Abstract
Objectives
To examine whether self reported health status and use of health services varies in children of different social class and ethnic group.
Design
Cross sectional study from the 1999 health survey for England.
Subjects
6648 children and young adults aged 2-20 years.
Setting
Private households in England.
Main outcome measures
Proportion of children (or their parents) reporting episodes of acute illness in the preceding fortnight and prevalence of self reported longstanding illness. Proportion reporting specific illnesses. Proportion reporting that they had consulted a general practitioner in the preceding fortnight, attended hospital outpatient departments in the three preceding months, or been admitted to hospital in the preceding year.
Results
Large socioeconomic differences were observed between ethnic subgroups; a higher proportion of Afro-Caribbean, Indian, Pakistani, and Bangladeshi children belonged to lower social classes than the general population. The proportion of children and young adults reporting acute illnesses in the preceding two weeks was lower in Bangladeshi and Chinese subgroups (odds ratio 0.41, 95% confidence interval 0.27 to 0.61 and 0.46, 0.28 to 0.77, respectively) than in the general population. Longstanding illnesses was less common in Bangladeshi and Pakistani children (0.52, 0.40 to 0.67 and 0.57, 0.46 to 0.70) than in the general population. Irish and Afro-Caribbean children reported the highest prevalence of asthma (19.5% and 17.7%) and Bangladeshi children the lowest (8.2%). A higher proportion of Afro-Caribbean children reported major injuiries than the general population (11.0% v 10.0%), and children from all Asian subgroups reported fewer major and minor injuries than the general population. Indian and Pakistani children were more likely to have consulted their general practitioner in the preceding fortnight than the general population (1.86, 1.35 to 2.57 and 1.51, 1.13 to 2.01, respectively). Indian, Pakistani, Bangladeshi, and Chinese children were less likely to have attended outpatient departments in the preceding three months. No significant differences were found between ethnic groups in the admission of inpatients to hospitals. Acute and chronic illness were the best predictors of children's use of health services. Social classes did not differ in self reported prevalence of treated infections, major injuries, or minor injuries, and no socioeconomic differences were seen in the use of primary and secondary healthcare services.
Conclusions
Children's use of health services reflected health status rather than ethnic group or socioeconomic status, implying that equity of access has been partly achieved, although reasons why children from ethnic minority groups are able to access primary care but receive less secondary care need to be investigated.
What is already known on this topic
Children from lower socioeconomic classes and from Indian ethnic subgroups may make more use of general practitioners' services than other children
Afro-Caribbean, Indian, Pakistani, and Bangladeshi children are less likely to be referred to outpatient and inpatient services at hospitals than white children
What this study adds
Indian, Pakistani, and Bangladeshi children reported less acute and chronic illness, asthma, and injuries than the general population, whereas Afro-Caribbean children reported more
Children's self reported health status and use of health services did not vary by social class
Indian and Pakistani children make more use of general practitioners' services, but Indian, Pakistani, Bangladeshi, and Chinese children are less likely to be referred to outpatient clinics
Self reported health status rather than socioeconomic status or ethnicity is the best predictor of use of primary and secondary services
Introduction
After the Acheson report into inequalities in health was published, the government of the United Kingdom declared the eradication of child poverty a national goal and called for detailed research to monitor the impact that such inequalities have on children's health.1 In the 1970s and 1980s, differentials in childhood mortality widened, such that death rates in children from social classes IV and V were up to five times higher than in children from social classes I and II.2,3 Morbidity is far harder to assess, mainly because most sources of data lack information on denominators.4 Some data are available on use of services, but real measures of health status are often lacking.5 Children account for a large proportion of the workload of general practitioners, and according to some reports doctors perceive that certain ethnic subgroups—for example, patients of Asian origin—add to their workload and use health services inappropriately.6,7 Socioeconomic data and especially data on self defined ethnicity are rarely available in large surveys.8,9 Socioeconomic differences exist in consultation rates in general practice for common childhood illnesses such as asthma and respiratory disease, infections, and injuries.10 We examined in a national study whether inequalities in health status and use of services exist in children and young adults, using information on socioeconomic status, health status, and use of health services collected at an individual level.
Methods
The health survey for England is an annual survey of households in England. The 1999 survey focused on the health of ethnic minority groups.11
Sampling and data collection
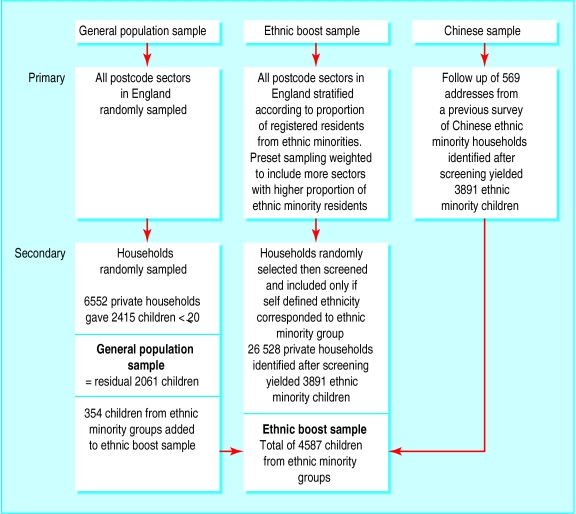
We used three separate samples (see figure). Firstly, a general population sample of 6552 households was obtained by using two stage random sampling of postcode sectors and then addresses in each sector. All participating households were interviewed in full. Secondly, an “ethnic boost” sample of 26 528 addresses was obtained by using stratified multistage probability sampling. Additional postcode sectors were systematically selected as primary sampling units to include a greater proportion of households from areas with a high percentage of ethnic minority groups. Each household in the ethnic boost sample was screened initially and included only if respondents identified themselves as belonging to an ethnic minority group. Individuals selected the most appropriate ethnic group from the categories “white,” “black Caribbean,” “black African,” “black other,” “Indian,” “Pakistani,” “Bangladeshi,” “Chinese,” and “other.” Interviewers who could speak and read the informants' language obtained household, socioeconomic, and personal information and information on health and use of health services. Parents or guardians responded for children aged less than 13. Children aged 13-15 were interviewed directly, with a parent present in the household. Thirdly, a sample for Chinese informants was obtained by following up 569 households that had participated in an earlier survey conducted by the health education authority.
Data analysis
We merged individual data from the ethnic boost and Chinese samples with data from the general population sample. We recategorised ethnic groups as “Afro-Caribbean,” “Indian,” “Pakistani,” “Bangladeshi,” “Chinese,” and “Irish,” and grouped all other ethnic groups together in a baseline group called “general population.”11 For this report, we use the term “Asian” to report collective findings on Indian, Pakistani, Bangladeshi, and Chinese groups.
We examined the prevalence of acute illnesses in the preceding fortnight, limiting longstanding illnesses, and specific illnesses in children and young adults of different ethnic groups and social class. In estimating the prevalence of asthma, we included children reporting an episode of wheeze treated in the preceding year. The category “treated infections” included all children who were taking prescribed medicines for infections. Major incidents were defined as any kind of injury in the preceding six months that resulted in seeing a doctor or going to hospital for treatment. Minor incidents included any injuries in the preceding four weeks that resulted in pain or discomfort lasting 24 hours or more but did not require seeing a doctor or going to hospital. We examined variations in the use of health services, such as consultations with a general practitioner in the fortnight preceding the interview, attendance at hospital as an outpatient in the preceding three months, and inpatient and day patient admissions in the preceding year. We analysed the data with Stata version 7, weighted according to sampling probability. We used logistic regression modelling to calculate odds ratios for univariate and multivariate analysis.
Results
Household response rates were 76% in the general population and 71% in the ethnic boost sample. We obtained interviews with 97% of children from the general population and 92-96% of children from ethnic minority groups. In all, 6648 people aged 2-20 years participated in the survey. Age and sex distributions of the different ethnic and social class groups were similar, but socioeconomic differences between the different ethnic groups were large (tables 1 and 2. Thirty three per cent (377/974) of Bangladeshi children and 26% (171/688) of Indian children belonged to social classes IV and V compared with 19% (395/2061) of children from the general population.
Table 1.
Distribution of sample used in cross sectional survey of socioeconomic and ethnic group differences in self reported health status and use of health services by children and young people in England by age, sex, ethnic group, and social class
| Characteristic
|
No
|
%
|
|---|---|---|
| Age (years): | ||
| 2-5 | 1630 | 24.5 |
| 6-10 | 1889 | 28.4 |
| 11-15 | 1738 | 26.1 |
| 16-20 | 1391 | 20.9 |
| Sex: | ||
| Male | 3358 | 50.5 |
| Female | 3290 | 49.5 |
| Ethnic group: | ||
| General population | 2061 | 31.0 |
| Afro-Caribbean | 807 | 12.1 |
| Indian | 668 | 10.1 |
| Pakistani | 1060 | 15.9 |
| Bangladeshi | 974 | 14.7 |
| Chinese | 342 | 5.1 |
| Irish | 736 | 11.1 |
| Social class of the head of household: | ||
| I | 356 | 5.4 |
| II | 1406 | 21.2 |
| III non-manual | 783 | 11.8 |
| III manual | 2008 | 30.2 |
| IV | 1373 | 20.7 |
| V | 214 | 3.2 |
| All other | 500 | 7.5 |
Percentages may not add to 100 owing to rounding.
Table 2.
Socioeconomic factors in children and teenagers by ethnic group. Data are numbers (percentages) unless otherwise indicated
| General population (n=2061)
|
Afro-Caribbean (n=807)
|
Indian (n=668)
|
Pakistani (n=1060)
|
Bangladeshi (n=974)
|
Chinese (n=342)
|
Irish (n=736)
|
P value (χ2 test for significance testing of differences across groups)
|
|
|---|---|---|---|---|---|---|---|---|
| Social class | ||||||||
| I | 148 (7.4) | 21 (2.7) | 64 (8.0) | 47 (4.8) | 11 (2.1) | 29 (9.0) | 36 (6.8) | <0.001 |
| II | 558 (26.3) | 156 (18.9) | 159 (20.0) | 134 (13.0) | 57 (7.1) | 99 (27.5) | 243 (31.7) | |
| III non-manual | 264 (12.9) | 183 (21.9) | 62 (10.2) | 72 (6.4) | 59 (6.5) | 49 (15.6) | 94 (14.6) | |
| III manual | 626 (30.5) | 176 (22.4) | 184 (30.1) | 405 (40.0) | 305 (35.2) | 102 (30.9) | 210 (29.1) | |
| IV | 316 (15.6) | 182 (23.6) | 157 (25.8) | 237 (20.8) | 339 (30.4) | 26 (7.2) | 116 (13.8) | |
| V | 79 (4.0) | 30 (4.1) | 14 (2.3) | 24 (2.3) | 38 (3.2) | 10 (2.9) | 19 (1.7) | |
| All other* | 70 (3.4) | 60 (7.4) | 28 (4.2) | 141 (13.3) | 165 (16.9) | 27 (7.9) | 18 (2.4) | |
| Living in lowest third of equivalised income | 658 (32.9) | 428 (52.0) | 244 (42.0) | 646 (60.0) | 678 (68.8) | 130 (34.8) | 213 (26.6) | <0.001 |
| No (%) of sample receiving income support | 271 (13.6) | 267 (31.7) | 86 (14.2) | 249 (24.0) | 368 (36.7) | 22 (4.5) | 117 (14.8) | <0.001 |
Includes children of parents in armed forces, full time students, and other.
Health status
Acute illness in children and young adults in the preceding two weeks was more common in Irish children than in the general population (odds ratio 1.45, 95% confidence interval 1.10 to 1.98) (table 3). Bangladeshi and Chinese subgroups had the lowest prevalence (0.41, 0.27 to 0.61 and 0.46, 0.28 to 0.77, respectively). Chronic or limiting longstanding illnesses were less common in Bangladeshi and Pakistani children than in the general population (0.52, 0.40 to 0.67 and 0.57, 0.46 to 0.70, respectively) (table 4). The prevalence of acute or longstanding illness in children from different social classes did not differ. The prevalence of asthma treated in the preceding 12 months was highest in social class groups II and III non-manual (17.7% and 18.9%). Social class did not differ for prevalence of treated infections or injuries. Irish and Afro-Caribbean children had the highest prevalence of asthma (19.5% and 17.7%) and Bangladeshi children the lowest (8.2%). Bangladeshi children had fewer major incidents than the general population (3.1% v 10.0%) and fewer minor incidents (0.6% v 7.3%).
Table 3.
Illness status in children and teenagers by ethnic group and social class
| Characteristic
|
Acute illness
|
Chronic illness
|
|||
|---|---|---|---|---|---|
| No (%) | Crude odds ratio*(95% CI) | No (%) | Crude odds ratio*(95% CI) | ||
| Ethnic group: | |||||
| General population | 209 (10.0) | 1.00 | 483 (23.3) | 1.00 | |
| Afro-Caribbean | 89 (11.5) | 1.17 (0.89 to 1.54) | 204 (25.9) | 1.15 (0.94 to 1.40) | |
| Indian | 50 (7.9) | 0.78 (0.55 to 1.09) | 109 (16.4) | 0.64 (0.50 to 8.30) | |
| Pakistani | 83 (8.0) | 0.79 (0.60 to 1.04) | 161 (14.8) | 0.57 (0.46 to 0.70) | |
| Bangladeshi | 45 (4.3) | 0.41 (0.27 to 0.61) | 127 (13.6) | 0.52 (0.40 to 0.67) | |
| Chinese | 19 (4.9) | 0.46 (0.28 to 0.77) | 65 (17.6) | 0.70 (0.52 to 0.95) | |
| Irish | 182 (27.3) | 1.45 (1.10 to 1.98) | 182 (27.3) | 1.24 (0.98 to 1.56) | |
| Social class of head of household: | |||||
| I | 24 (7.8) | 1.00 | 67 (21.9) | 1.00 | |
| II | 145 (10.9) | 1.44 (0.79 to 2.63) | 312 (23.5) | 1.09 (0.73 to 1.64) | |
| III non-manual | 78 (10.3) | 1.36 (0.70 to 2.62) | 151 (20.5) | 0.92 (0.58 to 1.45) | |
| III manual | 180 (10.2) | 1.35 (0.74 to 2.46) | 397 (24.0) | 1.12 (0.75 to 1.68) | |
| IV | 110 (9.2) | 1.19 (0.63 to 2.26) | 261 (24.3) | 1.15 (0.75 to 1.76) | |
| V | 20 (12.8) | 1.73 (0.75 to 4.02) | 43 (20.9) | 0.94 (0.50 to 1.79) | |
Adjusting for independent variables including age, sex, ethnic group, or social class did not alter odds ratios, so only unadjusted values are shown.
Table 4.
Numbers (percentages) of children and teenagers with specific diagnoses: asthma, infections, and accidents by social class and ethnicity
| Treated asthma
|
Treated infections
|
Major incident requiring hospital or doctor treatment in past 6 months
|
Minor incidents in past 4 weeks
|
|
|---|---|---|---|---|
| Social class: | ||||
| I | 24 (13.0) | 9 (12.9) | 35 (11.6) | 18 (6.6) |
| II | 127 (17.7) | 25 (20.3) | 113 (9.2) | 79 (6.7) |
| III non-manual | 81 (18.9) | 10 (11.6) | 82 (12.9) | 42 (5.1) |
| III manual | 118 (10.5) | 29 (11.4) | 134 (8.7) | 102 (7.8) |
| IV | 105 (12.7) | 13 (9.9) | 104 (10.3) | 59 (7.2) |
| V | 16 (14.4) | 4 (16.3) | 16 (7.1) | 12 (9.5) |
| P value (χ2)* | <0.001 | 0.34 | 0.79 | 0.61 |
| Ethnic group: | ||||
| General population | † | † | 208 (10.0) | 151 (7.3) |
| Afro-Caribbean | 115 (17.7) | 19 (14.3) | 88 (11.0) | 52 (6.2) |
| Indian | 73 (13.9) | 14 (19.4) | 50 (8.8) | 31 (4.7) |
| Pakistani | 98 (11.8) | 23 (21.2) | 53 (5.1) | 22 (1.9) |
| Bangladeshi | 63 (8.2) | 18 (20.1) | 30 (3.1) | 8 (0.6) |
| Chinese | 36 (13.6) | 7 (16.7) | 14 (4.2) | 15 (4.2) |
| Irish | 128 (19.5) | 12 (10.7) | 65 (9.2) | 48 (6.3) |
| P value (χ2)* | <0.001 | 0.13 | 0.004 | 0.003 |
χ2 test for significance testing of differences across groups.
Data for treated asthma and infections available for ethnic boost sample only.
Use of health services
The proportion of all children and young adults aged up to 20 years consulting their general practitioner in the preceding fortnight was 8.7% (equivalent to 2.3 consultations per person per year) (table 5). Girls were less likely to have attended outpatient clinics at hospital than boys (odds ratio 0.78, 0.66 to 0.93) (table 6). The associations between socioeconomic status and use of health services were non-significant. After adjusting for age, social class, and chronic health status, Indian and Pakistani children were more likely to have seen their general practitioner in the preceding fortnight than the general population (odds ratio for Indian children 1.86, 1.13 to 2.01). Asian children were, however, less likely to have attended outpatient departments in the preceding three months. The differences between in hospital inpatient admissions were non-significant. Children who had episodes of acute illness in the preceding two weeks were more likely to have seen their general practitioner (7.57, 5.52 to 10.38) and to have attended outpatient departments in the past three months (1.60, 1.23 to 2.08). Children who had chronic or limiting longstanding illnesses were more likely to have seen their general practitioner in the preceding fortnight (1.78, 1.28 to 2.48) and more than twice as likely have attended hospital as an outpatient or inpatient in the preceding year, (2.86, 2.34 to 3.50 and 2.49, 1.84 to 3.38, respectively) than children who did not have such illnesses.
Table 5.
Children and teenagers using general practitioner, outpatient, and inpatient services by social class and ethnic group. Data are numbers (percentages) unless otherwise indicated
| Visits to general practitioner in past 2 weeks
|
Hospital outpatient in past 3 months
|
Hospital inpatient or day patient in past year
|
|
|---|---|---|---|
| Social class: | |||
| I | 38 (9.6) | 76 (21.1) | 26 (7.9) |
| II | 127 (6.9) | 313 (25.6) | 81 (6.3) |
| III non-manual | 60 (6.2) | 213 (29.4) | 55 (5.7) |
| III manual | 173 (8.3) | 419 (25.9) | 152 (8.5) |
| IV | 121 (7.4) | 281 (29.8) | 101 (8.9) |
| V | 20 (10.0) | 44 (19.7) | 17 (11.3) |
| P value (χ2)* | 0.59 | 0.30 | 0.32 |
| Ethnic group: | |||
| General population | 155 (7.5) | 548 (26.3) | 162 (7.8) |
| Afro-Caribbean | 73 (8.5) | 207 (26.8) | 70 (9.2) |
| Indian | 80 (12.6) | 122 (19.0) | 34 (5.4) |
| Pakistani | 118 (11.1) | 155 (15.4) | 71 (6.8) |
| Bangladeshi | 71 (7.3) | 126 (14.5) | 53 (5.7) |
| Chinese | 25 (8.0) | 49 (14.3) | 17 (4.8) |
| Irish | 59 (7.9) | 206 (30.0) | 68 (9.4) |
| P value (χ2)* | 0.03 | <0.001 | 0.001 |
χ2 test for significance testing of differences across groups.
Table 6.
Use of health services by children and teenagers. Values are odds ratios (95% confidence intervals)
| Variable
|
GP visits in past 2 weeks
|
Hospital outpatient in past 3 months
|
Hospital inpatient or day patient in past year | |||||
|---|---|---|---|---|---|---|---|---|
| Crude
|
Adjusted*
|
Crude
|
Adjusted*
|
Crude | Adjusted* | |||
| Age | 0.90 (0.88 to 0.93) | 0.90 (0.88 to 0.93) | 1.00 (0.99 to 1.02) | 1.00 (0.98 to 1.02) | 1.01 (0.98 to 1.04) | 1.01 (0.98 to 1.04) | ||
| Sex: | ||||||||
| Male† | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||
| Female | 0.82 (0.62 to 1.09) | 0.85 (0.63 to 1.14) | 0.78 (0.66 to 0.93) | 0.79 (0.66 to 0.95) | 0.81 (0.61 to 1.08) | 0.80 (0.59 to 1.08) | ||
| Social class: | ||||||||
| I† | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||
| II | 0.70 (0.40 to 1.22) | 0.70 (0.40 to 1.23) | 1.29 (0.87 to 1.90) | 1.28 (0.86 to 1.90) | 0.77 (0.42 to 1.42) | 0.75 (0.41 to 1.39) | ||
| IIIn | 0.62 (0.33 to 1.19) | 0.64 (0.33 to 1.24) | 1.56 (1.02 to 2.38) | 1.64 (1.07 to 2.52) | 0.70 (0.35 to 1.39) | 0.70 (0.35 to 1.41) | ||
| IIIm | 0.84 (0.49 to 1.46) | 0.87 (0.50 to 1.52) | 1.31 (0.89 to 1.92) | 1.30 (0.88 to 1.93) | 1.08 (0.60 to 1.93) | 1.05 (0.58 to 1.89) | ||
| IV | 0.75 (0.41 to 1.35) | 0.78 (0.43 to 1.42) | 1.59 (1.05 to 2.39) | 1.59 (1.04 to 2.42) | 1.14 (0.61 to 2.13) | 1.10 (0.58 to 2.07) | ||
| V | 1.04 (0.44 to 2.45) | 1.07 (0.45 to 2.59) | 0.92 (0.50 to 1.69) | 0.94 (0.51 to 1.73) | 1.48 (0.65 to 3.38) | 1.52 (0.67 to 3.43) | ||
| Ethnicity: | ||||||||
| General population† | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||
| Afro-Caribbean | 1.15 (0.84 to 1.56) | 1.09 (0.78 to 1.52) | 1.02 (0.84 to 1.24) | 0.98 (0.79 to 1.22) | 1.20 (0.88 to 1.63) | 1.19 (0.85 to 1.66) | ||
| Indian | 1.77 (1.31 to 2.39) | 1.86 (1.35 to 2.57) | 0.66 (0.52 to 0.84) | 0.67 (0.52 to 0.86) | 0.68 (0.45 to 1.02) | 0.72 (0.47 to 1.09) | ||
| Pakistani | 1.53 (1.18 to 1.99) | 1.51 (1.13 to 2.01) | 0.51 (0.41 to 0.63) | 0.56 (0.45 to 0.70) | 0.86 (0.64 to 1.17) | 0.86 (0.61 to 1.21) | ||
| Bangladeshi | 0.97 (0.68 to 1.37) | 1.07 (0.73 to 1.57) | 0.48 (0.37 to 0.61) | 0.55 (0.41 to 0.73) | 0.72 (0.50 to 1.04) | 0.79 (0.53 to 1.20) | ||
| Chinese | 1.11 (0.70 to 1.77) | 1.19 (0.73 to 1.95) | 0.47 (0.34 to 0.66) | 0.49 (0.34 to 0.70) | 0.60 (0.35 to 1.03) | 0.58 (0.31 to 1.06) | ||
| Irish | 1.06 (0.73 to 1.54) | 1.02 (0.69 to 1.49) | 1.20 (0.96 to 1.50) | 1.14 (0.90 to 1.44) | 1.22 (0.87 to 1.71) | 1.29 (0.91 to 1.82) | ||
| Acute illness: | ||||||||
| None† | 1.00 | 1.00 | 1.00 | |||||
| In past 2 weeks | 7.57 (5.52 to 10.38) | 1.60 (1.23 to 2.08) | 1.48 (0.99 to 2.22) | |||||
| Chronic illness: | ||||||||
| None† | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||
| Limiting longstanding illness | 1.67 (1.23 to 2.28) | 1.78 (1.28 to 2.48) | 2.91 (2.39 to .53) | 2.86 (2.34 to 3.50) | 2.50 (1.87 to 3.36) | 2.49 (1.84 to 3.38) | ||
Adjusted for age, sex, social class, chronic health status, and ethnic group
Baseline group for univariate and multivariate comparisons of odds ratios by using logistic regression.
Discussion
Asian subgroups reported less ill health than the general population. Indian and Pakistani children made more use of general practitioners' services, but children from all ethnic minority groups were less likely to be referred to outpatient clinics. Self reported health status rather than socioeconomic status or ethnicity was the best predictor of use of primary and secondary care services.
Use of health services does not accurately reflect health status yet is often used to negotiate service needs on an area basis. Our study reports national data on the prevalence of both acute and chronic illness and on use of services among children and young adults from different ethnic and socioeconomic groups. We found lower overall mean consulting rates than reported in our earlier study (2.3 v 3.8 consultations per person per year).10 The earlier study was, however, limited to children aged under 16, and since use of general practitioners' services is lower among young adults this may account for some of the difference. Our study relates only to children living in private households and cannot be generalised to the health of children in institutions or homeless children, but this should not affect the validity of our findings.
Limitations of self reported health
The recording of socioeconomic status and ethnicity even when self completed categories are used is subject to misclassification bias.9 Our conclusions relate to health status and use of health services reported by parents on behalf of children under 13 years, and for older children and young adults to self rated health and use of services. To date no evidence exists that parents of children from different ethnic minority groups report different levels of subjective health, but this is a potentially important limitation of the study. The reporting of health depends on whether patients choose to consult their general practitioner and is based on their own decisions. Nevertheless, how self rated health status compares with more objective measures needs to be assessed in children from different ethnic groups and of different socioeconomic status.
Socioeconomic and ethnic group differentials in health of children
Interpreting findings relating to health inequalities is beset by confounding because lifestyle factors that predispose to ill health vary between socioeconomic groups.12,13 The prevalence of certain illnesses varies in different socioeconomic or ethnic groups, and differentials exist in service use and provision.14 For example, the lower prevalence of asthma in Bangladeshi children may not mean that actual prevalence is lower but that it is underdiagnosed.
Our findings of a lack of socioeconomic differentials are interesting. The categories of social class currently in use are gradually to be replaced by alternative instruments for assessing socioeconomic inequalities.15 It would be easy to dismiss our findings as not being real since a body of evidence suggests that inequalities are a consistent finding in all aspects of adult health.16,17 Another study examining data from the general household survey found no socioeconomic differences in the use of general practitioners' and hospital services and showed that after a period of increasing health differentials in the 1980s such inequality levelled.18 This finding is supported by our finding that health status rather than socioeconomic status or ethnic group predicts service use. Using general practitioners' services more does not necessarily imply worse health. The highest users of general practitioners' services were Asian ethnic subgroups, who reported fewer illnesses and fewest injuries. Non-illness related reasons for children consulting their general practitioner include child health surveillance and preventive care such as immunisation. Some groups may be using services more appropriately—for example, seeing their general practitioner for initial assessment rather than going direct to hospital. Nevertheless, for some children and young adults, poor socioeconomic circumstances and belonging to certain ethnic groups—for example, Afro-Caribbean—may place them doubly at risk of ill health and poorer quality of care.13 Whether general practitioners are less likely to refer children from ethnic minority groups also needs to be investigated.
Conclusions
Children's health status and use of health services did not vary significantly by social class, which implies that equity in this area has been partially achieved. Children from Asian ethnic groups report better health and Afro-Caribbean children report worse health than the general population. Although these groups were more likely to consult general practitioners, they were less likely to be referred to secondary care.
Figure.
Sampling method for 1999 health survey for England with focus on ethnic minorities. Target population: all private householders in England
Acknowledgments
We thank Rumana Omar and Richard Boreham for their statistical advice on this paper.
Footnotes
Funding: The Health Survey for England was funded by the Department of Health. JE receives some of his funding from the special trustees of University College London Hospitals NHS Trust. AM holds a primary care scientist award and is funded by the NHS Research and Development Directorate.
Competing interests: None declared.
References
- 1.Acheson D. The report of the independent inquiry into inequalities in health. London: Stationery Office; 1998. [Google Scholar]
- 2.Roberts I, Power C. Does the decline in child injury mortality vary by social class? A comparison of class specific mortality in 1981 and 1991. BMJ. 1996;313:784–786. doi: 10.1136/bmj.313.7060.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harding S, Rosato M, Brown J, Smith J. Social patterning of health and mortality: children, aged 6-15 years, followed up for 25 years in the ONS longitudinal study. Health Stat Q. 1999;8:30–34. [Google Scholar]
- 4.Kemp A, Sibert J. Childhood accidents: epidemiology, trends, and prevention. J Accid Emerg Med. 1997;14:316–320. doi: 10.1136/emj.14.5.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Staples B, Pharoah PO. Child health statistical review. Arch Dis Child. 1994;71:548–554. doi: 10.1136/adc.71.6.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ahmad WI, Baker MR, Kernohan EE. General practitioners' perceptions of Asian and non-Asian patients. Fam Pract. 1991;8:52–56. doi: 10.1093/fampra/8.1.52. [DOI] [PubMed] [Google Scholar]
- 7.Balarajan R, Yuen P, Soni Raleigh V. Ethnic differences in general practitioner consultations. BMJ. 1989;299:958–960. doi: 10.1136/bmj.299.6705.958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bhopal R, Donaldson L. White, European, Western, Caucasian, or what? Inappropriate labeling in research on race, ethnicity, and health. Am J Public Health. 1998;88:1303–1307. doi: 10.2105/ajph.88.9.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Senior PA, Bhopal R. Ethnicity as a variable in epidemiological research. BMJ. 1994;309:327–330. doi: 10.1136/bmj.309.6950.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saxena S, Majeed FA, Jones M. Socioeconomic differences in childhood consultation rates in general practice in England and Wales: prospective cohort study. BMJ. 1999;318:642–646. doi: 10.1136/bmj.318.7184.642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Office for Population Censuses and Surveys. Health survey for England. London: HMSO; 1992. www.official-documents.co.uk/document/doh/survey99/hse99-14.htm (accessed 10 Jun 2002). [Google Scholar]
- 12.Blaxter M. Health and lifestyles. London: Tavistock/Routledge; 1990. [Google Scholar]
- 13.Irvine L, Crombie IK, Clark RA, Slane PW, Goodman KE, Feyerabend C, et al. What determines levels of passive smoking in children with asthma? Thorax. 1997;52:766–769. doi: 10.1136/thx.52.9.766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bakhshi SS, Hawker J, Ali S. The epidemiology of tuberculosis by ethnic group in Birmingham and its implications for future trends in tuberculosis in the UK. Ethn Health. 1997;2:147–153. doi: 10.1080/13557858.1997.9961823. [DOI] [PubMed] [Google Scholar]
- 15.Chandola T. Ethnic and class differences in health in relation to British South Asians: using the new national statistics socio-economic classification. Soc Sci Med. 2001;52:1285–1296. doi: 10.1016/s0277-9536(00)00231-8. [DOI] [PubMed] [Google Scholar]
- 16.Smith GD, Blane D, Barley M. The Black report on socioeconomic inequalities in health 10 years on. BMJ. 1990;301:373–377. doi: 10.1136/bmj.301.6748.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roland M, Rice N, Carr-Hill R. Socioeconomic determinants of rates of consultation in general practice based on the fourth national morbidity survey of general practices. BMJ. 1996;312:1008–1013. doi: 10.1136/bmj.312.7037.1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cooper H, Smaje C, Arber S. Use of health services by children and young people according to ethnicity and social class: secondary analysis of a national survey. BMJ. 1998;317:1047–1051. doi: 10.1136/bmj.317.7165.1047. [DOI] [PMC free article] [PubMed] [Google Scholar]