Abstract
Access to clinical information is critical to support patient engagement. The 21st Century Cures Act grants patients immediate electronic access to their full medical records. To assess the potential impact of this transparency provision, we conducted a retrospective study in a large cancer center in New York City, focusing on clinically active patients’ accessing health information shared via the patient portal. We identified a significant increase (14%) in the number of pathology and radiology reports read by patients after the implementation ofimmediate release of reports. No changes were found in the rates of account creation or logins. Our results suggest that oncology patients show strong, consistent interest in their clinical data, with many taking advantage of the full electronic access granted by Cures. These findings shed new light on this legislation’s impact on patient engagement and access to clinical data.
Introduction
Oncology patients often have intensive healthcare information needs, as they frequently undergo numerous diagnostic tests, treatments, procedures, and other interventions.i Access to clinical information is pivotal to patients being informed participants in their own care. Previous studies have shown that direct access to health information supports patient engagement, improving such outcomes as medication adherence, blood pressure control and glycemic control.ii iii iv v Thus, granting patients easy, secure access to clinical data is a critical step to promoting engagement and improving healthcare outcomes. Patient groups and initiatives such as OpenNotes have long advocated for transparency in health care records to support patient engagement.vi
Recognizing the importance of transparency, the 21st Century Cures Act, enacted by Congress in 2016 and implemented in multiple phases, has given patients unprecedented access to their health records.vii In October 2022, a provision of Cures granted patients electronic access to their full medical records with the goal of improving transparency in healthcare information. However, little is known about the extent to which oncology patients are taking advantage of their new ability to access this information.
This study assessed patients’ involvement with their portal accounts and their access of clinical information at a large academic cancer center in New York City, before and after the Cures Act provision that granted patients full online access to their records. We hypothesized that the Cures Act provisions would boost patient engagement with the MSK patient portal and their clinical records.
Methods
Memorial Sloan Kettering Cancer Center (MSK) is a high-volume cancer center with brick-and-mortar facilities in New York City, primarily serving the New York, New Jersey, and Connecticut tri-state area. At the time of this study, MSK had an internally developed patient portal, MyMSK. Prior to October 6th, 2022, MSK released to MyMSK all laboratory reports and a subset of clinical notes immediately, and pathology and radiology reports within 48 hours. On October 6th, 2022, MSK implemented changes to make all clinical notes and diagnostic reports available immediately.
Between September 12 and 23, 2022, MSK rolled out a communication campaign to patients to make them aware of these upcoming changes. Approximately 250,000 patients received an email sharing that clinical reports, including pathology and radiology, would be available immediately and that patients could potentially see the results prior to the care team having had an opportunity to review it. MSK’s Patient and Family Advisory Council was an active participant and helped with the creation of the communication campaign.
To assess the impact of the interventions that increased patient access to their clinical data online, we conducted a retrospective time-series study of data related to the patient portal. We included patients that had at least one clinical encounter at MSK between April 7, 2022, through April 6, 2023 (i.e., 6 months prior to and 6 months after the implementation of the October 6th, 2022, Cures Act provision).
To support the time-series analysis, in every week, each patient in the sample was characterized as “clinically active” (or not) and an “active portal user” (or not). The patient was characterized as “clinically active” in each week if the patient had a clinical encounter at MSK in the 60 days prior to the start of the week in question. The patient was characterized as an “active portal user” in each week if the patient had logged in to the patient portal at least once during the week under consideration. These active periods ensured we did not underestimate our outcomes with patients who had no need to log into the portal or did not use the portal at all. A patient could alternate between active and inactive for both clinical and portal user definitions. As specified below, in the time series analyses, we included patients at various time points based on these definitions.
We analyzed changes in patterns of patient engagement for clinically active patients by measuring three outcomes. To ensure accurate estimation, each outcome had slightly different inclusion criteria:
The rate of patient portal accounts created: among clinically active patients without a portal account at the start of the week, we calculated the proportion who created a new account per week.
The number of portal logins per patient: among clinically active portal users, we determined the number of logins per week.
The proportion of pathology and radiology reports read: among clinically active portal users, we identified the proportion of the patient’s radiology and pathology reports created that were read within 30 days of being posted, per week.
Summary statistics, such as counts and percentages, were used to describe categorical variables and were compared using the chi-squared test. Continuous variables were described using medians and IQRs and compared using Wilcoxon rank sum tests. Each outcome was modeled over time at a weekly level using a general estimating equation (GEE). Weeks were calculated from Thursdays to Wednesdays to ensure that the date of October 6, 2022, coincided with the start of a week. GEEs were used to account for within-patient correlation between weeks. We used a non-parametric approach using restricted cubic splines (RCS) on time. The use of restricted cubic splines breaks our variable of time into multiple windows and fits a different polynomial curve for each window. The point where these windows meet is called a “knot”. These splines allow us to accurately estimate how outcomes change over time. To visualize the effect of time we used least squares (LS) means curves. Since time was our variable of interest, our univariable analysis was modified to include time with each of the other demographic covariates separately. The multivariable analysis includes time, age, gender, race, ethnicity, primary language, and marital status.
Our first outcome, portal account creation, included patients who had not created a portal account before our study start date, April 7, 2022, and were active patients. For this outcome, the active patient definition was extended 2 weeks prior to a clinical touchpoint as we found many patients created a portal account prior to an appointment. This outcome used a logistic GEE model. Our second outcome, login rates, used a Poisson GEE model and included active patients who were active portal users. The final outcomes, reports read, included active patients who were active portal users and received at least 1 report. For this outcome we calculated the rate opened per patient-week and used a linear regression GEE model. All GEE models used an exchangeable correlation structure. R (version 4.3.1; R Foundation for Statistical Computing, Vienna, Austria) was used for all analyses. All tests were two-sided and p<0.05 was considered significant.
This study was reviewed and approved by the Institutional Review Board (MSK Protocol 22-210-A2).
Results
During the period of our analysis, 236,164 patients had an encounter at MSK. The median age of the patients was 62 years. Most of the patients were female (62%), white (82%), non-Hispanic (92%), English-speaking (96%) and partnered (67%) (Table 1).
Table 1.
Patient demographics. Total sample = 236,164.
| Patient Characteristics | N (%*) |
|---|---|
| Sex | |
| Female | 145,945 (62%) |
| Indeterminate | 30 (<0.1%) |
| Male | 90,157 (38%) |
| Unknown | 32 |
| Age (years, median, interquartile range) | 62 (50, 72) |
| Race | |
| Asian-Far Fast/Indian-Subcontinent | 16,000 (7.4%) |
| Black | 16,536 (7.6%) |
| Other | 7,248 (3.3%) |
| White | 177,878 (82%) |
| Unknown | 18,502 |
| Ethnicity | |
| Hispanic or Latino | 16,342 (7.6%) |
| Not Hispanic | 198,047 (92%) |
| Unknown | 21,775 |
| Primary Language | |
| English | 220,446 (96%) |
| Other | 10,344 (4.5%) |
| Unknown | 5,374 |
| Marital Status | |
| Partnered | 151,883 (67%) |
| Single | 74,612 (33%) |
| Unknown | 9,669 |
Percentages reflect only known values
Rates of creation of MyMSK patient portal accounts
The total number of accounts created over the study period was 41,889. Of those, 35,170 (83.94%) were created while patients were clinically active or 2 weeks prior to the clinical encounter. Patients whose primary language was English or who were male, Asian or White, non-Hispanic, married/partnered, and younger were more likely than other patients to create portal accounts.
The rate of account creation per week among patients increased almost linearly during our study, from about 3.6% to 5.4% through our study period, while controlling for demographic variables. However, there was no inflection upward around October 6, 2022, to attribute this increase to the Cures Act (Figure 1, Table 2).
Figure 1.
Rate of patient portal accounts created over time during the study time period (GEE with restricted cubic spline).
Table 2.
Rate of patient portal accounts created over time during the study time period: full multivariable model.
| Characteristic | OR 1 | 95% CI 1 | p-value |
|---|---|---|---|
| Week | |||
| Knot1* | 1.01 | 1.00, 1.02 | 0.024 |
| Knot2 | 1.1 | 1.02, 1.20 | 0.017 |
| Knot3 | 0.63 | 0.49, 0.81 | <0.001 |
| Knot4 | 2.27 | 1.64, 3.15 | <0.001 |
| Knot5 | 0.52 | 0.39, 0.69 | <0.001 |
| Sex (Female is the reference) | |||
| Male | 1.19 | 1.16, 1.22 | <0.001 |
| Age per 10 years | 0.85 | 0.85, 0.86 | <0.001 |
| Race (White is the reference) | |||
| Asian-Far East/Indian-Subcontinent | 1.48 | 1.42, 1.54 | <0.001 |
| Black | 0.62 | 0.59, 0.65 | <0.001 |
| Other | 0.75 | 0.70, 0.81 | <0.001 |
| Ethnicity (Hispanic or Latino is the reference) | |||
| Non-Hispanic | 1.06 | 1.01, 1.12 | 0.015 |
| Primary Language (English is the reference) | |||
| Other | 0.58 | 0.55, 0.61 | <0.001 |
| Marital Status (Partnered is the reference) | |||
| Single | 0.72 | 0.70, 0.74 | <0.001 |
OR = Odds Ratio, CI = Confidence Interval.
See Methods for description of knots.
Number of portal logins per patient per week
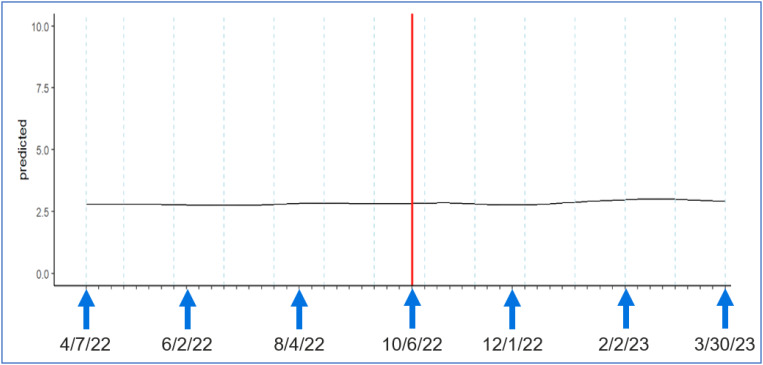
The number of unique clinically active patients who logged into their portal accounts at least once during the study period was 177,260. The number of portal logins was consistent over time, about 2.8 logins per week, both in univariable analysis and in multivariable analysis, controlling for demographic factors (Figure 2, Table 3). Patients whose primary language was not English or who were male, Asian or White, non-Hispanic, married/partnered, and younger logged into their portal accounts at a higher rate (Table 3).
Figure 2.
Rate of portal logins over time during the study time period (GEE with restricted cubic spline).
Table 3.
Rate of portal logins over time during the study time period: full multivariable model.
| Characteristic | IRR 1 | 95% CI 1 | p-value |
|---|---|---|---|
| Week | |||
| Knot1* | 1 | 1.00, 1.00 | 0.5 |
| Knot2 | 0.93 | 0.90, 0.96 | <0.001 |
| Knot3 | 1.52 | 1.35, 1.71 | <0.001 |
| Knot4 | 0.47 | 0.40, 0.55 | <0.001 |
| Knot5 | 2.29 | 1.96, 2.68 | <0.001 |
| Knot6 | 0.36 | 0.30, 0.44 | <0.001 |
| Knot7 | 4.11 | 3.31, 5.09 | <0.001 |
| Knot8 | 0.27 | 0.23, 0.33 | <0.001 |
| Knot9 | 1.53 | 1.28, 1.82 | <0.001 |
| Age per 10 years | 0.996 | 1.00, 1.00 | <0.001 |
| Sex (Female is the reference) | |||
| Male | 1.04 | 1.04, 1.04 | <0.001 |
| Race (White is the reference) | |||
| Asian-Far East/Indian-Subcontinent | 1.02 | 1.01, 1.02 | <0.001 |
| Black | 0.92 | 0.91, 0.92 | <0.001 |
| Other | 0.98 | 0.98, 0.99 | <0.001 |
| Ethnicity (Hispanic or Latino is the reference) | |||
| Not Hispanic | 1.02 | 1.01, 1.02 | <0.001 |
| Primary Language (English is the reference) | |||
| Other | 1.02 | 1.01, 1.02 | <0.001 |
| Marital Status (Partnered is the reference) | |||
| Single | 0.98 | 0.98, 0.98 | <0.001 |
IRR = Incidence Rate Ratio, CI = Confidence Interval.
See Methods for description of knots.
Proportion of pathology and radiology reports read
While controlling for demographic variables, at the beginning of the study period, the proportion of pathology and radiology reports being read by patients was 62%. By the end of the study period, this proportion had increased to 76%. The increase was sustained over time. The inflection point coincided with October 6, 2022, when the Cures Act provisions went into effect (Figure 3, Table 4).
Figure 3.
Rate of pathology and radiology reports read over time during the study time period (GEE with restricted cubic spline).
Table 4.
Rate of pathology and radiology reports read over time during the study time period: full multivariable model.
| Characteristic | Estimate | 95% CI 1 | p-value |
|---|---|---|---|
| Week | |||
| Knot1* | 0 | 0.0,0.0 | <0.001 |
| Knot2 | 0.02 | 0.01,0.02 | <0.001 |
| Knot3 | -0.04 | -0.05, -0.03 | <0.001 |
| Knot4 | 0.01 | 0.00, 0.03 | 0.078 |
| Sex (Female is the reference) | |||
| Male | -0.03 | -0.04, -0.03 | <0.001 |
| Age per 10 years | -0.004 | -0.01, 0.00 | <0.001 |
| Race (White is the reference) | |||
| Asian-Far East/Indian-Subcontinent | -0.01 | -0.02, 0.00 | 0.002 |
| Black | 0.20 | 0.21, -0.19 | <0.001 |
| Other | -0.06 | -0.08, -0.05 | <0.001 |
| Ethnicity (Hispanic or Latino is the reference) | |||
| Not Hispanic | 0.07 | 0.06, 0.08 | <0.001 |
| Primary Language (English is the reference) | |||
| Other | -0.12 | -0.13, -0.10 | <0.001 |
| Marital Status (Partnered is the reference) | |||
| Single | -0.05 | -0.05,-0.04 | <0.001 |
CI = Confidence Interval.
See Methods for description of knots.
Figures 1-3 and Tables 2-4 follow.
(Rest of this page left intentionally blank.)
Discussion and Conclusions
This study assessed changes in patient engagement with their medical records six months before and six months after the implementation of the October 6, 2022, provisions of the Cures Act that increased transparency to patients of their data in the medical record. Over the one-year period, we observed no significant changes that could be attributed temporally to the implementation of the Cures Act in the rates with which patients created portal accounts or the rate with which patients logged in to their portal accounts. However, among patients with some portal activity, we identified a significant increase in the number of pathology and radiology reports read by patients that was related to the implementation of the October 6, 2022, provisions. This elevated engagement persisted over time, demonstrating a long-standing impact of the policy change. Given that we observed a significant and sustained change in the rate of review of pathology and radiology reports by patients, we believe that patients perceived value in the additional access to their clinical information.
To control for contemporaneous trends in our outcomes, we treated time continuously and used splines rather than simply comparing outcomes before and after October 6, 2022. For example, the patient communication campaign related to the upcoming Cures Act provisions that took place at our institution between September 12 and 23, 2022 may have increased patient interest in the availability of reports even prior to October 6, 2022. Also, the Cures Act provisions received significant coverage by media prior to October, which may have increased patient interest in accessing their online data. Our use of time as a continuous variable allows these factors to be considered as part of the analysis.
In this study, although we observed an increase in patients’ access to diagnostic reports over time, we did not observe changes in the number of patients creating portal accounts or in the rates with which patients logged into their portal accounts. Rather, patients who already had accounts logged in at the same rate and sought more clinical information per login instance. Although these findings reflect an increase in engagement due to the Cures Act, additional interventions may be needed to get patients who do not yet have portal account to create one.
As with many industries, technology-enabled activities are increasingly becoming a routine part of healthcare. Patients will need to use technology to be fully and actively engaged in their health care. The field of informatics should be striving to continuously measure and improve patient engagement with technology. There are many challenges to be addressed as we strive to increase patient engagement with technology. First, it can be difficult to identify which patients may be able to use digital tools easily and which patients may need some kind of support.viii ix Even if it is known that a patient has limited eHealth literacy, it can be challenging to address the problem. Second, it is known that such factors as age, race, health conditions, health literacy and socioeconomic status can influence the rate of use of patient portals and additional research is needed to understand how to overcome these disparities at scale.x Third, although the concept of increased patient access to their data is felt to be a good thing, there are scenarios where thorny issues arise. Examples include access to data by adolescent patients and their guardians.xi Also, at least in some settings, health care providers continue to be concerned about the impact on workflow of patient access to data.xii Providers are key actors in the health care system and without their unflagging support, comprehensive adoption of digital technology by patients is sure to face headwinds. In summary, the journey to ubiquitous and routine use of technology by patients as part of their healthcare experience will require a sustained and multi-faceted effort. Trials of creative solutions, with research to measure impact, needs to be part of the approach.
One ramification of the Cures Act is that patients are now more likely to review their results – which may be abnormal -- via the portal before speaking with their doctors. This scenario can be especially problematic in oncology. The research is mixed on whether patients are comfortable reviewing abnormal results before speaking with their providers.xiii xiv Some providers feel negatively about the scenario.xv Provider organizations may want to consider the use of tools to support patients who are seeing abnormal results before having spoken with their providers. Emerging artificial intelligence-enabled capabilities may be able to help in these situations.
Even though the Cures Act provisions have enabled patients to have direct access to clinical information, there are other important health-related assets that are currently still are not accessible to patients. For example, easy and timely access to samples such as pathology specimens is not covered by the Cures Act. Lack of easy access to these assets can hinder effective and efficient care, especially when patients are trying to transition their care to a different healthcare system.
Our analysis has some limitations. First, this study took place at a single healthcare institution and findings may not be generalizable to other contexts. Second, we examined the policy change as a time series analysis without a concurrent comparison group. While we did not expect other influences on our outcomes to coincide with the Cures Act, our study does not account for secular trends.
In summary, our findings shed new light on the impact of medical record transparency and access on patient engagement with and use of their clinical data. Oncology patients show strong interest in their clinical data, and many are taking advantage of the full electronic access granted by Cures. This is an important finding, as easy electronic access can effectively promote engagement with the information and empower patients to be informed participants in their own care. Future research should focus on how to further increase patient engagement with digital capabilities and investigate how the changes implemented by Cures Act affect the relationship between the patient and the clinician.
Acknowledgements
This research was funded in part by the Cancer Center Support Grant to Memorial Sloan Kettering Cancer Center (P30 CA008748). It was also funded in part by MSK’s NCI Telehealth Research Centers of Excellence (TRACE) Grant (P50 CA271357).
Figures & Tables
References
- i.Rutten LJ, Arora NK, Bakos AD, Aziz N, Rowland J. Information needs and sources of information among cancer patients: a systematic review of research (1980-2003) Patient Educ Couns. 2005 Jun;57(3):250–61. doi: 10.1016/j.pec.2004.06.006. doi: 10.1016/j.pec.2004.06.006. PMID: 15893206. [DOI] [PubMed] [Google Scholar]
- ii.Tapuria A, Porat T, Kalra D, Dsouza G, Xiaohui S, Curcin V. Impact of patient access to their electronic health record: systematic review. Inform Health Soc Care. 2021 Jun 2;46(2):192–204. doi: 10.1080/17538157.2021.1879810. doi: 10.1080/17538157.2021.1879810. Epub 2021 Apr 10. PMID: 33840342. [DOI] [PubMed] [Google Scholar]
- iii.Zaidi M, Amante DJ, Anderson E, Ito Fukunaga M, Faro JM, Frisard C, Sadasivam RS, Lemon SC. Association Between Patient Portal Use and Perceived Patient-Centered Communication Among Adults With Cancer: Cross-sectional Survey Study. JMIR Cancer. 2022 Aug 9;8(3):e34745. doi: 10.2196/34745. doi: 10.2196/34745. PMID: 35943789; PMCID: PMC9399875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- iv.Park J, Liang M, Alpert JM, Brown RF, Zhong X. The Causal Relationship Between Portal Usage and Self-Efficacious Health Information-Seeking Behaviors: Secondary Analysis of the Health Information National Trends Survey Data. J Med Internet Res. 2021 Jan 27;23(1):e17782. doi: 10.2196/17782. doi: 10.2196/17782. PMID: 33502334; PMCID: PMC7875689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- v.Reynolds TL, Cobb JG, Steitz BD, Ancker JS, Rosenbloom ST. The State-of-the-Art of Patient Portals: Adapting to External Factors, Addressing Barriers, and Innovating. Appl Clin Inform. 2023 Aug;14(4):654–669. doi: 10.1055/s-0043-1770901. doi: 10.1055/s-0043-1770901. Epub 2023 Aug 23. PMID: 37611795; PMCID: PMC10446914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- vi. https://www.opennotes.org/ Accessed 3/12/2024.
- vii. https://www.healthit.gov/topic/oncs-cures-act-final-rule Accessed 3/12/2024.
- viii.Karnoe A., Kayser L. How is eHealth literacy measured and what do the measurements tell us? A systematic review. Knowledge Management & E-Learning. 2015;7(4):576–600. [Google Scholar]
- ix.Kim K, Shin S, Kim S, Lee E. The Relation Between eHealth Literacy and Health-Related Behaviors: Systematic Review and Meta-analysis. J Med Internet Res. 2023 Jan 30;25:e40778. doi: 10.2196/40778. doi: 10.2196/40778. PMID: 36716080; PMCID: PMC9926349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- x.Grossman LV, Masterson Creber RM, Benda NC, Wright D, Vawdrey DK, Ancker JS. Interventions to increase patient portal use in vulnerable populations: a systematic review. J Am Med Inform Assoc. 2019 Aug 1;26(8-9):855–870. doi: 10.1093/jamia/ocz023. doi: 10.1093/jamia/ocz023. PMID: 30958532; PMCID: PMC6696508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- xi.Sisk BA, Antes AL, Bereitschaft C, Enloe M, Lin S, Srinivas M, Bourgeois F, DuBois JM. Engaging Adolescents in Using Online Patient Portals. JAMA Netw Open. 2023 Aug 1;6(8):e2330483. doi: 10.1001/jamanetworkopen.2023.30483. doi: 10.1001/jamanetworkopen.2023.30483. PMID: 37610751; PMCID: PMC10448298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- xii.van Rijt AM, Hulter P, Weggelaar-Jansen AM, Ahaus K, Pluut B. Mental Health Care Professionals’ Appraisal of Patients’ Use of Web-Based Access to Their Electronic Health Record: Qualitative Study. J Med Internet Res. 2021 Aug 27;23(8):e28045. doi: 10.2196/28045. doi: 10.2196/28045. PMID: 34448705; PMCID: PMC8433850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- xiii.Steitz BD, Turer RW, Lin CT, MacDonald S, Salmi L, Wright A, Lehmann CU, Langford K, McDonald SA, Reese TJ, Sternberg P, Chen Q, Rosenbloom ST, DesRoches CM. Perspectives of Patients About Immediate Access to Test Results Through an Online Patient Portal. JAMA Netw Open. 2023 Mar 1;6(3):e233572. doi: 10.1001/jamanetworkopen.2023.3572. doi: 10.1001/jamanetworkopen.2023.3572. PMID: 36939703; PMCID: PMC10028486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- xiv.Bruno B., Steele S., Carbone J., et al. Informed or anxious: patient preferences for release of test results of increasing sensitivity on electronic patient portals. Health Technol. 2022;12:59–67. doi: 10.1007/s12553-021-00628-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- xv.Anyidoho PA, Verschraegen CF, Markham MJ, Alberts S, Sweetenham J, Cameron K, Abu Hejleh T. Impact of the Immediate Release of Clinical Information Rules on Health Care Delivery to Patients With Cancer. JCO Oncol Pract. 2023 May;19(5):e706–e713. doi: 10.1200/OP.22.00712. doi: 10.1200/OP.22.00712. Epub 2023 Feb 13. PMID: 36780583; PMCID: PMC10414766. [DOI] [PMC free article] [PubMed] [Google Scholar]