] [PubMed] [Google Scholar]
- 26.Ciebiera M, Ali M, Prince L, et al. The evolving role of natural compounds in the medical treatment of uterine fibroids. J Clin Med 2020; 9: 1479. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.