Abstract
Posterior shoulder instability accounts for a minority of shoulder instability cases. There is a lack of data and treatment algorithms compared to anterior shoulder instability; moreover, many of the proposed techniques focus on bony reconstruction. We describe an open technique of capsular reconstruction in the absence of glenoid bone loss using dermal allograft tissue secured with knotless fixation. This technique offers the advantage of direct visualization of graft placement and simplifies suture management.
Technique Video
Posterior shoulder instability is uncommon compared to anterior instability, accounting for 2% to 10% of reported shoulder instability cases.1 There is a paucity of data regarding treatment algorithms for posterior shoulder instability, especially in revision settings.2
Much of the recent literature has focused on glenoid bony reconstruction procedures for patients with glenoid bone loss.2, 3, 4, 5, 6 There remains a subset of patients who have poorly functioning capsular tissue and recurrent instability, despite the absence of glenoid bone loss. Options for these patients remain limited.
Multiple surgical treatment methods have been proposed, including posterior labral repair and capsular shift.7 These interventions are associated with varying results and high failure rates.8
Posterior capsular reconstruction has been previously described to treat recurrent posterior instability following failed posterior instability procedures or irreparable posterior labral injuries; however, due to the rarity of the procedure, there is no gold-standard technique.7,9
We describe an open technique of posterior capsular reconstruction using dermal allograft tissue secured with knotless fixation (Video 1).
Patient Evaluation, Imaging, and Indications
Patients with a history of posterior shoulder instability should undergo a thorough history and physical examination. A detailed history should include onset of symptoms, location and characteristics of pain or discomfort, previous operative and nonoperative interventions, and ability to voluntarily dislocate. Physical examination components/tests for posterior instability include jerk, Kim, posterior stress, and load-and-shift tests.10 Scapular function should also be assessed as scapular winging can present with posterior shoulder instability. Imaging should include plain radiographs to assess for fracture, magnetic resonance imaging to assess capsulolabral injury, and computed tomography with 3-dimensional reconstructions to characterize bony morphology and evaluate for bone loss.
The indications for open posterior capsular reconstruction are recurrent posterior instability without appreciable glenoid bone loss in the absence of scapular winging. This is typically after a primary failed soft tissue procedure.
Surgical Technique
Step 1: Setup and Patient Positioning
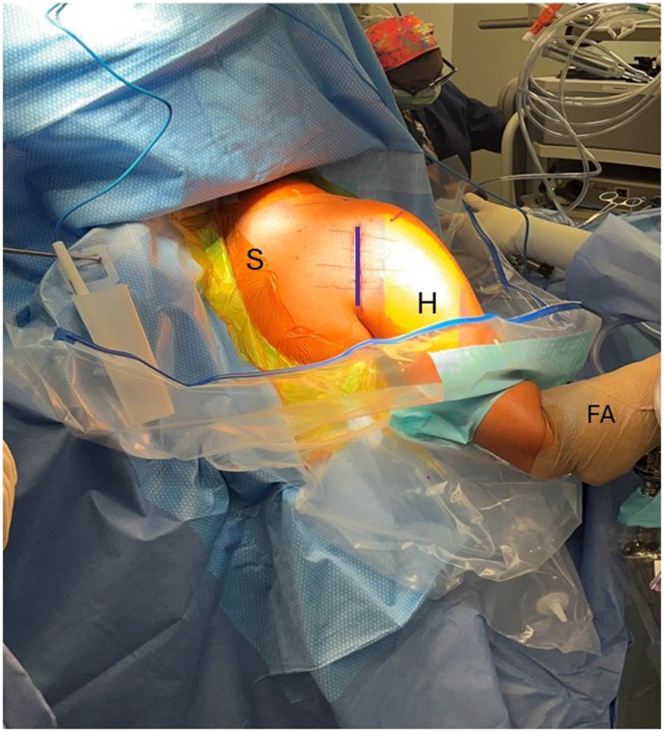
The patient is placed in a beach-chair position with a ramp pillow placed underneath the legs and the head in a neutral position within the head holder. It is important at this step to confirm that the backboard is pushed as far toward the contralateral shoulder as possible to ensure access to the posterior aspect of the operative shoulder (Fig 1). The patient undergoes an examination under anesthesia of the shoulder, and the range of motion, posterior translation, and examination for multidirectional instability are all documented before commencing. The patient is then prepped and draped in a wide fashion.
Fig 1.
Right shoulder exposed: viewed from posterior. Beach-chair positioning: the backboard (green star) is pushed as far toward the contralateral side as possible. Not pictured is the ramp pillow underneath the legs.
Step 2: Incision and Approach
An oblique 4- to 5-cm vertical incision is drawn centered over the glenohumeral joint and extended in line with the deltoid fibers (Fig 2). Dissection is carried through the subcutaneous tissue until the deltoid fascia is reached. Full-thickness flaps are developed. The fascia and deltoid muscle are split in line with the deltoid raphe between the posterior and middle deltoid (Fig 3). A Kolbel retractor is then inserted, and the deltoid is retracted (Fig 4). Care is taken not to split the deltoid too distally and cause injury to the axillary nerve. Deep to the divided deltoid, the posterior rotator cuff is identified and split in line with its fibers horizontally (Fig 5). A capsulotomy is made in line with the divided posterior rotator cuff. A deep blunt Gelpi retractor is placed, retracting the capsule and posterior rotator cuff superiorly and inferiorly.
Fig 2.
Draped right upper extremity viewed from posterior (S, H, FA). An oblique 4- to 5-cm vertical incision (purple line) is drawn centered over the glenohumeral joint and extended distally and laterally in line with the deltoid. (H, humerus; FA, forearm; S, scapula.)
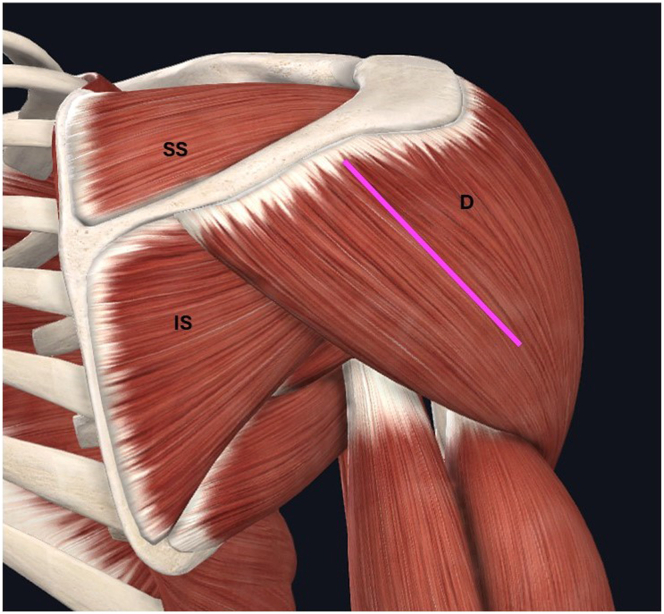
Fig 3.
The fascia/deltoid are then split in line with the deltoid raphe, between the posterior and middle thirds of the deltoid. (D, deltoid; IS, infraspinatus; SS, supraspinatus.)
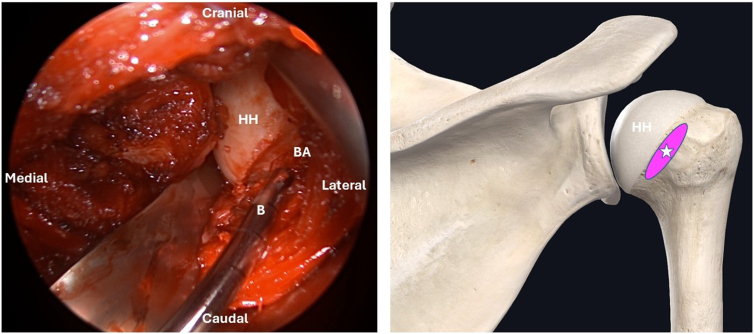
Fig 4.
Divided deltoid as viewed through a posterior approach. Kolbel retractor is inserted in the division created between the posterior deltoid and middle deltoid. (MD, middle deltoid; PD, posterior deltoid.)
Fig 5.
Posterior rotator cuff as viewed through posterior approach: deep to the divided deltoid, the infraspinatus is identified and split (pink-hash) horizontally in line with its fibers. (IS, infraspinatus.)
Step 3: Posterior Glenoid and Bare Area Preparation
The posterior glenohumeral joint is identified. Any loose sutures or previous hardware within the posterior glenoid or humerus are removed. A rasp and/or burr are used to decorticate the bare area medial to the posterior rotator cuff insertion (Fig 6) and the area just medial to the posterior labrum on the posterior aspect of the glenoid (Fig 7). This will assist in graft healing.
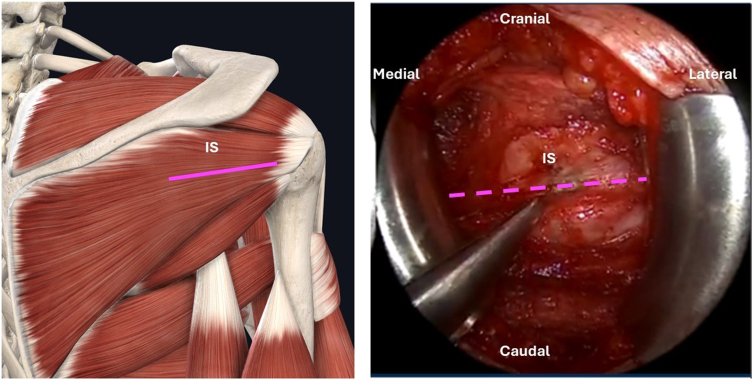
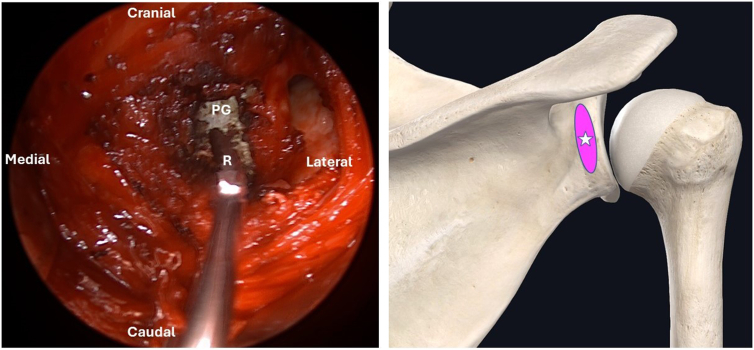
Fig 6.
Posterior glenohumeral joint as viewed through posterior approach. A rasp and/or burr is used to decorticate the bare area (star) medial to the posterior rotator cuff insertion to improve graft healing. (B, burr; BA, bare area; HH, humeral head.)
Fig 7.
Posterior glenohumeral joint as viewed through posterior approach. A rasp and/or burr is used to decorticate the area just medial to the posterior labrum on the posterior aspect of the glenoid (star). (PG, posterior aspect of the glenoid; R, rasp.)
Step 4: Preparations for Graft
Three 1.8-mm knotless FiberTak anchors (Arthrex) are placed just medial to the posterior labrum (Fig 8) at the superior, middle, and inferior aspect of the posterior glenoid. The sutures from the anchors are brought to the proposed insertion area on the humerus, just medial to the posterior cuff insertion, and measured with a suture-measuring instrument or a ruler. This is done with the arm in a neutral position of abduction and rotation. Measurements are made from the glenoid to the humerus at both the superior and inferior aspects of the planned graft as well as the vertical height of the graft on each side.
Fig 8.
Posterior glenohumeral joint with anchors in place as viewed through a posterior approach. Three 1.8-mm knotless FiberTak anchors (black dots) are placed just medial to the posterior labrum. (A, anchor; PL, posterior labrum.)
Step 5: Graft Preparation
A 3-mm ArthroFlex dermal allograft (Arthrex) is cut to the appropriate dimensions as measured using the sizing guide. It is important to measure and cut at least 2 to 3 mm smaller than the measured dimensions as the graft is prone to stretch and the construct is dependent on graft tension. Two FiberLoop sutures (Arthrex) are passed through the lateral side of the allograft in a “luggage tag” fashion (Fig 9). These will be about 2 mm from the edges to avoid pulling through the edge of the graft.
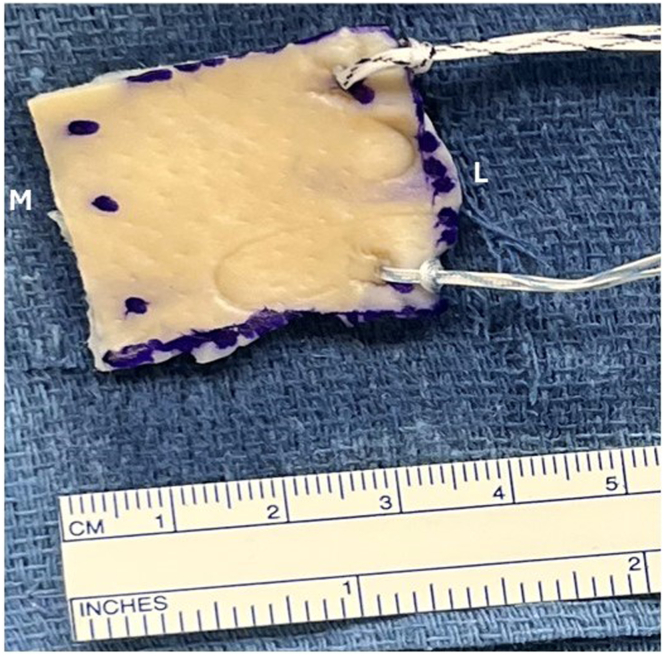
Fig 9.
Measured and prepared graft as viewed on back table prior to insertion. Two FiberLoop (Arthrex) sutures are passed through the lateral side of the allograft. These will be about 2 mm from the edges to avoid pulling through the edge of the graft. The 3 medial dots will be later used to insert the repair stitches from the anchors. (L, lateral; M, medial.)
Step 6: Graft Delivery
The repair sutures from each glenoid anchor are inserted through their designated location in the graft in a horizontal mattress fashion. A suture passer or a free needle can be used (Fig 10). After each repair suture is placed, the shuttle suture from the corresponding anchor is used to pull the repair suture back through the knotless mechanism of the anchor. This is repeated for each of the 3 glenoid anchors. At this point, the graft is shuttled onto the posteromedial glenoid by pulling on the 3 repair sutures in equal tension (Fig 11). When the graft is secured onto the glenoid, the lateral graft “luggage tag” stitches are pulled taut and placed against the planned insertion site on the humerus, and the tension is confirmed. It is important to note that at this point, if further tension is desired, the luggage tag sutures can be removed, and the graft can be carefully shortened in the horizontal plane and then the luggage tag sutures can be replaced. Once the graft tension is confirmed, the luggage tag sutures are loaded into a 3.5-mm self-punching PushLock anchor (Arthrex) and inserted into the superior and inferior aspects of the bare space on the humeral head. The dermal allograft is now positioned in place under slight tension with 3 medial points of fixation along the posterior-medial glenoid and 2 points of fixation on the humeral head (Fig 12). The posterior capsule can be closed over the graft with interrupted sutures and then the posterior cuff split is repaired as well. The deltoid fascia is also repaired prior to closing skin.
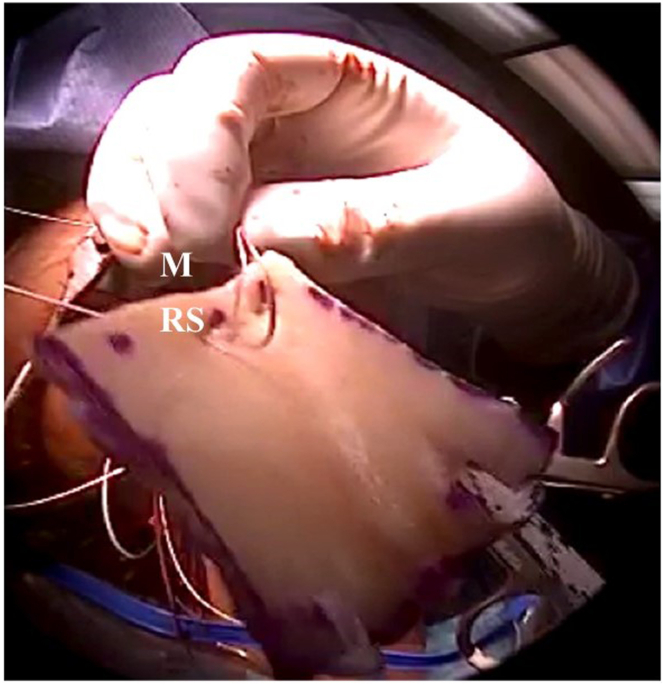
Fig 10.
View of measured and prepared graft prior to insertion. The FiberTak (Arthrex) repair sutures from each glenoid anchor are inserted through their designated location on the medial side of the graft as a horizontal mattress using a suture passer or a needle. (M, medial; RS, repair suture.)
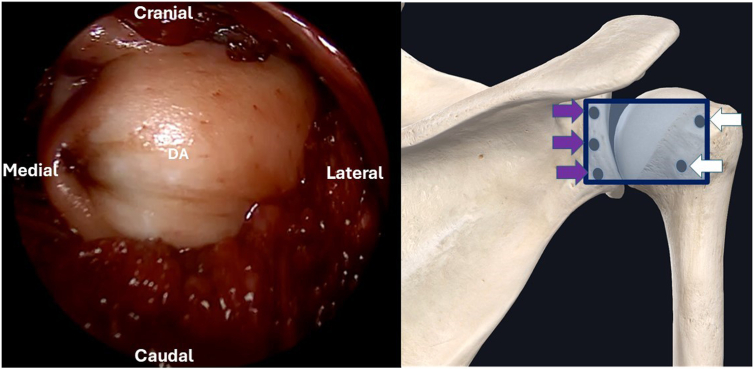
Fig 11.
Posterior glenohumeral joint as viewed through posterior approach. The dermal allograft is shuttled to the posteromedial glenoid by pulling on the 3 shuttle sutures in equal tension. (DA, dermal allograft; PMG, posteromedial glenoid; SS, shuttle suture.)
Fig 12.
Dermal allograft overlying the glenohumeral joint as viewed from a posterior approach. The dermal allograft is positioned in place under slight tension with 3 medial points of fixation (purple arrows) along the posterior-medial glenoid and 2 points of fixation (white arrows) on the bare area of the humeral head using push-lock anchors. (DA, dermal allograft.)
Postoperative Care
The patient is placed into a shoulder immobilizer in the neutral position following surgery with no shoulder range of motion for 2 weeks. The patient is permitted to perform elbow, wrist, and hand range of motion during this time. At the 2-week mark, the patient will advance to passive forward elevation and abduction to 45°. No active range of motion or passive internal rotation is permitted. At the 6-week mark, patients can begin progressing from passive to active motion. No aggressive stretching is performed. Active strengthening can be performed under the guidance of physical therapy at the 3- to 4-month mark. Care is taken to not overly “stretch” the repair by early initiation of physical therapy.
Discussion
This Technical Note demonstrates an open technique of posterior shoulder capsular reconstruction using dermal allograft tissue secured with knotless fixation, which adds to a developing list of treatment options.
As with any technique, ours confers certain advantages and disadvantages (Table 1), along with pearls and pitfalls (Table 2). Suture management and graft passage often complicate an already technically demanding surgery. This open approach significantly improves the ease of graft delivery and reduces the time of procedure associated with complex suture management compared to previously described all-arthroscopic techniques.9
Table 1.
Advantages/Disadvantages
| Advantages | Disadvantages |
|---|---|
| Direct visualization of posterior capsule/reconstruction | Technical difficulty |
| Simplified suture management | Implant costs |
| Knotless fixation, avoids suture knots adjacent to articular cartilage | No long-term outcome data |
| Posterior labrum is left intact |
Table 2.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| Leave posterior labrum intact | Oversizing graft will lead to continued instability |
| Place arm in neutral position when sizing graft | Distal split of deltoid fibers can place axillary nerve at risk |
| Place each labral repair suture through the graft and then shuttle back through the knotless mechanism one at a time as opposed to leaving all until the end to improve suture management efficiency |
Disclosures
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: S.A.P. is a consultant or advisor for Exactech and Arthrex, receives nonfinancial support from Exactech, and is a board member of the American Academy of Orthopaedic Surgeons and American Shoulder and Elbow Surgeons. All other authors (B.L.H., J.L.L., A.E.B.) declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Supplementary Data
This video demonstrates the surgical technique of open posterior capsular reconstruction using acellular dermal allograft.
References
- 1.Woodmass J.M., Lee J., Wu I.T., et al. Incidence of posterior shoulder instability and trends in surgical reconstruction: A 22-year population-based study. J Shoulder Elbow Surg. 2019;28:611–616. doi: 10.1016/j.jse.2018.08.046. [DOI] [PubMed] [Google Scholar]
- 2.Hurley E.T., Aman Z.S., Doyle T.R., et al. Posterior shoulder instability part II—glenoid bone-grafting, glenoid osteotomy, and rehabilitation/return to play—an international expert Delphi consensus statement. Arthroscopy. 2025;41:181–195.e7. doi: 10.1016/j.arthro.2024.04.034. [DOI] [PubMed] [Google Scholar]
- 3.Warner J.J., Gill T.J., O'Hollerhan J.D., Pathare N., Millett P.J. Anatomical glenoid reconstruction for recurrent anterior glenohumeral instability with glenoid deficiency using an autogenous tricortical iliac crest bone graft. Am J Sports Med. 2006;34:205–212. doi: 10.1177/0363546505281798. [DOI] [PubMed] [Google Scholar]
- 4.Testa E.J., van der List J.P., Waterman B.R., Caldwell P.E., III, Parada S.A., Owens B.D. Management of bone loss in posterior glenohumeral shoulder instability: Current concepts. JBJS Rev. 2024;12 doi: 10.2106/JBJS.RVW.23.00243. e23.00243. [DOI] [PubMed] [Google Scholar]
- 5.Testa E.J., Morrissey P., Albright J.A., et al. A posterior acromial bone block augmentation is biomechanically effective at restoring the force required to translate the humeral head posteriorly in a cadaveric, posterior glenohumeral instability model. Arthroscopy. 2024;40:1975–1981. doi: 10.1016/j.arthro.2024.01.014. [DOI] [PubMed] [Google Scholar]
- 6.van Spanning S.H., Picard K., Buijze G.A., Themessl A., Lafosse L., Lafosse T. Arthroscopic bone block procedure for posterior shoulder instability: Updated surgical technique. Arthrosc Tech. 2022;11:e1793–e1799. doi: 10.1016/j.eats.2022.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hurley E.T., Aman Z.S., Doyle T.R., et al. Posterior shoulder instability, part I—diagnosis, nonoperative management, and labral repair for posterior shoulder instability—an international expert Delphi consensus statement. Arthroscopy. 2025;41:166–180.e11. doi: 10.1016/j.arthro.2024.04.035. [DOI] [PubMed] [Google Scholar]
- 8.Provencher M.T., LeClere L.E., King S., et al. Posterior instability of the shoulder: Diagnosis and management. Am J Sports Med. 2011;39:874–886. doi: 10.1177/0363546510384232. [DOI] [PubMed] [Google Scholar]
- 9.Karpyshyn J., Gordey E.E., Coady C.M., Wong I.H. Posterior glenohumeral capsular reconstruction using an acellular dermal allograft. Arthrosc Tech. 2018;7:e739–e745. doi: 10.1016/j.eats.2018.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Frank R.M., Romeo A.A., Provencher M.T. Posterior glenohumeral instability: Evidence-based treatment. J Am Acad Orthop Surg. 2017;25:610–623. doi: 10.5435/JAAOS-D-15-00631. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video demonstrates the surgical technique of open posterior capsular reconstruction using acellular dermal allograft.