Abstract
Chronic obstructive pulmonary disease (COPD) and cardiovascular disease (CVD) share a complex and multifactorial relationship characterized by overlapping risk factors, systemic inflammation, and intertwined pathophysiological mechanisms, with atherosclerosis emerging as a central inflammatory process connecting COPD and CVD, driven by systemic inflammation, oxidative stress, and endothelial dysfunction. While systemic inflammation is recognized as a critical link between these conditions, the precise pathways through which inflammation arises remain under investigation. There is therefore a need for therapeutic strategies to mitigate cardiovascular risks in patients with COPD. Among the pathways contributing to this interplay, the phosphoinositide 3-kinase (PI3K) signaling pathway has gained significant attention. Dysregulated PI3K signaling contributes to inflammation, oxidative stress, and endothelial dysfunction, which are key drivers of both COPD and CVD. Consequently, PI3K inhibitors have emerged as a promising therapeutic approach to mitigate inflammation and oxidative damage, offering a targeted strategy to address the shared pathological mechanisms underlying these diseases. A comprehensive understanding of the role of PI3K signaling and its inhibitors could facilitate the development of novel interventions to reduce cardiovascular risk in patients with COPD.
Key Points
| Atherosclerosis plays a pivotal role in the intricate relationship between COPD and CVD, functioning as a crucial link between these conditions. This underscores the pressing need for a comprehensive care strategy that addresses the shared pathological processes underlying these associated conditions. |
| PI3Ks play a pivotal role in atherosclerosis and COPD by driving inflammation, oxidative stress, and tissue remodeling, contributing to disease progression and exacerbations. |
| The multifaceted role of PI3K inhibitors in addressing the overlapping pathophysiological mechanisms of COPD and atherosclerosis presents significant therapeutic potential. Selective targeting of isoforms such as PI3Kγ and δ can reduce inflammation and enhance immune regulation, while PI3Kα and β inhibitors may prevent vascular remodeling and fibrosis. |
| Employing localized delivery systems such as inhalable formulations and vascular stents can further enhance precision and minimize systemic side effects. |
Introduction
An increasing body of evidence indicates that there is a complex and multifactorial relationship between chronic obstructive pulmonary disease (COPD) and cardiovascular disease (CVD) [1]. This relationship is characterized by shared risk factors, systemic inflammation, and overlapping pathophysiological mechanisms. However, the mechanistic links between COPD and CVD remain complex and multifactorial, and the precise nature of these links is not yet fully understood [2].
Although systemic inflammation represents a crucial link between the two conditions, the precise pathways through which this inflammation arises remain a matter of debate. The spill-over theory, which proposes that inflammation originating in the lungs spreads into the systemic circulation, leading to systemic inflammation, and the systemic inflammatory syndrome hypothesis, which suggests that persistent low-grade systemic inflammation may precede or occur in parallel with damage to organs such as the lungs, heart and vasculature, and may contribute to multi-organ dysfunction, provide complementary perspectives that inform future therapeutic strategies [3]. It can be reasonably argued that the mitigation of cardiovascular risk in patients with COPD necessitates an approach that addresses shared risk factors, reduces systemic inflammation, and improves pulmonary health [4].
How Atherosclerosis Evolves in Cardiovascular Disease and Links to COPD
Atherosclerosis, which is fundamentally an inflammatory disease, represents a pivotal mechanism through which COPD and CVD are interrelated. This is evidenced by the fact that they share underlying processes, including systemic inflammation, oxidative stress, and endothelial dysfunction [5, 6]. In both conditions, elevated oxidative stress levels result in damage to the vascular endothelium, impairing its function and increasing permeability to lipids across the blood vessel. This damage allows low-density lipoprotein (LDL), a key factor in the development of atherosclerosis, to enter the arterial walls, where it can become oxidized [7].
The principal lipoprotein component of LDL, apolipoprotein B-100, is responsible for the binding of LDL to LDL-specific receptors found on the membranes of some cells. The oxidized LDL (oxLDL) accumulates in the arterial walls and is taken up by macrophages. The accumulation of lipid-laden macrophages leads to the formation of foam cells, which aggregate to form fatty streaks, the earliest visible lesions in atherosclerosis. Over time, these fatty streaks evolve into mature atherosclerotic plaques [7]. The transition from fatty streaks to mature plaques involves various biochemical and immunological processes primarily regulated by macrophages [8].
Macrophages are key regulators of inflammatory and metabolic signals within these plaques, orchestrating immune responses and influencing plaque stability or progression [9]. Evidence indicates that dysfunction in macrophage metabolism is a significant factor contributing to plaque development, exacerbated by various environmental influences, notably cigarette smoke. This exposure introduces reactive aldehydes and oxidative stress, which impair mitochondrial functions and disrupt lipid-handling capacities in macrophages [10]. Such metabolic impairments notably reduce the ability of macrophages to clear excess oxLDLs, leading to an increased propensity for foam cell formation. However, oxidative stress not only decreases the ability of macrophages to clear lipids, but also encourages the accumulation of proinflammatory cytokines [11]. These cytokines contribute to vascular inflammation and plaque instability, thereby fostering a vicious cycle of atherosclerosis [12]. However, excessive lipid metabolism in foam cells not only results in inflammatory cytokine production, but also induces cell death (apoptosis) [8]. During the progression of atherosclerosis, a large number of foam cells or macrophages undergo apoptosis induced by oxLDLs, but mainly in advanced plaques, efferocytosis is impaired, leading to secondary necrosis accompanied by the release of cellular contents such as lipids, cell debris, and damage-associated molecular patterns (DAMPs), which ultimately contribute to a lipid-rich necrotic core and unresolved inflammation [8].
As plaques grow, they become encapsulated by a fibrous cap. This fibrous cap is susceptible to rupture when it becomes thin and fragile. This is often due to persistent inflammation, enzymatic degradation, and increased mechanical stress [13]. The rupture exposes the thrombogenic lipid core to circulating blood, triggering platelet activation and the coagulation cascade. The result is the formation of a thrombus that can partially or completely occlude the vessel, leading to acute cardiovascular events such as myocardial infarction or stroke [14].
Atherosclerosis is the primary contributor to several CVDs, including stroke, coronary heart disease, myocardial infarction, and peripheral arterial disease. These collectively account for a significant proportion of mortality among patients with COPD [15]. Conversely, some studies have indicated a correlation between the severity of COPD and the extent of airflow limitation with the degree of atherosclerotic disease [16–18]. This creates a bidirectional relationship where COPD worsens CVD and vice versa.
The central role played by atherosclerosis in the reciprocal relationship between COPD and CVD, acting as a bridge between the former and the latter, emphasizes the necessity for comprehensive care that addresses the common pathological mechanisms of these interconnected diseases.
Understanding the Role of PI3K in Atherosclerosis and COPD
Phosphoinositides are ubiquitous membrane components in different cell types and tissues and act as dynamic second messengers in numerous intracellular signaling pathways that tightly regulate key physiological activities [19]. Phosphoinositide 3-kinase (PI3K) is a family of intracellular signaling enzymes that are responsible for the synthesis of specific phosphoinositides and thereby regulate various cellular processes, including inflammation, cell proliferation and differentiation, metabolism, survival and apoptosis [20].
The PI3K/Akt pathway is a critical regulator of inflammatory processes and macrophage polarization, modulating the balance between pro- and antiinflammatory immune responses [21]. Its involvement in the pathogenesis of atherosclerosis is well established [21, 22]. Activation of this pathway promotes vascular smooth muscle cell proliferation and migration, disrupts endothelial integrity, and enhances leukocyte adhesion and transendothelial migration into the arterial intima. Together, these mechanisms drive chronic vascular inflammation and contribute to the initiation, progression, and destabilization of atherosclerotic plaques [22].
In the context of COPD, activation of PI3K in response to inflammatory stimuli facilitates neutrophil activation, increases neutrophil chemotaxis and degranulation, and thereby exacerbates lung inflammation [23]. In addition, the PI3K/Akt pathway plays a critical role in regulating macrophage function, which is impaired in COPD [24]. Macrophages are key mediators of persistent lung inflammation and contribute to disease progression by promoting tissue damage and remodeling through the secretion of proinflammatory cytokines and proteolytic enzymes [25]. Dysregulated activation of the PI3K/Akt pathway is closely associated with the modulation of macrophage differentiation into distinct functional phenotypes, including the classically activated (M1) proinflammatory and alternatively activated (M2) antiinflammatory states [26]. In the chronic inflammatory milieu characteristic of COPD, there is typically a predominance of M1 macrophages, which perpetuate inflammatory responses and exacerbate tissue destruction [27].
The potential of PI3K inhibitors as therapeutic agents for the reduction of atherosclerosis has been the subject of recent considerable interest, as evidenced by the numerous studies that have been conducted in this area [28]. The inhibition of PI3K has been demonstrated to reduce both inflammation and the proliferation of vascular smooth muscle cells, thereby stabilizing plaques [22]. This may lead to a reduction in cardiovascular events and therefore an improvement in COPD. Nevertheless, its extensive suppression may compromise immune responses [29], thereby increasing susceptibility to infections, which represents a significant concern for patients with COPD.
In any case, the use of these agents in patients with COPD is complex and presents several challenges, primarily because they act on shared inflammatory pathways, which may have the effect of exacerbating respiratory symptoms [30].
Given the current evidence and the issues we have highlighted, we believe it is important to explore strategies to optimize the use of PI3K inhibitors to effectively reduce atherosclerosis while minimizing the risk of exacerbating COPD symptoms.
PI3K Isoenzymes
The PI3K family is classified into three distinct classes (I, II, and III) on the basis of structural characteristics, phospholipid substrates, and regulatory mechanisms [28, 31]. Phosphatidylinositol 3,4,5-trisphosphate, generated by class I PI3Ks through the action of growth factor receptors and G protein-coupled receptors, acts as a second messenger, promoting the recruitment of effector proteins to particular areas of the plasma membrane or intimal region [32]. The aforementioned effectors belong to a variety of functional protein classes, namely protein kinases and other enzymes, signaling adaptors, and regulators of small GTPases. Because of this diversity, class I PI3Ks are capable of initiating and contributing to a wide array of signaling pathways within cells.
The four class I enzymes, designated PI3Kα, PI3Kβ, PI3Kγ, and PI3Kδ, are heterodimers comprising a catalytic subunit of 110 kDa (p110α, p110β, p110γ, or p110δ) and a regulatory subunit [28, 31]. Class I PI3Ks can be further categorized into two subcategories on the basis of the catalytic subunits that they contain: class IA and class IB. In the mammalian system, class IA comprises three distinct isoforms: PI3Kα, PI3Kβ, and PI3Kδ. In contrast, class IB is represented by a single isoform, PI3Kγ. The diverse activation mechanisms of the class I PI3K isoforms suggest that each has specific biological functions that operate downstream of G protein-coupled receptors, such as those activated by chemokines. It is noteworthy that both PI3Kγ and PI3Kδ are predominantly (though not exclusively) expressed in leukocytes, indicating their substantial involvement in PI3K-mediated signaling within both the innate and adaptive immune systems.
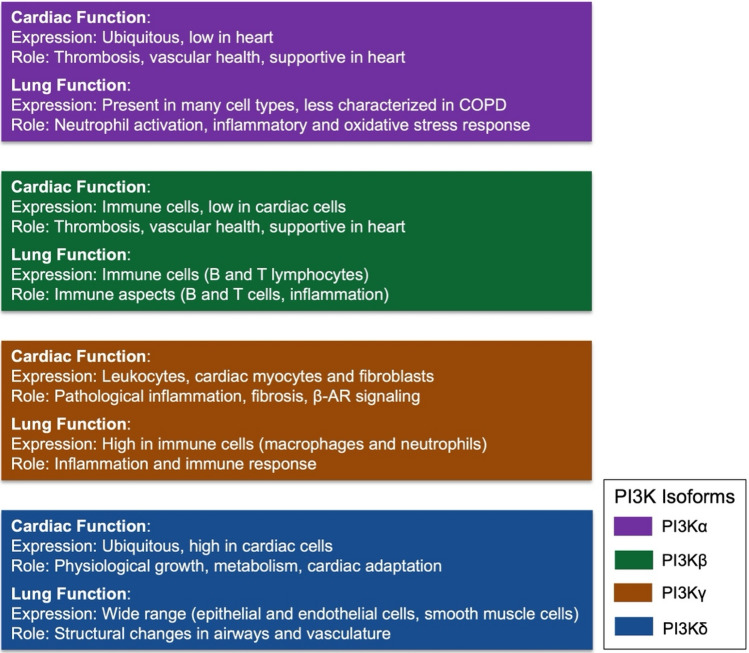
In the heart, the different PI3K class I isoenzymes fulfill distinct roles in maintaining normal function and in responding to stress or injury (Fig. 1) [28, 33, 34]. PI3Kα, which is expressed ubiquitously with significant expression in cardiac myocytes, is crucial for physiological growth and metabolic regulation, and thus essential for normal cardiac function and adaptation. PI3Kγ, which is predominantly expressed in leukocytes, but also in cardiac myocytes and fibroblasts, and PI3Kδ, which is predominantly expressed in immune cells with low expression in cardiac cells, are more involved in pathological processes, such as inflammation and fibrosis. Additionally, PI3Kγ is involved in the β-adrenoceptor (AR) signaling pathway. PI3Kβ, which is expressed ubiquitously, but with lower expression in the heart compared with PI3Kα, plays a supporting role in the heart but is more relevant to thrombosis and vascular health [28].
Fig. 1.
Summary of the expression and roles of PI3K isoforms in cardiac and lung function. Each bar corresponds to an isoform, with detailed annotations for its expression pattern and role in cardiac or lung function and pathology
The various PI3K class I isoenzymes also perform discrete functions within the lungs [31, 35] (figure). PI3Kγ, which is highly expressed in immune cells, including macrophages and neutrophils, which are abundant in the lungs of patients with COPD, and PI3Kδ, which is predominantly expressed in immune cells, particularly B and T lymphocytes, are principal contributors to the inflammatory and immune aspects. PI3Kα, which is expressed in a wide range of cells, including epithelial cells, endothelial cells, and smooth muscle cells in the lungs, influences structural changes in the airway and vasculature. PI3Kβ, which is present in many cell types present in the lung, plays a critical role in neutrophil activation by immune complexes [36] and works alongside other isoforms in inflammatory and oxidative stress responses. However, it is less well characterized than other isoforms in COPD.
The Contribution of PI3K Isoenzymes to Overlapping Pathophysiological Processes in Atherosclerosis and COPD
As previously stated, both atherosclerosis and COPD are driven by chronic inflammation, which involves the activation of inflammatory cells, the release of cytokines, and oxidative stress. PI3K isoenzymes play a pivotal role in immune cell signaling and recruitment and activation in both diseases, as well as in platelet activation and thrombosis (Table 1). In atherosclerosis, these enzymes facilitate the recruitment of monocytes/macrophages to vascular plaques and contribute to the systemic inflammation that can exacerbate COPD outcomes by intensifying pulmonary inflammation [37]. In COPD, there is a notable elevation in PI3K activity, which drives neutrophilic and lymphocytic inflammation in the lungs. The spillover of inflammatory mediators such as interleukin (IL)−6 and tumor necrosis factor (TNF)-α into the systemic circulation contributes to vascular dysfunction and accelerates the development of atherosclerosis [38]. Furthermore, PI3Kγ has been demonstrated to amplify oxidative stress by activating nicotinamide adenine dinucleotide phosphate (NADPH) oxidases in immune cells [39]. In COPD, systemic inflammation increases the risk of cardiovascular events, particularly during exacerbations [40].
Table 1.
Shared pathophysiological mechanisms in COPD and CVD and clinical implications of PI3K modulation
| Mechanism | Description | Focus area | Recommended approach |
|---|---|---|---|
| Systemic inflammation | Chronic inflammation affecting both pulmonary and cardiovascular systems | Reducing inflammation | Use PI3K inhibitors to target systemic and pulmonary inflammation |
| Oxidative stress | Elevated oxidative stress contributing to tissue damage and inflammation in both conditions | Managing oxidative stress | Incorporate PI3K inhibition to reduce oxidative damage in the lungs and vasculature |
| Endothelial dysfunction | Impairment in vascular endothelial function contributing to atherosclerosis and CVD progression | Reducing inflammation and vascular smooth muscle cells proliferation, thereby stabilizing plaques and potentially reducing cardiovascular events | Combine PI3K inhibitors with existing COPD and CVD therapies for synergistic effects |
Selective Isoform Targeting
Stabilizing atherosclerotic plaques and reducing systemic inflammation may lead to improved clinical outcomes in COPD by reducing the frequency of exacerbations and limiting systemic inflammatory spillover [37]. In this context, PI3K inhibitors have emerged as potential therapeutic agents capable of modulating inflammatory pathways and thereby reducing systemic inflammation, which contributes to both atherosclerotic plaque instability and COPD exacerbations.
The utilization of pan-PI3K inhibitors, which target all four catalytic isoforms of class I PI3K, has been demonstrated to induce a broad spectrum of activities and a broader inhibition. The inhibition of pan-PI3K with LY294002 has been shown to markedly augment the elevation of L-type Ca2⁺ channel currents, intracellular Ca2⁺ transients, and myocyte contractility induced by β1-ARs [41]. It has been evidenced that pan-PI3K inhibitors display cardiotoxicity, predominantly manifesting as arrhythmogenic effects [42]. Moreover, pan-PI3K inhibitors have been found to rapidly induce apoptosis, leading to decreased viability and impaired contractility of cardiomyocytes [43]. Nevertheless, the use of pan-PI3K inhibitors to target multiple PI3Ks with the aim of achieving maximal suppression of pathway activity may prove an effective approach in the treatment of COPD. ZSTK474, a pan-PI3K inhibitor, has been demonstrated to effectively inhibit the secretion of matrix metalloproteinase-9 and reactive oxygen species (ROS) from neutrophils obtained from patients with COPD [23]. Additionally, wortmannin, a further pan-PI3K inhibitor, has been found to facilitate the differentiation of alveolar stem cells into mature alveolar cells [44]. In animal studies focused on understanding COPD, pan-PI3K inhibitors have been shown to significantly promote the regeneration of alveoli, suggesting a promising role in enhancing lung regeneration for patients with COPD. However, it is important to note that this approach carries the potential risk of systemic adverse effects [45].
The assumption that all PI3K inhibitors will have the same effect on both atherosclerosis and COPD symptoms is an oversimplification that fails to account for the complexity of the underlying biological pathways. Isoform-specific inhibitors perhaps offer a more targeted and safer approach (Table 2).
Table 2.
Role of PI3K isoforms and their inhibitors in COPD and atherosclerosis
| PI3K isoform | Expression profile | Role in COPD | Role in atherosclerosis | Examples of inhibitors | Clinical relevance |
|---|---|---|---|---|---|
| PI3Kα | Highly expressed in epithelial cells and smooth muscle | Contributes to airway remodeling, epithelial cell proliferation, and oxidative stress | Promotes vascular smooth muscle cell proliferation and plaque formation | Alpelisib, taselisib, UCL-TRO-1938, NVS-PI3-2, PIK-75 | Targeted for epithelial dysfunction in COPD and plaque stability in atherosclerosis |
| PI3Kβ | Found in platelets, endothelial cells, and immune cells | May influence platelet aggregation and thrombosis associated with systemic inflammation in COPD | Regulates platelet activation and contributes to thrombosis in advanced plaques | TGX-221, AZD8186 | Relevant for thrombotic complications in both COPD and cardiovascular diseases |
| PI3Kγ | Expressed in immune cells (macrophages, neutrophils, T cells) | Modulates macrophage polarization and neutrophil infiltration, driving inflammation and tissue damage | Drives monocyte and macrophage recruitment in plaques, contributing to chronic inflammation | IPI-549, AS605240, LAS191954, IC87114, TG100-115 (dual γ/δ inhibitor), AZD8154 (dual γ/δ inhibitor), duvelisib (dual γ/δ inhibitor) | Targeted for inflammation and immune modulation in both COPD and atherosclerosis |
| PI3Kδ | Predominantly expressed in B cells and leukocytes | Enhances adaptive immune responses, contributing to chronic inflammation and mucus hypersecretion | Plays a role in chronic inflammation via immune cell activation in atherosclerotic plaques | Idelalisib, umbralisib, lenolisib, IHMT-PI3Kδ−372, nemiralisib, CHF6523 | Relevant for inflammation-driven progression of both diseases |
The inhibition of PI3Kγ or PI3Kδ may prove an effective means of reducing pathological inflammation and fibrosis in conditions such as heart failure or myocarditis. The selective inhibition of PI3Kγ with AS605240 was found to significantly reduce early atherosclerotic lesions in apolipoprotein E-null mice, and to attenuate advanced atherosclerotic lesions in LDL receptor-deficient mice [46]. However, it also resulted in an increased infarct size with defective reparative neovascularization and impaired recovery of left ventricular function in a mouse model of myocardial infarction [47]. Nevertheless, TG100-115, a PI3Kγ/δ inhibitor, has been demonstrated to effectively reduce infarct size following myocardial ischemia/reperfusion injury in rodent models [48]. However, the anticipated outcomes were not achieved in a phase I/II clinical trial in patients with post-myocardial infarction [49].
Given the established link between PI3Kγ and δ subtypes and the inflammation present in patients with COPD [50], the reduction of nitric oxide production by PI3K inhibitors through the inhibition of carbon monoxide synthase indicates that disrupting the PI3Kγ/δ signaling pathway may prove beneficial in addressing the imbalance in proteases observed in cases of severe COPD [51]. Aerosolized TG100-115 was demonstrated to be efficacious in inhibiting the activation of pulmonary neutrophils caused by intranasal LPS and smoke in a murine model of COPD [52]. Moreover, AS605240 was found to reduce the migration of polymorphonuclear leukocytes in vitro and to decrease their infiltration into the lungs of mice with LPS-induced lung injury [53]. It is noteworthy that the therapeutic application of TG100-115 demonstrated efficacy even in cases of steroid-resistant COPD resulting from smoking in these mice. AZD8154, another PI3Kγ/δ inhibitor, which demonstrated efficacy in a rat ovalbumin challenge model of allergic asthma and in cells derived from patients with asthma [54], has been successfully tested in healthy volunteers [55], but its development has been discontinued [56].
Several PI3Kδ inhibitors have been the subject of examination in preclinical and clinical studies with a focus on pulmonary conditions. The efficacy of LAS191954 was evaluated against concanavalin A-induced IL-2 production and a notable reduction in T cell cytokine production was found [57]. IHMT-PI3Kδ−372 has been shown to dose-dependently enhance lung function, increasing arterial oxygen saturation while decreasing arterial carbon dioxide levels in animals exposed to cigarette smoke [58]. In addition, the levels of inflammatory cytokines, including IL-1, IL-6, IL-8, and TNF-α, and the number of alveolar macrophages in bronchoalveolar lavage, were found to decrease in a dose-dependent manner. Nemiralisib is a potent and highly selective inhaled PI3Kδ inhibitor that inhibits the release of proinflammatory cytokines from human peripheral blood mononuclear cells and human lung tissue with nanomolar potencies [59]. CHF6523 is another PI3Kδ inhibitor that in a series of preclinical studies conducted in rodent models of airway inflammation demonstrated potent inhibition of eosinophilic/type-2 inflammation comparable to that of nemiralisib [60]. However, this drug did not induce demonstrable antiinflammatory effects in patients with stable COPD (chronic bronchitis phenotype) and evidence of type-2 inflammation [61]. These findings suggest that this pharmacological pathway is a questionable target for the treatment of inflammatory airway diseases.
A recent systematic review evaluated the effectiveness and safety of nemiralisib in patients with COPD, but the findings were inconclusive [62]. The effects of nemiralisib on lung function, as evaluated through spirometry and functional respiratory imaging, were unclear. Additionally, no significant disparities were observed between the nemiralisib and control groups with respect to the utilization of rescue medication or patient-reported outcomes, which included the COPD Assessment Test (CAT) score, St. George's Respiratory Questionnaire (SGRQ) score, and modified Medical Research Council (mMRC) score. Also RV-1729 has been investigated in patients with COPD (NCT02140346), but no results have been revealed.
Neutrophils, a pivotal component of the innate immune system, play a critical role in fighting pathogens. However, in the context of patients with COPD, there is a notable diminution in the migratory functionality of their blood-derived neutrophil population, both in terms of speed and directionality [63]. This phenomenon can be reversed through the utilization of PI3Kδ inhibitors [64]. These inhibitors have also been found to enhance the functionality of both B and T lymphocytes, leading to a reduction in the secretion of proinflammatory factors [65]. Consequently, the potential exists for PI3Kδ inhibitors to serve to decrease the incidence of pathogen-induced exacerbations by facilitating neutrophil-mediated clearance of pathogens and suppressing inflammatory responses [66], while also stabilizing atherosclerotic plaques by limiting macrophage-driven inflammation and oxidative damage. In addition, nemiralisib has been shown to decrease the secretion of proinflammatory cytokines and enhance survival rates in the context of infections [65]. Furthermore, the drug influenced the migratory patterns of neutrophils in patients with stable COPD, but this effect was not observed in acute exacerbations of COPD [67]. Indeed, the results on the efficacy of nemiralisib on key endpoints, such as exacerbation rate, time to next exacerbation, exacerbation recovery proportion, time to exacerbation recovery, and the use of rescue medication, are inconclusive according to the results of the examined review [62].
UCL-TRO-1938, a small-molecule activator of the PI3Kα isoform, has been demonstrated to provide cardioprotection from ischemia-reperfusion injury in rodent models [68]. However, there is also evidence that PI3Kα inhibition can result in an increased risk of arrhythmia, biventricular cardiac dysfunction, and impaired recovery from cardiotoxicity [69]. The use of alpelisib, a PI3Kα inhibitor, has been shown to exert detrimental effects on cardiac health and post-myocardial infarction cardiac repair, thereby indicating that both endothelial and cardiomyocyte PI3Kα plays an important role in cardiac recovery following a myocardial infarction [70]. Regarding the impact on the lungs, it was demonstrated that the inhibition of PI3Kα with NVS-PI3-2 led to a notable reduction in the production of TNF-α and IL-6 by alveolar macrophages [71]. Furthermore, it was found that PIK-75, a PI3Kα specific inhibitor, markedly suppressed particulate matter-induced inflammation and mucin hypersecretion in human bronchial epithelial cells [72].
Inhibition of PI3Kβ may be an effective strategy for reducing thrombotic risks. However, more research is needed to determine its direct relevance to COPD lung pathology, given the possibility that PI3Kβ may exacerbate inflammation under certain conditions and its inhibition may prolong bleeding time [73].
Nevertheless, the use of selective PI3Kα and PI3Kβ inhibitors also presents a promising avenue for the treatment of patients with concomitant COPD and atherosclerosis. Indeed, the selective inhibition of PI3Kα and PI3Kβ has the potential to prevent excessive vascular smooth muscle cell proliferation, remodeling, and platelet activation in atherosclerosis and to reduce airway fibrosis and remodeling in COPD, while avoiding the adverse effects associated with excessive suppression of immune responses.
It is also important to note that PI3Ks, particularly PI3Kδ, play a role in corticosteroid resistance in COPD by inhibiting histone deacetylase-2 activity. An increase in the efficacy of dexamethasone on the accumulation of inflammatory cells was observed in mice administered IC87114, a selective inhibitor of PI3Kδ [74]. Consequently, the inhibition of PI3Kδ may serve to enhance the antiinflammatory effects of corticosteroids in COPD [23], thereby reducing the risk of exacerbations while also conferring benefits with respect to atherosclerosis. It is noteworthy that formoterol, but not salmeterol, reversed oxidative stress-induced corticosteroid insensitivity and decreased β2-AR-dependent cAMP production via inhibition of PI3Kδ signaling [75].
The U.S. Food and Drug Administration (FDA) has granted approval for the use of several PI3K inhibitors. These include the PI3Kα inhibitor alpelisib, which has been approved for the treatment of breast cancer; the PI3Kδ inhibitors umbralisib and idelalisib; the dual inhibitor of PI3Kδ and PI3Kγ, duvelisib, which has been voluntarily withdrawn from the market by its developer; and the pan-PI3K inhibitor copanlisib, all of which have been approved for the treatment of blood disorders [76]. Furthermore, the FDA has granted approval for lenolisib to be used in the treatment of activated PI3Kδ syndrome, which is caused by mutations in the PIK3CD or PIK3R1 genes that encode PI3Kδ [77].
Optimizing PI3K Inhibitor Treatment to Achieve Dual Benefit
The simultaneous treatment of atherosclerosis and COPD poses a significant challenge due to the considerable overlap in the inflammatory and immune pathways of these two conditions [1]. In the context of an integrated pharmacological approach with smoking cessation, exercise, and diet modifications [78], the combination of PI3K inhibitors with other antiinflammatory or lipid-lowering agents might produce synergistic effects.
It is likely that combining low-dose PI3K inhibitors with corticosteroids and/or bronchodilators (e.g., formoterol) may improve outcomes in patients with COPD with coexisting atherosclerosis, given the ability of PI3Kδ inhibition to enhance corticosteroid efficacy [23] and the ability of formoterol to restore corticosteroid sensitivity and modulate cAMP production through PI3Kδ inhibition [75]. In addition, when corticosteroids interact with the glucocorticoid receptor, they activate PI3K and protein kinase Akt [79]. These, in turn, stimulate endothelial nitric oxide synthase and promote vasorelaxation through nitric oxide, which has also antithrombotic and antiproliferative properties [79].
Also the combination of statins and PI3K inhibitors may offer complementary benefits. Statins can stabilize atherosclerotic plaques [80] and reduce vascular inflammation [81], while PI3K inhibitors can attenuate chronic airway inflammation and oxidative stress [82], potentially enhancing the efficacy of corticosteroids. Moreover, both agents act on overlapping inflammatory pathways, including NF-κB and cytokine signaling cascades [83, 84].
In any case, a multifaceted approach incorporating the selective targeting of PI3K isoforms, in addition to tissue-specific delivery mechanisms and continuous monitoring of inflammatory responses, might ensure effective targeting of shared pathophysiology while circumventing any unintended exacerbation of either disease (Table 3).
Table 3.
Strategies for optimizing PI3K inhibitor treatment to achieve dual benefit in COPD and atherosclerosis
| Strategy | Mechanism of action | Relevance to COPD | Relevance to atherosclerosis | Challenges |
|---|---|---|---|---|
| Selective targeting of isoforms | Design inhibitors specific to PI3Kγ and PI3Kδ isoforms to reduce inflammation while minimizing side effects | Reduces neutrophil and macrophage-driven inflammation in the airways, improving lung function | Decreases monocyte and macrophage recruitment in plaques, limiting chronic vascular inflammation | Potential compensation by nontargeted isoforms, leading to resistance or limited efficacy |
| Dual targeting approaches | Combine PI3K inhibitors with other antiinflammatory or lipid-lowering agents for synergistic effects | Amplifies reduction in airway remodeling and oxidative stress, offering broader therapeutic benefits | Enhances plaque stabilization and reduces lipid accumulation in vascular walls | Risk of increased systemic toxicity and drug–drug interactions |
| Adjusting dosage | Optimize dosing regimens to minimize off-target effects and maximize therapeutic windows | Improves tolerability, allowing sustained suppression of airway inflammation without exacerbations | Enables long-term plaque stabilization without affecting healthy vascular functions | Identifying the ideal dose to balance efficacy with tolerability across patient populations |
| Nanocarrier-based drug delivery | Use of nanoparticles to deliver PI3K inhibitors directly to affected tissues, enhancing specificity | Targets inflamed airway tissues directly, minimizing systemic exposure and reducing side effects | Delivers drugs to inflamed atherosclerotic plaques selectively, reducing unintended vascular effects | Challenges in developing stable, biocompatible nanocarriers with effective targeting mechanisms |
| Biomarker-guided therapy | Employ biomarkers (e.g., inflammatory cytokines, PI3K activity levels) to identify responsive patient subsets | Identifies patients with high PI3K-mediated airway inflammation for tailored treatments | Stratifies patients on the basis of plaque inflammation or immune profile for targeted interventions | Requires validation of reliable biomarkers for clinical use in COPD and atherosclerosis |
| Combination with lifestyle interventions | Integrate pharmacological approaches with smoking cessation, exercise, and dietary changes | Reduces progression of COPD symptoms by addressing systemic inflammation and oxidative stress | Slows atherosclerosis progression by improving vascular health and reducing risk factors | Adherence to lifestyle interventions remains a challenge for long-term outcomes |
The objective should be to achieve a balance between the systemic antiinflammatory effects of PI3K inhibitors and the precise control of their tissue-specific actions to avoid undesirable adverse effects such as, for example, altered immune responses in the lungs or vascular complications. The selective inhibition of specific isoforms allows for the implementation of a targeted therapeutic action that reduces risk of impairing tissue repair or causing excessive immunosuppression, which is of particular significance for patients with COPD prone to infections. Thus, by targeting PI3Kγ and PI3Kδ for reducing inflammatory processes [85] and PI3Kα and β for vascular repair [86], broad-spectrum PI3K inhibition can be avoided, preventing potential impairments to critical cellular functions such as tissue repair and immune surveillance [87].
However, to optimize PI3K inhibitors to deliver dual benefits to enhance the therapeutic efficacy of these inhibitors in patients with concurrent cardiovascular and respiratory conditions, there is also the need to employ localized delivery systems [88].
The administration of PI3K inhibitors at a systemic level may result in off-target effects, particularly in patients with preexisting comorbidities. This is because, although each class I PI3K is prominently associated with a specific set of functions, there is a considerable degree of redundancy within this family of enzymes [87]. The use of localized delivery systems, such as inhalable formulations for COPD or vascular stents coated with PI3K inhibitors for atherosclerosis, can facilitate the precision of drug delivery. Inhalable PI3K inhibitors, for example, can directly diminish lung inflammation without substantial systemic exposure [77], thereby reducing adverse effects such as immunosuppression. Similarly, vascular-specific drug delivery systems, including the incorporation of PI3K inhibitors as drug-eluting stents or drug-coated balloons [89], could focus treatment on atherosclerotic lesions, thereby reducing the risk of adverse effects in the lungs. The strategy of formulating PI3K inhibitors as prodrugs for potential inhalation administration is a particularly fascinating area of research. CL27 is a prodrug pan-PI3K inhibitor that is engineered to be activated within airway epithelial cells through the action of cytoplasmic esterases, resulting in the release of the active compound [90]. The hydrophobic characteristics of the active drug ensure that it remains intracellular, thus minimizing its access to the bloodstream and other tissues.
Recently it has been suggested that utilizing targeted nanoparticles can enhance the therapeutic effects of PI3K inhibitors while minimizing systemic exposure [91]. The nanoparticle-based delivery system is expected to enhance the bioavailability of PI3K inhibitors at the target sites in the lungs and atherosclerotic plaques. This would reduce inflammation and improve lung function in the COPD model and stabilize atherosclerotic plaques and reduce plaque burden in the atherosclerosis model. However, there are potential limitations that mainly include the variability in nanoparticle behavior in different biological environments [92]. Furthermore, long-term effects of PI3K inhibition on cardiovascular health need further investigation.
It is crucial to closely monitor inflammatory responses in patients receiving PI3K inhibitors to evaluate therapeutic responses. This need arises from the understanding that, in the context of COPD, excessive suppression of inflammation can impede host defenses against respiratory infections, thereby increasing the risk of exacerbations. Conversely, in the setting of atherosclerosis, insufficient control of inflammation can lead to plaque instability and subsequent cardiovascular events. A proactive approach, involving close monitoring and timely adjustments to treatment regimens, is essential to achieve the delicate balance between reducing harmful inflammation and maintaining essential immune function. This strategy ensures that the benefits of atherosclerosis reduction do not come at the cost of respiratory health.
It was deemed vital to employ panels of biomarkers to assess the various components and pathways linked to the pathophysiology of COPD and atherosclerosis, due to the inefficiency of any single biomarker when used in isolation [93, 94]. Circulating C-reactive protein (CRP), IL-6, and TNF-α are three blood biomarkers frequently linked to chronic inflammation. When used in conjunction with white blood cell count, fibrinogen, and IL-8, TNF-α has also been shown to be a valuable predictor of increased mortality and exacerbation rates in COPD patients with inflammation, in comparison with those without inflammation [93]. It has also been established that CRP functions as an independent predictor of both primary and secondary events related to coronary heart disease [93]. However, due to the tendency of CRP levels to rise in response to different inflammatory triggers, it is still unknown whether increased CRP levels actually occur prior to the onset of vascular disease [94]. IL-6 levels in the blood of patients with coronary heart disease are elevated in comparison with healthy individuals, with a direct relationship between the severity of the disease and higher concentrations of this inflammatory marker [94]. Additionally, there is a significant rise in IL-6 levels during episodes of plaque rupture [94].
In any case, a comprehensive biomarker panel to assess COPD and atherosclerosis at the same time should include markers of systemic inflammation (CRP, IL-6, TNF-α), oxidative stress (malondialdehyde, 8-isoprostane), immune activation (neutrophil-to-lymphocyte ratio, matrix metalloproteinases), and endothelial dysfunction (asymmetric dimethylarginine, Von Willebrand factor), along with disease-specific indicators such as surfactant protein D for lung injury and oxidized LDL for vascular risk. These biomarkers should provide insights into shared pathological mechanisms, supporting early diagnosis, risk stratification, and personalized treatment strategies.
Conclusions
Atherosclerosis acts as a critical link between COPD and CVD due to shared mechanisms such as systemic inflammation, oxidative stress, and endothelial dysfunction. By serving as the underlying cause of many cardiovascular events, atherosclerosis highlights the need for integrated management approaches to address these interconnected conditions effectively.
The multifaceted role of PI3K inhibitors in addressing the overlapping pathophysiological mechanisms of COPD and atherosclerosis has significant therapeutic potential. Indeed, selective targeting of specific isoforms, such as PI3Kγ and δ, has been shown to reduce inflammation and improve immune regulation. This approach is particularly promising for achieving a dual benefit, as it targets the inflammatory pathways common to both COPD and atherosclerosis. However, it is also worth considering the use of PI3Kα and β inhibitors, as these may prevent vascular remodeling and fibrosis. The employment of localized delivery systems, such as inhalable formulations and vascular stents, is pivotal for improving specificity, thus enhancing precision and reducing systemic adverse effects. Obviously, dual targeting in conjunction with lifestyle interventions can enhance outcomes; however, this approach necessitates meticulous patient monitoring. Lastly, comprehensive biomarker panels, encompassing markers of inflammation, oxidative stress, and endothelial dysfunction are imperative for optimizing treatment, facilitating early diagnosis, and achieving personalized care for patients with these comorbid conditions.
There is a clear need for further investigation into isoform-selective PI3K inhibitors that can maintain a balance between therapeutic efficacy and safety in the context of atherosclerosis and COPD. In this regard, clinical trials should be conducted in patients with comorbid atherosclerosis and COPD to assess the therapeutic window of PI3K inhibitors. Exploration of drug delivery systems, such as nanoparticles, for localized PI3K inhibition is also of great importance.
Declarations
Funding
Open access funding provided by Università degli Studi di Roma Tor Vergata within the CRUI-CARE Agreement.
Conflict of interest
The authors have no financial or non-financial relationships or activities concerning this article.
Availability of data and material
Not applicable.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Not applicable.
Author contributions
All authors were involved in the initial conception of the manuscript. M.C. and C.P.P. led the drafting and coordinated the revisions of the manuscript among all authors. P.R, L.C., and M.G.M. critically revised the content on their areas of expertise. All authors approved the final draft.
References
- 1.Rabe KF, Hurst JR, Suissa S. Cardiovascular disease and COPD: dangerous liaisons? Eur Respir Rev. 2018;27(149): 180057. 10.1183/16000617.0057-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Decramer M, Janssens W. Chronic obstructive pulmonary disease and comorbidities. Lancet Respir Med. 2013;1(1):73–83. 10.1016/S2213-2600(12)70060-7. [DOI] [PubMed] [Google Scholar]
- 3.Barnes PJ, Celli BR. Systemic manifestations and comorbidities of COPD. Eur Respir J. 2009;33(5):1165–85. 10.1183/09031936.00128008. [DOI] [PubMed] [Google Scholar]
- 4.Cazzola M, Calzetta L, Rinaldi B, et al. Management of chronic obstructive pulmonary disease in patients with cardiovascular diseases. Drugs. 2017;77(7):721–32. 10.1007/s40265-017-0731-3. [DOI] [PubMed] [Google Scholar]
- 5.Rogliani P, Calzetta L. Cardiovascular disease in COPD. In: Martínez-García MÁ, Pépin J-L, Cazzola M, editors. Cardiovascular complications of respiratory disorders (ERS Monograph). Sheffield, European Respiratory Society, 2020; pp. 47–65. 10.1183/2312508X.10027319.
- 6.Miklós Z, Horváth I. The role of oxidative stress and antioxidants in cardiovascular comorbidities in COPD. Antioxidants (Basel). 2023;12(6):1196. 10.3390/antiox12061196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schade DS, Helitzer D, Eaton P. Evidence that low density lipoprotein is the primary cause of atherosclerotic cardiovascular disease: a Bradford-Hill approach. WJCD. 2017;07(9):271–84. 10.4236/wjcd.2017.79025. [Google Scholar]
- 8.Hou P, Fang J, Liu Z, et al. Macrophage polarization and metabolism in atherosclerosis. Cell Death Dis. 2023;14(10):691. 10.1038/s41419-023-06206-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moore KJ, Tabas I. Macrophages in the pathogenesis of atherosclerosis. Cell. 2011;145(3):341–55. 10.1016/j.cell.2011.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lara-Guzmán OJ, Gil-Izquierdo Á, Medina S, et al. Oxidized LDL triggers changes in oxidative stress and inflammatory biomarkers in human macrophages. Redox Biol. 2018;15:1–11. 10.1016/j.redox.2017.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Groh LA, Ferreira AV, Helder L, et al. oxLDL-induced trained immunity is dependent on mitochondrial metabolic reprogramming. Immunometabolism. 2021;3(3): e210025. 10.20900/immunometab20210025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen C, Khismatullin DB. Oxidized low-density lipoprotein contributes to atherogenesis via co-activation of macrophages and mast cells. PLoS ONE. 2015;10(3): e0123088. 10.1371/journal.pone.0123088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baaten CCFMJ, Nagy M, Bergmeier W, Spronk HMH, van der Meijden PEJ. Platelet biology and function: plaque erosion vs. rupture. Eur Heart J. 2024;45(1):18–31. 10.1093/eurheartj/ehad720. [DOI] [PMC free article] [PubMed]
- 14.Benjamin EJ, Muntner P, Alonso A, et al. Heart disease and stroke statistics—2019 Update: a from the American Heart Association. Circulation. 2019;139(10):e56–528. 10.1161/CIR.0000000000000659. [DOI] [PubMed] [Google Scholar]
- 15.Sá-Sousa A, Rodrigues C, Jácome C, et al. Cardiovascular risk in patients with chronic obstructive pulmonary disease: a systematic review. J Clin Med. 2024;13(17):5173. 10.3390/jcm13175173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barr RG, Ahmed FS, Carr JJ, et al. Subclinical atherosclerosis, airflow obstruction and emphysema: the MESA Lung Study. Eur Respir J. 2012;39(4):846–54. 10.1183/09031936.00165410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chandra D, Gupta A, Strollo PJ Jr, et al. Airflow limitation and endothelial dysfunction. Unrelated and independent predictors of atherosclerosis. Am J Respir Crit Care Med. 2016;194(1):38–47. 10.1164/rccm.201510-2093OC [DOI] [PMC free article] [PubMed]
- 18.Engström G, Lampa E, Dekkers K, et al. Pulmonary function and atherosclerosis in the general population: causal associations and clinical implications. Eur J Epidemiol. 2024;39(1):35–49. 10.1007/s10654-023-01088-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Balla T. Phosphoinositides: tiny lipids with giant impact on cell regulation. Physiol Rev. 2013;93(3):1019–137. 10.1152/physrev.00028.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Koyasu S. The role of PI3K in immune cells. Nat Immunol. 2003;4(4):313–9. 10.1038/ni0403-313. [DOI] [PubMed] [Google Scholar]
- 21.Linton MF, Moslehi JJ, Babaev VR. Akt signaling in macrophage polarization, survival, and atherosclerosis. Int J Mol Sci. 2019;20(11):2703. 10.3390/ijms20112703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhao Y, Qian Y, Sun Z, et al. Role of PI3K in the progression and regression of atherosclerosis. Front Pharmacol. 2021;12: 632378. 10.3389/fphar.2021.632378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gupta V, Khan A, Higham A, et al. The effect of phosphatidylinositol-3 kinase inhibition on matrix metalloproteinase-9 and reactive oxygen species release from chronic obstructive pulmonary disease neutrophils. Int Immunopharmacol. 2016;35:155–62. 10.1016/j.intimp.2016.03.027. [DOI] [PubMed] [Google Scholar]
- 24.Finicelli M, Digilio FA, Galderisi U, Peluso G. The emerging role of macrophages in chronic obstructive pulmonary disease: the potential impact of oxidative stress and extracellular vesicle on macrophage polarization and function. Antioxidants (Basel). 2022;11(3):464. 10.3390/antiox11030464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barnes PJ. Inflammatory mechanisms in patients with chronic obstructive pulmonary disease. J Allergy Clin Immunol. 2016;138(1):16–27. 10.1016/j.jaci.2016.05.011. [DOI] [PubMed] [Google Scholar]
- 26.Murray PJ, Allen JE, Biswas SK, et al. Macrophage activation and polarization: nomenclature and experimental guidelines. Immunity. 2014;41(1):14–20. 10.1016/j.immuni.2014.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim GD, Lim EY, Shin HS. Macrophage polarization and functions in pathogenesis of chronic obstructive pulmonary disease. Int J Mol Sci. 2024;25(11):5631. 10.3390/ijms25115631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Durrant TN, Hers I. PI3K inhibitors in thrombosis and cardiovascular disease. Clin Transl Med. 2020;9(1):8. 10.1186/s40169-020-0261-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nunes-Santos CJ, Uzel G, Rosenzweig SD. PI3K pathway defects leading to immunodeficiency and immune dysregulation. J Allergy Clin Immunol. 2019;143(5):1676–87. 10.1016/j.jaci.2019.03.017. [DOI] [PubMed] [Google Scholar]
- 30.Cazzola M, Calzetta L, Rogliani P, Matera MG. Emerging anti-inflammatory COPD treatments: potential cardiovascular impacts. Int J Chron Obstruct Pulmon Dis. 2024;19:2481–95. 10.2147/COPD.S498255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cazzola M, Page CP, Calzetta L, Matera MG. Emerging anti-inflammatory strategies for COPD. Eur Respir J. 2012;40(3):724–41. 10.1183/09031936.00213711. [DOI] [PubMed] [Google Scholar]
- 32.Durrant TN, Hutchinson JL, Heesom KJ, et al. In-depth PtdIns(3,4,5)P3 signalosome analysis identifies DAPP1 as a negative regulator of GPVI-driven platelet function. Blood Adv. 2017;1(14):918–32. 10.1182/bloodadvances.2017005173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ghigo A, Laffargue M, Li M, Hirsch E. PI3K and calcium signaling in cardiovascular disease. Circ Res. 2017;121(3):282–92. 10.1161/CIRCRESAHA.117.310183. [DOI] [PubMed] [Google Scholar]
- 34.Rathinaswamy MK, Burke JE. Class I phosphoinositide 3-kinase (PI3K) regulatory subunits and their roles in signaling and disease. Adv Biol Regul. 2020;75: 100657. 10.1016/j.jbior.2019.100657. [DOI] [PubMed] [Google Scholar]
- 35.Marwick JA, Chung KF, Adcock IM. Phosphatidylinositol 3-kinase isoforms as targets in respiratory disease. Ther Adv Respir Dis. 2010;4(1):19–34. 10.1177/1753465809352792. [DOI] [PubMed] [Google Scholar]
- 36.Kulkarni S, Sitaru C, Jakus Z, et al. PI3Kβ plays a critical role in neutrophil activation by immune complexes. Sci Signal. 2011;4(168):ra23. 10.1126/scisignal.2001617 [DOI] [PubMed]
- 37.Aoyagi T, Matsui T. Phosphoinositide-3 kinase signaling in cardiac hypertrophy and heart failure. Curr Pharm Des. 2011;17(18):1818–24. 10.2174/138161211796390976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Van Eeden S, Leipsic J, Paul Man SF, Sin DD. The relationship between lung inflammation and cardiovascular disease. Am J Respir Crit Care Med. 2012;186(1):11–6. 10.1164/rccm.201203-0455PP. [DOI] [PubMed] [Google Scholar]
- 39.Kim HJ, Kim SR, Park JK, Kim DI, Jeong JS, Lee YC. PI3Kγ activation is required for LPS-induced reactive oxygen species generation in respiratory epithelial cells. Inflamm Res. 2012;61(11):1265–72. 10.1007/s00011-012-0526-7. [DOI] [PubMed] [Google Scholar]
- 40.Hawkins NM, Nordon C, Rhodes K, et al. Heightened long-term cardiovascular risks after exacerbation of chronic obstructive pulmonary disease. Heart. 2024;110(10):702–9. 10.1136/heartjnl-2023-323487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jo SH, Leblais V, Wang PH, Crow MT, Xiao RP. Phosphatidylinositol 3-kinase functionally compartmentalizes the concurrent Gs signaling during beta2-adrenergic stimulation. Circ Res. 2002;91(1):46–53. 10.1161/01.res.0000024115.67561.54. [DOI] [PubMed] [Google Scholar]
- 42.Zhabyeyev P, Chen X, Vanhaesebroeck B, Oudit GY. PI3Kα in cardioprotection: cytoskeleton, late Na+ current, and mechanism of arrhythmias. Channels (Austin). 2019;13(1):520–32. 10.1080/19336950.2019.1697127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ziegler R, Häusermann F, Kirchner S, Polonchuk L. Cardiac safety of kinase inhibitors—improving understanding and prediction of liabilities in drug discovery using human stem cell-derived models. Front Cardiovasc Med. 2021;8: 639824. 10.3389/fcvm.2021.639824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Horiguchi M, Oiso Y, Sakai H, Motomura T, Yamashita C. Pulmonary administration of phosphoinositide 3-kinase inhibitor is a curative treatment for chronic obstructive pulmonary disease by alveolar regeneration. J Control Release. 2015;213:112–9. 10.1016/j.jconrel.2015.07.004. [DOI] [PubMed] [Google Scholar]
- 45.Akinleye A, Avvaru P, Furqan M, Song Y, Liu D. Phosphatidylinositol 3-kinase (PI3K) inhibitors as cancer therapeutics. J Hematol Oncol. 2013;6(1):88. 10.1186/1756-8722-6-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fougerat A, Gayral S, Gourdy P, et al. Genetic and pharmacological targeting of phosphoinositide 3-kinase-γ reduces atherosclerosis and favors plaque stability by modulating inflammatory processes. Circulation. 2008;117(10):1310–7. 10.1161/CIRCULATIONAHA.107.720466. [DOI] [PubMed] [Google Scholar]
- 47.Siragusa M, Katare R, Meloni M, et al. Involvement of phosphoinositide 3-kinase gamma in angiogenesis and healing of experimental myocardial infarction in mice. Circ Res. 2010;106(4):757–68. 10.1161/CIRCRESAHA.109.207449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Doukas J, Wrasidlo W, Noronha G, et al. Phosphoinositide 3-kinase gamma/delta inhibition limits infarct size after myocardial ischemia/reperfusion injury. Proc Natl Acad Sci U S A. 2006;103(52):19866–71. 10.1073/pnas.0606956103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lanahan SM, Wymann MP, Lucas CL. The role of PI3Kγ in the immune system: new insights and translational implications. Nat Rev Immunol. 2022;22(11):687–700. 10.1038/s41577-022-00701-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wang C, Zhou J, Wang J, et al. Progress in the mechanism and targeted drug therapy for COPD. Signal Transduct Target Ther. 2020;5(1):248. 10.1038/s41392-020-00345-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vlahos R, Wark PA, Anderson GP, Bozinovski S. Glucocorticosteroids differentially regulate MMP-9 and neutrophil elastase in COPD. PLoS ONE. 2012;7(3): e33277. 10.1371/journal.pone.0033277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Doukas J, Eide L, Stebbins K, et al. Aerosolized phosphoinositide 3-kinase gamma/delta inhibitor TG100-115 [3-[2,4-diamino-6-(3-hydroxyphenyl)pteridin-7-yl]phenol] as a therapeutic candidate for asthma and chronic obstructive pulmonary disease. J Pharmacol Exp Ther. 2009;328(3):758–65. 10.1124/jpet.108.144311. [DOI] [PubMed] [Google Scholar]
- 53.Stockley JA, Walton GM, Lord JM, Sapey E. Aberrant neutrophil functions in stable chronic obstructive pulmonary disease: the neutrophil as an immunotherapeutic target. Int Immunopharmacol. 2013;17(4):1211–7. 10.1016/j.intimp.2013.05.035. [DOI] [PubMed] [Google Scholar]
- 54.Perry MWD, Björhall K, Bold P, et al. Discovery of AZD8154, a dual PI3Kγδ inhibitor for the treatment of asthma. J Med Chem. 2021;64(12):8053–75. 10.1021/acs.jmedchem.1c00434. [DOI] [PubMed] [Google Scholar]
- 55.Sadiq MW, Asimus S, Belvisi MG, et al. Characterisation of pharmacokinetics, safety and tolerability in a first-in-human study for AZD8154, a novel inhaled selective PI3Kγδ dual inhibitor targeting airway inflammatory disease. Br J Clin Pharmacol. 2022;88(1):260–70. 10.1111/bcp.14956. [DOI] [PubMed] [Google Scholar]
- 56.AdisInsight. AZD 8154. https://adisinsight.springer.com/drugs/800051370. Accessed 12 Jan 2025.
- 57.Erra M, Taltavull J, Gréco A, et al. Discovery of a potent, selective, and orally available PI3Kδ inhibitor for the treatment of inflammatory diseases. ACS Med Chem Lett. 2016;8(1):118–23. 10.1021/acsmedchemlett.6b00438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Li F, Liang X, Jiang Z, et al. Discovery of (S)-2-(1-(4-Amino-3-(3-fluoro-4-methoxyphenyl)-1H-pyrazolo[3,4-d]pyrimidin-1-yl)propyl)-3-cyclopropyl-5-fluoroquinazolin-4(3H)-one (IHMT-PI3Kδ-372) as a potent and selective PI3Kδ inhibitor for the treatment of chronic obstructive pulmonary disease. J Med Chem. 2020;63(22):13973–93. 10.1021/acs.jmedchem.0c01544. [DOI] [PubMed] [Google Scholar]
- 59.Down K, Amour A, Baldwin IR, et al. Optimization of novel indazoles as highly potent and selective inhibitors of phosphoinositide 3-kinase δ for the treatment of respiratory disease. J Med Chem. 2015;58(18):7381–99. 10.1021/acs.jmedchem.5b00767. [DOI] [PubMed] [Google Scholar]
- 60.Bruno P, Pala D, Micoli A, et al. Discovery of CHF-6523, an inhaled selective PI3Kδ inhibitor for the treatment of chronic obstructive pulmonary disease. J Med Chem. 10.1021/acs.jmedchem.4c02062. [DOI] [PubMed]
- 61.Govoni M, Bassi M, Girardello L, et al. CHF6523 data suggest that the phosphoinositide 3-kinase delta isoform is not a suitable target for the management of COPD. Respir Res. 2024;25(1):380. 10.1186/s12931-024-02999-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Yang H, He S, Liang L, Pan J. Efficacy of nemiralisib in chronic obstructive pulmonary disease: a systematic review. Clin Ther. 2024;46(4):360–7. 10.1016/j.clinthera.2024.02.008. [DOI] [PubMed] [Google Scholar]
- 63.Milara J, Lluch J, Almudever P, Freire J, Xiaozhong Q, Cortijo J. Roflumilast N-oxide reverses corticosteroid resistance in neutrophils from patients with chronic obstructive pulmonary disease. J Allergy Clin Immunol. 2014;134(2):314–22. 10.1016/j.jaci.2014.02.001. [DOI] [PubMed] [Google Scholar]
- 64.Sapey E, Stockley JA, Greenwood H, et al. Behavioral and structural differences in migrating peripheral neutrophils from patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2011;183(9):1176–86. 10.1164/rccm.201008-1285OC. [DOI] [PubMed] [Google Scholar]
- 65.Stark AK, Chandra A, Chakraborty K, et al. PI3Kδ hyper-activation promotes development of B cells that exacerbate Streptococcus pneumoniae infection in an antibody-independent manner. Nat Commun. 2018;9(1):3174. 10.1038/s41467-018-05674-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Scott J, Ruchaud-Sparagano MH, Musgrave K, et al. Phosphoinositide 3-kinase δ inhibition improves neutrophil bacterial killing in critically ill patients at high risk of infection. J Immunol. 2021;207(7):1776–84. 10.4049/jimmunol.2000603. [DOI] [PubMed] [Google Scholar]
- 67.Begg M, Hamblin JN, Jarvis E, et al. Exploring PI3Kδ molecular pathways in stable COPD and following an acute exacerbation, two randomized controlled trials. Int J Chron Obstruct Pulmon Dis. 2021;16:1621–36. 10.2147/COPD.S309303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gong GQ, Bilanges B, Allsop B, et al. A small-molecule PI3Kα activator for cardioprotection and neuroregeneration. Nature. 2023;618(7963):159–68. 10.1038/s41586-023-05972-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sadasivan C, Zhabyeyev P, Labib D, White JA, Paterson DI, Oudit GY. Cardiovascular toxicity of PI3Kα inhibitors. Clin Sci (Lond). 2020;134(19):2595–622. 10.1042/CS20200302. [DOI] [PubMed] [Google Scholar]
- 70.Chen X, Zhabyeyev P, Azad AK, et al. Pharmacological and cell-specific genetic PI3Kα inhibition worsens cardiac remodeling after myocardial infarction. J Mol Cell Cardiol. 2021;157:17–30. 10.1016/j.yjmcc.2021.04.004. [DOI] [PubMed] [Google Scholar]
- 71.Bewley MA, Belchamber KB, Chana KK, et al. Differential effects of p38, MAPK, PI3K or Rho kinase inhibitors on bacterial phagocytosis and efferocytosis by macrophages in COPD. PLoS ONE. 2016;11(9): e0163139. 10.1371/journal.pone.0163139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wang J, Zhu M, Wang L, Chen C, Song Y. Amphiregulin potentiates airway inflammation and mucus hypersecretion induced by urban particulate matter via the EGFR-PI3Kα-AKT/ERK pathway. Cell Signal. 2019;53:122–31. 10.1016/j.cellsig.2018.10.002. [DOI] [PubMed] [Google Scholar]
- 73.Bird JE, Smith PL, Bostwick JS, Shipkova P, Schumacher WA. Bleeding response induced by anti-thrombotic doses of a phosphoinositide 3-kinase (PI3K)-β inhibitor in mice. Thromb Res. 2011;127(6):560–4. 10.1016/j.thromres.2011.02.007. [DOI] [PubMed] [Google Scholar]
- 74.To Y, Ito K, Kizawa Y, et al. Targeting phosphoinositide-3-kinase-delta with theophylline reverses corticosteroid insensitivity in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2010;182(7):897–904. 10.1164/rccm.200906-0937OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Rossios C, To Y, Osoata G, Ito M, Barnes PJ, Ito K. Corticosteroid insensitivity is reversed by formoterol via phosphoinositide-3-kinase inhibition. Br J Pharmacol. 2012;167(4):775–86. 10.1111/j.1476-5381.2012.01864.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Li H, Wen X, Ren Y, et al. Targeting PI3K family with small-molecule inhibitors in cancer therapy: current clinical status and future directions. Mol Cancer. 2024;23(1):164. 10.1186/s12943-024-02072-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.FDA approves first treatment for activated phosphoinositide 3-kinase delta syndrome. https://www.fda.gov/drugs/news-events-human-drugs/fda-approves-first-treatment-activated-phosphoinositide-3-kinase-delta-syndrome. Accessed 12 Jan 2025.
- 78.Mozaffarian D, Afshin A, Benowitz NL, et al. Population approaches to improve diet, physical activity, and smoking habits: a scientific statement from the American Heart Association. Circulation. 2012;126(12):1514–63. 10.1161/CIR.0b013e318260a20b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hafezi-Moghadam A, Simoncini T, Yang Z, et al. Acute cardiovascular protective effects of corticosteroids are mediated by non-transcriptional activation of endothelial nitric oxide synthase. Nat Med. 2002;8(5):473–9. 10.1038/nm0502-473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Mujaj B, Bos D, Selwaness M, et al. Statin use is associated with carotid plaque composition: the Rotterdam Study. Int J Cardiol. 2018;260:213–8. 10.1016/j.ijcard.2018.02.111. [DOI] [PubMed] [Google Scholar]
- 81.German CA, Liao JK. Understanding the molecular mechanisms of statin pleiotropic effects. Arch Toxicol. 2023;97(6):1529–45. 10.1007/s00204-023-03492-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Song B, Hu J, Chen S, Zhang Y. The mechanisms and therapeutic implications of PI3K signaling in airway inflammation and remodeling in asthma. Biologics. 2025;19:73–86. 10.2147/BTT.S497622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Jiang R, Lou L, Shi W, et al. Statins in mitigating anticancer treatment-related cardiovascular disease. Int J Mol Sci. 2024;25(18):10177. 10.3390/ijms251810177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kloo B, Nagel D, Pfeifer M, et al. Critical role of PI3K signaling for NF-kappaB-dependent survival in a subset of activated B-cell-like diffuse large B-cell lymphoma cells. Proc Natl Acad Sci U S A. 2011;108(1):272–7. 10.1073/pnas.1008969108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ghigo A, Damilano F, Braccini L, Hirsch E. PI3K inhibition in inflammation: toward tailored therapies for specific diseases. BioEssays. 2010;32(3):185–96. 10.1002/bies.200900150. [DOI] [PubMed] [Google Scholar]
- 86.Morello F, Perino A, Hirsch E. Phosphoinositide 3-kinase signalling in the vascular system. Cardiovasc Res. 2009;82(2):261–71. 10.1093/cvr/cvn325. [DOI] [PubMed] [Google Scholar]
- 87.Fruman DA, Chiu H, Hopkins BD, Bagrodia S, Cantley LC, Abraham RT. The PI3K pathway in human disease. Cell. 2017;170(4):605–35. 10.1016/j.cell.2017.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cazzola M, Cavalli F, Usmani OS, Rogliani P. Advances in pulmonary drug delivery devices for the treatment of chronic obstructive pulmonary disease. Expert Opin Drug Deliv. 2020;17(5):635–46. 10.1080/17425247.2020.1739021. [DOI] [PubMed] [Google Scholar]
- 89.Marlevi D, Edelman ER. Vascular lesion-specific drug delivery systems: JACC state-of-the-art review. J Am Coll Cardiol. 2021;77(19):2413–31. 10.1016/j.jacc.2021.03.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Campa CC, Silva RL, Margaria JP, et al. Inhalation of the prodrug PI3K inhibitor CL27c improves lung function in asthma and fibrosis. Nat Commun. 2018;9(1):5232. 10.1038/s41467-018-07698-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Fergusson AD, Zhang R, Riffle JS, Davis RM. Encapsulation of PI3K inhibitor LY294002 within polymer nanoparticles using ion pairing flash nanoprecipitation. Pharmaceutics. 2023;15(4):1157. 10.3390/pharmaceutics15041157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Mülhopt S, Diabaté S, Dilger M, et al. Characterization of nanoparticle batch-to-batch variability. Nanomaterials (Basel). 2018;8(5):311. 10.3390/nano8050311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Cazzola M, Rogliani P, Barnes PJ, et al. An update on outcomes for COPD pharmacological trials: a COPD investigators report—reassessment of the 2008 American Thoracic Society/European Respiratory Society statement on outcomes for COPD pharmacological trials. Am J Respir Crit Care Med. 2023;208(4):374–94. 10.1164/rccm.202303-0400SO. [DOI] [PubMed] [Google Scholar]
- 94.Della Corte V, Todaro F, Cataldi M, Tuttolomondo A. Atherosclerosis and its related laboratory biomarkers. Int J Mol Sci. 2023;24(21):15546. 10.3390/ijms242115546. [DOI] [PMC free article] [PubMed] [Google Scholar]