Abstract
Purpose
The effectiveness of exercise therapy for moderate adolescent idiopathic scoliosis and its potential benefits when combined with other treatments require further investigation. This systematic review and meta-analysis evaluated the efficacy of exercise therapy as a conservative management strategy for AIS.
Methods
Following PRISMA guidelines, we searched PubMed, Cochrane Library, Embase, and Web of Science up to June 4, 2024, for RCTs. Eligible studies included AIS patients (10–18 years, Cobb angle 20°–45°) undergoing various exercise therapies, such as scoliosis-specific exercises and core stabilization training. Primary outcomes included Cobb angle, ATR, trunk appearance, QoL, and respiratory function. Data extraction and risk-of-bias assessment followed Cochrane guidelines, and study quality was evaluated using the 11-item PEDro scale. Meta-analyses were conducted based on standardized mean differences.
Results
Eight RCTs with nine intervention groups were analyzed. At six months, exercise alone showed no significant advantage over bracing in improving Cobb angle, ATR, QoL, or trunk appearance (p < 0.05). However, exercise combined with other therapies significantly improved Cobb angle (MD = -6.11, 95% CI: -9.21 to -3.02), QoL (SMD = 0.89, 95% CI: 0.27 to 1.51), and lung function (SMD = 0.46, 95% CI: 0.13 to 0.80) at three months. These effects persisted for Cobb angle at six months (MD = -4.87, 95% CI: -8.77 to -0.98).
Conclusions
Low to moderate evidence suggests exercise alone is comparable to bracing for AIS, while exercise combined with other therapies offers short-term benefits for Cobb angle, QoL, and lung function.
Keywords: Scoliosis, Exercise, Systematic review, Meta-analysis
Introduction
Adolescent idiopathic scoliosis (AIS), the most common form of scoliosis of unknown cause,1 is diagnosed when the Cobb angle on the posterior-anterior radiographs exceeds 10° while standing. Approximately 90% of cases are diagnosed or worsen during puberty before bone development reaches maturity.2 At present, the prevalence of AIS reported by many studies around the world ranges from 3% to 14%.3–10 Severe scoliosis may have long-term adverse impacts on health, such as appearance problems, lung disease, psychological effects, and reduced quality of life.11,12 Reducing spinal deformities can be difficult13 depending on the range of motion of the spine and limited motor function.14,15 Early identification and effective treatment of scoliosis can slow or stop the development of scoliosis before bone development matures, thereby improving long-term outcomes in adulthood.1 The Society On Scoliosis Orthopaedic and Rehabilitation Treatment (SOSORT) made recommendations based on Cobb angle: only observation at 10-20°, observation or wearing of braces at 20°-25° and wearing of braces at 26°-45°.16 In the treatment of scoliosis of less than 25° Cobb, specific exercise is recommended to avoid the use of a brace.17 Too many doctors adopted the so-called “wait and see” approach when assessing patients with spinal curvature ranging between 10°-25°. However, over the past decade, various stakeholders, including parents of AIS patients, have advocated for a revision of this “watch” management protocol for scoliosis.18 Current best practice guidelines for AIS brace treatment recommend considering scoliosis-specific exercises in conjunction with bracing.19 Additionally, adverse effects resulting from bracing, such as muscle weakness, can be mitigated.20
Exercise therapy has demonstrated promising outcomes in the management of AIS, including core strength training, aerobic exercises, Schroth therapy13,21,22 and so on. Despite limited evidence quality from two studies,23,24 findings suggest that integrating exercise therapy with other modalities may yield superior results compared to treatments such as electrical stimulation, traction, and posture training in mitigating scoliosis progression among patients with mild AIS. Prior systematic reviews and meta-analyses have highlighted the positive effects of exercise either as a standalone intervention or in conjunction with other therapies like bracing.25,26 To our knowledge, no systematic literature review or meta-analysis has reported the efficacy of exercise therapy in patients with moderate AIS. For patients with moderate AIS at this special stage, the effect of exercise therapy compared with other therapies and whether exercise combined with other therapies is more effective than monotherapy deserve further study.
The Scoliosis Research Society (SRS) has developed standard care guidelines with Cobb angle as the primary outcome. However, Cobb angle correlates poorly with the overall quality of life (QoL).27 Therefore, in addition to Cobb angle, it is important to evaluate patient-relevant outcomes such as QoL. SOSORT suggests that the goals of conservative AIS treatment can be divided into two groups: morphological and functional (physiological and psychological)11 including radiology, aesthetics, quality of life, mental health, and disability.28 Therefore, this meta-analysis conducted a quantitative synthesis of published studies according to guidelines to investigate the effects of exercise on trunk morphology and function in AIS patients. This meta-analysis was designed to examine the efficacy of exercise therapy in patients with moderate AIS in multiple randomized controlled trials (RCTs) by calculating the overall effect size to draw more evidence-based conclusions as a conservative management strategy for adolescent idiopathic scoliosis.
Method
This study was conducted following the Cochrane Handbook29 and Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines30 for systematic reviews. This review was registered in the International Prospective Register of Systematic Reviews (PROSPERO) under the identification number (CRD 42023432333).
We searched PubMed, Cochrane Library, Embase, and Web of Science from the beginning to June 5, 2024. All search strategies were completed by an experienced librarian (WRR) and are summarized in Appendix 1. Citation tracking was performed for the included literature and related systematic reviews. Grey literature searching included references included studies and conference proceedings of the following organizations: the International Society on Scoliosis Orthopaedic and Rehabilitation Treatment, the International Meeting on Advanced Spine Technique, and the Annual Meeting of Scoliosis Research Society. For studies with no results, researchers contacted the original authors by email.
Two reviewers (ZP and LM) independently screened the titles and abstracts of the eligible studies. Studies were included and imported the results into Zotero if they met the following criteria: (1) populations: aged between 10 to 18 years old diagnosed with AIS, cobb between 20°-45°; (2) intervention: exercise therapies; (3) controls: other therapies excluding exercise; (4) Cobb angle, angle of trunk rotation (ATR), trunk appearance, QoL, and respiratory function. ATR and Cobb angle are the two golden standards for evaluating spinal curvature31 ; (5) study design: clinical controlled trial. If the screening could not be judged by title and abstract, read the full text. The kappa (κ) statistics, an index of the observer disagreement that compares the agreement found against that which might be expected by chance, was used to judge the consistency of the screening results between the two reviewers32 (0-0.2 poor, 0.2-0.4 fair, 0.4-0.6 moderate, 0.6-0.8 good, 0.8-1.0 very good). All disagreements were decided by the discussion of two other reviewers (HYW and WJL).
Assessment of characteristics of studies
Quality and risk of bias of included studies
The 11-item PEDro scale was used to assess the quality of included studies by two independent reviewers (ZP and LM).33,34 One item of the PEDro Scale (eligibility criteria) was related to external validity and was not used to calculate the total score. A study with a score ≥ 6 was considered high quality as reported previously.35
Two researchers (HYW and WJL) independently assessed the risk of bias in RCTs using the Cochrane risk-of-bias tool (Review Manager 5.3). The risk of bias was rated as low risk, high risk, or uncertain from the following seven domains: (1) random-sequence generation (selection bias); (2) allocation concealment (selection bias); (3) blinding of participants and personnel (performance bias); (4) blinding of outcome assessment (detection bias); (5) incomplete outcome data (attrition bias); (6) selective reporting (reporting bias); (7) other bias.29 Methods for evaluating the risk of bias of each article included: low risk of bias: evaluate the results of all items are low risk of bias; unclear risk of bias: evaluate the results of one or more items for bias risk uncertainty; high risk of bias assessment results of one or more items for the high risk of bias. The results were summarized using Review Manager 5.3 and all disagreements were settled by the discussion of two other reviewers (WRR and CXW). Both tools are reliable in assessing research quality and assessing the risk of bias.33,36
Data synthesis
The results were quantitatively synthesized according to the results considered: Cobb angle, QoL, ATR, trunk appearance, and lung function. All outcome indicators were continuous variables and the data were pooled and analyzed using Review Manger 5.3. Researchers pooled MD if tools for assessing morphology or function were consistent within groups, and pooled standardized mean difference (SMD) to eliminate the differences if tools or units were inconsistent within groups. Outcomes were expressed as MD or SMD between groups and 95% confidence interval (CI).28
Data extraction and analysis
Following a standardized procedure, two independent researchers (HYW and WJL) completed the data extraction and analysis, during which all discrepancies were resolved by discussion with two other researchers (WRR and CXW). The mean difference (MD) and standard deviation (SD) between the baseline and post-intervention or follow-up results reported in the included studies were extracted or converted into a standard format to ensure that our meta-analysis could be performed successfully. For each study, the following information was extracted: first author, year of publication, experimental group size, control size, gender and age of participants, outcome measures, intervention mode, and intervention duration. Table 2 (online only) illustrates the data for the eight included studies. There was no blinding of study authors, institutions, or journals during the data extraction process. If the research is inadequate or unclear, we will attempt to contact the authors for more details. Cobb angle, ATR, trunk appearance, QoL, and lung function were coded as results of the exercise intervention to calculate effect size.
Table 2. Methodological classification assessed by PEDro scale.
| Criteria | Marlene 2021 40 |
Zheng 2018 41 |
Moawd 2023 42 |
Gao 2019 43 |
Yagci 2018 44 |
Basbug 2023 45 |
Athanasopoulos 1999 46 |
Gözde Gür 2016 47 |
Cumulative score∗ |
|---|---|---|---|---|---|---|---|---|---|
| Eligibility criteria specified? | √ | √ | √ | √ | √ | √ | √ | √ | 8 |
| Random allocation? | √ | √ | √ | √ | √ | √ | √ | √ | 8 |
| Concealed allocation? | √ | √ | × | √ | × | √ | × | √ | 5 |
| Baseline comparability? | √ | √ | √ | √ | √ | √ | × | √ | 7 |
| Blind participants? | × | × | × | × | × | √ | × | √ | 2 |
| Blind therapists? | × | × | × | × | × | √ | × | × | 1 |
| Blind assessors? | √ | × | √ | √ | √ | √ | × | × | 5 |
| Follow-up? | × | × | × | × | × | × | × | × | 0 |
| Intention-to-treat analysis? | × | × | × | × | √ | × | √ | √ | 3 |
| Group comparisons? | √ | √ | √ | √ | √ | √ | × | √ | 7 |
| Point and variability measures? | √ | √ | √ | √ | √ | √ | √ | √ | 8 |
| Cumulative score | 7 | 6 | 6 | 7 | 7 | 9 | 4 | 8 | 6.75† |
∗Out of the 8 total studies.
†Maximum score of 10.
Assessment of quality of evidence
The quality of evidence was assessed using Grade evidence profiles. The quality of the evidence applies to each outcome, and this classification classifies the evidence as “high”, “medium”, “low” or “very low”. These levels imply a gradient of confidence in estimates of summary measures of treatment effect. Randomized controlled trials begin as high quality. The quality of evidence in meta-analyses is downgraded according to the following:
study limitations (risk of bias: drop one or two grades if more than 25% or 50% of participants came from studies of poor or average methodological quality; Lack of randomization or assignment hiding, no sample size estimation or blind method);
inconsistency of results (If there is significant heterogeneity in the outcome measure or intervention, or if the I2 value is ≥50%, drop one level);
indirectness of evidence (If a different population, intervention, or comparator is included, the level is lowered);
imprecision of estimates (wide confidence intervals crossing a decision threshold: If the 95% confidence interval of the SMD is greater than 0.2 points, it is reduced by one level; If the 95% CI in both directions is>0.5 points, then two levels are reduced.); one level was also downgraded if the 95% CI of the risk ratio crossed the null value when the sample sizes were<50 individuals and two levels when the sample sizes were ≤30 individuals)
e.publication bias (missing evidence, typically from studies that show no effect).37,38
Homogeneity
Clinical heterogeneity was determined by reviewing the participants, intervention, and control therapies. Study heterogeneity was assessed using the inconsistency index (I2 -statistic) with values of 25-50%, 50-75%, and 75-100%, indicating low, medium, and high heterogeneity, respectively. When significant heterogeneity existed (I2 ≥50%, p <0.1), sensitivity or subgroup analyses were performed to explore the source of heterogeneity. If the cause of heterogeneity could not be identified and the heterogeneity was within the allowed range, a random-effects model was used to pool the effect size.39
We planned to assess reporting bias using Egger’s test and a graphical aide funnel plot.29 Egger’s test mainly uses the linear regression method to detect whether there is a systematic deviation between the effect size and its standard error. In the absence of publication bias, the distribution of effect sizes should be symmetrical, with no systematic bias. Publication bias was evaluated visually by creating funnel plots via the Review Manager 5.3 version, as well as by conducting Egger’s test using the Stata 12.0 version.
The data was extracted and entered into Microsoft Excel software, statistical analysis was performed using Review Manager (RevMan 5.3) and Stata 12.0 version. P<0.05 was considered statistically significant.
Results
Study selection
Initially, 244 studies were extracted by searching the database; citations tracked 15 studies. 179 studies did not meet the inclusion criteria after screening the title and abstract. Of the remaining 65 studies, 57 were excluded when the full article was reviewed. Therefore, the meta-analysis included eight studies (Table 1), including nine experimental and control groups. The agreement between reviewers was calculated by kappa, with a value of 0.86. The inclusion flow chart (Figure 1) shows the number of studies excluded and the reasons for exclusion.
Table 1. Basic characteristics of exercise and control group in included studies.
| Experimental design | Study | Group | N (drop out) |
Mean age (sd) |
Gender (male/ female) |
Risser Sign | Program design and type | Outcome type | Period |
|---|---|---|---|---|---|---|---|---|---|
| Exercise: brace | Marlene 202140 Sweden |
Experimental | 45 (5) | 12.6 (1.4) | 33/12 | NR | Experimental: A 60-90 minute SSE session is held once a month, and a 30-minute SSE session is held at home the rest of the time. Control: Hyoercorrective Boston brace (night shift) |
Cobb angle ATR (Scoliometer) HR-QOL (SRS-22r) Trunk appearance (pSAQ) |
6months |
| Control | 45 (5) | 12.7 (1.4) | 39//6 | ||||||
| Zheng 201841 China |
Experimental | 30 (1) | 12.4 (0.9) | 22/7 | 0~2 | Experimatal: Take the 1.5-hour supervised SEAS course in the clinic every 2 to 3 months + home exercise: 10-15 min/day. Control: TLSO (23h) |
Cobb angle ATR (Radiology) HR-QOL (SRS-22) Trunk appearance (shoulder balance) |
6months 12months |
|
| Control | 30 (6) | 12.3 (0.8) | 19/5 | ||||||
| Moawd 202342 Saudi Arabia |
Experimental | 14 (1) | 14.1 (1.2) | 0/13 | NR | Experimental: Five days a week, 10 to 15 minutes a day of conventional scoliosis exercises, which include pelvic leaning back, catwalk, double leg abdominal compression, and standing on one leg. Control: Cheneau Gensingen Brace |
Cobb angle ATR Lung function (FVC) |
8weeks 6mmonths |
|
| Control | 14 (2) | 13.8 (1.5) | 0/12 | ||||||
| Exercise+other: others | Gao 201943 China |
Experimental | 25 (2) | 12.22 (1.35) | 18/5 | 0~2 | Experimental: Subjects are taught in the scoliosis clinic every 2-3 months, followed by 40 minutes of clinical therapy per week and 10-15 minutes of home exercise per day. Control: TLSO (23h) |
Cobb angle Lung function (FVC) |
4weeks 6months |
| Control | 25 (3) | 12.14 (1.32) | 18/4 | ||||||
| Yagci 201844 Turkey |
Experimental | 10 (0) | 14.20 (2.04) | 10/0 | 1~3 | Experimental: BBAT + Traditional Exercise + brace, home exercise 1 h/session, 5sessions/week Control: Traditional Exercise only + brace same dosage as the study group |
Cobb angle ATR (Scoliometer) HR-QoL (SRS-22) Trunk appearance (POTSI) |
10weeks | |
| Control | 10 (0) | 13.60 (1.65) | 10/0 | ||||||
| Basbug 202345 Turkey |
Experimental | 18 (1) | 13.9 (1.83) | 17/1 | NR | Experimental: A 45-minute home exercise program for scoliosis combined with IMT, inspiratory muscle training using the Threshold IMT device ® twice a day for 15 minutes/ times Control: Scoliosis home training program only |
Lung function (FVC) | 8weeks | |
| Control | 18 (1) | 13.7 (1.8) | 17/1 | ||||||
| Athanasopoulos 199946 Greece |
Experimental | 20 (0) | 13.54 (0.16) | 20/0 | 0~3 | Experimental: Interval aerobic training four times a week. The training intensity is 80%-100% of the load so that the subject's heart rate reaches 170 beats/min. During each training session, the subjects performed 30 minutes of cycling exercise for 5 to 15 minutes at a time, combined with brace therapy. Control: Boston brace |
Lung function (FVC) | 8weeks | |
| Control | 20 (0) | 13.62 (0.18) | 20/0 | ||||||
| Gözde Gür 201647 Turkey |
Experimental | 12 (0) | 14.2 (1.8) | 11/1 | 2 (0.6) | Experimental: Twice a week, 1-hour core training program + traditional scoliosis home exercise 22h wearing SpoRT brace Control: Traditional exercise + 22h wearing SpoRT brace |
Cobb angle Trunk appearance (TAPS) HR-QoL (SRS-22 ) |
10weeks | |
| Control | 13 (0) | 14 (1.6) | 13/0 | ||||||
| Moawd 202342 Saudi Arabia |
Experimental | 14 (1) | 13.5 (1.2) | 0/13 | NR | Experimental: The intervention began with one hour of individual training per day for the first two weeks, followed by one hour of Schroth training per week, performed in three dimensions, including spinal elongation, pelvic alignment, thoracic rotation, and shoulder correction + wearing a Gensingen brace Control: Gensingen brace |
Cobb angle ATR (Scoliometer) Lung function (FVC) |
8weeks 6months |
|
| Control | 14 (1) | 13.8 (1.5) | 0/13 |
N (drop out): number of participants and number of drop out; NR: Not Reported; TLSO: thoracic-lumbar sacral orthoses; BBAT: Basic body awareness therapy; SPoRT: Scoliosis Physiotherapeutic Specific Exercises and Rigid Thoraco-lumbo-sacral Orthosis; FVC: Forced Vital Capacity.
Figure 1. PRISMA flow diagram of article inclusion.
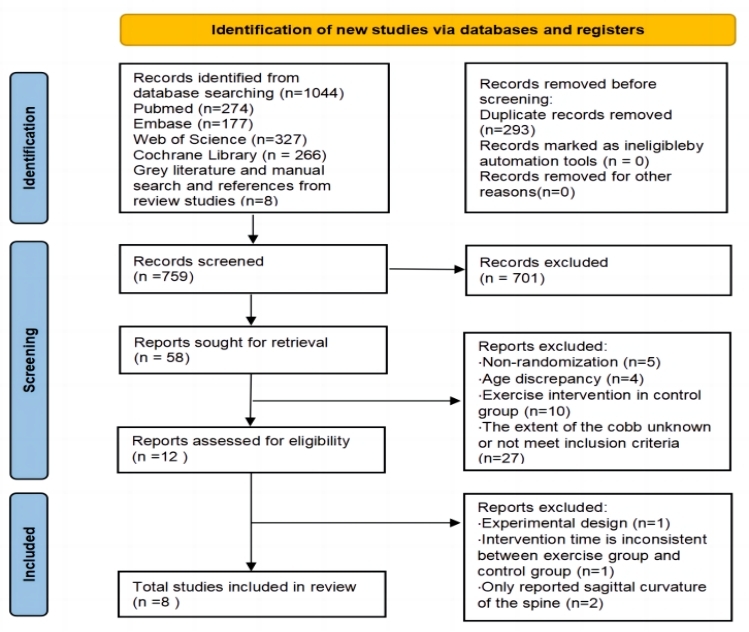
244 studies were extracted by searching the database; citations tracked 15 studies. Finally, 8 articles were included in the study. The flow chart shows the number of studies excluded and the reasons for exclusion.
Eligible Study Characteristics
A total of 9 parallel group studies were included in 8 articles, and 3 studies separately discussed the efficacy of exercise comparison braces in the treatment of moderate AIS, and exercise therapy was SSE, Scientific exercise approach to scoliosis (SEAS), and traditional scoliosis exercise. Six studies discussed the effects of exercise combined with other therapies versus the use of other therapies alone. Of these, five studies compared the effects of exercise combined with braces alone: SSE, Basic body awareness therapy (BBAT), interval aerobic training, core training, and Schroth; one study used inspiratory muscle training (IMT) in combination with home exercise to compare the therapeutic effects of home training alone. The duration of the exercise intervention ranged from 4 weeks to 12 months. Table 1 (online only) summarizes the relevant data for exercise training in the parallel group trial and the control group. In the summary analysis, the overall shedding rate was 9.06% (11/188) in the exercise group and 9.52% (18/189) in the control group, with a significant statistical difference (P<0.05). However, no adverse events such as worsening symptoms or death occurred among the participants during the training period.
Outcome measures
The results considered in this systematic review and meta-analysis were Cobb angle, ATR, QoL, lung function, and trunk appearance. Seven studies evaluated Cobb angle using anteroposterior and anteroposterior X-rays to measure the degree of scoliosis,40–44,47 five studies evaluated ATR.40–42,44,47 Four studies assessed QoL using the Scoliosis Research Society SRS-22.40,41,44,47 Four studies assessed spine trunk aesthetics using posterior trunk symmetry index (POSTI), shoulder balance, spinal appearance questionnaire (SAQ), and trunk appearance perception scale (TAPS).40,41,44,47 Four studies assessed lung function using forced vital capacity.42,43,45,46 All studies were evaluated against baseline and post-intervention outcome variables.
Quality and risk of bias within studies
PEDro
Of the eight studies assessed using the PEDro scale, seven were considered to be of high methodological quality (Table 2), with an average score of 6.75 across all trials. The most consistent items on the PEDro scale were randomization, measurement of variability in key outcomes, and comparison between groups, which were evident in almost all trials. Allocation hiding was used in 5 trials, and evaluator blindness was used in 5 trials. Three trials reported intention-to-treat analyses, and most of the studies had participants drop out and were unable to collect raw data. Only one trial blinded therapists, and the treatment was administered by different physiotherapists. The overall risk assessment of bias showed a high risk of bias in all included studies (Figure 2).40–47 The two reviewers agreed on the PEDro and Cochrane tools and did not use the kappa (κ) statistic.
Figure 2. The Cochrane risk-of-bias tool results.
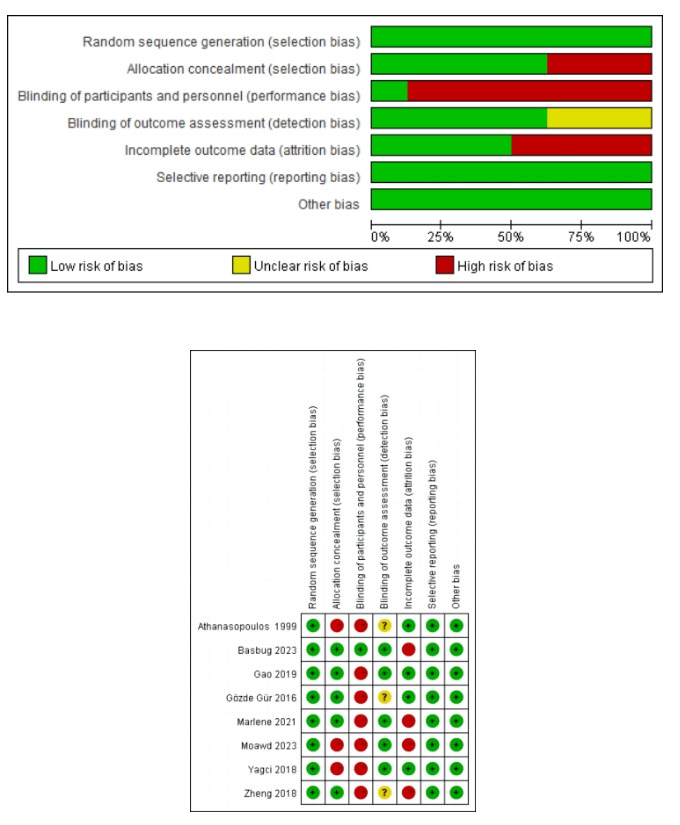
The overall risk assessment of bias showed a high risk of bias in all included studies because each study with at least one item was at high risk of bias.
Homogeneity
A random-effects model was used with treatment effects reported as the mean differences (MD) and 95% confidence intervals (CIs), 17 with significant differences set at P < 0.05. In this meta-analysis, since the homogeneity test results were statistically significant (Q= 101.31, df=6, p<0.001), and the I2 index was greater than 75% (I2 =94), as shown in Table 1, a random model was used for the main effect. The p values of the Egger’s and Begg’s tests were 0.549 and 0.764, respectively, indicating that no publication bias existed among the studies included. The symmetric pattern of the funnel plot also confirmed the preceding statistical tests visuall (Appendix 2).
Synthesis of results
Table 2 presents the detailed results of both the exercise and control groups included in the study. Across the nine analyzed studies, we identified 37 effect sizes. Results from the classification analysis by outcome (Supplementary Figure 1) indicate that the heterogeneity of the combined results for the four outcomes exceeded 50%. The synthesized findings revealed no significant difference in Cobb angle, ATR, QoL, and trunk appearance among patients with moderate AIS (P>0.05). Using the fixed-effect model combined with lung function only, revealed that the exercise group demonstrated a superior effect on this outcome compared to the control group (P=0.007). Sensitivity analysis, performed by altering the model method, yielded results (Appendix 3) indicating that, in contrast to the control group, the intervention effects of Cobb angle, ATR, trunk appearance, and QoL in the exercise group had statistical differences (P<0.05), which meant that the meta-analysis results of these outcomes were not robust.
In subgroup analysis, first, of the included studies, three studies separately discussed the effect of exercise comparative brace for moderate scoliosis, and six studies discussed the effect of exercise combined brace versus brace alone. Therefore, data were pooled to compare effect sizes according to the study design of the included studies. The effect of the study design on exercise is shown in Figures 3 to 5. Secondly, referring to the previous meta-analysis of exercise therapy for scoliosis,26 the outcomes were divided into 1-3 months and 3-6 months according to the length of treatment, to explore whether the duration of exercise intervention regulated the effectiveness of exercise. Table 3 summarized the quality of the evidence assessed, according to the GRADE Evidence Profiles.
Figure 3. Exercise: Brace (6 months).
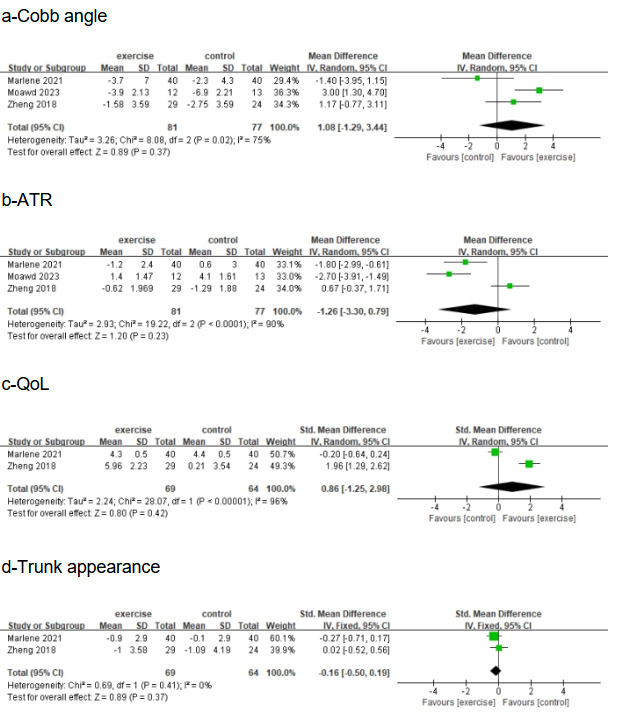
Forest plot of Cobb angle; b) forest plot of ATR; c) forest plot of QoL; d) forest plot of trunk appearance
Table 3. GRADE. Summary of evidence of the results.
| Outcomes | Number of studies | Risk of Bias | Ratio of studies (PEDro<6) |
Number of participants | Effect Absolute (95% CI) |
I2 | Quality of evidence (GRADE) |
|---|---|---|---|---|---|---|---|
| a.Exercise: brace(6months) | |||||||
| Cobb | 3 | 100% | 0% | 158 | MD 1.08[-1.29,3.44] | 75% | Very low a,b,c |
| ATR | 3 | 100% | 0% | 158 | MD -1.26[-3.30,0.79] | 90% | Very low a,b,c |
| QoL | 2 | 100% | 0% | 133 | SMD 0.86[-1.25,2.98] | 96% | Very low a,b,c |
| Trunk Appearance | 2 | 100% | 0% | 133 | SMD -0.16[-0.5,0.19] | 0% | Low a,c |
| b.Exercise + others: Others (1-3mmonths) | |||||||
| Cobb | 3 | 100% | 0% | 70 | MD -6.11[-9.21,-3.02] | 54% | Very low a,b,c |
| QoL | 2 | 100% | 0% | 45 | SMD 0.89 [0.27,1.51] | 0% | Very low a,c,d |
| Lung function | 4 | 100% | 25% | 144 | SMD 0.46[0.13,0.80] | 0% | Low a,c |
| ATR | 2 | 100% | 0% | 45 | MD -0.80[-2.79,1.19] | 0% | Very low a,c,d |
| Trunk appearance | 2 | 100% | 0% | 45 | SMD -6.62[-14.27,1.04] | 48% | Very low a,c,d |
| c.Exercise + others: Others (6months) | |||||||
| Cobb | 2 | 100% | 0% | 70 | MD -4.87[-8.77,-0.98] | 87% | Very low a,b,c |
| Lung function | 2 | 100% | 0% | 70 | SMD 1.21[-0.21 2.62] | 83% | Very low a,b,c |
GRADE: GRADE working group grades of evidence. CI: Confidence interval; MD: Mean difference; SMD: Standard mean difference. a: more than 25% of participants came from studies with poor or fair methodological quality; b: Statistical heterogeneity results downgrade (I2 > 50%); c: 95% CI of SMD >0.5 results downgrade; d: sample sizes <50 individuals results downgrade. High quality: Further research is very unlikely to change our confidence in the estimate ofeffect. Moderate quality: Furher research is likely to have an important impact on our confidence in the estimate of efiect and may change the estimate. Low quality: Furher research is very likely to have an important impact on our confidence in the estimate ofefect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate.
Exercise:Brace(6months)
The results and evidence levels of each sub-combination are shown in Table 3a and Figure 3. The heterogeneity of the study is still large, and only the heterogeneity of the combined trunk appearance results decreased to under 50%. The results of meta-analysis on Cobb angle, ATR and QoL are not robust. Low to moderate-quality evidence showed that exercise made no difference in improving Cobb angle, ATR, quality of life, and trunk appearance compared to brace therapy.
Exercise+others:Others (1-3months)
Table 3b and Figure 4 present the results of the study on the additional effects of exercise in the treatment of moderate AIS at the intervention time of 1 to 3 months.
Figure 4. Exercise+Others:Others (1-3months).
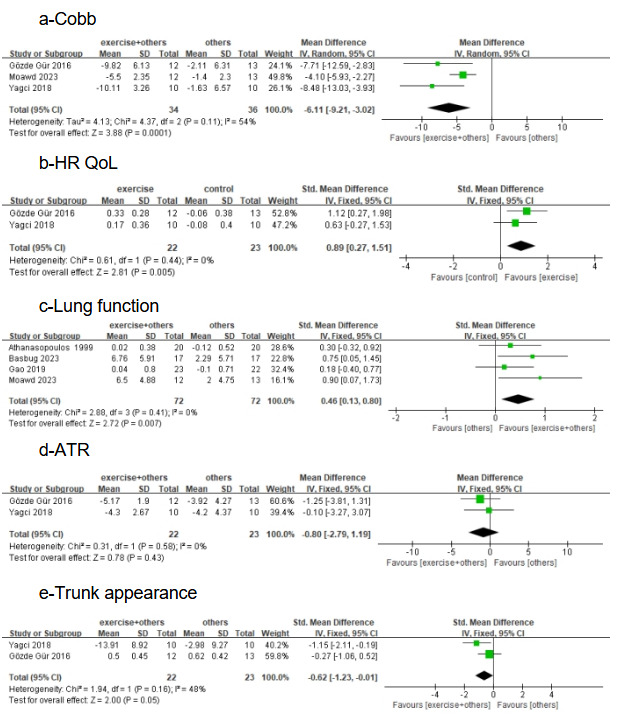
- forest plot of Cobb angle; b) forest plot of QoL; c) forest plot of lung function.; d) forest plot of Trunk Rotation Angle; e) forest plot of trunk appearance.
Effect of Exercise on Cobb Angle
Meta-analysis of three studies42,44,47 provided low-quality evidence, among which 4 studies had significant effect size estimates (P<0.0001), and the overall effect size was estimated to be MD= -6.11[95%CI, -9.21 to -3.02], as shown in figure 4. After pooled analysis by study type, the heterogeneity of all outcomes decreased. Based on the random effects model, The combined results were statistically significant: exercise combined with other therapies was more beneficial in reducing Cobb angle than the control group (Figure 4). The result of subgroup data merging changed compared with the original merging result.
Effect of Exercise on Quality of Life
Low-quality evidence was provided in a meta-analysis of 2 studies ,44,47 of which the effect size point was estimated to be significant (P=0.005), and the overall effect size point was estimated at SMD=0.89 [95%CI, 0.27 to 1.51], based on a fixed-effect model, compared with the control group. Exercise combined with other therapies is more effective in improving quality of life (Tables 3b and Figure 4).
Effect of Exercise on Lung Function
A meta-analysis of four studies42,43,45,46 provided moderate-quality evidence, four of which had significant effect size estimates (P=0.007), and an overall effect size estimate of SMD=0.46 [95%CI, 0.13 to 0.80] based on a fixed-effect model compared with controls. Exercise combined with other therapies is more beneficial in improving lung function (Tables 3b and Figure 4).
Effect of Exercise on Angle of Rotation
A meta-analysis of two studies ,44,47 two of which had insignificant effect size point estimates (P = 0.43), provided moderate-quality evidence that exercise combined with other therapies was more effective in improving ATR compared to controls, based on a fixed-effect model (Tables 3b and Figure 4).
Effect of Exercise on Trunk Appearance
A meta-analysis of two studies44,47 provided very low-quality evidence with no significant effect (P=0.05), based on a fixed-effect model, and showed no difference in reducing self-perception of trunk appearance with exercise combined with other therapies compared to controls (Tables 3b and Figure 4).
Exercise+Others: Others(6months)
Figure 5 and Table 3c show the additional effects of exercise for moderate AIS at the intervention time of 6 months.
Figure 5. Exercise + Others: Others (6 months).
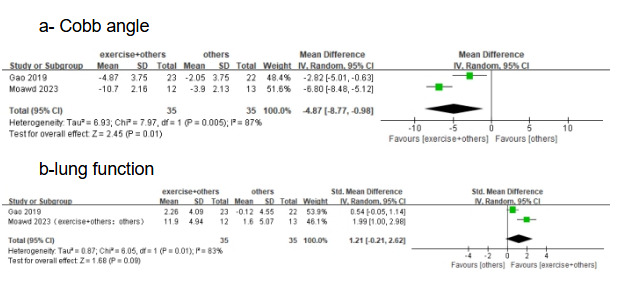
- forest plot of Cobb angle; b) forest plot of lung function.
Effect of Exercise on Cobb Angle
A meta-analysis of two studies42,43 provided low-quality evidence, with significant effect size estimates (P=0.01) and an overall effect size estimate of MD= -4.87[95%CI, -8.77 to -0.98], based on a random effects model, compared to a control group. Exercise combined with other therapies was more beneficial in reducing Cobb angle (Figure 5 and Table 3c).
Effect of Exercise on Lung Function
Low-quality evidence was provided by a meta-analysis of two studies ,42,43 two of which had insignificant effect size point estimates (P=0.12), and based on a random-effects model, exercise combined with other therapies made no difference in improving lung function compared to controls (Figure 5 and Table 3c).
A meta-analysis in the same intervention cycle showed no statistical difference between exercise alone and brace therapy in improving Cobb angle (P=0.37), showed in Supplementary Table 2, while the additional effects of exercise combined with other therapies were significant compared to the use of other therapies alone, with an effect size of Z=2.45 (P=0.01) (Figure 4a). Under the same study design, at short-term intervention, the combination of exercise and other therapies significantly improved Cobb angle, QoL, and lung function in patients compared to controls; however, with the extension of intervention time, lung function did not show significant differences despite significant changes in Cobb angle.
The quality of evidence assessed by the GRADE evidence profile (Table 3) showed that the overall quality of evidence for outcomes was low, which means that in the future, robust data with a low risk of bias may overturn some of the outcomes of the interventions evaluated in this meta-analysis.
Discussion
This systematic review and meta-analysis evaluated the effects of exercise therapy compared with other conservative therapies or in combination with other therapies on Cobb angle, ATR, QoL, trunk appearance, and lung function in patients with moderate AIS. However, the duration, frequency, etc. of treatment must be taken into account when developing guidelines.26 Therefore, we explored existing differences in intervention duration to determine the optimal minimum duration required for exercise to effectively improve patients’ clinical indications.
To date, there have been many systematic reviews and meta-analyses examining the efficacy of a certain exercise alone or in combination with other therapies for AIS.25,26,48 The results of this study are consistent with the results of previous systematic reviews and meta-analyses about exercise treating moderate AIS parents, namely, exercise therapy can reduce Cobb and improve QoL in AIS patients, and achieve a similar therapeutic effect. However, this study is the first to analyze the effects of exercise therapy in intervening with moderate AIS. Our results showed that at 6 months of intervention, exercise therapy did not differ from brace in improving Cobb angle, QoL, ATR, and trunk appearance. One article41 discussed the efficacy of the intervention at 12 months. Except for the significant increase in SRS-22 compared to 6 months, the duration of exercise intervention did not modulate the effectiveness of exercise. Cobb angle and SRS-22 in patients wearing the brace for 12 months were better than those at 6 months.
Exercise combined with other therapies was still more effective in improving Cobb angle and Qol than other therapies alone. Orthopedic surgeons and physiotherapists use Cobb angle to diagnose scoliosis, and improvements in Cobb angle reduce the need for surgery in AIS patients.26 The SRS standardized Cobb angle as the primary outcome measure in non-surgical studies.49 Typically, a threshold of 5° is described as the Cobb difference for clinically relevant improvement or deterioration.50 The mean differences observed according to the results of the systematic review and meta-analysis of this study (MD, -4.92; 95%CI, -6.11 to -9.21; I2 , 54%) close to the clinically relevant threshold. Park et al26 found a larger effect size in interventions lasting longer than 6 months compared to interventions lasting less than 6 months. However, in our study, two studies of exercise interventions lasting 6 months42,43 produced an effect (MD, -4.87; 95%CI, -8.77 to -0.98; Z, 2.45) that was not larger than that of interventions lasting 1 to 3 months (MD, -6.11; 95%CI, -9.21 to -3.02; Z, 3.88).41,46,47 It can be found that there are three types of exercise interventions under short-term intervention, namely core strength training, Basic Body Awareness Therapy, and Schroth therapy, while the two studies with 6-month intervention selected the therapies of SEAS and Schroth. Different types of exercise intervention may be the reason why the duration of intervention does not regulate the effect of the intervention. In addition, only one article extended the intervention time to 6 months, and this intervention result was consistent with the analysis results of Park et al26: the longer the intervention time, the more significant the improvement in Cobb angle. It is important to note that none of the studies had follow-up, and the follow-up of both short-term and long-term intervention effects deserves further investigation. In addition to Cobb, some studies have proposed Cobb angle and ATR as the gold standard for evaluating AIS.31 It is worth noting that not all radiographic scoliosis patients have trunk rotation.51 The difference between trunk rotation and actual curvature of the spine is increased during adolescence.52 This may explain why, with short-term intervention, exercise combined with brace therapy effectively improved Cobb angle in patients with moderate AIS compared to brace therapy alone, while ATR did not change significantly.
SRS-22 is the most common criterion for measuring QoL in idiopathic scoliosis.53 It has become an accepted QoL questionnaire to assess the perception of their condition in patients with scoliosis. The minimum significant difference in the questionnaire was between 0.7 and 0.4 minimum important change values for adolescents and adults.54 Four studies40,41,44,47 evaluated QoL using SRS-22 or SRS-22r. The results showed that exercise combined with other therapies could effectively improve QoL (SMD, 0.89;95%CI, 0.27 to 1.51; I2 , 0%), which exceeds the minimum significant change in AIS.
The quality of life and mental health of AIS patients are largely influenced by aesthetic self-perception and appearance .11,55 As a result, trunk aesthetics has gradually become a major concern for patients and families.28 This study analyzed the effects of exercise on the appearance of the spine. There was no difference in the combined outcome between the two study designs of subgroup analysis. However, after excluding one article, the efficacy of the exercise group was significantly better than that of the control group (P<0.05). This paper discusses the efficacy of SEAS compared with wearing rigid TLSO. Previous studies have found that two treatments, including the core stabilization of support and the support of scientific exercise methods for scoliosis, have similar effects in the short-term treatment of trunk appearance symmetry in patients with moderate AIS.
Limited lung function is an important clinical indication in patients with scoliosis, especially in patients with severe scoliosis with high chest wall inflation impedance.56 This meta-analysis considered lung function as an outcome. In this study, exercise combined with other therapies was more effective in improving lung function in AIS patients in the short term than other therapies alone (SMD, 0.46; 95%CI, 0.13 to 0.80; I2 , 0%) but this advantage does not occur consistently. When the intervention lasted for six months, the additional effect of exercise was diminished (p=0.12). Only one study46 reassessed and adjusted exercise intensity every two weeks. The lack of progression of other exercise interventions (Table 1) may contribute to this result, as cardiorespiratory functions adapt to exercise stimulation.57 Therefore, in the future, AIS exercise therapy should be designed according to the patient’s cardiopulmonary level, rather than maintaining a single intervention intensity.
Exercise combined with non-exercise management is recommended for patients with moderate AIS to improve quality of life or lung function. This study provides more references for the treatment of patients with moderate AIS and the selection of corresponding treatment cycles in clinical practice. Due to this study being based on a group of patients with moderate curvature (25°-40°) of AIS, generalizing the current findings to patients with mild or severe spinal malformations remains an important extension of this study.
Limitation
There are some limitations to the study. First, only a limited number of clinical trials were included to evaluate the effectiveness of exercise therapy for scoliosis, which can lead to unstable results, and the weight of a single study is too large and easily influenced by the results of individual studies. Second, of the nine parallel group trials included in the pooled analysis, three studies were designed to compare exercise with other therapies, while the remaining studies were designed to explore the additional effects of exercise combined with other therapies, highlighting the heterogeneity of the pooled analysis in this study. Three, The efficacy of exercise therapy may vary among adolescents of different ages, genders, and even ethnicities. However, very few studies in the included RCTs strictly defined certain demographic information of the subjects in a range, which led to this limitation in our meta-analysis. In the future, more targeted RCT studies are needed to compare the efficacy of exercise therapy for moderate AIS. Finally, most of the included studies were single-center based, with relatively short intervention duration and lack of follow-up, and longer multi-center, well-designed randomized controlled trials are needed in the future.
Conclusions
In conclusion, these results need to be treated with caution: very low to low evidence suggests that exercise is clinically equivalent to brace in improving Cobb angle, ATR, QoL, and trunk symmetry on moderate AIS in the long term. Very low to low evidence suggests that exercise combined with other therapies is more effective in improving Cobb angle, QoL, and lung function on moderate AIS in the short term compared to other therapies alone.
Authors’ contributions
Peng Zhao and Meng Li contributed equally to this work. Peng Zhao and Meng Li served as principal authors, had full access to all the data in the study, and took responsibility for the accuracy of the data analysis and its integrity. Peng Zhao and Meng Li prepared the initial manuscript draft, revised the article, and gave final approval. Yuwei He and Jialin Wang contributed to data acquisition and interpretation. Ruirui Wang and Xinwen Cui contributed to the conception and design.
Competing Interests
The authors of this article have no financial affiliations (including research funding) or involvement with any commercial organization to disclose.
Supplementary Material
a)forest plot of Cobb angle; b) forest plot of ATR; c) forest plot of QoL; d) forest plot of trunk appearance; e) forest plot of lung function.
Funding Statement
This research was supported by Project 24-51 Supported by the Fundamental Research Funds for the China Institute of Sport Science.
References
- Screening for Adolescent Idiopathic Scoliosis: US Preventive Services Task Force Recommendation Statement. US Preventive Services Task Force. Grossman D. C., Curry S. J.., et al. 2018JAMA. 319(2):165–172. doi: 10.1001/jama.2017.19342. [DOI] [PubMed] [Google Scholar]
- Epidemiology of adolescent idiopathic scoliosis. Konieczny M. R., Senyurt H., Krauspe R. 2013J Child Orthop. 7(1):3–9. doi: 10.1007/s11832-012-0457-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prevalence of adolescent idiopathic scoliosis in Turkey: an epidemiological study. Yılmaz H., Zateri C., Kusvuran Ozkan A.., et al. 2020The Spine Journal. 20(6):947–955. doi: 10.1016/j.spinee.2020.01.008. [DOI] [PubMed] [Google Scholar]
- A 5-year epidemiological study on the prevalence rate of idiopathic scoliosis in Tokyo: school screening of more than 250,000 children. Ueno M., Takaso M., Nakazawa T.., et al. 2011J Orthop Sci. 16(1):1–6. doi: 10.1007/s00776-010-0009-z. [DOI] [PubMed] [Google Scholar]
- Epidemiological study of adolescent idiopathic scoliosis in Eastern China. Zheng Y., Dang Y., Wu X.., et al. 2017J Rehabil Med. 49(6):512–519. doi: 10.2340/16501977-2240. [DOI] [PubMed] [Google Scholar]
- Idiopathic scoliosis in Korean schoolchildren: a prospective screening study of over 1 million children. Suh S. W., Modi H. N., Yang J. H.., et al. 2011Eur Spine J. 20(7):1087–1094. doi: 10.1007/s00586-011-1695-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prevalence of Idiopathic Scoliosis in Chinese Schoolchildren: A Large, Population-Based Study. Hengwei F., Zifang H., Qifei W.., et al. 2016Spine (Phila Pa 1976) 41(3):259–264. doi: 10.1097/BRS.0000000000001197. [DOI] [PubMed] [Google Scholar]
- Prevalence of Scoliosis Among Primary and Middle School Students in Mainland China: A Systematic Review and Meta-analysis. Zhang H., Guo C., Tang M.., et al. 2015Spine. 40(1):41–49. doi: 10.1097/BRS.0000000000000664. [DOI] [PubMed] [Google Scholar]
- Prevalence of scoliosis in secondary school children in Osogbo, Osun State, Nigeria. Jenyo M. S., Asekun-Olarinmoye E. O. 2005Afr J Med Med Sci. 34(4):361–364. [PubMed] [Google Scholar]
- RATE OF VENTILATORY DISORDERS IN PATIENTS WITH THE IDIOPATHIC SCOLIOSIS AFTER THE CORRECTIVE OPERATION AND INFLUENCE OF REHABILITATION ON VENTILATORY PARAMETERS. Barinow-Wojewudzki A., Rychlewski T., Laurentowska M.
- 2016 SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Negrini S., Donzelli S., Aulisa A. G.., et al. 2018Scoliosis. 13(1):3. doi: 10.1186/s13013-017-0145-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study. Weinstein S. L., Dolan L. A., Spratt K. F.., et al. 2003JAMA. 289(5):559–567. doi: 10.1001/jama.289.5.559. [DOI] [PubMed] [Google Scholar]
- Exercises for adolescent idiopathic scoliosis. Romano M., Minozzi S., Bettany-Saltikov J.., et al. 2012Cochrane Database Syst Rev. 2012(8):CD007837. doi: 10.1002/14651858.CD007837.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muscle dysfunction and exercise limitation in adolescent idiopathic scoliosis. Martínez-Llorens J., Ramírez M., Colomina M. J.., et al. 2010Eur Respir J. 36(2):393–400. doi: 10.1183/09031936.00025509. [DOI] [PubMed] [Google Scholar]
- Association between physical activity and scoliosis: a prospective cohort study. Tobias J. H., Fairbank J., Harding I.., et al. 2019International Journal of Epidemiology. 48(4):1152–1160. doi: 10.1093/ije/dyy268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Screening for Adolescent Idiopathic Scoliosis: Evidence Report and Systematic Review for the US Preventive Services Task Force. Dunn J., Henrikson N. B., Morrison C. C.., et al. 2018JAMA. 319(2):173. doi: 10.1001/jama.2017.11669. [DOI] [PubMed] [Google Scholar]
- Exercises for adolescent idiopathic scoliosis. Romano M., Minozzi S., Bettany-Saltikov J.., et al. 2012Cochrane Database Syst Rev. 2012(8):CD007837. doi: 10.1002/14651858.CD007837.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Physiotherapy scoliosis-specific exercises – a comprehensive review of seven major schools. Berdishevsky H., Lebel V. A., Bettany-Saltikov J.., et al. 2016Scoliosis. 11(1):20. doi: 10.1186/s13013-016-0076-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Establishing consensus on the best practice guidelines for the use of bracing in adolescent idiopathic scoliosis. Roye B. D., Simhon M. E., Matsumoto H.., et al. 2020Spine Deform. 8(4):597–604. doi: 10.1007/s43390-020-00060-1. [DOI] [PubMed] [Google Scholar]
- The effectiveness of combined bracing and exercise in adolescent idiopathic scoliosis based on SRS and SOSORT criteria: a prospective study. Negrini S., Donzelli S., Lusini M.., et al. 2014BMC Musculoskelet Disord. 15:263. doi: 10.1186/1471-2474-15-263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Physiotherapeutic scoliosis-specific exercises for adolescents with idiopathic scoliosis. Bettany-Saltikov J., Parent E., Romano M.., et al. 2014EUROPEAN JOURNAL OF PHYSICAL AND REHABILITATION MEDICINE. 50(1) [PubMed] [Google Scholar]
- Core stabilization exercises versus scoliosis-specific exercises in moderate idiopathic scoliosis treatment. Yagci G., Yakut Y. 2019Prosthetics & Orthotics International. 43(3):301–308. doi: 10.1177/0309364618820144. [DOI] [PubMed] [Google Scholar]
- Exercises reduce the progression rate of adolescent idiopathic scoliosis: results of a comprehensive systematic review of the literature. Negrini S., Fusco C., Minozzi S.., et al. 2008Disabil Rehabil. 30(10):772–785. doi: 10.1080/09638280801889568. [DOI] [PubMed] [Google Scholar]
- Exercise therapy in treatment of essential S-shaped scoliosis: Evaluation of Cobb angle in breast and lumbar segment through a follow-up of half a year. Wan L., Wang G. X., Bian R. 2005Chinese Journal of Clinical Rehabilitation. 9:82–84. [Google Scholar]
- The effectiveness of Schroth exercises in adolescents with idiopathic scoliosis: A systematic review and meta-analysis. Burger M., Coetzee W., du Plessis L. Z.., et al. 2019S Afr J Physiother. 75(1):904. doi: 10.4102/sajp.v75i1.904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Effects of the Schroth exercise on idiopathic scoliosis: a meta-analysis. Park J. H., Jeon H. S., Park H. W. 2018Eur J Phys Rehabil Med. 54(3) doi: 10.23736/S1973-9087.17.04461-6. [DOI] [PubMed] [Google Scholar]
- The association between Scoliosis Research Society-22 scores and scoliosis severity changes at a clinically relevant threshold. Parent E. C., Wong D., Hill D.., et al. 2010Spine (Phila Pa 1976) 35(3):315–322. doi: 10.1097/BRS.0b013e3181cabe75. [DOI] [PubMed] [Google Scholar]
- Why do we treat adolescent idiopathic scoliosis? What we want to obtain and to avoid for our patients. SOSORT 2005 Consensus paper. Negrini S., Grivas T. B., Kotwicki T.., et al. 2006Scoliosis. 1:4. doi: 10.1186/1748-7161-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cumpston M., Li T., Page M. J.., et al. 2019Cochrane Database Syst Rev. 10(10):ED000142. doi: 10.1002/14651858.ED000142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preferred Reporting Items for a Systematic Review and Meta-analysis of Diagnostic Test Accuracy Studies: The PRISMA-DTA Statement. McInnes Matthew D. F.., et al. 2018JAMA. 319(4):388–396. doi: 10.1001/jama.2017.19163IF. https://doi.org/10.1001/jama.2017.19163IF [DOI] [PubMed] [Google Scholar]
- Scoliometer measurements of patients with idiopathic scoliosis. Coelho D. M., Bonagamba G. H., Oliveira A. S. 2013Braz J Phys Ther. 17(2):179–184. doi: 10.1590/S1413-35552012005000081. [DOI] [PubMed] [Google Scholar]
- Altman D. G. Practical statistics for medical research. [DOI] [Google Scholar]
- Reliability of the PEDro scale for rating quality of randomized controlled trials. Maher C. G., Sherrington C., Herbert R. D.., et al. 2003Phys Ther. 83(8):713–721. doi: 10.1093/ptj/83.8.713. [DOI] [PubMed] [Google Scholar]
- The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. de Morton N. A. 2009Aust J Physiother. 55(2):129–133. doi: 10.1016/S0004-9514(09)70043-1. [DOI] [PubMed] [Google Scholar]
- Pre-operative interventions (non-surgical and non-pharmacological) for patients with hip or knee osteoarthritis awaiting joint replacement surgery--a systematic review and meta-analysis. Wallis J. A., Taylor N. F. 2011Osteoarthritis Cartilage. 19(12):1381–1395. doi: 10.1016/j.joca.2011.09.001. [DOI] [PubMed] [Google Scholar]
- Reliability of the revised Cochrane risk-of-bias tool for randomised trials (RoB2) improved with the use of implementation instruction. Minozzi S., Dwan K., Borrelli F.., et al. 2022J Clin Epidemiol. 141:99–105. doi: 10.1016/j.jclinepi.2021.09.021. [DOI] [PubMed] [Google Scholar]
- The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. Higgins J. P. T., Altman D. G., Gotzsche P. C.., et al. 2011BMJ. 343(oct18 2):d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clinimetrics: Grading of Recommendations, Assessment, Development and Evaluation (GRADE) Xie C. X., Machado G. C. 2021Journal of Physiotherapy. 67(1):66. doi: 10.1016/j.jphys.2020.07.003. [DOI] [PubMed] [Google Scholar]
- Fixed-Effect vs Random-Effects Models for Meta-Analysis: 3 Points to Consider. Dettori J. R., Norvell D. C., Chapman J. R. 2022Global Spine J. 12(7):1624–1626. doi: 10.1177/21925682221110527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Six-Month Results on Treatment Adherence, Physical Activity, Spinal Appearance, Spinal Deformity, and Quality of Life in an Ongoing Randomised Trial on Conservative Treatment for Adolescent Idiopathic Scoliosis (CONTRAIS) Dufvenberg M., Diarbakerli E., Charalampidis A.., et al. 2021J Clin Med. 10(21):4967. doi: 10.3390/jcm10214967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whether Orthotic Management and Exercise are Equally Effective to the Patients With Adolescent Idiopathic Scoliosis in Mainland China?: A Randomized Controlled Trial Study. Zheng Y., Dang Y., Yang Y.., et al. 2018Spine. 43(9):E494–E503. doi: 10.1097/BRS.0000000000002412. [DOI] [PubMed] [Google Scholar]
- Combined effect of Schroth method and Gensingen brace on Cobb’s angle and pulmonary functions in adolescent idiopathic scoliosis: a prospective, single blinded randomized controlled trial. Moawd S. A., Nambi G., El-Bagalaty A. E.., et al. doi: 10.26355/eurrev_202301_31061. [DOI] [PubMed]
- Could the Clinical Effectiveness Be Improved Under the Integration of Orthotic Intervention and Scoliosis-Specific Exercise in Managing Adolescent Idiopathic Scoliosis?: A Randomized Controlled Trial Study. Gao C., Zheng Y., Fan C.., et al. 2019Am J Phys Med Rehabil. 98(8):642–648. doi: 10.1097/PHM.0000000000001160. [DOI] [PubMed] [Google Scholar]
- Effectiveness of basic body awareness therapy in adolescents with idiopathic scoliosis: A randomized controlled study1. Yagci G., Ayhan C., Yakut Y. 2018BMR. 31(4):693–701. doi: 10.3233/BMR-170868. [DOI] [PubMed] [Google Scholar]
- Effects of inspiratory muscle training on respiratory muscle strength, respiratory function and functional capacity in adolescents with idiopathic scoliosis: A randomized, controlled trial. Basbug G., Gurses H. N., Zeren M.., et al. 2023Wien Klin Wochenschr. 135(11-12):282–290. doi: 10.1007/s00508-023-02197-1. [DOI] [PubMed] [Google Scholar]
- The effect of aerobic training in girls with idiopathic scoliosis. Athanasopoulos S., Paxinos T., Tsafantakis E.., et al. 2007Scandinavian Journal of Medicine & Science in Sports. 9(1):36–40. doi: 10.1111/j.1600-0838.1999.tb00204.x. [DOI] [PubMed] [Google Scholar]
- The effectiveness of core stabilization exercise in adolescent idiopathic scoliosis: A randomized controlled trial. Gür Gözde. Prosthetics and Orthotics International. doi: 10.1177/0309364616664151. [DOI] [PubMed]
- The effectiveness of Schroth method in Cobb angle, quality of life and trunk rotation angle in adolescent idiopathic scoliosis: a systematic review and meta-analysis. Ceballos-Laita L., Carrasco-Uribarren A., Cabanillas-Barea S.., et al. 2023Eur J Phys Rehabil Med. 59(2) doi: 10.23736/S1973-9087.23.07654-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on Bracing and Nonoperative Management. Richards B. S., Bernstein R. M., D’Amato C. R.., et al. 2005Spine (Phila Pa 1976) 30(18):2068–2077. doi: 10.1097/01.brs.0000178819.90239.d0. [DOI] [PubMed] [Google Scholar]
- Measurement of scoliosis and kyphosis radiographs. Intraobserver and interobserver variation. Carman D. L., Browne R. H., Birch J. G. 1990J Bone Joint Surg Am. 72(3):328–333. doi: 10.2106/00004623-199072030-00003. [DOI] [PubMed] [Google Scholar]
- Adolescent idiopathic scoliosis: etiology, anatomy, natural history, and bracing. Parent S., Newton P. O., Wenger D. R. 2005Instr Course Lect. 54:529–536. [PubMed] [Google Scholar]
- The effect of growth on the correlation between the spinal and rib cage deformity: implications on idiopathic scoliosis pathogenesis. Grivas T. B., Vasiliadis E. S., Mihas C.., et al. 2007Scoliosis. 2:11. doi: 10.1186/1748-7161-2-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Reliability and Concurrent Validity of the Scoliosis Research Society-22 Patient Questionnaire for Idiopathic Scoliosis. Asher M., Min Lai S., Burton D.., et al. 2003Spine. 28(1):63–69. doi: 10.1097/00007632-200301010-00015. [DOI] [PubMed] [Google Scholar]
- Responsiveness and Minimal Important Changes of the Scoliosis Research Society-22 Patient Questionnaire in Subjects With Mild Adolescent and Moderate Adult Idiopathic Scoliosis Undergoing Multidisciplinary Rehabilitation. Monticone M., Ambrosini E., Rocca B.., et al. 2017Spine. 42(11):E672–E679. doi: 10.1097/BRS.0000000000001923. [DOI] [PubMed] [Google Scholar]
- A Review of Quality of Life and Psychosocial Issues in Scoliosis. Tones M., Moss N., Polly D. W. 2006Spine. 31(26):3027–3038. doi: 10.1097/01.brs.0000249555.87601.fc. [DOI] [PubMed] [Google Scholar]
- High- and low-level pressure support during walking in people with severe kyphoscoliosis. Menadue C., Alison J. A., Piper A. J.., et al. 2010Eur Respir J. 36(2):370–378. doi: 10.1183/09031936.00115009. [DOI] [PubMed] [Google Scholar]
- Refuting the myth of non-response to exercise training: “non-responders” do respond to higher dose of training. Montero D., Lundby C. 2017J Physiol. 595(11):3377–3387. doi: 10.1113/JP273480. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
a)forest plot of Cobb angle; b) forest plot of ATR; c) forest plot of QoL; d) forest plot of trunk appearance; e) forest plot of lung function.


