Abstract
Objectives
This study aimed to identify risk factors associated with intraoperative hypertension and new-onset electrocardiographic (ECG) abnormalities in hypertensive patients undergoing tooth extraction.
Materials and methods
This case-control study included 2,059 cases of tooth extractions performed in hypertensive patients under intraoperative ECG monitoring at Peking University School and Hospital of Stomatology. Blood pressure (BP) and heart rate (HR) were recorded at four key time points. We specifically analyzed patients who required antihypertensive intervention and those with new-onset intraoperative ECG abnormalities, employing logistic regression to identify independent risk factors. Additionally, ROC curves were used to determine the optimal cutoff points for linear variables, thereby developing the most effective predictive model.
Results
A total of 8.01% of patients required temporary intraoperative antihypertensive medication for blood pressure control, while 37.20% exhibited transient intraoperative ECG abnormalities. Only two cases resulted in temporary procedure termination due to inadequate blood pressure control, while all other procedures were successfully completed. Preoperative systolic blood pressure(SBP) ≥ 159 mmHg (AUC = 0.91, Sensitivity = 84.24%, Specificity = 88.75%) and operative time (OR = 3.620, P<0.001) were significantly associated with intraoperative blood pressure fluctuations. In addition, sex (OR = 0.796, P = 0.019), age (OR = 1.024, P < 0.001), history of cerebrovascular disease (OR = 1.301, P = 0.020), SBP at the start of the operation (OR = 1.011, P = 0.006), number of teeth extracted per session (OR = 1.182, P < 0.001), and estimated operative time (OR = 1.236, P = 0.017) were all significantly associated with new-onset intraoperative ECG abnormalities.
Conclusions
Intraoperative hypertension was strongly associated with preoperative SBP ≥ 159 mmHg and prolonged operative time. New-onset intraoperative ECG abnormalities were significantly associated with both patient-related factors (age, sex, cerebrovascular disease, baseline BP) and procedural variables (number of teeth extracted, and operative time).
Clinical relevance
This study provides evidence-based recommendations for optimizing cardiovascular risk management in hypertensive patients undergoing oral procedures, highlighting the need for individualized monitoring strategies.
Keywords: Hypertension, Tooth extraction, Cardiovascular risk, Electrocardiographic monitoring
Introduction
With the accelerating pace of population aging, the demand for tooth extraction treatments is steadily increasing [1]. Ensuring the safety and efficacy of these procedures remains a major challenge for dental practitioners, particularly when managing high-risk populations [2]. Among these, hypertensive patients require special attention due to their increased susceptibility to cardiovascular complications during surgery.
Hypertension is one of the most prevalent chronic diseases, especially among older individuals [3]. In China, approximately 24.7% of the population had been diagnosed with hypertension as of 2018, with a significant proportion being elderly [4]. Hypertension is closely linked to elevated cardiovascular risks, especially during physiologically stressful procedures such as tooth extraction [5]. Given these risks, effective preoperative assessment and intraoperative blood pressure management are essential for ensuring procedural safety [6, 7].
Despite the availability of general perioperative guidelines, such as the 2014 ACC/AHA classification of dental procedures as low-risk, no specific risk assessment tools exist for hypertensive patients undergoing tooth extraction [8, 9]. Previous studies have emphasized the role of dynamic blood pressure and electrocardiogram (ECG) monitoring in mitigating risks, yet the lack of a standardized protocol limits clinical decision-making [2, 6, 10, 11]. Existing research has explored factors potentially influencing cardiovascular risks during tooth extraction. Lu et al. examined the risks of tooth extraction in elderly patients with cardiovascular diseases, concluding that advanced age and comorbidities elevate surgical risks and recommending dynamic ECG monitoring during treatment [7]. Li et al. identified key factors influencing cardiovascular responses during tooth extractions, including age, gender, systemic diseases, and the number of teeth extracted [12]. Ma et al. suggested that blood pressure and psychological factors are important indicators for predicting cardiovascular risks during tooth extraction [1]. However, current evidence remains fragmented, and a consensus on the key determinants of cardiovascular risk in hypertensive patients undergoing tooth extraction has yet to be established.
These gaps highlight the urgent need for further research to identify and mitigate the specific risks faced by hypertensive patients during dental procedures. This study retrospectively analyzes hypertensive patients undergoing tooth extraction under ECG monitoring, focusing on preoperative characteristics influencing intraoperative cardiovascular risks. By addressing these critical gaps, the study aims to provide evidence-based insights to develop a tailored risk assessment framework, ultimately enhancing procedural safety and patient outcomes.
Materials and methods
Study design
This case-control study was conducted by collecting blood pressure (BP) and continuous electrocardiogram (ECG) monitoring data from hypertensive patients during oral treatment. Fluctuations in blood pressure and electrocardiographic abnormalities during treatment were analyzed to identify risk factors associated with cardiovascular responses. This study was approved by the Ethics Committee of the Peking University School of Stomatology (PKUSSIRB-202385014). All patients in the study have signed an informed consent form.
Patient selection
This retrospective study collected 3,312 consultation records from the electrocardiographic monitoring clinic of Peking University School of Stomatology in 2022. After data screening, 1,253 records were excluded: 1,003 records involved patients without a confirmed diagnosis of hypertension, 235 records corresponded to non-extraction procedures, and 15 records were excluded due to incomplete intraoperative monitoring data. Among these 15 records, 9 patients were rescheduled for elective surgery due to severe local inflammation or poor cooperation, and 6 cases lacked intraoperative monitoring data and were therefore excluded from the final analysis. Notably, telephone follow-up revealed that none of these patients experienced major cardiovascular adverse events during the follow-up period.
Ultimately, 2,059 consultation records from 1,314 unique hypertensive patients undergoing tooth extraction with complete ECG and blood pressure monitoring were included in the final analysis. Among these, 745 were repeat visits by the same patients. Each consultation was treated as an independent event based on the clinical independence of each dental treatment session.
All patients underwent a comprehensive preoperative evaluation, including an ECG, medical history review, and physical examination by a cardiologist. Blood pressure and ECG data were continuously monitored throughout the treatment. Inclusion criteria for the subjects were: (1) a confirmed diagnosis of hypertension based on patient medical history and medication history; (2) at least one dental treatment procedure performed under ECG monitoring with complete medical records. Patients with fewer than three intraoperative heart rate and blood pressure recordings were excluded, as procedures lasting less than 10 min did not provide sufficient monitoring data for statistical analysis.
Data collection
Monitoring data were obtained from the cardiologist’s continuous ECG (NIHON KOHDEN CORPORATION, BSM-2351 C) and BP records. These included details such as the patient’s medical history, BP, and heart rate upon admission to the treatment room, as well as intraoperative continuous ECG and BP monitoring data. BP was recorded at 5–10-minute intervals throughout the procedure.
The independent variables in this study were grouped into three categories for analysis:
Basic patient information: Gender, age and systemic comorbidities (e.g., coronary heart disease, arrhythmia, diabetes, cerebrovascular disease).
Preoperative clinical parameters: BP, HR, and ECG findings recorded at the initial consultation and at the start of surgery.
Surgical characteristics: Procedural complexity (e.g., number of teeth extracted, use of high-speed turbine handpieces), whether surgical incision was performed, whether the extraction was due to periodontitis, and the estimated operative time based on intraoperative ECG monitoring records.
Risk analysis
Risk assessment focused on two aspects: comparing patients requiring intraoperative antihypertensive interventions versus those who did not, and comparing patients with new intraoperative ECG abnormalities versus those without.
Intraoperative intervention criteria: (1) administering oral antihypertensive medications to patients with systolic blood pressure exceeding 180 mmHg during surgery; (2) administering oral antihypertensive medications to patients whose systolic blood pressure remained above 170 mmHg after at least two intraoperative measurements.
Definition of intraoperative ECG abnormalities: Newly detected ECG abnormalities were defined as those not present in the preoperative ECG but observed for the first time during intraoperative ECG monitoring.
Statistical analysis
Statistical analyses were conducted using SPSS version 27.0. Continuous variables were presented as mean ± standard deviation (SD) and analyzed using independent-samples t-tests. In cases where the assumption of equal variances was violated, Welch’s correction was applied. Categorical variables were expressed as frequencies and percentages [n (%)].
Multivariate logistic regression analysis was conducted to identify independent risk factors associated with intraoperative BP fluctuations and new-onset ECG abnormalities, with variables selected using the enter method. Receiver operating characteristic (ROC) curves were utilized to assess the predictive accuracy of significant variables. Statistical significance was defined as P < 0.05.
Result
Demographic characteristics
Among the 2,309 medical records of hypertensive patients seen at the ECG monitoring clinic, 250 cases were excluded due to procedures unrelated to tooth extraction. Ultimately, 1,314 hypertensive patients who underwent tooth extractions were included, contributing a total of 2,059 medical records for analysis. Of these, 702 patients (53.42%) were female and 612 (46.58%) were male. The mean age of the study population was 74.62 ± 11.42 years, ranging from 27 to 99 years.
Regarding antihypertensive medication regimens, calcium channel blockers (CCBs) were the most frequently used. A total of 332 patients (25.27%) received CCB monotherapy. Among combination therapies, the most common regimen was CCBs combined with β-blockers, prescribed in 156 cases (11.87%). All patients continued their regular antihypertensive regimens without modification. Temporary antihypertensive medication was administered only during the procedure when systolic blood pressure reached or exceeded 180 mmHg, based on the recommendation of the internal medicine physician.
Additionally, 925 patients (70.40%) had at least one other systemic chronic condition. The most common comorbidities included coronary heart disease, arrhythmia, diabetes mellitus, and cerebrovascular disease.
Of the 2,059 visits, two surgeries were terminated due to excessively elevated intraoperative blood pressure. In total, 945 visits (45.90%) involved the extraction of a single tooth, while one patient underwent extraction of up to eight teeth in a single session. Incisions were performed in 101 cases (4.91%), and a high-speed turbine handpiece was used in 47 cases (2.28%).
Periodontitis accounted for approximately 37.77% of the indications for extraction, with other causes including residual roots/crowns and impacted teeth. According to intraoperative ECG monitoring, most procedures lasted between 20 and 30 min, accounting for 56.63% of all cases. Detailed characteristics are summarized in Table 1.
Table 1.
Demographic characteristics of study participants (N = 1314)
| Characteristic | n | % | |
|---|---|---|---|
| Age | Years (x̄±s) | 74.62 ± 11.42 | |
| Gender | Male | 612 | 46.58% |
| Female | 702 | 53.42% | |
| Medication regimen | |||
| CCB only | 332 | 25.27% | |
| ARB only | 188 | 14.31% | |
| ACEI only | 12 | 0.91% | |
| β-blocker only | 98 | 7.46% | |
| CCB + β-blocker | 156 | 11.87% | |
| CCB + ARB | 153 | 11.64% | |
| ARB + β-blocker | 113 | 8.60% | |
| CCB + ARB + β-blocker | 87 | 6.62% | |
| Others | 34 | 2.59% | |
| Unknows | 141 | 10.73% | |
| Other Systemic Chronic Diseases | |||
| Coronary heart disease | 425 | 32.34% | |
| Arrhythmia | 217 | 16.51% | |
| Diabetes | 388 | 29.53% | |
| Cerebrovascular disease | 295 | 22.45% | |
| Number of teeth extracted | |||
| 1 | 945 | 45.90% | |
| 2 | 616 | 29.92% | |
| 3 | 308 | 14.96% | |
| 4–8 | 188 | 9.13% | |
| Surgical procedures | |||
| Incisions | 101 | 4.91% | |
| High-speed turbine handpiece | 47 | 2.28% | |
| Reasons for extraction | |||
| Periodontitis | 757 | 37.77% | |
| Others | 1302 | 63.23% | |
| Estimated operative time | |||
| ≤20 min | 866 | 42.06% | |
| 20–30 min | 1166 | 56.63% | |
| >30 min | 27 | 1.31% | |
Blood pressure and heart rate values
Table 2 presents the systolic blood pressure (SBP), diastolic blood pressure (DBP), and heart rate (HR) at three timepoints: preoperatively, at the start of the operation, and intraoperatively. Overall, female patients showed significantly higher SBP and HR, and lower DBP, compared to males across all timepoints. Patients aged ≥ 76 years had consistently higher SBP, lower DBP, and slower HR than those < 76 years.
Table 2.
Preoperative, at the start of operation, and intraoperative maximum blood pressure and heart rate measurement results (x̄±s) (N = 2,059)
| Preoperative BP and HR | At the start of the operation’s BP and HR | Intraoperative BP and HR | |||||||
|---|---|---|---|---|---|---|---|---|---|
| SBP (mmHg) | DBP (mmHg) | HR | SBP (mmHg) | DBP (mmHg) | HR | SBP (mmHg) | DBP (mmHg) | HR | |
| Total | 141.74 ± 19.06 | 70.61 ± 12.31 | 76.27 ± 12.58 | 143.16 ± 17.01 | 71.17 ± 11.48 | 78.28 ± 12.83 | 146.80 ± 17.33 | 72.41 ± 11.55 | 74.47 ± 12.50 |
| Sex | |||||||||
| Male | 139.56 ± 18.45 | 71.85 ± 12.33 | 74.94 ± 12.22 | 141.50 ± 17.03 | 72.38 ± 11.35 | 76.88 ± 12.44 | 144.67 ± 17.05 | 73.64 ± 11.31 | 73.04 ± 12.27 |
| Female | 143.62 ± 19.38 | 69.53 ± 12.19 | 77.42 ± 12.78 | 144.60 ± 16.87 | 70.12 ± 11.49 | 79.50 ± 13.05 | 148.63 ± 17.36 | 71.35 ± 11.66 | 75.71 ± 12.57 |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Age | |||||||||
| 27–75 | 138.70 ± 18.65 | 74.31 ± 12.11 | 77.94 ± 12.92 | 140.97 ± 16.90 | 74.64 ± 11.06 | 79.81 ± 13.18 | 144.61 ± 17.57 | 75.79 ± 11.01 | 76.13 ± 12.98 |
| 76–99 | 144.29 ± 19.03 | 67.50 ± 11.60 | 74.88 ± 12.12 | 145.00 ± 16.90 | 68.25 ± 11.00 | 77.00 ± 12.40 | 148.64 ± 16.91 | 69.58 ± 11.23 | 73.08 ± 11.91 |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Coronary heart disease | |||||||||
| Yes | 137.54 ± 17.35 | 68.98 ± 11.85 | 73.31 ± 11.48 | 140.30 ± 16.99 | 69.93 ± 11.02 | 75.16 ± 11.70 | 144.02 ± 16.60 | 71.40 ± 11.00 | 71.45 ± 11.66 |
| No | 143.92 ± 19.54 | 71.45 ± 12.46 | 77.81 ± 12.85 | 144.64 ± 16.84 | 71.81 ± 11.66 | 79.90 ± 13.10 | 148.24 ± 17.53 | 72.94 ± 11.80 | 76.04 ± 12.63 |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.004 | <0.001 |
| Arrhythmia | |||||||||
| Yes | 140.83 ± 19.43 | 71.83 ± 12.98 | 77.20 ± 15.13 | 141.71 ± 18.63 | 71.92 ± 12.59 | 78.81 ± 15.05 | 144.77 ± 17.20 | 73.06 ± 12.25 | 75.18 ± 14.63 |
| No | 141.91 ± 18.99 | 70.38 ± 12.17 | 76.10 ± 12.04 | 143.43 ± 16.68 | 71.03 ± 11.25 | 78.18 ± 12.37 | 147.18 ± 17.33 | 72.29 ± 11.42 | 74.34 ± 12.06 |
| P-value | 0.350 | 0.050 | 0.326 | 0.094 | 0.200 | 0.216 | 0.021 | 0.270 | 0.482 |
| Diabetes | |||||||||
| Yes | 140.26 ± 19.55 | 68.55 ± 11.98 | 77.18 ± 13.48 | 143.19 ± 17.50 | 69.83 ± 11.39 | 79.00 ± 13.30 | 146.29 ± 17.67 | 71.17 ± 11.84 | 75.29 ± 13.22 |
| No | 142.38 ± 18.81 | 71.51 ± 12.35 | 75.88 ± 12.15 | 143.15 ± 16.80 | 71.76 ± 11.47 | 77.97 ± 12.61 | 147.02 ± 17.18 | 72.96 ± 11.38 | 74.12 ± 12.16 |
| P-value | 0.020 | <0.001 | 0.051 | 0.958 | <0.001 | 0.030 | 0.383 | 0.001 | 0.094 |
| Cerebrovascular disease | |||||||||
| Yes | 139.86 ± 18.76 | 69.01 ± 11.88 | 75.30 ± 11.23 | 142.48 ± 16.44 | 69.97 ± 10.70 | 76.84 ± 11.45 | 145.96 ± 16.54 | 71.14 ± 11.08 | 73.47 ± 11.36 |
| No | 142.31 ± 19.12 | 71.10 ± 12.40 | 76.57 ± 12.95 | 143.37 ± 17.18 | 71.53 ± 11.68 | 78.72 ± 13.20 | 147.05 ± 17.56 | 72.80 ± 11.67 | 74.78 ± 12.81 |
| P-value | 0.013 | 0.001 | 0.032 | 0.316 | 0.009 | 0.037 | 0.228 | 0.006 | 0.002 |
Patients with coronary heart disease exhibited significantly lower SBP, DBP, and HR throughout the perioperative period. Similarly, those with cerebrovascular disease had lower DBP and HR. Diabetic patients had lower DBP and a modestly lower HR, while arrhythmia was associated with a slight reduction in intraoperative SBP.
The trends were largely consistent across the three phases of measurement, and all statistically significant differences are indicated in Table 2.
Risk analysis
Blood pressure and heart rate indicators
Among the 2,059 consultation records, 167 patients were assessed as high-risk by the internist and required medication intervention. Of these, 165 interventions were followed by successful completion of surgery, while 2 cases were deemed too high-risk by the internist, leading to the termination of treatment. Thus, 165 (8.01%) consultation records were included in the medication intervention group for analysis.
Among them, 164 cases involved intraoperative systolic blood pressure peaks exceeding 180 mmHg. In only one case, temporary administration of nitroglycerin (0.3 mg) was given due to two consecutive systolic BP readings above 170 mmHg with an upward trend; the two measurements were 170/74 mmHg and 175/67 mmHg, respectively. Of the patients who received intraoperative medication, 86.06% used nitroglycerin, with doses ranging from 0.3 to 0.5 mg. A few patients used captopril, metoprolol, or a combination of nitroglycerin and captopril, depending on their condition. A detailed summary is available in Table 3.
Table 3.
Intervention during surgery (N = 165)
| Type | n(%) |
|---|---|
| Nitroglycerin | 142 (86.06%) |
| Captopril | 1 (0.61%) |
| Captopril + Nitroglycerin | 4 (2.42%) |
| Metoprolol | 4 (2.42%) |
| Metoprolol + Nitroglycerin | 5(3.03%) |
| Metoprolol + Captopril | 7(4.24%) |
| Nitroglycerin + Metoprolol + Captopril | 2(1.21%) |
| Total | 165 (100%) |
Logistic regression analysis was conducted to examine factors associated with the need for intraoperative medication intervention. The analysis revealed that higher preoperative systolic blood pressure (OR = 1.138, P < 0.001), higher systolic blood pressure at the start of the operation (OR = 1.019, P = 0.028), and higher HR at the start of the operation (OR = 1.064, P = 0.004) were significantly associated with an increased likelihood of requiring medication intervention. Furthermore, estimated operative time associated with a greater likelihood of intraoperative medication intervention (OR = 3.620, P<0.001). However, comorbidities such as coronary heart disease, arrhythmia, cerebrovascular disease, and diabetes showed no statistically significant association with the need for intraoperative medication intervention. Detailed results are presented in Table 4.
Table 4.
Multivariate analysis of the blood pressure intervention group
| OR | OR 95%CI Lower limit |
OR 95%CI Higher limit | P-value | |
|---|---|---|---|---|
| Sex | 1.323 | 0.826 | 2.120 | 0.245 |
| Age | 0.987 | 0.967 | 1.007 | 0.211 |
| Coronary heart disease | 0.745 | 0.441 | 1.258 | 0.271 |
| Diabetes | 1.220 | 0.747 | 1.991 | 0.427 |
| Cerebrovascular disease | 1.434 | 0.797 | 2.581 | 0.229 |
| Arrhythmia | 1.180 | 0.643 | 2.165 | 0.594 |
| Preoperative SBP | 1.138 | 1.117 | 1.159 | <0.001*** |
| Preoperative HR | 0.958 | 0.918 | 1.001 | 0.053 |
| At the start of the operation’s SBP | 1.019 | 1.002 | 1.036 | 0.028* |
| At the start of the operation’s HR | 1.064 | 1.021 | 1.110 | 0.004** |
| Number of tooth extractions per time | 1.114 | 0.913 | 1.360 | 0.286 |
| Dental high-speed turbine handpieces | 0.837 | 0.230 | 3.046 | 0.787 |
| Surgical incision | 0.438 | 0.180 | 1.063 | 0.068 |
| Tooth extraction due to periodontitis | 0.823 | 0.528 | 1.282 | 0.389 |
| Estimated operative time | 3.620 | 2.341 | 5.599 | <0.001*** |
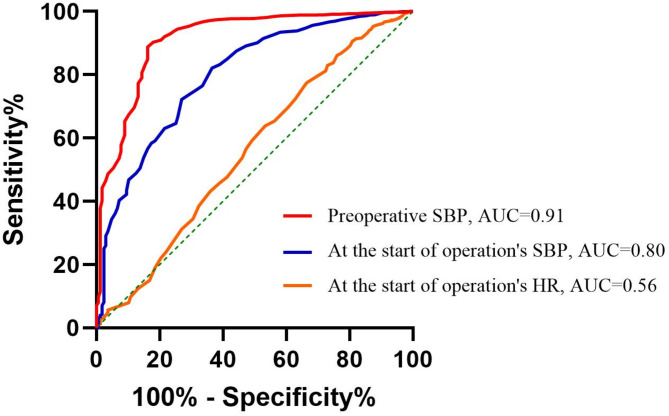
Further receiver operating characteristic (ROC) curves were plotted to determine the cut-off points for continuous variables. The ROC curve is shown in Fig. 1. Preoperative SBP, HR and SBP at the start of the operation were all associated with the need for intraoperative medication intervention. Among these, preoperative SBP had the highest predictive efficiency, with an area under the curve (AUC) of 0.91. Using 158.5 mmHg as the threshold for preoperative SBP yielded the highest Youden index of 0.73. When 159 mmHg was used as the cut-off, the sensitivity for predicting the need for intraoperative medication intervention to control blood pressure was 84.24%, and the specificity was 88.75%.
Fig. 1.
ROC curves for preoperative SBP, SBP and HR at the start of the operation
ECG abnormality indicators
Among the 2,059 consultation records in this study, 766 cases (37.20%) exhibited new ECG abnormalities detected through continuous monitoring during surgery. The most frequently observed abnormalities were supraventricular premature atrial contraction (44.39%) and Ventricular premature contraction (42.30%), together accounting for 86.69% of the new ECG findings. Less common abnormalities included sinus arrhythmia (5.61%), ventricular premature contraction combined with premature atrial contraction (4.31%). A detailed summary of these findings is provided in Table 5.
Table 5.
Types of abnormal cardiac rhythms (N = 766)
| Type | N (%) |
|---|---|
| Supraventricular premature atrial contraction | 340 (44.39%) |
| Ventricular premature contraction | 324 (42.30%) |
| Sinus arrhythmia | 43 (5.61%) |
| Ventricular premature contraction + Premature atrial contraction | 33 (4.31%) |
| Atrioventricular conduction block | 6 (0.78%) |
| Supraventricular tachycardia | 7 (0.91%) |
| Ventricular premature contraction + Atrioventricular conduction block | 1 (0.13%) |
| Ventricular premature contraction + Sinus arrhythmia | 5 (0.65%) |
| Supraventricular premature atrial contraction + Sinus arrhythmia | 6 (0.78%) |
| Sinus arrhythmia + Supraventricular premature atrial contraction | 1 (0.13%) |
To avoid potential interference in the analysis, factors other than arrhythmias were included in the logistic regression analysis, with the results presented in Table 6. The analysis revealed that patient age (OR = 1.024, P<0.001), sex (OR = 0.796, P = 0.019), SBP at the start of the operation (OR = 1.011, P = 0.006), number of tooth extractions per time(OR = 1.182, P<0.001) and estimated operative time (OR = 1.236, P = 0.017) were all statistically significantly associated with new intraoperative ECG abnormalities.
Table 6.
Multivariate analysis of abnormal electrocardiogram group
| OR | OR 95%CI Lower limit |
OR 95%CI Higher limit | P-value | |
|---|---|---|---|---|
| Sex | 0.796 | 0.658 | 0.963 | 0.019* |
| Age | 1.024 | 1.015 | 1.034 | <0.001*** |
| Coronary heart disease | 0.960 | 0.782 | 1.178 | 0.695 |
| Diabetes | 1.054 | 0.862 | 1.288 | 0.610 |
| Cerebrovascular disease | 1.301 | 1.042 | 1.624 | 0.020* |
| Preoperative SBP | 0.997 | 0.990 | 1.004 | 0.373 |
| Preoperative HR | 1.010 | 0.990 | 1.031 | 0.327 |
| At the start of the operation’s SBP | 1.011 | 1.003 | 1.019 | 0.006** |
| At the start of the operation’s HR | 0.996 | 0.976 | 1.017 | 0.709 |
| Number of tooth extractions per time | 1.182 | 1.082 | 1.290 | <0.001*** |
| Dental high-speed turbine handpieces | 0.880 | 0.468 | 1.658 | 0.693 |
| Surgical incision | 0.935 | 0.598 | 1.463 | 0.769 |
| Tooth extraction due to periodontitis | 1.059 | 0.875 | 1.282 | 0.558 |
| Estimated operative time | 1.236 | 1.038 | 1.471 | 0.017* |
ROC curves were generated for the identified continuous variables (shown in Fig. 2). Among them, patient age showed the highest predictive ability, with an AUC of 0.57. The optimal cutoff value for age was 79.5 years, yielding the highest Youden index of 0.10, with a sensitivity of 48.83% and specificity of 61.56%.
Fig. 2.
ROC curves of SBP at the start of operation and age
Discussion
This study investigated the potential cardiovascular risks associated with tooth extractions in patients with hypertension, underscoring the need for effective preoperative BP management and continuous intraoperative ECG monitoring. The findings indicate that while most intraoperative BP and cardiac rhythm abnormalities were manageable, certain patient subgroups may require enhanced monitoring and targeted interventions. In particular, patients with preoperative SBP ≥ 159 mmHg or those undergoing prolonged procedures should receive intensified monitoring intraoperative BP fluctuations, and temporary antihypertensive treatment should be considered when necessary. Furthermore, female patients, elderly individuals, those with a history of cerebrovascular disease, patients requiring the extraction of multiple teeth, and those undergoing prolonged procedures were more likely to develop new-onset intraoperative ECG abnormalities.
BP control is widely recognized as a primary concern in dental procedures involving hypertensive patients [13–15]. According to current guidelines, elective surgery should be postponed in patients with SBP ≥ 180 mmHg or DBP ≥ 110 mmHg unless urgent intervention is required [16]. In this study, similar criteria were applied to determine the need for intraoperative antihypertensive medication. Continuous ECG monitoring is also a crucial component of dental management in hypertensive individuals [7], as psychological stress and local anesthetic administration during extractions may provoke arrhythmias [17]. The most commonly observed arrhythmia in this study was premature contraction. Although often benign, ventricular premature beats have been statistically associated with increased all-cause mortality in hypertensive patients with underlying heart disease [18, 19], warranting clinical attention.
In the present cohort, approximately 8.01% of patients required intraoperative pharmacologic intervention for BP control, while 37.20% developed new-onset ECG abnormalities during the procedure. All of these arrhythmias were non-lethal. Only two procedures were temporarily terminated due to excessive BP elevations, with no life-threatening emergencies recorded. Overall, tooth extraction in hypertensive patients appears to be relatively safe, but close intraoperative monitoring remains essential.
The present study revealed that female patients exhibited significantly higher SBP and HR both preoperatively and intraoperatively, while DBP was significantly lower compared to male patients. These findings are consistent with those reported by Li et al. [12], suggesting that female patients may require more rigorous blood pressure management in daily clinical care. However, despite these baseline hemodynamic differences, no statistically significant sex-based difference was observed in the incidence of intraoperative hypertension. Similarly, Nathan et al. reported that hypertensive female patients generally have a lower overall risk of coronary events compared to males [20]. In terms of ECG monitoring, women were more likely to develop new-onset intraoperative ECG abnormalities [21], which may be partly attributed to higher emotional stress during surgery.
Patients aged ≥ 76 years exhibited significantly higher SBP, lower DBP, and greater pulse pressure differences both before and during surgery. These age-related hemodynamic alterations are well-documented and are generally associated with increased arterial stiffness and diminished vascular compliance in older individuals [22]. However, our multivariate regression analysis did not identify age as a significant independent predictor of intraoperative hypertension requiring medication, suggesting that other factors may play a more dominant role in intraoperative blood pressure control. Notably, older patients were significantly more likely to experience intraoperative cardiac arrhythmias, likely due to diminished physiological reserves [23]. This finding is consistent with the study by Ma et al. [1], which identified age as a critical factor in surgical risk assessment. Additionally, a large cohort study has demonstrated that advanced age is significantly associated with increased occurrence of ECG abnormalities [21]. These findings underscore the necessity of routine ECG monitoring during dental procedures in elderly patients to enable timely detection and intervention of arrhythmic events.
Patients with preoperative SBP ≥ 159 mmHg were more likely to require intraoperative antihypertensive medication, while those with elevated SBP and HR at the start of the procedure were at increased risk of developing new-onset intraoperative ECG abnormalities. These results align with earlier studies indicating that a preoperative SBP of ≥ 160 mmHg serves as a reliable predictor of inadequate long-term BP control [24]. Therefore, preoperative BP assessment is not only essential as a baseline vital sign but also serves as an effective screening tool to identify high-risk patients who may benefit from continuous ECG monitoring and tailored intraoperative interventions [25].
Patients with a history of cerebrovascular disease were more likely to develop new-onset intraoperative ECG abnormalities. Previous studies have also shown a correlation between cerebrovascular disease and cardiac abnormalities, with stroke survivors being at higher risk of subsequent major cardiovascular events [26, 27]. Greater attention should thus be paid to intraoperative ECG monitoring in these patients. In contrast, this study did not find statistically significant associations between intraoperative BP or ECG abnormalities and comorbidities such as coronary heart disease or diabetes. Nonetheless, previous literature suggests that hypertensive patients with such comorbidities often have worse long-term outcomes [28], indicating that intraoperative monitoring remains clinically important in these populations.
We also analyzed surgery-related risk factors. Operative time was significantly associated with both intraoperative BP fluctuations and new-onset ECG abnormalities, and the number of teeth extracted per session was similarly associated with ECG changes. These findings suggest that for patients with existing cardiovascular risk factors, reducing the number of extractions per visit and shortening the overall operative duration may help minimize intraoperative cardiovascular stress. This is consistent with findings by Li et al., who also reported that increased extraction numbers may elevate the risk of cardiovascular events during dental procedures [12].
Surgical incision, often necessary for complex extractions, showed a trend toward association with intraoperative hypertension in our study, although the result did not reach statistical significance (P = 0.068). Clinicians should be particularly cautious about BP changes in patients undergoing surgical incisions for difficult extractions. Although periodontitis has been linked to adverse cardiovascular outcomes [29], our study did not find a significant association between the cause of extraction (e.g., periodontitis) and intraoperative BP or ECG changes. It is possible that the cardiovascular impact of periodontitis manifests more gradually over time and may not be readily apparent during the surgical procedure. Longer-term studies are needed to explore this potential relationship further.
This study has several limitations. As a single-center retrospective analysis, it is inherently subject to potential biases, including selection bias, and causality cannot be clearly established. The findings primarily reflect the characteristics of the patient population and clinical practices at our institution, and may not be generalizable to hypertensive patients undergoing dental treatment in other healthcare settings. Due to limitations in data availability, key variables such as the dosage of local anesthetics, the time interval between the last antihypertensive medication intake and the start of surgery, and the occurrence of postoperative complications (e.g., bleeding or infection) were not assessed. Future prospective studies incorporating longitudinal follow-up data and a broader range of clinical variables are warranted to provide a more comprehensive understanding of cardiovascular risks in hypertensive patients undergoing dental procedures.
Conclusion
This study investigated the cardiovascular risks associated with tooth extractions in patients with hypertension, highlighting the importance of preoperative blood pressure control and continuous intraoperative ECG monitoring. The findings indicated that patients with preoperative SBP exceeding 159 mmHg, elevated SBP and HR at the start of the procedure, and longer operative times were more likely to experience intraoperative hypertension requiring pharmacological intervention. Furthermore, female patients, older individuals, those with a history of cerebrovascular disease, elevated SBP at the start of the operation, a greater number of teeth extracted per session, and longer surgical times were at increased risk of intraoperative arrhythmias.
Acknowledgements
We gratefully acknowledge the support from the Clinical Research Foundation of Peking University School and Hospital of Stomatology.
Author contributions
Y. Y wrote the main manuscript text, W. W and X. X provided guidance on the writing and ensured the scientific accuracy of the content, Y.J was responsible for the scientific validity of the statistical analysis and revised the manuscript, C.L and J.L collected and analyzed the data. All authors reviewed the manuscript.
Funding
This work was supported by grants from Clinical Research Foundation of Peking University School and Hospital of Stomatology (PKUSS-2023CRF205).
Data availability
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Declarations
Consent for publication
This study does not contain any personally identifiable information, and all data have been anonymized. Therefore, consent for publication is not applicable.
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare that the research was conducted without any commercial or financial relationships that could potentially create a conflict of interest.
Ethical approval and consent to participate
This study was conducted in accordance with the principles of the Declaration of Helsinki. Ethical approval was obtained from the Ethics Committee of the Peking University School of Stomatology (PKUSSIRB-202385014). Written informed consent was obtained from all participants prior to their inclusion in the study.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yifan Yang and Wenying Wang contributed equally to this work.
Contributor Information
Ying Ji, Email: Jiyingpku@163.com.
Xiangliang Xu, Email: Kqxxl@126.com.
References
- 1.Ma S, Chen X, Zhai Y, Sun X, Sheng J, Sun Y, Wang H. Predictive risk factors for adverse events during tooth extraction among elderly patients with cardiovascular diseases. Ann Med. 2025;57:2448274. 10.1080/07853890.2024.2448274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Valtellini R, Ouanounou A. Management of the hypertensive dental patient. J Can Dent Assoc. 2023;89:n2. [PubMed] [Google Scholar]
- 3.Chapel JM, Ritchey MD, Zhang D, Wang G. Prevalence and medical costs of chronic diseases among adult medicaid beneficiaries. Am J Prev Med. 2017;53:S143–54. 10.1016/j.amepre.2017.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Worldwide trends in. Hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398:957–80. 10.1016/S0140-6736(21)01330-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang M, Shi Y, Zhou B, Huang Z, Zhao Z, Li C, Zhang X, Han G, Peng K, Li X, Wang Y, Ezzati M, Wang L, Li Y. Prevalence, awareness, treatment, and control of hypertension in China, 2004-18: findings from six rounds of a National survey. BMJ. 2023;380:e071952. 10.1136/bmj-2022-071952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rapsomaniki E, Timmis A, George J, Pujades-Rodriguez M, Shah AD, Denaxas S, White IR, Caulfield MJ, Deanfield JE, Smeeth L, Williams B, Hingorani A, Hemingway H. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1·25 million people. Lancet. 2014;383:1899–911. 10.1016/S0140-6736(14)60685-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lu P, Gong Y, Chen Y, Cai W, Sheng J. Safety analysis of tooth extraction in elderly patients with cardiovascular diseases. Med Sci Monit. 2014;20:782–8. 10.12659/MSM.890131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Koutsaki M, Patoulias D, Tsinivizov P, Doumas M, Kallistratos M, Thomopoulos C, Poulimenos L, Agnelli G, Mancia G, Manolis A. Evaluation, risk stratification and management of hypertensive patients in the perioperative period. Eur J Intern Med. 2019;69:1–7. 10.1016/j.ejim.2019.09.012. [DOI] [PubMed] [Google Scholar]
- 9.Hartle A, McCormack T, Carlisle J, Anderson S, Pichel A, Beckett N, Woodcock T, Heagerty A. The measurement of adult blood pressure and management of hypertension before elective surgery: joint guidelines from the association of anaesthetists of great Britain and Ireland and the British hypertension society. Anaesthesia. 2016;71:326–37. 10.1111/anae.13348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang K, Aleexenko V, Jeevaratnam K. Computational approaches for detection of cardiac rhythm abnormalities: are we there yet? J Electrocardiol. 2020;59:28–34. 10.1016/j.jelectrocard.2019.12.009. [DOI] [PubMed] [Google Scholar]
- 11.Lip GYH, Coca A, Kahan T, Boriani G, Manolis AS, Olsen MH, Oto A, Potpara TS, Steffel J, Marín F, de Oliveira Figueiredo MJ, de Simone G, Tzou WS, En C, Chiang, Williams B. Hypertension and cardiac arrhythmias: executive summary of a consensus document from the European heart rhythm association (EHRA) and ESC Council on hypertension, endorsed by the heart rhythm society (HRS), Asia-Pacific heart rhythm society (APHRS), and sociedad Latinoamericana de estimulación cardíaca y electrofisiología (SOLEACE). Eur Heart J Cardiovasc Pharmacother. 2017;3:235–50. 10.1093/ehjcvp/pvx019. [DOI] [PubMed] [Google Scholar]
- 12.Li J, Tian Z, Qi S, Zhang J, Li L, Pan J. Cardiovascular response of aged outpatients with systemic diseases during tooth extraction: A Single-Center retrospective observational study. Front Public Health. 2022;10:938609. 10.3389/fpubh.2022.938609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kubota K, Yamaga E, Ueda K, Inokoshi M, Minakuchi S. Comparison of cardiovascular response between patients on warfarin and hypertensive patients not on warfarin during dental extraction. Clin Oral Investig. 2021;25:2141–50. 10.1007/s00784-020-03526-8. [DOI] [PubMed] [Google Scholar]
- 14.Safar ME. Systolic blood pressure, pulse pressure and arterial stiffness as cardiovascular risk factors. Curr Opin Nephrol Hypertens. 2001;10:257–61. [DOI] [PubMed] [Google Scholar]
- 15.Brand HS, Gortzak RA, Palmer-Bouva CC, Abraham RE. Abraham-Inpijn, cardiovascular and neuroendocrine responses during acute stress induced by different types of dental treatment. Int Dent J. 1995;45:45–8. [PubMed] [Google Scholar]
- 16.Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I. 2018 ESC/ESH guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European society of cardiology and the European society of hypertension: the task force for the management of arterial hypertension of the European society of cardiology and the European society of hypertension. J Hypertens. 2018;36:1953–2041. 10.1097/HJH.0000000000001940. [DOI] [PubMed] [Google Scholar]
- 17.Blinder D, Manor Y, Shemesh J, Taicher S. Electrocardiographic changes in cardiac patients having dental extractions under a local anesthetic containing a vasopressor. J Oral Maxillofac Surg 56 (1998). [DOI] [PubMed]
- 18.Almendral J, Villacastin JP, Arenal A, Tercedor L, Merino JL, Delcan JL. Evidence favoring the hypothesis that ventricular arrhythmias have prognostic significance in left ventricular hypertrophy secondary to systemic hypertension. Am J Cardiol. 1995;76:D60–3. [DOI] [PubMed] [Google Scholar]
- 19.Bayés-Genís A, Guindo J, Viñolas X, Tomás L, Elosua R, Duran I. Bayés de Luna, cardiac arrhythmias and left ventricular hypertrophy in systemic hypertension and their influences on prognosis. Am J Cardiol. 1995;76:D54–9. [DOI] [PubMed] [Google Scholar]
- 20.Wong ND, Thakral G, Franklin SS, L’Italien GJ, Jacobs MJ, Whyte JL, Lapuerta P. Preventing heart disease by controlling hypertension: impact of hypertensive subtype, stage, age, and sex. Am Heart J. 2003;145:888–95. [DOI] [PubMed] [Google Scholar]
- 21.Yu L, Ye X, Yang Z, Yang W, Zhang B. Prevalences and associated factors of electrocardiographic abnormalities in Chinese adults: a cross-sectional study. BMC Cardiovasc Disord. 2020;20:414. 10.1186/s12872-020-01698-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tsai T-Y, Cheng H-M, Chuang S-Y, Chia Y-C, Soenarta AA, Minh HV, Siddique S, Turana Y, Tay JC, Kario K, Chen C-H. Isolated systolic hypertension in Asia. J Clin Hypertens (Greenwich). 2021;23:467–74. 10.1111/jch.14111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381:752–62. 10.1016/S0140-6736(12)62167-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schonberger RB, Nwozuzu A, Zafar J, Chen E, Kigwana S, Monteiro MM, Charchaflieh J, Sophanphattana S, Dai F, Burg MM. Elevated preoperative blood pressures in adult surgical patients are highly predictive of elevated home blood pressures. J Am Soc Hypertens. 2018;12:303–10. 10.1016/j.jash.2018.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Venkatesan S, Myles PR, Manning HJ, Mozid AM, Andersson C, Jørgensen ME, Hardman JG, Moonesinghe SR, Foex P, Mythen M, Grocott MPW, Sanders RD. Cohort study of preoperative blood pressure and risk of 30-day mortality after elective non-cardiac surgery. Br J Anaesth. 2017;119:65–77. 10.1093/bja/aex056. [DOI] [PubMed] [Google Scholar]
- 26.Buckley BJR, Harrison SL, Hill A, Underhill P, Lane DA, Lip GYH. Stroke-Heart syndrome: incidence and clinical outcomes of cardiac complications following stroke. Stroke. 2022;53:1759–63. 10.1161/STROKEAHA.121.037316. [DOI] [PubMed] [Google Scholar]
- 27.Rohner MH, Gebhard C, Luft A, Hänsel M, Wegener S. Cardiac findings following cerebrovascular disease. J Am Heart Assoc. 2024;13:e034131. 10.1161/JAHA.124.034131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhu B, Liu Y, Zhou W, Du Y, Qi D, Wang C, Cheng Q, Zhang Y, Wang S, Gao C. Clinical characteristics and outcomes of Chinese patients with coronary heart disease and resistant hypertension. J Clin Hypertens (Greenwich). 2023;25:350–9. 10.1111/jch.14651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Norhammar A, Näsman P, Buhlin K, de Faire U, Ferrannini G, Gustafsson A, Kjellström B, Kvist T, Jäghagen EL, Lindahl B, Nygren Å, Näslund U, Svenungsson E, Klinge B, Rydén L. Does periodontitis increase the risk for future cardiovascular events?? Long-Term Follow-Up of the PAROKRANK study. J Clin Periodontol. 2025;52:16–23. 10.1111/jcpe.14064. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.