Abstract
Among the multiple challenges faced by children from low- and middle-income countries (LMICs) with congenital heart disease (CHD), the economics of care remains foremost, contributing significantly to morbidity and mortality. This paper evaluates the four existing finance models available for healthcare systems and proposes a new model—the GIVE model (government, institutions and individuals, values, and engagements)—as the fifth model for global sustainable healthcare systems. The paper presents an evaluation of a chain of three paediatric cardiac hospitals in India to assess the sustainability of their philanthropy-based operational model, through which surgeries are offered completely free of cost to children with CHD. The three Sri Sathya Sai Sanjeevani Centres for Child Heart Care in India have been proponents of this philanthropic model for over a decade. From February 2013 to January 2024, 19,684 patients with CHD received surgeries at no cost. The average cost of surgery was reported to be USD (United States Dollar) 1800. A case study of one of the Sanjeevani Centres showed that 23.8% of patients were in STAT Category 3 and above, as defined by the Society of Thoracic Surgeons-European Association for Cardio-Thoracic Surgery, with an in-hospital mortality rate of 2.08%. The evaluation highlighted the institution’s numerous strategies to enable sustainability in key aspects of operations, economics, and social impact. Despite challenges, the Sai Sanjeevani philanthropic model, which encompasses both economic and social impact, is dependable and can be replicated. The proposed GIVE model is recommended for adoption by LMICs as a global way forward to enable free CHD surgeries through sustained philanthropy, strengthened by a shared vision and collaborations.
Keywords: Congenital heart disease, CHD, Free healthcare, Philanthropy, Sustainability, GIVE model, India, Sri Sathya Sai Sanjeevani, Low-middle income countries
Introduction
Universal health coverage (UHC) aims to ensure equity in access to healthcare, provide a comprehensive range of need-based services, and shield individuals from the economic burden associated with seeking medical care. The explicit inclusion of UHC in the United Nations (UN) Sustainable Development Goals (SDG) Goal 3–Good Health and Well-being and World Health Organization (WHO) programmatic objectives emphasises its heightened focus in global policies [1]. World Health Organization and World Bank published measurement framework identifiers—promotion, prevention, treatment, rehabilitation, and palliation as the services to be included to ensure UHC [2]. With over 150 million (M) individuals annually estimated to be pushed to poverty around the world, access to healthcare and UHC is an issue which is far from addressed, particularly in lower to middle Sustainable Development Index (SDI) countries [3]. In the Indian context, 62% dependence on the private sector for healthcare services exacerbates accessibility issues, especially for low-income individuals. Rural India is grappling with inadequate infrastructure and shortage of medical and nursing professionals and thus continues to experience poor access to healthcare services [4, 5].
Congenital heart diseases—unveiling global challenges
Congenital heart diseases (CHD) account for one-third of all congenital birth defects [2, 6]. The global incidence of CHD varies, but it is estimated that approximately 8 to 12 in 1000 live births globally or 1.35–1.4 M infants are born every year with CHD, of which 25% die in their first year [6–10]. The prevalence number is more alarming at close to 12 M [6].
A status report on availability, access, and funding across 193 countries highlights insufficient or intermittent care in more than 75% of the countries, particularly across most parts of Africa, Asia, and South America. Lower SDI countries are found to be reporting higher CHD mortalities, indicating a direct relationship between income levels and CHD mortalities [7, 11]. A marked variation is also reported on the costs of paediatric cardiac surgeries estimated to be between United States dollar (USD) 800–6000 in India, USD 10,000 in Africa, and between USD 12,000 and 50,000 in the USA (United States of America), with out-of-pocket expenditure as the most prevalent financing option [8, 12].
Tiny hearts, big challenges—the India story
The India Newborn Action Plan emphasises focus on child survival programs, systems, and delivery platforms as an essential step towards the country’s commitment to child health [13]. It is estimated that each year in India, around 240,000 children (8 out of 1000 live births) are born with CHDs [13, 14]. Congenital heart disease–related mortality accounts for close to one-third of all mortalities due to congenital defects and less than 5% of babies born with critical CHD undergo receive definitive treatment [15, 16]. This indirectly contributes to deaths due to birth defects, which are the third leading cause of neonatal mortality in over 70% of Indian states [17].
Demand–supply gap
Of the total CHD children born each year, about one-fifth require early intervention in the first year to survive. The burden staring at the country is grave with the annual paediatric cardiac surgeries conducted being much lesser than the estimated prevalence of 2 M children with CHD [6, 18]. Close to 150 practicing paediatric cardiac surgeons address this large problem, which falls short of the estimate that the country needs 300–500 paediatric cardiac programs or 1000 paediatric cardiac surgeons to meet accessibility requirements [12, 19].
Access inequities
Geographical disparities further exacerbate the challenges impacted by factors including varying birth rates, concentration of paediatric cardiac services in South India, delayed diagnoses, and limited access to timely interventions in rural India [14].
Unaffordable care
Most centres caring for CHDs are in the private sector and are therefore not affordable for most of the Indian population. Very few studies attempt to estimate the number of families who painfully wait for some financing option as their little one continues to grow with increasing morbidities. With India’s per capita net national income (NNI) being less than USD 1200, paediatric cardiac surgeries are unaffordable by most families [20]. Among those who access care, a shocking 35% of paediatric cardiac surgeries are funded by families themselves, 40% by government schemes, 20% by hospitals run by charitable and non-government organisations, and 5% by other ad hoc financing programs [14]. This need supply gap is also reflected in the huge waiting lists under charitably run programs.
The need for free CHD surgeries: an investment not an expenditure
Access to free paediatric cardiac surgeries is both a moral duty and an economic necessity. It reflects a society’s commitment to its vulnerable members and prevents long-term consequences of untreated CHDs, fostering a generation vital for economic growth. The trauma of not being able to save one’s child is a poor statement of a society or a nation’s humaneness. A CHD child is rightly described ‘a child whose name is Today’, for many a time it has no tomorrow.
The inability to afford surgical expenses can strain finances, impacting essential needs like education and housing. Conversely, providing free surgeries reduces economic burdens on families and society, with each surviving child potentially contributing significantly to national income, making free cardiac care a societal imperative. A study conducted in low-middle income countries (LMICs) for cost-effectiveness of humanitarian missions for free CHD surgeries reports that each surviving child potentially gains 39.9 disability-adjusted life-years averted and potentially contributes USD 159,533 in gross national income per capita at purchasing power during his or her extended lifetime [21].
Exploring financing models for affordable paediatric cardiac care
To evaluate the need and relevance of sustainable philanthropy for CHD care, it is essential to examine current models of healthcare systems. Four prominent models have evolved over decades to meet varying patient and system needs [22].
Beveridge model
Where healthcare services are publicly funded and provided, it is relevant to CHDs, but often in low SDI countries it faces challenges of mid to severely inadequate infrastructure, insufficient skilled specialists, insufficient medical supplies, and compromised quality.
Bismarck model
Where healthcare services rely on mostly mandatory social insurance contributions/premium, it is found challenging in the context of middle and low SDI countries, including India, which do not implement the model due to employment and affordability issues.
National health insurance
Where elements of both Beveridge and Bismarck models are combined, it has the potential of offering comprehensive coverage for CHD patients, by balancing public and private strengths to meet the goals of national paediatric cardiac care. Two examples stand out in the context of Indian Child Health.
Rashtriya Bal Swasthya Karyakram (RBSK)—a flagship scheme of the Government of India, launched in 2013, which focusses on identification, prevention, and management and medical, surgical, and therapy-based, child health and also empanels healthcare institutions to provide care for screened patients across 32 conditions, including congenital defects [14, 23, 24].
Ayushman Bharat and state-run programs—launched in 2018, the Pradhan Mantri Jan Arogya Yojana (PM-JAY), a part of the Government of India’s Ayushman Bharat Program, is the world’s largest health insurance scheme, providing financial protection to close to 500 M beneficiaries, including 107.5 M poor, deprived rural families and other identified underprivileged workers [25, 26]. With regard to CHDs, the program covers a wide range of CHD presentations through empaneled hospitals, covering all the costs. However, low package bands (ranging between USD 350 and 1500 based on the condition), reimbursement delays, and state-level implementation variations continue to be challenges [27, 28]. Certain states also run dedicated CHD programs towards increased reach.
Out-of-pocket
Which is estimated at an alarming 62.6% of overall healthcare expenditure in India, impacting households and underscoring the need for comprehensive insurance coverage [29].
Introducing the GIVE model—the 5th model for a sustainable healthcare system
Healthcare systems globally have made significant clinical progress and increased availability of care but struggle to adequately meet the burden of paediatric cardiac issues, evident in the prevalence of CHD. Addressing this challenge necessitates a paradigm shift. This paper defines a new approach—the GIVE model that integrates key strengths of the current models and builds on them (Table 1). At the core of the GIVE model lies the acknowledgment that ‘giving is intrinsic to human nature’. It stems from the virtue of compassion, going beyond the nuances of a balance sheet.
Table 1.
New proposed model for sustainable healthcare
| G | Governments |
Prioritise CHD care in national child health policy Define national frameworks for CHD screening, treatment, research, training, and philanthropy Strengthen public infrastructure Implement engagement programs with private and charitable organisations to address more children |
| I | Institutions and individuals |
Build institutions of healthcare excellence for comprehensive CHD care Prioritise CHD philanthropy—infrastructure, screening, treatment, research, training, advocacy, and awareness programs Offer infrastructural, medical, strategic, and operational voluntary services towards strengthening CHD programs |
| V | Values |
CHD institutions, programs, and healthcare professionals exemplifying social values of love, compassion, equality, and service Shift from human capital to human development approach [30] |
| E | Engagements |
Strategic instruments for universal CHD care Collaborative multistakeholder engagements between governments, institutions, and the society Value creation goals, impact outcomes, and pathways Informed policy, implementation, advocacy, learning, research, and funding [31] |
Philanthropy in CHD care
The evolution of philanthropy in CHD has shifted from sporadic donations to comprehensive support, focusing on underserved populations. Specialised teams from developed countries conduct surgeries and aid capacity-building in LMICs through humanitarian missions, benefiting children, training local teams, and strengthening healthcare systems [32]. Some organisations prioritise awareness campaigns, long-term support programs, and innovation in diagnostics and treatment through translational research. This facilitates the creation of a shared vision between socially motivated individual and institutions creating a collaborative and sustainable model which fits into the GIVE framework.
What is sustainability?
Every model, more in the healthcare space, needs to be scalable and sustainable. Sustainability is often viewed by policy makers, economic experts, and societal influencers through the prism of finance alone. Numerous studies on sustainability have defined social sustainability as the process of addressing social concerns while confronting risk, and an integration of social values and economic risk [33, 34]. However, there is a need for more systemic reviews on social sustainability [35].
Over the years, it is established that the social sector is a non-negotiable partner in achieving global sustainable development goals [35]. With regard to CHD care in India, charitable or non-governmental organisations already contribute to 20% of all care provided. This paper aims to evaluate the proposed GIVE model and its sustainability, defined as social impact and economics, through the study of Sri Sathya Sai Sanjeevani Centres for Child Heart Care, India.
The Sri Sathya Sai Sanjeevani story—exemplifying sustainable philanthropy
Twenty-nine thousand twelve free CHD surgeries and interventions in 11 years—face of the unknown Indian child
Background
Sri Sathya Sai Sanjeevani Hospitals (SSSSH) in India commenced their journey in 2012 with a vision to serve the cause of ‘Right to Healthy Childhood’ through creation of a holistic ecosystem resulting in reducing the global CHD burden. The first Centre for Child Heart Care was set up in Nava Raipur, Chhattisgarh, India, in November 2012. In November 2016, the second Sri Sathya Sai Sanjeevani International Centre for Child Heart Care & Research was inaugurated in Palwal, Haryana, and the third Centre was set up in Navi Mumbai, Maharashtra, in 2018. The fourth centre is set to commence paediatric cardiac surgeries in the state of Telangana in 2024 (Fig. 1).
Fig. 1.

Sri Sathya Sai Sanjeevani Centres for Child Heart Care
Today Sai Sanjeevani Hospitals are the largest dedicated centres providing totally free of cost paediatric cardiac care for children with CHDs. The hospitals provide the entire spectrum of paediatric cardiac services to families accessing care including outpatient consultations, echocardiography (ECHO), radiology, pre-admission care, surgery/catheter-interventional procedures, post operative care, laboratory investigations, medicines, nutritional supplements, and counselling services. All these services are provided totally free of cost to all. To alleviate the financial strain on families with limited income, the hospital also provides complimentary accommodation and meals to patient attendants for the entire duration of treatment on the hospital premises.
Infrastructure and impact
‘Healthcare for the poor does not mean poor healthcare’
The SSSSH are equipped with state-of-the-art technology ensuring the children receive the best medical attention. The centres are staffed by an exemplary team of paediatric cardiac specialists, medical professionals, skilled nursing staff, and paramedical teams, deeply committed to serving the needs of the children seeking care (Table 2).
Table 2.
Infrastructure of Sai Sanjeevani Centres for Child Heart Care
| Paediatric cardiac operation theatres (OT) | 10 |
| Paediatric cardiac cath labs | 3 |
| Dedicated beds | 300 |
| Paediatric cardiac intensive care unit (ICU) beds | 145 |
| Specialists | 38 |
| Manpower: medical, nursing, paramedical, administrative, and support staff | 902 |
As of 31 January 2024
For the period Feb 2013 to January 2024, the three operational centres managed 245,343 paediatric cardiac outpatients and conducted 29,012 procedures—19,684 paediatric cardiac surgeries and 9328 paediatric cardiac catheter-interventions from all states of India and 12 developing countries. Table 3 categorises the surgeries conducted into the STAT risk categories defined by the Society of Thoracic Surgeons-European Association for Cardio-Thoracic Surgery; a tool used to analyze risk of mortality for paediatric cardiac surgeries [36].
Table 3.
STAT classification of CHD surgeries conducted by Sai Sanjeevani Centres, Feb 2013–June 2023 [36]
| Overall mortality | 1.38% |
|---|---|
| STAT 1 | 47.1% |
| STAT 2 | 44.8% |
| STAT 3 | 1.9% |
| STAT 4 | 6.2% |
| STAT 5 | 0.0% |
Comprehensive approach to CHD
Sri Sathya Sai Sanjeevani acknowledged the necessity of embracing a comprehensive strategy for managing CHDs, by implementing a multifaceted approach, incorporating diverse initiatives focused on prevention, early detection, treatment, training, and research to pilot an ecosystem approach to address the prevalence of CHD.
Mother and child health (MCH)
Recognising the interconnected health of both MCH, the first totally free of cost Mother & Child hospital was set up in Nava Raipur (Chhattisgarh) in 2021. Upon the invitation of governmental, social, and private parties across states, four more Mother & Child hospitals were operationalised in a span of 1 year in Palwal (Haryana), Yavatmal (Maharashtra), Raiwala (Uttarakhand), and Jamshedpur (Jharkhand). The hospitals provide the entire spectrum of maternal care for rural and tribal pregnant women. Free fetal ECHO services are also offered by the Departments of Pediatric Cardiology at the centres, particularly for the detection of complex anomalies and to enable informed pregnancy decision based of probable postnatal outcomes [37, 38]. The hospitals also work closely with district administrations to integrate national- and state-level maternal health programs like the Janani Suraksha Yojana, Janani Shishu Suraksha Yojana, and ASHA (Accredited Social Health Activist) program.
Screening
To address the estimated prevalence of CHDs in schools (3.8 out of 1000 school children [39]), the hospitals initiated the Divine Mother & Child Health Program in September 2017 which is a comprehensive antenatal and CHD screening program for rural children. This is a comprehensive early detection and systemic health screening initiative based on the Government of India’s RBSK program. Dedicated outreach programs screen children for CHDs in government-run anganwadi centres (rural child care centres) and schools and refer them to Sai Sanjeevani Hospitals for confirmatory ECHO tests and treatment, as required [40]. The number of children screened for CHDs from September 2017 to January is 206,527.
Training
The availability of paediatric cardiac specialists, nursing, and paramedical teams is considered a major barrier in ensuring paediatric cardiac care. The hospitals conduct numerous academic, training, and skill development programs for doctors, nurses, and allied healthcare providers to contribute to national capacities and inspire young specialists to expand paediatric cardiac services in the country. All courses offered by the hospitals are again totally free of cost, thus removing any financial barriers for bright medical and paramedical providers to get trained. Some of the courses offered include:
Doctorate of National Board (DrNB) in Pediatric Cardiology under the National Board of Examinations—India, Institutional Fellowships in Paediatric Cardiac Surgery, Paediatric Cardiac Anaesthesia, and Paediatric Cardiology—46 specialists trained.
Masters in cardiothoracic nursing by the Sri Sathya Sai Sanjeevani Institute of Nursing & Allied Healthcare Sciences—53 nurses trained.
Specialised training for nursing, paramedical, and technical staff (including critical care nursing, ECHO technicians, X-ray technicians, lab technicians, OT assistants, physician assistants, physiotherapists, perfusionists, and bio-medical engineers)—187 nurses and technicians trained.
Research
The Sri Sathya Sai Sanjeevani Research Centre for CHDs was set up in 2018 to understand and contribute to ‘life’ through the pursuit of advanced human genomic research in CHD. Housing two biobanks with over 6000 heart tissue and blood samples, the Research Centre, run by dedicated researchers, envisions to do collaborative work on finding causes and solutions to address the issue of CHDs.
The case of Sai Sanjeevani, Kharghar, Navi Mumbai, Maharashtra, India
To get a more comprehensive view on patient care parameters, the full journey of Sri Sathya Sai Sanjeevani Centre for Child Heart Care, Kharghar, Navi Mumbai, Maharashtra, is being discussed. The centre commenced outpatient services in November 2018. With basic infrastructure including one operating room and a six-bedded ICU, the first surgical procedure was performed in May 2019. By the end of the year, 125 free CHD surgeries were conducted with no mortality. As work progressed amidst scaling of infrastructure and manpower building, clinical care was affected by the pandemic with Mumbai being one of the worst affected cities of India during the coronavirus disease (COVID-19) pandemic. This was in line with the trend seen across 24 paediatric cardiac centres in India which reported 66.8% reduction in inpatient admission between 2019 and 2020 [41]. Soon services reopened with strict protocols and patient testing, amidst restricted travels for patient families and supply chains for consumables. Soon the centre expanded to a new OT—Cath lab—ICU complex, with two operating rooms, one cath lab, and a 26-bedded cardiac ICU.
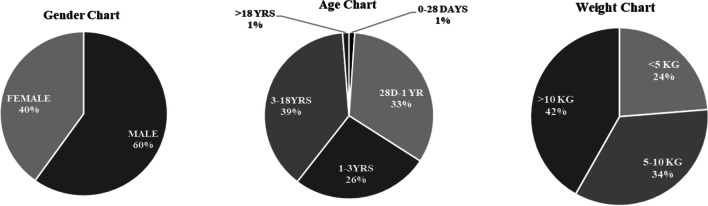
Analysis of retrospective data of the hospital highlights that 2541 paediatric cardiac surgeries were conducted by the hospital in the period May 2019–January 2024, all totally free of cost. This included both primary and redo procedures on the same patient (surgery for complication or revision of procedure or residual defects) or new staged procedures, but excludes reoperations for bleeding, pacemaker insertion, and wound debridement. Key areas in which patient data was captured were weight, age, gender, Society of Thoracic Surgeons (STS) category, cyanotics/acyanotics, morbidity, mortality, and ICU stay (Table 4; Table 5). The overall mortality rate was 2.08%. The average ICU stay across all STAT categories, inclusive of main and step-down ICU stay, was 2.65 days for 82% children, 7.29 days for 11% children, and 13.5 days for 7% children. Among the operated, 34.16% of children were neonates and infants and 23.73% were less than 5 kg (Fig. 2). The Kharghar Centre is currently revising its protocols to share data with the International Quality Improvement Collaborative (IQIC). Going forward, the Sai Sanjeevani centres will have a joint database, with other like-minded programs, capturing the data of the all children who have received treatment thus far.
Table 4.
Type of CHD surgeries conducted at Sri Sathya Sai Sanjeevani Centre for Child Heart Care, Kharghar, Navi Mumbai
| Surgical procedure | Total cases performed | Mortality | % Mortality |
|---|---|---|---|
| ASD closure | 341 | 0 | 0% |
| VSD closure | 968 | 09 | 0.92% |
| TOF repair (annulus sparing) | 219 | 0 | 0% |
| AVSD repair | 47 | 02 | 4.25% |
| SAM excision | 04 | 0 | 0% |
| PAPVC repair | 58 | 0 | 0% |
| DCRV repair | 04 | 0 | 0% |
| Pulmonary valvotomy | 01 | 0 | 0% |
| CoA repair | 24 | 0 | 0% |
| RSOVA repair | 01 | 0 | 0% |
| TOF repair with TAP | 412 | 11 | 2.66% |
| ALCAPA repair | 04 | 0 | 0% |
| PDA ligation | 51 | 01 | 1.96% |
| TV repair | 06 | 0 | 0% |
| BDG | 64 | 02 | 3.12% |
| AP window closure | 14 | 0 | 0% |
| MV repair | 03 | 0 | 0% |
| RVOTO relief | 06 | 0 | 0% |
| ROSS procedure | 03 | 0 | 0% |
| Atrial septation | 06 | 0 | 0% |
| Aortic valve repair | 02 | 0 | 0% |
| Cor-triatriatum | 01 | 0 | 0% |
| Implantation of RPA-MPA | 06 | 01 | 16.6% |
| Rastelli/Nikaidoh procedure | 09 | 01 | 11.11% |
| ASO | 12 | 02 | 10.8% |
| Fontan completion | 06 | 01 | 16.6% |
| Double aortic arch repair | 04 | 0 | 0% |
| Potts shunt | 01 | 0 | 0% |
| RV-PA conduit | 09 | 01 | 11.11% |
| TAPVC repair | 115 | 06 | 5.21% |
| Truncus repair | 11 | 03 | 27.27% |
| PA banding | 05 | 0 | 0% |
| Aortic arch repair | 14 | 01 | 7.14% |
| IVTR for DORV | 10 | 01 | 10% |
| Senning repair | 06 | 01 | 16.6% |
| Cone repair for Ebstein’s anomaly | 08 | 0 | 0% |
| ASO + VSD closure | 34 | 05 | 14.7% |
| Left atrial (LA) myxoma | 02 | 0 | 0% |
| ASO + arch repair | 01 | 0 | 0% |
| Double switch operation | 02 | 02 | 100% |
| Norwood procedure | 02 | 02 | 100% |
List of surgeries placed in order of complexity, excludes redo procedures on the same patient (surgery for complication or revision of procedure or residual defects), ASO arterial switch operation, CoA coarctation of aorta, RVOTO right ventricular outflow tract obstruction, RSOVA ruptured sinus of valsalva aneurysm, RPA right pulmonary artery, TAP trans annular patch, MPA main pulmonary artery, ALCAPA anomalous left coronary artery from pulmonary artery, ASD atrial septal defect, PDA patent ductus arteriosus, VSD ventricular septal defect, TV tricuspid valve, TOF tetralogy of Fallot, BDG bidirectional Glenn, AVSD atrio ventricular septal defect, AP aorto pulmonary, SAM sub aortic membrane, MV mitral valve, PAPVC partial anomalous pulmonary venous connection, TAPVC total anomalous pulmonary venous connection, DCRV double-chambered right ventricle, IVTR intraventricular tunnel repair, AV repair aortic valve repair, RV-PA conduit right ventricle to pulmonary artery conduit
Table 5.
Morbidities reported
| Neurological deficits | 1 | 0.04% |
| Renal failure | 1 | 0.04% |
| Chylothorax | 12 | 0.47% |
| Paralysis of diaphragm | 4 | 0.16% |
| Blood stream infections | 83 | 3.27% |
| Urinary infections | 0 | 0.00% |
| Ventilator associated infections | 6 | 0.24% |
| Deep sternal infections | 6 | 0.24% |
| Re-intubations | 21 | 0.83% |
Fig. 2.
Gender, age, and weight distribution of 2541 CHD surgeries in Sai Sanjeevani, Kharghar (May 19–Jan 24)
Assessment using the GIVE model
This section attempts to evaluate the SSSSH’s work using the GIVE model introduced in this paper as the fifth model for healthcare systems.
Governments
Ensuring that all citizens have access to essential health services without facing financial hardship is the principal responsibility of the government through policy and regulation, health financing, infrastructure and capacity development, public awareness, quality standards, and partnerships. Recognising that the vision of the SSSSH is aimed at achieving and strengthening the government’s efforts to achieve UHC for MCH, the hospitals work closely with the Government of India and respective state governments to integrate with existing MCH programs. Particularly for CHDs, the Rashtriya Bal Swasthya Karyakram of the Government of India aims to screen, diagnose, and treat CHDs also powered by the Ayushman Bharat. SSSSH have signed memorandums of understanding (MOUs) under RBSK with the states of Chhattisgarh, Odisha, Uttarakhand, Uttar Pradesh, Maharashtra, Telangana, and Haryana, thus becoming a referral centre for CHDs.
Institutions and individuals
Hospitals of this scale and vision is only possible through the vision and strategic direction of the leadership, which is provided by the three trustees and six members on the board of advisors, who are dedicated and inspired leaders with a commitment to provide solace to parents whose children suffer unfortunate condition, understanding that it is not a matter of choice, but it is the only choice [40]. It is a constant effort by the leadership to recruit like-minded medical, nursing, paramedical, and administrative staff members, passionate about giving back to the society. The model exemplifies individual-, team-, and organisation-level social entrepreneurship to address one objective of quality, sustainable and free of cost CHD care for the underprivileged.
The inception of Sai Sanjeevani Hospitals was marked by the generous philanthropic contributions from both individual and institutional donors within the community who supported the cause of accessible child healthcare. Sai Sanjeevani continues to run and grow due to the continued philanthropy—CSR and individual, having the shared vision of addressing national MCH. Those individuals, genuinely inspired by the success of the free healthcare model, made substantial contributions, thereby significantly contributing to the well-being and future health of numerous beneficiaries [40]. Additionally, long-term engagements and associations with vendors, volunteers, and medical fraternity contribute to quality of care, beneficiary experience, and cost efficiencies.
Values
The values of love and service drive the efforts of Sai Sanjeevani. The investment made by Sanjeevani in saving a child’s life goes beyond the money spent. A child’s life is more important and precious than the money involved in saving it. By saving the child, the hospitals believe they restore humanity and faith in each other, like we did in saving lives in COVID times. No questions were asked; only the will and means to save life made sense. The SSSSH give face and voice to the unknown Indian child by providing each child and their family the primary right of dignity to life.
Every centre has a dedicated impact assessment and counselling team for managing in-hospital queries and stress and long-term follow-up of children treated at Sanjeevani Hospital for CHD to track their progress, social impact, and transformation in a program called Ab Zindagi Sanjeevani ke Saath (Life with Sanjeevani). Every discharge at Sanjeevani is a special event. Every discharged family is explained about the support provided by society for their child, also highlighting their increased responsibility in taking special care of the child and ensuring that the child grows to live the values of giving back to society. This connection to each family reflected in the presence of over 3000 children coming together in Sai Sanjeevani, Nava Raipur, to light oil lamps in celebration of the centre’s 10th-year anniversary, setting a new record under the Guiness World Records.
Engagements
Powerful engagements are binding factors that can potentially enable innovative approaches, mobilise expertise, broaden resource access, and foster accountability. SSSSH have fostered numerous engagements across verticals to power collaborative intent, vision, and efforts to achieve their social goals. Some key engagements with the private and social sectors include:
Training—National Board of Examinations, Maharashtra University of Health Sciences, Indian Nursing Council, Children’s HeartLink, SRM University, DY Patil University
Research—National University of Singapore; Advanced Centre for Treatment, Research and Education in Cancer; SRM University
Public Health—National Institute of Public Health and Research for Public Health
Evaluating sustainability of SSSSH
The sustainability of Sri Sathya Sai Sanjeevani model is being evaluated using two key parameters—economics and social impact.
Economics
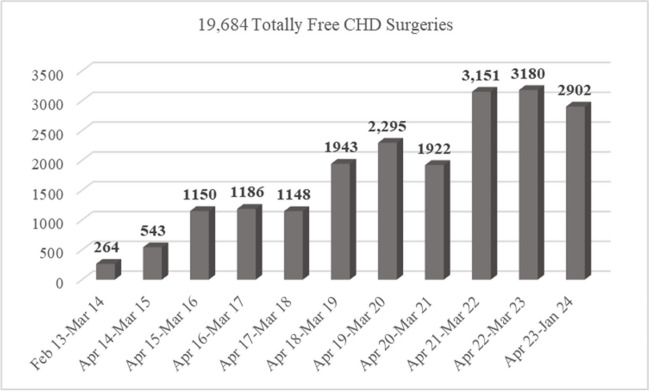
In times when profitability drives business models, SSSSH, in 11 years, have conducted over 29,000 paediatric cardiac surgeries and cath interventions, totally free of cost. The model has seen an increase in the number of CHD procedures conducted year on year reflecting its sustainability (Fig. 3).
Fig. 3.
Graph of year on year growth of Pediatric Cardiac Surgeries at Sri Sathya Sai Sanjeevani Centres for Child Heart Care. Data considered up to 31 January, 2024
Cost of services rendered
Since inception in 2012, SSSSH have raised and invested over Indian rupee (INR) 4.85 billion (B) (~ USD 58.4 M) in building hospital infrastructure (four child heart centres—three operational and one upcoming) and conducting paediatric cardiac surgeries, amounting to INR 2.95 B (~ USD 35.4 M), strongly establishing that the GIVE model is not just sustainable, but also scalable (Table 6).
Table 6.
Calculating the cost of services rendered by SSSSH for the period Feb 2013–Jan 2024
| Average cost of paediatric cardiac surgery at SSSSH* |
INR 150,000 (USD 1800) |
| Total number of paediatric cardiac surgeries conducted for the period Feb 2013–Jan 2024 | 19,684 |
| Total cost of child heart services |
INR 2.95 B USD 35.4 M |
*Inclusive of all services—outpatients, radiology, pathology, blood services, surgery, intensive care, inpatient care, physiotherapy, dietetics, food, and accommodation of families. Foreign exchange rates as of May 2024
The actual cost of surgery was reported to be INR 150,000 (USD 1800), based on the risk, comorbidities, age, weight, complications, and presence of major non-cardiac anomalies [40, 42]. SSSSH have managed to bring the costs down significantly by building economies of scale, operational efficiency, and sensitising hospital teams to avoid any wastage of resources, without any compromise on patient outcomes. With an expected increase in the number of cases in the coming years, the centres plan to monitor costs stratified by CHD category, age, and weight.
Philanthropy and corporate social responsibility (CSR)
Philanthropy in its traditional sense, donation of money by individuals and institutions for good causes, continues to be the binding factor between society and institutions.
In the Indian context, the country embarked on a bold experiment in mandating CSR for large companies, requiring spending at least 2% of profits in CSR, among other frameworks, through tightly defined and scrutinised processes by the Government of India [43]. As per published data by the Government of India—CSR portal, for the financial year 2021–2022, 19,043 companies participated in the CSR program with over 43,338 projects. The total national spend on CSR across 14 development areas for the aforesaid period was INR 262.78 B (~ USD 3166 M) [44]. The soul of this act is the responsibility for corporates to give back to society what they have gained from it to address poverty, education, health, sanitation, skill, water needs, among others [45]. Some key aspects of the CSR program that are encouraging for institutions attempting to provide free CHD care and healthcare are [46]:
% of companies have healthcare as first priority—26%
% companies prefer institutions with government partnerships—55%
% companies prefer 3-year project durations—64%
% of companies prefer sustainable implementing agencies—55%
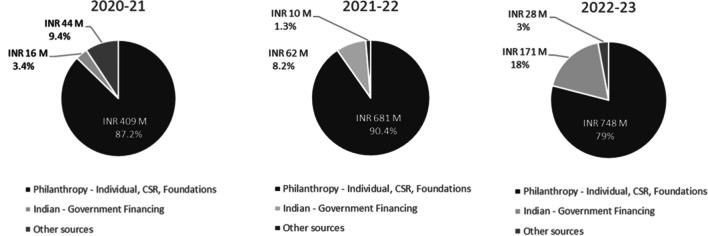
With regard to SSSSH, a study of the trust’s annual financial reports highlights that funds received through donations (including individuals, CSR programs, and Indian foundations) for three financial years (FY 2020–2021, 2021–2022, and 2022–2023) were INR 409 M, INR 681 M, and INR 748 M respectively. Each year has witnessed a significant increase of fund inflow through donations indicating a strong relationship of faith built with donors, thus indicating sustainability. Another critical aspect of philanthropy that has driven sustainability is the operational efficiency, governance, and transparency of the institutions that influences donor trust, relationship, and retention.
Increased Government Support
With regard to SSSSH, support from the governments increased from 3.4% of all fund sources on 2020–2021 to 18% in 2022–2023, thus diversifying the risks from the philanthropy mode of funding, strengthening the model (Fig. 4).
Fig. 4.
Sources of funds for Sai Sanjeevani Hospitals for 3 financial years. INR - Indian Rupee, M - Million
Social impact
Since 2012, SSSSH have made a significant social impact through their steadfast commitment to the tenet of ‘one world-one family’. This visionary approach has not only transformed lives but has also set a precedent for global healthcare, with compassion and inclusivity at its core.
At a macro level, the key impact areas of the hospitals are:
Establishment and running of three Centres for Child Heart Care for 11 years
Establishment and running of five Mother & Child hospitals for rural pregnant women for 3 years
Over 29,000 totally free of cost child heart surgeries and interventions in 11 years
Technical expertise and system strengthening support to address the burden of CHDs in LMICs by helping set up two philanthropy-based paediatric cardiac hospitals in the Fiji Islands and Sri Lanka.
While the impact achievements of Sai Sanjeevani Hospitals, through its free of cost model, are undeniable, it is crucial for us to look beyond the statistics and delve into the profound impact on social values and the lives of families benefiting from the provision of free healthcare.
An independent third-party study was conducted by the Social Audit Network [47], India, to measure the impact of Sai Sanjeevani Hospitals with a societal perspective for the period Apr 2018–Mar 2021, defined as all aspects of affordability, acceptability, and social return.
Affordability
The study reported costs of paediatric cardiac surgeries across 12 states of India varying from INR 175,000 to INR 425,000 (USD 2000 to USD 5000). While at Sai Sanjeevani, none of the parents had to pay anything for their child’s treatment, without which they would have been driven to poverty by selling their property and other movable assets or taking loans from friends, family, or money lenders (Fig. 5).
Fig. 5.

Feedback from beneficiary families on the potential financial risk averted
Socioeconomic profile
Seventeen percent of the beneficiaries were reported to be from the most underprivileged socioeconomic strata of the society based on the Kuppuswamy Scale [48]. The majority of patients served report a monthly salary of between INR 7887 and INR 13,160 (USD 100–USD 150).
Impact on child health
Over 81% of families reported a remarkable level of improvement in the symptoms of their children. The majority of parents also reported a significant improvement in school attendance, performance, and participation (Fig. 6).
Fig. 6.

Feedback from beneficiary families on improvement in their child’s health post-surgery
Impact on families
The hospitals have not only delivered ‘the gift of life’ to thousands of children—our future generation—but has also offered joy to thousands of parents and families since its beginnings, thus transforming into institutions spreading health and goodness in the society (Fig. 7).
Fig. 7.
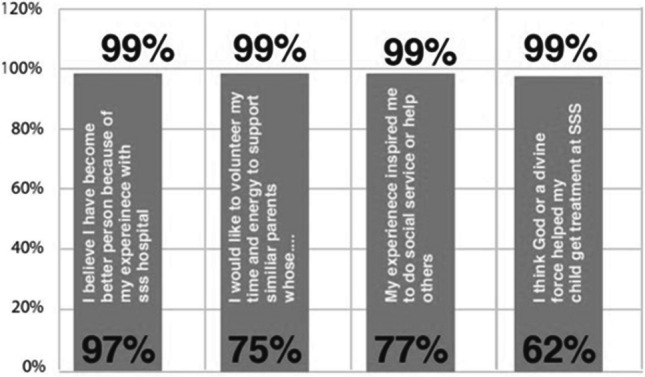
Feedback from beneficiary families on impact of Sanjeevani Hospitals on them
Operational sustainability
Continued vision and nurturing young organisation leaders living the values of the institutions were highlighted as key success factors of the model [40]. The study also reported the medical, nursing, and paramedical training programs in paediatric cardiac care contributing back to the operational sustainability of the Sai Sanjeevani model, thus making highly specialised skills available for current and new centres for Child Heart Care.
Social return of investment (SROI)
SROI generates a benefit to cost ratio for organisations to communicate the value-add of their intervention and highlights how social change is created. Considering numerous parameters such as access to effective healthcare, financial benefit to families, savings for beneficiary families, and improved education opportunities as key benefits, the SROI of the SSSSH was reported to be 16.2. Thus, each operation conducted on a child at SSSSH generates a social value 16.2 times more than what was invested.
Global impact
Over the last decade, SSSSH have emerged as global models of Child Heart Care for replication by developing models, focusing on quality care and efficient operations, and serving the underserved. Apart from treating over 145 patients from 17 developing countries who have sought care at the Sai Sanjeevani Hospitals in India, the hospitals have conducted 12 international humanitarian missions for Child Heart Care in the Fiji Islands, Sri Lanka, Nigeria, and Malaysia, resulting in training local specialists, nursing, and paramedical teams.
In order to contribute to global capacities in terms of increase in centres for child heart care, Sai Sanjeevani Hospitals, India, over the last 5 years, have provided training and system strengthening support to organisations in the Fiji Islands and Sri Lanka to set up independent centres for Child Heart Care to provide free of cost screening and outpatient and surgical care to children with CHDs from the region.
Sri Lanka—The SSSSH in Sri Lanka was established in Batticaloa in 2022 in association with the Karuna Nilayam Foundation to address adult and congenital heart conditions. Since commencement up to Jan 2024, the hospital has managed 21 CHD and 36,099 adult outpatients and conducted 11 paediatric cardiac surgeries and 537 adult cardiac interventions, all totally free of cost.
Fiji Islands—The Sri Sathya Sai Sanjeevani Children’s hospital in the Fiji Islands was established in Suva in 2022 by Sai Prema Foundation Fiji to address CHD. Since commencement and until January 2024, the hospital has managed over 14,500 CHD outpatients and conducted 260 paediatric cardiac surgeries, all totally free of cost. The hospital provides free surgeries for children with CHD not only in Fiji, but all the surrounding South Pacific Islands as there is no other facility in the Pacific Islands.
Conclusion
The global burden of CHDs demands urgent attention, particularly for low-middle income countries that face affordability and accessibility challenges. The assertion of this paper is that free care in Child Heart Care is no longer a choice. The case of SSSSH in India that run largely through philanthropy exemplifies collaborations between governments, institutions, and individuals bonded by societal values and provide a possible approach for international and social organisations in low-middle income countries seeking to commence and offer free CHD care through a sustained philosophy. Redefining sustainability as a composite result of both social impact and economics, the paper also marks a departure from a purely financial perspective of sustainability.
The success of the Sri Sathya Sai Sanjeevani model underscores the relevance of adopting a holistic approach, including state-of-the-art infrastructure, service mapping, advocacy, screening, training and education, research and phased growth to ensure sustained care provision, scalable philanthropy, and continued collaborations [49, 50]. The model also highlights the need for organisations to focus on operational efficiencies, transparency, and governance for donor retention, a key contributor to sustainable philanthropy. Collaborations have in them the intrinsic power of partnerships which would be the main driving and success factor towards developing a global strategy for philanthropy driven CHD care in LMICs, as is seen in the cases of Sri Lanka and Fiji.
The paper suggests that providing free CHD surgeries through sustained philanthropy is a possibility and recognises the need for more research to evaluate the GIVE model, relevance of the discussed sustainability model in different geographies and implementation models, success factors for sustained philanthropy, relevance of philanthropy in low-income countries, and global examples on collaborations with regard to CHD care. In the pursuit of this noble goal, it is time for the world to unite, rise to the challenges, and pave the way for a future where every child, regardless of socioeconomic background, can receive the life-saving care they deserve.
Acknowledgements
The authors acknowledge the contributions of Mr. Vivek N. Gour, Mr. Ravikiran Sreepada, and Mr. Niraj Acharya for their editorial and review inputs, which have impacted the completeness of the paper. The authors also extend their gratitude to Dr. Ashish Katewa for his guidance regarding secondary research-related activities and the contributions of Dr. Prachi Kukshal and Dr. Radha Joshi for their resourceful support in building the article’s referencing. The authors express their appreciation to the entire staff at Sri Sathya Sai Sanjeevani Centres for Child Heart Care for their continued service to children with CHDs.
Author contribution
CS, SS, and PRM devised the idea and design of study.
PRM and SJ contributed to literature search.
SJ, PRM, SS, and CS Data collection, analysis and representation.
SJ, PRM, SS, and CS prepared and drafting of initial manuscript.
Funding
None.
Data availability
Not applicable as it is a review article. However, the authors confirm that the data supporting the findings of this study are available within the article or its supplementary material.
Declarations
Ethics committee approval
Not applicable.
Informed consent
Not applicable.
Competing interests
The authors declare that there is no competing interest.
Human and animal rights violation
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Declaration of generative artificial intelligence (AI) and AI-assisted technologies in the writing process.
During the preparation of this work the authors used Openai for minor grammar checks. After using this tool/service, the authors reviewed and edited the content as needed and take full responsibility for the content of the publication.
References
- 1.Lozano R, Fullman N, Mumford JE, Knight M, Barthelemy CM, Abbafati C, et al. Measuring universal health coverage based on an index of effective coverage of health services in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet [Internet]. 2020;396:1250–84. 10.1016/S0140-6736(20)30750-9. Accessed 14 January 2024. [DOI] [PMC free article] [PubMed]
- 2.World Health Organization, World Bank Group. Monitoring progress towards universal health coverage at country and global levels: framework, measures and targets [Internet]. 2014. Available from: https://iris.who.int/bitstream/handle/10665/112824/WHO_HIS_HIA_14.1_eng.pdf?sequence=1. Accessed 14 February 2024.
- 3.Thakur R, Sangar S, Ram B, Faizan M. Quantifying the burden of out-of-pocket health expenditure in India. Public Health. 2018;159:4–7. 10.1016/j.puhe.2018.02.017. Accessed 13 January 2024. [DOI] [PubMed]
- 4.Prinja S, Bahuguna P, Pinto AD, Sharma A, Bharaj G, Kumar V, et al. The cost of universal health care in India: a model based estimate. PLoS One [Internet]. 2012;7. 10.1371/journal.pone.0030362. Accessed 13 January 2024. [DOI] [PMC free article] [PubMed]
- 5.Kumar S, Chen LC, Choudhury M, Ganju S, Mahajan V, Sinha A, et al. Financing health care for all: challenges and opportunities. Lancet [Internet]. 2011;377:532. 10.1016/S0140-6736(10)61884-3. Accessed 7 January 2024. [DOI] [PubMed]
- 6.Zimmerman MS, Smith AGC, Sable CA, Echko MM, Wilner LB, Olsen HE, et al. Global, regional, and national burden of congenital heart disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Child Adolesc Health [Internet]. 2020;4:185–200. 10.1016/S2352-4642(19)30402-X. Accessed 2 January 2024. [DOI] [PMC free article] [PubMed]
- 7.Katewa A. Pediatric cardiac surgery: a status report on availability, access, and funding across 193 countries. Indian J Thorac Cardiovasc Surg [Internet]. 2021;37:190–2. 10.1007/s12055-020-01115-8. Accessed 13 February 2024. [DOI] [PMC free article] [PubMed]
- 8.Hoffman JIE. The global burden of congenital heart disease. Cardiovasc J Afr [Internet]. 2013;24:141–5. 10.5830/CVJA-2013-028. Accessed 2 January 2024. [DOI] [PMC free article] [PubMed]
- 9.Maluf MA, Franzoni M, Melgar E, Hernandez A, Perez R. The pediatric cardiac surgery as a philanthropic activity in the country and humanitarian mission abroad. Rev Bras Cir Cardiovasc [Internet]. 2009;24:VII-IX. 10.1590/S0102-76382009000400003. Accessed 2 January 2024. [DOI] [PubMed]
- 10.Saxena A. Status of pediatric cardiac care in developing countries. Children [Internet]. 2019;6:34. 10.3390/children6020034. Accessed 2 January 2024. [DOI] [PMC free article] [PubMed]
- 11.Wu W, He J, Shao X. Incidence and mortality trend of congenital heart disease at the global, regional, and national level, 1990–2017. Medicine (United States) [Internet]. 2020;99:23. 10.1097/MD.0000000000020593. Accessed 2 January 2024. [DOI] [PMC free article] [PubMed]
- 12.Ramakrishnan S. Pediatric cardiology: is India self-reliant?. Ann Pediatr Cardiol [Internet]. 2021;14:253–9. 10.4103/apc.apc_153_21. Accessed 2 January 2024. [DOI] [PMC free article] [PubMed]
- 13.National Health Mission, Ministry of Health & Family Welfare, Govt of India. INAP - India New Born Action Plan. [Internet]. NHM. 2014. Available from: https://nhm.gov.in/images/pdf/programmes/child-health/guidelines/India_Newborn_Action_Plan_(INAP).pdf. Accessed 2 January 2024.
- 14.Saxena A. Congenital heart disease in India: a status report. Indian J Pediatr [Internet]. 2018;55:1075–1082. 10.1007/BF02724185. Accessed 1 January 2024. [PubMed]
- 15.Baranwal AK, Prinja S, Kaur N, Kumar Baranwal A. Congenital heart disease: would it be the key driver of infant survival during Amrit Kaal (2022–2047)?. Indian Pediatr [Internet]. 2023;60:98–102. Accessed 2 January 2024. [PubMed]
- 16.Press Information Bureau, Ministry of Health & Family Welfare, Govt of India. Status of IMR & MMR in India. [Internet]. 2022. Available from: https://www.pib.gov.in/PressReleasePage.aspx?PRID=1796436. Accessed 2 January 2024.
- 17.Ujagare D, Kar A. Birth defect mortality in India 1990–2017: estimates from the Global Burden of Disease data. J Community Genet [Internet]. 2021;12:81–90. 10.1007/s12687-020-00487-z. Accessed 2 January 2024. [DOI] [PMC free article] [PubMed]
- 18.Saxena A. Pediatric cardiac care in India: current status and the way forward. Future Cardiol. 2018;14:1–4. 10.2217/fca-2017-0084. Accessed 2 January 2024. [DOI] [PubMed]
- 19.Kumar RK. Training pediatric heart surgeons for the future: a global challenge. Ann Pediatr Cardiol. 2015;8:99–102. 10.4103/0974-2069.157020. Accessed 12 January 2024. [DOI] [PMC free article] [PubMed]
- 20.Press Information Bureau, Ministry of Statistics & Programme Implementation, Govt of India. Per capita income - India. [Internet]. 2023. Available from: https://pib.gov.in/PressReleaseIframePage.aspx?PRID=1945144#:~:text=As%20per%20latest%20provisional%20estimate%20published%20on%2031st,72%2C805%20in%202014-15%20to%20Rs.%2098%2C374%20in%202022-23. Accessed 2024 Feb 14.
- 21.Cardarelli M, Vaikunth S, Mills K, DiSessa T, Molloy F, Sauter E, et al. Cost-effectiveness of humanitarian pediatric cardiac surgery programs in low- and middle-income countries. JAMA Netw Open [Internet]. 2018;1:e184707. 10.1001/jamanetworkopen.2018.4707. Accessed 12 January 2024. [DOI] [PMC free article] [PubMed]
- 22.Mitonga HK, Shilunga APK. International health care systems: models, components, and goals. Handbook of Global Health [Internet]. 2020;1–20. 10.1007/978-3-030-05325-3_60-1. Accessed 12 January 2024.
- 23.Chakraborty S, Chakraborty A, Mitra S, Gupta S, Lahiri A, Banerjee N. Evaluation of the Rashtriya Bal Swasthya Karyakram (RBSK): a national children healthcare program in a health district of West Bengal, India. Indian J Public Health [Internet]. 2022;66:307–12. 10.4103/ijph.ijph_1690_21. Accessed 5 January 2024. [DOI] [PubMed]
- 24.Hemapriya AS, Arunkrishna SR, Sundar JS. Insights of Rashtriya Bal Swasthya Karyakram: a strength, weaknesses, opportunities, and threats analysis. Int J Community Med Public Health [Internet]. 2022;9:4279. 10.18203/2394-6040.ijcmph20222926. Accessed 18 January 2024.
- 25.Press Information Bureau, Ministry of Information and Broadcasting, Govt of India. Ayushman Bharat - holistic healthcare for India 2022. [Internet]. PIB: New Delhi; 2022. Available from: https://static.pib.gov.in/WriteReadData/specificdocs/documents/2022/apr/doc202243051901.pdf. Accessed 2024 January 3.
- 26.WHO India. Report on evolution of Ayushman Bharat Pradhan Mantri Jan Arogya Yojana. [Internet]. WHO: India; 2022. Available from: https://iris.who.int/bitstream/handle/10665/354267/9789290229438-eng.pdf?sequence=1. Accessed 2024 January 3.
- 27.Pradhan Mantri Jan Arogya Yojana, Government of India. Empanelment guidelines under Pradhan Mantri Jan Arogya Yojana (PMJAY) [Internet]. PMJAY: India; 2018. Available from: https://pmjay.gov.in/sites/default/files/2018-07/HBP.pdf. Accessed 2024 January 3.
- 28.Controller and Auditor General of India, Govt of India. Report of the comptroller and auditor general of India on performance audit of Ayushman Bharat-Pradhan Mantri Jan Arogya Yojana. [Internet]. 2023. Available from: https://cag.gov.in/en/audit-report/details/119060. Accessed 2024 January 3.
- 29.Sriram S, Albadrani M. Impoverishing effects of out-of-pocket healthcare expenditures in India. J Fam Med Prim Care [Internet]. 2022;11:7120. 10.4103/jfmpc.jfmpc_590_22. Accessed 2024 February 5. [DOI] [PMC free article] [PubMed]
- 30.Bajpai V, Saraya A. Healthcare financing: approaches and trends in India. Natl Med J India [Internet]. 2010;23:231–5. Accessed 2024 January 4. [PubMed]
- 31.Niti Ayog, Govt of India. SDG INDIA Index & Dashboard 2020–21 partnerships in the decade of action. [Internet]. 2022. Available from: https://sdgindiaindex.niti.gov.in/assets/Files/SDG3.0_Final_04.03.2021_Web_Spreads.pdf. Accessed 2024 January 3.
- 32.Nichani S, Nichani S. The unexplored benefits of paediatric cardiac humanitarian work in the developing world. Front Pediatr [Internet]. 2021;9:555085. 10.3389/fped.2021.555085. Accessed 2024 January 19. [DOI] [PMC free article] [PubMed]
- 33.Eizenberg E, Jabareen Y. Social sustainability: a new conceptual framework. Sustainability (Switzerland) [Internet]. 2017;9:68. 10.3390/su9010068. Accessed 2024 January 12.
- 34.Weerawardena J, McDonald RE, Mort GS. Sustainability of nonprofit organizations: an empirical investigation. J World Bus. 2010;45:346–56. 10.1016/j.jwb.2009.08.004. Accessed 2024 January 13.
- 35.Ab Samad NH, Ahmad NH, Suria K. Sustainability of non-profit organizations: a systematic review. Accounting and Finance Research [Internet]. 2023;12:25. 10.5430/afr.v12n2p25. Accessed 2024 January 13.
- 36.Sreenivas C, Prabhatha R, Ragini P, Anagha T, Shaun S. The Sri Sathya Sai Sanjeevani experience: 25,000 free procedures in 10 years [Internet]. 8th World Congress of Pediatric Cardiology and Cardiac Surgery [Internet]. Washington DC; 2023. Available from: https://www.wcpccs2023.org/event/1da8563e-0f65-486c-88df-70c3db431af5/summary. Accessed 2024 February 14.
- 37.Makkar N, Satau G, DeVore GR, Sklansky M. Prenatal detection of congenital heart disease: importance of fetal echocardiography following fetal cardiac screening. Pediatr Cardiol [Internet]. 2022. 10.1007/s00246-022-03032-6. Accessed 2024 January 2. [DOI] [PubMed]
- 38.Simpson JM. Impact of fetal echocardiography. Ann Pediatr Cardiol [Internet]. 2009;2:41–50. 10.4103/0974-2069.52806. Accessed 2024 January 2. [DOI] [PMC free article] [PubMed]
- 39.Liu Y, Chen S, Zühlke L, Babu-Narayan SV, Black GC, Choy M kit, et al. Global prevalence of congenital heart disease in school-age children: a meta-analysis and systematic review. BMC Cardiovasc Disord [Internet]. 2020;20. 10.1186/s12872-020-01781-x. Accessed 2024 January 2. [DOI] [PMC free article] [PubMed]
- 40.Shroff A, Shah BJ. Healthcare service delivery models for emerging economies: insights from India. Asian J Manag Cases [Internet]. 2022. 10.1177/097282012210993. Accessed 2024 January 13.
- 41.Choubey M, Ramakrishnan S, Sachdeva S, Mani K, Gangopadhyay D, Sivakumar K, et al. Impact of COVID-19 pandemic on pediatric cardiac services in India. Ann Pediatr Cardiol [Internet]. 2021;14:260–8. 10.4103/apc.apc_133_21. Accessed 2024 January 3. [DOI] [PMC free article] [PubMed]
- 42.Faraoni D, Nasr VG, DiNardo JA. Overall hospital cost estimates in children with congenital heart disease: analysis of the 2012 Kid’s Inpatient Database. Pediatr Cardiol [Internet]. 2016;37:37–43. 10.1007/s00246-015-1235-0. Accessed 2024 January 2. [DOI] [PubMed]
- 43.KPMG. India’s CSR reporting survey 2019. [Internet]. KPMG: India; 2020. Available from: https://assets.kpmg.com/content/dam/kpmg/in/pdf/2020/02/india-s-csr-reporting-survey-2019.pdf. Accessed 2024 January 24.
- 44.National CSR Portal, Ministry of Corporate Affairs, Govt of India. CSR in India. [Internet]. GOI: India; 2023. Available from: https://www.csr.gov.in/content/csr/global/master/home/home.html. Accessed 2024 February 14.
- 45.Dawra S, Chauhan KK. Corporate social responsibility (CSR) in India-evolution and challenges (from ancient period to present age). International Journal of Applied Business & Economic Research [Internet]. 2017;15:23–36. Available from: https://www.researchgate.net/publication/334624821_Corporate_Social_Responsibility_CSR_in_India_-Evolution_and_Challenges_From_Ancient_Period_to_Present_Age. Accessed 2024 January 12.
- 46.India CSR. India CSR Outlook Report - 2023. [Internet]. India CSR: India; 2023. Available from: https://indiacsr.in/wp-content/uploads/2023/10/India-CSR-Outlook-Report-2023.pdf. Accessed 2024 January 12.
- 47.Social Audit Network. Social impact assessment of Sri Sathya Sai Sanjeevani Hospital. Sri Sathya Sai Sanjeevani Centres for Child Heart Care: Internal Assessment Report; 2022. [Google Scholar]
- 48.Sahu P, Agrawal A, Jain D, Choudhary N. Association of early childhood caries and multiple variable factors in 3–6-year-old children. Int J Clin Pediatr Dent [Internet]. 2023;16:42–7. 10.5005/jp-journals-10005-2515. Accessed 2024 February 13. [DOI] [PMC free article] [PubMed]
- 49.Hasan BS, Bhatti A, Mohsin S, Barach P, Ahmed E, Ali S, et al. Recommendations for developing effective and safe paediatric and congenital heart disease services in low-income and middle-income countries: a public health framework. BMJ Glob Health [Internet]. 2023;8. 10.1136/bmjgh-2023-012049. Accessed 2024 January 12. [DOI] [PMC free article] [PubMed]
- 50.Kim S, Seshadrinathan S, Jenkins KJ, Murala JS. Can the public–private business model provide a sustainable quality pediatric cardiac surgery program in low- and middle-income countries?. World J Pediatr Congenit Heart Surg [Internet]. 2023;14:316–325. 10.1177/21501351221151057. Accessed 2024 January 12. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable as it is a review article. However, the authors confirm that the data supporting the findings of this study are available within the article or its supplementary material.