Abstract
Background
People who undergo lumbar spine surgery experience variable pain, disability, and quality of life outcomes. Mindfulness-based interventions (MBIs) are recommended for chronic low back pain and may be an effective approach for surgical patients.
Objectives
Evaluate the feasibility and acceptability of a telehealth MBI following lumbar spine surgery and refine the intervention for optimal delivery.
Methods
This was a prospective, mixed-methods, single-arm cohort study with measurements preoperatively and 2 weeks and 3 months postoperatively. Participants were adults undergoing lumbar spine surgery for a degenerative condition at an academic medical center. A telehealth MBI was delivered one-on-one within 4 weeks after surgery and consisted of 8 weekly sessions modeled after Mindfulness-Based Cognitive Therapy for Chronic Pain. Outcomes were feasibility (enrollment rate, retention, session attendance, homework completion), acceptability (intervention satisfaction questionnaire and exit interview); and pre- to 3-month postoperative improvements in patient-reported disability, pain, and psychosocial factors including depression, anxiety, pain catastrophizing, kinesiophobia, self-efficacy, perceived stress, and dispositional mindfulness.
Results
Fifteen participants who received a laminectomy (n = 3) or fusion with (n = 9)/without (n = 3) laminectomy initiated the MBI. Enrollment (35%) and retention (80%) rates were lower than hypothesized, but participants had high levels of session attendance (80% completed) and home practice (median = 95% days assigned). The MBI was perceived as highly acceptable on the satisfaction questionnaire and exit interviews. Most participants reported improvements at or above established minimal clinically important differences for disability and pain at 3 months postoperatively and improvements in most psychosocial factors. Themes from exit interviews informed future modifications to the intervention.
Conclusions
Delivery of an 8-session, one-on-one, telehealth MBI to patients after lumbar spine surgery is feasible and acceptable and patients perceive meaningful benefits to their surgical recovery from the MBI. Results support fully powered randomized controlled trials to determine longer-term post-surgical effects of the MBI.
Keywords: mindfulness, spine surgery, psychosocial intervention, chronic pain, post-surgical pain, telemedicine
Introduction
People who undergo lumbar spine surgery experience variable pain, disability, and quality of life outcomes.1-3 Rehabilitation interventions targeting psychosocial risk factors after lumbar spine surgery result in improved pain and mental and physical functioning compared with exercise or education alone. 4 These psychosocial-based rehabilitation trials involved in-person interventions and/or drew from traditional cognitive behavioral therapy for chronic pain.5-7 Although effective for some patients, not all patients achieve benefit from cognitive behavioral therapy. In qualitative studies, emotional factors have been described as salient experiences before and after spine surgery8,9 and patients identified a need for more nonpharmacological postoperative pain management strategies. 8
Mindfulness-based interventions (MBIs) are recommended as first-line nonpharmacological treatment for chronic low back pain and may be an effective approach for surgical patients. 10 Standardized MBIs including Mindfulness-Based Stress Reduction and its adapted protocols involve skills to self-regulate one’s attention to present-moment body sensations, thoughts and emotions with less reactivity and greater acceptance. 11 MBIs have traditionally been offered as in-person, group-based interventions with 8 weekly sessions lasting 2 to 2.5 hours each. 11 This format is impractical for patients who live long distances from a surgical center and may have difficulty driving after a complex surgical spine procedure. Both telehealth- and individually-delivered MBIs are feasible and efficacious in chronic pain populations.12-15 In addition, a study that directly compared a group-delivered to an individual-delivered mindfulness-based cognitive therapy intervention in patients with depression and a chronic somatic disease indicated that both were similarly effective in improving psychological well-being outcomes. 16 Therefore, an individually delivered, telehealth MBI is a promising alternative for patients after spine surgery.
While MBIs have demonstrated efficacy for managing chronic low back pain, the concerns specific to the spine surgery population may differ. Patients in this group face acute postsurgical pain, which may coexist with pre-existing pain and/or new pains that emerge postoperatively. 17 Patients have to balance post-operative physical activity restrictions with guidance to gradually build their activity levels. Qualitative research indicates that patients experience fears after surgery specific to falling, reinjury, and worsening pain. 9 Studies indicate that early postoperative psychosocial factors—such as fear of movement, pain-related anxiety, and pain catastrophizing—are strong predictors of pain and disability outcomes 6 to 12 months following lumbar spine surgery.3,18,19 MBIs have been shown to reduce pain catastrophizing in patients with chronic pain in non-surgical contexts.20,21 Mechanistic reviews suggest that mindfulness meditation can alter pain perception by enhancing attentional flexibility and sensory processing, including exposure to painful sensations, while diminishing cognitive and emotional evaluations of those sensations.22-24 Implementing an MBI during the postoperative period could potentially address the psychological mechanisms contributing to persistent pain and disability after lumbar spine surgery. However, such interventions may need to be specifically tailored to the unique challenges faced by patients recovering from spine surgery.
The objectives of this prospective, mixed-methods, single-arm cohort study were to evaluate the feasibility and acceptability of an 8-week telehealth MBI delivered one-on-one to patients following lumbar spine surgery and to refine the intervention as needed for this population. Feasibility benchmarks were enrolling 50% of patients approached for participation, retaining 90% of participants who initiated the intervention, and averaging 75% MBI session attendance and home practice completion. The acceptability benchmark was 80% of participants reporting satisfaction with the MBI. Potential clinical promise of the intervention was evaluated with pre- to post-intervention change and percentage of participants achieving clinically meaningful improvements in patient-reported disability, pain and psychosocial factors. Results from this study will have direct implications for the refinement of MBIs for patients recovering from spine surgery.
Methods
Participants
Participants were adults aged 18 and older who were scheduled for their first lumbar spine surgery due to a degenerative condition (including but not limited to, spinal stenosis, spondylosis with or without myelopathy, and spondylolisthesis) at a single academic spine center. Additional inclusion criteria were: (1) radiographic evidence of compression of cauda equina or nerve roots by degenerative changes; (2) presence of back and/or lower extremity pain persisting for at least 3 months, and (3) access to stable internet. Exclusion criteria were: (1) microsurgical technique as the primary procedure (ie, isolated laminotomy or microdiscectomy); (2) having surgery for the primary indication of a spinal deformity; (3) having surgery secondary to pseudarthrosis, trauma, infection, or tumor; (4) history of a psychotic disorder or hospitalization for reasons related to psychosis; (5) diagnosis of Alzheimer’s disease or another form of dementia; (6) traumatic brain injury greater than mild severity; (7) history of bipolar disorder or dissociative disorder; (8) active substance use disorder (in past month); and (9) symptoms in the past month indicating likely posttraumatic stress disorder (PTSD) diagnosis. Patients with these psychiatric conditions may require substantially adapted mindfulness programs and concurrent psychotherapy to prevent adverse experiences during mindfulness meditation practice such as dissociation, flashbacks or panic attacks.25,26
Procedures
The Vanderbilt University Institutional Review Board approved all study procedures. The research coordinator identified participants in collaboration with the treating surgeon through review of the electronic medical record and surgery schedule. Written informed consent to participate in eligibility screening and the study was obtained electronically 27 after discussion with the research coordinator at the preoperative clinic visit or preoperatively over the phone.
Self-report questionnaires were emailed to participants via Research Electronic Data Capture (REDCap)28-30 survey links preoperatively and 2 weeks (pre-intervention) and 3 months following surgery (post-intervention). After the 3-month survey, participants completed a 30-minute semi-structured exit interview over the phone. Two study investigators with qualitative research experience (CEB/BR) who did not deliver the intervention conducted interviews. Adverse events were not systematically assessed but were recorded and monitored if reported.
Measures
Sociodemographic information and current opioid use status were collected from participants via REDCap prior to undergoing spine surgery and included age, sex, race, ethnicity, education, marital status, and employment. Information regarding surgical characteristics including degenerative spine diagnosis, surgical procedure, and number of spinal levels operated on, as well as comorbid psychiatric conditions was obtained from the electronic medical record.
Feasibility
Data were collected regarding enrollment, retention, session attendance, and homework completion. The study interventionist assessed homework completion at the beginning of each telehealth session as the number of days on which mindfulness practice occurred since the previous session.
Acceptability
Intervention satisfaction was measured with a 9-item survey (Supplemental Appendix 1) assessing participants’ overall satisfaction with the MBI, likelihood of recommending it to a friend, and the importance of the program to changes in pain, emotional well-being and physical well-being. Semi-structured exit interviews (Supplemental Appendix 2) inquired about participants’ overall impression of the program, each intervention component, and perceived benefits, as well as recommendations to improve the program.
Patient-Reported Clinical Outcomes
Disability was measured with the 10-item Oswestry Disability Index (ODI) assessing how much one’s back and/or leg pain have affected the ability to manage everyday life activities. 31 Back pain and leg pain intensity when not on pain medication or after pain medication had worn off over the past 7 days were assessed with an 11-item Numeric Rating Scale ranging from 0 (no pain) to 10 (worst imaginable pain). 32 Pain Bothersomeness over the past 7 days was measured with a scale from 0 (not at all bothersome) to 4 (extremely bothersome). 33
Pain interference, depression, and anxiety were measured with Patient-Reported Outcomes Measurement Information System (PROMIS) 34 scales including Pain Interference Short-form 4a, Depression Short-form 4a, and Anxiety Short-form 4a. PROMIS measures have previously been validated in spine surgery populations. 35 Each scale is scored by converting the raw score into a standardized T-score with a mean of 50 and a standard deviation of 10 based on a general or reference population.
Kinesiophobia, which refers to the level of pain-related fear of movement and physical activity and the belief that pain always signifies a serious medical issue was measured with the 13-item Tampa Scale of Kinesiophobia (TSK-13). 36 The 13-item Pain Catastrophizing Scale (PCS) 37 measured the tendency to experience pain-related cognitions including helplessness, magnification, and rumination. One’s confidence in the ability to engage in activities and achieve goals despite pain was measured with the Pain Self-Efficacy Questionnaire (PSEQ). 38 Perceived stress over the past month was measured with the 4-item Perceived Stress Scale (PSS-4). 39 Dispositional [ie, trait] mindfulness, defined as the general tendency to be aware of present-moment experiences without judgment in daily life, was measured with the 15-item Five Facet Mindfulness Questionnaire (FFMQ-short form) assessing aspects of mindfulness in daily life including observing, describing, acting with awareness, non-judgment, and non-reactivity. 40
Intervention
The MBI was initiated with patients within 4 weeks after surgery and consisted of eight, weekly one-on-one sessions with a study interventionist. Sessions were delivered over HIPAA-compliant Zoom and audio-recorded. The first session was 90 minutes and sessions 2-8 were 75-minute. The intervention was modeled after the manualized Mindfulness-Based Cognitive Therapy (MBCT) for Chronic Pain. 41 MBCT was originally developed for preventing relapse of depression 42 and has since been adapted and tested in chronic pain populations, including chronic low back pain and headache pain.43,44 The MBCT for Chronic Pain manual 41 tailors the MBCT program for individuals with chronic pain by incorporating pain-specific education and by applying mindfulness skills to chronic pain coping. Educational components include the Gate-Control Theory of Pain to explain how cognitions, emotions, and behaviors modulate pain perception; understanding the relationship between stress and pain; identifying common thinking patterns in chronic pain and their impact on emotions, behaviors and sensations; and the role of acceptance in coping with pain. Mindfulness practices, both guided and un-guided, are taught to train individuals to both regulate their attention to non-painful sensations as well as to approach painful sensations with acceptance, reducing cognitive and emotional reactivity. There is also a focus on awareness of pain-related cognitions during meditation and daily life, enabling conscious responses to pain rather than habitual reactions. MBCT for Chronic Pain is typically delivered in-person and in groups but was modified by the research team for one-on-one telehealth delivery, with terminology and discussion prompts tailored for postsurgical pain and recovery. For example, discussions after guided meditation focused on applying mindfulness skills to acute, post-surgical pain and to daily routine movement and activities prescribed by the treating surgeon or physical therapist. Activity pacing (alternating between activity and rest) was added to help participants manage pain with increasing activity levels over the course of surgical recovery. Each session included didactic information introduced interactively, a mindfulness skill with discussion, and review of previous skills (Supplemental Table 1).
Participants were asked to complete home practice 6 days per week, including: (1) One to two guided meditation practices per day (eg, body scan; mindfulness of breath; mindful movement; mindfulness of sounds and thoughts); (2) informal practices like mindfully attending to routine daily activities (eg, eating, brushing teeth) and to daily movement (eg, walking, prescribed home exercises); (3) Scheduling the 3-minute breathing space daily as well as practicing the breathing space during moments of pain or difficulty; and (4) Cognitive and behavioral assignments such as completing pleasant and unpleasant experiences logs and trying activity pacing. Home practice assignments varied weekly based on session content, and from session 6 onwards, participants could choose any guided practices. All participants received a manual with session handouts, daily home practice logs, and audio recordings of guided mindfulness practices.
Interventionists were four postgraduate-level mental health clinicians who participated in a 44-hour Professional Development in Mindfulness Facilitation workshop and a 45-hour MBCT teacher-training intensive. Interventionists received training in the intervention manual through weekly meetings for three months with two investigators trained in mindfulness facilitation (CEB/MP) and through role-plays and mock sessions with feedback.
Statistical Analyses
Descriptive statistics were calculated to characterize the study sample and report feasibility and acceptability outcomes, as well as the percentage of participants achieving a minimal clinically important difference (MCID) in pain and disability. A MCID in disability, back and leg pain intensity and pain bothersomeness was defined as achieving at least 30% reduction in score from pre-surgery to 3 months post-surgery,33,45 while PROMIS Pain Interference was defined as a reduction of at least 3.5 T-score points. 46 Participants who reported scores of 0 at the preoperative time point were excluded when calculating the percentage achieving MCID. Paired t-tests were conducted to examine within-participant change from pre-surgery to 3 months post-surgery for each patient-reported measure of pain, disability, and psychosocial factors. Results are reported in supplemental tables as the mean (SD) at each time-point (pre-surgery, 2 weeks post-surgery and 3 months post-surgery) and as mean differences from pre-surgery to 3 months post-surgery with standard deviations, 95% confidence intervals (CIs) around the differences, and Hedge’s g effect sizes (ie, Cohen’s d standardized effect size with a correction for small sample sizes). Spaghetti plots to display individual differences in pain and disability outcomes at pre-surgery and 3 months post-surgery are shown in supplemental figures.
Exit interviews were audio-recorded and transcribed with a transcription service (rev.com) and verified before analysis. Qualitative analyses were conducted in Dedoose. 47 Two investigators (CEB/ELC) read the first two interviews and developed an initial codebook based on the interview guide and initial read-through. The same two independent coders met after coding every 3 additional interviews to discuss and revise the codebook as needed until all interviews were coded. Where applicable, codes were given a weight (+1, 0, −1) to indicate if a perception of an intervention component was positive (ie, helpful), negative (ie, unhelpful), or neutral (ie, neither helpful nor unhelpful). The quantity of positive, neutral, and negative perceptions of the overall program and its individual components were calculated and are presented in bar graphs as a method of visualizing the acceptability of the intervention. Through discussions, the same two investigators identified themes in the data regarding participant experiences with the MBI and suggestions to improve it, with the objective of refining the MBI as needed to optimize future trials. A separate manuscript will present results of a more in-depth analysis of the qualitative exit interviews with a focus on potential MBI mechanisms contributing to patient-reported benefits.
Results
Participants
Fifteen participants initiated the postsurgical MBI and were 47% female, mean age 56 years (SD = 17), 87% identified as White race, and 60% reported having at least a 4-year college degree (Table 1). The most common diagnosis was lumbar stenosis (47%), with most participants (60%) having a laminectomy with fusion and 1 spinal level operated on (60%). One adverse event (infection) that was related to surgery but unrelated to the study intervention or procedures was reported. At preoperative baseline, on average, participants reported having moderate levels of back pain intensity (M = 6.58, SD = 1.51), leg pain intensity (M = 4.17, SD = 2.86), and pain interference (M = 68.20, SD = 4.90), and severe disability (M = 43.65, SD = 14.10). Average baseline levels of depression (M = 53.18, SD = 6.08) and anxiety (M = 56.95, SD = 7.53) were within normal to mild levels, respectively. Baseline scores on all measures are shown in Supplemental Tables 2 and 3).
Table 1.
Baseline Demographic and Surgical Characteristics (N = 15, Includes Participants Who Initiated the Postoperative Mindfulness-Based Intervention).
| Variable | N (%) or M (SD), Range |
|---|---|
| Age | 55.7 (17.2), 30 - 77 |
| Sex | |
| Female | 7 (46.7%) |
| Male | 8 (53.3%) |
| Ethnicity | |
| Hispanic/Latino | 0 (0.00%) |
| Not Hispanic/Latino | 15 (100.0%) |
| Race | |
| White | 13 (86.7%) |
| Black/African American | 1 (6.7%) |
| Other | 1 (6.7%) |
| Education | |
| High School/GED | 3 (20.0%) |
| Two-year college degree | 3 (20.0%) |
| Four-year college degree | 5 (33.3%) |
| Post-college | 4 (26.7%) |
| Marital Status | |
| Single/Widower | 0 (0.0%) |
| Married | 11 (73.3%) |
| Divorced | 1 (6.7%) |
| Living with partner | 3 (20.0%) |
| Employment | |
| Currently working | 5 (33.3%) |
| Short-term disability or leave | 2 (13.3%) |
| Unemployed | 6 (40.0%) |
| Attending school | 1 (6.7%) |
| Unknown/not reported | 1 (6.7%) |
| Current preoperative opioid use | |
| No | 15 (100%) |
| Yes | 0 (0%) |
| Primary lumbar degenerative spine diagnosis | |
| Spinal Stenosis | 7 (46.7%) |
| Spondylosis | 1 (6.7%) |
| Degenerative Spondylolisthesis | 2 (13.3%) |
| Isthmic spondylolisthesis | 3 (20.0%) |
| Other | 2 (13.3%) |
| Surgical procedure performed | |
| Laminectomy without fusion | 3 (20.0%) |
| Laminectomy with fusion | 9 (60.0%) |
| Fusion only | 3 (20.0%) |
| Number of spinal levels operated | |
| 1 | 9 (60.0%) |
| 2 | 3 (20.0%) |
| 3 | 2 (13.3%) |
| >3 | 1 (6.7%) |
| Psychiatric Diagnosis (per electronic medical record) a | 5 (33.3%) |
aDiagnoses present included depressive disorders, anxiety disorders, and ADHD.
Feasibility
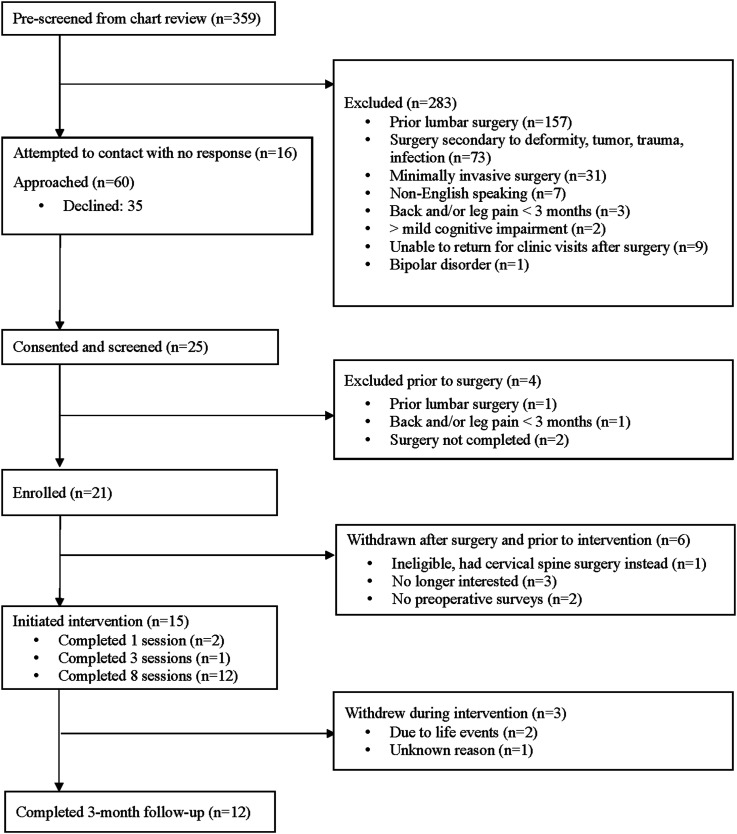
Sixty patients were approached during recruitment, 25 (42% of approached) consented and completed screening, and 21 (35% of approached) were enrolled prior to surgery. After surgery, 6 participants were ineligible or withdrawn; thus, 15 initiated the postoperative MBI and 12 (80%) completed 3-month follow-up. Three participants who withdrew from the study prior to completing the intervention attended fewer than 75% of sessions. Reported reasons for discontinuing the intervention included time constraints due to unexpected life events (n = 2) and for unknown reason (n = 1). The remaining 12 participants completed all 8 sessions (Figure 1).
Figure 1.
Flow diagram.
Eleven participants had complete home practice data. Participants reported practicing any of the assigned mindfulness skills on a median of 95.2% of days assigned (interquartile range [IQR] = 28.0, range 56.5% to 102.6%), and a median of 5.7 days per week (IQR = 1.5, range 3.4 to 6.3). Some participants reported practicing 7 days in a week (instead of the assigned 6), and in some instances reported practicing for more than 7 days if scheduling conflicts or illness resulted in two weeks elapsing between sessions. Consequently, the range included greater than 100% of days assigned. Participants’ reported total number of days practicing each of the mindfulness skills were as follows: Body Scan meditation (M = 16.82 [SD = 4.09], range 10-22); Informal mindfulness during a routine daily activity (M = 9.73 [SD = 3.10], range 4-15); Guided sitting meditations, including any combination of mindfulness of breath, body, sounds, thoughts, and difficulty (M = 25.73 [SD = 5.93], range 13-36); Mindful movement and/or walking (M = 13.00 [SD = 7.10], range 1-23); Scheduled 3-minute breathing space (M = 23.36 [SD = 10.26], range 9-38); Responsive 3-minute breathing space (M = 11.27 [SD = 7.85], range 0-26).
Acceptability
On the satisfaction questionnaire, most participants (92%) rated the overall helpfulness and the likelihood of recommending the mindfulness program to a friend at least 7 on a scale of 1 to 10 (Table 2). Most participants reported that the benefits of the program outweighed the effort put in (82%), the importance of the program to surgical recovery was as or more important compared to other services received (92%), and the program led to meaningful improvements in pain bothersomeness (67%), physical well-being (83%) and emotional well-being (92%). Fewer participants felt that the program led to meaningful reductions in pain intensity (42%) or the need to take pain medications (42%).
Table 2.
Intervention Satisfaction Questionnaire Responses and Bivariate Correlations Between Item Response and Number of Neutral/Negatively Coded Exit Interview Perceptions (N = 12).
| Item | N (%) | Spearman’s Rank Correlations (Rho, 2-tailed P-value) |
|---|---|---|
| Overall helpfulness of program to surgical recovery (1-10) | −0.69, P = .01 | |
| 3 out 10 | 1 (8%) | |
| 7 out of 10 | 2 (17%) | |
| 8 out of 10 | 5 (42%) | |
| 10 out of 10 | 4 (33%) | |
| Likelihood of recommending program to a friend (1-10) | −0.77, P = .003 | |
| 3 out 10 | 1 (8%) | |
| 7 out of 10 | 1 (8%) | |
| 8 out of 10 | 1 (8%) | |
| 9 out of 10 | 2 (17%) | |
| 10 out of 10 | 7 (60%) | |
| Overall benefit of program taking into account effort (1-5) | −0.46, P = .13 | |
| 1, The effort far outweighed the benefits | 0 (0%) | |
| 2, The effort somewhat outweighed the benefits | 0 (0%) | |
| 3, The benefits equaled the effort | 2 (17%) | |
| 4, The benefits somewhat outweighed the effort | 1 (8%) | |
| 5, The benefits far outweighed the effort | 9 (75%) | |
| Importance of program to recovery compared to other services received (1-5) | −0.40, P = .20 | |
| 1, Much less important | 0 (0%) | |
| 2, Somewhat less important | 1 (8%) | |
| 3, As important | 2 (17%) | |
| 4, Somewhat more important | 2 (17%) | |
| 5, Much more important | 7 (58%) | |
| Importance of program to any changes in need to take pain medications (1-5) | −0.22, P = .50 | |
| 1, Increased a meaningful amount | 0 (0%) | |
| 2, Some increase, but not enough to be meaningful | 0 (0% | |
| 3, No change | 6 (50%) | |
| 4, Some decrease, but not enough to be meaningful | 1 (8%) | |
| 5, Decreased a meaningful amount | 5 (42%) | |
| Importance of program to any changes in pain intensity (1-5) | −0.28, P = .37 | |
| 1, Increased a meaningful amount | 0 (0%) | |
| 2, Some increase, but not enough to be meaningful | 0 (0%) | |
| 3, No change | 5 (42%) | |
| 4, Some decrease, but not enough to be meaningful | 2 (17%) | |
| 5, Decreased a meaningful amount | 5 (42%) | |
| Importance of program to any changes in pain bothersomeness (1-5) | −0.32, P = .31 | |
| 1, Increased a meaningful amount | 0 (0%) | |
| 2, Some increase, but not enough to be meaningful | 1 (8%) | |
| 3, No change | 1 (8%) | |
| 4, Some decrease, but not enough to be meaningful | 2 (17%) | |
| 5, Decreased a meaningful amount | 8 (67%) | |
| Importance of program to any changes in physical well-being (1-5) | −0.55, P = .06 | |
| 1, Decreased a meaningful amount | 0 (0%) | |
| 2, Some decrease, but not enough to be meaningful | 1 (8%) | |
| 3, No change | 0 (0%) | |
| 4, Some increase, but not enough to be meaningful | 1 (8%) | |
| 5, Increased a meaningful amount | 10 (83%) | |
| Importance of program to any changes in emotional well-being (1-5) | −0.37, P = .23 | |
| 1, Decreased a meaningful amount | 0 (0%) | |
| 2, Some decrease, but not enough to be meaningful | 0 (0%) | |
| 3, No change | 0 (0%) | |
| 4, Some increase, but not enough to be meaningful | 1 (8%) | |
| 5, Increased a meaningful amount | 11 (92%) |
Semi-Structured Exit Interviews
Perceived Benefits of the MBI
All participants reported that the MBI was beneficial for at least one aspect of their postsurgical recovery and/or general well-being. Over half of participants reported that the MBI provided tools to either manage or cope with postsurgical pain. For example, some shared that the skills improved their ability “to set it [pain] aside” (pt 21) or to attend to pain sensations such that they could reframe their thoughts about or reactions to the pain. Many participants described how the program was beneficial for addressing difficult emotions after surgery, including depression, anxiety, stress, fear of movement and reinjury, guilt around social role limitations, and frustration about activity limitations. One participant described being “super anxious” about movement after surgery and shared that the mindfulness practices were “just really helpful for kind of dispelling some of that anxiety within” (pt 10).
Perceptions of MBI Program Components
Most participants (75%) reported that the number of sessions and the length of sessions was just right. All 12 participants reported positive perceptions of the telehealth format, with 3 (25%) also reporting sound challenges or difficulty finding an uninterrupted space to participate. Six out of 11 participants (55%) would have considered the option to participate in the MBI in a group format, whereas 5 participants stated they would not.
Perceptions of each mindfulness skill and cognitive/behavioral component were largely coded as positive (Figure 2(A) and (B)). Of the twelve participants, six (50%) had all positively coded interview excerpts, with no neutral or negatively coded excerpts. The remaining six participants (50%) had at least one neutral and/or negatively coded excerpt. The distribution of the combined number of neutral and negatively coded excerpts per participant was as follows: 1 excerpt (n = 1), 3 excerpts (n = 1), 4 excerpts (n = 1), 5 excerpts (n = 2), and 6 excerpts (n = 1). In a post-hoc analysis, we examined whether the number of neutral or negatively coded excerpts was correlated with participants’ responses on each of the nine satisfaction questionnaire items, using Spearman’s rank non-parametric correlations. The results showed large, negative correlations with ratings of overall helpfulness of the program (rho = −0.69, P = .01) and with the likelihood of recommending the program to a friend (rho = −0.77, P = .003). Additionally, there were small to moderate negative correlations with other items (Table 2). These findings suggest that having a higher number of neutral or negatively coded perceptions of individual MBI components in exit interviews was associated with lower satisfaction ratings on the questionnaire.
Figure 2.
(A) perceptions of program and mindfulness skills from exit interviews (N = 12). (B) Perceptions of didactic and cognitive/behavioral components from exit interviews (N = 12).
Intervention Modification
Themes and suggestions were identified to inform intervention modifications (Table 3) and included: (1) Too much home practice during the latter part of the program, (2) Pain management component of program not relevant to everyone, (3) More explanation of program and practice objectives needed, and (4) More emphasis on mindful movement components.
Table 3.
Qualitative Exit Interview Themes and Future Intervention Modifications or Research Considerations.
| Theme/s | Illustrative Quote/s | Intervention Modifications or Considerations for Future Research |
|---|---|---|
| Too much home practice during the latter part of the program | “Before I got back to work, it [home mindfulness practice] gave some structure to my day because otherwise it was just laying on the couch all day long… You can get listless. You can get depressed, all these things, and having it provide some structure to my day was, for me, really healthy. Then by the time I got back to work, it did get a little bit more difficult fitting in time to do that because all of a sudden I’m very busy” (Pt 01) | Modifications: |
| • Reductions in home practice amounts throughout (eg, alternating days instead of two audio-guided practices per day) | ||
| • Greater emphasis in 2nd half of program on individual tailoring of home practice assignments and on integrating mindfulness into daily movement, physical therapy home exercises, moments of pain or stress, and other activities | ||
| Pain management component of program not relevant to everyone | “By two weeks my pain was gone, and I think that’s when you started it about, and so I wasn’t dealing with pain…It wasn’t a pain relief study for me because of my situation. What I had said to [interventionist name] was I would’ve loved that study three weeks pre-surgery and five weeks post-surgery after two weeks or so till you’re ready to do it.” (Pt 12) | Modifications: |
| • If participant reports little to no pain, apply skills to other aspects of surgical recovery (eg, stress/emotional reactions, fear of movement, bodily awareness) and to managing potential future pains | ||
| Considerations for future research: | ||
| • Compare varied timing of program delivery (eg, preoperative, postoperative, spanning pre- to post-operative); determine who benefits most from specific timing | ||
| More explanation of program and practice objectives needed | “I would say the only negative thing about the program was the very first day probably could have spent a little more time actually emphasizing what the goals in this program were. Cause I didn’t understand it until maybe the third or fourth session. Then I realized, oh, this is the object of this. So yeah, if I could have understood it a little bit sooner, I probably would’ve gotten a little more out of the program. (Pt 03) | Modifications: |
| • Session 1: Provide clearer and more detailed explanation of the scientific rationale and the purpose of the MBI for surgical recovery | ||
| “I guess, maybe, a definition of the object of each practice ahead of time would help…if you identify the practice and give the purpose for the practice, as opposed to just doing the practice first, it might make it easier to understand.” (Pt 03) | • Include themes for each session in manual, integrated into discussions by interventionist | |
| • Provide clear objective of each new mindfulness skill and how it builds on previous skills before guiding in session | ||
| More emphasis on mindful movement components | “I thought that [mindful movement and walking] was really good. Very good. I think we could have done more with it in the program…Obviously mobility is so important, I think, for reducing pain and everything.” (Pt 12) | Modifications: |
| “I think that one [mindful movement] would be more useful, I think presented maybe a little earlier on.” (pt 10) | • Introduce mindful movement and activity pacing skills earlier in the program (sessions 3 & 4 instead of 5 & 7, respectively | |
| “I remember going over that one [activity pacing] briefly. It didn’t stick. I remember doing it, but it didn’t stick with as something that I’m currently using.” (pt 02) | • Deliver guided mindful movement or walking skills during 4 sessions instead of 3 sessions | |
| • Increased integration of mindful movement and activity pacing skills during discussions and in tailoring of home practice assignments. |
Close to half (42%) of participants reported there was too much assigned home practice, especially after returning to work or activity, whereas 2 participants (17%) thought there was not enough. Several participants shared that they were experiencing very little pain at the start of the MBI and thus the pain-management component of the program was less relevant to them, although they found the MBI beneficial for other aspects of recovery. Those participants reported that they might have preferred having several of the sessions before surgery or starting the program within 1 week after surgery.
Two participants expressed that the purpose of the program was not clear and that they may have obtained more benefit had they understood the purpose earlier. Some participants did not understand the objective of each individual mindfulness skill prior to practicing it in session. Some participants thought that the mindful movement, mindful walking, and activity pacing skills could have been introduced earlier in the program and emphasized more than they were.
Improvement in Self-Reported Pain, Disability, and Psychosocial Measures
There were significant within-subject improvements with large effect sizes from preoperatively to 3-month follow-up for pain and disability outcomes (Supplemental Table 2) and most psychosocial factors, except for perceived stress and dispositional mindfulness (Supplemental Table 3). The percentage of participants achieving MCID ranged from 75% for the ODI and back pain intensity to 92% for pain bothersomeness (Supplemental Table 2). Spaghetti plots displaying individual participant scores on pain and disability outcomes at preoperative baseline and 3-month follow-up are shown in Supplemental Figures 1-5.
Discussion
This study evaluated the feasibility, acceptability, and potential clinical promise of an 8-week telehealth MBI delivered one-on-one to patients following lumbar spine surgery. Utilizing both quantitative and qualitative methods facilitated collection of key feasibility and acceptability outcomes to inform a future intervention trial. 48 Enrollment and retention rates were lower than expected benchmarks of 50% and 90%, respectively; however, session attendance and home practice completion were higher than the expected benchmark of 75%. The overall MBI and its components were perceived as highly acceptable on the satisfaction questionnaire and exit interviews. There were significant improvements for disability, pain, and psychosocial factors (except perceived stress and dispositional mindfulness) at 3 months post-surgically. Qualitative data informed future modifications to the MBI that included reductions in and individual tailoring of home practice; applying skills to postsurgical concerns besides pain; providing clearer explanations for MBI objectives and each individual skill; and earlier introduction and greater emphasis on the mindful movement components. These modifications will be applied in subsequent trials of this intervention.
Our enrollment rate of 35% was lower than expected based on earlier studies conducted at the participating site.5,49 This might be related to a difference in the type of behavioral intervention, with earlier studies focused on CBT-based programs that were 6 sessions long compared with 8 in our study. The COVID-19 pandemic might also have impacted patients’ willingness to participate in research studies, as this study was conducted in 2021-2022 during the pandemic. Recruitment in the spine center clinic involved a warm hand-off from the treating surgeon to the recruiting study coordinator during preoperative visits. We speculate that patients were less likely to accept meetings with the coordinator during the pandemic. Another pilot study at our institution with a similar patient population from 2020-2021 had a comparable enrollment rate of 41%. 50 Additionally, our study’s retention rate of 80% was slightly below the 90% benchmark, possibly due to not collecting 3-month follow-up data from participants who discontinued the intervention sessions. However, 80% of participants completed all 8 sessions, exceeding completion rates in other trials of MBIs involving chronic low back pain populations.14,33,44 In future trials, we will aim to collect follow-up data from all willing participants, regardless of intervention completion
The average days of home mindfulness practice in our sample was higher than in prior studies of group-delivered, 8-session MBIs in patients with chronic low back pain.51-53 This may be due to surgical patients having more time available to practice due to sick leave or driving/activity restrictions. Participants reported that practice was easier to complete during the early recovery period and more challenging after returning to work or daily activities. The high engagement between sessions suggests that early after surgery may be an opportune time to deliver the intervention to optimize home practice. It is also possible that adherence was high due to the individualized attention participants received, as the intervention was delivered one-on-one instead of in the typical group format.
Around half of participants interviewed said they would consider participating in a group-delivered intervention. Group interventions provide the benefit of peer support and shared experiences, as noted by participants of group MBIs for chronic pain management.54-56 To date, one pilot study 16 has directly compared a group- to individual-delivered MBCT intervention in adults with depression and comorbid somatic conditions and found improvements in psychological outcomes with no differences between group or individual MBCT. 16 Delivering a group MBI has challenges in a surgical spine population since surgical volumes at many centers are too low for group formation. Alternatives include centralizing group-delivered MBIs across sites or initiating a group-delivered MBI before surgery, similar to preoperative educational sessions in patients undergoing total joint surgery,57,58 and then offering drop-in sessions after surgery.
The high satisfaction reported by patients is consistent with prior studies of MBIs for chronic pain.52,54 Participants’ perception that the MBI was meaningful to aspects of recovery was mirrored in the high percentages of participants achieving MCID in patient-reported outcomes. Notably, very high percentages of participants achieved MCID for pain bothersomeness and pain interference, patient-reported outcomes that are less commonly reported in lumbar spine surgery trials. 59 These pain outcomes are targeted in trials of MBIs and other psychosocial interventions for chronic pain and should be considered for future surgical populations.13,33
Significant within-participant improvements in psychosocial risk and protective factors including kinesiophobia, pain catastrophizing, and pain-related self-efficacy were observed from preoperative baseline to 3-month follow-up. Exit interviews corroborated most quantitative findings, with participants describing how the MBI benefitted them with regards to pain coping, re-appraisal of pain sensations, and reduced fear of movement. Reductions in Perceived Stress measured with the PSS-4 were not significant, yet several participants described in exit interviews a benefit of the MBI for general stress management.
Some participants recommended earlier and greater emphasis on mindful movement and activity pacing skills during the MBI, intervention components that we speculate could play a role in reducing kinesiophobia (ie, pain-related fear of movement or physical activity). Higher levels of kinesiophobia early after lumbar spine surgery predict poorer long-term surgical outcomes 18 and further study of the impact of a postsurgical MBI on kinesiophobia is warranted. There was not a significant improvement in dispositional mindfulness, as measured by the FFMQ-short form. Increases in dispositional mindfulness during MBIs are found inconsistently.33,60 Lack of increases in mindfulness can result from measurement response-shift, in which participants’ frame of reference for survey items shifts as a result of the MBI, leading to similar or lower post-intervention mindfulness scores. 61 Methods of adjusting for response-shift in MBIs have been proposed and may enhance the reliability of mindfulness measurement in future trials. 61 The effect size for the change in mindfulness in our study was moderate, and the study was not powered to detect small to medium-sized effects. It is also possible that measures of dispositional mindfulness other than the FFMQ may be more sensitive to intervention-related change in this patient population and could be explored in future trials. The benefits of MBIs in pain populations might also stem from improvements in key factors such as pain catastrophizing and self-efficacy, which improved similarly to cognitive behavioral therapy in two studies comparing mindfulness-based stress reduction to cognitive behavioral therapy in patients with chronic low back pain.20,21 In one of these studies, cross-lagged analyses indicated that only prior-week changes in pain catastrophizing and pain self-efficacy, but not in mindfulness as measured by the FFMQ-short form, predicted unique variance in next-week pain interference and pain intensity. 20
Limitations
The sample size was small as the study objective was to test initial feasibility and acceptability of the intervention, which resulted in limited diversity with respect to racial and ethnic background. Patients of racial and ethnic minority status are underrepresented within the spine surgery population compared with the general population of the United States.62,63 Future multi-site studies could enroll patients across geographically distinct spine centers, thereby enrolling a sample that is more representative of the patient population undergoing spine surgery and increasing external generalizability of study results. Enrolling study samples representative of the targeted patient population is a common challenge in trials of MBIs, and strategies have been recommended such as collaborating with stakeholders from diverse populations and diversifying the research investigators, MBI interventionists, and study settings. 64 There was no comparison group in this study so improvements in outcomes cannot be attributed specifically to the telehealth MBI. Comparison to usual postoperative care, attention-controlled conditions, and/or active postoperative interventions can help address this limitation and disentangle benefits specific to the MBI or shared across interventions. In addition, outcomes were collected at 3 months postoperatively and future work is needed to determine maintenance of treatment effects up to 12 months postoperatively, the commonly accepted time frame for outcome assessment after lumbar spine surgery.45,65 Other limitations are the possibility of biases introduced during exit interviews conducted by researchers involved in the study in addition to the reliance on patient-reported outcomes without objective measures of improvement, particularly in this nonblinded study.
If future randomized controlled trials demonstrate the efficacy of the postsurgical MBI, its implementation could be expanded by training pain psychologists—professionals who specialize in treating pain conditions through psychological and behavioral approaches. These specialists are already employed within many major pain treatment centers. Furthermore, research has shown that a web-based, self-paced MBI can be as effective as an instructor-delivered telehealth MBI for patients with chronic pain, 15 suggesting that this format could provide a lower-resource alternative for scaling the postsurgical MBI, making it more accessible to a broader patient population.
Conclusions
Results indicate an 8-session telehealth MBI delivered one-on-one to patients after elective lumbar spine surgery is feasible, acceptable and most patients perceive meaningful benefits to their surgical recovery from the MBI. Due to the single-group design lacking a comparison group, the MBI cannot be inferred as the cause of the reported improvements. Results support future fully powered randomized controlled trials with longer-term follow-up to determine effects of MBIs after lumbar spine surgery for chronic spine pain. Given the limited demographic diversity in the study sample, we recommend that future randomized trials include multiple sites and utilize strategies to recruit a sample that is representative of the larger patient population undergoing lumbar spine surgery.
Supplemental Material
Supplemental Material for Feasibility, Acceptability and Modification of a Post-surgical Telehealth Mindfulness-Based Intervention to Enhance Recovery After Lumbar Spine Surgery: A Prospective Intervention Study by Carrie E. Brintz, Erin Connors Kelly, Geneva Polser, Bethany A. Rhoten, Michelle Foote Pearce, Rogelio A. Coronado, Roisin O’Donnell, Shannon Block, Amanda Priest, Rishabh Gupta, Sarah T. Whitaker, Stephen Bruehl, Byron F. Stephens, Amir M. Abtahi, Jacob Schwarz, Scott L. Zuckerman, Benjamin French and Kristin R. Archer in Global Advances in Integrative Medicine and Health.
Acknowledgments
The authors would like to acknowledge Dr Shelby Reyes and Dakota Lawrence for their feedback on the intervention manual and delivering the intervention to participants.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Carrie Brintz receives compensation from the Academic Consortium for Integrative Medicine and Health for her role as Associate Editor of Global Advances in Integrative Medicine and Health. Stephen Bruehl is a consultant for Akigai. Byron Stephens receives institutional research support and paid travel to teach from Globus and institutional research support from Stryker. Kristin Archer receives compensation from Spine journal for her role as Deputy Editor and as a consultant for NeuroSpine Innovation, Inc.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institutes of Health (NIH)/National Center for Complementary and Integrative Health [grant number K23AT011569], the Osher Center for Integrative Health at Vanderbilt, and the Vanderbilt Center for Musculoskeletal Research. Dr Coronado was supported by the NIH/National Center for Advancing Translational Sciences [grant number KL2TR002245]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Supplemental Material: Supplemental material for this article is available online.
Ethical Statement
Ethical Approval
The Vanderbilt University Institutional Review Board approved all study procedures (IRB #201486).
Consent to Participate
All participants provided written informed consent to participate in eligibility screening and in the study.
ORCID iD
Carrie E. Brintz https://orcid.org/0000-0003-4915-9023
Data Availability Statement
Deidentified data is available from the corresponding author by request.*
References
- 1.Laufenberg-Feldmann R, Kappis B, Mauff S, Schmidtmann I, Ferner M. Prevalence of pain 6 months after surgery: a prospective observational study. BMC Anesthesiol. 2016;16(1):91. doi: 10.1186/s12871-016-0261-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Orhurhu VJ, Chu R, Gill J. Failed back surgery syndrome. In: StatPearls. StatPearls Publishing; 2019. https://www.ncbi.nlm.nih.gov/books/NBK539777/. Accessed October 24, 2019. [PubMed] [Google Scholar]
- 3.Coronado RA, George SZ, Devin CJ, Wegener ST, Archer KR. Pain sensitivity and pain catastrophizing are associated with persistent pain and disability after lumbar spine surgery. Arch Phys Med Rehabil. 2015;96(10):1763-1770. doi: 10.1016/j.apmr.2015.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Parrish JM, Jenkins NW, Parrish MS, et al. The influence of cognitive behavioral therapy on lumbar spine surgery outcomes: a systematic review and meta-analysis. Eur Spine J. 2021;30(5):1365-1379. doi: 10.1007/s00586-021-06747-x [DOI] [PubMed] [Google Scholar]
- 5.Archer KR, Devin CJ, Vanston SW, et al. Cognitive-behavioral-based physical therapy for patients with chronic pain undergoing lumbar spine surgery: a randomized controlled trial. J Pain. 2016;17(1):76-89. doi: 10.1016/j.jpain.2015.09.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abbott AD, Tyni-Lenné R, Hedlund R. Early rehabilitation targeting cognition, behavior, and motor function after lumbar fusion: a randomized controlled trial. Spine. 2010;35(8):848-857. doi: 10.1097/BRS.0b013e3181d1049f [DOI] [PubMed] [Google Scholar]
- 7.Monticone M, Ferrante S, Teli M, et al. Management of catastrophising and kinesiophobia improves rehabilitation after fusion for lumbar spondylolisthesis and stenosis. A randomised controlled trial. Eur Spine J. 2014;23(1):87-95. doi: 10.1007/s00586-013-2889-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Accardi-Ravid M, Eaton L, Meins A, et al. A qualitative descriptive study of patient experiences of pain before and after spine surgery. Pain Med. 2019;21:604-612. doi: 10.1093/pm/pnz090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brintz CE, Coronado RA, Schlundt DG, et al. A conceptual model for spine surgery recovery: a qualitative study of patients’ expectations, experiences, and satisfaction. Spine. 2023;48(14):E235-E244. doi: 10.1097/BRS.0000000000004520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Qaseem A, Wilt TJ, McLean RM, et al. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American college of physicians. Ann Intern Med. 2017;166(7):514-530. doi: 10.7326/M16-2367 [DOI] [PubMed] [Google Scholar]
- 11.Crane RS, Brewer J, Feldman C, et al. What defines mindfulness-based programs? The warp and the weft. Psychol Med. 2017;47(6):990-999. doi: 10.1017/S0033291716003317 [DOI] [PubMed] [Google Scholar]
- 12.Gardner-Nix J, Backman S, Barbati J, Grummitt J. Evaluating distance education of a mindfulness-based meditation programme for chronic pain management. J Telemed Telecare. 2008;14(2):88-92. doi: 10.1258/jtt.2007.070811 [DOI] [PubMed] [Google Scholar]
- 13.Day MA, Ciol MA, Mendoza ME, et al. The effects of telehealth-delivered mindfulness meditation, cognitive therapy, and behavioral activation for chronic low back pain: a randomized clinical trial. BMC Med. 2024;22:156. doi: 10.1186/s12916-024-03383-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burns JW, Jensen MP, Thorn B, et al. Cognitive therapy, mindfulness-based stress reduction, and behavior therapy for the treatment of chronic pain: randomized controlled trial. Pain. 2022;163(2):376-389. doi: 10.1097/j.pain.0000000000002357 [DOI] [PubMed] [Google Scholar]
- 15.Burgess DJ, Calvert C, Hagel Campbell EM, et al. Telehealth mindfulness-based interventions for chronic pain: the LAMP randomized clinical trial. JAMA Intern Med. 2024;184(10):1163-1173. doi: 10.1001/jamainternmed.2024.3940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schroevers MJ, Tovote KA, Snippe E, Fleer J. Group and individual mindfulness-based cognitive therapy (MBCT) are both effective: a pilot randomized controlled trial in depressed people with a somatic disease. Mindfulness. 2016;7(6):1339-1346. doi: 10.1007/s12671-016-0575-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu Q, Cui X, Guan LC, et al. Chronic pain after spine surgery: insights into pathogenesis, new treatment, and preventive therapy. J Orthop Transl. 2023;42:147-159. doi: 10.1016/j.jot.2023.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Archer KR, Seebach CL, Mathis SL, Riley LH, Wegener ST. Early postoperative fear of movement predicts pain, disability, and physical health six months after spinal surgery for degenerative conditions. Spine J. 2014;14(5):759-767. doi: 10.1016/j.spinee.2013.06.087 [DOI] [PubMed] [Google Scholar]
- 19.Archer KR, Wegener ST, Seebach C, et al. The effect of fear of movement beliefs on pain and disability after surgery for lumbar and cervical degenerative conditions. Spine. 2011;36(19):1554-1562. doi: 10.1097/BRS.0b013e3181f8c6f4 [DOI] [PubMed] [Google Scholar]
- 20.Burns JW, Jensen MP, Gerhart J, et al. Cognitive therapy, mindfulness-based stress reduction, and behavior therapy for people with chronic low back pain: a comparative mechanisms study. J Consult Clin Psychol. 2023;91(3):171-187. doi: 10.1037/ccp0000801 [DOI] [PubMed] [Google Scholar]
- 21.Turner JA, Anderson ML, Balderson BH, Cook AJ, Sherman KJ, Cherkin DC. Mindfulness-based stress reduction and cognitive behavioral therapy for chronic low back pain: similar effects on mindfulness, catastrophizing, self-efficacy, and acceptance in a randomized controlled trial. Pain. 2016;157(11):2434-2444. doi: 10.1097/j.pain.0000000000000635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zeidan F, Vago DR. Mindfulness meditation-based pain relief: a mechanistic account: mechanisms supporting mindfulness-based analgesia. Ann N Y Acad Sci. 2016;1373(1):114-127. doi: 10.1111/nyas.13153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jinich-Diamant A, Garland E, Baumgartner J, et al. Neurophysiological mechanisms supporting mindfulness meditation–based pain relief: an updated review. Curr Pain Headache Rep. 2020;24(10):56. doi: 10.1007/s11916-020-00890-8 [DOI] [PubMed] [Google Scholar]
- 24.Lu C, Moliadze V, Nees F. Dynamic processes of mindfulness-based alterations in pain perception. Front Neurosci. 2023;17:1253559. doi: 10.3389/fnins.2023.1253559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Santorelli SF, Meleo-Meyer F, Koerbel L, Kabat-Zinn J. Mindfulness-Based Stress Reduction (MBSR) Authorized Curriculum Guide © 2017. Published online 2017:65.
- 26.Dobkin PL, Irving JA, Amar S. For whom may participation in a mindfulness-based stress reduction program be contraindicated? Mindfulness. 2012;3(1):44-50. doi: 10.1007/s12671-011-0079-9 [DOI] [Google Scholar]
- 27.Lawrence CE, Dunkel L, McEver M, et al. A REDCap-based model for electronic consent (eConsent): moving toward a more personalized consent. J Clin Transl Sci. 2020;4(4):345-353. doi: 10.1017/cts.2020.30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Obeid JS, McGraw CA, Minor BL, et al. Procurement of shared data instruments for research electronic data capture (REDCap). J Biomed Inf. 2013;46(2):259-265. doi: 10.1016/j.jbi.2012.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inf. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inf. 2009;42(2):377-381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fairbank J, Couper J, Davies J, O’Brien JP. The Oswestry low back pain questionnaire. Spine. 1980;66:271-273. [PubMed] [Google Scholar]
- 32.Ferreira-Valente MA, Pais-Ribeiro JL, Jensen MP. Validity of four pain intensity rating scales. Pain. 2011;152(10):2399-2404. doi: 10.1016/j.pain.2011.07.005 [DOI] [PubMed] [Google Scholar]
- 33.Cherkin DC, Sherman KJ, Balderson BH, et al. Effect of mindfulness-based stress reduction vs cognitive behavioral therapy or usual care on back pain and functional limitations in adults with chronic low back pain: a randomized clinical trial. JAMA. 2016;315(12):1240-1249. doi: 10.1001/jama.2016.2323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cella D, Choi SW, Condon DM, et al. PROMIS® adult health profiles: efficient short-form measures of seven health domains. Value Health. 2019;22(5):537-544. doi: 10.1016/j.jval.2019.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Arciero E, Desai S, Coury J, et al. Comparison of psychometric properties of patient-reported outcomes measurement information system with traditional outcome metrics in spine surgery. JBJS Rev. 2023;11(3):00193. doi: 10.2106/JBJS.RVW.22.00193 [DOI] [PubMed] [Google Scholar]
- 36.Goubert L, Crombez G, Van Damme S, Vlaeyen JWS, Bijttebier P, Roelofs J. Confirmatory factor analysis of the Tampa scale for Kinesiophobia: invariant two-factor model across low back pain patients and fibromyalgia patients. Clin J Pain. 2004;20(2):103-110. [DOI] [PubMed] [Google Scholar]
- 37.Sullivan MJL, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess. 1995;7(4):524-532. doi: 10.1037/1040-3590.7.4.524 [DOI] [Google Scholar]
- 38.Nicholas MK. The pain self-efficacy questionnaire: taking pain into account. Eur J Pain. 2007;11(2):153-163. doi: 10.1016/j.ejpain.2005.12.008 [DOI] [PubMed] [Google Scholar]
- 39.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385-396. doi: 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- 40.Gu J, Strauss C, Crane C, et al. Examining the factor structure of the 39-item and 15-item versions of the Five Facet Mindfulness Questionnaire before and after mindfulness-based cognitive therapy for people with recurrent depression. Psychol Assess. 2016;28(7):791-802. doi: 10.1037/pas0000263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Day MA. Mindfulness-Based Cognitive Therapy for Chronic Pain: A Clinical Manual and Guide. John Wiley & Sons, Ltd; 2017. doi: 10.1002/9781119257875 [DOI] [Google Scholar]
- 42.Teasdale JD, Segal ZV, Williams JM, Ridgeway VA, Soulsby JM, Lau MA. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. J Consult Clin Psychol. 2000;68(4):615-623. doi: 10.1037//0022-006x.68.4.615 [DOI] [PubMed] [Google Scholar]
- 43.Day MA, Thorn BE, Ward LC, et al. Mindfulness-based cognitive therapy for the treatment of headache pain: a pilot study. Clin J Pain. 2014;1:152-161. doi: 10.1097/AJP.0b013e318287a1dc [DOI] [PubMed] [Google Scholar]
- 44.Day MA, Ward LC, Ehde DM, et al. A pilot randomized controlled trial comparing mindfulness meditation, cognitive therapy, and mindfulness-based cognitive therapy for chronic low back pain. Pain Med. 2019;20(11):2134-2148. doi: 10.1093/pm/pny273 [DOI] [PubMed] [Google Scholar]
- 45.Asher AM, Oleisky E, Pennings J, et al. Measuring clinically relevant improvement after lumbar spine surgery: is it time for something new? Spine J. 2020;20:847-856. doi: 10.1016/j.spinee.2020.01.010 [DOI] [PubMed] [Google Scholar]
- 46.Ostelo RWJG, Deyo RA, Stratford P, et al. Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine. 2008;33(1):90-94. doi: 10.1097/BRS.0b013e31815e3a10 [DOI] [PubMed] [Google Scholar]
- 47.Dedoose Version 9.2.007, cloud application for managing, analyzing, and presenting qualitative and mixed method research data. Published online 2024. https://www.dedoose.com/
- 48.Aschbrenner KA, Kruse G, Gallo JJ, Plano Clark VL. Applying mixed methods to pilot feasibility studies to inform intervention trials. Pilot Feasibility Stud. 2022;8(1):217. doi: 10.1186/s40814-022-01178-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Archer K, Haug C, Pennings J. Comparing two programs to improve disability, pain, and health among patients who have had back surgery. Patient-Centered Outcomes Research Institute (PCORI). 2020. doi: 10.25302/04.2020.CER.130601970 [DOI] [Google Scholar]
- 50.Master H, Coronado RA, Whitaker S, et al. Combining wearable technology and telehealth counseling for rehabilitation after lumbar spine surgery: feasibility and acceptability of a physical activity intervention. Phys Ther. 2023;104:pzad096. doi: 10.1093/ptj/pzad096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Morone NE, Rollman BL, Moore CG, Li Q, Weiner DK. A mind–body program for older adults with chronic low back pain: results of a pilot study. Pain Med. 2009;10(8):1395-1407. doi: 10.1111/j.1526-4637.2009.00746.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zgierska AE, Burzinski CA, Cox J, et al. Mindfulness meditation-based intervention is feasible, acceptable, and safe for chronic low back pain requiring long-term daily opioid therapy. J Alternative Compl Med. 2016;22(8):610-620. doi: 10.1089/acm.2015.0314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Barceló-Soler A, Morillo-Sarto H, Fernández-Martínez S, et al. A Systematic review of the adherence to home-practice meditation exercises in patients with chronic pain. Int J Environ Res Publ Health. 2023;20(5):4438. doi: 10.3390/ijerph20054438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Brintz CE, Roth I, Faurot K, Rao S, Gaylord SA. Feasibility and acceptability of an abbreviated, four-week mindfulness program for chronic pain management. Pain Med. 2020;21(11):2799-2810. doi: 10.1093/pm/pnaa208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Foulk M, Montagnini M, Fitzgerald J, Ingersoll-Dayton B. Mindfulness-based group therapy for chronic pain management in older adults. Clin Gerontol. 2023;1-10. doi: 10.1080/07317115.2023.2229307 [DOI] [PubMed] [Google Scholar]
- 56.Chen SP, Liu HT, Appelt JC, et al. Feasibility of mindfulness-based intervention for veterans managing chronic pain. Can J Occup Ther. 2023;90(3):303-314. doi: 10.1177/00084174231156276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pitaro NL, Herrera MM, Stern BZ, et al. Synthesis of ‘joint class’ curricula at high volume joint replacement centres and a preliminary model for development and evaluation. J Eval Clin Pract. 2024;30(1):46-59. doi: 10.1111/jep.13865 [DOI] [PubMed] [Google Scholar]
- 58.Hanley AW, Gililland J, Garland EL. To be mindful of the breath or pain: comparing two brief preoperative mindfulness techniques for total joint arthroplasty patients. J Consult Clin Psychol. 2021;89(7):590-600. doi: 10.1037/ccp0000657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Beighley A, Zhang A, Huang B, et al. Patient-reported outcome measures in spine surgery: a systematic review. J Craniovertebral Junction Spine. 2022;13(4):378-389. doi: 10.4103/jcvjs.jcvjs_101_22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Morone NE, Greco CM, Moore CG, et al. A mind-body program for older adults with chronic low back pain: a randomized clinical trial. JAMA Intern Med. 2016;176(3):329-337. doi: 10.1001/jamainternmed.2015.8033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bartos LJ, Posadas MP, Wrapson W, Krägeloh C. Increased effect sizes in a mindfulness- and yoga-based intervention after adjusting for response shift with then-test. Mindfulness. 2023;14(4):953-969. doi: 10.1007/s12671-023-02102-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wang MC, Shivakoti M, Sparapani RA, Guo C, Laud PW, Nattinger AB. Thirty-day readmissions after elective spine surgery for degenerative conditions among US Medicare beneficiaries. Spine J. 2012;12(10):902-911. doi: 10.1016/j.spinee.2012.09.051 [DOI] [PubMed] [Google Scholar]
- 63.Al JOM, Shahrestani S, Delavar A, et al. Demographic predictors of treatments and surgical complications of lumbar degenerative diseases: an analysis of over 250,000 patients from the National Inpatient Sample. Medicine (Baltim). 2022;101(11):e29065. doi: 10.1097/MD.0000000000029065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Eichel K, Gawande R, Acabchuk RL, et al. A Retrospective systematic review of diversity variables in mindfulness research, 2000–2016. Mindfulness. 2021;12(11):2573-2592. doi: 10.1007/s12671-021-01715-4 [DOI] [Google Scholar]
- 65.Staartjes VE, Siccoli A, De Wispelaere MP, Schröder ML. Patient-reported outcomes unbiased by length of follow-up after lumbar degenerative spine surgery: do we need 2 years of follow-up? Spine J. 2019;19(4):637-644. doi: 10.1016/j.spinee.2018.10.004 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Feasibility, Acceptability and Modification of a Post-surgical Telehealth Mindfulness-Based Intervention to Enhance Recovery After Lumbar Spine Surgery: A Prospective Intervention Study by Carrie E. Brintz, Erin Connors Kelly, Geneva Polser, Bethany A. Rhoten, Michelle Foote Pearce, Rogelio A. Coronado, Roisin O’Donnell, Shannon Block, Amanda Priest, Rishabh Gupta, Sarah T. Whitaker, Stephen Bruehl, Byron F. Stephens, Amir M. Abtahi, Jacob Schwarz, Scott L. Zuckerman, Benjamin French and Kristin R. Archer in Global Advances in Integrative Medicine and Health.
Data Availability Statement
Deidentified data is available from the corresponding author by request.*