Abstract
WISP stands as an efficacious solution to the challenges associated with Stereoelectroencephalography (SEEG) strategic planning, offering lightweight and interactive web interfaces for rendering multiple brain views. These interfaces facilitate collaborative engagement among care team members across various disciplines during patient case conferences and SEEG strategic planning sessions. Moreover, WISP incorporates a collaborative electrode and electrode group library, serving as a standardized repository of knowledge. The application enables seamless conversion of case conference outcomes and SEEG plans into images and PDF files, with transmission to Electronic Health Record (EHR) systems through a customized HL7 engine. The initial assessment findings demonstrate WISP provides good usability according to the System Usability Scale (SUS) score, with physicians exhibiting a clear preference for its utilization over conventional approaches to case conference documentation and SEEG planning. Furthermore, physicians have actively embraced WISP in their collaborative sessions, indicating its seamless integration into their clinical workflows.
Introduction
Stereoelectroencephalography (SEEG) is a mildly invasive neurological technique to precisely locate the seizure onset zone (SOZ) and its propagation path by implanting multiple depth electrodes to the lesion’s presumed location. The result, combining with anatomical structure, provides the fundamental support data for surgical resection 1,2,3.
SEEG is often considered a long-term monitoring method to localize the SOZ when the noninvasive methods, such as electroencephalography (EEG) recording, cannot provide enough information about the lesion. It’s also a preferred method when the presumed SOZ is deep or the lesion is not near eloquent cortex4,5.
SEEG requires a significant commitment to pre-operational planning. The recommendation should come from multidisciplinary evaluation in the care conference based on considerations from seizure semiology, scalp EEG, neuropsychology data and imaging modalities such as MEG, MRI, fMRI, PET, SPECT analysis3,4.
Precise SEEG trajectory planning requires input from multiple modalities and the entire epilepsy monitoring unit (EMU). 1) The team works together to finalize the number of targets and calculate all the anatomical structures of interest. This is done usually during a live surgical case conference discussion between epileptologists, neurosurgeons, neuroradiologists, neuropsychologists, fellows, residents, and data analysis engineers. 2) The surgeon with operating room (OR) team then plans accurate targeting of these anatomical structures by simulating an avascular corridor, drilling angle of the skull, calculating SEEG electrode length, sampling, etc on robotic stereotactic assistance software. The timeline for this entire pre-operational process can take anywhere between 3 to 6 months from the first surgical care conference planning to the actual surgery.
Researchers have been exploring the solution to lessen the burden of planning. Nowell, Mark, et al7. Compare manual modeling to a computer-assisted modeling software and concluded that the computer assistant could reduce the planning time and increase surgery safety by automated entry point calculation. Cardinale et al8. proves that 3D digital subtraction angiography (DSA) is a safe procedure to aid SEEG planning by constructing vascular trees. Scorza D9,10. proposed a methodology that built a set of average trajectories based on historical planning data, which could apply to a new patient as initiated settings. The innovation of robotic devices further assists the operation with this technique11,12. For example, ROSA robotic assistant device13,14 is an integrated operating solution combining robotic arm and neurological planning software.
However, these existing tools focus more on surgical assisting and computing trajectories. The case team still lacks a tool for early-stage and quick SEEG planning. Inadequate strategic planning tools cause the problems of ineffective collaboration during the case conference. The Neurosurgical team typically only knew the extent and number of contacts to be placed on a patient; however, a more collaborative process is desired. These higher-level SEEG modeling tools used by the surgeon are heavy-weighted applications that do not fit into a scenario that expects more cooperation and high-paced communication. Moreover, these tools are expensive, have steep learning curves and consume a significant amount of computer resources as a trade-off of its diversified functions.
Lack of integration with the electronic health records (EHR) is another disadvantage of the current modeling tools assisting SEEG strategic planning. EHR is the core system for clinical decision support, automated procedures, and health information exchange between different interest groups15. However, most of the EHR systems don’t support the file format of these modeling applications. Insufficient integration with EHR makes it hard to collect data from the SEEG planning, hindering the secondary use of such data. Therefore, a collaborative, EHR-integrated, easy-to-reach planning tool is urgently needed.
In this paper, we introduce a Web-based Interactive SEEG Planner (WISP) that works as a data entry and visualization tool for the epilepsy care conference. It’s designed for SEEG planning but is also applicable to other clinical settings that possess similar characteristics such as efficient anatomical data visualization and annotation. WISP presents an interface with the rendering of six anatomical views of a template brain and creates a library of conventional electrodes. Users can add electrodes from the library and mark trajectories of electrodes as simply as drag and drop elements over the brain views. It is a lightweight web application that provides real-time rendering and role-based access control function, allowing collaborative data entries from multiple case team members. The data in WISP can be exported and transferred to EHR systems for future reference. Lastly, this brings value as an educational tool for fellows and residence learning from the case conference.
Methods
System architecture
Figure 2 shows WISP’s system architecture. During a case conference, WISP allows the multidisciplinary team to collaborate on a text-based data capture form. Team members can mark trajectory paths on six anatomical views of the brain or add standard electrodes with the library created by domain experts. A role-based access control system manages the access and privilege of the application. Both the descriptive and graphic data can be exported to an integrated case conference report and send to EHR using the HL7 interface.
Figure 2:
System architecture of WISP. Case conference members collaborate on the target planning with the electrode library. The system integrates the planning result into case conference report and transfers to EHR via HL7 interface.
Visualization of the brain atlas
Lack of visualization is one reason that causes the communication gap in SEEG planning. The traditional “sketching on whiteboard” method makes it hard to convey the information to other case team members, especially to the residents and trainees. To solve this problem, we design an interface with a template brain that displays six anatomical angles, including lateral and mesial views of each side of hemispheres with a dorsal view and a ventral view. Each view is segmented into different functional areas with labels and supported with a grid system and surgical lines. We also add a half-transparent Insula underneath the lateral view and create a toolbar that allows users to hide or display some of the supportive visual elements.
To make the image interactable on the web page, we first illustrate the template brain with drawing software and trace each functional area’s border to create vector paths. The vector paths present in an SVG format and are suitable for being handled with web applications. Second, we use Data-Driven Documents (D3)17 to render the six brain views’ vector paths and add additional graphic features such as grids and support lines. D3 is a JavaScript library that visualizes data on web applications. It provides modules that can render geographic data from an SVG file, allowing us to transfer the drawing into interactive components. Finally, we add drawing features that enable users to create dots and lines representing the electrodes and their trajectory on the template brain with mouse actions such as click and drag-n-drop.
Besides SEEG target planning, this interface also supports subdural electrodes (SDEs) planning, a rarer technique that implants a grid of electrodes to the patient. We extend the electrode drawing function and allow users to generate a rotatable grid on the canvas.
Electrode and electrode group library
Using standard electrodes is an effective communication method in a case conference. These electrodes are accumulated knowledge of a health center, and each health center might develop its own terminology of electrodes. We design a library that allows users to select an electrode from it and display on the brain views without memorizing all the electrodes. Multiple electrodes can be grouped together according to brain regions. Residents, trainees, and anyone with an entry level of domain-specific knowledge can also use WISP to be familiar with these electrodes’ conventional naming and their location.
To create an electrode library in WISP, we set up a unique data entry page with six brain views - similar to the WISP’s interface - and request a neurosurgeon to mark all the standard electrodes on the brain atlas. The neurosurgeon annotates on different views with the same label if an electrode is visible on multiple angles. The electrodes list is saved to the database and appears as selectable options in the WISP drawing interface. Common electrode groups are pre-populated in WISP based on the best practice of domain experts.
Web-based collaboration with role-based access control
WISP adapts a web-based architecture that accelerates collaboration of the case team. In the preliminary phases of SEEG planning, they need an uncomplicated and easily accessible tool to assist a discussion. The case team generally draws on a whiteboard or PowerPoint slides, but such formats are hard to collaborate. We decided to construct our solution as a web-based application that allows the user to access it by web browsers and share the editable document with other team members. The program’s architecture follows the modern Model–View–Controller (MVC) pattern that separates the development data structure, program logic and interfaces, which make it possible to embed WISP into other web-based health information systems. Moreover, we use a RESTful architecture18 combining a Role-based access control system (RBAC)19. The RESTful structure supports the CREATE, UPDATE, VIEW, and DELETE action to a data entry through an HTTP request. The RBAC system allows us to set up collaborative roles within WISP and prevent users from reaching information that doesn’t relate to them.
Interface design and implementation
The interface design is based on the understanding of targeted users and their usage scenarios. We inquiry the requirement of the preliminary case conference among the neurologists and surgeons of different proficiency levels and study their current workaround when a communication gap occurs. Then, we iterate a prototype that demonstrates our ideas and collects feedback from the three case team members on a weekly basis.
As a collaborative tool for preliminary SEEG planning, efficiency is the essential requirement. To increase the efficiency of the WISP, we try to reduce the cognitive load by two design decisions: (1) Adopting a minimal design style that avoids complex layout, decorative elements, and any other visual clutters. (2) Offloading tasks by providing instruction, references, and hints to interactive elements.
HL7 information exchange
To solve insufficient documentation of the case conference, WISP supports the Health Level Seven (HL7)16 interface to exchange information with EHR systems. Hl7 is an exchange standard protocol widely adopted by EHR systems, including EPIC, Allscripts, and Cerner. When transferring SEEG planning document, WISP will convert the electrode data into a PDF format and HL7 message to pass the data to the EHR systems.
Usability evaluation
We use structured testing methods to evaluate the usability of WISP. In the testing, we invite 5-8 case team members of different proficiency levels and exclude those who participated in the development stage to prevent bias. These case team members are asked to go through three designed tasks (table 1). We ask them to think out loud during the test, and calculate the steps and time they spend on each task. The goal is to collect opinions and observe their behavior during the test.
Table 1:
Task script of the usability test
After they complete tasks, we ask the participant to complete a survey about the experience after using the WISP. We use the System Usability Scale (SUS)20,21 that consists of 10 questions on a five-point Likert scale that range from Strongly Agree (5) to Strongly disagree (1):
I think that I would like to use this system frequently.
I found the system unnecessarily complex.
I thought the system was easy to use.
I think that I would need the support of a technical person to be able to use this system.
I found the various functions in this system were well integrated.
I thought there was too much inconsistency in this system.
I would imagine that most people would learn to use this system very quickly.
I found the system very cumbersome to use.
I felt very confident using the system.
I needed to learn a lot of things before I could get going with this system.
The SUS score is an industry-standard usability evaluation questionnaire and has been proved to work on a small sample size.
Results
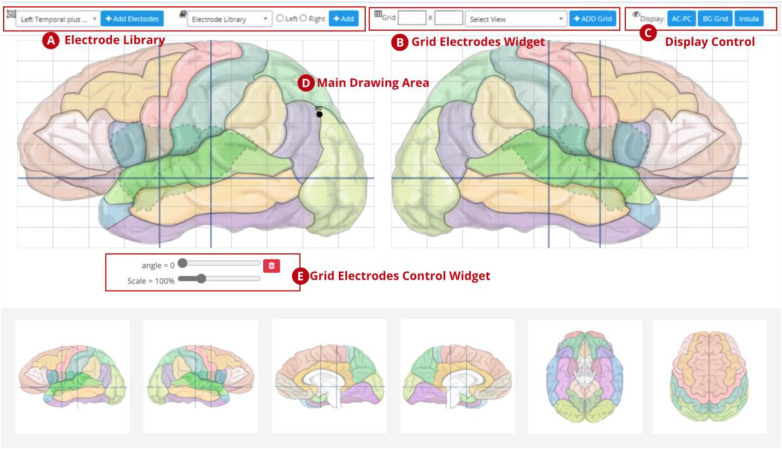
Atlas rendering and target planning interface
Figure 5 displays the outcome of the atlas rendering views and the target planning interface. The brain templates represent the inner and outer view from each side of the hemispheres (lateral and mesial views) and both the high-angle (dorsal) view and a low-angle (ventral) view. Each view is segmented with different colors to represent different functional areas and has an interactive label to display the area’s name when a mouse hovers over it.
Figure 5:
visualization of standard electrodes
The electrode planning interface allows users to mark the target of an electrode by mouse-clicking on any part of the main drawing area (D). When users click on the drawing canvas, an electrode is created, and they can attach a label to it. Users can also add electrodes from the electrode library (A). Moreover, the display control (C) area can toggle the background grid, surgical lines, and insula as supportive visual elements.
The (B) and (E) areas are the electrode grid control tool that can create a group of electrodes for subdural electrodes (SDEs) surgery.
Electrode and electrode group library
We collect 52 standard electrodes from the domain expert (Table 2). Each electrode’s data consists of the short name, full name, and location on the template brain, as displayed in figure 5. Each dot is the electrode’s target point. A dashed line is presented if the electrode has a specific entry point. Moreover, we populated 14 electrode groups including seven on the left hemisphere and the other seven on the right hemisphere. (Table 3).
Table 2:
List of electrodes
| Abbreviation | Full name | Abbreviation | Full name | Abbreviation | Full name |
|---|---|---|---|---|---|
| AMY | Amygdala | LOF | Lateral OrbitoFrontal | MPAR/MPL | Mid ParietaL |
| AH | Anterior Hippocampus | MOF | Medial OrbitoFrontal | IPL | Inferior ParietaL |
| PH | Posterior Hippocampus | RC | Rostral Cingulate | PPAR | Posterior PARietal |
| TP | Temporal Pole | AC | Anteior Cingulate | IPAR | Inferior PARietal |
| ABT | Anterior Basal Temporal | MC | Mid Cingulate | POP | Parietal OPerculum |
| MBT | Mid Basal Temporal | PC | Posterior Cingulate | PO | Parieto-Occipital |
| PBT | Posterior Basal Temporal | APF | Anterior PreFrontal | ASO | Anterior Sub-Occipital |
| TOP | Temporal OPerculum | PPF | Posterior PreFrontal | PSO | Posterior Sub-Occipital |
| LIN | Lingula | PSMA/PSM | Pre-Supplementary Motor | SO | Superior Occipital |
| AIN | Anterior INsula | SMA | Supplementary Motor Area | IO | Inferior Occipital |
| PIN | Posterior INsula | SM1/SPM | Superior Primary Motor | CAL | Calcarine |
| MIN | Mid INsula | MM1/MPM | Mid Primary Motor | OP | Occipital Pole |
| AIIN | Anterior Inferior INsula | SS1/SPS | Superior Primary Sensory | MEG | MEG localization |
| MIIN | Mid Inferior INsula | MS1/MPS | Mid Primary Sensory | LES(A/P, etc) | LESion(Anterior/Posterior) |
| MSIN | Mid Superior INsula | IPS | Inferior Primary Sensory | PMG(A/P, etc) | PolyMicroGyria (Anterior/Posterior) |
| PIIN | Posterior Inferior INsula | PRE | Precuneus | AER | Anterior EntoRhinal |
| PSIN | Posterior Superior INsula | SPAR/SPL | Superior ParietaL | MER | Mid EntoRhinal |
| POF | Posterior OrbitoFrontal |
Table 3:
List of electrode groups
| Group Name | Hemisphere | Electrodes |
|---|---|---|
| Left Temporal Lobe | Left | TP, AMY, AH, PH, ABT, MBT, PBT, AIN, AIIN, PIIN, MIIN, TOP, LIN, ASO, PSO |
| Right Temporal Lobe | Right | TP, AMY, AH, PH, ABT, MBT, PBT, AIN, AIIN, PIIN, MIIN, TOP, LIN, ASO, PSO |
| Left Posterior Quadrant SEEG | Left | ASO, PSO, CAL, PRE, IPL, LIN, PBT, MBT, SPL, MPL, SO, PO, IO, PC, SPS, PSIN, PIIN, MSIN, PH |
| Right Posterior Quadrant SEEG | Right | ASO, PSO, CAL, PRE, IPL, LIN, PBT, MBT, SPL, MPL, SO, PO, IO, PC, SPS, PSIN, PIIN, MSIN, PH |
| Left Frontal SEEG | Left | MOF, LOF, APF, AC, PSM, AIN, SMA, ASIN, RC, PPF, MC, MPM, SPM, SPS, POF, MPS |
| Right Frontal SEEG | Right | MOF, LOF, APF, AC, PSM, AIN, SMA, ASIN, RC, PPF, MC, MPM, SPM, SPS, POF, MPS |
| Left Occipital SEEG | Left | ASO, PSO, IO, CAL, CO, PO, PRE, MPL, SPL, IPL, LIN |
| Right Occipital SEEG | Right | ASO, PSO, IO, CAL, CO, PO, PRE, MPL, SPL, IPL, LIN |
| Left Central Lobe SEEG | Left | SPS, MPS, SPM, MC, PSIN, IPS, MIIN, MSIN, ASIN, PSM, SMA, MPM, AC, PPF, IPM, PIIN |
| Right Central Lobe SEEG | Right | SPS, MPS, SPM, MC, PSIN, IPS, MIIN, MSIN, ASIN, PSM, SMA, MPM, AC, PPF, IPM, PIIN |
| Left Temporal plus SEEG | Left | AMY, AH, PH, MBT, ABT, PBT, AIN, PIN, PIIN, MIIN, LIN, PRE, RC, POF, PC, TP, PSIN, MSIN, AIIN, LOF, MOF, ASO, PSO, PO, MPL, IPL, AC |
| Right Temporal plus SEEG | Right | AMY, AH, PH, MBT, ABT, PBT, AIN, PIN, PIIN, MIIN, LIN, PRE, RC, POF, PC, TP, PSIN, MSIN, AIIN, LOF, MOF, ASO, PSO, PO, MPL, IPL, AC |
| Left Standard Temporal SEEG | Left | TP, AMY, AH, PH, PC, PBT, MBT, ABT, AIN, PRE, POF, MIIN, PIN |
| Right Standard Temporal SEEG | Right | TP, AMY, AH, PH, PC, PBT, MBT, ABT, AIN, PRE, POF, MIIN, PIN |
Electrode grid
WISP can create a grid of electrodes that represent SDEs surgery. It is resizable, rotatable, and movable by dragging and dropping the grid over the canvas and using the slide bar to change the size or angle precisely. We use the highlighted blue dot as the anchor and highlight it with blue color so that users can quickly get the grid’s orientation.
Report (PDF) generator
Users can choose to export the document into a PDF file on the index page or the report page. The drawing would be converted from SVG to PNG and then being embedded into PDF. Also, WISP can combine the case conference form and the neuroanatomical target planning data into one single PDF file, which can be transferred to EHR or archive as a case conference record.
Usability evaluation
We arranged structured one-on-one usability tests with 3 attendings and 3 fellows to learn about their attitudes toward WISP. In task 1, we asked them to add a specific electrode from the library. All participants notice the toolbar immediately and click the dropdown menu without hesitation. Most (4/6, 67%) of them used the keyword search to find the electrode and 2 of them chose to browse the options. The average time they spend on this task is 21 second and the average steps are 4.5. In task 2, they spent averagely 16 second to complete the task with an average 3.5 steps. The average steps they spend on task 1 and task 2 are only slightly higher than the minimum required steps, which indicates that the flow is straightforward and easy to understand.
In task 3, it took participants an average of 65 seconds to complete, and they also spent almost five more steps than the minimum required number. Those additional steps usually happen when they try to rotate or move the grid.
The final score of the SUS score is 80.4. Usually, a score of 68 is considered good and acceptable, and above 85 is considered as excellent. Responses to each of the questions are displayed in Figure 7. Overall, participants say they are willing to use it frequently and they consider the tool well-integrated and consistent. They agree on the ease of using it, but they have diverged opinions on if they should learn a lot of things before using it (Q10). Our interpretation is that some of the participants might include medical knowledge as “the thing to learn”.
Figure 7:
Responses for survey questions 1-10
Production usage statistics
As of March 18, 2024, WISP has been operational for over two years since its establishment in March 2022. During this period, 591 care conferences have been held for 354 unique patients. Across six different brain views, a total of 6,637 electrodes have been planned. The TP (Temporal Pole) and ABT (Anterior Basal Temporal) electrodes was the most utilized, with 434 and 420 times of planning respectively. In contrast, only 16 electrode grids were planned for 8 distinct cases, indicative of their infrequent usage in surgeries.
Discussion and Conclusions
Structured documentation of SEEG Planning
We developed WISP to support the strategic planning of SEEG. SEEG planning is a lengthy and complex process that can take 3-6 months. During the process, various information is collected and generated. WISP provides a structured way to capture these data, which can be exported and queried for secondary use.
Collaborative Data Entry
SEEG planning involves care teams from multiple disciplines. WISP adopts a role-based access control strategy to allow clinicians with different roles to work together collaboratively.
Integration with EHR
It is impractical for clinicians to manage an stand-alone clinical informatics system because of redundant patient data entry and inconsistencies among systems. WISP solves this problem by implementing a HL7 messaging engine, which can pull patient demographic data from EHR systems and push the SEEG planning documents back. HL7 protocol is widely accepted by the main-stream EHR systems such as EPIC, Cerner, and ALLSCRIPTS.
Usability and Physician Feedback
The SUS score for WISP is 80.4, which is notably higher than the ‘good’ benchmark of 68 and close to the ‘excellent’ benchmark of 85. While further evaluation of WISP’s impact on planning time, burden, and surgical safety could be conducted through a focus group or larger-scale survey in the future, we’ve already received positive feedback from physicians during the think-aloud interviews: (1) One respondent mentioned that the visualization tool would greatly assist in recording case management conferences, saying, ‘I don’t have to draw electrodes on a glass brain (a sketch of an abstract brain).’ (2) Another respondent noted, ‘I can quickly find the electrode from the electrode library during the case conference.’ Several physicians believe that WISP can help them better track case conference records.
Educational Platform
WISP’s six interactive brain views of different anatomical angles, the separation of different function regions, and the pre-built electrode library provide rich information for clinical trainees to explore and learn. WISP is expected to act as an educational tool for clinical trainees.
Generalizability
Although WISP is specifically designed for SEEG planning, the implemented features such as brain view visualization, role-based access control, and HL7 messaging engine are generally applicable to similar application scenarios.
Future Enhancement
Given the recent advancements in AI technology, we believe that integrating AI-generated summaries or transcriptions could significantly enhance the tool by efficiently capturing key discussions, decisions, and insights during the care conference. We plan to explore this possibility in a future iteration of the tool.
Acknowledgements
Funding
This research was supported by the National Institutes of Health (NIH) through grants U01NS090408, U01NS090405, and R01NS116287. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author Contribution
GQZ, SL, and ST conceptualized this study. ST, WC and AB implemented the system with contributions from GQZ, SL, and JH. WC, ST, and JH designed the survey. WC and JH administrated the survey. WC and ST and developed and refined the manuscript with contributions from and JH, SL, and GQZ.
Figures & Tables
Figure 1:
Flowchart of the SEEG planning procedure.
Figure 3:
the flow of document transferred from WISP to EHRs
Figure 4:
six views of atlas and control widgets
Figure 6:
create a grid of electrodes
Table 4:
Average time and steps for each task
| average time | average steps | minimum required steps | |
|---|---|---|---|
| Task 1: please mark “PO” on the left hemisphere. | 21s | 4.5 | 4 |
| Task 2: Please add a custom electrode for a left occipital lobe lesion | 16s | 3.5 | 3 |
| Task 3: Please add a 5×5 electrode grid and try to rotate and move it | 65s | 13.6 | 8 |
References
- 1.Talairach J, Bancaud J, Bonis A, Szikla G, Tournoux P. Functional stereotaxic exploration of epilepsy. Confin Neurol. 1961;22:328e330. doi: 10.1159/000104378. [DOI] [PubMed] [Google Scholar]
- 2.Musolino A, Tournoux P, Missir O, Talairach J. Methodology of “in vivo” anatomical study and stereoelectroencephalograhic exploration in brain surgery for epilepsy. J Neuroradiol. 1990;17:67e102. [PubMed] [Google Scholar]
- 3.Chassoux Francine, et al. “Planning and management of SEEG.”. Neurophysiologie Clinique. 2018;48.1:25–37. doi: 10.1016/j.neucli.2017.11.007. [DOI] [PubMed] [Google Scholar]
- 4.Stricsek Geoffrey, et al. Functional Neurosurgery and Neuromodulation. Elsevier; 2019. “Chapter 16 - Stereoelectroencephalography (sEEG) Versus Grids and Strips.”; pp. 113–120. [Google Scholar]
- 5.Diehl B., Lüders H. O. “Temporal lobe epilepsy: when are invasive recordings needed?.”. Epilepsia. 2000;41:S61–S74. doi: 10.1111/j.1528-1157.2000.tb01536.x. [DOI] [PubMed] [Google Scholar]
- 6.Jayakar P, Gotman J, Harvey AS, Palmini A, Tassi L, Schomer D, Dubeau F, Bartolomei F, Yu A, Kršek P, Velis D. Diagnostic utility of invasive EEG for epilepsy surgery: indications, modalities, and techniques. Epilepsia. 2016 Nov;57(11):1735–47. doi: 10.1111/epi.13515. [DOI] [PubMed] [Google Scholar]
- 7.Nowell Mark, et al. “Comparison of computer-assisted planning and manual planning for depth electrode implantations in epilepsy.”. Journal of neurosurgery. 2016;124.6:1820–1828. doi: 10.3171/2015.6.JNS15487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cardinale F, Pero G, Quilici L, Piano M, Colombo P, Moscato A, Castana L, Casaceli G, Fuschillo D, Gennari L, Cenzato M. Cerebral angiography for multimodal surgical planning in epilepsy surgery: description of a new three-dimensional technique and literature review. World neurosurgery. 2015 Aug 1;84(2):358–67. doi: 10.1016/j.wneu.2015.03.028. [DOI] [PubMed] [Google Scholar]
- 9.Scorza D, De Momi E, Plaino L, Amoroso G, Arnulfo G, Narizzano M, Kabongo L, Cardinale F. Retrospective evaluation and SEEG trajectory analysis for interactive multi-trajectory planner assistant. International journal of computer assisted radiology and surgery. 2017 Oct 1;12(10):1727–38. doi: 10.1007/s11548-017-1641-2. [DOI] [PubMed] [Google Scholar]
- 10.Scorza D, Amoroso G, Cortés C, Artetxe A, Bertelsen Á, Rizzi M, Castana L, De Momi E, Cardinale F, Kabongo L. Experience-based SEEG planning: from retrospective data to automated electrode trajectories suggestions. Healthcare technology letters. 2018 Sep 14;5(5):167–71. doi: 10.1049/htl.2018.5075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vakharia VN, Duncan JS. Automation advances in stereoelectroencephalography planning. Neurosurgery Clinics. 2020 Jul 1;31(3):407–19. doi: 10.1016/j.nec.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cardinale Francesco, et al. “Stereoelectroencephalography: surgical methodology, safety, and stereotactic application accuracy in 500 procedures.”. Neurosurgery. 2013;72.3:353–366. doi: 10.1227/NEU.0b013e31827d1161. [DOI] [PubMed] [Google Scholar]
- 13.González-Martínez J, Bulacio J, Thompson S, Gale J, Smithason S, Najm I, Bingaman W. Technique, results, and complications related to robot-assisted stereoelectroencephalography. Neurosurgery. 2016 Feb 1;78(2):16980. doi: 10.1227/NEU.0000000000001034. [DOI] [PubMed] [Google Scholar]
- 14. https://www.zimmerbiomet.com/medical-professionals/cmf/rosa-brain.html .
- 15.Menachemi N., Collum T. H. Benefits and drawbacks of electronic health record systems. Risk Management and Healthcare Policy. 2011;4:47. doi: 10.2147/RMHP.S12985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Health Level7. HL7 International website. Available at: http://www.hl7.org Accessed July 28, 2020.
- 17.Bostock M, Ogievetsky V, Heer J. D3 data-driven documents. IEEE transactions on visualization and computer graphics. 2011 Nov 3;17(12):2301–9. doi: 10.1109/TVCG.2011.185. [DOI] [PubMed] [Google Scholar]
- 18.Ferraiolo D, Kuhn DR, Chandramouli R. Artech House; 2003. Role-based access control. [Google Scholar]
- 19.Fielding RT, Taylor RN. Irvine: University of California, Irvine; 2000 Jun. Architectural styles and the design of network-based software architectures. [Google Scholar]
- 20.Brooke J. “SUS: A “quick and dirty” usability scale”. In: Jordan P. W., Thomas B. A., Weerdmeester, McClelland I. L., editors. In Usability evaluation in industry. London: Taylor & Francis; 1996. pp. 189–194. [Google Scholar]
- 21.Bangor A, Kortum PT, Miller JT. An empirical evaluation of the system usability scale. Intl. Journal of Human– Computer Interaction. 2008 Jul 29;24(6):574–94. [Google Scholar]