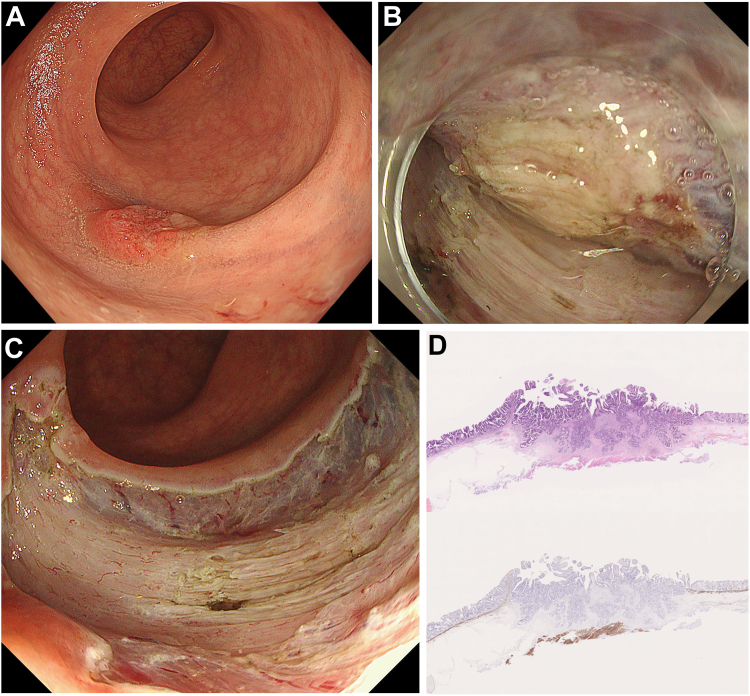
An 87-year-old man was referred for colonoscopy due to a positive fecal occult blood test. His medical history included prostate cancer treated with radiation therapy, emphysema, hypertension, and hyperlipidemia. Colonoscopy revealed a 17-mm nongranular type laterally spreading tumor in the lower rectum (Figure A). Although pretreatment endoscopic assessment suggested an invasion depth of T1b or T2, endoscopic treatment was chosen over surgery because of the patient’s comorbidities, overall condition, and advanced age. To ensure negative vertical margins, endoscopic intermuscular dissection was performed instead of endoscopic submucosal dissection. Endoscopic intermuscular dissection is a technique that involves precise dissection within the intermuscular space between the inner and outer layers of the muscularis propria, in this case between the inner layers (Figure B). This approach is primarily indicated for lower rectal cancers with deep submucosal invasion or cases with significant fibrosis. No complications occurred during or after the procedure (Figure C). Histopathological examination revealed well to moderately differentiated adenocarcinoma with slight invasion into the muscularis propria (Figure D). The muscularis propria was confirmed in the resected specimen. Lymphatic invasion was absent, but vascular invasion was present. Follow-up computed tomography scans, performed every six months, have shown no evidence of recurrence two and a half years posttreatment.
Footnotes
Conflicts of Interest: The authors disclose no conflicts.
Funding: The authors report no funding.
Ethical Statement: This study did not require the approval of a review board.
Reporting Guidelines: None.