Abstract
Background
Self-management and empowerment are critical components in the treatment of diabetes, a chronic condition that has become an increasingly significant global health issue. While standard diabetes education is essential for effective disease management, personalized interventions aligned with the patient’s preferences are also necessary. One promising solution is the integration of coaching approaches into chronic disease management.
Methods
This study was designed as a randomized controlled trial with a pretest-posttest design and three parallel arms: a Holistic Nurse Coaching group (n = 34), a Diabetes Education (n = 34) group, and a control group (n = 34). Data were collected through a Sociodemographic Data Collection Form, a Diabetes Data Collection Form, the Type 2 Diabetes Mellitus Self-Management Scale and the Diabetes Empowerment scale. The aim was to evaluate the effect of Holistic Nurse Coaching on glycemic control, diabetes self-management, and empowerment in individuals with type 2 diabetes. The Holistic Nurse Coaching group received nine individualized holistic nurse coaching sessions over a three-month period. The Diabetes Education group participated in nine group-based diabetes education sessions over the same period. The control group received no intervention. Mean comparison tests, correlation tests and multiple regression analysis techniques were employed in the statistical analysis. A 5% margin of error (p < 0.05) was adopted to determine statistical significance.
Results
Following the holistic nurse coaching intervention, statistically significant improvements were observed in participants’ diabetes self-management, empowerment, and HbA1c levels (d = 3.752, d = 3.104, and d = 1.147, respectively; p < 0.001). A strong, positive, and statistically significant correlation was identified between posttest diabetes self-management and empowerment scores. Furthermore, the diabetes empowerment scores accounted for approximately 68.5% of the variance in diabetes self-management scores (p < 0.05).
Conclusions
Holistic nurse coaching was found to significantly enhance diabetes self-management and empowerment. These findings suggest that holistic nurse coaching may serve as an effective, person-centered intervention to support individuals with type 2 diabetes in managing their condition.
Trial registration
The study was registered in ClinicalTrials NCT05545722. Retrospectively registered. 16/09/2022.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12912-025-03252-0.
Keywords: Diabetes, Diabetes empowerment, Holistic nurse coach, Nursing, Self-management
Highlights
What is known about the topic:
Diabetes education is a fundamental component of effective diabetes management and empowerment.
Individualized interventions are essential to support diabetes self-management.
To date, no randomized controlled trials have compared diabetes education and holistic nurse coaching using a three-arm study design.
What this paper adds:
Holistic nurse coaching enhances diabetes self-management, glycemic control, and patient empowerment.
Both holistic nurse coaching and diabetes education improve self-management and empowerment; however, holistic nurse coaching was found to be more effective across all measured outcomes.
Holistic nurse coaching offers a safe, cost-effective, and promising alternative for improving glycemic control and managing diabetes.
Holistic nurse coaching can be delivered digitally, making it easily accessible and scalable for broader populations, including those in remote or underserved areas.
Relevance to Clinical Practice and/or Recommendations for Further Research:
Holistic nurse coaching has been shown to be more effective than standard diabetes education in improving diabetes-related outcomes.
Integrating holistic nurse coaching into routine clinical practice may enhance long-term treatment adherence and overall patient well-being.
As a safe and cost-effective intervention, holistic nurse coaching represents a viable alternative for managing diabetes and, potentially, other chronic conditions.
Large-scale, multi-center randomized controlled trials are needed to further confirm the effectiveness of holistic nurse coaching in diverse healthcare settings.
The long-term cost-effectiveness of holistic nurse coaching compared to conventional diabetes education warrants further investigation.
Future studies should examine the impact of holistic nurse coaching on quality of life, treatment adherence, and broader health outcomes.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12912-025-03252-0.
Strengths of the Research
This is the first randomized controlled study in Türkiye in which holistic nurse coaching was offered to individuals with diabetes. The presence of two interventions and a control group in the study makes the study powerful. The researchers spent 54 h on diabetes education and 306 h on the holistic nurse coaching interviews.
Background
Self-management and empowerment are critical for helping individuals with diabetes better manage their condition and improve their health. “Empowerment” refers to an approach that enables individuals with diabetes to gain a deeper understanding of their condition, actively engage in self-care, and adopt healthy lifestyle practices [1]. Key self-management behaviors include maintaining a healthy diet, engaging in regular physical activity, monitoring blood glucose levels, adhering to prescribed medications, and developing effective coping strategies and problem-solving skills. Both self-management and empowerment play pivotal roles in treating diabetes, which is a chronic condition that has become an increasing global health concern [2, 3].
For decades, diabetes education has been a cornerstone of effective diabetes management. It provides individuals with the essential knowledge, skills, and motivation needed to make informed decisions about their care. Structured diabetes education programs are designed to support behavioral changes by addressing topics such as nutrition, physical activity, medication adherence, blood glucose monitoring, and the prevention of complications [2]. Research has shown that diabetes education significantly improves glycemic control, self-efficacy, quality of life, and reduces healthcare costs [4, 5]. However, its long-term effectiveness is limited by challenges in sustaining changes in behavior. Many individuals with diabetes revert to previous habits and experience a decline in glycemic control once the formal stage of education ends, underscoring the need for ongoing, individualized support beyond the initial education [6–8].
To ensure effective self-management in individuals with diabetes, it is essential to develop an individualized treatment plan that considers the patient’s preferences, values, and goals [9]. Chronic disease management requires assessing the patient’s readiness for change and considering the psychosocial factors that affect them. Integrating coaching into this process can provide a personalized approach that helps support improvements [10]. Given their pivotal role in diabetes education and motivation, nurses are ideally positioned to take on this coaching role [11]. Holistic nurse coaching (HNC) can be defined as a structured, purpose-driven, and results-oriented approach in which nurses provide supportive, relationship-centered guidance to patients in order to enhance their health and well-being [11, 12]. HNC can help patients with chronic disease to acquire the necessary skills and expertise and become more empowered, enabling them to adopt healthier lifestyle behaviors, enhance their coping strategies, and more effectively manage their health challenges [13–15]. This innovative strategy, grounded in a holistic paradigm rather than a traditional medical model, has already demonstrated its effectiveness in improving outcomes for patients with chronic conditions [14, 16, 17]. Digital coaching and digital self-management interventions are increasingly recognized as effective methods for delivering diabetes self-management education and support [18]. In addition, HNC is now frequently seen as a critical adjunctive treatment for diabetes and one that should be leveraged as an extension of the nursing role [11]. By improving treatment adherence, encouraging a healthy lifestyle, and helping patients through the process of accepting their condition, HNC supports better disease management and leads to significant improvements in patient outcomes. In recent years, the number of studies examining the effectiveness of coaching in improving diabetes management has significantly increased [19, 20]. Coaching has been shown to positively influence key clinical outcomes such as HbA1c levels, glycemic control, and diabetes-related quality of life [21, 22]. However, there remains a gap in population-based randomized controlled trials that explore the effects of these interventions on both clinical outcomes and patient-reported results [22].
Given the well-known limitations of traditional diabetes education in sustaining behavioral change, it is essential to compare its effectiveness with HNC. Unlike standard diabetes education, which primarily focuses on delivering information, HNC emphasizes the development of self-efficacy through personalized coaching, goal setting, and emotional support, all of which may contribute to more sustainable health improvements. This study compared these two interventions– diabetes education and HNC–in an effort to identify which approach better supports self-management and empowerment in individuals with type 2 diabetes mellitus (T2DM). By assessing the effects of both interventions on glycemic control, diabetes self-management, and empowerment, the study sought to clarify the relative benefits of incorporating HNC into diabetes care.
Research hypotheses
H0:
HNC has no significant effect on glycemic control, diabetes self-management, and diabetes empowerment in the patients who receive it, when compared to patients in the Diabetes Education and control groups.
H1:
HNC has a significant effect on glycemic control, diabetes self-management, and diabetes empowerment in the patients who receive it, when compared to patients in the Diabetes Education and Control groups.
Methods
Design
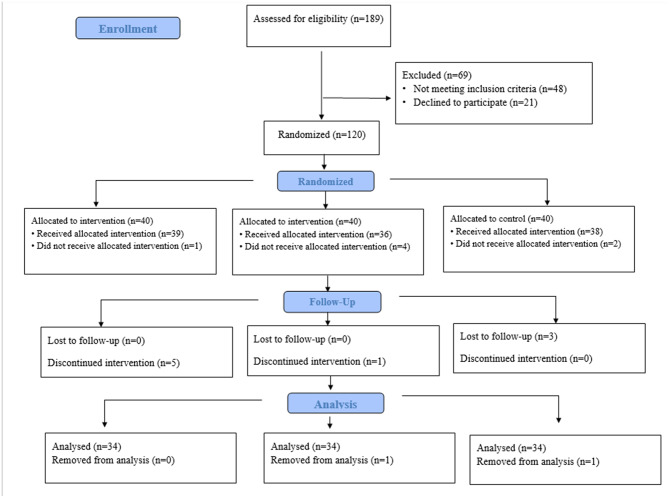
The study was a three-arm randomized controlled trial utilizing a pretest-posttest experimental design in order to compare the effectiveness of HNC and diabetes education. The study was conducted in accordance with the Consolidated Standards of Reporting Trials (CONSORT) guidelines to ensure methodological transparency and comprehensive reporting. Figure 1 presents the study design and flow diagram in alignment with the CONSORT framework [23].
Fig. 1.
CONSORT flow chart
Participants
The study was conducted between April 2021 and July 2022 with patients who presented to the internal medicine outpatient clinic of a state hospital in Ankara. The inclusion criteria were as follows: (1) being between the ages of 18 and 65; (2) owning and actively using a smartphone; (3) having been diagnosed with T2DM for at least one year with an HbA1c level > 7; (4) having no diagnosed psychiatric disorders; (5) being able to speak, understand, read, and write in Turkish; and (6) voluntarily agreeing to participate in the study. The exclusion criteria included: (1) having advanced retinopathy, nephropathy, neuropathy, or a diabetic foot wound; (2) pregnancy; and (3) a cancer diagnosis; (4) a diagnosis of Type 1 Diabetes Mellitus; and (5) gestational diabetes.
Participants were excluded from the sample during the study if: (1) they voluntarily chose to withdraw from the study; (2) they missed more than one coaching session in the HNC group; or (3) they failed to attend more than one group session in the Diabetes Education group or (4) became pregnant during the study period.
Sample size calculation
The population of the study included individuals with T2DM who applied to the polyclinic. In order for conduct ANOVA to determine the distinction between the groups, it was decided to interview 102 people in groups of 34, with a 0.05 first type error, 0.95 power and 0.40 high effect size calculated using the G*Power (ver. 3.1.9.2) program. To account for potential data loss or participant dropout, a total of 120 individuals were included. (Fig. 1).
Randomization, allocation and blind technique
To prevent bias in the allocation of participants to the three study groups, they were each given a number from 1 to 120 and assigned randomly to each group using https://randomizer.org. A CONSORT flowchart has been included to illustrate the study design (Fig. 1).
A blinded approach was employed for data collection, statistical analysis, and reporting. Prior to initiation, the responsible investigator assessed participants for eligibility. The purpose and scope of the study were explained to participants, and written informed consent was obtained. To minimize researcher bias, a specialized nurse (rather than the principal investigator) was responsible for collecting and entering the pre- and posttest data. Data were labeled anonymously using the codes “A,” “B,” and “C,” without indicating which group corresponded to the first intervention, the second intervention, or the control group. Data analysis and report writing were carried out by an independent statistician who remained blinded to the group allocation throughout the process. The group codes were only revealed to the primary researcher after statistical analyses had been completed and the research report was finalized.
Ethical considerations
Ethical approval
for the study was obtained from the Ankara Yıldırım Beyazıt University Heath Science Ethics Committee (Research Code: 2021-20; meeting date and decision number: 16.02.2021–20). In addition, the necessary institutional permission was granted by the state hospital where the study was conducted. Participants were informed about the study’s purpose, significance, and data collection procedures, and it was clearly stated that only the research team would have access to the data collected. The informed consent form was read aloud to participants, and it was emphasized that participation was entirely voluntary. Written informed consent was obtained from all individuals who agreed to take part in the study. Participants were also informed that they could withdraw from the study at any time without any consequences. The research was conducted in full accordance with the principles outlined in the Declaration of Helsinki.
Intervention
The study was conducted at a public hospital in Ankara, Türkiye. The recruitment of participants began in April 2021 and the study was completed in July 2022. Following the approval of the institutional ethics committee and after the hospital administration had granted the necessary permissions, the researcher visited the study site to screen patients diagnosed with T2DM for eligibility. A total of 120 individuals were assessed for inclusion based on the predefined inclusion and exclusion criteria. Eligible participants were informed about the study, and those who agreed to participate provided their written informed consent. After this, the participants were randomly assigned to one of three groups: Intervention Group 1 (the Diabetes Education group), Intervention Group 2 (the HNC group), and the control group. The study was completed with 102 participants across the three groups. As shown in the CONSORT flow diagram (Fig. 1), some participants did not receive the allocated intervention or were excluded from the final analysis for a variety of reasons.
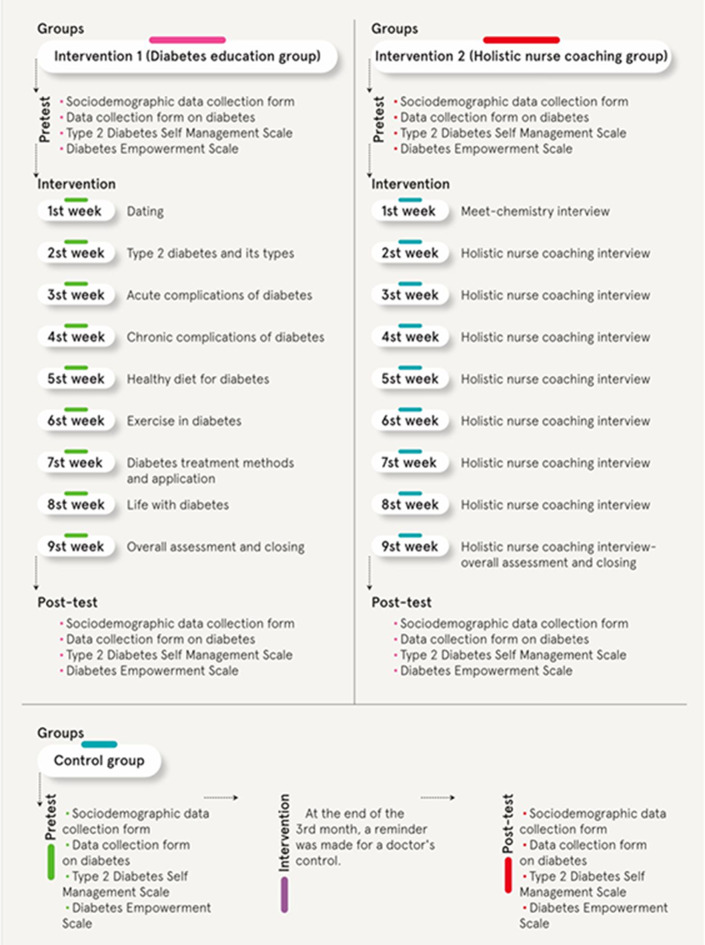
Intervention Group 1 (Diabetes education)
Pretests were administered to participants assigned to Intervention Group 1 after they had signed the informed consent form. Individuals in this group, all of whom were diagnosed with T2DM, received structured diabetes education. The entire education program was conducted online. Educational content was delivered via PowerPoint presentations, incorporating relevant visuals and utilizing an interactive teaching approach. A total of nine group sessions were conducted with the participants in Intervention Group 1. These sessions were held once every 10 days and the participants were organized into subgroups of approximately eight individuals for each session. The first session served as an introduction. Subsequent sessions covered a range of topics including the definition of diabetes, normal fasting and postprandial blood glucose values, acute and chronic complications of diabetes, foot health and care, healthy nutrition, the importance of exercise, diabetes treatment, and living with diabetes (Fig. 2). Each session concluded with a question-and-answer segment, and sessions lasted approximately 45 to 60 min. All sessions were conducted online at pre-scheduled times. Following each session, educational materials were shared with the participants. The diabetes education component was completed within a three-month period for each subgroup. Upon completion of the diabetes education program, the participants underwent a routine medical check-up. Thereafter, posttests were administered by a specialist nurse who was not involved in the educational intervention. At the end of the study, the participants in this group were offered the opportunity to take part in the HNC sessions on a voluntary basis.
Intervention Group 2 (Holistic nurse coaching)
Pretests were administered to participants assigned to Intervention Group 2 after they had signed the informed consent form. In this group, the interviews were conducted individually and tailored to the specific needs of each person with diabetes. The intervention consisted of nine HNC sessions, conducted once every 10 days. Each session lasted approximately 45 to 60 min and was held online at scheduled times agreed upon with the counselee.
The first session served as an introductory meeting. If both the counselee and the HNC agreed to proceed with the coaching relationship following this session, they signed an “HNC Agreement.” The second through eighth sessions were conducted using established coaching materials and techniques, adapted to the counselee’s personal agenda and goals (Fig. 2). These materials included thought-provoking and Cartesian questions, a strategic planning checklist, to-do lists, a coaching preparation form, a daily habits follow-up chart, a priority focus and planning form, “ saying yes/saying no” exercises, the Diabetes Wheel of Life, visualization of the counselee’s future condition, sabotage identification, SWOT analysis, SMART goal-setting, priority management in diabetes, brainstorming activities, and the GROW model [24, 25]. The HNC sessions were conducted over a three-month period for each participant. Upon completion of the HNC sessions, the participants underwent a routine medical check-up. Posttests were then administered by a specialist nurse, independent of the researcher, to ensure objectivity in data collection.
Fig. 2.
Study design
Control group
The pretest was administered to the participants assigned to the control group after they had signed the informed consent form. At the end of the third month, the individuals in this group were reminded to attend a routine medical check-up. The participants in the control group were individuals who had previously received at least one diabetes education session from a diabetes nurse (Fig. 2). Following the medical check-up, posttests were administered by a specialist nurse, rather than the researcher, to maintain objectivity. At the conclusion of the study, the participants in the control group were offered the opportunity to take part in the HNC sessions on a voluntary basis.
Measurements
Data for the study were collected using a Sociodemographic Data Form, a Diabetes Data Collection Form, the Diabetes Empowerment (DES) Scale, and the T2DM Diabetes Self-Management Scale (T2DM-DSMS).
Sociodemographic data collection form
This form, developed by the researcher based on a review of the relevant literature, included items to collect the participants’ sociodemographic characteristics. It contained questions related to gender, age, height, and other basic personal information [22, 26].
Diabetes data collection form
This form gathered information specific to the participant’s diabetes status. It included questions related to the duration of diabetes and the most recent HbA1c value, which was obtained during the participant’s routine medical check-up [27–29].
Type 2 Diabetes Mellitus Self-Management Scale (T2DM-DSMS)
Developed by Koç and Özkan (2020), this scale assesses self-management behaviors in individuals with type 2 diabetes. It is a five-point Likert-type scale consisting of 19 items across three sub-dimensions: “Healthy Lifestyle Behaviors” (11 items), “Blood Glucose Management” (four items), and “Health Services Utilization” (four items). The total score ranges from 19 to 95, with higher scores indicating better self-management and lower scores indicating poorer self-management. The original Cronbach’s alpha for the total scale was reported as 0.856. In the present study, the Cronbach’s alpha values were calculated as 0.828 in the pretest and 0.947 in the posttest, indicating high internal consistency [30].
Diabetes Empowerment Scale (DES)
This scale was developed in 2000 by Anderson and Funnell to assess the psychosocial self-efficacy of individuals with T2DM [31]. The scale was adapted into Turkish by Özcan et al. It is a five-point Likert-type scale consisting of 28 items across three sub-dimensions: “Managing the Psychosocial Aspects of Diabetes” (9 items), “Assessing Dissatisfaction and Readiness to Change” (9 items), and “Setting and Achieving Diabetes Goals” (10 items). Subscale scores range from 1 to 5 and are calculated by summing the item scores within each sub-dimension and dividing the result by the number of items in that subscale. The original scale had a Cronbach’s alpha coefficient of 0.886. In the present study, the Cronbach’s alpha was calculated as 0.828 for the pretest and 0.964 for the posttest, indicating high internal consistency [32].
Statistical analysis
A number of techniques were employed in the statistical analysis of the results, including validity analysis, mean comparison tests, correlation tests, and multiple regression analysis. To determine the most appropriate statistical tests for hypothesis testing, the Shapiro-Wilk test was used to assess normality, and the Levene test was applied to evaluate the assumption of homogeneity of variances. For data that met the assumption of normal distribution, a paired t-test was used for comparisons between two dependent groups, while ANOVA was used for comparisons among three or more independent groups. In cases where ANOVA indicated significant differences, Bonferroni correction and independent samples t-tests were performed for post-hoc multiple comparisons. Effect sizes were calculated for all statistically significant results from the paired t-tests and ANOVA, using Cohen’s d. A 5% margin of error (p < 0.05) was adopted to determine statistical significance. All analyses were conducted using R Project software [33], with the lavaan package utilized for relevant statistical procedures [34].
Results
Information regarding the sociodemographic characteristics of the participants is presented in Table 1. Examining the findings, it was determined that a plurality of the male participants (36.00%) were in the HNC group, while female participants made up 34.62% of both the Diabetes Education and the control groups. Additionally, it was found that a plurality of the unmarried diabetic individuals (47.37%) were in the coaching group, while married diabetic individuals made up 34.94% of both the Diabetes Education and the control groups (Table 1).
Table 1.
Sociodemographic characteristics of the participants
| Variable | Education | Coaching | Control | |
|---|---|---|---|---|
| Age | 52.79 ± 7.69 | 45.62 ± 9.93 | 52.09 ± 8.69 | |
| Diabetes duration | 8.15 ± 3.77 | 7.94 ± 4.65 | 7.82 ± 4.42 | |
| Gender | ||||
| Male | 32.00% (16) | 36.00% (18) | 32.00% (16) | |
| Female | 34.62% (18) | 30.77% (16) | 34.62% (18) | |
| Marital status | ||||
| Single | 26.32% (5) | 47.37% (9) | 26.32% (5) | |
| Married | 34.94% (29) | 30.12% (25) | 34.94% (29) | |
| Education level | ||||
| Primary school | 25.00% (4) | 18.75% (3) | 56.25% (9) | |
| High school | 34.29% (12) | 40.00% (14) | 25.71% (9) | |
| Undergraduate | 36.36% (16) | 34.09% (15) | 29.55% (13) | |
| Postgraduate | 28.57% (2) | 28.57% (2) | 42.86% (3) | |
| Income level | ||||
| Less than expenditure | 26.47% (9) | 44.12% (15) | 29.41% (10) | |
| Equal to expenditure | 40.91% (18) | 25.00% (11) | 34.09% (15) | |
| More than expenditure | 29.17% (7) | 33.33% (8) | 37.50% (9) | |
| Place of residence | ||||
| Urban area | 33.33% (30) | 33.33% (30) | 33.33% (30) | |
| District | 33.33% (4) | 33.33% (4) | 33.33% (4) | |
The results of the intra-group and inter-group comparisons of the T2DM-DSMS and DES total scores, and the HbA1c values of the diabetic participants in relation to the education, control, and coaching groups are presented in Table 2. Examining the inter-group comparison results, it was found that there were no statistically significant differences in the T2DM-DSMS and DES total scores, and the HbA1c values measured at pretest between the education, control, and coaching groups (p > 0.05). However, statistically significant differences were observed in the T2DM-DSMS and DES total scores, and HbA1c values measured at posttest between the education, control, and coaching groups (p < 0.05). According to these findings, the participants in the control group had significantly lower T2DM-DSMS total scores at posttest compared to those in the education and coaching groups, with effect sizes of (d = 1.544) and (d = 3.483), respectively, both indicating a very large effect. Furthermore, it was found that diabetic participants in the education group had significantly lower T2DM-DSMS total scores at posttest compared to those in the coaching group, with an effect size of (d = 1.856), indicating a very large effect (Table 2).
Table 2.
Comparison of HbA1c levels, diabetes Self-Management, and empowerment scores by group
| Group | Pretest | Posttest | T | p | Effect size | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Diabetes self-management total | Education | 50.00 ± 9.45 | 65.26 ± 9.40 | -9.242 | < 0.001 | 1.619 | |||||
| Control | 49.00 ± 9.44 | 50.74 ± 9.41 | -5.207 | < 0.001 | 0.184 | ||||||
| Coaching | 46.44 ± 10.35 | 81.82 ± 8.41 | -14.932 | < 0.001 | 3.752 | ||||||
| F | 1.203 | 99.612 | |||||||||
| p | 0.305 | < 0.001 | |||||||||
| T0-T1* | - | 1.544 | |||||||||
| T1-T2* | - | 3.483 | |||||||||
| T0-T2* | - | 1.856 | |||||||||
| Diabetes empowerment total | Education | 2.96 ± 0.34 | 3.39 ± 0.44 | -8.930 | < 0.001 | 1.114 | |||||
| Control | 3.06 ± 0.28 | 3.05 ± 0.30 | 0.455 | 0.652 | - | ||||||
| Coaching | 2.97 ± 0.41 | 4.36 ± 0.48 | -13.948 | < 0.001 | 3.104 | ||||||
| F | 0.899 | 90.854 | |||||||||
| p | 0.410 | < 0.001 | |||||||||
| T0-T1* | - | 0.909 | |||||||||
| T1-T2* | - | 3.263 | |||||||||
| T0-T2* | - | 2.089 | |||||||||
| HbA1c | Education | 9.30 ± 1.45 | 8.89 ± 1.31 | 5.042 | < 0.001 | 0.294 | |||||
| Control | 9.43 ± 1.73 | 9.40 ± 1.68 | 0.692 | 0.494 | - | ||||||
| Coaching | 9.41 ± 1.54 | 7.93 ± 0.97 | 9.299 | < 0.001 | 1.147 | ||||||
| F | 0.072 | 10.254 | |||||||||
| p | 0.930 | < 0.001 | |||||||||
| T0-T1* | - | - | |||||||||
| T1-T2* | - | 1.066 | |||||||||
| T0-T2* | - | - | |||||||||
T0: Education, T1: Control, T2: Coaching, * Effect size
According to the findings, the participants in the control group had significantly lower DES total scores at posttest compared to those in the education and coaching groups, with effect sizes of (d = 0.909) and (d = 3.263), respectively, both indicating a very large effect. Additionally, it was observed that the participants in the education group had significantly lower DES total scores at posttest compared to those in the coaching group, with an effect size of (d = 2.089), indicating a very large effect (Table 2).
According to the findings, the participants in the control group had significantly higher HbA1c values at post-test compared to those in the coaching group, with an effect size of (d = 1.066), indicating a very large effect (Table 2).
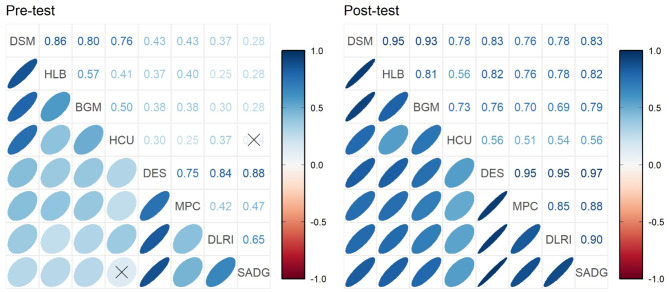
The results of the Pearson correlation test showing the relationship between the T2DM-DSMS and DES total scores, as well as their subscale scores, measured at pretest and posttest, are presented in Fig. 3. Examining the correlation analysis results, a strong positive relationship was found between the T2DM-DSMS total scores and the DES total scores measured at posttest, with a statistically significant correlation (r = 0.83; p < 0.05).
Fig. 3.
Relationship between pretest–posttest diabetes self-management and empowerment scores. T2DM-DSM: Diabetes Self-Management Scale; HLB: Healthy lifestyle behaviors; BGM: Blood glucose management; HCU: Healthcare utilization; DES: Diabetes Empowerment Scale; MPC: Management of psychosocial characteristics; DLRI: Dissatisfaction level and readiness for improvement; SADG: Setting and achieving diabetes goals
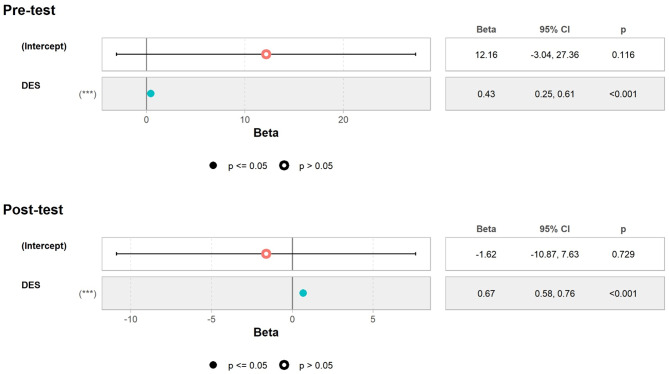
The results of the simple regression analysis, in which the T2DM-DSMS total scores measured at pre-test and post-test were used as the dependent variable and the DES total scores as the independent variable, are presented in Fig. 4. Examining the findings, the total score for the DES explained approximately 68.5% of the variance in the T2DM-DSMS total scores (p < 0.05). Based on this result, a one-unit increase in a participant’s total diabetes empowerment score was associated with an approximate 0.670-point increase in their diabetes self-management score (Fig. 4).
Fig. 4.
Simple regression analysis of pretest–posttest diabetes self-management scores. DES: Diabetes empowerment scale
Discussion
This study investigated the effect of HNC on glycemic control, diabetes self-management, and diabetes empowerment in individuals with T2DM.
According to the American Diabetes Association (ADA), one of the most essential members of the diabetes care team is the coach [35]. Holistic nurse coaches adopt a counselee/patient-centered approach and play an active role in promoting self-management. They place the individual at the core of diabetes management, ensuring their active participation and respecting their preferences during the entire process. The present study revealed that the posttest total scores for the T2DM-DSMS were lower in the control group than in both the education and coaching groups, with notably large effect sizes (d = 1.544 and d = 3.483, respectively) (Table 2). These results indicate a statistically significant improvement in diabetes self-management among the participants in the HNC group compared to those in the education group. Diabetes education remains a fundamental part of helping individuals with diabetes effectively manage their condition [36]. However, emerging evidence also supports the effectiveness of coaching in sustaining glycemic control and promoting self-management in such individuals [20, 27, 30]. Consistent with the results of the present study, other research comparing education and coaching has also found improvements in self-management, with coaching having a greater overall impact [37]. Coaching thus appears to be a highly effective approach for improving diabetes self-management. It is easy to implement and also promotes individualized and patient-centered goal setting. In this way, it helps patients become more autonomous in managing their own care. It is thus a valuable addition to diabetes care strategies.
The present study found that both diabetes education and HNC contributed significantly to diabetes empowerment (Table 2). However, the mean scores and effect sizes for diabetes empowerment and its sub-dimensions were higher in the HNC group than in the education group. This suggests that, while both interventions are beneficial, HNC is more effective in promoting diabetes empowerment.
This finding is encouraging for individuals with diabetes, because it highlights the potential of HNC as a complementary strategy alongside traditional diabetes education. A previous study of weekly 30-minute coaching provided over a six-month period reported statistically significant improvements in both HbA1c levels and diabetes empowerment, with a 10% increase in empowerment scores [28]. In a study conducted by Young et al., individuals received nurse coaching for nine months, delivered via telephone or online face-to-face sessions according to the participant’s preference [38]. Individuals who had received coaching had significantly higher diabetes empowerment scores than those in the control group (p < 0.001) [38]. In light of these findings, our results suggest that the integration of HNC into standard diabetes education may be the final “missing piece” in the comprehensive management of diabetes. Providing HNC alongside nurse-led diabetes education could significantly enhance diabetes empowerment and offer a more personalized approach to patient care.
Developing self-management skills through a person-centered approach has been shown to positively influence HbA1c levels in individuals with diabetes [39, 40]. The present study revealed a statistically significant difference in HbA1c values among the education, control, and HNC groups (p < 0.05). It can be assumed that the HNC did not directly affect HbA1c levels. Rather, it exerted its influence indirectly by improving diabetes self-management and empowerment. This, in turn, contributed to better glycemic control. Previous research has also supported the effectiveness of coaching interventions in reducing HbA1c levels [41]. For instance, in one study of individuals with T2DM, six months of weekly 30-minute telephone sessions with trained peer coaches led to a reduction in HbA1c from 8.4 to 7.6% [28]. Similarly, Bollyky et al. found that individuals with T2DM who received three months of intensive lifestyle coaching had a statistically significant reduction in HbA1c when compared to those in the control group [42]. Pamungkas et al. reported that nurse-led diabetes coaching resulted in a significantly greater HbA1c reduction in the intervention group than in the control group [27]. Prior studies comparing the effects of coaching and diabetes education have also produced similar findings to those of the present research. In Cinar and Schou’s study, coaching resulted in a 7% decrease in HbA1c, while no significant change was observed in the education-only group [37]. The substantial reduction in HbA1c in the HNC group in our study can be attributed to several factors: the individualized nature of coaching sessions; the provision of support outside the scheduled sessions; regular goal-setting and follow-up; and a consistent focus on helping individuals accept and take ownership of their condition. Effective diabetes management requires both expert guidance and emotional support. HNC uniquely fulfills both needs, offering professional expertise and empathetic companionship throughout the process. Offering HNC as a follow-up to standard diabetes education will be valuable in improving glycemic control and supporting long-term diabetes management.
There was a positive, strong, and statistically significant correlation between the posttest T2DM-DSMS total scores and both the total and sub-dimension scores for the DES (Fig. 4). In a study conducted by Tejeda et al., correlation analysis revealed significant relationships between diabetes empowerment and various self-care domains: medication adherence (r = -0.17, p = 0.003); diabetes knowledge (r = 0.16, p = 0.007); diet (r = 0.24, p < 0.001); exercise (r = 0.25, p < 0.001); blood glucose monitoring (r = 0.12, p = 0.043); and foot care (r = 0.18, p = 0.002) [1]. These findings are supported by the literature. They suggest that diabetes empowerment and diabetes self-management are complementary and interrelated components of effective diabetes care.
Patient empowerment is a process which aims to facilitate positive behavioral changes. It has increasingly become an integral component of diabetes education worldwide. Empowerment enables individuals with diabetes to develop the knowledge and skills necessary to become better at self-management and to improve their quality of life. The DES reflects the strength and direction of the changes that occur, serving as an indicator of the effectiveness of the intervention made [31]. During coaching, a central objective is to help individuals unlock their potential and guide them from their current state (point A) to their desired goals (point B). The primary focus is on supporting behavioral change and uncovering the inner strength of the individual. For individuals with diabetes, recognizing this inner strength is often the first step toward transforming their lives. Helping such patients become aware of their own power is a core responsibility of their coaches. When individuals with diabetes are given help to harness their internal resources, their self-care and disease management are likely to significantly improve. The findings of this study demonstrate that HNC can lead to meaningful changes and behavioral improvements in individuals with diabetes. They also highlight the powerful role that HNC can play in the effective management of chronic disease.
Limitations of the study
This study has several limitations. First, the research was conducted in a single center, which may limit the generalizability of the findings to broader populations. Second, the duration of the study was relatively short, and the long-term effects of the intervention on glycemic control and behavioral outcomes remain unknown. Third, while randomization and blinding techniques were applied, there may still have been potential sources of bias, as well as other factors that could have influenced the outcomes, particularly changes in HbA1c levels. Additionally, the reliance on self-reported measures for self-management and empowerment may have been subject to response bias. Despite these limitations, the study provides valuable insights into the effectiveness of HNC as a supportive intervention for individuals with T2DM.
Conclusion
As a result of the study, the first hypothesis (H0), that “HNC has no significant effect on glycemic control, diabetes self-management, and diabetes empowerment in the patients who receive it, when compared to patients in the Diabetes Education and control groups”, can be rejected.
HNC is an extension of the traditional functions of nursing and a versatile method applicable across various healthcare setting. It is increasingly recognized in international research and clinical practice. Its rising popularity can be attributed to its practical nature, ease of implementation, emphasis on active patient participation, foundation in the nursing process, and evidence-based positive outcomes. HNC is a promising healthcare intervention that can complement and strengthen existing diabetes care services by enhancing glycemic control, supporting self-management, and fostering empowerment in individuals with diabetes. Nevertheless, it is important to acknowledge that the findings of this study are context-specific, as it was conducted at a single center with a specific patient population. Future research should thus include multicenter trials conducted across diverse settings and patient groups to assess the generalizability and scalability of HNC in different healthcare contexts. Furthermore, while HbA1c levels were assessed in all groups following the education and coaching sessions, follow-up measurements could not be performed after the intervention. It is thus recommended that future studies incorporate follow-up HbA1c measurements at three months post-intervention to provide a more accurate evaluation of the long-term impact on glycemic control.
Relevance for clinical practice
HNC presents a promising, applicable, and cost-effective approach to improving diabetes self-management, glycemic control, and patient empowerment. By utilizing individualized and patient-centered strategies, this method goes beyond the boundaries of traditional diabetes education. It can foster long-term behavioral change, strengthen treatment adherence, and improve the overall quality of care.
The findings of this study underscore the substantial impact of HNC in equipping individuals with T2DM with the knowledge, skills, and confidence required to manage their condition effectively. Importantly, the intervention is highly flexible, and can be easily implemented online. This makes it highly suitable for integration into various clinical settings, including primary care, outpatient clinics, and community-based diabetes programs. Given its grounding in the nursing process and its compatibility with existing healthcare systems, HNC can be seamlessly incorporated into routine diabetes care. Doing so may improve patient engagement, support individualized goal-setting, and optimize both short- and long-term clinical outcomes. As healthcare systems continue to seek innovative, person-centered solutions for chronic disease management, HNC offers a valuable and practical addition to nursing practice and diabetes care models.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to thank the type 2 diabetes persons who participated in the study.
Author contributions
Conception and design: TB, Bİ; Data acquisition and interpretation TB; Drafting of the manuscript or critical revision of the manuscript for important intellectual content: TB; Final approval of the version to be published: TB, Bİ; Agreement to be accountable for all aspects of the work: TB, Bİ. no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Funding
No funding was received for this research.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Approval to conduct the study was obtained from the Ethics Committee of Ankara Yıldırım Beyazıt University with the research code 2021-20 and the meeting date and decision number 16.02.2021-20. The necessary institutional permission was received from the state hospital where the study was conducted. The research was conducted in accordance with the principles of the Declaration of Helsinki.
Consent for publication
This study does not contain any identifiable personal data, images, or videos of individual participants. However, all the participants were informed about the study’s purpose, significance, and data collection process. They were assured that only the researchers would have access to the data collected. An informed consent form, which explicitly included consent for the publication of anonymized data, was signed by the participants. They were also informed of their right to withdraw from the study at any time.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hernandez-Tejada MA, Campbell JA, Walker RJ, Smalls BL, Davis KS, Egede LE. Diabetes empowerment, medication adherence and self-care behaviors in adults with type 2 diabetes. Diabetes Technol Ther. 2012;14(7):630–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Powers MA, Bardsley J, Cypress M, Duker P, Funnell MM, Hess Fischl A, et al. Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American diabetes association, the American association of diabetes educators, and the academy of nutrition and dietetics. Diabetes Care. 2015;38(7):1372–82. [DOI] [PubMed] [Google Scholar]
- 3.American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes. Diabetes care. 2021;44(1):5–33. [DOI] [PubMed]
- 4.Yu X, Chau JPC, Huo L, Li X, Wang D, Wu H, Zhang Y. The effects of a nurse-led integrative medicine-based structured education program on self-management behaviors among individuals with newly diagnosed type 2 diabetes: a randomized controlled trial. BMC Nurs. 2022;21(1):217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shiferaw WS, Akalu TY, Desta M, Kassie AM, Petrucka PM, Aynalem YA. Effect of educational interventions on knowledge of the disease and glycaemic control in patients with type 2 diabetes mellitus: a systematic review and meta-analysis of randomised controlled trials. BMJ Open. 2021;11(12):e049806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carvalho M, Morrissey E, Dunne P, Drury A, Byrne M, McSharry J. Understanding behaviour change maintenance after attending a self-management education and support programme for type 2 diabetes: A longitudinal qualitative study. Diabet Med. 2025;42(6):e70032. [DOI] [PMC free article] [PubMed]
- 7.Chatterjee S, Davies MJ, Heller S, Speight J, Snoek FJ, Khunti K. Diabetes structured self-management education programmes: a narrative review and current innovations [published correction appears in lancet. Diabetes Endocrinol. 2018;6(2):130–42. [DOI] [PubMed] [Google Scholar]
- 8.Hermanns N, Ehrmann D, Finke-Groene K, Kulzer B. Trends in diabetes self-management education: where are we coming from and where are we going? A narrative review. Diabet Med. 2020;37(3):436–47. [DOI] [PubMed] [Google Scholar]
- 9.American Diabetes Association. 4. Comprehensive Medical Evaluation and Assessment of Comorbidities: Standards of Medical Care in Diabetes. Diabetes care. 2021; 44(1):53–72. [DOI] [PubMed]
- 10.Lanese BS, Dey A, Srivastava P, Figler R. Introducing the health coach at a primary care practice: impact on quality and cost. Hosp Top. 2011;89(1):16–22. [DOI] [PubMed] [Google Scholar]
- 11.Erickson HL, Erickson ME, Southard ME, Brekke ME, Sandor MK. Natschke MA proactive innovation for health care transformation: health and wellness nurse coaching. J Holist Nurs. 2016;34(1):44–55. [DOI] [PubMed] [Google Scholar]
- 12.Southard M, Dossey BM, Bark L, Schaub BG. Professional Nurse Coaching. In: The art and science of nurse coaching: The providers’ guide to coaching scope and competencies. 2nd ed. Maryland, Silver spring, American Nurses Association. 2021:7–22.
- 13.Schaub B, Luck S, Dossey B. Integrative nurse coaching for health and wellness. Altern Complement Ther. 2012;18(1):14–20. [Google Scholar]
- 14.Jiang Y, Shorey S, Seah B, Chan W, Tam W, Wang W. The effectiveness of psychological interventions on self-care, psychological and health outcomes in patients with chronic heart failure: A systematic review and meta-analysis. Int J Nurs Stud. 2018;78:16–25. [DOI] [PubMed] [Google Scholar]
- 15.Morales F, Hernandez A, Morales-Asencio J, Canca-Sanchez J, Moreno-Martin G. Group for management hospital Costa Del Sol members. Impact on quality of life of a nursing intervention programme for patients with chronic non-cancer pain: an open, randomized controlled parallel study protocol. J Adv Nurs. 2016;72(5):1182–90. [DOI] [PubMed] [Google Scholar]
- 16.Delaney C, Bark L. The experience of holistic nurse coaching for patients with chronic conditions. J Holist Nurs. 2019;37(3):225–37. [DOI] [PubMed] [Google Scholar]
- 17.Delaney C, Barrere C, Bark L. A metaphor analysis of patients’ with chronic conditions experiences with holistic nurse coaching. Holist Nurs Pract. 2020;34(1):24–34. [DOI] [PubMed] [Google Scholar]
- 18.American Diabetes Association Professional Practice Committee. 5. Facilitating behavior change and well-being to improve health outcomes: Standards of Medical Care in Diabetes—2022. Diabetes care. 2022;45(1):60–82. [DOI] [PubMed]
- 19.Sherifali D, Viscardi V, Bai JW, Ali RM. Evaluating the effect of a diabetes health coach in individuals with type 2 diabetes can. J Diabetes. 2016;40(1):84–94. [DOI] [PubMed] [Google Scholar]
- 20.Pirbaglou M, Katz J, Motamed M, Pludwinski S, Walker K, Ritvo P. Personal health coaching as a type 2 diabetes mellitus self-management strategy: a systematic review and meta-analysis of randomized controlled trials. Am J Health Promot. 2018;32(7):1613–26. [DOI] [PubMed] [Google Scholar]
- 21.O’Reilly DJ, Blackhouse G, Bowen JM, Brozic A, Agema P, Punthakee Z, et al. Economic analysis of a diabetes health coaching intervention for adults living with type 2 diabetes: A Single-Centre evaluation from a communitybased randomized controlled trial. Can J Diabetes. 2022;46(2):165–70. [DOI] [PubMed] [Google Scholar]
- 22.Sherifali D, Brozic A, Agema P, Gerstein HC, Punthakee Z. The diabetes health coaching randomized controlled trial: Rationale, design and baseline characteristics of adults living with type 2 diabetes. Can J Diabetes. 201;43(7):477– 82. [DOI] [PubMed]
- 23.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–69. [DOI] [PubMed] [Google Scholar]
- 24.Whitworth L, House KK, House HK, Sandahl P, Whitworth L, House KK, House HK, Sandahl P, İstanbul. Mediacat Yayınevi. 2020:169–275.
- 25.Teeter BS, Westrick SC. Marketing applications. In: Zgarrick DP, Alston GL, Moczygemba LR, Desselle SP, editors, Pharmacy Management: Essentials for All Practice Settings, McGraw Hill 2016.
- 26.Pamungkas RA, Chamroonsawasdi K. Self-management based coaching program to improve diabetes mellitus self-management practice and metabolic markers among uncontrolled type 2 diabetes mellitus in Indonesia: A quasiexperimental study. Diabetes Metabolic Syndrome: Clin Res Reviews. 2020;14(1):53–61. [DOI] [PubMed] [Google Scholar]
- 27.Pamungkas RA, Usman AM, Chamroonsawasdi K. A smartphone application of diabetes coaching intervention to prevent the onset of complications and to improve diabetes self-management: A randomized control trial. Diabetes Metabolic Syndrome: Clin Res Reviews. 2022;16(7):102537. [DOI] [PubMed] [Google Scholar]
- 28.McGowan P, Lynch S, Hensen F. The role and effectiveness of telephone peer coaching for adult patients with type 2 diabetes. Can J Diabetes. 2019;43(6):399–405. [DOI] [PubMed] [Google Scholar]
- 29.Lin CL, Huang LC, Chang YT, Chen RY, Yang SH. Effectiveness of health coaching in diabetes control and lifestyle improvement: a randomized-controlled trial. Nutrients. 2021;13(11):3878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Koç E, Özkan Ö. Evaluation of Disease Self-Management in Persons Diagnosed with Type 2 Diabetes and Development of the Type 2 Diabetes Self-Management Scale, Faculty of Medicine, Department of Public Health, Specialization Thesis, Ankara: Gazi University, 2020.
- 31.Anderson RM, Funnell MM, Fitzgerald JT, Marrero DG. The diabetes empowerment scale: a measure of psychosocial self-efficacy. Diabetes Care. 2000;23(6):739–43. [DOI] [PubMed] [Google Scholar]
- 32.Özcan H, Korkmaz M, Diabetes Empowerment Scale Reliability Analysis Of Validity For The Turkish Society. Institute of Health Sciences, Department of Internal Medicine Nursing, Master Thesis, Isparta: Süleyman Demirel University, 2012.
- 33.Team RC. A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/. 10 Temmuz 2022.
- 34.Rosseel Y, Lavaan. An R package for structural equation modeling and more. Version 0.5–12 (BETA). J Stat Softw. 2012;48(2):1–36. [Google Scholar]
- 35.American Diabetes Association. Good to know: information from the American diabetes association for people with diabetes. Clin Diabetes. 2017;35(5):353–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Steinsbekk A, Rygg LO, Lisulo M, Rise MB, Fretheim A. Group based diabetes self-management education compared to routine treatment for people with type 2 diabetes mellitus. A systematic review with meta-analysis. BMC Health Serv Res. 2012;12(1):1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cinar AB, Schou L. The role of self-efficacy in health coaching and health education for patients with type 2 diabetes. Int Dent J. 2014;64(3):155–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Young H, Miyamoto S, Ward D, Dharmar M, Tang-Feldman Y, Berglund L. Sustained effects of a nurse coaching intervention via telehealth to improve health behavior change in diabetes. Telemed J E Health. 2014;20(9):828–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Greenwood DA, Young HM, Quinn CC. Telehealth remote monitoring systematic review: structured self-monitoring of blood glucose and impact on A1C. J Diabetes Sci Technol. 2014;8(2):378–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Thomas D, Elliott EJ, Naughton GA. Exercise for type 2 diabetes mellitus. Cochrane Database Syst Rev. 2006;(3):1–42. [DOI] [PMC free article] [PubMed]
- 41.Killebrew E, Huelsman M, Bonareri V, Furfaro T. Utilizing a personal health coach in the management of T2DM. School of nursing. Doctor Nurs Pract Projects. 2022;215.
- 42.Bollyky JB, Bravata D, Yang J, Williamson M, Schneider J. Remote lifestyle coaching plus a connected glucose meter with certified diabetes educator support improves glucose and weight loss for people with type 2 diabetes. J Diabetes Res. 2018;1–7. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.