Abstract
Background
Reducing under-five mortality is a global health priority. Countries need specific data on which interventions have the most potential to lead to improvements to inform their programs and policies.
Methods
Group-based trajectory modeling was applied to identify distinct trajectories of under-five mortality from 2000 to 2019 in 78 low and lower-middle income countries. Both health and non-health variables were studied as time-stable covariates of trajectory group membership and as time-varying covariates of mortality rates within groups.
Results
We identified four distinct groups that were primarily distinguished based on trajectory level rather than shape–low mortality, medium mortality, medium–high mortality and high mortality. All four groups had under-five trajectories that declined over time with the highest mortality group having the largest declines. We conducted two sets of bivariate analyses. The first analysis was conducted to understand what factors distinguished the different groups from one another (time stable covariate analysis), and the second analysis was done to understand what factors were significant within a group (time vaying covariate analysis). Results indicated that five factors were associated with all three comparisons of being in the low, medium and medium high groups compared to the highest mortality group. These factors were fertility rate, % of population with an improved water source, female secondary school enrollment rate, diphtheria, pertussis, tetanus dose 3 (DPT3) coverage and % of gross domestic product (GDP) on health expenditures. Results of the modeling of the within group analysis with time-varying factors indicated that higher fertility rates and higher out-of-pocket expenditures were significantly associated with greater mortality rates for all four groups. High DPT3 coverage, greater political stability, high coverage of births in a health facility and a greater % GDP on health expenditures were significantly associated with reduced under-five mortality for all four groups.
Conclusion
Findings from our study revealed the importance of considering both health and non-health factors in understanding trajectories of under-five mortality. In particular the fertility rate and % of GDP on health expenditures were signicant for all three comparisons of the trajectory group membership analysis (time-stable covariates) and were significant for all four groups in the within group analysis (time varying covariates). Other factors were significant for some comparisons and groups. Focusing on a number of key factors relevant to their group could help countries to further improve the health of young children.
Keywords: Group-based trajectory modeling, Under-five mortality, Low and middle income countries
Background
The five million deaths, that occurred to children under the age of five in 2021 are a global tragedy. [1] Most of these deaths were from causes that could have been prevented with access to simple and known interventions, including immunizations and curative care (i.e., for diseases such diarrhea, pneumonia, malaria), maternal and newborn care provided during and after delivery, adequate nutrition, and access to clean water and sanitation. Forty-seven percent of these deaths occurred during the very first month of life, the neonatal period [1], highlighting the importance of care provided to both mother and newborn during labor, delivery and the postnatal period. Ending preventable deaths in children under-five is a target under the health-focused Goal 3 of the Sustainable Development Goals (SDG) [2]. The target is for countries to have an under five-mortality rate of less than 25 deaths per 1,000 live births by 2030 [2]. Current trends indicate that 54 countries may not meet this target unless changes are made, and the Covid-19 may have impeded declines during the pandemic [1]. Even though many low-cost interventions necessary to reduce under-five deaths exist, resources to implement these interventions are often limited. Understanding what policies and programs are most effective at reducing under-five mortality in different settings could help funders and countries allocate resources effectively.
Several studies have used statistical modeling to understand the contributions of health and non-health sector factors on under-five mortality and child health [3–6]. The Success Factor Study presented a statistical and econometric analysis of health and non-health sector factors associated with declines in under-five mortality in 144 low- and middle-income countries (LMIC). The study found that health and non-health sector factors fairly evenly accounted for the declines, and that 22 factors were necessary for “fast-track progress.” [3] A decomposition analysis of 146 low- and middle-income countries likewise indicated that both health sector and non-health sector factors played roles in under-five mortality declines from 1990 to 2010. [4] A synthetic control analysis was used to study the role of the United States Agency for International Development (USAID) donor funding on under-five mortality declines and found that countries with above average USAID funding had significantly lower under-five mortality than those with less than average funding. [5] This analysis highlighted the importance of resources in the form of donor funding. Andrus et al. employed a multi-level longitudinal model to study predictors of oral rehydration solution use among children with diarrhea in 103 low and middle income countries. [6] Four variables predicted a greater likelihood of oral rehydration solution use: four or more antenatal care visits; care-seeking for suspected pneumonia; government effectiveness; and out of pocket (OOP) expenditures. All of these studies carefully considered both health and non-health variables as factors important to under-five health and mortality, based upon on theory and conceptual models, as well as, data availability.
The current study
While the aforementioned studies are informative, relatively little longitudinal research has been conducted to examine trajectories of change in under-five mortality rates in LMIC and/or identify variables that explain differences in these trajectories. Such research can inform understanding of heterogeneity across countries in change in mortality over time and identify modifiable factors that may be targeted by prevention efforts. To this end, in our paper we employed group-based trajectory modeling (GBTM), a type of latent class growth analysis, to identify groups of LMIC that follow distinct under-five mortality trajectories across 2000–2019. [7, 8] We used 2019 as the end-point to focus on the pre-Covid period and avoid complexities in interpretation that could arise by including the time of the peak of the Covid pandemic. GBTM was used to approximate the true distribution of trajectories by identifying subgroups of countries who follow similar patterns of change across time in under-five mortality rates. While GBTM has been used in the fields of medicine and psychology to assess individual differences in trajectories of change [9], its application to assess change over time in outcomes within and between countries is new.
In addition to identifying trajectory groups, we examined the role of health and non-health related variables as both between- and within-group predictors of under-five mortality. This study was guided by the Mosely Chen Proximate Determinant Framewiork which indicates that both proximate (biological or health-related) and distal (socio-economic) factors are important determinants of under-five mortality [10]. Using this framework as a guide, an extensive literature reciew was conducted to select health-related and socio-economic factors for our study of under-five mortality. Identifying a distinct trajectory for a specific group of countries can help lead to refinements in policies and program. For example, a group of countries seeing the least improvement may look to factors associated with the trajectory of a group of countries showing the greatest improvements. This knowledge would also allow for sharing of ideas among the country groups to foster cross-country learning. Therefore, the objectives of this study were: (1) to identify distinct under-five mortality trajectory groups in a sample of low- and lower-middle income countries, assessed from 2000 to 2019; (2) to examine factors that are associated with membership in lower mortality groups as compared with the highest mortality group; and (3) to understand factors that are associated with lower under-five mortality within groups.
Methods
Measures and data sources
Outcome
Our outcome variable was under-five mortality, defined as the probability of dying by age five per 1000 live births. Historical data on under-five mortality were downloaded from the United Nations Inter-agency Group for Child Mortality Estimation (UN IGME), for all available countries (n = 78) from 2000 to 2019. [11].
Covariates
Through our literature review, guided by the Mosley-Chen Proiximate Determinant Framework [10], we selected covariates for our study. Health related factors were categorized into water, sanitation and hygiene serices; nutrition; health delivery/health services; health system and health financing. The nonhealth factors were categorized into wealth; demographics; education and governance. Through this process a list of 19 covariates were identified that were conceptually distinct and unique and which had available data. (These factors are presented in Table 1). Information on current and historical income classification (i.e. low income, lower middle income etc.) for each country was downloaded from the World Bank [12]. Data on the health and socio-economic factors came from USAID’s Idea Database. [13]
Table 1.
Selected covariates by sector and category
| Sector | Category | Covariates |
|---|---|---|
| Non-Health | Wealth | Fertility rate |
| Demographics |
Women with access to newspaper, television and radio at least once a week (% of total) HIV prevalence (ages 15 to 49) |
|
| Education |
Mean years of education for females age 20–24 Net secondary school enrollment rate for females |
|
| Governance | Political Stability | |
| Health | Water, sanitation and hygiene services |
Population living in households using an improved water source (% of total) Population living in households with an improved sanitation facility (% of total) |
| Nutrition |
Child malnutrition: Stunting (%) Child malnutrition: Wasting (%) |
|
| Health delivery/health services |
At least four antenatal care visits (% of total) Births delivered in a health facility (%) % of infants surviving to the age of 1 that received DTP1 vaccine % of infants surviving to the age of 1 that received DTP3 vaccine Care seeking for children under age 5 with fever (%) Postnatal health check for newborns within 2 days (%) |
|
| Health system | Nurse and midwife density (per 1,000 population | |
| Health financing |
OOP expendtiures (% of current health expenditures) Domestic general government health expenditure (% of GDP) |
DTP = Diphtheria, Tetanus, Pertussis; OOP: out of pocket; GDP = gross domestic product
Analysis
Group based trajectory modeling
We used a latent class growth analysis, a type of GBTM that fixes variance and covariances of growth factors to zero, to identify subgroups of countries with distinct under-five mortality trajectories with year (2000–2019) as the unit of time. More complex models, which allow for subgroup heterogeneity in trajectory parameters were not estimable, likely due to small sample size.
Model selection
Key components of GBTM are the trajectory parameters for each group (i.e., intercepts, slopes) and the probability of membership of that trajectory group [8]. We used the Traj program for STATA [14] to fit a sequence of models to the under-five mortality data varying the polynomial type and the number of trajectory groups from one to eight. We also compared models that did and did not allow residual variances to vary across groups. We started by specifying a cubic functional form because of the shape of the spaghetti plot (Fig. 1). Across all of the models the cubic trajectory parameter was not statistically significant for any group. We thus respecified the functional form as quadratic and again estimated models with up to 8 groups. Across all of these models, the quadratic parameter was statistically significant for at least one class. For our model selection we compared fit statistics including Akaike Information Criterion (AIC), the Bayesian Information Criterion (BIC), parsimony, interpretability, and within class sample size. Table 2 presents model fit statistics for the quadratic models with residual variances constrained and unconstrained. Models with unconstrained residual variances had better fit, as indicated by a lower AIC and BIC, than those with constrained variances. Of the unconstrained models, the lowest AIC and BIC were found for the six class model; however this model, as well as the five class model, included classes with very small sample sizes (n < 10). Further, the additional trajectories that were extracted in the five and six class models were not substantively different from those in models with fewer classes. As such, balancing the criteria of fit, parsimony, and interpretability we selected a four class model with unconstrained residuals. All of the quadratic growth factors in the four class model were statistically significant and thus we did not trim any polynomial terms from the selected model.
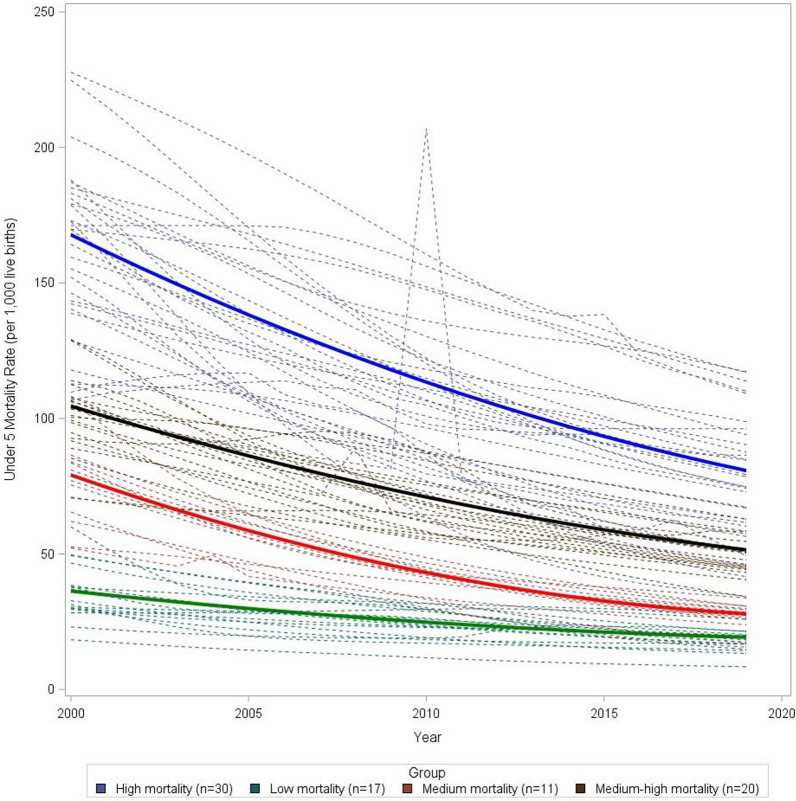
Fig. 1.
Trajectories of under-five mortality rates from 2000 to 2019 of individual countries by group membership, with group trajectories overlaid
Table 2.
Fit Statistics
| Residuals constrained | Residuals unconstrained | |||||
|---|---|---|---|---|---|---|
| No. of classes | AIC | BIC (n = 78) | Sample size per class | AIC | BIC (n = 78) | Sample size per class |
| Quadratic functional form | ||||||
| 1 | − 7981.36 | − 7986.08 | 78 | − 7981.36 | − 7986.08 | 78 |
| 2 | − 7197.60 | − 7207.03 | 40/38 | − 7102.54 | − 7113.15 | 26/52 |
| 3 | − 6599.43 | − 6613.57 | 28/32/18 | − 6513.87 | − 6530.37 | 21/26/31 |
| 4 | − 6360.65 | − 6379.50 | 21/16/23/18 | − 6286.66 | − 6309.05 | 17/11/20/30 |
| 5 | − 6135.94 | − 6159.51 | 21/14/22/11/9 | − 6016.72 | − 6045.00 | 12/9/14/20/23 |
| 6a | – | – | – | − 5821.04 | − 5855.21 | 12/8/7/12/20/18 |
| 7 | − 6186.52 | − 6219.52 | 1/11/8/14/16/14/13 | – | – | – |
| 8a | – | – | – | – | – | – |
aSignifies that the model did not converge
Inclusion of covariates
Covariates were included into the base GBTM model both as time-stable predictors of trajectory group membership and as time-varying predictors of under five mortality within trajectory groups (described further below). Given the number of covariates under consideration, the complexity of the underlying GBTM approach, and the small sample size for our study, we assessed bivariate associations between the selected covariates (rather than estimate multivariate models).
Time stable covariates
Time-stable covariates were created by averaging scores on predictors across the assessment period (2000–2019). We then looked at the associations between each covariate and trajectory group membership using the method described by Nagin et al. (2010) [8]. In particular, following class enumeration, we fitted several GBTM models, one for each covariate, with the number of trajectories fixed at four and the highest mortality group specified as the reference group [8]. A positive (or negative) coefficient estimate for a particular trajectory group indicates that the associated covariate increases (or decreases) the probability of membership in that group relative to the high mortality group.
Time-varying covariates
Covariates were also operationalized as varying over time within-countries. These time-varying covariates were included within the base GBTM model as additional predictors of the under-5 mortality outcome, with the assumption of conditional independence of the repeated measures within groups. A positive (or negative) coefficient estimate for a particular covariate within a specific trajectory group implies that a change in the covariate is associated with a change in U5 mortality rate in that group (i.e., the time-varying covariate is affecting the trajectory specific course; further, group specific estimates capture any differences between groups in these associations.
Results
Description of the selected model
Table 3 presents the trajectory parameter estimates, and Fig. 1 shows mean trajectories for each group overlaid on top of individual country trajectories. We can see four distinct patterns or grouping of countries with all groups experiencing a downward trajectory in under five mortality over time. Of note is that Group 4, which has the highest mortality, also has the steepest slope or largest decline in mortality. The country in Group 4 with the sharp peak in 2010 is Haiti, which suffered a devastating earthquarke. Table 4 contains a listing of each country in each group.
Table 3.
Trajectory parameter estimates for group
| Group | Parameter | Estimate | SE | T − value | p value |
|---|---|---|---|---|---|
| 1 | Intercept | 36.30 | 1.14 | 31.71 | 0.00 |
| Linear | − 1.42 | 0.25 | − 5.67 | 0.00 | |
| Quadratic | 0.03 | 0.01 | 2.38 | 0.02 | |
| 2 | Intercept | 79.12 | 1.79 | 44.16 | 0.00 |
| Linear | − 4.61 | 0.39 | − 11.71 | 0.00 | |
| Quadratic | 0.10 | 0.02 | 5.53 | 0.00 | |
| 3 | Intercept | 104.55 | 1.68 | 62.30 | 0.00 |
| Linear | − 3.98 | 0.37 | − 10.85 | 0.00 | |
| Quadratic | 0.06 | 0.02 | 3.70 | 0.00 | |
| 4 | Intercept | 167.74 | 3.51 | 47.74 | 0.00 |
| Linear | − 6.39 | 0.77 | − 8.29 | 0.00 | |
| Quadratic | 0.10 | 0.04 | 2.67 | 0.01 |
SE = standard error
Table 4.
Group membership for low- and lower-middle-income countries
| Groups | Countries |
|---|---|
| 1 (Low mortality) | Cabo Verde, Democratic People’s Republic of Korea, Egypt, El Salvador, Honduras, Kyrgyzstan, Morocco, Nicaragua, Philippines, Republic of Moldova, Solomon Islands, State of Palestine, Syrian Arab Republic, Tunisia, Ukraine, Uzbekistan, Vanuatu, Vietnam |
| 2 (Medium mortality) | Bangladesh, Bhutan, Bolivia (Plurinational State of), Cambodia, Indonesia, Micronesia, Mongolia, Nepal, Sao Tome and Principe, Tajikistan, Uzbekistan |
| 3 (Medium–high mortality) | Comoros, Congo, Djibouti, Eritrea, Gambia, Ghana, India, Kenya, Kiribati, Lao People’s Democratic Republic, Madagascar, Myanmar, Pakistan, Papua New Guinea, Senegal, Sudan, Timor-Leste, United Republic of Tanzania, Yemen, Zimbabwe |
| 4 (High mortality) | Afghanistan, Angola, Benin, Burkina Faso, Burundi, Cameroon, Central African Republic, Chad, Cote d’Ivoire, Democratic Republic of the Congo, Eswatini, Ethiopia, Guinea, Guinea-Bissau, Haiti, Lesotho, Liberia, Malawi, Mali, Mauritania, Mozambique, Niger, Nigeria, Rwanda, Sierra Leone, Somalia, South Sudan, Togo |
Characteristics of the four groups are displayed in Table 5. Group 1, the lowest mortality group, had an average under-five mortality of 35.9 in 2000 and 18.4 in 2019 and included 17 countries (6% from Sub-Saharan Africa and 12% low income). Group 2, the medium mortality group, had an average under-five mortality that dropped from 75.1 to 26.6 from 2000 to 2019 and consisted of 11 countries (9% from Sub-Saharan Africa and 18% low income). Group 3, the medium–high mortality group, had an average under-five mortality of 100.6 in 2000 and 49.9 in 2019 and included 20 countries (55% from Sub-Saharan Africa and 25% low income). Group 4, the high mortality group, had an average under-five mortality of of 160.6 in 2000 and 78.5 in 2019 and consisted of 30 countries (93% from Sub-Saharan Africa and 73% low income).
Table 5.
Key characteristics of groups of under-five mortality rate trajectories from 2000 to 2019
| Characteristic | 1 (Low mortality) | 2 (Medium mortality) | 3 (Medium–high mortality) | 4 (High mortality) |
|---|---|---|---|---|
| N = 17 | N = 11 | N = 20 | N = 30 | |
| Average under-five mortality 2000 (per 1,000 live births) | 35.9 | 75.1 | 100.6 | 160.6 |
| Average under-five mortality 2019 (per 1,000 live births) | 18.4 | 26.6 | 49.9 | 78.5 |
| Average annual rate of decline | 0.9 | 2.4 | 2.5 | 4.1 |
| Regions, n(col%) | ||||
| East Asia and Pacific | 5 (29) | 4 (36) | 5 (25) | 0 (0) |
| Europe and central Asia | 3 (18) | 2 (18) | 0 (0) | 0 (0) |
| Latin America and Caribbean | 3 (18) | 1 (9) | 0 (0) | 1 (3) |
| Middle East and North Africa | 5 (29) | 0 (0) | 2 (10) | 0 (0) |
| South Asia | 0 (0) | 3 (27) | 2 (10) | 1 (3) |
| Sub-Saharan Africa | 1 (6) | 1 (9) | 11 (55) | 28 (93) |
| Income groups, (col%) | ||||
| Low income | 2 (12) | 2 (18) | 5 (25) | 22 (73) |
| Lower-middle income | 15 (88) | 9 (82) | 15 (75) | 8 (27) |
col% = column percent. Annual Rate
Covariates associated with group membership (time stable)
Bivariate associations between covariates and group membership are displayed in Table 6 with the high mortality group (Group 4) as the reference. The odds ratio (OR) for each covariate thus denotes the change in the odds of membership in each lower mortality group compared to the highest mortality group for a one unit increase in the covariate. A higher OR suggests that a higher score on the covariate is protective against membership in the highest mortality group. All selected covariates significantly distinguished membership in the low mortality group (Group 1) compared to the high mortality group (Group 4) in the expected direction with the exception of two covariates. Care-seeking for children under-five and out-of-pocket (OOP) expenditures were not significant. Eleven covariates emerged as explanatory factors that distinguished the medium mortality group (Group 2) from Group 4,the highest mortality There were seven factors that were significant for the comparison of Group 3, medium–high mortality, from Group 4 (high mortality). Five covariates were significant for all three comparisons and included the fertility rate, percent of population living with an improved water source, net secondary school enrollment of females, coverage for the third doses of Diphtheria, Tetanus, Pertussis (DTP3), and % of Gross Domestic Product (GDP) on health expenditures. Higher fertility was associated with being in Group 4, highest mortality, compared to each of the three other groups. A higher value for the other four factors was associated with the odds of membership in Groups 1, 2 and 3 compared to the highest mortality group (Group 4). For example greater DTP3 coverage was associated with a 16% increased odds of being in Group 1 compared to Group 4.
Table 6.
Bivariate associations of risk factors and group membership
| Risk factor | Group reference = group 4 (high mortality) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 (low mortality) | 2 (medium mortality) | 3 (medium–high mortality) | ||||||||||
| OR | LCL | UCL | p | OR | LCL | UCL | p | OR | LCL | UCL | p | |
| Fertility/demographics | ||||||||||||
| Fertility rate (births per woman) | 0.03 | 0.01 | 0.13 | *** | 0.05 | 0.01 | 0.20 | *** | 0.22 | 0.09 | 2.55 | ** |
| Governance | ||||||||||||
| Political stability and absence of violence/terrorism | 2.96 | 1.24 | 7.02 | * | 3.01 | 1.14 | 7.95 | * | 1.56 | 0.75 | 2.07 | |
| Demographics | ||||||||||||
| Women with access to newspaper, television and radio at least once per week (%) | 1.31 | 1.12 | 1.53 | *** | 1.08 | 1.05 | 1.43 | *** | 1.08 | 0.95 | 1.16 | |
| HIV prevalence (ages 15 to 49) | 0.11 | 0.02 | 0.52 | ** | 2.25 | 0.07 | 0.75 | * | 1.81 | 0.91 | 1.10 | |
| Water, sanitation and hygiene | ||||||||||||
| Population living in households with an improved water source (%) | 1.09 | 1.02 | 1.17 | ** | 1.04 | 1.02 | 1.20 | * | 1.04 | 1.00 | 1.06 | * |
| Population living in households with an improved sanitation facility (%) | 1.12 | 1.05 | 1.18 | *** | 1.04 | 0.99 | 1.10 | 1.05 | 1.00 | 1.05 | * | |
| Nutrition | ||||||||||||
| Stunting (%) | 0.82 | 0.73 | 0.91 | *** | 0.92 | 0.84 | 1.01 | 1.00 | 0.93 | 1.07 | ||
| Wasting (%) | 0.73 | 0.59 | 0.91 | ** | 1.07 | 0.91 | 1.25 | 1.08 | 0.94 | 1.15 | ||
| Education | ||||||||||||
| Mean years of education for females age 20–24 | 2.57 | 1.53 | 4.32 | *** | 1.57 | 0.99 | 2.48 | 1.41 | 1.03 | 1.37 | * | |
| Net female secondary school enrollment rate (%) | 1.22 | 1.12 | 1.33 | *** | 1.17 | 1.08 | 1.27 | *** | 1.17 | 1.08 | 1.09 | ** |
| Health delivery/health services | ||||||||||||
| At least four visits of antenatal care (%) | 1.11 | 1.06 | 1.17 | *** | 1.02 | 0.98 | 1.07 | 1.02 | 0.99 | 1.03 | ||
| Births delivered in a health facility (%) | 1.10 | 1.05 | 1.15 | *** | 1.04 | 1.00 | 1.08 | * | 1.00 | 0.98 | 1.03 | |
| Care seeking for children under age 5 with fever (%) | 1.06 | 0.99 | 1.15 | 1.02 | 0.95 | 1.09 | 1.00 | 0.96 | 1.05 | |||
| Post-natal health check for newborn within 2 days (%) | 1.07 | 1.03 | 1.11 | *** | 1.03 | 0.99 | 1.06 | 1.02 | 0.99 | 1.03 | ||
| Surviving infants who received first dose of DTP (%) | 1.25 | 1.06 | 1.49 | * | 1.15 | 1.01 | 1.32 | * | 1.04 | 0.98 | 1.07 | |
| Surviving infants who received third dose of DTP (%) | 1.16 | 1.07 | 1.26 | *** | 1.18 | 1.07 | 1.31 | ** | 1.05 | 1.00 | 1.05 | * |
| Health system | ||||||||||||
| Nurse and midwife density (per 1,000 population) | 46.76 | 4.90 | 446.30 | *** | 33.65 | 3.24 | 349.62 | ** | 3.12 | 0.26 | 12.12 | |
| Health financing | ||||||||||||
| Out-of-pocket expenditures (% of current health expenditure) | 0.99 | 0.96 | 1.02 | 0.99 | 0.96 | 1.03 | 1.00 | 0.97 | 1.03 | |||
| % of GDP on health expenditures | 2.94 | 1.44 | 6.00 | ** | 1.88 | 0.88 | 4.00 | * | 1.46 | 0.73 | 1.99 | * |
OR = odds ratio; SE = standard error; LCL = lower confidence limit of 95% confidence interval; UCL = upper confidence limit of 95% confidence interval; DTP = Diphtheria, Tetanus, Pertussis. The basis for comparison is trajectory group 4 (the highest mortality group). For political stability and absence of violence and terrorism: range = − 2.5–2.5 (higher indicates more stable and less violence and terrorism)
* p < 0.05; **p < 0.01; ***p < 0.001
Analysis of time varying covariates and under-five mortality rates within groups
Table 7 presents the bivariate analysis of the associations between time-varying predictors and under-five mortality within each trajectory group. The results of the bivariate analysis indicate that, across all groups, greater fertility rates were significantly associated with increased under-five mortality; in other words, results suggest that at time points when fertility rates increase, under five mortality also increases. Greater OOP expenditures were also significantly assocated with increased mortality for all four groups. Acoss all four groups, increases in childbirth in a health facility, political stability and % GDP on health expendtitures were significantly associated with decreases in under-five mortality. Other time-varying associations differed depending on trajectory group. In particular, higher DTP3 vaccination coverage and greater political stability were significantly associated with lower under-five mortality for all groups, except the low mortality group (Group 1). Increases in the prevalence of stunting was associated with increases in under-five mortality for three of the groups (Groups 1, 2 and 3), while increases in the prevalence of wasting was associated with higher under-five mortality for two of the groups (Group 2 and 4). Increases in coverage of four or more ANC visits was significantly associated with decreases in under-five mortality for the two lower mortality groupss (Groups 1 and 2). A high nurse-midwife per population ratio was significantly associated with lower under-five mortality for countries in the the lower three mortality groups (Groups 1, 2 and 3).
Table 7.
Group-based trajectory bivariate models: coefficients (standard error) (n = 78^): modeling within Groups
| 4 Group Model | ||||
|---|---|---|---|---|
| 1 (Low Mortality) | 2 (Medium Mortality) | 3 (Medium − High Mortality) | 4 (High Mortality) | |
| Bivariate models: variables (sample size) | Coefficients (Standard Error) | |||
| Fertility rate (n = 77) | 3.50 (0.31)*** | 10.95 (0.38)*** | 9.35 (0.44)*** | 14.88 (0.93)*** |
| DTP 3 vaccine (n = 77) | − 0.01 (0.03) | − 0.41 (0.03)*** | − 0.40 (0.04)*** | − 0.83 (0.05)*** |
| Political stability (n = 77) | − 2.33 (0.47)*** | − 6.93 (0.45)*** | − 5.72 (0.44)*** | − 11.22 (1.20)*** |
| Stunting (n = 74) | 0.49 (0.10)*** | 0.76 (0.05)*** | 0.38 (0.13)** | 0.43 (0.33) |
| Wasting (n = 74) | 0.32 (0.26) | 0.68 (0.12)*** | − 0.27 (0.32) | 2.60 (0.50)*** |
| ANC 4 visit (n = 75) | − 0.15 (0.07)* | − 0.27 (0.05)*** | − 0.03 (0.06) | − 0.01 (0.13) |
| Births in health facilities (n = 77) | − 0.36 (0.04)*** | − 0.24 (0.01)*** | − 0.38 (0.06)*** | − 0.90 (0.11)*** |
| Nurse and midwives density (n = 76) | − 0.52 (0.26)* | − 1.36 (0.12)*** | − 1.92 (0.78)* | − 4.57 (3.72) |
| OOP expenditures (n = 75) | 0.06 (0.03)* | 0.24 (0.02)*** | 0.34 (0.02)*** | 0.70 (0.05)*** |
| % GDP on health expenditures (n = 75) | − 3.14 (0.28)*** | − 4.01 (0.53)*** | − 2.08 (0.26)*** | − 5.42 (1.15)*** |
*p < 0.05,**p <.01,***p < 0.001
^Some observations (countries) dropped in bivariate models due to missing covariate data
Summary
Table 8 presents a succinct summary of the results. For each group of countries, significant findings are indicated for both the analysis of group membership (time stable) and within groups (time varying).
Table 8.
Summary of findings from analyses of trajectory group membership and the within group analyses
| Significant factors: bivariate analysis | |||
|---|---|---|---|
| Group | Countries in group | Trajectory group membership (reference: group 4 high mortality) | Within group analysis |
| 1 (Low mortality | Cabo Verde, Democratic People’s Republic of Korea, Egypt, El Salvador, Honduras, Kyrgyzstan, Morocco, Nicaragua, Philippines, Republic of Moldova, Solomon Islands, State of Palestine, Syrian Arab Republic, Tunisia, Ukraine, Uzbekistan, Vanuatu, Vietnam | Fertility rate, Political stability, Women with access to media at least once per week, HIV prevalence, Population living in household with improved water source, Population living in household with improved sanitation source, Stunting, Wasting, Mean years of education for females age 20 − 24, Net female secondary school enrollment, At least four ANC visits, Births delivered in a health facility, Postnatal check for newborns within 2 days, Infants receiving DPT1, Infants receiving DPT3, Nurse and midwife density, % of GDP on health expenditures | Fertility rate, Political stability, Stunting, At least four ANC visits Births in a health facility, Nurse and midwife density, OOP expenditures, % of GDP on healthcare |
| 2 (Medium mortality) | Bangladesh, Bhutan, Bolivia (Plurinational State of), Cambodia, Indonesia, Micronesia, Mongolia, Nepal, Sao Tome and Principe, Tajikistan, Uzbekistan | Fertility rate, Political stability, Women with access to media at least once per week, HIV prevalence, Population living in household with improved water source, Net female secondary school enrollment, Births delivered in a health facility, Infants receiving DPT1, Infants receiving DPT3, Nurse and midwife density, % of GDP on health expenditures | Fertility rate, Infants receiving DPT3, Political stability, Stunting, Wasting, Four or more ANC visits, Births in a health facility Nurse and midwife density, OOP expenditures, % of GDP on health expenditures |
| 3 (Medium high mortality) | Comoros, Congo, Djibouti, Eritrea, Gambia, Ghana, India, Kenya, Kiribati, Lao People’s Democratic Republic, Madagascar, Myanmar, Pakistan, Papua New Guinea, Senegal, Sudan, Timor − Leste, United Republic of Tanzania, Yemen, Zimbabwe | Fertility rate, Population living in household with improved water source, Population living in household with improved sanitation source, Mean years of education for females age 20 − 24, Net female secondary school enrollment, Infants receiving DPT3, % of GDP on health expenditures | Fertility rate, Infants receiving DPT3, Political stability, Stunting, Births in a health facility, Nurse and midwife density, OOP expenditures, % of GDP on health expenditures |
| 4. (High mortality) | Afghanistan, Angola, Benin, Burkina Faso, Burundi, Cameroon, Central African Republic, Chad, Cote d’Ivoire, Democratic Republic of the Congo, Eswatini, Ethiopia, Guinea, Guinea − Bissau, Haiti, Lesotho, Liberia, Malawi, Mali, Mauritania, Mozambique, Niger, Nigeria, Rwanda, Sierra Leone, Somalia, South Sudan, Togo | N/A | Fertility rate, Infants receiving DTP3, Political Stability, Wasting, Births in a health facility, OOP Expenditures, % of GDP on health expenditures |
Discussion
Group-based trajectory model is a useful methodology for identifying groups of observations which share similar trajectories. In this paper, we applied this methodology to identify countries with similar under-five mortality trajectories and then employed bivariate analyses to understand which covariates were associated with group membership (time stable) and which covariates were significant within groups (time varying). The analysis is intended to inform countries and donors about what programmatic interventions could lead to the greatest reductions in under-five mortality.
Based on our results we have distinct groups of countries ranging from Group 1 with the lowest under five mortality to Group 4 with the highest under-five mortality. On average, countries in Group 1 had an average under-five mortality of 18.4 per 1000 in 2019, indicating that they are already meeting the SDG-3 under-five mortality target of less than 25 under five deaths per 1000 live births. Countries in Group 2 are on average slightly above the target in 2019, however many are expected to reach the target by 2030. Countries in Group 3 and 4 are still above the SDG-3 under-five mortality target and may be of particular focus for global donors. It is important for all countries to continue efforts to decrease under-five mortality as much as possible, and countries in Groups 3 to 4 could learn from what has worked in Groups 1 and 2. Though Group 4 countries have the highest mortality, they also have the fastest rate of under-five mortality decline suggesting that improvements are happening.
Similar to other studies, we find that both health and non-health factors play a role in under-five mortality trajectories. [3, 4] In particular, five time stable factors (both health and non-health) distinguished countries in the high mortality group from all other groups. These factors were fertility rate, percent of population living with an improved water source, net female secondary school enrollment rate, DTP3 coverage and % of GDP on health expenditures, Thus, a combination of demographics (fertility) social factors (education), environmental factors (clean water), health/financing (health expenditures) and service delivery factors (immunization) are important in distinguishing countries within the trajectory that had the highest under-five mortality rates in the study period. As countries and donors work to improve the health of children under-five, they must look comprehensively at the potential of these factors to improve the health and well-being of children under-five. Note that the factors associated with being a high vs low trajectory group are likely to also have been influential in the years prior to the study and may operate on a longer time horizon than just the study period.
Policy makers should understand that the benefits of shifting resources to better address factors associated with the group trajectory that represents their country may require a decade or more of investment. However, covariates associated with more rapid under-five mortality declines within a group may point to factors that are influential in the shorter term. These factors might operate within the study period itself and operate among countries that are similar on other important factors that comprise group membership. Policy makers should also consider shifting resources to address the factors associated with more rapid under-five mortality declines within their country’s trajectory group, as discussed below.
Our work on understanding what factors (time varying) are significantly associated with under-five mortality declines within trajectory groups indicated that five covariates were significant for all frour groups. Higher fertility was significantly associated with higher mortality within all four groups in the multivariable analysis; thus a focus on family planning is important for all countries. A study of high fertility countries estimated that increased contraceptive use could lead to 10 percent decline in under-five mortality [15]. Delivery in a health facility was associated with reduced under five mortality for all countries. Maternal and newborn care are intertwined, and care provided to the mother at delivery and care provided to both mother and newborn after delivery are crucial for newborn survival. Given that neonatal mortality accounts for nearly half of under-five mortality globally [2], national attention to care received around the time of birth appears to have important impact on under-five mortality. Greater political stability was associated with lower mortality for all groups, suggesting the importance of conflict resolution and the devastation of war and conflict on the health of children. A greater percentage of GDP spent on health care was significant for all groups, suggesting the importance of political will and a country’s focus on healthcare. Greater OOP expenditures were significantly associated with higher under-five mortality in all groups and may signal that high OOP expenditures could make healthcare inaccessible for many households. Initiatives such as universal health care could enable more families living in poverty to access health services [16]. Higher DPT3 coverage was significantly associated with reduced under-five mortality for all groups except the low mortality group. Immunization programs are a pillar of child survival programs and one of the most cost-effective interventions [17, 18]. Other factors were significant for some, but not all groups, indicating the importance of countries looking at significant factors in their own group.
There are some key limitations to our work. Because of missing data, we could not assess time-varying associations for all of our factors. Countries also did not have an equal number of years of the time-varying data. For example, South Sudan did not become an independent country until 2011 and had much less data than most of the other countries. The small sample size was another notable limitation. In addition, we identify associations with under-five mortality but are unable to look at causality. Relatedly our choice to assess bivariate associations, which was made based on pragmatic considerations of small sample sizes, the large number of relevant covariates and the complexity of the GBTM approach. Bivariate analyses are limited in not accounting for confounding factors. In addition we identifitied our groups without any covariates in the initial modeling. However the addition of covariates can actually change group shape and size.
Conclusion
Group-Based Trajectory Modeling (GBTM) holds promise as a data-driven approach to organize and classify units of analysis into similar groupings based on the trajectory of an outcome of interest, in this case under-five mortality. GBTM would also be a suitable technique to study other outcomes of interest for which long-term data are available. Once the grouping is determined, factors associated with better vs poorer outcomes can be identified across and within groups and policy makers can use this information to inform programs that address the outcome of interest. While GBTM has been used in the past to assess individual differences in trajectories of change, its application to assess change over time in population-based outcomes within and between countries is new. Program relevant factors to reduce under-five mortality in low- and lower-middle income countries groups with different levels of mortality were identified through this approach. GBTM has the potential to inform policy making/programming decision making by identifying subgroups of countries that need additional investment and by identifying factors that may be targeted by new prevention efforts.
Acknowledgements
We would like to thank Ollie Kuo for her assistance with data management.
Abbreviations
- AIC
Akaike information criterion
- ANC
Antenatal care
- BIC
Bayesian information criterion
- DPT
Diphtheria, pertussis and tetanus
- GDP
Gross domestic product
- GBTM
Group based trajectory modeling
- LMIC
Low and middle income countries
- OOP
Out of pocket expenditures
- OR
Odds ratio
- SDG
Sustainable development goal
- UN IGME
United nationals inter-agency group for child mortality estimation
- USAID
United States agency for international development
Author contributions
KS and ES led the writing of the paper. GA, HLMR and WW provided statistical expertise, guidance and oversight, while ES and AS led the day-to-day analysis. All authors read and approved the final manuscript.
Funding
We are grateful to the Carolina Population Center and its NIH Center for Scientific Review Grant (R24 HD050924) for general support. This publication was produced with funding from the United States Agency for International Development (USAID) through the Data for Impact (D4I) Associate Award number7200 AA18LA00008. The contents of this manuscript represent the views and opinions of the authors and do not necessarily reflect the views and opinions of the U.S. Agency for International Development (USAID) or the United States Government.
Data Availability
The datasets analyzed for the current study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable. (This paper only used aggregated country-level data and did not involve human subjects.)
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.UNICEF. Levels and Trends in Child Mortality. Estimates Developed by the UN Inter-agency Group for Child Mortality Estimation. New Year. 2021.
- 2.United Nations. Sustainable Development Goals https://sustainabledevelopment.un.org/topics/sustainabledevelopmentgoals. Accessed April 5, 2022.
- 3.Kuruvilla S, Schweitzer J, Bishai D, et al. Success factors for reducing maternal and child mortality. Bull World Health Organ. 2014;92(7):533–44. 10.2471/blt.14.138131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bishai DM, Cohen R, Alfonso YN, Adam T, Kuruvilla S, Schweitzer J. Factors contributing to maternal and child mortality reductions in 146 low- and middle-income countries between 1990 and 2010. PLoS ONE. 2016;11(1):1–13. 10.1371/journal.pone.0144908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weiss W, Piya B, Andrus A, et al. Estimating the impact of donor programs on child mortality in low- and middle-income countries: a synthetic control analysis of child health programs funded by the United States Agency for International Development. Popul Health Metrics. 2022;20:2. 10.1186/s12963-021-00278-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Andrus A, Cohen R, Carvajal-Aguirre L, El Arifeen S, Weiss W. Strong community-based health systems and national governance predict improvement in coverage of oral rehydration solution (ORS): A multilevel longitudinal model. J Glob Health. 2020. 10.7189/jogh.10.010503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bauer DJ, McNaughton Reyes HL. Modeling variability in individual development: differences of degree or kind? Child Dev Perspect. 2010;4(2):114–22. 10.1111/j.1750-8606.2010.00129.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nagan DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol. 2010;6:109–38. [DOI] [PubMed] [Google Scholar]
- 9.Nagin DS, Jones BL, Ria V, Passos L, Tremblay RE. Group-based multi-trajectory modeling. Stat Methods Med Res. 2016. 10.1177/0962280216673085. [DOI] [PubMed] [Google Scholar]
- 10.Mosley,W,H and Chen, L C. An Analytical Framework for the Study of Child Survival in Developing Countries. Popul Dev Rev. 1984;10(Suppl):25–45. [PMC free article] [PubMed]
- 11.UNIGME. UN Inter-agency Group for Child Mortality Estimation: Download data and estimates. https://childmortality.org/data. Published 2019. Accessed May 7, 2020.12. The World Bank. World Bank Country and Lending Groups. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups. Published 2020. Accessed May 7, 2020.
- 12.The World Bank. World Bank Country and Lending Groups. 2020. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups. Accessed 7 May 2020.
- 13.USAID.IDEA Database. https://idea.usaid.gov/Accessed February 17, 2024.
- 14.Jones BL. traj: group-based modeling of longitudinal data. https://www.andrew.cmu.edu/user/bjones/. Published 2020. Accessed February 17, 2024.
- 15.Cleland J, Bernstein S, Ezeh A, Faundes A, Glasier A, Innis J. Family planning: the unfinished agenda. Lancet. 2006;368:1810–27. [DOI] [PubMed] [Google Scholar]
- 16.WHO. Universal Health Coverage. https://www.who.int/health-topics/universal-health-coverage#tab=tab_1. Last Accessed April 26, 2022.
- 17.UNICEF.Immunuzation. https://www.unicef.org/immunization. Last Accessed April 26, 2022.
- 18.Ozawa S, Clark S, Portnoy A, Grewal S, Brenzel L, Walker DG. Return on investment from childhood immunization in low-and middle-income countries, 2011–20. Health Aff. 2016;35(2):199–207. 10.1377/hlthaff.2015.108. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets analyzed for the current study are available from the corresponding author upon reasonable request.